Abstract
Introduction
The ongoing COVID-19 pandemic and the lockdown measures employed by the government have forced neurologists across the world to look upon telemedicine as the only feasible and practical option to continue providing health care towards children with epilepsy in home isolation. Children with epilepsy are challenging for teleconsultation as direct information from the patient is missing, regarding seizures and adverse effects, especially behavioral and psychological side effects.
Methods
Clinical and epilepsy-related details of telephonic consultations for children 1 month-18 years, performed between 26th March and 17th May 2020 in a tertiary care teaching hospital in Uttarakhand (a state of India known for hilly terrains with low per capita income) were recorded. Suitable changes in the dose/commercial brand of antiepileptic drug (AED) regimen were performed, along with the addition of new AED and referral to local practitioners for immediate hospitalization, when urgent health care issues were detected. Voice call, text message, picture/video message, and all other possible measures were employed to accumulate maximum clinical information in real-time.
Results
A total of 153 children(95 males [62 %], 9.45 ± 3.24 years, 140 lower/middle socioeconomic status) were enrolled after screening 237 children with various neurological disorders, whose caregivers contacted for teleconsultation. A total of 278 telephone consultations performed for these 153 children (1-5 telephone calls per patient). Hundred-thirteen children were identified to have a total of 152 significant clinical events (breakthrough seizure/uncontrolled epilepsy (108), AED related (13), and unrelated systemic adverse effects (24), worsening of associated co-morbidities (7). In rest of the patients, the query of the caregiver included unavailability of AED/prescribed commercial brand in the locality, query related to the dose of drugs, proxy for a scheduled routine visit (no active issues), and concern regarding COVID-19 related symptoms and effect of COVID-19 and lockdown in children with epilepsy. Ninety-three (60 %) patients required hiking up of AED dose, whereas 29 (17 %) patients required the addition of a new AED/commercial brand. Five children were advised immediate admission to a nearby hospital. Overall, 147 (96 %) caregivers were satisfied with the quality of medical advice.
Conclusion
Teleconsultation is one of the few feasible options with good effectiveness for providing medical advice to children with epilepsy during pandemic times.
Keywords: Teleconsultation, Epilepsy, COVID-19, Antiepileptic drugs, Child neurology
1. Introduction
The COVID-19 pandemic, which has currently engulfed most countries, has taught mankind unexpected lessons and forced to develop innovative ways to deal with this unprecedented havoc [1]. Only a few living persons have limited experience of dealing with such a huge pandemic, spreading like wildfire as the last worldwide influenza pandemic occurred nearly 100 years back. The SARS CoV-2 predominantly causes a respiratory illness, which culminates in severe pneumonia, acute respiratory distress syndrome (ARDS), and cytokine storm response and death in 5–10 % of affected patients [2]. Primary neurological illness including seizures, encephalitis, and stroke has only been shown in anecdotal case reports, but not proven in the larger epidemiological studies till now. But children with epilepsy are deprived of antiepileptic drugs (AEDs), health care advice, emergency consultation, and other supports at this challenging time because of lockdown implemented by governments of most countries [[2], [3], [4], [5], [6]]. As COVID-19 has been proven to be many times more infectious as compared to previous coronavirus epidemics, these lockdown measures implemented by the government are justified. But this has forced neurologists across the globe to explore innovative measures including telemedicine to continue providing quality care to patients with epilepsy. Telemedicine, which has been previously proven to be highly efficacious in various neurological disorders like stroke, epilepsy, and parkinsonism remains the most promising and practically the only feasible option to provide uninterrupted health care currently [[6], [7], [8], [9]]. Recently high-speed internet connectivity, availability of smartphones, and internet data at nominal prices, with the opportunity of video calling, free pictures, and video messages in various social media services have revolutionized the telecommunication sector in developing countries like India.
In March 2020, medical council of India (MCI) gave a nod to telemedicine practice by registered medical practitioners, spelled out guidelines for the same and made it a part of the Indian Medical Council (Professional Conduct, Etiquette and Ethics) Regulations, 2002. This guideline for the first time provided legal rights to registered medical practitioners to prescribe all drugs except those in schedule X category, narcotics or psychotropic substances. This guideline even allowed physicians to change or add new drugs to the previous treatment regimen. Most importantly this guideline came when COVID 19 pandemic has just started to engulf most parts of India and a nationwide lockdown was about to ensue, forcing physicians to move towards teleconsultation, with a drive never seen before. As a part of this guideline, a registered medical practitioner (RMP) can utilize any of the following telemedicine tools suitable for providing technology-based patient consultation (telephone, video, devices connected over the internet, WAN, LAN, landline or mobile phones, Chat Platforms like Facebook Messenger, WhatsApp, Mobile Apps, internet-based digital platforms for data transmission systems like Skype/ email/ fax) [10]. In the wake of such guidelines, a systematic study to explore the feasibility and efficacy of advanced telecommunication measures to provide an all-inclusive and precise teleconsultation for children with epilepsy is highly needed. The current study has been designed to fulfill this motive.
2. Methods
This prospective follow up study was carried out in the Pediatric Neurology Division, Department of Pediatrics, All India Institute of Medical Sciences, Rishikesh, during the COVID-19 lockdown period in India, over 52 days from 26th March 2020 to 17th May 2020. The study aimed to determine the feasibility and effectiveness of teleconsultation during a pandemic, using the new teleconsultation guidelines formulated in India, that allowed us to perform drug/dose modifications and all other activities which couldn’t be done previously. We attempted to determine whether a pediatric neurology specialist can answer queries raised by caregivers of children with epilepsy successfully, correctly identify and treat clinical problems in the patient. The study also intended to analyze the feasibility of changing the AED/hiking the dose of AED in children with uncontrolled or breakthrough seizures.
All the patients had previously been enrolled in the pediatric neurology specialty clinic, run exclusively by the two qualified pediatric neurologists for the last one year. They received all the telephone calls and text messages and provided the teleconsultations. All of the participants have been already evaluated as per the standard epilepsy management guidelines including magnetic resonance imaging (MRI) of the brain (3 T) with epilepsy protocol and video electroencephalogram (V-EEG). All of them were receiving antiepileptic drugs at the time of enrollment and had been assigned with the best possible clinical diagnosis including the electroclinical syndromes described by the International league against epilepsy (ILAE). The pediatric neurologist who had previously managed the child in a face-to-face visit only performed the teleconsultation, to avoid bias. In the absence of personal presence, explicit verbal consent over telephone call/text message was taken from caregivers for participation in the study. Ethical approval was taken from the institutional ethical committee. MOHFW/MCI guidelines regarding teleconsultation published in March 2020 were thoroughly adhered to during the study.
All consecutive children with epilepsy, aged 1 month to 18 years, of either sex, whose caregivers contacted any of the pediatric neurologists were enrolled in the study. Children with other neurological disorders with epilepsy as comorbidity were enrolled in the study only when their caregivers contacted for issues related to seizure or antiepileptic drugs. But caregivers of Children with epilepsy, if contacted for issues unrelated to epilepsy, then also they were included in the study. The children, whose caregivers contacted by text messages including short message services (SMS) or WhatsApp messages were also included in the study. Children, whose caregivers contacted for diseases other than epilepsy (migraine, neurodegenerative disorders, neuromuscular disorders, and metabolic disease, etc.), and queries unrelated to seizures, children, in whom inadequate clinical details could be obtained from the caregiver, despite the best effort and when a telephone call was disconnected before teleconsultation was complete and could not be connected afterward were excluded from the study.
All these caregivers have been previously provided (as a routine practice) with two specific mobile numbers during their previous face-to-face visits before COVID-19 pandemic, with advice to contact in case of any health care emergency or any difficulty in reaching for face-to-face visit arises. After obtaining verbal consent, demographic details of the child, information regarding the primary illness of the child (as much information as the caregivers could reveal, depending on their literacy), current concern for which they called the physician and current physical condition and status of epilepsy in the child were inquired and documented on a structured predesigned proforma. Any clinical problem including breakthrough seizure in a child with well-controlled epilepsy, persistence or uncontrolled seizure, antiepileptic drug-related adverse effects, unrelated systemic health care issues, or worsening of associated co-morbidities requiring any change in already prescribed medications was defined as a significant clinical event for the purpose of the study.
If the child had a breakthrough or uncontrolled seizure, then the pediatric neurologist, inquired for detailed information regarding epilepsy and antiepileptic drugs and asked the caregiver to send all previous documents bearing clinical details, neuroimaging, and EEG reports and prescribed medications to the investigators through picture message in WhatsApp. If any ambiguity was felt by the investigator regarding the physical condition of the child or seizure semiology than the caregivers were advised to send video records of child or seizure activity through WhatsApp video messages. After reviewing all these, the change in prescribed medication (hiking up the existing antiepileptic drug or addition of new antiepileptic drug) was conveyed to the caregiver through text message and also verbally, to avoid misinterpretation and ensure proper compliance. For the study, all these telephonic interactions on a single occasion were considered a single teleconsultation only.
In case a particular AED or prescribed commercial brand could not be obtained by the caregiver, due to logistic issues arising from lockdown measures, they were advised a suitable change in prescribed AED or commercial brand respectively, with the help of text messages and verbal advice. After obtaining the new AED/commercial brand, they were advised to send the image of the medicine strip or syrup by WhatsApp picture message to avoid any inadvertent medication error. All the adverse effects reported by caregivers, related or unrelated to epilepsy/AED were documented, graded according to Common Terminology Criteria for Adverse Events (CTCAE) grading system. Medications were added or changed when the adverse effect was grade 2 or beyond in severity. If the physician felt that the physical condition of the child needed immediate medical concern, or likely to worsen over the next few days, then they were advised only emergency interventions for stabilizing the child at home and to contact a competent pediatrician in vicinity subsequently at earliest possible. They were also advised to ask the local practitioner to contact in case of any specialized advice was required from a pediatric neurologist.
If the child had a significant clinical event than the caregiver was asked to provide clinical follow-up details, at a particular time on a particular day, by repeat telephone call. If the caregiver did not contact on that day than he was contacted telephonically the next day to ensure the child was doing well. Duration of teleconsultation, any technical glitches, network errors, and satisfaction of the caregiver (as denoted by the caregiver himself at the end of consultation) was also documented. If adequate clinical details of epilepsy were found to be missing after the teleconsultation than it was retrieved from the case records of that child maintained in the registry of the pediatric neurology clinic run by the department.
The teleconsultations performed in this study were not arranged follow-ups; rather they were more like providing the best possible medical advice during an emergency period. As the nationwide lockdown was imposed, most of our follow up patients could not reach us. Thus the only option left for our patients to get a specialty consultation was calling over the telephone.
2.1. Statistical analysis
Categorical variables were expressed in terms of frequency in percentage with a 95 % confidence interval. Continuous variables were expressed as mean and standard deviation or median with interquartile range. Whether data describing a particular parameter follows a normal distribution or not was decided by the Kolmogorov-Smirnov normality test. To determine whether the difference between the two variables was statistically significant, chi-square or Fisher’s exact test were used for categorical variables and the student’s t-test was used for continuous variables. For non-parametric variables, the Mann Whitney U test and Kruskal Wallis test were used as tests of statistical significance. SPSS version 24.0 was used to perform all these statistical analyses.
3. Results
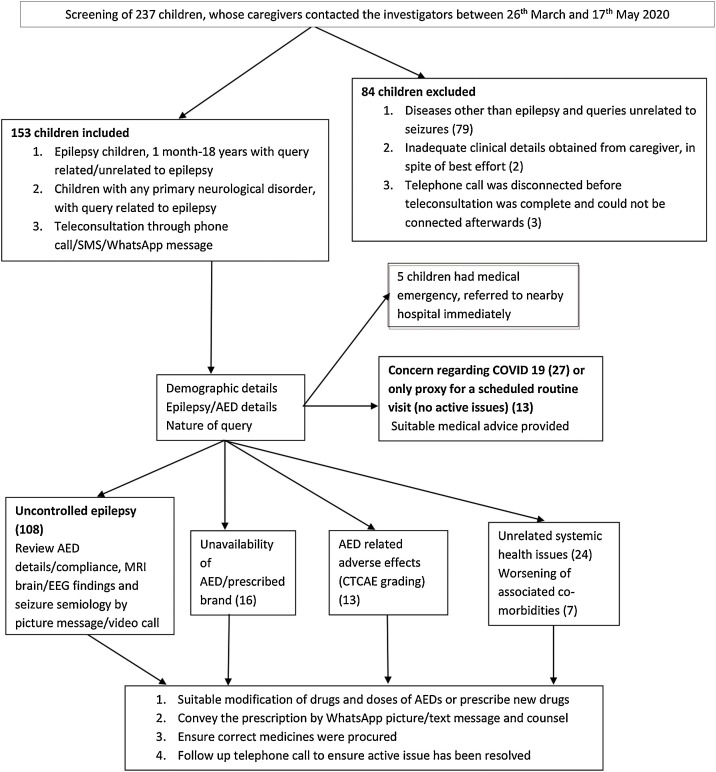
During the study period, caregivers of a total of 237 children suffering from various neurological disorders contacted the investigators, out of which 153 children were included. The total number of teleconsultations performed in these enrolled children was 278 (including the follow-up telephone calls, range-1−5 calls per patient). Hundred-thirteen children were found to have significant clinical events. Baseline demographic and clinical characteristics of the sample population have been described in Table 1 . Fig. 1 provides a brief overview of the study flow and results.
Table 1.
Baseline demographic and clinical variables of the sample population.
| Variable | Frequency (n = 153) | |
|---|---|---|
| Male | 95(62 %) | |
| Age (mean, SD)(in years) | 9.45 ± 3.24 | |
| Residency | Urban area | 48(31 %) |
| Rural area | 105(68 %) | |
| Socioeconomic status | Lower | 58(38 %) |
| Middle | 82(54 %) | |
| Higher | 13(8 %) | |
| Total number of telephone calls | 278 | |
| Number of telephone calls interrupted by network issues/technical glitches | 5(3.2 %) | |
| Number of telephone calls per patient (median, range) | 1 (1−5) | |
| Duration of telephone calls per patient (mean, SD) (minutes) | 7.64 ± 1.97 | |
| Caregiver satisfaction with teleconsultation | 147 (96 %) | |
Fig. 1.
Study flow.
Around 62 % (95) of enrolled children were boys, 68 % (105) resided in rural areas and most (140) children belonged to lower/middle socioeconomic status. Out of the 58 participants belonging to lower socioeconomic status, 19 caregivers were requested to supplement with picture messages of drugs, other clinical images, or video recording of paroxysmal events in children. Twelve caregivers were able to comply while the remaining seven caregivers did not have well-equipped smartphones to have a good quality video recording of seizures. Further clinical information through picture message/video recording could not be obtained in them and the treatment was prescribed based on the best possible clinical judgment of the investigator. However, no untoward events occurred in these seven children as determined on follow up telephone calls. Out of the 58 caregivers with lower socioeconomic status, 27 caregivers were unable to understand English prescriptions. For these children, Hindi was used as a second written language to communicate the medical advice through text messages in an understandable manner and sometimes help of a communicator; especially the persons working in pharmacy stores were employed. Most children (135 out of 153) resided in Uttarakhand, one of the most geographically and economically challenged state of India.
Around half of the children (79, 51 %) had a structural abnormality in the MRI brain, among which perinatal asphyxia, meningoencephalitis, traumatic brain injury, and neurocysticercosis were predominant etiologies. EEG was abnormal in 81 % (124)of children. Primary generalized epilepsy, juvenile myoclonic epilepsy, BCECTS, and Lennox Gastut syndrome were predominant electroclinical syndromes identified in the study population. The epilepsy characteristics, including neuroimaging, EEG findings, and details of antiepileptic drugs have been described in Table 2, Table 3 respectively.
Table 2.
The epilepsy characteristics, including neuroimaging and EEG findings of the sample population.
| Epilepsy variables | Number of participants (n = 153) | Children with uncontrolled seizure (n = 108) | Children with AED related adverse effects (n = 13) | Children with unrelated systemic adverse effects (n = 24) |
|---|---|---|---|---|
| Baseline seizure frequency (mean, SD) (per year) | 5.63 ± 1.78 | 4.67 ± 1.23 | 5.10 ± 1.48 | 4.13 ± 1.17 |
| Abnormal EEG | 124(81 %) | 105(97 %) | 8(61 %) | 18 (77 %) |
| Abnormal MRI brain | 79(51 %) | 71(65 %) | 3(23 %) | 13 (54 %) |
| Focal seizure | 82(53 %) | 63(58 %) | 7(53 %) | 12 (50 %) |
| Generalized seizure | 87(56 %) | 56(52 %) | 8(61 %) | 13(54 %) |
| Both generalized and focal seizure | 16(10.5 %) | 11(10 %) | 2(15 %) | 1(4 %) |
| Myoclonic seizure | 8(5.2 %) | 7(6.4 %) | 5(38 %) | 1(4 %) |
| Atonic seizure | 6(3.9 %) | 5(4.6 %) | 4(30 %) | 1(4 %) |
| Absence seizure | 3(2 %) | 1(1 %) | 0 | 0 |
| Perinatal hypoxia sequelae | 37(24 %) | 32(29 %) | 7(53 %) | 9(37 %) |
| Traumatic brain injury sequelae | 6(3.9 %) | 4(3.7 %) | 0 | 0 |
| Meningoencephalitis sequelae | 13(8.4 %) | 11(10 %) | 2(15 %) | 2(8 %) |
| Neurocysticercosis | 28(18.3 %) | 15(13.8 %) | 0 | 0 |
| Focal cortical dysplasia | 5(3.2 %) | 5(4.6 %) | 0 | 0 |
| Lennox Gastaut syndrome | 14(9.1 %) | 13(12 %) | 4(30 %) | 4 (16 %) |
| West syndrome | 2(1.3 %) | 2(1.8 %) | 0 | 0 |
| BCECTS | 17(11 %) | 7(6.4 %) | 0 | 0 |
| Early/late onset childhood occipital epilepsy | 5(3.2 %) | 3(2.7 %) | 0 | 0 |
| Primary generalized epilepsy | 16(10.4 %) | 10(9.2 %) | 0 | 0 |
| Childhood/Juvenile absence epilepsy | 3(2 %) | 1(1 %) | 0 | 0 |
| Juvenile myoclonic epilepsy | 7(4.5 %) | 5(4.6 %) | 0 | 0 |
Table 3.
The use of various antiepileptic drugs in the sample population.
| Variables | Number of participants (n = 153) | Children with uncontrolled seizure (n = 108) | Children with AED related adverse effects (n = 13) | Children with unrelated systemic adverse effects (n = 24) |
|---|---|---|---|---|
| Number of AEDs (mean, SD) | 1.93 ± 0.82 | 2.32 ± 0.71 | 2.86 ± 0.89 | 2.01 ± 0.87 |
| Number of patients on 1 AED | 105(68 %) | 67(62 %) | 0 | 16 (67 %) |
| Number of patients on 2 AEDs | 32(21 %) | 27(25 %) | 6(46 %) | 4(16 %) |
| Number of patients on 3 AEDs | 13(8.4 %) | 11(10 %) | 5(38 %) | 3(12 %) |
| Number of patients on 4 AEDs | 3(2 %) | 3(2.7 %) | 2(15 %) | 1(4 %) |
| Phenytoin | 37(24 %) | 29(26.8 %) | 11(84 %) | 8(33 %) |
| Valproate | 72(47 %) | 58(53.7 %) | 2(15 %) | 12(50 %) |
| Levetiracetam | 51(33 %) | 37(34.2 %) | 0 | 9(37 %) |
| Benzodiazepine | 25(16.3 %) | 16(14.8 %) | 12(92 %) | 2(8 %) |
| Oxcarbazepine | 20(13 %) | 13(12 %) | 9(69 %) | 4(16 %) |
| Topiramate | 6(4 %) | 5(4.6 %) | 1(7.6 %) | 1(4 %) |
| Zonisamide | 3(2 %) | 3(2.7 %) | 0 | 1(4 %) |
| Lamotrigine | 4(2.6 %) | 3(2.7 %) | 0 | 0 |
| Lacosamide | 2(1.3 %) | 2(1.8 %) | 0 | 0 |
Details of the telephone calls/text messages received have been described in Table 4 . A total of 152 significant clinical events were identified during telephonic consultation in 113 children. Ninty two children with previously well-controlled epilepsy had at least one breakthrough seizure, 16 children had uncontrolled epilepsy on previously prescribed medications, 13 children had AED related adverse effects, 24 children had unrelated systemic complaints and 7 children had worsening of associated co-morbidities. Four out of these seven children had cerebral palsy and were found to have increased spasticity. The rest of the three children had worsening of preexisting hyperactivity and disruptive behavior.
Table 4.
Distribution of variables related to the nature of telephonic consultation and caregiver queries.
| Variable | Number of participants (n = 153) |
|---|---|
| Contacted by telephone call | 141(92 %) |
| Required follow-up telephone calls/text messages | 64(42 %) |
| Contacted by text message only | 12(7.8 %) |
| Telephone calls were supplemented by picture messages | 83(54 %) |
| Telephone calls were supplemented by video messages | 14(9.1 %) |
| Detected to have significant clinical events | 113 (74 %) |
| Advised immediate hospitalization in a nearby hospital | 5(3.2 %) |
| Merely asking for information (no active issues) | 38(25 %) |
| Grade 1 adverse effects | 8(5.2 %) |
| Adverse effects grade 2 and beyond in severity | 29(19 %) |
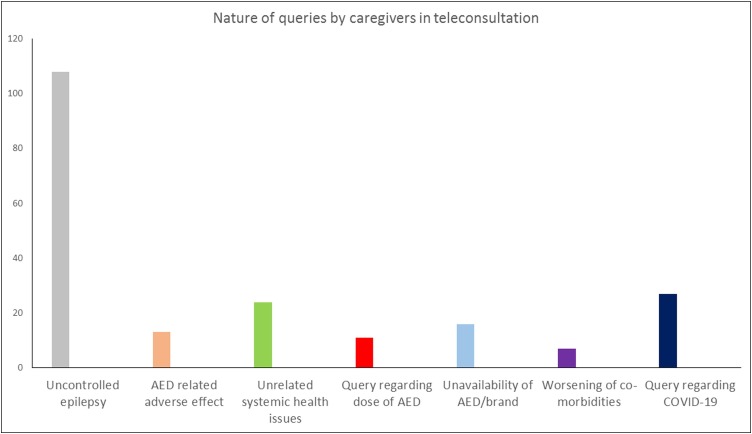
Caregivers of the remaining 40 children contacted for issues related to the availability of drugs (5), commercial brands (11), or doubt regarding the dose of AEDs (11). A significant proportion of caregivers (41, 26 %) contacted merely to inquire regarding COVID-19 symptoms and whether their child is at increased risk of COVID-19. Only a small number of caregivers (12, 7 %) contacted solely as a proxy for their scheduled visits, which was missed due to lockdown without any active health care issues. Fig. 2 describes the nature of queries raised by caregivers.
Fig. 2.
Nature of the queries raised by the caregivers.
A total of 29(17 %) children required modification of the AED dose, commercial brand, and sometimes altogether the drug, for reasons including unavailability of the drug, adverse effects, and uncontrolled epilepsy. On follow up telephonic inquiry none of them had any medication errors and active issues were resolved in all of them after changing medications. Details of children who required modification of AEDs/their doses have been described in Table 5 .
Table 5.
Description of children who required modification of antiepileptic drugs or their doses.
| Variable | Number of participants (n = 153) |
|---|---|
| Required hiking up of antiepileptic drugs | 93(60 %) |
| Required addition of new antiepileptic drug due to uncontrolled seizure | 15(9.8 %) |
| Required reduction of an antiepileptic drug due to adverse effects | 9(5.8 %) |
| Required replacement of antiepileptic drug due to adverse effects | 4(2.6 %) |
| Required replacement of antiepileptic drug due to unavailability in the locality | 5(3.2 %) |
| Required replacement of prescribed commercial brand due to unavailability in the locality | 11(7.1 %) |
Only 5 patients were identified to have clinical issues requiring immediate hospitalization and they were referred to local practitioners. All of them were found to be stabilized on subsequent telephonic inquiry, a week after the previous. Out of the total 278 telephone calls of average 7 min duration, only 5 calls were interrupted by technical glitches/network error and 147 (96 %)caregivers were satisfied with medical advice provided over the telephone, as expressed by them at the end of the telephone call.
Children with perinatal asphyxia or meningoencephalitis sequelae i.e. children with cerebral palsy, compared to those without had more prevalence of breakthrough/uncontrolled seizure (43/50, 86 %) vs. (65/103, 63 %),(p = 0.04) and adverse effects (9/50, 18 %) vs (4/103, 4%)(p = 0.005).
Although there was no statistically significant difference between the children on different antiepileptic drugs on the prevalence of breakthrough seizure, but children on phenytoin (11), benzodiazepine (12), and oxcarbazepine (9) were more likely to have adverse effects (p = 0.01) (Table 5). Excessive sleepiness (7) and behavioral abnormalities (4) were the most common AED related adverse effects.
4. Discussion
The current study is the first clinical study after the recently proposed MCI guidelines to implement all possible telecommunication measures successfully to prescribe, modify AEDs, and treat adverse effects in children with epilepsy by pediatric neurologists over the telephone. Atypical seizure semiologies and complex electroclinical epilepsy syndromes, as well as adverse effects of variable severity, were recognized by the investigators with excellent accuracy and precise medical advice was provided without any untoward events and medication errors. Previous clinical studies exploring teleconsultation in epilepsy depended almost entirely on traditional telephone calls and text messages, included mainly adult population and enrolled preferably stable children with epilepsy, who only needed continuation of previous prescription [8,9]. Few recent studies have employed innovative methods like smartphone-based applications, epilepsy nursing workers (ENW), and epilepsy helplines.
Recently in 2019, Patterson et al. have developed an algorithm based on 50 routinely asked questions to determine whether a paroxysmal event was epileptic or not. The algorithm used pre-test odds for having epilepsy, a probability score based on response to questions in the algorithm, and finally a posttest probability score. Subsequently, they converted it into a smartphone-based application, which was found to be more useful than other paper-based, electronic, or online web-based platforms [9,11].
It was later validated by Rajbhandari et al. for use by non-physician health workers and inexperienced doctors. This freely available Epilepsy Diagnosis Aid app was found to have comparable results with face-to-face consultation (gold standard). The authors believed that all the essential components in the so-called “AIDARP” public health approach towards epilepsy including awareness, identification, diagnosis, AEDS and education, review, and prevention can be performed through teleconsultation [12,13].
Elger et al. have described the challenges in shifting from traditional to innovative teleconsultation approach for epilepsy recently. The former only includes telephone reports on the recurrence of seizure, its semiology, current physical and mental status of the patient. But a more holistic approach towards children with epilepsy requires more technology-enriched information including the telephonic transmission of EEG and videos showing seizures, information gathered in automatic seizure detection devices, and home monitoring of blood levels of AEDs [14]. Similar results were also shown by other studies [[15], [16], [17], [18], [19], [20]].
Innovations in telemedicine in neurological disorders have speeded up with the COVID-19 pandemic [21]. American Academy of Neurology in the time being has released a document named “Telemedicine and Remote Care Implementation Guide” (American Academy of Neurology web seminar on telemedicine and COVID-19 infections), mentioning the proper coding elements neurologists should follow during this pandemic for teleconsultation. American epilepsy society has also recently released various guidelines on telehealth during COVID-19 pandemic and webinars on how to put these guidelines into clinical practice and overcoming various obstacles. The recently launched COVID-19 Telehealth Program intends to provide funding worth $200 million, sanctioned by American Congress as part of the “Coronavirus Aid, Relief, and Economic Security (CARES) Act”, to help clinicians in providing telehealth services to patients in their homes. This program will fully fund all expenditures regarding telecommunications and information services, and devices necessary to provide telehealth services to eligible health care providers in the USA. It is high time for the Indian Government to implement such health care programs for physicians practicing in our country [7,22,23].
Till recently the available technical tools in developing countries do not have sufficiently satisfactory performance in high rate data transfer uninterruptedly for months together required for these applications and hence it was difficult to implement in routine clinical service in most parts of India, except metro cities. In villages and remote, hilly places, the major hindrance in applying these technologies was the slow, inconsistent speed of internet connectivity and lack of smartphones with residents.
Moreover, very few trained neurologists and radiologists well versed in EEG and MRI brain reporting respectively are available currently in India, predominantly in an urban area. Although MRI images can be successfully transferred over a distance telemetrically, tele-EEG transportation is still out of reach for most places. Installation of expensive equipment for the same can be justified as it will reduce the cost of travel and stay for a large number of patients in a rural area. The government health sector will also be benefitted because of overall fewer requirements of manpower and infrastructure [24]. In developed countries, on the other hand, often concern arises regarding security and privacy of medical and personal data and legal repercussions in case the advice goes wrong.
But the recent technological revolution with easy availability of flexible audio and video online chatting platforms like Zoom, Skype, Webex (CISCO), WhatsApp, Live class, Go-to-meeting, Go-towebinar, High-five, Hangouts, Viber has helped clinicians in overcoming the previously mentioned logistic difficulties. Similarly with the introduction of fourth-generation (4 G) broadband cellular network technology and advanced facility smartphones, the dream of high speed (up to 50–100 MBPS) transmission of digital voice, data, and video signals in India has also become a reality [25]. All these were key contributing factors behind the success of the current study in a geographically and economically challenged area of India.
Because of these recent developments, telemedicine for children with epilepsy can now be expected to reach the vicinity of children belonging to lower socioeconomic status residing in resource-constrained settings like India. Poor internet speed, inadequate technological knowledge related to lack of proper formal education in caregivers, availability of only a few numbers of super-specialty units, lack of emergency medical care facilities in nearby localities in suburban and rural areas, traditional, social and cultural diversities, plenty of false beliefs and superstitions, lack of motivation, unsolicited reliance on traditional medicinal systems and more than 10 lakh fake practitioners in the country pose several challenges in making teleconsultation successful. However, in recent years belief and motivation of Indian people have changed, making the current study successful in the wake of the COVID-19 pandemic in India. As teleconsultation has already been implemented for long in most of the apex health care institutions in developed countries with the help of advanced video conferencing systems, we consider the results of this study can be at least generalized to developed countries and most of the developing countries with a progressive attitude towards the modern medicinal system.
ILAE task force on COVID-19 has also recommended that telemedicine for epilepsy is a user-friendly tool, non-inferior to face-to-face visit in terms of detection of seizure, AED compliance, and reduction of hospitalization, emergency room visits. ILAE also particularly stressed on implementing teleconsultation during COVID-19 times to reduce face-to-face visit at hospital and emergency room visits, which is recommended nowadays. Most of the doubts and clinical issues of children with epilepsy can be sorted out and patients can also be counseled properly over telephone calls, as demonstrated in previous studies. The follow-up visits for children with epilepsy rarely require a detailed physical examination and mostly revolves around adherence to AED regimen, breakthrough seizure, EEG, and serum AED levels, making teleconsultation an attractive option for them [26].
The current study is first of its kind to explore the advanced telemedicine technologies successfully in children with epilepsy during the COVID-19 pandemic, especially in a geographically challenging region like Uttarakhand, where the lockdown has further impaired already difficult transportation of patients.
5. Conclusion
Teleconsultation is one of the few feasible options with good effectiveness for providing medical advice to children with epilepsy during pandemic times. Moreover, the antiepileptic drugs and their doses can be safely changed over telephonic review if neurology specialists are available, unlike the traditional belief of implementing telephonic consultation only for stable patients. Since it might be the only feasible option to cater to quality health care to children with epilepsy all over the country, clinicians and public health officials need to work in this direction to make its widespread use.
Transparency document
References
- 1.Caso V., Federico A. No lockdown for neurological diseases during COVID19 pandemic infection. Neurol Sci. 2020:1–3. doi: 10.1007/s10072-020-04389-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Matías-Guiu J., Porta-Etessam J., Lopez-Valdes E., Garcia-Morales I., Guerrero-Solá A., Matias-Guiu J.A. Management of neurological care during the COVID-19 pandemic. Neurol Engl Ed. 2020 doi: 10.1016/j.nrleng.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Panda P.K., Sharawat I.K. COVID-19 (SARS-CoV-2 infection) and children: pediatric neurologist’s perspective. Indian J Pediatr. 2020 doi: 10.1007/s12098-020-03326-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sethi N.K. EEG during the COVID-19 pandemic: what remains the same and what is different. Clin Neurophysiol. 2020;131:1462. doi: 10.1016/j.clinph.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Poyiadji N., Shahin G., Noujaim D., Stone M., Patel S., Griffith B. COVID-19-associated acute hemorrhagic necrotizing encephalopathy: CT and MRI features. Radiology. 2020 doi: 10.1148/radiol.2020201187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brigo F., Bonavita S., Leocani L., Tedeschi G., Lavorgna L., Digital Technologies, Web and Social Media Study Group of the Italian Society of Neurology Telemedicine and the challenge of epilepsy management at the time of COVID-19 pandemico. Epilepsy Behav EB. 2020 doi: 10.1016/j.yebeh.2020.107164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hatcher-Martin J.M., Adams J.L., Anderson E.R., Bove R., Burrus T.M., Chehrenama M., et al. Telemedicine in neurology: telemedicine work group of the american academy of neurology update. Neurology. 2020;94:30–38. doi: 10.1212/WNL.0000000000008708. [DOI] [PubMed] [Google Scholar]
- 8.Kissani N., Lengané Y.T.M., Patterson V., Mesraoua B., Dawn E., Ozkara C., et al. Telemedicine in epilepsy: how can we improve care, teaching, and awareness? Epilepsy Behav EB. 2020;103 doi: 10.1016/j.yebeh.2019.106854. [DOI] [PubMed] [Google Scholar]
- 9.Patterson V. Managing epilepsy by telemedicine in resource-poor settings. Front Public Health. 2019;7:321. doi: 10.3389/fpubh.2019.00321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Telemedicine Practice Guidelines. https://www.mohfw.gov.in/pdf/Telemedicine.
- 11.Patterson V. Telemedicine for epilepsy support in resource-poor settings. Front Public Health. 2014;2:120. doi: 10.3389/fpubh.2014.00120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rajbhandari H., Joshi S., Malakar S., Paudel P., Jain P., Uppadaya K., et al. Epilepsy field workers, a smartphone application and telephone telemedicine: safe and effective epilepsy care in rural Nepal. Seizure. 2019;64:54–58. doi: 10.1016/j.seizure.2018.12.005. [DOI] [PubMed] [Google Scholar]
- 13.Haddad N., Grant I., Eswaran H. Telemedicine for patients with epilepsy: a pilot experience. Epilepsy Behav EB. 2015;44:1–4. doi: 10.1016/j.yebeh.2014.11.033. [DOI] [PubMed] [Google Scholar]
- 14.Elger C.E., Burr W. Advances in telecommunications concerning epilepsy. Epilepsia. 2000;(41 Suppl 5):S9–12. doi: 10.1111/j.1528-1157.2000.tb06041.x. [DOI] [PubMed] [Google Scholar]
- 15.Ahmed S.N., Mann C., Sinclair D.B., Heino A., Iskiw B., Quigley D., et al. Feasibility of epilepsy follow-up care through telemedicine: a pilot study on the patient’s perspective. Epilepsia. 2008;49:573–585. doi: 10.1111/j.1528-1167.2007.01464.x. [DOI] [PubMed] [Google Scholar]
- 16.Bahrani K., Singh M.B., Bhatia R., Prasad K., Vibha D., Shukla G., et al. Telephonic review for outpatients with epilepsy-A prospective randomized, parallel group study. Seizure. 2017;53:55–61. doi: 10.1016/j.seizure.2017.11.003. [DOI] [PubMed] [Google Scholar]
- 17.Konanki R., Gulati S., Prasad K., Saini L., Pandey R.M., Paul V.K. Comparison of telephone with face to face consultation for follow up of Neurocysticercosis. Epilepsy Res. 2018;145:110–115. doi: 10.1016/j.eplepsyres.2018.06.005. [DOI] [PubMed] [Google Scholar]
- 18.Gulati S., Jauhari P., M SN, Panda P.K., Jossy M., Chakrabarty B., et al. ICNC 2018; 2018. Telephone Based Follow-Up of Children with Epilepsy Aged 4 Months To 18yrs: Comparison of Accuracy Between a Specialty Nurse and a DM Pediatric Neurology Fellow to identify Critical Clinical Events Requiring Face-to -Face Evaluation. [Google Scholar]
- 19.Santos-Peyret A., Durón R.M., Sebastián-Díaz M.A., Crail-Meléndez D., Goméz-Ventura S., Briceño-González E., et al. E-health tools to overcome the gap in epilepsy care before, during and after COVID-19 pandemics. Rev Neurol. 2020;70:323–328. doi: 10.33588/rn.7009.2020173. [DOI] [PubMed] [Google Scholar]
- 20.Hernando-Requejo V., Huertas-González N., Lapeña-Motilva J., Ogando-Durán G. The epilepsy unit during the COVID-19 epidemic: the role of telemedicine and the effects of confinement on patients with epilepsy. Neurol Barc Spain. 2020 doi: 10.1016/j.nrl.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kuroda N. Epilepsy and COVID-19: associations and important considerations. Epilepsy Behav EB. 2020;108 doi: 10.1016/j.yebeh.2020.107122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.COVID-19 | delivery of care. Am Epilepsy Soc. 2020 https://www.aesnet.org/about_aes/position_statements/covid-19/delivery-of-care nrodriguez@aesnet.org. (Accessed May 21, 2020) [Google Scholar]
- 23.Ask the expert webinar series. Am Epilepsy Soc. 2016 https://www.aesnet.org/professional_education/ask-the-expert-webinar kkramer@aesnet.org. (Accessed May 21 2020) [Google Scholar]
- 24.Kappal R., Mehndiratta A., Anandaraj P., Tsanas A. Current impact, future prospects and implications of mobile healthcare in India. Cent Asian J Glob Health. 2014;3:116. doi: 10.5195/cajgh.2014.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dheer A., Chaturvedi R.K. Embracing a revolution - telemedicine. Med J Armed Forces India. 2005;61:51–56. doi: 10.1016/S0377-1237(05)80121-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.2020. COVID-19 and epilepsy // international league against epilepsy. n.d. https://www.ilae.org/patient-care/covid-19-and-epilepsy (Accessed May 22 2020) [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.