Abstract
Background
The current pandemic crisis, caused by a novel human coronavirus named severe acute respiratory syndrome coronavirus 2 (SARS-CoV2), has forced a dramatic change in our society. A key portion of the medical work force on the frontline is composed of resident physicians. Thus, it becomes imperative to create an adequate and effective action plan to restructure this valuable human resource amid the SARS-CoV2 pandemic. We sought to describe a comprehensive approach taken by a Neurosurgery Department in quaternary care academic institution in the United States of America amid the SARS-CoV2 pandemic focused in resident training and support.
Objective
To describe a comprehensive approach taken by a Neurosurgery Department in quaternary care academic institution in the United States of America amid the SARS-CoV2 pandemic focused on resident training and support.
Results
A restructuring of the Neurosurgery Department at our academic institution was performed focused on decreasing their risk of infection/exposure and transmission to others, while minimizing negative consequences in the training experience. An online academic platform was built for resident education, guidance, and support, as well as continue channel for pandemic update by the department leadership.
Conclusions
The SARS-CoV2 pandemic constitutes a global health emergency full of uncertainty. Treatment, scope, duration, and economic burden forced a major restructuring of our medical practice. In this regard, academic institutions must direct efforts to diminish further negative impact in the training and education of the upcoming generation of physicians, including those currently in medical school. Perhaps the only silver lining in this terrible disruption will be greater appreciation of the role of current health care providers and educators, whose contributions to our society are often neglected or unrecognized.
Key words: Coronavirus, COVID-19, Education, Neurosurgery, Pandemic, SARS-CoV2
Abbreviations and Acronyms: AANS, American Association of Neurological Surgeons; CNS, Congress of Neurological Surgeons; PPE, Personal protective equipment; SARS-CoV2, Severe acute respiratory syndrome coronavirus 2; SSF, Seattle Science Foundation
Introduction
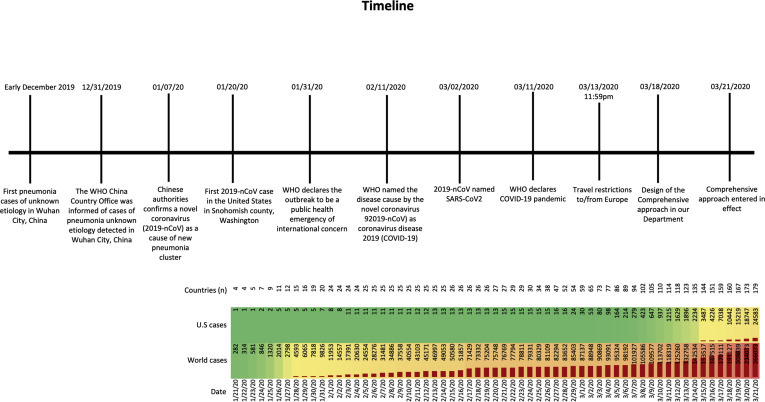
The current pandemic crisis caused by a novel human coronavirus, named severe acute respiratory syndrome coronavirus 2 (SARS-CoV2),1 has forced a dramatic change in our society (Figure 1 ). Although this is primarily a medical condition affecting the respiratory system,2, 3, 4, 5 its virulence and contagiousness have affected how medicine is practiced in every specialty.6, 7, 8, 9, 10, 11 Each hospital around the world will have to adapt its practice to continue to provide high-quality care efficaciously and safely.
Figure 1.
Timeline of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV2) pandemic. Summary of the events that have occurred since the very first cases in Wuhan, China to the implementation of the comprehensive approach at the Department of Neurological Surgery at the University of Pittsburgh Medical Center (Pittsburgh, Pennsylvania, USA). WHO, World Health Organization.
A key portion of the medical workforce includes resident physicians. It is imperative to create an adequate and effective action plan to restructure this valuable human resource. These actions necessitate reducing the risk of resident exposure to the virus while maintaining excellent patient care and resident education. The balance between providing timely care to patients with emergent or urgent medical conditions while maintaining a low risk of illness to the health of providers is the dilemma facing medical care across the world.
Herein, we provide a comprehensive stepwise action plan for neurosurgical care implemented at our quaternary academic medical center facing SARS-CoV2 outbreak. This approach could be applied, modified, and improved by other academic departments around the globe and perhaps serve as a reference for future pandemics.
Comprehensive Approach
The approach taken by our department was based on the Hippocratic principle of “primum non nocere” (first do no harm). We aimed to decrease the exposure and infection of both health care providers (faculty, residents, advanced practice providers, nurses, and supporting staff) as well as patients seeking care in our hospital system. The different actions taken by our team are detailed herein (Figure 2 ). Of note, at the time of the implementation of this comprehensive plan (March 31, 2020), the disease burden in our region was as follows: total cases in the state of Pennsylvania was 4843 cases, Allegheny county 325 cases.
-
1.
Health system and departmental leadership monitor the national and local status of the number of positive SARS-CoV2 cases, number of admissions, intensive care unit bed and ventilator availability, extracorporeal membrane oxygenation machines, PPE (personal protective equipment), and human resources available in our institution.
-
2.
As a general rule, every individual entering the hospital is screened with a noncontact infrared forehead thermometer, a questionnaire for SARS-CoV2 symptoms, and provided with a shift-use face mask. Initially, accompanying visitors were restricted to a single family member or friend and eventually no visitors were permitted. Patients and accompanying visitors were provided with a mask, which was discarded at the time they would leave the hospital. For health care providers, masks could be exchanged as needed and special considerations for N95, googles, gown, and boots were set with regard to taking care of patients who are being rule out for or already confirmed positive for SARS-CoV2 infection.
-
3.Outpatient clinic: Routine new or follow-up visits rapidly were moved toward a virtual telemedicine platform pre-existing within our health care system (Figure 3).
-
a.Telemedicine visits were to be used to screen urgent surgical cases in a time-sensitive manner. Patients were scheduled for 15-minute telemedicine visits (or longer on a case-by-case basis). This would decrease the volume of patients having to come to the hospital and thus reduce the risk of virus exposure to the patient and health care providers
-
b.Patients who required in-person visits (e.g., concerning wound checks, suture/staples removal, or inability to access the online platform) were scheduled for an outpatient appointment. These visits would adhere to social distancing guidelines in the waiting room and involve short wait times. Clear demarcations were placed on the outpatient floor to facilitate a distance of at least 6 feet away between individuals.
-
c.Institutions without telemedicine infrastructure alternatively would be permitted to use commercial video-conferencing platforms such as Skype, Microsoft Teams, Zoom, FaceTime, and WhatsApp depending on their local availability, patient confidentiality, and individual institutional policies.
-
a.
-
4.Patient care provider coverage:
-
a.Resident distribution: our 7-year program has 4 residents per year, for a total of 28 residents covering 5 of the 40 hospitals in our health system. Every resident class was divided by half and residents were reassigned to each of the 5 covered hospitals. Of note, any neurosurgery resident rotating on an off-service rotation (e.g., neuropathology, neurology, emergency room, and other electives) was reassigned back to the neurosurgery service. This arrangement generated 2 resident groups with alternating “weeks on” and “weeks off” assignments. Group “A” had clinical coverage for 7 days, whereas group “B” remained quarantined at home. Sign-out was conducted via phone to avoid physical proximity. The restructuring of resident duties afforded adaptability in case a resident became ill and required quarantine for 2 weeks.
-
b.Operating room participation: We implemented a plan so that only one resident was in each operating room per day to decrease the risk of exposure to multiple residents at a given time, to limit the use of PPE, and preserve the surgical training experience. In cases in which no resident was available, the responsible attending neurosurgeon performed the surgery without resident assistance. Endoscopic endonasal approaches and other skull base operations that require sinus drilling (and which have a greater risk of viral aerosolization) were to be performed by attending physicians only. This policy derived from initial reports suggesting that transmissibility of the virus during such procedures was high.12 , 13 In addition, only minimal essential nursing and technical personnel sufficient to safely provide care in the operating room were permitted.
-
a.
-
5.Emergencies, urgent, and elective surgeries:
-
a.Patients requiring emergency surgeries were managed without delay. These patients would be subsequently monitored for any sign of SARS-CoV2 infection. When appropriate, a SARS-CoV2 test would be performed, and the patient was placed in isolation precautions until they tested negative. Of note, our institution has its own validated SARS-CoV2 polymerase chain reaction test; results were usually available within 6–12 hours after sample collection.
-
b.Neurosurgical case committees: In neurosurgery, the term “elective surgery” proved ambiguous in practice. As an example, patients with newly diagnosed brain tumors may not require emergent care, but timely or even urgent care is appropriate. To determine the timing of nonemergent cases, 5 committees were created: cranial, spine, endovascular, radiosurgery, and pediatric. The function of these committees was to evaluate each case a priori to confirm urgency and to insure appropriate supporting staff availability. Each of these committees had a senior chair and 2 other rotating faculty members who reviewed the cases on a secure teleconference platform (Microsoft TEAMS; Microsoft Corp., Redmond, Washington, USA). Each case was classified as urgent or nonurgent. For nonurgent cases, surgery was postponed until either the current restrictions were to be lifted or if the patient developed any new or progressive neurologic deficit. Once a case was approved by the respective committee, the patient was scheduled for surgery (Figure 3).
-
a.
Figure 2.

Restructure overview. OR, operating room.
Figure 3.
Outpatient clinic workflow. SARS-CoV2, severe acute respiratory syndrome coronavirus 2; ER, emergency room.
Every person was screened and tested for SARS-CoV2 at least 1 day before the proposed surgery. If a patient had symptoms concerning for SARS-CoV2 infection a test was ordered, and if stable, surgery was delayed until the test results returned. Patients with advanced symptoms such as respiratory distress, were admitted to a unique coronavirus disease 2019 unit in our hospital, where they received inpatient testing.14 , 15 If the final test result was negative, and patient deemed appropriate to undergo surgery, we would proceed to surgery. All patients who underwent an endoscopic endonasal approach were tested for SARS-CoV2 preoperatively, because of the increased risk of viral aerosolization during this procedure.13 If SARS-CoV2 positive, surgery was postponed until patient the patient was medically cleared (symptoms free and SARS-CoV2 test negative). Patients with neurologic or life-threatening symptoms underwent surgery even in the face of COVID-19 as long as the respiratory status of the patient allowed it. For instance, a patient in acute respiratory distress syndrome, prone, or in high-ventilator settings would be deemed high risk for transport to the operating room or to undergo a major surgical intervention.
Absorbable skin wound closure was preferred whenever possible and appropriate to reduce the need for a patient to return for suture removal.
-
6.
N95 mask fit testing: scheduled N95 fit testing was organized by our institution to assure all the department members were aware of their mask size and to avoid wasting or suboptimal use of this greater-level PPE.16
-
7.
Didactic lectures: residents lectures were conducted on a daily basis using online platforms. These lectures were mandatory for the off-service group at home and optional for the in-house team. Ninety-minute morning lectures would cover a wide-variety to topics and usually were given by senior or chief residents and faculty with dynamic interaction among attendees.
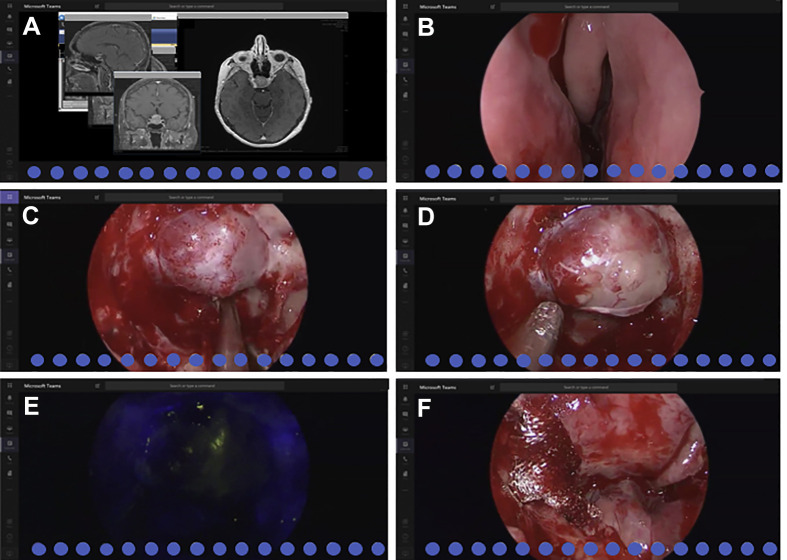
Televised live surgery using either the operating microscope or endoscopy would facilitate back and forth conversation between the residents watching remotely and residents and faculty in the operating room (Figure 4 ). TV cameras embedded in the surgical lights themselves would be another valuable resource for remote observation of ongoing procedures. This infrastructure was already available in our institution and has been extensively used in the past in courses delivered by our faculty.
Figure 4.
Live pituitary adenoma surgery transmitted through virtual platform (participants were covered with blue circles to respect privacy). (A) Faculty responsible for the case discuss the clinical history, imaging findings, and treatment alternatives with the residents. (B) endoscopic endonasal approach (EEA) through the left nostril. (C) Exposure of the sella turcica. (D) Eura matter opening and exposure of the pituitary adenoma. (E) Tumor appearance after intravenous fluorescein injection. (F) Final reconstruction and closing.
Besides these intra-institutional academic activities, the residents would be encouraged to use a wide variety of online resources that have been posted by various organizations, such as the Congress of Neurological Surgeons (CNS), American Association of Neurological Surgeons (AANS), Seattle Science Foundation (SSF), and the Neurosurgical Atlas among many others.
-
8.
Departmental conference: weekly departmental morbidity & mortality meetings are to be held on a secure teleconference facilitating interaction between attendings and residents. In addition to the main departmental conference, we would still run our weekly conferences in each subspecialty via teleconference (radiosurgery, neuro-oncology, skull base, pituitary, and neurovascular, among others).
-
9.Situational meetings: the leadership of the department (Chairman and Program Director) hosted a biweekly online meeting with the residents and faculty to review the following topics:
-
a.Evaluation of our action plan.
-
b.Provide further updates of the current situation in our hospital system and community.
-
c.Review the situation in the rest of the country.
-
d.Review our institutional guidelines.
-
e.Receive feedback from the residents and faculty in the frontline.
-
a.
Discussion
In the last 2 decades, several viruses with pandemic potential have affected the world. The most recent of these was the influenza A in the spring of 2009.17 Similar to the current SARS-CoV2 pandemic, the influenza A pandemic revealed the deficiencies and vulnerabilities of the health care system in a local and global scale.18 However, the social and economic impact of the current pandemic goes far beyond any other threat of this century, and is more comparable with the 1918 influenza pandemic.19
This extraordinary situation harbors several challenges, especially in those regions in which the outbreak has surpassed the capabilities of the health system. One of the major challenges is the lack of adequate testing both in identifying actively infected individuals (63% sensitivity in nasal swabs)20 and serologic testing that could identify those already immune. As a consequence, academic institutions have tried to adapt to ensure the safest work and training environment possible while providing high-quality care.
Contrary to many who can work from home, physicians have the responsibility of continuing to perform their duties while exposing themselves to the risk of contracting the virus. Resident physicians are the frontline workforce of the health care system. We believe that a temporary restructuring in the organization of a residency program should be strongly considered to protect the residents while continuing to provide medical care. Thus, the approach taken in our academic institution has focused in the resident safety and education.
The cancellation of the majority of our “elective” surgical schedule has dramatically decreased patient volume. We took advantage of this and performed a temporary restructuring of our clinical rotations. Having all of our residents working at the same time would only increase the risk of infections, compromising the number of residents available for overall coverage. For this reason, we decided to divide our group by half and have them work in alternating weeks.
Current Challenges
As any surgical specialty, neurosurgery training requires immersive surgical exposure. Inevitably, the current scenario will be detrimental to surgical training. To attempt overcome this, we instituted a series of lectures and conferences to support resident's education. Furthermore, faculty members have actively engaged with residents in several research projects.
Another challenge that is worthy to discuss is the potential repercussions that the current pandemic might have in the mental health of the residents and their families. Physicians are at greater risk of moral injury and developing mental health problems during the current pandemic.21, 22, 23 Moreover, specific situations such as the closing of schools have created an additional load to the residents who are parents and need to take a more demanding role in their children care and education. Also, some residents could be even facing economic crisis if their significant other cannot longer work due to the lockdown. For these and other reasons, residency programs should be proactive in taking actions to protect the mental health of their residents. Greenberg et al.22 outlined some key early interventions that could be taken amid the SARS-CoV2 outbreak: honest assessment of the situation, frequent discussions with the team based on Schwarz rounds (where the residents could share the challenges of caring for patients during these circumstances), routine support process with peer support program, and guidance from more senior faculties.
Support from the residency program should go far beyond. Once this current situation has started to improve, the academic program must take an active role in monitoring any potential sign of resident post-traumatic stress. For instance, our institution has a confidential peer-to-peer program that allows residents to seek mental health support for themselves and their family at no cost.
Future Challenges
A critical challenge to come in the near future will be how to return to a more “normal” schedule in the face the post-pandemic world. Active disease monitoring should continue, further actions might need to be taken to ensure safety, including a massive widespread testing program, contact tracing, and serologic evaluation. Nevertheless, some of the biggest challenges we might need to face in a near future will be in economics. Some reports estimate that U.S. economy will contract by 10%–25%.24 Traditionally, health care systems have been less affected from recessions; however, the current pandemic is changing this reality. The need for social distancing and the governmental mandates for the reduction of elective surgeries have decreased the revenues for the health care systems. For residents in the last year of training, this scenario could potentially harm their ability to get hired. For instance, as of March 21, 2020, the second largest source of unemployment insurance claims in the State of Michigan was from health care employees.24
Conclusions
The SARS-CoV2 pandemic constitutes a global health emergency full of uncertainty. Treatment, scope, duration, and economic burden forced a major restructuring of our medical practice. Daily research publications in high-impact medical journals have been a guiding force in determining the policies and medical management during this pandemic. In this regard, academic institutions must direct efforts to diminish further negative impact in the training and education of the upcoming generation of physicians including those currently in medical school. Perhaps the only silver lining in this terrible disruption will be greater appreciation of the role of current health care providers and educators, whose contributions to our society are often neglected or unrecognized.
CRediT authorship contribution statement
David T. Fernandes Cabral: Conceptualization, Data curation, Formal analysis, Methodology, Writing - original draft, Writing - review and editing. Nima Alan: Conceptualization, Methodology, Writing - review & editing, Writing - original draft. Nitin Agarwal: Conceptualization, Methodology, Writing - review & editing, Writing - original draft. Dade Lunsford: Conceptualization, Methodology, Writing - original draft, Writing - review & editing. Edward A. Monaco: Conceptualization, Methodology, Writing - review & editing, Writing - original draft.
Footnotes
Conflict of interest statement: Dr. L. Dade Lunsford, M.D., is an equity ownership for AB Elekta and DSMB InSightec.
References
- 1.Coronaviridae Study Group of the International Committee on Taxonomy of V. The species Severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol. 2020;5:536–544. doi: 10.1038/s41564-020-0695-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Arentz M., Yim E., Klaff L., et al. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington State. JAMA. 2020;323:1612–1614. doi: 10.1001/jama.2020.4326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang D., Hu B., Hu C., et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guan W.J., Ni Z.Y., Hu Y., et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;l382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Holshue M.L., DeBolt C., Lindquist S., et al. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382:929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Seah I., Su X., Lingam G. Revisiting the dangers of the coronavirus in the ophthalmology practice. Eye (Lond) 2020;34:1155–1157. doi: 10.1038/s41433-020-0790-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cook T.M., El-Boghdadly K., McGuire B., McNarry A.F., Patel A., Higgs A. Consensus guidelines for managing the airway in patients with COVID-19. Anaesthesia. 2020;75:785–799. doi: 10.1111/anae.15054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lie S.A., Wong S.W., Wong L.T., Wong T.G.L., Chong S.Y. Practical considerations for performing regional anesthesia: lessons learned from the COVID-19 pandemic. Can J Anaesth. 2020;67:885–892. doi: 10.1007/s12630-020-01637-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ficarra V., Novara G., Abrate A., et al. Urology practice during COVID-19 pandemic. Minerva Urol Nefrol. 2020;72:369–375. doi: 10.23736/S0393-2249.20.03846-1. [DOI] [PubMed] [Google Scholar]
- 10.Tao K.X., Zhang B.X., Zhang P., et al. [Recommendations for general surgery clinical practice in 2019 coronavirus disease situation] Zhonghua Wai Ke Za Zhi. 2020;58:170–177. doi: 10.3760/cma.j.issn.0529-5815.2020.03.003. [in Chinese] [DOI] [PubMed] [Google Scholar]
- 11.Meng L., Hua F., Bian Z. Coronavirus disease 2019 (COVID-19): emerging and future challenges for dental and oral medicine. J Dent Res. 2020;99:481–487. doi: 10.1177/0022034520914246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chang D., Xu H., Rebaza A., Sharma L., Dela Cruz C.S. Protecting health-care workers from subclinical coronavirus infection. Lancet Respir Med. 2020;8:e13. doi: 10.1016/S2213-2600(20)30066-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zou L., Ruan F., Huang M., et al. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020;382:1177–1179. doi: 10.1056/NEJMc2001737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Poston J.T., Patel B.K., Davis A.M. Management of critically ill adults with COVID-19. https://doi.org/10.1001/jama.2020.4914 [e-pub ahead of print]. JAMA. accessed March 31, 2020. [DOI] [PubMed]
- 15.Murthy S., Gomersall C.D., Fowler R.A. Care for critically ill patients with COVID-19. https://doi.org/10.1001/jama.2020.3633 [e-pub ahead of print]. JAMA. accessed March 31, 2020. [DOI] [PubMed]
- 16.Center for Disease Control and Prevention Healthcare supply of personal protective equipment; 2020, March 12. https://www.cdc.gov/coronavirus/2019-ncov/hcp/healthcare-supply-ppe-index.html Available at:
- 17.Writing Committee of the WHOCoCAoPI. Bautista E., Chotpitayasunondh T., et al. Clinical aspects of pandemic 2009 influenza A (H1N1) virus infection. N Engl J Med. 2010;362:1708–1719. doi: 10.1056/NEJMra1000449. [DOI] [PubMed] [Google Scholar]
- 18.Fineberg H.V. Pandemic preparedness and response—lessons from the H1N1 influenza of 2009. N Engl J Med. 2014;370:1335–1342. doi: 10.1056/NEJMra1208802. [DOI] [PubMed] [Google Scholar]
- 19.Morens D.M., Taubenberger J.K. Influenza cataclysm, 1918. N Engl J Med. 2018;379:2285–2287. doi: 10.1056/NEJMp1814447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang W., Xu Y., Gao R., et al. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA. 2020;323:1843–1844. doi: 10.1001/jama.2020.3786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen Q., Liang M., Li Y., et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7:e15–e16. doi: 10.1016/S2215-0366(20)30078-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Greenberg N., Docherty M., Gnanapragasam S., Wessely S. Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ. 2020;368:m1211. doi: 10.1136/bmj.m1211. [DOI] [PubMed] [Google Scholar]
- 23.Lai J., Ma S., Wang Y., et al. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw Open. 2020;3:e203976. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cutler D.P. How will COVID-19 affect the health care economy? JAMA Health Forum. 2020;323:2237–2238. doi: 10.1001/jama.2020.7308. [DOI] [PubMed] [Google Scholar]