Abstract
Background
After the emergence of Covid-19 in China, Hubei Province, the epidemic quickly spread to Europe. France was quickly hit and our institution was one of the first French university to receive patients infected with Sars-COV2. The predicted massive influx of patients motivated the cancellation of all elective surgical procedures planned to free hospitalization beds and to free intensive care beds. Nevertheless, we should properly select patients who will be canceled to avoid life-threatening. The retained surgical indications are surgical emergencies, oncologic surgery, and organ transplantation.
Material and methods
We describe the organization of our institution which allows the continuation of these surgical activities while limiting the exposure of our patients to the Sars Cov2.
Results
After 4 weeks of implementation of intra-hospital protocols for the control of the Covid-19 epidemic, 112 patients were operated on (104 oncology or emergency surgeries and 8 liver transplants). Only one case of post-operative contamination was observed. No mortality related to Covid-19 was noted. No cases of contamination of surgical care personnel have been reported.
Conclusion
We found that the performance of oncological or emergency surgery is possible, safe for both patients and caregivers.
Keywords: Surgery anesthesiology Covid19
Highlights
-
•
During Covid-19 pandemic, we should properly select patients to avoid a life threatening.
-
•
Need to continue surgical activities while limiting the exposure to the Sars Cov2.
-
•
With all preventive actions, no mortality related to Covid-19 was noted.
-
•
With all preventive actions, no cases of contamination of surgical care personnel.
Abbreviations
- COVID +
COVID positive
- COVID -
COVID negative
- CT
Computed tomography
- ICU
Intensive Care Unit
- NMBA
Neuromuscular blocking agents
- PPE
Personal protective equipment
- RT PCR
Reverse transcriptase-polymerase chain reaction
1. Introduction
After the emergence of Covid-19 in China, France was quickly hit and our institution was one of the first French University Hospitals to receive patients infected with Sars-COV2. To date, the number of infected patients in France is 122577 including 86657 hospitalized patients and 4870 in intensive care, of which 22245 patients have died. The experience acquired in China and neighboring countries has shown rapid development of the pandemic and the need for rapid implementation of a specific organization within our institution [1,2]. The predicted massive influx of patients motivated the cancellation of all elective surgical procedures planned in an attempt to free standard and intensive care unit beds. The anesthesiology and intensive care teams usually dedicated to the operating rooms were gradually reassigned to the new intensive care units. The number of active operating theatres was reduced from 20 to 5.
Nevertheless, proper patient selection is mandatory to avoid any loss of chance among patients with life-threatening conditions. The retained surgical indications were surgical emergencies, oncologic surgery, and vital organ transplantation. One major challenge is to reorganize the hospital system to limit the risk of exposure to Sars-COV2 in surgical patients more prone to develop serious forms of Covid-19 [3] while keeping enough acute care resources for managing both COVID+ and COVID-.
Our institution combines 2 specificities: firstly, it consists of one of the leading infectious disease departments in France and Europe, and the principal investigator of the large-scale European DISCOVERY study (NCT04315948) belongs to the institution. Second, it represents a tertiary referral center for several surgical specialties, including general surgery, head and neck surgery, gynecologic surgery, and liver transplantation.
The present work aimed to describe the reorganization of the anesthesiology and surgical departments in a tertiary university hospital at the frontline of the management of both COVID+ and surgical patients and to report the outcome of patients admitted to the institution for surgery during the first month after implementing the described reorganization.
2. Methods
This retrospective quality improvement study has been registered in a publicly accessible database: Clinical Trials (NCT04379232). The work has been reported in line with the STROCSS criteria [4], and the work has been reported in line with the Standards for Quality Improvement Reporting Excellence (SQUIRE) criteria.
Patients were operated in our institution.
2.1. General organization of the surgical department
2.1.1. Postponement of non-urgent interventions
Only urgent surgeries and oncologic surgery with risk of loss of opportunity in the short or medium-term (4 weeks) are maintained.
2.1.2. Covid-19 detection
Standardized management is defined for patients hospitalized for urgent surgery or for whom an elective surgery cannot be delayed. A medical examination is carried out the day before surgery in the usual surgical department or by a phone call before admission to evaluate the risk of Covid-19.
Systematic screening tests are carried out even in the absence of symptoms. RT-PCR and a chest computed tomography (CT) scan without injection are performed. For elective surgery, results must be known before surgery.
Achieving these two tests is necessary to lower the rate of false-negative patients [[5], [6], [7]]. Pending the results, medical and paramedical teams should follow personal protective equipment adapted to the management of COVID + patients.
2.1.3. Creation of a COVID-negative surgical department
In COVID-negative (COVID-) surgical department each patient has to be tested negative before surgery. The paramedical team should not have any activity in COVID + units. In case of suspicion during hospitalization, the patient is tested and isolated during the time to get the result.
With the cancellation of many elective surgeries, some surgical departments are free and reserved to become COVID + departments if necessary.
2.1.4. Dedicated surgical COVID + unit
A dedicated surgical unit was created specifically for COVID + patients. Before integrating the unit, the entire medical and paramedical staff benefitted from a theoretical course provided by the hospital's operational hygiene team. Drug and medical prescriptions are the responsibility of the surgeon in charge; however, daily ward rounds are limited to the strict minimum, and performed by a single surgeon, regardless of his specialty. Pictures of surgical wounds, drain fluid aspects and other clinical features are sent if necessary to the surgeon in charge, and physical examination is restricted. All medical care and nursing are performed using maximal individual protective measures, including the use of surgical or FFP2 masks depending on the type of gesture, disposable and protective aprons, gloves, protective headwear, and glasses.
2.1.5. Organization of the operating theater
For non-deferrable surgeries, patients are tested preoperatively and operated in conventional operating rooms and then hospitalized in COVID-units.
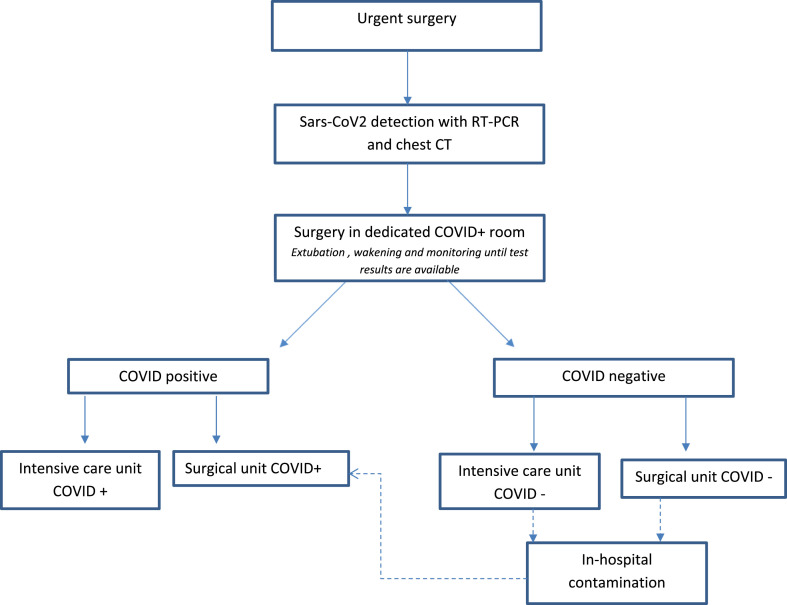
For urgent surgeries: an emergency room has been specially equipped for negative patients. A second room is reserved for COVID + patients or awaiting results. Fig. 1 shows the perioperative algorithm.
Fig. 1.
Perioperative protocol.
This dedicated operating room for COVID + patients is organized to contain the spread of infection: only the necessary materials should be placed in the room, traffic should be minimized, surgical approaches should be chosen to reduce the exposure … Every surgical team received appropriate information on the procedure to access into this operating room [8].
2.1.6. Department of anesthesia: perioperative organization
2.1.6.1. Preoperative evaluation
When possible, consultations are dematerialized and a preoperative evaluation is carried out. Each patient is thoroughly examined the day before the intervention by an anesthesiologist.
2.1.6.2. Screening
As explained before, preoperative screening must be systematic regardless of the urgency of the surgery and involves RT-PCR on a nasopharyngeal swab and a chest CT scan. Performing a lower respiratory sample after induction of anesthesia improves the sensitivity of preoperative screening [9]. Endotracheal aspirate or plugged telescopic catheter specimen with or without mini-bronchoalveolar lavage should be preferred to bronchoalveolar lavage which increases the risk of contamination.
A lower respiratory sample must, therefore, be systematically performed if:
-
•
preoperative screening in progress
-
•negative preoperative screening (both NP swab and CT scan) but high-risk factors for COVID-19:
-
-COVID+ “contact patients”
-
-symptomatic patient: fever ≥ 38°, cough, dyspnea, respiratory rate > 22/min, deterioration of the general condition, and digestive symptoms in the elderly patient.
-
-
2.1.6.3. Management
In case of screening in progress or discrepancy between the two tests (negative swab positive CT scan), patients should be considered COVID+. In the case of negative screening, patients at high risk for COVID-19 (symptomatic patients or COVID + contact), should also be considered COVID+.
The use of alternative molecules for the induction and maintenance of anesthesia is strongly encouraged. Balanced or inhaled anesthesia should be preferred to total intravenous anesthesia (TIVA), and neuromuscular blocking agents (NMBA) different from what is commonly needed in ICU should be used. Succinylcholine or rocuronium are alternatives to cisatracurium and atracurium for example.
-
•
COVID-patients: to avoid contamination from a falsely negative tested patient, FFP2 type protective mask, protective glasses, and gloves should be used for management of upper airways, because of the known risk of transmission by this pathway. Standard anesthesia procedures are then performed.
-
•
COVID + confirmed or suspected patients: The patient should wear a face mask during transport to the procedure room. Anesthesia team should wear complete personal protective equipment (PPE) and an FFP2 type protective mask. The operating room is put under negative pressure (if possible).
Anesthesia is then performed according to the French Society of Anesthesia & Intensive Care Medicine's recommendations [10]:
-
-
Use of a high-efficiency hydrophobic filter between the face mask and breathing circuit or between the face mask and airway bag. A filter on the expiratory branch of the respirator is also added.
-
-
Airway management reserved for the most experienced anesthetist.
-
-
Preoxygenation with 100% oxygen: sealed mask connected to the respirator with spontaneous breathing or continuous positive airway pressure.
-
-
Rapid sequence induction (RSI) to avoid patient ventilation.
-
-
Tracheal intubation with the use of video laryngoscopy
-
-
No ventilation is started until the respiratory circuit is connected to the intubation probe
-
-
Circuit connection with closed suction system
-
-
Extubation and wakening in the operation room. A face mask is quickly given to the patient after extubation.
2.2. Management of COVID – patients (if beds still available)
2.2.1. Emergencies
2.2.1.1. Head and neck surgery
Head and neck surgery particularly exposes the surgeon to contamination. Thus for any surgical procedure on the upper airways (including tracheotomy), the surgeon must wear an FFP2 mask and personal protective equipment. Given the rate of false negatives and the risk of exposure during upper airways management, these precautions must be taken even if the test is negative.
Whenever possible, prolonged endotracheal intubation should be preferred to emergency tracheotomy.
2.2.1.2. Gynecological, general and digestive surgery
Contrary to head and neck surgery, intraabdominal surgical procedures are not supposedly associated with a major risk of exposure to the virus. Therefore, no additional recommendations were provided in addition to the usual ones. However, due to the theoretical risk of aerosol release, all surgical staff present in the operative theatre during laparoscopic procedures are asked to wear FFP2 masks, although the level of evidence regarding the latter risk remains low.
2.2.2. Oncologic surgery
2.2.2.1. Head and neck surgery
Only patients with a risk of loss of opportunity in the short or medium-term (4 weeks) are operated. In case of surgery affecting the pharyngeal-laryngeal mucosa, oral cavity, or nasosinusal mucosa, the surgical team must wear an FFP2 mask and personal protective equipment. If tracheotomy is necessary after extensive oncologic resection, a non-surgical treatment alternative should be preferred.
2.2.2.2. Gynecological surgery
All oncological surgical records have been the subject of a multidisciplinary meeting. The surgical procedures have been simplified to limit the risk of surgical complications as much as possible. Heavy pelvic oncological surgery, which might require hospitalization in continuous care, is postponed when possible, and chemotherapy is carried out when possible and without loss of opportunity for ovarian cancer [11]. Surgical management of endometrial and cervical cancers in patients without risk factors is maintained. Surgery for breast cancer is maintained in patients without other risk factors. In elderly or frail patients, hormone therapy is introduced to avoid surgical management and hospitalization during the pandemic period [12].
2.2.2.3. Digestive and hepatobiliary surgery
All patient files are discussed in a dedicated multidisciplinary team meeting. Various factors are taken into account: (i) oncological impact and risk of decreased survival in case of delayed surgery; (ii) existence of an alternative bridging therapy (such as chemotherapy, percutaneous minimally invasive ablation or radiation therapy) that could allow to safely delay the surgery; (iii) requirement for postoperative heavy ICU management; We also took into consideration some recent National French recommendations issued by experts regarding the management of digestive and hepatobiliary cancers [13]. Most surgeries could be delayed depending on the histology and organ involved. For pre-malignant colonic lesions and those with a good predicted prognosis (T1 or T2, N0), delaying the procedure is recommended. For more advanced colonic lesions, the possibility of neoadjuvant therapy has been suggested despite the lack of validity for such a strategy. For most pancreatic cancers, experts have recommended delaying the surgical procedure since pancreatic cancer surgery is associated with an important rate of severe postoperative morbidity, usually requiring intensive postoperative resuscitation. When malignancy has been proven by histology, it is suggested to perform neoadjuvant chemotherapy to decrease the risk of tumor progression. For oesogastric tumors, neoadjuvant chemotherapy alone or chemoradiation therapy is widely proposed, since such therapies have proven to be very effective in controlling the tumor locally. Finally, for primary liver tumors, due to the moderate risk of local progression during the epidemic combined to the existence of effective percutaneous therapies, including radiofrequency or microwave ablations, experts advised delaying the surgical procedures, except for patients requiring a limited gesture, such as wedge resections or monosegmentecomies that could be performed through a laparoscopic approach.
2.2.3. Liver transplant surgery
Contrary to kidney transplant, which could be delayed (thanks to the existence of renal replacement therapy), liver transplantation is a vital procedure that is offered to patients with more or less urgent medical conditions such as acute liver failure or primary liver tumors. Without transplantation, such diseases result in death within days, weeks, or months because of the current lack of effective hepatic replacement therapy. Therefore, and according to the recommendations by the French National Authority for organ transplant [14] and the French hepatobiliary and transplant surgical association [15], we decided to maintain our liver transplant program during the pandemic outbreak. However, due to the lack of knowledge regarding the true impact of COVID-19 on liver transplant recipients, and the possible increased risk of severe respiratory distress syndrome, we decided to limit our indications to the most severe patients who would otherwise be exposed to the risk of death. In addition to recipient testing for COVID-19, all donors also undergo a combined COVID testing including RT-PCR and chest CT, and those with suspected or proven COVID-19 were excluded for organ procurement.
2.3. Management of COVID + patients
2.3.1. Emergencies
Patients requiring emergency surgical management are treated in the dedicated operating room dedicated to these patients. Isolation precautions are taken. In COVID + patients, the risk of contamination of personnel is major because of exposure to the upper airways. For respiratory emergencies, prolonged intubation should be preferred to tracheotomy whenever possible. Personal protective equipment and FFP2 masks are mandatory. Patients are then hospitalized in the COVID + unit.
2.3.2. Oncologic surgery
Oncologic surgeries in COVID + patients are postponed for 2–4 weeks to await recovery and reduction of the patient's contagiousness.
2.3.3. Liver transplant surgery
Despite the absence of strong evidence suggesting a risk of more severe disease in immunosuppressed patients [16], we decided to contra-indicate liver transplant in recipients with a positive COVID test.
3. Results
3.1. General data of the institution
The medical units have been adapted to accommodate a total of 195 COVID + beds in the institution (97 in conventional hospitalization and 98 in rehabilitation care).
We organized 6 COVID + intensive care units with a total of 54 beds and 2 COVID-intensive care units with a total of 15 beds. At the time of writing, 510 COVID + patients have been hospitalized and 90 patients in intensive care units.
3.2. Surgical departments
Data from patients undergoing surgery were collected during the first 4 weeks (23rd March to 19th April) after the opening of the dedicated units and diffusion of the institutional protocols for intra-hospital screening. Each surgical procedure has been classified according to the POSSUM scale, which has been adapted to head and neck procedures [17,18]. Briefly, this classification makes it possible to classify the interventions from minor to major plus according to the degree of severity and surgical technicality.
The total number of patients operated on was 112 patients for the three specialties described in this article (Table 1 ). Among the patients operated on, 28 (27%) were hospitalized in the dedicated COVID + unit, either because it was urgent surgery awaiting screening results or because the screening was positive (5 patients (4.9%)).
Table 1.
Total number of patients operated on for the three specialties with POSSUM scale classification and Sars-Cov2 related outcome.
| General surgery | Gynaecoloical surgery | Head and neck surgery | Liver transplant | Total | |
|---|---|---|---|---|---|
| Total No. of procedures | 39 | 37 | 28 | 8 | 112 |
| Operative severity | |||||
| Minor (%) | 3 (8) | 21 (57) | 7 (25) | 0 (0) | 31 (27.7) |
| Moderate (%) | 13 (33) | 16 (43) | 7 (25) | 0 (0) | 36 (32.1) |
| Major (%) | 14 (36) | 0 (0) | 7 (25) | 0 (0) | 21 (18.8) |
| Major plus (%) | 9 (23) | 0 (0) | 7 (25) | 8 (100) | 24 (14.3) |
| COVID + status at the time of surgery (%) | 0 (0) | 1 (3) | 0 (0) | 0 (0) | 1 (0.9) |
| No. ambulatory procedures (%) | 0 (0) | 22 (59) | 3 (11) | 0 (0) | 25 (22.3) |
| Postoperative ICU stay (%) | 6 (15) | 0 (0) | 8 (29) | 8 (100) | 22 (19.6) |
| Contamination of medical or paramedical staff (%) | 0 | 0 | 0 | 0 | 0 (0) |
8 liver transplants have been performed with 100% survival at the time of writing this article.
No mortality related to Covid-19 was noted.
No postoperative contamination was observed in the COVID-patients. Follow-up with RT-PCR was not routinely performed, only if the patient had symptoms compatible with COVID post-operatively. No contamination of nursing staff, surgeons, or anesthesiologists caring for these surgical patients was observed.
3.2.1. Digestive surgery
In digestive surgery (Table 2 ), 39 patients were operated on from March 23 to April 19. None of the patients were COVID+. One patient (2%) had post-operative contamination discovered on CT. This patient was asymptomatic. According to the POSSUM scale, all types of minor to major plus surgeries were performed, 6 patients (15%) were hospitalized in the intensive care unit after complex surgery.
Table 2.
Digestive surgeries with POSSUM scale classification and Covid status.
| Age (Years) | Indication | Indication type (malignancy/emergency/other) | Procedure | Surgical Approach | Operative severity (POSSUM scale) | COVID Test (PCR + CT Chest) | |
|---|---|---|---|---|---|---|---|
| 1 | 47 | Acute cholecystitis | emergency | Cholecystectomy | Laparoscopy | moderate | negative |
| 2 | 90 | Acute cholecystitis | emergency | Cholecystectomy | Laparoscopy | moderate | negative |
| 3 | 62 | Acute cholecystitis | emergency | Cholecystectomy | Laparoscopy | moderate | negative |
| 4 | 46 | Acute cholecystitis | emergency | Cholecystectomy | Laparoscopy | moderate | negative |
| 5 | 36 | Anal Abscess | emergency | Drainage | Perineal | minor | negative |
| 6 | 91 | Biliary Peritonitis | emergency | Laparoscopic drainage | Laparoscopy | moderate | negative |
| 7 | 68 | Cholangiocarcinoma | malignancy | Bi-segmentectomy | Laparotomy | major plus | negative |
| 8 | 62 | Cholangiocarcinoma | malignancy | No resection | Conversion to Laparotomy | major | negative |
| 9 | 63 | Cholangiocarcinoma | malignancy | Non-anatomical Liver Resection | Laparotomy | major plus | negative |
| 10 | 64 | Colorectal Adenocarcinoma | malignancy | Right Colectomy | Laparotomy | major | negative |
| 11 | 55 | Colorectal Adenocarcinoma | malignancy | Left Colectomy | Laparoscopy | major | negative |
| 12 | 61 | Colorectal Adenocarcinoma | malignancy | Transvers Colectomy | Laparoscopy | major | negative |
| 13 | 66 | Colorectal Adenocarcinoma | malignancy | Colostomy | Laparotomy | major | negative |
| 14 | 66 | Colorectal Adenocarcinoma | malignancy | Left Colectomy | Conversion to Laparotomy | major | negative |
| 15 | 67 | Colorectal Adenocarcinoma | malignancy | Left colectomy | Conversion to Laparotomy | major | negative |
| 16 | 57 | Colorectal Adenocarcinoma | malignancy | Total Coloprotectomy | Laparotomy | major | negative |
| 17 | 72 | Colostomy | malignancy | Left colectomy | Laparoscopy | moderate | negative |
| 18 | 63 | Congenital Bie Dilatation (Todani IV) | Main Bile Duct Resection | Laparotomy | major | negative | |
| 19 | 53 | Colorectal Liver Metasteses | malignancy | Laparoscopy and focal destruction | Laparoscopy | moderate | negative |
| 20 | 72 | Gallbladder Tumor | malignancy | Bi-segmentectomy | Conversion to Laparotomy | major plus | negative |
| 21 | 59 | Gallbladder Tumor | malignancy | Cholecystectomy | Laparotomy | major | negative |
| 22 | 69 | Gastric Adenocarcinoma | malignancy | Gastrectomy | Laparotomy | major plus | negative |
| 23 | 71 | Hepatocellular Carcinoma | malignancy | Bi-segmentectomy | Laparotomy | major plus | negative |
| 24 | 58 | Hepatocellular Carcinoma | malignancy | Cholecystectomy-Focal Ablation | Laparoscopy | moderate | negative |
| 25 | 61 | Umbilical Hernia | emergency | Umbilical Hernia Repair | Laparotomy | minor | negative |
| 26 | 84 | Inguinal Hernia | emergency | Inguinal Hernia Repair | Laparotomy | minor | negative |
| 27 | 37 | Liver Adenoma | other | Segmentectomy | Laparoscopy | major plus | negative |
| 28 | 69 | Liver Adenoma | other | Segmentectomy | Laparoscopy | major plus | negative |
| 29 | 73 | Common Bile Duct Stone | emergency | Cholecystectomy | Laparoscopy | major | negative |
| 30 | 70 | Common Bile Duct Stone | emergency | Cholecystectomy | Laparoscopy | major | negative |
| 31 | 65 | undetermined malignancy | malignancy | exploratory thoracoscopy | Thoracoscopy | moderate | negative |
| 32 | 60 | Hepatocellular Carcinoma | malignancy | Uni-segmentectomy | Laparotomy | major plus | negative |
| 33 | 64 | Hepatocellular Carcinoma | malignancy | right hemihepatectomy | Laparotomy | major | negative |
| 34 | 63 | Acute cholecystitis | emergency | Cholecystectomy | Laparoscopy | moderate | negative |
| 35 | 65 | Acute cholecystitis | emergency | Cholecystectomy | Laparoscopy | moderate | negative |
| 36 | 34 | Acute cholecystitis | emergency | Cholecystectomy | Laparoscopy | moderate | negative |
| 37 | 64 | Pancreatic adenocarcinoma | malignancy | Pancreaticoduodenectomy | Laparotomy | major plus | negative |
| 38 | 67 | Inflammatory colic stricture | emergency | Colostomy | Laparotomy | major | negative |
| 39 | 56 | Common Bile Duct Stone | emergency | Cholecystectomy | Laparoscopy | moderate | negative |
No cases of contamination of the caregivers were reported in the follow-up of these patients.
3.2.2. Liver transplantation
8 liver transplants have been performed.
All of these procedures were a major plus on the POSSUM scale, all patients were hospitalized in intensive care and the survival is 100% at the time of writing this article.
No cases of postoperative contamination of transplanted patients have been described (Table 1).
3.2.3. Gynecological surgery
In gynecological surgery (Table 3 ), 37 patients were operated on. One patient (3%) had a positive preoperative COVID screening. 57% of the procedures were minor surgery on the POSSUM scale and 43% were moderate surgery. 22 (59%) surgeries were performed as ambulatory surgeries.
Table 3.
Gynaecological surgeries with POSSUM scale classification and Covid status.
| Age (Years) | Indication | Indication type (malignancy/emergency/other) | Procedure | Surgical Approach | Operative severity (POSSUM scale) | Ambulatory surgery | COVID Test (PCR + CT Chest) | Clinical screening for COVID | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 28 | Miscarriage | emergency | Aspiration-curettage | vaginal | Minor | yes | negative | |
| 2 | 37 | Miscarriage | emergency | Hysteroscopy | vaginal | Minor | yes | negative | |
| 3 | 36 | Miscarriage | emergency | Aspiration-curettage | vaginal | Minor | yes | negative | |
| 4 | 54 | postmenopausal metrorragia | malignancy | Hysteroscopy | vaginal | Minor | yes | negative | |
| 5 | 58 | breast neoplasm | malignancy | Mastectomy | direct | Moderate | yes | negative | |
| 6 | 78 | breast neoplasm | malignancy | Mastectomy | direct | Moderate | no | negative | |
| 7 | 73 | breast neoplasm | malignancy | Tumorectomy | direct | Minor | yes | negative | |
| 8 | 34 | Miscarriage | emergency | Aspiration-curettage | vaginal | Minor | yes | negative | |
| 9 | 53 | breast neoplasm | malignancy | Tumorectomy + AD | direct | Moderate | yes | negative | |
| 10 | 55 | breast neoplasm | malignancy | Tumorectomy | direct | Minor | yes | negative | |
| 11 | 51 | breast neoplasm | malignancy | Tumorectomy + AD | direct | Moderate | yes | negative | |
| 12 | 71 | breast neoplasm | malignancy | Tumorectomy | direct | Minor | no | negative | |
| 13 | 52 | breast neoplasm | malignancy | axillary dissection | direct | Moderate | yes | negative | |
| 14 | 30 | cervical intraepithelial neoplasia | malignancy | Cone biopsy | vaginal | Minor | yes | negative | |
| 15 | 30 | Adnexal torsion | emergency | laparoscopy | laparoscopy | Moderate | no | negative | negative |
| 16 | 47 | breast neoplasm | malignancy | Tumorectomy | direct | Minor | yes | negative | |
| 17 | 39 | breast neoplasm | malignancy | Tumorectomy | direct | Minor | yes | negative | |
| 18 | 51 | Cancer | malignancy | Port-a-cath placement | direct | Minor | yes | negative | |
| 19 | 77 | breast neoplasm | malignancy | Tumorectomy | direct | Minor | yes | negative | |
| 20 | 43 | breast neoplasm | malignancy | Tumorectomy | direct | Minor | yes | negative | |
| 21 | 40 | Miscarriage | emergency | Aspiration-curettage | vaginal | Minor | no | negative | negative |
| 22 | 32 | Ovarian cyst | malignancy | laparoscopy | laparoscopy | Moderate | no | negative | negative |
| 23 | 39 | ectopic pregnancy | emergency | salpingotomy | laparoscopy | Moderate | no | negative | negative |
| 24 | 39 | ectopic pregnancy | emergency | salpingectmoy | laparoscopy | Moderate | no | negative | negative |
| 25 | 29 | Miscarriage | emergency | Aspiration-curettage | vaginal | Minor | no | negative | negative |
| 26 | 36 | Miscarriage | emergency | Aspiration-curettage | vaginal | Minor | yes | negative | |
| 27 | 35 | Adnexal torsion | emergency | laparoscopy | laparoscopy | Moderate | no | negative | negative |
| 28 | 27 | pregnancy | emergency | Cerclage | vaginal | Minor | no | positive | positive |
| 29 | 30 | Unexplained pelvic pain | emergency | laparoscopy | laparoscopy | Moderate | no | negative | negative |
| 30 | 29 | ectopic pregnancy | emergency | Salpingectomy | laparoscopy | Moderate | no | negative | negative |
| 31 | 27 | ectopic pregnancy | emergency | salpingectomy | laparoscopy | Moderate | no | negative | negative |
| 32 | 35 | pregnancy | emergency | cerclage Benson | vaginal | Moderate | yes | negative | |
| 33 | 38 | Miscarriage | emergency | Aspiration-curettage | vaginal | Minor | yes | negative | |
| 34 | 63 | breast neoplasm | malignancy | Tumorectomy | direct | Minor | yes | negative | |
| 35 | 29 | Adnexal torsion | emergency | laparoscopy | laparoscopy | Moderate | no | negative | negative |
| 36 | 36 | breast neoplasm | malignancy | Tumorectomy | direct | Minor | yes | negative | |
| 37 | 33 | Adnexal torsion | emergency | laparoscopy | laparoscopy | Moderate | no | negative | negative |
3.2.4. Head and neck surgery
In head and neck surgery (Table 4 ), 28 patients were operated on. No patients tested positive in pre-operative care. According to the POSSUM scale adapted to head and neck surgery, minor to major plus surgeries were performed. 29% of patients were admitted to the intensive care unit postoperatively. 11% of the procedures were performed in outpatient surgery. No cases of postoperative contamination were described in any of the patients.
Table 4.
Head and Neck surgeries with POSSUM scale classification and Covid status.
| Age (Years) | Indication | Indication type (malignancy/emergency/other) | Procedure | Operative severity (POSSUM scale) | Ambulatory surgery | ICU after surgery | COVID test (PCR + CT chest) | Clinical screening for COVID | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 57 | laryngeal cancer | malignancy | endoscopy + laser | minor | yes | no | negative | |
| 2 | 57 | hemorragae | emergency | cervicotomy | moderate | no | no | negative | negative |
| 3 | 79 | oral cavity cancer | malignancy | endoscopy | minor | yes | no | negative | |
| 4 | 65 | pharyngeal cancer | malignancy | endoscopy | minor | yes | no | negative | |
| 5 | 89 | parotid cancer | malignancy | radical parotidectomy | major | no | no | negative | negative |
| 6 | 82 | cutaneaous cancer | malignancy | resection and local reconstruction | moderate | no | no | negative | negative |
| 7 | 51 | nodal recurrnce of nasopharyngeal cancer | malignancy | neck dissection | moderate | no | no | negative | negative |
| 8 | 54 | laryngeal cancer | malignancy | endoscopy | major | no | no | negative | negative |
| 9 | 63 | oral cavity cancer | malignancy | pelviglossectomy, neck disection, free flap | major plus | no | yes | negative | negative |
| 10 | 64 | oral cavity cancer | malignancy | glossectomy, neck dissection | major | no | no | negative | negative |
| 11 | 66 | parotid cancer | malignancy | radical parotidectomy, free flap for facial reinnervation | major plus | no | yes | negative | negative |
| 12 | 47 | tracheal stenosis | other | endoscopy + laser | moderate | no | no | negative | negative |
| 13 | 74 | sinus cancer | malignancy | endoscopy | minor | no | no | negative | negative |
| 14 | 63 | maxillary sinus cancer | malignancy | endoscopy | minor | no | no | negative | negative |
| 15 | 78 | oral cavity cancer | malignancy | pelviglossectomy, neck disection, free flap | major plus | no | yes | negative | negative |
| 16 | 60 | laryngeal cancer | malignancy | endoscopy + laser | moderate | no | no | negative | negative |
| 17 | 61 | oral cavity cancer | malignancy | pelviglossectomy, neck disection, locoregional flap | major | no | no | negative | negative |
| 18 | 51 | oral cavity cancer | malignancy | pelviglossectomy | moderate | no | no | negative | negative |
| 19 | 55 | oral cavity cancer | malignancy | total glossectomy, neck dissection, free flap | major plus | no | yes | negative | negative |
| 20 | 83 | ethmoidal sinus cancer | malignancy | bicoronal approach | major | no | no | negative | negative |
| 21 | 62 | maxillary sinus cancer | malignancy | maxillectomy, neck dissection, free flap | major plus | no | yes | negative | negative |
| 22 | 60 | laryngeal cancer | malignancy | endoscopy | minor | no | no | negative | negative |
| 23 | 58 | laryngeal stenosis | other | endoscopy + laser | moderate | no | no | negative | negative |
| 24 | 70 | oral cavity cancer | malignancy | glossectomy, neck dissection | major | no | no | negative | negative |
| 25 | 88 | maxillary sinus cancer | malignancy | maxillectomy, neck dissection, free flap | major plus | no | yes | negative | negative |
| 26 | 65 | pharyngeal cancer | malignancy | endoscopy + laser | major | no | no | negative | negative |
| 27 | 82 | oral cavity cancer | malignancy | cheek resection, neck dissection, free flap | major plus | no | yes | negative | negative |
| 28 | 88 | dyspnea | emergency | tracheotomy | minor | no | yes | negative | negative |
| 29 | 42 | laryngeal cancer | malignancy | post poned | no | positive | positive |
4. Discussion
The Covid-19 pandemic exposes all the world's health care institutions to management challenges and the need for a major reorganization. All elective surgeries are being deprogrammed and medical departments must free up as many beds as possible to accommodate the wave of patients affected by Covid-19.
Nevertheless, certain surgical indications in patients not affected by Covid-19 must be maintained with the risk of perioperative contamination.
Our article, therefore, describes the results of surgical management in 3 different specialties that have decided to continue their oncology and emergency surgery activity. Our results show that an organization adapted to the pandemic context with strict compliance with protective measures makes it possible to continue a surgical activity without contamination of the most fragile patients. No mortality related to Covid-19 was noted.
We, therefore, believe that these surgical activities must be maintained so that our patients do not suffer a loss of opportunity in their care.
On the other hand, during these 4 weeks after the implementation of intra-hospital screening protocols and after the creation of dedicated surgical COVID + units, we have not noted any cases of contamination of the nursing staff in the surgical departments, even among anaesthesiologists or in endoscopic airway surgery, which are highly exposed to contamination by Sars Cov-2. Nevertheless, our article has some limitations such as its retrospective nature and the absence of post-operative systematic screening for Covid-19 in all surgeons, anesthesiologists, residents, and nursing staff in charge of the patients.
5. Conclusion
After 4 weeks of implementation of intra-hospital protocols during the Covid-19 pandemic, we find that the performance of oncological or emergency surgery is possible, safe for both patients and caregivers.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Fund
No funding.
Data statement
All the data is available.
CRediT authorship contribution statement
P. Philouze: Conceptualization, Funding acquisition, Formal analysis, Writing - original draft. M. Cortet: Conceptualization, Funding acquisition, Formal analysis, Writing - original draft. D. Quattrone: Conceptualization, Funding acquisition, Formal analysis, Writing - original draft. P. Céruse: Conceptualization, Funding acquisition, Formal analysis, Writing - original draft. F. Aubrun: Conceptualization, Funding acquisition, Formal analysis, Writing - original draft. G. Dubernard: Conceptualization, Funding acquisition, Formal analysis, Writing - original draft. J.Y. Mabrut: Conceptualization, Funding acquisition, Formal analysis, Writing - original draft. M.C. Delignette: Conceptualization, Funding acquisition, Formal analysis, Writing - original draft. K. Mohkam: Conceptualization, Funding acquisition, Formal analysis, Writing - original draft.
Declaration of competing interest
None.
Contributor Information
P. Philouze, Email: pierre.philouze@chu-lyon.fr.
M. Cortet, Email: marion.cortet@chu-lyon.fr.
D. Quattrone, Email: diego.quattrone@chu-lyon.fr.
P. Céruse, Email: philippe.ceruse@chu-lyon.fr.
F. Aubrun, Email: frederic.aubrun@chu-lyon.fr.
G. Dubernard, Email: gil.dubernard@chu-lyon.fr.
J.Y. Mabrut, Email: jean-yves.mabrut@chu-lyon.fr.
M.C. Delignette, Email: marie-charlotte.delignette@chu-lyon.fr.
K. Mohkam, Email: kayvan.mohkam@chu-lyon.fr.
References
- 1.Tao K.X. Recommendations for general surgery clinical practice in 2019 coronavirus disease situation. Zhonghua Wai Ke Za Zhi. mars 2020;58(3):170–177. doi: 10.3760/cma.j.issn.0529-5815.2020.03.003. [DOI] [PubMed] [Google Scholar]
- 2.Ficarra V. Urology practice during COVID-19 pandemic. Minerva Urol. Nefrol. mars 2020 doi: 10.23736/S0393-2249.20.03846-1. [DOI] [PubMed] [Google Scholar]
- 3.Liang W. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21(3):335–337. doi: 10.1016/S1470-2045(20)30096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Agha R. STROCSS 2019 Guideline: strengthening the reporting of cohort studies in surgery. Int. J. Surg. déc. 2019;72:156–165. doi: 10.1016/j.ijsu.2019.11.002. [DOI] [PubMed] [Google Scholar]
- 5.Ai T. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. févr. 2020:200642. doi: 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lin C. « Asymptomatic novel coronavirus pneumonia patient outside Wuhan: the value of CT images in the course of the disease ». Clin. Imag. févr. 2020;63:7–9. doi: 10.1016/j.clinimag.2020.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Han R., Huang L., Jiang H., Dong J., Peng H., Zhang D. Early clinical and CT manifestations of coronavirus disease 2019 (COVID-19) pneumonia. AJR Am. J. Roentgenol. mars 2020:1–6. doi: 10.2214/AJR.20.22961. [DOI] [PubMed] [Google Scholar]
- 8.Peng P.W.H., Ho P.-L., Hota S.S. « Outbreak of a new coronavirus: what anaesthetists should know ». Br J Anaesth, févr. 2020 doi: 10.1016/j.bja.2020.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bouadma L., Lescure F.-X., Lucet J.-C., Yazdanpanah Y., Timsit J.-F. « Severe SARS-CoV-2 infections: practical considerations and management strategy for intensivists ». Intensive Care Med. 2020;46(4):579–582. doi: 10.1007/s00134-020-05967-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.2020. Propositions pour la prise en charge anesthésique d’un patient suspect ou infecté à Coronavirus COVID-19 - La SFAR.https://sfar.org/propositions-pour-la-prise-en-charge-anesthesique-dun-patient-suspect-ou-infecte-a-coronavirus-covid-19 Société Française d'Anesthésie et de Réanimation, mars 06. (consulté le avr. 03, 2020) [Google Scholar]
- 11.Synthèse - conduites à tenir initiales devant des patientes atteintes d’un cancer épithélial de l’ovaire - ref : recokovaires19. https://www.e-cancer.fr/Expertises-et-publications/Catalogue-des-publications/Synthese-Conduites-a-tenir-initiales-devant-des-patientes-atteintes-d-un-cancer-epithelial-de-l-ovaire consulté le mars 30, 2020.
- 12.S. de C. G. et P.- SCGP . SCGP; 2020. Face au COVID-19 : RPC Cancers du sein », Société de Chirurgie Gynécologique et Pelvienne.https://www.scgp-asso.fr/actualites/rpc-cancers-du-sein/ mars 27. (consulté le mars 30, 2020) [Google Scholar]
- 13.Voron T. Surgical management of gastric adenocarcinoma. Official expert recommendations delivered under the aegis of the French Association of Surgery (AFC) J. Vis. Surg. mars 2020 doi: 10.1016/j.jviscsurg.2020.02.006. [DOI] [PubMed] [Google Scholar]
- 14.Recommandation concernant l’activité de prélèvement et de (…) - agence de la biomédecine. mars 27, 2020. https://www.agence-biomedecine.fr/Recommandation-concernant-l-activite-de-prelevement-et-de-greffe-d-organes-et-1314 consulté le avr. 06, 2020.
- 15.Association chirurgie hepato bilio pancreatique transplantation. achbt. 2020 doi: 10.21037/hbsn-2021-4. https://www.achbt.org consulté le avr. 06, [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.D'Antiga L., Coronaviruses and immunosuppressed patients The facts during the third epidemic Liver Transplant. mars 2020 doi: 10.1002/lt.25756. [DOI] [PubMed] [Google Scholar]
- 17.Copeland G.P., Jones D., Walters M. « POSSUM: a scoring system for surgical audit ». Br. J. Surg. mars 1991;78(3):355–360. doi: 10.1002/bjs.1800780327. [DOI] [PubMed] [Google Scholar]
- 18.Griffiths H., Cuddihy P., Davis S., Parikh S., Tomkinson A. Risk-adjusted comparative audit. Is Possum applicable to head and neck surgery? Clin. Otolaryngol. Allied Sci. déc. 2002;27(6):517–520. doi: 10.1046/j.1365-2273.2002.00626.x. [DOI] [PubMed] [Google Scholar]