To the Editor: During the COVID-19 pandemic, proper use of personal protective equipment has played an important role in protecting frontline health care workers from infection.1 Because of temperature differences between the inner and outer surfaces of goggles, moist, warm exhaled air escaping from respirators can condense into tiny water droplets on the inner surface. This obscures visibility and impairs workflow. In our previous research, we showed the effectiveness of hydrogel patches in reducing facial pressure injuries caused by N95 respirators.2 Thereafter, we conducted a prospective, self-controlled study to evaluate the efficacy of hydrogel patches as an antifog measure.
This study was approved by the Medical Ethics Committee of Huazhong University of Science and Technology (no. [2020]0131-1). Twenty health care workers aged 25 to 55 years took part in 2 separate experiments, conducted at a temperature of 64.4°F to 77°F. In both experiments, the right, inner side of the goggles was treated with an antifog agent, and the left side remained untreated. In the first experiment, participants wore only goggles and an N95 respirator. The left, untreated side was the control. In the second experiment, participants wore goggles and hydrogel patches, which were placed in a “W” shape under the upper edges of the N95 respirator (Fig 1 ). Before starting, the respirator seal was checked for air leaks (Supplemental Materials; available via Mendeley at https://doi.org/10.17632/rbrw7zvp6y.2).3 At hourly intervals, participants and a clinician scored the fogging observed on each side of the goggles by using the Subject Self-Assessment Fogging Score (SSAFS) and Clinician Assessment Fogging Score (CAFS), respectively (Supplemental Materials; available via Mendeley at https://doi.org/10.17632/rbrw7zvp6y.2). Statistical analysis was performed with SPSS 26.0 (IBM, Armonk, NY) using a paired-sample t test (P < .05).
Fig 1.
Study flowchart.
A total of 19 participants (14 [73.7%] female) were included. At 1 hour, the mean score for goggles with hydrogel patches was lower than control individuals (SSAFS: 3.29 ± 2.80 vs 5.35 ± 2.47; P < .01; CAFS: 1.91 ± 1.35 vs 4.35 ± 2.06; P < .001). Hydrogel patches plus antifog agent resulted in lower scores than just antifog agent (SSAFS: 1.82 ± 1.88 vs 2.41 ± 2.81; P < .05; CAFS: 0.91 ± 0.71 vs 1.62 ± 0.78; P < .01). This difference persisted at 2, 3, and 4 hours. There was no statistically significant difference between hydrogel and antifog agent scores at 1, 3, and 4 hours, except at 2 hours by the SSAFS (Fig 2 ). Twelve (63.2%) participants without hydrogel patches reported mild air leaks from the N95 respirator versus only 3 (15.8%) with hydrogel patches. Participants did not report skin irritation with hydrogel patches. The main reasons reported by participants for reluctance to use antifog agents were difficulty in even application, long drying times, and concerns about viral contamination of goggles during processing.
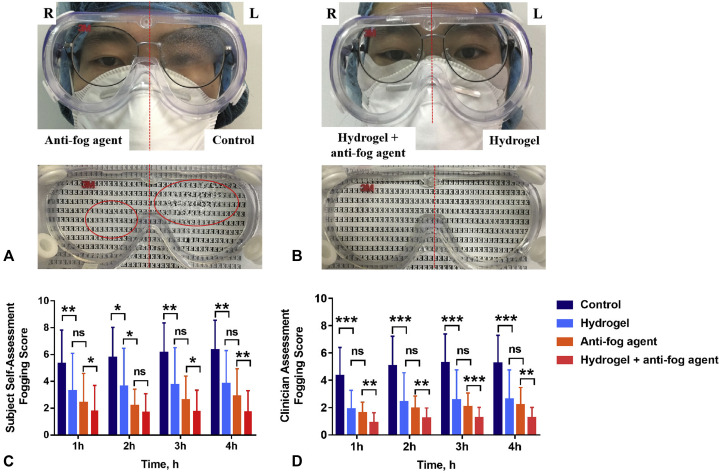
Fig 2.
Photographs after wearing the goggles for 4 hours and fogging scores plotted with respect to time. A, Without hydrogel patches: the left side of the goggles is the blank control; the right side is treated with an antifog agent. The fogged goggles are placed on a lettered background, and red circles show the extent of fogging. B, With hydrogel patches: the left side is untreated; the right side is treated with an antifog agent. C, Graphs plotted to show the SSAFS for both experiments after every hour. D, The CAFS for both experiments after every hour. ∗P < .05, ∗∗P < .01, ∗∗∗P < .001. CAFS, Clinician Assessment Fogging Score; ns, not statistically significant; SSAFS, Subject Self-Assessment Fogging Score.
This study suggests that hydrogel patches are a useful adjunct to respirators; they enable a tighter fit of the respirators, are well tolerated, and prevent facial pressure injuries. The efficacy of these patches is similar to commercially available antifog agents, and they provide better antifogging results when used in combination with the latter.
Study limitations included the unblinded design and possible confounders between the 2 experiments, such as amount of speech, activities performed, and environmental humidity. A larger, controlled, and blinded study is warranted to further verify these findings.
Footnotes
Drs Zhou and Suo contributed equally to this article.
Funding sources: Supported by Huazhong University of Science and TechnologyCOVID-19 Rapid Response Call Program (2020kfyXGYJ056 and 2020kfyXGYJ081) and Hubei Provincial Emergency Science and Technology Program for COVID-19 (2020FCA037).
Conflicts of interest: None disclosed.
IRB approval status: Reviewed and approved by Medical Ethics Committee of Huazhong University of Science and Technology (approval no. [2020]0131-1).
Reprints not available from the authors.
References
- 1.Gupta M.K., Lipner S.R. Personal protective equipment recommendations based on COVID-19 route of transmission. J Am Acad Dermatol. 2020;83:e45–e46. doi: 10.1016/j.jaad.2020.04.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dong L., Yang L., Li Y., et al. Efficacy of hydrogel patches in preventing facial skin damage caused by mask compression in fighting against coronavirus disease-2019: a short-term, self-controlled study. J Eur Acad Dermatol Venereol. 2020 doi: 10.1111/jdv.16638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ortega R., Gonzalez M., Nozari A., Canelli R. Personal protective equipment and Covid-19. N Engl J Med. 2020;382:e105. doi: 10.1056/NEJMvcm2014809. [DOI] [PubMed] [Google Scholar]