Abstract
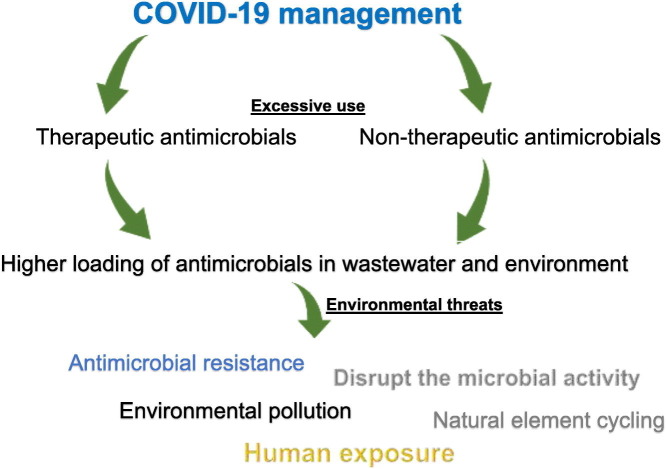
Use of antimicrobials in the treatment and prevention of COVID-19, caused by novel coronavirus SARS-CoV-2, is on the rise. The increased use of antimicrobials can have serious consequences on the environment. Antibiotics have had a reasonable role in bacterial co-infections with regards to the management of COVID-19. However, recent evidences suggest that there has been injudicious prescription of antimicrobials. Moreover, a large number of people are self-medicating with antibiotics in a misguided attempt to protect themselves from the virus. This practice is especially prevalent in developing communities. Although common soaps are effective at inactivating enveloped viruses, such as the SARS-CoV-2, use of antibacterial products bearing biocides has increased during this pandemic. Current wastewater treatment techniques are unable to offer complete elimination of antibacterial biocides. These compounds can then accumulate in different environmental compartments thus, disrupting the functioning of native microbes. These microbes are involved in the biogeochemical cycling of elements and environmental remediation. In addition, the presence of antimicrobial elements in the environment can stimulate antimicrobial resistance. Concrete actions are needed to address this issue. Development of an antimicrobial policy specific for COVID-19 is urgently needed. Investments into improving wastewater infrastructure as well as public awareness is crucial. Moreover, global monitoring programs and multidisciplinary collaborations are required to understand the environmental impact of this pandemics.
Keywords: COVID-19, Antibiotics in environment, Antibacterial soaps, Antimicrobial resistance (AMR), Wastewater contamination
Graphical abstract
Highlights
-
•
COVID-19 is caused by novel coronavirus SARS-CoV-2.
-
•
Injudicious use of antimicrobials is rising in COVID-19 treatment and prevention.
-
•
Increased loading of antimicrobials would affect the environment.
-
•
Investments are called in wastewater infrastructure and public awareness.
1. Introduction
The ongoing global pandemic of coronavirus disease 2019 (named as COVID-19) is today's most significant health concern. This disease was first reported in Wuhan, China in December 2019. On January 30th, 2020 the World Health Organization (WHO) declared this outbreak a Public Health Emergency of International Concern and on March 11th, 2020 it was characterized as a “pandemic”. As of June 30, 2020, this pandemic has infected >10 millions of people and caused >0.5 million deaths. There is a global urgency to develop vaccines to prevent infection and create treatments for this disease. As a response to this pandemic there has been rapid adaptation of infection control and antimicrobial stewardship programs.
Use of antibiotics in the treatment and prevention of COVID-19 is rising (Rawson et al., 2020a) despite it being a viral disease (caused by a novel coronavirus—SARS-CoV-2). Therefore, researchers have become increasingly concerned about the in-clinic impacts of COVID-19 on overall levels of antimicrobial resistance (AMR) (Hsu, 2020).
It is well recognized that excessive use of antimicrobials in medicine and agriculture drives AMR which is a global threat to human, animal and environmental health (Maillard et al., 2020). According to the US Center for Disease Prevention and Control (2019), up to 50% of antibiotic use is not medically justified. This situation is particularly worse in developing communities which have unregulated over-the-counter sales and a weak water and sewage infrastructure. For example, a recent typhoid fever outbreak in Pakistan has been associated to the antibiotic resistance caused by inappropriate use of drugs as well as poor sanitation and contaminated water supplies (Cohen, 2018). Recent estimates by UN Interagency Coordination Group on Antimicrobial Resistance (2019) suggest that AMR diseases are responsible for about 700,000 annual deaths worldwide. Without concrete action, the death toll could reach up to 10 million a year by 2050.
The intent of this communication is to highlight the consequences of COVID-19 management on the environment. The focus will be on the unnecessary use of antibacterial drugs and personal hygiene products in the treatment and prevention of COVID-19. A brief description of these issues is provided below.
2. Excessive use of therapeutic antimicrobials
Antibiotics have reasonable roles in the management of COVID-19 particularly to treat suspected or confirmed bacterial co-infections (Rawson et al., 2020a). The World Health Organization has advised that antibiotics should not be used for the purposes of treating COVID-19 except in the presence of bacterial co-infections (WHO, 2020). However, growing evidence suggests that very high proportion of COVID-19 patients are being unnecessarily treated with antibiotics. Empirical antibiotics were prescribed for 90% of patients despite low confirmation of secondary bacterial infections (<10%) (Lai et al., 2020). Wei et al. (2020) also noted that antibiotics were started on admission in 59% of COVID-19 patients despite the absence of definitive evidence of bacterial coinfection in these patients. Moreover, 98% of these prescriptions were empiric. Similarly, another very recent review of data from covid-19 cases, mostly from Asia, reported that >70% of patients received antimicrobial treatment despite only <10% having bacterial or fungal coinfections (Rawson et al., 2020a). Moreover, the same study found that broad spectrum antibiotics, intended to kill a wide range of bacteria, are being administered. Overuse of these antibiotics can stimulate AMR in the acute care settings (Hsu, 2020; Rawson et al., 2020b). Premature hype surrounding possible treatments for COVID-19 could also spike the prescription of antibiotics. This has been seen for the antibiotic azithromycin in combination with the drug hydroxychloroquine causing shortages in the US (Reardon, 2020). Though unmeasured, there is a possibility of a large number of people taking antibiotics in misguided attempts to self-medicate to protect themselves from the virus. This has the potential to be very prevalent in developing communities where antibiotics can be easily obtained without a prescription. A high proportion of these drugs in bioactive forms is excreted into the wastewater from where they may enter in natural systems (Slater et al., 2011).
Release of antibiotic resistant bacteria along with large quantities of antibiotics to the wastewater would spur the AMR and other unintended consequences on the environment. A recent review detailing pharmaceutical pollutants in global aquatic systems found antibiotics as the most-frequently detected compounds (Patel et al., 2019). It should be noted that wastewater is the major hotspot for AMR as it is characterized by extremely high bacterial loads coupled with subtherapeutic antibiotics (Berendonk et al., 2015).
3. Excessive use of non-therapeutic antimicrobials
Proper hand hygiene has been recognized as the first line of defense against this pandemic. Therefore, frequent hand-washing with plain soap and water for at least 20 s has been advised as an impactful way to prevent the spread of COVID-19 (WHO, 2020). Soaps contain surfactants that dissolve the lipid-bilayer, an integral part of SARS-CoV-2 envelop, leading to the deactivation of virus. These deactivated viral molecules are then encapsulated within micelles which are then washed away (Chaudhary et al., 2020). A 20-second wash provides sufficient time for the soap molecules to dissolve the lipid-bilayer of the SARS-CoV-2 virus.
All regular soaps available in the marketplace have the basic ingredients and chemistry required to disrupt the virus (Chaudhary et al., 2020). Common soaps are effective at inactivating the enveloped viruses such as the SARS-CoV-2 therefore, antibacterial soaps are not required (UNESCO, 2020). The US-Food and Drug Administration (FDA) has also advocated the same and moved to ban 19 antimicrobial chemicals from soaps acknowledging their dangerous impacts (McNamara and Levy, 2016). Despite this, use of antibacterial soaps and disinfectants has increased during this pandemic as evident from sharp increase in their sale worldwide (Cleaning Matters, 2020). Similar increase in demand for antibacterial products/soaps was noted in the era of 2009 Swine flu (Hickman, 2009; Slater et al., 2011).
Antibacterial products contain high amounts of biocides which result in a sharp increase in their presence in wastewater. As a matter of fact, antimicrobial chemicals from soaps could occur in wastewater biosolids (that are land applied as soil conditioners) at multiple orders of magnitude higher than the concentrations of antibiotics (McClellan and Halden, 2010). This may pose severe risks to ecosystem and to the spread of AMR in the environment. In addition to the AMR, persistence of these biocides in the environment is a major environmental threat that calls for suitable remediation (McNamara and Levy, 2016). Moreover, presence of these biocides can sabotage the wastewater treatment processes that rely on microbial activity (McNamara et al., 2014). These compounds may enter into soil system disrupting the functioning of native biota playing crucial roles in biogeochemical cycling of elements and environmental remediation (Patel et al., 2019).
4. Concluding remarks and recommendations
Antibiotic stewardship principles should continue to be applied and promoted in the times of COVID-19 (Huttner et al., 2020). However, development of an antimicrobial policy specific for COVID-19 is urgently needed. For this, coordinated strategies at the individual, health-care and policy levels are essential (Rawson et al., 2020b).
Since current wastewater treatment techniques are unable to offer complete elimination of these compounds (Kümmerer et al., 2018; Rodriguez-Mozaz et al., 2020), our daily exposure to various antibiotics, biocides and their active metabolites in environment becomes inevitable. Pollutant input prevention at the production source complemented with wastewater treatment is crucial to ensure water safety (Kümmerer et al., 2018). However, effective input prevention in case of antimicrobials and other pharmaceuticals calls for responsible use of drugs and personal care products by individuals. Intensive information campaigns should be launched to educate the masses about the ecological consequences of misusing antibacterial products. A large portion of the population is creating the habit of regular hand washing as a result of the pandemic. These practices will remain embedded even after the pandemic subsides. Therefore, educating the public about the unwanted effects of antimicrobial/antibacterial products during the pandemic will have the greatest opportunity to instilling change. Governments should ensure that advertising material and message of hygienic products are aligned with COVID-19 guidelines. We also urge researchers to evaluate the environmental consequences of the response measures to COVID-19 by focusing on therapeutic as well as non-therapeutic antimicrobials.
CRediT authorship contribution statement
M. Usman: Conceptualization, Writing - original draft, Writing - review & editing. M. Farooq: Writing - review & editing. K. Hanna: Writing - review & editing.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgments
Dr. M. Usman gratefully acknowledges the research grant from PEIE Research Chair for the Development of Industrial Estates and Free Zones, Sultan Qaboos University, Oman (CHAIR/DVC/MADAYN/20/02).
Editor: Damia Barcelo
References
- Berendonk T.U., Manaia C.M., Merlin C., Fatta-Kassinos D., Cytryn E., Walsh F., Bürgmann H., Sørum H., Norström M., Pons M.-N., Kreuzinger N., Huovinen P., Stefani S., Schwartz T., Kisand V., Baquero F., Martinez J.L. Tackling antibiotic resistance: the environmental framework. Nat. Rev. Microbiol. 2015;13:310–317. doi: 10.1038/nrmicro3439. [DOI] [PubMed] [Google Scholar]
- Chaudhary N.K., Chaudhary N., Dahal M., Guragain B., Rai S., Chaudhary R., Sachin K., Lamichhane-Khadka R., Bhattarai A. 2020. Fighting the SARS CoV-2 (COVID-19) Pandemic with Soap. (Preprints, 2020050060) [Google Scholar]
- Cleaning Matters Coronavirus: supplies run low of anti-bacterial hand-soaps. 2020. https://www.cleaning-matters.co.uk/Coronavirus-anti-bacterial-soaps
- Cohen J. ‘Frightening’ typhoid fever outbreak spreads in Pakistan. Science. 2018;361:214. doi: 10.1126/science.361.6399.214. [DOI] [PubMed] [Google Scholar]
- Centre for Disease Prevention and Control, USA . 2019. Measuring Outpatient Antibiotic Prescribing.https://www.cdc.gov/antibiotic-use/community/programs-measurement/measuring-antibiotic-prescribing.html [Google Scholar]
- Hickman M. The Independent. 2009. Soap and medicine sales soar due to swine flu. [Google Scholar]
- Hsu J. How COVID-19 is accelerating the threat of antimicrobial resistance. BMJ. 2020;369:m1983. doi: 10.1136/bmj.m1983. [DOI] [PubMed] [Google Scholar]
- Huttner B.D., Catho G., Pano-Pardo J.R., Pulcini C., Schouten J. COVID-19: don’t neglect antimicrobial stewardship principles! Clin. Microbiol. Infect. 2020;26:808–810. doi: 10.1016/j.cmi.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kümmerer K., Dionysiou D.D., Olsson O., Fatta-Kassinos D. A path to clean water. Science. 2018;361:222. doi: 10.1126/science.aau2405. [DOI] [PubMed] [Google Scholar]
- Lai C.-C., Shih T.-P., Ko W.-C., Tang H.-J., Hsueh P.-R. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int. J. Antimicrob. Agents. 2020;55 doi: 10.1016/j.ijantimicag.2020.105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maillard J.-Y., Bloomfield S.F., Courvalin P., Essack S.Y., Gandra S., Gerba C.P., Rubino J.R., Scott E.A. Reducing antibiotic prescribing and addressing the global problem of antibiotic resistance by targeted hygiene in the home and everyday life settings: a position paper. Am. J. Infect. Control. 2020 doi: 10.1016/j.ajic.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClellan K., Halden R.U. Pharmaceuticals and personal care products in archived U.S. biosolids from the 2001 EPA national sewage sludge survey. Water Res. 2010;44:658–668. doi: 10.1016/j.watres.2009.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNamara P.J., Levy S.B. Triclosan: an instructive tale. Antimicrob. Agents Chemother. 2016;60:7015. doi: 10.1128/AAC.02105-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNamara P.J., LaPara T.M., Novak P.J. The impacts of triclosan on anaerobic community structures, function, and antimicrobial resistance. Environ. Sci. Technol. 2014;48:7393–7400. doi: 10.1021/es501388v. [DOI] [PubMed] [Google Scholar]
- Patel M., Kumar R., Kishor K., Mlsna T., Pittman C.U., Mohan D. Pharmaceuticals of emerging concern in aquatic systems: chemistry, occurrence, effects, and removal methods. Chem. Rev. 2019;119:3510–3673. doi: 10.1021/acs.chemrev.8b00299. [DOI] [PubMed] [Google Scholar]
- Rawson T.M., Moore L.S.P., Zhu N., Ranganathan N., Skolimowska K., Gilchrist M., Satta G., Cooke G., Holmes A. Bacterial and fungal co-infection in individuals with coronavirus: a rapid review to support COVID-19 antimicrobial prescribing. Clin. Infect. Dis. 2020 doi: 10.1093/cid/ciaa530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rawson T.M., Ming D., Ahmad R., Moore L.S.P., Holmes A.H. Antimicrobial use, drug-resistant infections and COVID-19. Nat. Rev. Microbiol. 2020 doi: 10.1038/s41579-020-0395-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reardon S. Antibiotic treatment for COVID-19 complications could fuel resistant bacteria. Science. 2020 doi: 10.1126/science.abc2995. [DOI] [Google Scholar]
- Rodriguez-Mozaz S., Vaz-Moreira I., Varela Della Giustina S., Llorca M., Barceló D., Schubert S., Berendonk T.U., Michael-Kordatou I., Fatta-Kassinos D., Martinez J.L., Elpers C., Henriques I., Jaeger T., Schwartz T., Paulshus E., O’Sullivan K., Pärnänen K.M.M., Virta M., Do T.T., Walsh F., Manaia C.M. Antibiotic residues in final effluents of European wastewater treatment plants and their impact on the aquatic environment. Environ. Int. 2020;140:105733. doi: 10.1016/j.envint.2020.105733. [DOI] [PubMed] [Google Scholar]
- Slater F.R., Singer A.C., Turner S., Barr J.J., Bond P.L. Pandemic pharmaceutical dosing effects on wastewater treatment: no adaptation of activated sludge bacteria to degrade the antiviral drug Oseltamivir (Tamiflu®) and loss of nutrient removal performance. FEMS Microbiol. Lett. 2011;315:17–22. doi: 10.1111/j.1574-6968.2010.02163.x. [DOI] [PubMed] [Google Scholar]
- UN Interagency Coordination Group on Antimicrobial Resistance . 2019. No Time to Wait: Securing the Future from Drug-Resistant Infections. Report to the Secretary-General of the United Nations Washington. [Google Scholar]
- UNESCO How soap kills COVID-19 on hands. 2020. https://en.unesco.org/news/how-soap-kills-covid-19-hands
- Wei W., Ortwine J.K., Mang N.S., Joseph C., Hall B.C., Prokesch B.C. 2020. Limited Role for Antibiotics in COVID-19: Scarce Evidence of Bacterial Coinfection. medRxiv. [DOI] [Google Scholar]
- WHO Q&A on coronaviruses (COVID-19) 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/question-and-answers-hub/q-a-detail/q-a-coronaviruses