Abstract
Purpose
Our purpose was to evaluate the implementation of a postoperative hand and upper extremity telemedicine program. We aimed to compare travel burden, visit time, and patient satisfaction between an initial postoperative telemedicine visit and a second conventional in-clinic visit.
Methods
Telemedicine guidelines established by our hospital system were used as inclusion criteria for this prospective study, which included patients indicated for surgery in the outpatient clinic during a 3-month period. Patients were excluded if they had wounds closed with nonabsorbable suture, remained admitted to the hospital, or required a custom orthosis at their first postoperative visit. Baseline demographics and patient-reported outcome measures were collected prior to surgery. Information pertaining to technology usage was collected for the telemedicine visit and travel information was obtained for the in-clinic visit. Patient satisfaction was recorded for both visits.
Results
Fifty-seven of 87 patients (66%) who met the inclusion criteria elected to participate in the study. A cell phone was utilized by 89% of patients and 88% of visits were performed from the patient’s home. There were 4 technological complications during the study period (7%). Mean round-trip travel distance for the in-clinic visit was 60 miles with an average drive time of 85 minutes. Visit times were significantly shorter with telemedicine (7 minutes vs 38 minutes). Telemedicine was preferred by 90% of patients for subsequent encounters. All 4 clinical complications were recognized during the telemedicine visit.
Conclusions
A telemedicine program for postoperative care after hand and upper extremity surgery decreases travel burdens associated with conventional in-clinic appointments. Telemedicine significantly decreases visit times without decreasing patient satisfaction for patients who elect to participate in remote video visits. The ability to recognize early postsurgical complications was not compromised by utilizing this technology, even during our early experience.
Clinical relevance
Telemedicine after hand and upper extremity surgery results in high levels of patient satisfaction and decreases visit times and the travel burdens associated with conventional in-clinic appointments.
Key words: Hand surgery, technology, telehealth, telemedicine, virtual visits
As mobile video-conferencing technologies have evolved, so have telemedicine programs. Purported benefits of telemedicine include cost-savings, decreased travel burden, and patient convenience.1, 2, 3 As with any new technology, there are concerns regarding the safety and efficacy of telemedicine visits compared with conventional, in-clinic encounters. Specific to hand and upper extremity surgery, recent investigations have focused on the utilization of this technology for the evaluation of emergent conditions in the emergency department setting.2 There is a relative paucity of literature investigating the use of telemedicine after upper extremity surgery.
The purpose of this investigation was to evaluate the implementation of a postoperative hand and upper extremity telemedicine program. We aimed to compare travel burden, visit time, patient satisfaction, and ease of use between an initial postoperative telemedicine visit and the second conventional in-clinic visit. In addition, we aimed to evaluate our early experience while implementing a new postoperative telemedicine program. We hypothesized that patients participating in telemedicine would have decreased visit times and demonstrate high levels of satisfaction.
Materials and Methods
Institutional review board approval was obtained for this prospective study. Our outpatient clinic is part of a rural, academic, level-I trauma center with a catchment area of approximately 25,000 square miles. The study period was prior to the COVID-19 pandemic, and during that time, outpatient telemedicine visits were only approved within our division for postoperative care within the 90-day global billing period after surgery. During this 90-day period, normal postoperative care is bundled into the global surgery fee.
We utilized the telemedicine guidelines established by our hospital system as inclusion criteria for this study. Patients younger than 18 years were included with parental consent. Parents were required to initiate the telemedicine call for pediatric patients. In order to be eligible for telemedicine visits, patients must meet all of the following criteria:
-
1.
Patient must own a smartphone, personal computer, tablet, or laptop with video-calling capability.
-
2.
Patient must have access to reliable Wi-Fi internet.
-
3.
Patient must be in-state during the telemedicine visit.
-
4.
Patient must have an e-mail address.
In addition to exclusion for technological criteria, we also established clinical exclusion criteria. Patients were excluded if they had wounds that were closed with nonabsorbable suture, remained admitted to the hospital or nursing facility during the time of the postoperative visit, or required casting/custom orthosis at their first postoperative visit. Although we did not establish specific exclusion criteria based on case complexity, the previously discussed clinical exclusion criteria resulted in the inclusion of mostly lower-complexity cases. For example, cases involving limb salvage or tendon reconstruction often require the use of a postoperative orthosis fitted by a therapist, and these types of cases were excluded. Patients who required a radiograph at their first postoperative visit were allowed to do so at a location close to home and were not excluded from this study.
Telemedicine screening and scheduling
The study period corresponded with the implementation of a postoperative telemedicine program within the Hand Surgery Division at our institution. All patients from the senior author’s (L.C.G.) outpatient clinic who were indicated for surgery during a 3-month period from February 2019 to April 2019 were screened for eligibility for this investigation. The first patient enrolled in this investigation was the first telemedical visit performed in our division. When a patient was indicated for surgical intervention, technological and clinical inclusion criteria were reviewed, and those patients meeting the criteria were offered the option of scheduling their first postoperative visit (7–14 days after surgery) as a telemedicine visit. The second postoperative visit (4–6 weeks after surgery) was a conventional in-clinic appointment in the outpatient clinic for all patients.
Patients electing for a telemedicine postoperative visit were given a 1-page FAQ (frequently asked questions) and trouble-shooting guide (Appendix A; available on the Journal’s Web site at www.jhandsurg.org). They were then contacted by the scheduling department via e-mail. This e-mail contained a link to the telemedicine video-call application, which utilized a web-browser–based video conferencing feature for Android and Windows users and a downloadable mobile app for iOS (Apple) users. The telemedicine platform utilized was designed by InTouch Health (Santa Barbara, CA), and customized for our institution. Telemedicine visits were conducted during regular clinic hours, during administrative time and between surgical cases. We utilized the same scheduling templates for both telemedicine and in-clinic visits. Patients were sent automated appointment reminders 24 hours prior and 1 hour prior to their appointment. Patients could log into the telemedicine platform prior to the visit in order to familiarize themselves with the software. The type of device utilized by the patient was recorded. The senior author (L.C G.) performed all of the postoperative telemedicine visits on a tablet device.
Telemedicine visit
Both the patient and the surgeon logged into the telemedicine platform at the scheduled visit time. Prior to initiating the visit, the patient signed an electronic informed consent. Information relating to HIPAA (Health Insurance Portability and Accountability Act) compliance and protected health information relative to the software can be found on the InTouch Web site (https://intouchhealth.com/privacy-policy/). To further safeguard protected health information, the patient was informed whether any other people were present in the room, which included medical students, residents, and therapists. All visits were conducted with the office door closed.
For the physical examination, patients were asked to remove their dressing and the wound was inspected. All wounds were closed with absorbable suture. A remote physical examination was then performed on all patients. We asked the patient to perform passive and active range of motion. Sensation was assessed by having the patient compare sensation to light touch on regions of the surgical extremity to the nonsurgical side.
If radiographs were obtained prior to the visit, they were viewed within the electronic medical record system. For patients who lived near a facility within our health system that had the ability to obtain radiographs, these images were immediately available within our Picture Archiving and Communication Systems (PACS). Radiographs obtained at outside facilities were uploaded into LifeImage (Newton, MA) and could be viewed during the encounter. Orders for any medications were placed electronically. Physical and occupational therapy referrals, if indicated, were ordered electronically as well. We utilized our electronic medical record system to document the clinic note, which included documentation stating that this was a telemedicine visit. This was the same process utilized for conventional in-clinic visits.
Data collection
Baseline demographics were recorded for each patient. At the time of the initial consultation prior to surgery, patients were asked to complete a Numeric Pain Rating Scale (NPRS) and Patient-Reported Outcomes Measurement Information System (PROMIS) instruments, which included the PROMIS Self-Efficacy for Managing Symptoms Short-Form 4a, PROMIS Pain Interference Short-Form 4a, and the PROMIS Upper Extremity Short-Form 7a.
Patients completed an NPRS during the first postoperative telemedicine visit. Both the patient and the surgeon were asked to rate the audio and video quality of the call on a 3-point scale with 1 indicating no audio or visual availability, 2 indicating reduced audio or visual feed quality, and 3 indicating a well-functioning, clear audio or visual feed. The length of the telemedicine call was also recorded.
During the second in-clinic postoperative visit, patients were asked to complete an NPRS and the PROMIS Upper Extremity questionnaire. In addition, we recorded visit time, travel time, travel distance, and patient satisfaction information. Mileage and travel times were recorded using Google Maps (Google LLC, Mountain View, CA), utilizing the patient’s home address and the address of our outpatient clinic. Travel times were determined at the time of the clinic visit in order to account for traffic fluctuations. When multiple routes were available, the shortest travel time was recorded. Visit times were recorded using the appointment “check-in” and “check-out” times within our electronic medical records system.
At the conclusion of the in-clinic visit, patients were asked to rate the telemedicine program with respect to ease of use on an 11-point Likert scale, with 0 indicating very difficult and 10 indicating very easy. Patients also completed an 11-point Likert scale to rate their satisfaction with both the telemedicine and the in-clinic postoperative visits, with 0 indicating very unsatisfied and 10 indicating very satisfied. Patients were asked whether they would choose a telemedicine or an in-clinic postoperative visit in the future. Utilizing a similar written questionnaire distributed by Abel et al4 for a telemedicine program, patients were asked to select their reasons for choosing telemedicine. The time required to complete outcome measures and questionnaires was included in the visit times for both the telemedicine and the in-clinic visit.
Statistics
Descriptive statistics were used for baseline demographics. We used Student t testing and chi-square testing to compare the means or proportions between the 2 visits. Differences of P less than .05 were considered statistically significant.
Results
During the 3-month study period, the senior author (L.C.G.) preformed a total of 147 surgical procedures. Twenty-four patients did not meet the inclusion criteria. An additional 36 patients had clinical exclusion criteria and were not eligible to participate. Fifty-seven of the 87 patients who met inclusion criteria, and were eligible for the study, elected to participate (66%). All of the 57 included patients completed both postoperative visits. Baseline demographics for all patients included in this investigation are presented in Table 1 . Demographic information for patients who met inclusion criteria but declined to participate in presented in Table 2 .
Table 1.
Baseline Demographics for All Included Patients
| Variables | All Included Patients |
|---|---|
| Patients, n | 57 |
| Procedures, n | 61 |
| Age, y | |
| Mean (SD) | 51 (13) |
| Range | 16–78 |
| Male, n (%) | 15 (25) |
| Right hand involved, n (%) | 36 (63) |
| Dominant hand involved, n (%) | 37 (65) |
| Patient-Reported Outcome Measures, mean (SD) | |
| NPRS | 4.7 (2) |
| PROMIS Pain Interference | 58.2 (9) |
| PROMIS Self-Efficacy for Managing Symptoms | 44.4 (9) |
| PROMIS Upper Extremity | 33.6 (10) |
| Procedures, n (% of procedures performed) | |
| Carpal tunnel release | 33 (54) |
| Trigger digital release | 6 (10) |
| Mass excision | 4 (7) |
| de Quervain release | 3 (5) |
| Rotator cuff repair | 3 (5) |
| Distal biceps repair | 2 (4) |
| Implant removal | 2 (4) |
| Cubital tunnel release | 1 (2) |
| ORIF distal radius | 1 (2) |
| ORIF clavicle | 1 (2) |
| ORIF humerus | 1 (2) |
| ORIF hand fracture | 1 (2) |
| Medial epicondyle debridement | 1 (2) |
| Shoulder arthroscopy | 1 (2) |
| Reverse total shoulder | 1 (2) |
ORIF, open reduction internal fixation.
Table 2.
Baseline Demographics for Eligible Patients Who Declined Study Participation
| Variables | Patients That Declined Participation |
|---|---|
| Patients who declined study participation, n | 30 |
| Procedures, n | 35 |
| Age, y | |
| Mean (SD) | 49 (13) |
| Range | 22–78 |
| Male, n (%) | 18 (60) |
| Procedures, n (% of procedures performed) | |
| Carpal tunnel release | 15 (43) |
| Shoulder arthroscopy | 4 (11) |
| Trigger digit release | 3 (9) |
| Distal biceps repair | 2 (5.7) |
| Reverse total shoulder | 2 (5.7) |
| Mass excision | 2 (5.7) |
| Cubital tunnel | 2 (5.7 |
| ORIF hand | 1 (5.7) |
| Implant removal | 1 (2.8) |
| ORIF scaphoid nonunion | 1 (2.8) |
| Shoulder manipulation | 1 (2.8) |
| de Quervain release | 1 (2.8) |
ORIF, open reduction internal fixation.
Table 3 describes the technological quality and types of devices utilized. Eighty-nine percent of patients utilized a cell phone and 88% of visits were preformed from the patient’s home. There were 4 visits (7%) with technological complications during the study period. During 1 visit, the surgeon was unable to see the patient on video, but the audio was working. In this case, the patient sent images of the surgical site via the electronic medical record system and the visit was conducted with audio only for the surgeon (the patient had normal audio and video feeds). In 3 additional cases, the audio and video feed did not work for either the patient or the surgeon. These visits were rescheduled for later the same day and the telemedicine visit was completed without incident. Overall, patients rated technological ease of use as 9.5 on an 11-point Likert scale, with 10 being very easy.
Table 3.
Description of Telemedicine Visit Factors for Patients and Surgeon
| Variables | All Included Patients |
|---|---|
| Location of visit, n (%) | |
| Home | 50 (88) |
| Work | 7 (12) |
| Device used, n (%) | |
| Cell phone | 51 (89) |
| Laptop | 5 (9) |
| Tablet | 1 (2) |
| Ease of use, 0–10 Likert scale | |
| Mean (SD) | 9.5 (1) |
| Range | 5–10 |
| Prefer Telemed for future visits, n (%) | 56 (98) |
| Video quality for patient, n (%) | |
| 1. None | 3 (5) |
| 2. Reduced/poor | 0 (0) |
| 3. Good | 54 (93) |
| Audio quality for patient, n (%) | |
| 1. None | 3 (5) |
| 2. Reduced/poor | 0 (0) |
| 3. Good | 54 (95) |
| Video quality for surgeon, n (%) | |
| 1. None | 4 (7) |
| 2. Reduced/poor | 0 (0) |
| 3. Good | 53 (93) |
| Audio quality for surgeon, n (%) | |
| 1. None | 3 (5) |
| 2. Reduced/poor | 0 (0) |
| 3. Good | 54 (95) |
Table 4 illustrates the differences between travel and visit times for the telemedicine visit and the in-clinic visit. The mean travel distance for patients was 60 miles round-trip (range, 5–304 miles) and patients spent an average of 85 minutes driving. Visit times were significantly shorter for telemedicine visits (7 minutes vs 38 minutes; P < .05). Visit satisfaction was higher for telemedicine visits (9.9) than for in-clinic visits (9.5) and these results were statistically significant (P < .05).
Table 4.
Comparison of Pain Scores, Visit Times, Travel Times, Distances, and Patient Satisfaction Between Telemedicine Visits and Conventional In-Clinic Visits
| Variables | Visit 1 Telemedicine | Visit 2 In-Clinic | P Value |
|---|---|---|---|
| NPRS, mean (SD) | 2 (1) | 2.0 (2) | .33 |
| Visit time, min | |||
| Mean (range) | 7 (4–17) | 38 (14–87) | <.05 |
| Travel time, min round trip | |||
| Mean (range) | 0 | 85 (14–308) | <.05 |
| Travel distance, mean miles round trip | |||
| Mean (range) | 0 | 60 (5–304) | <.05 |
| Satisfaction with visit, 0–10 Likert scale | |||
| Mean (range) | 9.9 (8–10) | 9.5 (3–10) | <.05 |
Bold indicates statistical significance (P < .05).
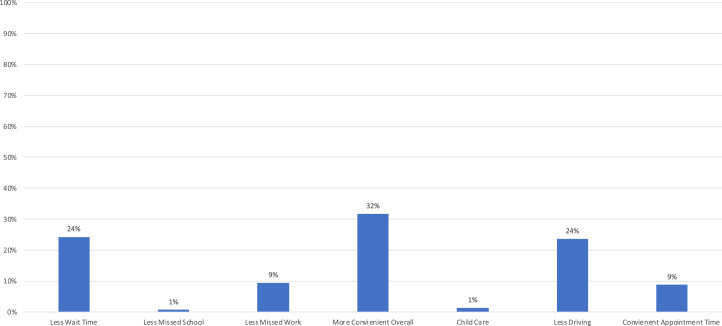
Figure 1 includes the results to a survey asking patients why they chose to utilize telemedicine for their postoperative visit. All 57 patients responded and a total of 148 responses were recorded. The most common reasons for choosing telemedicine were that it was “more convenient overall” (32%) followed by “less driving” and “less wait time” (24%).
Figure 1.
Patient reasons for choosing telemedicine. Fifty-seven patients provided 148 responses to the survey questionnaire.
There were 4 patients (7%) with recognized clinical complications during the study period: wound dehiscence after mass excision, supraclavicular sensory neurapraxia after an open reduction internal fixation (ORIF) of a clavicle fracture, digital stiffness after a combined carpal tunnel and trigger digit release, and a lateral antebrachial cutaneous neurapraxia after a distal biceps tendon repair. All 4 complications that were identified during the study period were recognized during the telemedicine visit. The patient with digital stiffness and the 2 patients with neurapraxic injuries had resolution of their symptoms with observation only. No additional clinic visits were required. The patient with a wound dehiscence after mass excision healed by secondary intention with local wound care. Wound care instructions were provided during the telemedicine encounter and the wound was healed by the scheduled in-clinic visit.
Discussion
These data support our initial hypothesis that patients participating in telemedicine would have decreased visit times and demonstrate high levels of satisfaction. There are several advantages for patients electing to participate in telemedicine after hand and upper extremity procedures. Telemedicine visits decreased total encounter times by 31 minutes in our series and patients avoided an average round-trip drive time of 85 minutes. Similar to our findings, Sathiyakumar et al1 demonstrated that telemedicine can reduce travel time, visit times, and time away from work for patients undergoing nonsurgical treatment of orthopedic trauma injuries.
Whereas patient satisfaction with both telemedicine and in-clinic visits was high in our series, all but 1 patient (98%) preferred the telemedicine visits for future encounters. It is unlikely that the differences in patient satisfaction scores for telemedicine and conventional in-clinic visits were clinically significant. For general orthopedic patients, previous authors have demonstrated that 63% of patients randomized to an in-clinic consultation and 86% of patients randomized to a telemedicine visit preferred telemedicine for future encounters.5 Able et al4 found that, for adolescent patients after knee arthroscopy, two-thirds preferred telemedicine visits.
In implementing this program and analyzing our early experience, we were concerned about technological access issues, particularly for older patients. The average age of patients in our series was 51 and patients up to 78 years old elected to participate. At our rural center, patient convenience appears to be a factor in choosing to participate in telemedicine. Thirty-two percent of patients stated that visits were “more convenient overall” and 9% cited “convenient appointment times.” In addition, we found these visits were often more convenient for the surgeon because they could be conducted outside of standard clinic times, particularly during longer-case turnovers at our main hospital.
Limitations of this study include that it involved a single surgeon and a single institution in a rural location with a homogeneous patient population. The methodology utilized for this investigation is subject to selection bias with respect to patient satisfaction and preferences for telemedicine over conventional clinic visits because all these patients chose to participate in a telemedicine program. However, in clinical practice, only patients willing and able to participate in telemedicine will choose to perform these visits, so our results likely reflect the patient experience with this technology. We recorded travel distances from patient’s home addresses. In some cases, it is possible that the patient may have traveled from work or another location to their in-clinic visit. In addition, the patients in our series underwent lower-complexity surgical procedures owing, in part, to the clinical exclusion criteria. There are inherent limitations associated with physical examination during telemedicine encounters, particularly with respect to the assessment of sensation and provocative maneuvers. Although the remote examination appears to be sufficient for these lower complexity postoperative visits, future analysis of the accuracy of telemedicine examinations is necessary. Future investigations are necessary to analyze the utility of this technology for higher-complexity procedures, particularly with respect to complication recognition.
A telemedicine program for postoperative care after hand and upper extremity surgery decreases travel burdens associated with conventional in-clinic appointments. Furthermore, telemedicine significantly decreases visit times without decreasing patient satisfaction for patients who elect to participate in remote video visits. The ability to recognize early postsurgical complications was not compromised by utilizing this technology, even during our early experience.
Acknowledgments
The authors would like to acknowledge Amy Reitz and Janice Heimbach, RN, for their assistance with patient scheduling and study coordination.
Footnotes
No benefits in any form have been received or will be received related directly or indirectly to the subject of this article.
Supplementary Data
Telehealth FAQ and Troubleshooting Tips
References
- 1.Sathiyakumar V., Apfeld J.C., Obremskey W.T., Thakore R.V., Sethi M.K. Prospective randomized controlled trial using telemedicine for follow-ups in an orthopedic trauma population: a pilot study. J Orthop Trauma. 2015;29(3):e139–e145. doi: 10.1097/BOT.0000000000000189. [DOI] [PubMed] [Google Scholar]
- 2.Tripod M., Tait M., Bracey J., Sexton K., Beck W., Wyrick T.O. The use of telemedicine decreases unnecessary hand trauma transfers. Hand (N Y) 2020;15(3):422–427. doi: 10.1177/1558944718810877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Harno K., Arajärvi E., Paavola T., Carlson C., Viikinkoski P. Clinical effectiveness and cost analysis of patient referral by videoconferencing in orthopaedics. J Telemed Telecare. 2001;7(4):219–225. doi: 10.1258/1357633011936435. [DOI] [PubMed] [Google Scholar]
- 4.Abel K.C., Baldwin K., Chuo J. Can telemedicine be used for adolescent postoperative knee arthroscopy follow-up? JBJS J Orthop Phys Assist. 2017;5(4):e26. [Google Scholar]
- 5.Buvik A., Bugge E., Knutsen G., Småbrekke A., Wilsgaard T. Patient satisfaction with remote orthopaedic consultation by using telemedicine: a randomized controlled trial. J Telemed Telecare. 2019;25(8):451–459. doi: 10.1177/1357633X18783921. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Telehealth FAQ and Troubleshooting Tips