Highlights
-
•
Factors of examination pressure of Bangladeshi tertiary level students are hardly researched.
-
•
Stress, anxiety and depression was evaluated using DASS-21 for 210 youths aged between 17–25 years.
-
•
The significant contributors are living with family, family time, sleeping pattern and diets.
Keywords: Mental health, Stress, Depression, Anxiety, Examination, Socio-demographic status
Abstract
An estimated 25% people suffer from mental health disorders worldwide. Almost 7 million suffer from anxiety and depression in Bangladesh. There are several factors that can cause stress among youths, both academic and non-academic, ranging from socioeconomic, environmental, cultural and psychological attributes. However, these are not widely researched in Bangladesh. This study identified the factors that affect the mental health of students due to examinations in Bangladesh, particularly the socio-demographic, lifestyle and psychological factors. An online cross-sectional survey was conducted on May 2020 with a sample size of 210 tertiary level students in Dhaka. A modified DASS-21 was used to measure stress, anxiety and depression scores related to examination. Binary logistic model showed that those who lived with family, spent time with parents, had regular sufficient (self-assessed) sleeps and consumed balanced (self-assessed) diets had significantly lower stress, anxiety, and depression. Balanced lifestyle with greater social bonding might help to better equip youths to reduce stress, anxiety, and depression during examination, which could be an avenue for future intervention studies.
1. Introduction
One in four people suffer from mental or neurological disorders worldwide (World Health Organisation, 2001), including 264 million who suffer from depression (World Health Organization, 2020a). A person with depression often functions poorly at work, school or in family environment, which, at its worst, can lead to suicide. Due to depression, suicide is the second leading cause of death for 15–29 year-olds (World Health Organization, 2020a). The global prevalence of moderate to extreme levels of depression is 60.8%, anxiety 73%, and stress 62.4% (Bayram and Bilgel, 2008, Beiter et al., 2015, Kulsoom and Afsar, 2015). Although not widely discussed, mental health issues are increasingly becoming a threat to low- and middle-income countries such as Bangladesh.
Almost 7 million people in Bangladesh experience depressive and anxiety disorders respectively (World Health Organization, 2020b). An estimate of 10,167 committed suicide in 2012, and suicide attempts were considered by 4% of boys and 6% of girls by youths aged 13–17 years (World Health Organization, 2020b). In Bangladesh, the levels of depression, anxiety, and stress has been reported to be as high as 54.3%, 64.8%, and 59.0%, respectively (Hossain et al., 2014, Alim et al., 2017, Saeed et al., 2018, Mamun and Griffiths, 2019, Mamun et al., 2019).
There are myriads of factors that can cause stress among students, both academic and non-academic, ranging from socioeconomic, environmental, cultural to psychological attributes (Brand and Schoonheim-Klein, 2009). Stress levels vary across students depending on symptoms of anxiety, especially during examination periods. A prevalence rate of 10–35% of university students experience “functionally impairing levels of test anxiety” (Chapell et al., 2005, Neuderth et al., 2009). Students with test anxiety are more likely to delay and drop-out in university, which could lead to suicidal behaviors and high economic costs (Schaefer et al. 2007). It can be bidirectional as majority of students with stress display poor self-confidence and often poor academic performance (Sohail, 2013, Baste and Gadkari, 2014).
Several contributing factors of stress, anxiety, and depression among students were identified in literature including sex, strained relationships, family and peer pressure, high parental expectation, lack of financial support and hardships, sleep deprivation, future worries, loneliness, longer screen time, toxic psychological environment, academic pressure, workload, size of the academic curriculum, and heavy test schedules (Brenneisen Mayer et al., 2016, Abdel Wahed and Hassan, 2017, Saeed et al., 2018, Silva and Figueiredo-Braga, 2018, ul Haq et al., 2018, Mamun and Griffiths, 2019). Some of the major academic stressors for students include examinations, time demands, competition and class environment while the most common personal stressors have been intimate relationships, finance and parental conflicts (Murphy and Archer, 1996).
The stress of examinations and mental health of students are correlated. According to Bayram and Bilgel (2008), exam stress and anxiety has negative impacts on students’ academic achievement, physical health & development and standard of life. Causes of exam anxiety can be associated with social stigma, where students from a rural background could feel incompetent compared to those who grew up in the metropolitan, coupled with the fear of not having competitive skills in English, the general medium for higher education in Bangladesh, can demotivate them prior to and during exams which could lead to anxiety, stress, and frustration.
Higher education in recent times involves considerable financial burden (Callender & Kemp, 2000). Richardson et al.’s (2017) cross-sectional survey indicate that financial difficulties often lead to mental disorders such as depression for students. Richardson et al.’s (2017) cross-sectional survey indicate that financial difficulties make students particularly vulnerable to depression. Of all the adverse experiences assessed, financial hardship was the only one to show an independent relationship with depression when pre-entry anxiety and depression were controlled which indicates that the direction of causality is more likely to be from financial problems to depression than vice versa (Andrews and Wilding, 2004). Moreover, excessive parental control is assumed to inhibit the development of children's autonomy, which leads to perceptions of the environment as ”uncontrollable and a limited sense of personal competence or mastery” (Chorpita et al., 1996, Hudson and Rapee, 2001, Dadds, 2002, Barlow, 2004, Chorpita et al., 2016). In turn, these factors are postulated to contribute to the triggering anxiety in children.
There is a knowledge gap concerning mental health problems in Bangladesh. In 2019, four suicides and one suicide rescued among students attracted media and public attention nationwide, which suggested a need to examine the existing mental health issues among students in Bangladesh (Shamsuddin et al., 2013, Arafat and Al Mamun, 2019). To contribute to that gap, the present study investigated the prevalence of depression, anxiety, and stress among Bangladeshi students and their associated risk factors with respect to socio-demographics and lifestyle measures.
The objective of the study was to identify factors that affect the mental health of students due to examinations, particularly the socio-demographic and psychological factors using a survey conducted in Dhaka, Bangladesh in 2020.
2. Theoretical framework
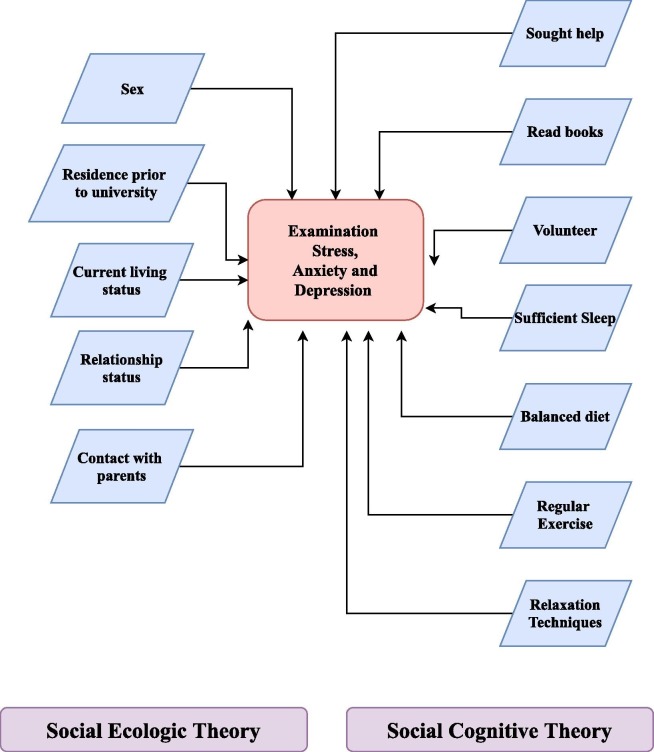
There are several theories that discuss risk factors associated with individual mental health. These include the social ecologic theory, the social cognitive theory, as well as the social stress model, among others (van Praag et al., 2009, Yen et al., 2009). The present study was framed by the social ecologic theory and the social cognitive theory.
The social ecologic theory suggests that individual and environment factors are interrelated and that good health can be achieved with behavioral, economic, and social factors promoting it (Krieger, 1994, Cohen et al., 2000). Thus, the social ecologic theory suggested that a person living in a neighborhood with low socioeconomic status (SES) and low social support is expected to have worse health outcomes than someone from a better environment. The theory posits that environmental factors, socio-demographic factors in the current study context, influence the mental health of students. The most common socio-demographic factors discussed in the literature are the student’s age, sex, place of residence, education, parents’ education, family income, personal income, relationship status, frequency of contact with family and extra-curricular activities.
Social cognitive theory links these socio-demographic factors with the thought processes of students that contribute to their emotional, behavioral and psychological development such as seeking help, reading books, engaging in volunteering activities, getting sufficient sleep, maintaining a balanced diet, getting regular exercise and practicing relaxation techniques (Fig. 1 ). The theory also suggests that good health is linked to individuals having beliefs that they can achieve healthy outcomes, having goals to achieve these outcomes as well as having expectations of these outcomes. (Bandura, 2004, Fisher et al., 2004).
Fig. 1.
Theoretical hypothesis for the study based on social ecologic and social cognitive theories.
3. Materials and methods
3.1. Data overview
An online survey was conducted among undergraduate and postgraduate students from tertiary institutions of Dhaka, Bangladesh. Due to the COVID-19 pandemic in Bangladesh, the authors had to settle for online option and could only collect quantitative data. A total of 210 youths aged between 17 and 25 years participated in the survey using google online survey platform after receiving ethical clearance from University of Dhaka, Bangladesh. The data was collected during May 2020.
4. Variables
The survey questionnaire included sociodemographic information as well as DASS 21 Scale which measured examination stress, anxiety and depression, and possible coping mechanisms. Demographic information included sex, residence before joining university, current living status, relationship status, and contact with parents. The Depression, Anxiety and Stress Scale − 21 Items (DASS-21) is a set of scales designed to measure the psychological states of depression, anxiety and stress. There are 7 items in each of the three DASS-21 scales, divided into subscales with similar content. The depression scale assesses dysphoria, hopelessness, devaluation of life, self-deprecation, lack of interest/involvement, anhedonia and inertia (Lovibond and Lovibond, 1995). The anxiety scale assesses autonomic arousal, skeletal muscle effects, situational anxiety, and subjective experience of anxious affect during examination. It examines the difficulty to relax, nervous arousal, and being easily upset/agitated, irritable/over-reactive and impatient (Lovibond and Lovibond, 1995). Scores for the three emotional states of mind are calculated by summing the scores for the relevant items. The stress/anxiety coping mechanism included questions regarding whether the participant ever sought help for depression/anxiety/stress, reading habits, engagement in volunteering activities, whether the participant made any effort to replace negative thoughts with positive ones, and self-assessment on quality of sleep and eating habits.
4.1. Statistical analysis
Bivariate distribution of the relevant variables across DASS stress, DASS anxiety and DASS depression were quantified. The primary associations were evaluated using t-tests or analysis of variance (ANOVA). To assess the relationships between the DASS scores and socio-demographic variables, linear regression model was fitted. These models included only the variables that were found significant in the primary bivariate associations. P-value < 0.05 was considered as threshold for the level of significance. All statistical analysis was conducted with R (version 3.5.0).
5. Results
The online survey resulted to 210 responses. In the sample 169 were studying in undergraduate degrees, 40 in master’s degrees and one in high school and aged between 17 and 25 years.
The validity of the three DASS scores were assessed using Cronbach's alpha. The alpha values for stress, anxiety and depression were 0.84 (95% CI: 0.81 ~ 0.84), 0.80 (95% CI: 0.76 ~ 0.84) and 0.88 (95% CI: 0.85 ~ 0.90) respectively. These show that the scores were reliable.
5.1. Bivariate association
In the bivariate association, variables such as current living status, contact with parents, sufficient sleep and balanced diet were significantly associated with DASS scores during examination periods (Table 1 ). Most of the participants (N = 145) lived with family but higher scores of stress (21.01), anxiety (17.87) and depression (18.27) were observed for those who lived without family compared to those who lived with family. Similarly, most of the participants (N = 164) had daily contact with family but higher scores of stress (25.63), anxiety (19.09) and depression (24) were observed for those who contacted their family 1–2 times a month compared to those who contacted daily and 1–2 times a week. Moreover, the result suggests that higher scores of stress (21.58), anxiety (17.58) and depression (20.65) was prevalent in those who did not have sufficient sleep compared to the highest number of participants who had sufficient sleep (N = 91). Lastly, participants who did not have a regular and healthy food habit had the highest scores of stress (19.90), anxiety (17.69) and depression (18.05) during examination compared to those who had regular and balanced diet (Table 1). The four significant variables – current living status, contact with family, sufficient sleep and balanced diet were fitted to linear regression model.
Table 1.
Distribution of stress, anxiety and depression across all variables.
| Variable | Category | Sample size (N) | DASS Stress | DASS Anxiety | DASS Depression | |||
|---|---|---|---|---|---|---|---|---|
| Mean (SD) | P-value | Mean (SD) | P-value | Mean (SD) | P-value | |||
| Sex | Male | 86 | 17.28 (8.54) | 0.167 | 14.44 (8.46) | 0.178 | 15.48 (9.63) | 0.576 |
| Female | 124 | 19.03 (9.63) | 16.08 (8.89) | 16.27 (10.49) | ||||
| Residence before joining university | Urban | 167 | 17.67 (9.02) | 0.060 | 15 (8.82) | 0.176 | 15.56 (10.12) | 0.285 |
| Rural | 43 | 20.79 (9.65) | 16.97 (8.31) | 17.44 (10.16) | ||||
| Current living status | Live with family | 145 | 17.10 (9.05) | 0.004 | 14.30 (8.55) | 0.007 | 14.91 (9.91) | 0.029 |
| Live without family | 65 | 21.01 (9.06) | 17.87 (8.70) | 18.27 (10.3) | ||||
| Relationship status | Single | 154 | 18.49 (8.85) | 0.618 | 15.48 (8.65) | 0.335 | 16.15 (10.19) | 0.692 |
| Married | 3 | 13.33 (10.06) | 8 (8.71) | 11.33 (11.01) | ||||
| In a relationship | 53 | 18.07 (10.25) | 15.62 (8.96) | 15.62 (10.03) | ||||
| Contact with parents | Daily | 164 | 17.52 (9.05) | 0.011 | 15.24 (8.66) | 0.356 | 15.13 (9.65) | 0.013 |
| 1/2 times a week | 35 | 19.71 (9.43) | 15.02 (8.98) | 17.25 (11.27) | ||||
| 1/2 times a month | 11 | 25.63 (7.68) | 19.09 (8.96) | 24 (10.39) | ||||
| Sought help | Yes | 93 | 18.45 (9.61) | 0.849 | 16.27 (9.39) | 0.207 | 15.48 (10.14) | 0.552 |
| No | 117 | 18.21 (8.92) | 14.71 (8.15) | 16.32 (10.15) | ||||
| Read books | Yes | 146 | 18.05 (9.19) | 0.541 | 14.94 (8.65) | 0.252 | 15.47 (10.16) | 0.307 |
| No | 64 | 18.90 (9.30) | 16.46 (8.89) | 17.03 (10.06) | ||||
| Volunteering | Yes | 74 | 16.94 (8.62) | 0.103 | 14.43 (8.11) | 0.219 | 14.81 (9.56) | 0.218 |
| No | 136 | 19.05 (9.47) | 15.94 (9.04) | 16.57 (10.41) | ||||
| Positive thoughts | Yes | 137 | 18.40 (8.92) | 0.844 | 15.51 (8.38) | 0.812 | 15.21 (9.77) | 0.159 |
| No | 73 | 18.13 (9.47) | 15.20 (9.42) | 17.34 (10.70) | ||||
| Sufficient Sleep | Yes | 91 | 15.53 (8.40) | <0.001 | 13.56 (8.12) | 0.021 | 12.74 (8.60) | <0.001 |
| Sometimes | 76 | 19.78 (9.46) | 16.39 (8.50) | 17.13 (10.43) | ||||
| No | 43 | 21.58 (8.93) | 17.58 (9.76) | 20.65 (10.51) | ||||
| Balanced diet | Yes | 105 | 16.72 (8.86) | 0.012 | 13.12 (7.73) | <0.001 | 13.84 (9.29) | 0.002 |
| No | 105 | 19.90 (9.32) | 17.69 (9.11) | 18.05 (10.54) | ||||
| Regular Exercise | Yes | 40 | 17.50 (9.25) | 0.539 | 14.35 (8.11) | 0.371 | 13.45 (8.80) | 0.058 |
| No | 170 | 18.50 (9.22) | 15.65 (8.88) | 16.54 (10.35) | ||||
| Relaxation Techniques | Yes | 162 | 18.37 (9.40) | 0.866 | 15.22 (8.53) | 0.592 | 15.37 (10.13) | 0.126 |
| No | 48 | 18.12 (8.63) | 16.04 (9.44) | 17.91 (9.97) | ||||
5.2. Linear regression model
The linear regression models observed a significant association of contact with parents with stress and depression (Table 2 ). Those who kept contact with parents only once or twice a month were more likely to have higher examination stress and depression respectively compared to those who contacted daily with their parents. Similarly, sleeping pattern was significantly (P < 0.05) associated with stress and depression during examinations. Those who had sufficient sleep were less likely to have higher stress or depression compared to those who self-reported of insufficient sleep. Only diet was associated with anxiety (Table 2). Those who had balanced diet were likely to have lower anxiety during examination period compared to those with unbalanced diet. Also, anxiety was marginally associated (P < 0.058) with living status, that is those living without family were more likely to experience anxiety than those living with it. For all the linear regression model, generalized variance-inflation factors (GVIF) were computed and all scores were under 2, which means there were no multicollinearity in the models (Fox and Monette, 1992)
Table 2.
Linear regression model fitted to the DASS scores with demographic information.
| DASS Stress | DASS Anxiety | DASS Depression | ||||
|---|---|---|---|---|---|---|
| Variable | b (95% CI) | P-value | b (95% CI) | P-value | b (95% CI) | P-value |
| Current living status (ref: Live with family) | ||||||
| Live without family | 2.01 (-0.75, 4.77) | 0.152 | 12.85 (0.917, 179.95) | 0.058 | 0.92 (-2.09, 3.92) | 0.548 |
| Contact with parents (ref: Daily) | ||||||
| 1/2 times a week | 1.24 (-2.13, 4.61) | 0.468 | −1.00 (-4.23, 2.22) | 0.540 | 1.65 (-2.03, 5.33) | 0.377 |
| 1/2 times a month | 5.77 (0.20, 11.34) | 0.042 | 1.32 (-4.02, 6.65) | 0.627 | 6.39 (0.31, 12.46) | 0.039 |
| Sufficient Sleep (ref: No) | ||||||
| Sometimes | −1.23 (-4.62, 2.16) | 0.474 | −0.37 (-3.62, 2.87) | 0.820 | −3.07 (-6.76, 0.63) | 0.104 |
| Yes | −4.58 (-7.92, −1.23) | 0.008 | −2.16 (-5.36, 1.05) | 0.186 | −6.39 (-10.04, −2.74) | 0.001 |
| Balanced diet (ref: No) | ||||||
| Yes | −1.64 (-4.14, 0.86) | 0.197 | −3.61 (-6.00, −1.22) | 0.003 | −2.59 (-5.31, 0.14) | 0.063 |
6. Discussion
The results showed that living with family, time spent with parents, sleeping patterns and diets were significantly associated with mental health factors. Given the current study evaluated students who only had mild or moderate stress, anxiety or depression, it could be argued that a balanced lifestyle with sound social communication would help students deal with stress, anxiety and depression related to examination.
Talking with parents daily seemed to be a stress relieving mechanism among youths, as results indicate. Students who talked to their parents daily over phone had the lower stress and depression scores resulting from examinations compared to those who talked 1–2 times a month. A pilot study of children with separation anxiety disorder (Choate et al., 2005) found that a parent–child intervention designed to improve the attachment bond resulted in children no longer fitting criteria for separation anxiety disorder in most cases. That would work for examination stress as well, given, a student who shares the concerns are more likely to receive support and encouraging behaviors from their parents. Social bonding has proved to be a good depression coping mechanism (Karriker-Jaffe, Foshee and Ennett, 2011). Thus, improving the parent–youth attachment, particularly for academic examination related mental health issues, could be an avenue to alleviate excess anxiety and depression.
Students who generally had sufficient sleep regularly had lower examination related stress and depression compared to those who never had sufficient sleep. Recent epidemiological studies suggest that insomnia is not just a typical symptom of depression, rather it could be an independent risk factor for depression in the long run (Hohagen et al., 1993). Although this study did not evaluate a bi-directional relationship, depression is considered to be one of the most frequent and prominent causes of insomnia (Hohagen et al., 1993). However, academic performance might not necessarily be hindered due to insomnia (Taylor, Bramoweth, Grieser, Tatum, and Roane, 2013) but lack of adequate sleep was found to be associated with a range of impairments in terms of academic functioning (Hysing, Pallesen, Stormark, Lundervold, and Sivertsen, 2013). A disruptive sleeping pattern or lack of it during examination period would suggest higher likelihood of stress, which would result in a deterioration in academic performance.
Many young adults face traumatic experiences and mental illnesses during university period. Higher consumption of food due to anxiety is common. More often, anxiety leads to unbalanced diet and overconsumption of processed food, which hampers the bodily functions (Kemp et al., 2013, Weng et al., 2012). In one study, M. Hossain, Naher, and Shahabuddin 2005, found that participants who had healthy food habit had the lowest scores of anxiety, stress and depression respectively whereas students who did not have healthy food habit had the highest scores. Food habit is also affiliated with students who live without family, more often they rely on campus canteens or substandard dormitory cafes. This could lead to less than adequate nutrient intake, particularly when studies have repeatedly questioned nutrition in food sources in Bangladesh (Hossain et al., 2005, Khan et al., 2019). All these are compounded by factors such as financial condition, sufficient resources and facilities which play a major role here.
Higher levels of examination anxiety were observed for students who lived without their family compared to those who lived with their family. Results indicated that youths with higher anxiety level perceived their mothers and fathers as being more socially isolating, more concerned about others’ opinions, more ashamed of the students’ shyness and poor performance, and less socially active than youths with low anxiety level (Caster et al., 1999). Staying with family reduces their stress, anxiety and depression, particularly during examination, as they could share some responsibilities with their families and focus more on academic workload. This, in turn, relieves some anxiety and improves their mental health.
There were a few limitations to this study. First, there was no active identification of severely stressed individuals to be included in the survey, which might have observed stronger effect sizes in the models. Second, this study was limited to only quantitative data, which means future studies could consider in-depth interviews to explore more focused examination related stress factors. Also, as the sample size was small, the beta scores in the regression model might not be adjusted to reflect population estimates. Thirdly, as the data was cross-sectional, there is hardly a scope to assess a causal link. Based on the study findings, some intervention studies can explore the causal link between healthy lifestyle and mental health related factors during examination in Bangladesh. Moreover, future studies can consider calculating Quality-Adjusted Life Year (QALY) & Disability-Adjusted Life Year (DALY) and assess their impacts. Fourthly, the financial barrier between public universities and private institutions in Bangladesh could act as a stressor, which was not collected in the current survey. Finally, the sample was limited to only youths pursuing higher education in Dhaka, Bangladesh. For more generalized conclusion, wide scale surveys with funding would be necessary.
7. Conclusion
Examinations have a negative effect on the mental health of students in terms of stress, anxiety, and depression. This study explored some demographic factors associated with mental health for Bangladeshi tertiary level students. Balanced lifestyle with greater social bonding might help better equip fighting stress, anxiety, and depression during examination. Future research could examine the relationship between academic results and its association with stresses and psychological disorders. Amidst the high density of infections and non-communicable diseases, mental health is still not highly reorganized in Bangladesh. Implementation of stress management workshops, improvisation of academic environment, use of problem-focused and emotion focused strategies at the policy level should be targeted. Moreover, students need assistance and co-curricular programming to help them develop “stress-related coping strategies” attuned to performance and the outcomes borne regarding the effects of stress, in particular regarding eustress, where a positive impact has been cited with respect to the effects of stress on financial aid, institutional commitment, academic performance, and intent to persist.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethical clearance
Ethical permission was taken from the Department of English, University of Dhaka, Bangladesh. The responses from the participants were voluntary and consent from them was taken.
Contributor statement
AR Arusha conceptualized the study, conducted online survey, coded the data, framed the manuscript, drafted the manuscript, and conducted the literature review. RK Biswas performed the statistical analysis, drafted the theoretical framework, and critically reviewed the manuscript. The final manuscript was read and approved by all the authors.
Declaration of Competing Interest
The authors declared that there is no conflict of interest.
Acknowledgements
The authors would like to acknowledge the Department of English, University of Dhaka, Bangladesh for their support. We also convey our gratitude to the participants who took time to fill up the online survey during COVID-19 pandemic.
References
- Abdel Wahed W.Y., Hassan S.K. Prevalence and associated factors of stress, anxiety and depression among medical Fayoum University students. Alexandria Journal of Medicine. 2017;53(1):77–84. doi: 10.1016/j.ajme.2016.01.005. [DOI] [Google Scholar]
- Alim S.A.H.M. Translation of DASS 21 into Bangla and validation among medical students. Bangladesh Journal of Psychiatry. 2017 doi: 10.3329/bjpsy.v28i2.32740. [DOI] [Google Scholar]
- Andrews B., Wilding J.M. The relation of depression and anxiety to life-stress and achievement in students. British Journal of Psychology. 2004:509–521. doi: 10.1348/0007126042369802. [DOI] [PubMed] [Google Scholar]
- Arafat S.M.Y., Al Mamun M.A. Repeated suicides in the University of Dhaka (November 2018): Strategies to identify risky individuals. Asian Journal of Psychiatry. Elsevier. 2019;B.V:84–85. doi: 10.1016/j.ajp.2018.12.014. [DOI] [PubMed] [Google Scholar]
- Bandura, A. (2004) ‘31; 143 Health Educ Behav at UNIV OF ROCHESTER LIBRARY on’, journals.sagepub.com, 31(2), pp. 143–164. doi: 10.1177/1090198104263660.
- D. Barlow Anxiety and its disorders: The nature and treatment of anxiety and panic Available at: Https://books.google.com/books?hl=en&lr=&id=Lx9hf-3ZJCQC&oi=fnd&pg=PA1&dq=Barlow,+D.+H.+(2002).+Anxiety+and+its+disorders:+The+nature+and+treatment+of+anxiety+and+panic.+(2nd+ed.).+New+York:+Guilford+Press.&ots=WhBkFubR9m&sig=HxiHmQYX6wnvzaxLgFiy07lX32w 2004 Accessed: 26 May 2020.
- Baste, V. S. and Gadkari, J. V (2014) Source: PubMed 298 Baste and Gadkari Indian, Indian J Physiol Pharmacol. Available at: https://www.researchgate.net/publication/275357730 (Accessed: 7 May 2020).
- Bayram N., Bilgel N. The prevalence and socio-demographic correlations of depression, anxiety and stress among a group of university students. Social Psychiatry and Psychiatric Epidemiology. 2008;43(8):667–672. doi: 10.1007/s00127-008-0345-x. [DOI] [PubMed] [Google Scholar]
- Beiter R. The prevalence and correlates of depression, anxiety, and stress in a sample of college students. Journal of Affective Disorders. 2015;173:90–96. doi: 10.1016/j.jad.2014.10.054. [DOI] [PubMed] [Google Scholar]
- Brand H.S., Schoonheim-Klein M. Is the OSCE more stressful? Examination anxiety and its consequences in different assessment methods in dental education. European Journal of Dental Education. 2009;13(3):147–153. doi: 10.1111/j.1600-0579.2008.00554.x. [DOI] [PubMed] [Google Scholar]
- Brenneisen Mayer F. Factors associated to depression and anxiety in medical students: A multicenter study. BMC Medical Education. BioMed Central Ltd. 2016;16(1):1–9. doi: 10.1186/s12909-016-0791-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callender, C., Kemp, M. (2000) Changing Student Finances: Income, Expenditure and the Take-up of Student Loans Among Full- and Part-time Higher Education Students in 1998/9, Department for Education and Employment. Available at: https://core.ac.uk/download/pdf/4154527.pdf (Accessed: 18 July 2020).
- Caster J.B. Relationship between Youth and Parent Perceptions of Family Environment and Social Anxiety. Elsevier. 1999 doi: 10.1016/S0887-6185(99)00002-X. [DOI] [PubMed] [Google Scholar]
- Chapell M.S. Test anxiety and academic performance in undergraduate and graduate students. Journal of Educational Psychology. 2005;97(2):268–274. doi: 10.1037/0022-0663.97.2.268. [DOI] [Google Scholar]
- Choate M.L. Parent-Child Interaction therapy for treatment of separation anxiety disorder in young children: A pilot study. Cognitive and Behavioral Practice. 2005;12(1):126–135. doi: 10.1016/S1077-7229(05)80047-1. [DOI] [Google Scholar]
- Chorpita B.F., Albano A.M., Barlow D.H. ‘Cognitive processing in children: Relation to anxiety and family influences’, Journal of Clinical Child Psychology. Informa UK Limited. 1996;25(2):170–176. doi: 10.1207/s15374424jccp2502_5. [DOI] [Google Scholar]
- Chorpita B.F., Brown T.A., Barlow D.H. Perceived Control as a Mediator of Family Environment in Etiological Models of Childhood Anxiety – Republished Article. Behavior Therapy. 2016;47(5):622–632. doi: 10.1016/j.beth.2016.08.008. [DOI] [PubMed] [Google Scholar]
- Cohen D.A., Scribner R.A., Farley T.A. A structural model of health behavior: A pragmatic approach to explain and influence health behaviors at the population level. Preventive Medicine. 2000;30(2):146–154. doi: 10.1006/pmed.1999.0609. [DOI] [PubMed] [Google Scholar]
- M.R. Dadds 2002 87 104 10.1007/978-1-4615-1739-9_5.
- Fisher K.J. Neighborhood-Level Influences on Physical Activity among Older Adults: A Multilevel Analysis. Journal of Aging and Physical Activity. 2004;12(1):45–63. doi: 10.1123/japa.12.1.45. [DOI] [PubMed] [Google Scholar]
- Fox J., Monette G. Generalized collinearity diagnostics. Journal of the American Statistical Association. 1992;87(417):178–183. doi: 10.1080/01621459.1992.10475190. [DOI] [PubMed] [Google Scholar]
- Hohagen F. ‘Prevalence and treatment of insomnia in general practice - A longitudinal study’, European Archives of Psychiatry and Clinical Neuroscience. Springer-Verlag. 1993;242(6):329–336. doi: 10.1007/BF02190245. [DOI] [PubMed] [Google Scholar]
- Hossain M.D. Mental disorders in Bangladesh: A systematic review. BMC Psychiatry. BioMed Central Ltd. 2014;14(1) doi: 10.1186/s12888-014-0216-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hossain, M., Naher, F. and Shahabuddin, Q. (2005) Food Security and Nutrition in Bangladesh: Progress and Determinants, ageconsearch.umn.edu. Available at: www.fao.org/es/esa/ (Accessed: 26 May 2020).
- Hudson J.L., Rapee R.M. Parent-child interactions and anxiety disorders: An observational study. Behaviour Research and Therapy. 2001;39(12):1411–1427. doi: 10.1016/S0005-7967(00)00107-8. [DOI] [PubMed] [Google Scholar]
- Hysing M., Pallesen S., Stormark K.M., Lundervold A.J., Sivertsen B. Sleep patterns and insomnia among adolescents: A population-based study. Journal of sleep research. 2013;22(5):549–556. doi: 10.1111/jsr.12055. [DOI] [PubMed] [Google Scholar]
- Karriker-Jaffe K.J., Foshee V.A., Ennett S.T. Examining How Neighborhood Disadvantage Influences Trajectories of Adolescent Violence: A Look at Social Bonding and Psychological Distress. Journal of School Health. 2011;81(12):764–773. doi: 10.1111/j.1746-1561.2011.00656.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kemp E., Bui M.Y., Grier S. When food is more than nutrition: Understanding emotional eating and overconsumption. Wiley Online Library. 2013;12(3):204–213. doi: 10.1002/cb.1413. [DOI] [Google Scholar]
- Khan J.R. Factors associated with the availability of iodized salt at household level: A case study in Bangladesh. Public Health Nutrition. 2019;22(10):1815–1823. doi: 10.1017/S1368980018003907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N. Epidemiology and the web of causation: Has anyone seen the spider? Social Science and Medicine. 1994 doi: 10.1016/0277-9536(94)90202-X. [DOI] [PubMed] [Google Scholar]
- Kulsoom B., Afsar N.A. Stress, anxiety, and depression among medical students in a multiethnic setting. Neuropsychiatric Disease and Treatment. 2015;11:1713–1722. doi: 10.2147/NDT.S83577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovibond P.F., Lovibond S.H. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy. 1995;33(3):335–343. doi: 10.1016/0005-7967(94)00075-U. [DOI] [PubMed] [Google Scholar]
- M.A.A. Mamun M.D. Griffiths The association between Facebook addiction and depression: A pilot survey study among Bangladeshi students Psychiatry Research 2019 10.1016/j.psychres.2018.12.039. [DOI] [PubMed]
- M.A. Mamun M.A. Rafi A.H.M.S. Al Mamun M.Z. Hasan K. Akter K. Hsan M.D. Griffiths Prevalence and Psychiatric Risk Factors of Excessive Internet Use among Northern Bangladeshi Job-Seeking Graduate Students: A Pilot Study 10.1007/s11469-019-00066-5 http://link.springer.com/10.1007/s11469-019-00066-5.
- Murphy, M. C. and Archer, J. (1996) ‘Stressors on the College Campus: A Comparison of 1985 and 1993’, Journal of College Student Development, 37(1), pp. 20–28. Available at: https://psycnet.apa.org/record/1996-94176-002 (Accessed: 7 May 2020).
- Neuderth S., Jabs B., Schmidtke A. Strategies for reducing test anxiety and optimizing exam preparation in German university students: A prevention-oriented pilot project of the University of Würzburg. Journal of Neural Transmission. 2009;116(6):785–790. doi: 10.1007/s00702-008-0123-7. [DOI] [PubMed] [Google Scholar]
- Richardson T. A longitudinal study of financial difficulties and mental health in a national sample of British undergraduate students. Community Mental Health Journal. 2017;53(3):344–352. doi: 10.1007/s10597-016-0052-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saeed H. ‘Determinants of Anxiety and Depression Among University Students of Lahore’, International Journal of Mental Health and Addiction. Springer, New York LLC. 2018;16(5):1283–1298. doi: 10.1007/s11469-017-9859-3. [DOI] [Google Scholar]
- Schaefer A. Mental health and performance of medical students with high and low test anxiety. PPmP Psychotherapie Psychosomatik Medizinische Psychologie. 2007;57(7):289–297. doi: 10.1055/s-2006-951974. [DOI] [PubMed] [Google Scholar]
- Shamsuddin K. Correlates of depression, anxiety and stress among Malaysian university students. Asian Journal of Psychiatry. 2013;6(4):318–323. doi: 10.1016/j.ajp.2013.01.014. [DOI] [PubMed] [Google Scholar]
- Silva R.G., Figueiredo-Braga M. Evaluation of the relationships among happiness, stress, anxiety, and depression in pharmacy students. Currents in Pharmacy Teaching and Learning. 2018;10(7):903–910. doi: 10.1016/j.cptl.2018.04.002. [DOI] [PubMed] [Google Scholar]
- N. Sohail Stress and academic performance among medical students Journal of the College of Physicians and Surgeons Pakistan 2013 01.2013/JCPSP.6771. [PubMed]
- Taylor D.J., Bramoweth A.D., Grieser E.A., Tatum J.I., Roane B.M. Epidemiology of insomnia in college students: Relationship with mental health, quality of life, and substance use difficulties. Behavior Therapy. 2013;44(3):339–348. doi: 10.1016/j.beth.2012.12.001. [DOI] [PubMed] [Google Scholar]
- ul Haq, M. A. et al. ‘Psychometric study of depression, anxiety and stress among university students’, Journal of Public Health (Germany) Springer Verlag 26 2 2018 211 217 10.1007/s10389-017-0856-6.
- van Praag L. Mental health in a gendered context: Gendered community effect on depression and problem drinking. Health and Place. 2009;15(4):990–998. doi: 10.1016/j.healthplace.2009.04.003. [DOI] [PubMed] [Google Scholar]
- Weng T.T. Is there any relationship between dietary patterns and depression and anxiety in Chinese adolescents? Public Health Nutrition. 2012;15(4):673–682. doi: 10.1017/S1368980011003077. [DOI] [PubMed] [Google Scholar]
- World Health Organisation Mental disorders affect one in four people. World Health Organization. 2001 doi: 10.1192/bjp.180.1.29. [DOI] [Google Scholar]
- World Health Organization (2020a) Depression, World Health Organization. Available at: https://www.who.int/news-room/fact-sheets/detail/depression.
- World Health Organization (2020b) Mental Health: Current mental health situation in Bangladesh. Available at: http://www.searo.who.int/bangladesh/mental-health/en/.
- Yen I.H., Michael Y.L., Perdue L. Neighborhood Environment in Studies of Health of Older Adults. A Systematic Review. American Journal of Preventive Medicine. 2009;37(5):455–463. doi: 10.1016/j.amepre.2009.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]