Abstract
Background:
Femoroacetabular impingement (FAI), particularly cam-type, is now well accepted as a risk factor for the development of hip osteoarthritis (OA). However, many hips with FAI morphology will never develop hip pain or OA, identifying that our current understanding of FAI disease progression remains limited. The purposes of this retrospective case-control study were to (1) report the patient and disease characteristics of patients with rapidly progressive FAI requiring hip arthroplasty by the age of 40 and (2) to identify patient and imaging factors associated with rapidly progressive FAI.
Methods:
Cases were retrospectively identified from an arthroplasty registry as patients 40 years old or younger with underlying FAI deformity and end stage OA requiring primary total hip arthroplasty. Patients were excluded for known DDH, AVN, SCFE, inflammatory arthritis, and previous ipsilateral surgery. Controls were identified from a hip preservation database as patients with symptomatic FAI undergoing surgical intervention over the same time period, and were matched 2:1 by gender and age. Alpha angles were calculated on frog-leg lateral and anteroposterior (AP) radiographs with both inclusion and exclusion of any osteophytic prominences (representing minimum and maximal possible underlying FAI morphology). Patient characteristics, radiographic parameters, and baseline patient reported outcomes were compared between the two groups using student’s t-tests.
Results:
The rapidly progressive FAI cohort of 31 patients had a mean age of 35.8 years at surgery and was 39% female and 61% male. Alpha angles were significantly larger compared to controls when osteophytes were included (Frog: 74.7±10.8 vs. 57.2±12.7°, p<0.001; AP: 91.7±10.7 vs. 61.2±19.4°, p<0.001), but not when osteophytes were excluded (Frog: 61.2±11.1 vs. 57.2±12.7°, p=0.15; AP: 64.9±17.1 vs. 61.3±19.4°, p=0.38). Except for UCLA activity score, all baseline outcome measures were significantly lower for rapidly progressive FAI cases (p<0.001 for all).
Conclusions:
When compared to controls with symptomatic FAI, rapidly progressive cases did not demonstrate major differences in cam deformity magnitude. Thus severity of bony deformity may only be one aspect of a multifactorial etiology of hip OA progression in FAI.
Level of Evidence: III
Keywords: hip osteoarthritis, hip arthroscopy, femoroacetabular impingement
Introduction
Femoroacetabular impingement (FAI), particularly cam-type, is increasingly recognized as one of the two most common causes of hip osteoarthritis (OA), as well as pain in the pre-arthritic state secondary to labral and cartilage pathology. However, our understanding of the role of various factors in the pathophysiology of FAI remains limited with significant gaps in knowledge. Several studies have documented a high prevalence of FAI in asymptomatic patients,1,2 with a higher frequency of deformity in populations of athletes (66% with cam, 51% pincer, 57% mixed) compared to purely asymptomatic individuals (22% cam, 55% pincer, 8% mixed).3 Thus many, and perhaps most hips with FAI morphology will never develop hip pain or OA. In a systematic review comparing these patient populations when symptomatic, Mascarenhas et al. found that athletes and non-athletes had a similar prevalence of cam deformity.3 However, cam deformities in symptomatic non-athletes were significantly larger compared to athletes (mean alpha angle 67 vs. 56°, respectively), suggesting deformity severity may play a role in symptom generation and disease progression.
The association of the cam-type FAI deformity with the development of OA is supported by several population-based studies.4-10 In a prospective cohort study of over 1,400 symptomatic hips without clear preexisting osteoarthritis, patients with moderate and severe cam deformity (AP alpha angle >60° and 83°, respectively) more commonly developed incident and end stage arthritis.4 However, while FAI appears to be a risk factor for OA, only 7% of patients (mean age 55.9 years) developed OA during the 5 year study period, highlighting that our understanding of the determinants of FAI disease progression remains relatively limited. While some patients with radiographic evidence of early OA and coexistent FAI deformity rapidly progress to end-stage OA at a young age, others with similar deformity have demonstrated lack of significant disease progression at 10 years of follow up.11,12 It remains unclear which patients with symptomatic FAI deformity are at greatest risk to develop OA that rapidly progresses, whether severity of bony deformity is the predominant driver of disease, and what other patient factors contribute to disease progression.
The purpose of the current study was (1) to describe a cohort of patients 40 years of age and younger with end-stage OA attributed to underlying FAI and (2) to identify patient characteristics associated with rapidly progressive FAI, by comparing them to age matched controls with symptomatic FAI (without radiographic evidence of advanced OA).
Methods
We performed a retrospective case-control study approved by our institutional IRB (# 201704064). Cases were identified using our institution’s arthroplasty registry, which at the time of our search contained records for 8,318 hip arthroplasties in 6,642 patients at our institution (Figure 1). Amongst these cases, the senior author performed 413 primary total hip replacements in patients less than or equal to 40 years old with end-stage OA during a 10-year period (August 2006 -July 2016). Exclusion criteria were then applied in order to remove patients with underlying etiologies other than FAI leading to their OA (hip dysplasia with lateral center edge angle <20°, avascular necrosis, posttraumatic arthritis, slipped capital femoral epiphysis, Legg-Calve-Perthes Disease, inflammatory arthritides, and previous ipsilateral surgeries). A total of 55 potential cases remained after exclusion and underwent radiographic review for evidence of FAI and to confirm no evidence of any exclusionary criteria/conditions. A total of 24 additional hips were excluded because of radiographic evidence of previously listed conditions. This included three additional hips with acetabular protrusio (two female, one males; age 19-24 years) that were excluded due to the focus on the current study on cam-type FAI. An alpha angle of 50° was utilized a cutoff for cam-type FAI, after exclusion of any other associated causes. The final cohort included 31 cases that were identified as having both end-stage OA and FAI deformities, a cohort we will refer to as having “rapidly progressive FAI.”
Figure 1.
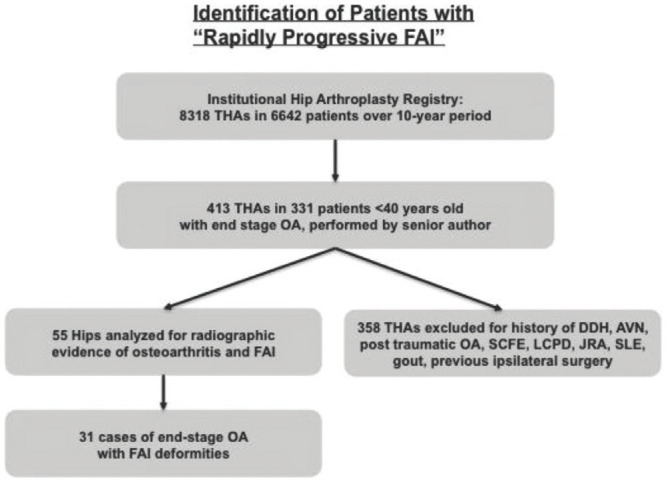
Case Identification. Cases were identified from our arthroplasty registry over a 10-year period. THA = total hip arthroplasty, DDH =developmental dysplasia of the hip, AVN = avascular necrosis, OA = osteoarthritis, SCFE = slipped capital femoral epiphysis, LCPD = Legg–Calvé–Perthes disease, JRA = Juvenile rheumatoid arthritis, SLE= Systemic Lupus Erythematosus, FAI= Femoroacetabular impingement
Controls were identified from an institutional hip preservation database. Patients were considered for inclusion if they had symptomatic cam-type FAI (cam or combined type) and had elected to undergo hip preservation surgery over the same 10-year period as the cases of primary THA. Hip preservation surgery was performed arthroscopically or with an open surgical hip dislocation and included femoral osteoplasty and/or acetabular rim trimming, chondroplasty, and labral repair or debridement as indicated on a case-by-case basis. The same aforementioned exclusion criteria were applied to this population, with the additional criterion that patients did not have radiographic evidence of osteoarthritis (Tonnis OA Grade >2). A total of 710 hips remained for potential inclusion, and controls were randomly selected in a 2:1 fashion by matching sex and age at time of surgery (±2 years). Body Mass Index (BMI) and alpha angle were not matched so that this variable could be compared between cases and controls to identify a potential role in pathophysiology of OA. A total of 62 controls were identified and similarly underwent radiographic review to confirm absence of the aforementioned exclusionary conditions.
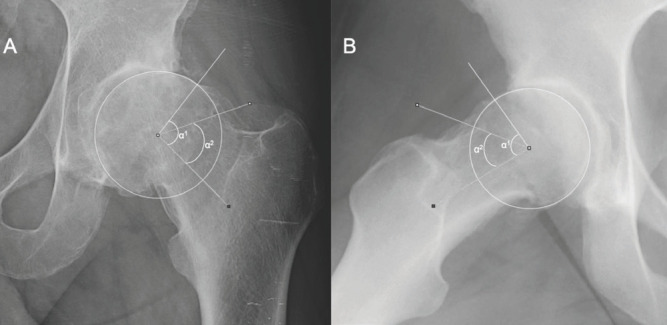
One reader analyzed AP pelvis and frog lateral radiographs for all cases and controls. The intraobserver and interobserver reliability of radiographic analysis including the alpha angle has been previously demonstrated by our group13 with intraobserver/ interobserver intraclass correlation coefficients (ICC) of 0.76/0.21 for alpha angle measurements on frog leg lateral radiographs and 0.88/0.64 for lateral center edge angle measurements on AP radiographs.14 Cam FAI morphology severity was characterized utilizing the alpha angle. Alpha angles were measured on both frog-leg lateral and AP radiographs15 to assess the magnitude of both anterior and more lateral deformities. With the presence of osteophytes, osteoarthritis can influence the presence and appearance of FAI deformities by increasing the alpha angle in some cases. In order to account for this, alpha angles were calculated with both inclusion and exclusion of any osteophytes (reactive cam) (Figure 2). Thus the maximum alpha angle represents the maximal potential FAI severity (if no osteophytic component is actually present), while the minimum alpha angle represents the minimum potential FAI severity (if an osteophytic presence is accounting for the prominence). Of note, frog leg lateral radiographs were not available for two cases. As such, these patients and their matched controls were excluded from analysis of frog leg lateral alpha angles.
Figure 2.
Alpha Angle Calculations.
A. AP radiograph depicting alpha angle calculation including (alpha 1= alpha maximum) and excluding the osteophyte (alpha 2 = alpha minimum).
B. Frog leg lateral radiograph in a different patient similarly depicting alpha angle calculation including (alpha 1 = alpha maximum) and excluding (alpha 2 = alpha minimum) the osteophyte.
*Alpha angle measurements excluding osteophytes were made using the sclerotic outline of the femoral neck.
Co-existing pincer FAI morphology severity was characterized utilizing the lateral center edge angles (LCEA).15 While LCEA may also be affected by underlying OA, differentiation of potential osteophytes is less clear so no attempt at differentiation was performed. The presence of a crossover sign was not assessed given the difficulty in assessing this parameter in the presence of OA, as well as the limited associated with osteoarthritis and prevalence of this finding in normal hips.16
Patient characteristics and baseline patient reported outcomes were compared between the two groups, comparing preoperative UCLA,17 modified Harris Hip score,18 WOMAC pain, stiffness, and physical function scores.19 Two cases did not have documented preoperative clinical outcome measures, and were removed from average calculations along with their matched controls. Two-tailed T-tests used for statistical comparisons for radiographic and clinical scoring measures (p-value ≤ 0.05)
Results
The rapidly progressive FAI cohort of 31 patients was 39% female and 61% male. The mean age of this group at time of surgery was 35.8 years (range 22-40; 29% ages 20-25, 35.5% ages 25-30, 13% ages 30-35, 22.5% ages 35-40). The average male and female age at time of surgery was 36.3 and 34.2 years, respectively. The mean minimum alpha angle (with exclusion of possible osteophytes) on frog lateral radiographs was 61.2±11.1° and maximum alpha angle (with inclusion of possible osteophytes) was 74.7±10.8°. When comparing male and female cases, males had larger maximum values (minimum: 62.8°vs. 58.7°, p= 0.34; maximum: 78.3° vs. 68.9°, p =0.02). The mean minimum alpha angle (with exclusion of possible osteophytes) on AP radiographs was 64.9±17.1° and maximum alpha angle (with inclusion of possible osteophytes) was 91.7±10.7° (Table 1). The measured alpha angles on AP radiographs were significantly larger in males at both the minimum and maximum values (minimum: 70.6°, vs. 56.0°, p=0.02; maximum 96.1°, vs. 84.8°, p < 0.01). The presence of possible osteophytes resulted in at least a 5-degree increase in alpha angle on frog leg lateral and AP radiographs in 76% and 79% of cases, respectively. Overall, 72% of patients had a frog leg lateral alpha angle greater than 55° with osteophytes excluded, and 93% when included.
Table 1.
Alpha Angles, Cases vs. Controls
| Cases: Minimum Alpha Angle | Cases: Maximum Alpha Angle | FAI Controls | |
|---|---|---|---|
| Frog Leg Lateral Alpha Angle (deg) | 61.2±11.1 | 74.7±10.8* | 52.7±12.7 |
| AP Alpha Angle (deg) | 64.9±17.1 | 91.7±10.7* | 61.3±19.4 |
| Percentage with Mild Frog Cam Deformity (50-55 deg) | 27.6 | 6.9 | 48.3 |
| Percentage with Moderate Frog Cam Deformity (55-63 deg) | 41.4 | 3.4 | 17.2 |
| Percentage with Severe Frog Cam Deformity (63 deg) | 31 | 89.7 | 34.5 |
Comparisons of alpha angles between cases and controls were significantly different when osteophytes were included in the measurements, but not when excluded (p-value ≤ 0.05).
Additionally, the mean LCEA in cases was 30.4±11.0°. 26% (8/31) of patients had a lateral center edge angle greater than 40°. In hips with LCEA less than 40°, 74% had native alpha angles >55° on frog leg lateral radiographs.
On radiographic analysis, alpha angles on frog leg lateral radiographs were significantly larger compared to controls when osteophytes were included (p<0.001) but not when excluded (p=0.15) (Table 1). Likewise, alpha angles on AP radiographs were significantly larger compared to controls when osteophytes were included (p<0.001) but not when excluded (p=0.38). In total, 84% and 29% of rapidly progressive FAI cases had a severe cam deformity (alpha angle greater than 63°) on frog leg lateral radiographs with osteophytes included and excluded, respectively. In comparison, 34% of FAI controls had a severe cam deformity. Additionally, mean LCEAs were similar in rapidly progressive FAI cases and controls (30.4±11.0°vs. 27.8±6.2°, p=0.15), although 26% vs. 3% of patients had abnormal measures (greater than 40°) in rapidly progressive FAI and FAI controls, respectively.
Patients with rapidly progressive FAI (OA cases) had a greater mean BMI compared to FAI controls (non-OA) (29.8 vs. 26.5, p=0.02). Overall, 39% (12/31) and 22% (7/31) of cases had a BMI greater than 30 and 35, respectively, compared to 21 and 5% from controls. Additionally, the clinical outcome measures for the rapidly progressive FAI cases demonstrated significantly greater symptoms compared to FAI controls for all but one measure. The UCLA values were similar (6.6±2.7, 7.0±2.6; p=0.43) between cases and controls. However, patients in rapidly progressive FAI cohort demonstrated lower Modified Harris Hip scores (50.5±14.3 vs. 63.7±14.2; p<0.001), WOMAC-pain scores (41.3±19.6 vs.66.5±19.8; p<0.001), WOMAC-stiffness scores (37.1+15.0 vs. 59.5+23.9, p<0.001), and WOMAC-physical function scores (46.0±18.3 vs. 69.9±19.0, p<0.001).
Discussion
This study reports the characteristics of a patient population with end-stage OA due to apparent underlying FAI in patients 40 years old and younger. This population had slightly more males (61%) than females, a distribution similar to that reported in the average population presenting with symptomatic impingement (57% male).20 Surprisingly many hips with end-stage OA had relatively mild cam deformities (after exclusion of osteophytes). Additionally, in patients with native frog leg lateral alpha angles (without osteophytic inclusion) less than 55°, only 25% (2/8) had an LCEA greater than 40°, highlighting that some patients progressed to end-stage arthritis without large magnitude cam or pincer deformities. Lastly, after exclusion of osteophytes, the alpha angles of cases and controls did not differ. This finding underscores the role of other potential factors, including obesity, in the pathophysiology of FAI progression.
Our study has several weaknesses including its retrospective assessment at a single time point. The retrospective nature of the study is inherent for the rare outcome and ability to acquire a meaningful cohort of patients with this condition. The retrospective nature of the study made more detailed assessment of range of motion, participation in athletics, and femoral version not possible. Cases and controls in the current study were assessed at a single age-matched time-point. This allows for assessment of the patient and radiographic characteristics of hips at a single time point in the disease process and thus allows comparison between a more aggressive and less aggressive FAI time course. Additionally, while FAI was attributed as the cause of OA after exclusion of other potential causes, the retrospective nature of the study limits any ability to precisely attribute FAI as the true cause of OA, rather than just a coexisting morphology. For cases, most importantly this means the presence and severity of FAI are assessed in the presence of end-stage OA. Through the radiographic analysis in the current study, the influence of osteophytes on measurements was minimized. Longitudinal population-based studies that follow patients over time would be ideal for characterization of deformity prior to the development of OA, but are impractical in the current study focus given the resources required and rare outcome. Additionally, the assessment of patient characteristics at a single time point within a case-control study also has limitations. For example, BMI was assessed in cases in the presence of end-stage OA without the ability to define if BMI was potentially confounded by hip pain for several years prior to undergoing surgery. Thus we demonstrate the association of BMI with hip OA but fail to establish any causal relationship.
The present work also compares two points of the spectrum of FAI presentations, comparing similarly aged cases of severe OA requiring arthroplasty to symptomatic controls amenable to hip preservation surgery. The goal of this comparison was to potentially identify factors associated with rapid progression in order to better understand the pathophysiology of FAI in this subset of patients. It is currently not well understood what relative role FAI deformity severity and patient characteristics play in the development of OA. The current study demonstrates that radiographic deformity alone does not explain rapid progression. In fact, most FAI hips progressing to OA have fairly mild to moderate deformities (69% of cases when osteophytes were excluded). When excluding osteophytes from the alpha angle evaluation, there was no measurable difference between the size of cam deformities between cases and controls. Similarly, cases and controls had similar percentages of patients with severe cam deformity, defined by alpha angles greater than 63°. Additionally, no difference in the presence of pincer-type global overcoverage defined as a LCEA greater than 40° was present between cases and controls.21 Although cases had significantly larger cam deformity with inclusion of osteophytes, it is possible that these deformities were not the original stimulus for the degenerative cascade, and were not responsible for the earlier stages of disease progression. The radiographic analysis utilized in the study helps to estimate the range of true underlying deformity in the setting OA through a best case and worst case approach (with exclusion or inclusion of possible osteophytes). Even when possible osteophytes are included, many hips with apparent mild FAI deformities have progressed to OA at a very young age. It is however important to consider the limitations of our limited radiographic analysis. As our understanding of key determinants of outcomes in hip preservation surgery has improved,22 there has been a better appreciation for the impact of detailed three-dimensional anatomy including femoral and acetabular version on impingement.23 Three-dimensional low-dose CT is increasingly utilized for preoperative assessment and may someday be replaced by three-dimensional MRI reconstructions of bony anatomy.24,25 In the current study, given the retrospective nature, it was not feasible to have three-dimensional CT data in the current population, but factors including femoral version may indeed play an important role.
Although FAI has been well established as a risk factor for the onset of osteoarthritis,4-10 our findings illustrate that the rate and risk of arthritic progression cannot be explained by the magnitude of cam deformity alone. Our results are supported by several studies documenting populations of patients with radiographic FAI deformity that fail to progress to end-stage arthritis.11,12 In a single center study of patients younger than 55 who had undergone unilateral THA, Wyles et al. retrospectively evaluated the radiographs of the contralateral hips of 172 patients. Only hips with baseline Tonnis Grade 0 scoring and at least 10 year of radiographic follow up were analyzed. In this population, 74 patients were identified to have FAI, compared to 48 with dysplasia and 40 with normal morphology. The authors found that hips with both normal morphology or FAI (without concomitant DDH) progressed similarly as evaluated with Tonnis grading.11 Although the authors did not quantify alpha angles or the magnitude of cam deformities, their work importantly demonstrates not all FAI deformities destine a hip for rapid onset of end stage OA. Similarly, Bardakos et al. analyzed 43 hips with “pistol -grip” deformities and Tonnis grade 1 or 2, comparing AP radiographs 10 years apart and demonstrated 65% of patients demonstrated progression of OA. OA Progression was associated with the presence of a posterior wall sign (39% vs. 7%, p=0.02) and lower medial proximal femoral angle (81° vs. 87°, p=0.004), but not alpha angle magnitude.12
Collectively, these findings support that cam deformities are a single component of a complex, multifactorial explanation for rapidly progressive FAI. The determinates of disease progression likely involve several factors, including obesity, activity history,26 genetic/biologic predispositions,27 and other bony abnormalities such as femoral and acetabular version that contribute to FAI. In the current study, we demonstrate higher BMI and prevalence of obesity in cases, compared to controls. However, a higher BMI may be partially confounded by the development of OA and the greater morbidity associated with this and its effects of general health. In the current study, no difference in UCLA activity score was seen between case and controls at the time of surgical intervention. Future studies would be useful to characterize activity level at a younger age and involvement in competitive athletics. Overall, the current study emphasizes the strong effect these often overlooked factors may have on the pathophysiology of FAI. This is additionally supported by the number of asymptomatic hips with FAI morphology that will never develop hip pain or OA.
References
- 1.Frank JM, Harris JD, Erickson BJ, Slikker W, Bush-Joseph CA, Salata MJ, et al. Prevalence of Femoroacetabular Impingement Imaging Findings in Asymptomatic Volunteers: A Systematic Review. Arthroscopy. 2015;31(6):1199–204. doi: 10.1016/j.arthro.2014.11.042. [DOI] [PubMed] [Google Scholar]
- 2.Nardo L, Parimi N, Liu F, Lee S, Jungmann PM, Nevitt MC, et al. Femoroacetabular Impingement: Prevalent and Often Asymptomatic in Older Men: The Osteoporotic Fractures in Men Study. Clin Orthop Relat Res. 2015;473(8):2578–86. doi: 10.1007/s11999-015-4222-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mascarenhas VV, Rego P, Dantas P, Morais F, McWilliams J, Collado D, et al. Imaging prevalence of femoroacetabular impingement in symptomatic patients, athletes, and asymptomatic individuals: A systematic review. Eur J Radiol. 2016;85(1):73–95. doi: 10.1016/j.ejrad.2015.10.016. [DOI] [PubMed] [Google Scholar]
- 4.Agricola R, Heijboer MP, Bierma-Zeinstra SM, Verhaar JA, Weinans H, Waarsing JH. Cam impingement causes osteoarthritis of the hip: a nationwide prospective cohort study (CHECK). Ann Rheum Dis. 2013;72(6):918–23. doi: 10.1136/annrheumdis-2012-201643. [DOI] [PubMed] [Google Scholar]
- 5.Agricola R, Waarsing JH, Arden NK, Carr AJ, Bierma-Zeinstra SM, Thomas GE, et al. Cam impingement of the hip: a risk factor for hip osteoarthritis. Nat Rev Rheumatol. 2013;9(10):630–4. doi: 10.1038/nrrheum.2013.114. [DOI] [PubMed] [Google Scholar]
- 6.Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87(7):1012–8. doi: 10.1302/0301-620X.87B7.15203. [DOI] [PubMed] [Google Scholar]
- 7.Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–20. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 8.Kowalczuk M, Yeung M, Simunovic N, Ayeni OR. Does Femoroacetabular Impingement Contribute to the Development of Hip Osteoarthritis? A Systematic Review. Sports Med Arthrosc. 2015;23(4):174–9. doi: 10.1097/JSA.0000000000000091. [DOI] [PubMed] [Google Scholar]
- 9.Zebala LP, Schoenecker PL, Clohisy JC. Anterior femoroacetabular impingement: a diverse disease with evolving treatment options. Iowa Orthop J. 2007;27:71–81. [PMC free article] [PubMed] [Google Scholar]
- 10.Gosvig KK, Jacobsen S, Sonne-Holm S, Palm H, Troelsen A. Prevalence of malformations of the hip joint and their relationship to sex, groin pain, and risk of osteoarthritis: a population-based survey. J Bone Joint Surg Am. 2010;92(5):1162–9. doi: 10.2106/JBJS.H.01674. [DOI] [PubMed] [Google Scholar]
- 11.Wyles CC, Heidenreich MJ, Jeng J, Larson DR, Trousdale RT, Sierra RJ. The John Charnley Award: Redefining the Natural History of Osteoarthritis in Patients With Hip Dysplasia and Impingement. Clin Orthop Relat Res. 2017;475(2):336–50. doi: 10.1007/s11999-016-4815-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bardakos NV, Villar RN. Predictors of progression of osteoarthritis in femoroacetabular impingement: a radiological study with a minimum of ten years follow-up. J Bone Joint Surg Br. 2009;91(2):162–9. doi: 10.1302/0301-620X.91B2.21137. [DOI] [PubMed] [Google Scholar]
- 13.Nepple JJ, Martell JM, Kim YJ, Zaltz I, Millis MB, Podeszwa DA, et al. Interobserver and intraobserver reliability of the radiographic analysis of femoroacetabular impingement and dysplasia using computer-assisted measurements. Am J Sports Med. 2014;42(10):2393–401. doi: 10.1177/0363546514542797. [DOI] [PubMed] [Google Scholar]
- 14.Carlisle JC, Zebala LP, Shia DS, Hunt D, Morgan PM, Prather H, et al. Reliability of various observers in determining common radiographic parameters of adult hip structural anatomy. Iowa Orthop J. 2011;31:52–8. [PMC free article] [PubMed] [Google Scholar]
- 15.Clohisy JC, Carlisle JC, Beaule PE, Kim YJ, Trousdale RT, Sierra RJ, et al. A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am. 2008;90(Suppl 4):47–66. doi: 10.2106/JBJS.H.00756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Larson CM, Moreau-Gaudry A, Kelly BT, Byrd JW, Tonetti J, Lavallee S, et al. Are normal hips being labeled as pathologic? A CT-based method for defining normal acetabular coverage. Clin Orthop Relat Res. 2015;473(4):1247–54. doi: 10.1007/s11999-014-4055-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Naal FD, Impellizzeri FM, Leunig M. Which is the best activity rating scale for patients undergoing total joint arthroplasty? Clin Orthop Relat Res. 2009;467(4):958–65. doi: 10.1007/s11999-008-0358-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Soderman P, Malchau H. Is the Harris hip score system useful to study the outcome of total hip replacement? Clin Orthop Relat Res. 2001;384:189–97. doi: 10.1097/00003086-200103000-00022. [DOI] [PubMed] [Google Scholar]
- 19.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15(12):1833–40. [PubMed] [Google Scholar]
- 20.Clohisy JC, Knaus ER, Hunt DM, Lesher JM, Harris-Hayes M, Prather H. Clinical presentation of patients with symptomatic anterior hip impingement. Clin Orthop Relat Res. 2009;467(3):638–44. doi: 10.1007/s11999-008-0680-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nepple JJ, Prather H, Trousdale RT, Clohisy JC, Beaule PE, Glyn-Jones S, et al. Diagnostic imaging of femoroacetabular impingement. J Am Acad Orthop Surg. 2013;21(Suppl 1):S20–6. doi: 10.5435/JAAOS-21-07-S20. [DOI] [PubMed] [Google Scholar]
- 22.Degen RM, Pan TJ, Chang B, Mehta N, Chamberlin PD, Ranawat AS, et al. Risk of failure of primary hip arthroscopy-a population-based study. J Hip Preserv Surg. 2017;4(3):214–23. doi: 10.1093/jhps/hnx018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lerch TD, Boschung A, Todorski IAS, Steppacher SD, Schmaranzer F, Zheng G, et al. Femoroacetabular Impingement Patients With Decreased Femoral Version Have Different Impingement Locations and Intra- and Extraarticular Anterior Sub-spine FAI on 3D-CT-Based Impingement Simulation: Implications for Hip Arthroscopy. Am J Sports Med. 2019;47(13):3120–32. doi: 10.1177/0363546519873666. [DOI] [PubMed] [Google Scholar]
- 24.Atkins PR, Shin Y, Agrawal P, Elhabian SY, Whitaker RT, Weiss JA, et al. Which Two-dimensional Radiographic Measurements of Cam Femoroacetabular Impingement Best Describe the Three-dimensional Shape of the Proximal Femur? Clin Orthop Relat Res. 2019;477(1):242–53. doi: 10.1097/CORR.0000000000000462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lerch TD, Siegfried M, Schmaranzer F, Leibold CS, Zurmuhle CA, Hanke MS, et al. Location of Intra- and Extra-articular Hip Impingement Is Different in Patients With Pincer-Type and Mixed-Type Femoroacetabular Impingement Due to Acetabular Retroversion or Protrusio Acetabuli on 3D CT-Based Impingement Simulation. Am J Sports Med. 2020. p. 363546519897273. [DOI] [PubMed]
- 26.Packer JD, Safran MR. The etiology of primary femoroacetabular impingement: genetics or acquired deformity? J Hip Preserv Surg. 2015;2(3):249–57. doi: 10.1093/jhps/hnv046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pollard TC, Villar RN, Norton MR, Fern ED, Williams MR, Murray DW, et al. Genetic influences in the aetiology of femoroacetabular impingement: a sibling study. J Bone Joint Surg Br. 2010;92(2):209–16. doi: 10.1302/0301-620X.92B2.22850. [DOI] [PubMed] [Google Scholar]


