Abstract
Disengagement from HIV care has emerged as a challenge to the success of universal test and treat strategies for HIV-infected women. Technology may enhance efforts to monitor and support engagement in HIV care, but implementation barriers and facilitators need to be evaluated. We conducted a mixed-method study among HIV-infected, pregnant women and healthcare workers (HCWs) in Malawi to evaluate barriers and facilitators to three technologies to support monitoring HIV care: 1) text messaging, 2) SIM card scanning and 3) biometric fingerprint scanning. We included 123 HIV-infected, pregnant women and 85 HCWs in a survey, 8 focus group discussions and 5 in-depth interviews. Biometric fingerprint scanning emerged as the preferred strategy to monitor engagement in HIV care. Among HCWs, 70% felt biometrics were very feasible, while 48% thought text messaging and SIM card scanning were feasible. Nearly three quarters (72%) of surveyed women reported they would be very comfortable using biometrics to monitor HIV appointments. Barriers to using text messaging and SIM card scanning included low phone ownership (35%), illiteracy concerns, and frequent selling or changing of mobile phones. Future work is needed to explore the feasibly of implementing biometric fingerprint scanning or other technologies to monitor engagement in HIV care.
Keywords: HIV, pregnancy, technology, engagement in HIV care, mobile phones, biometrics
Introduction
Since its introduction in 2013, the WHO’s policy of universal test and treat for all pregnant and breastfeeding women with HIV, known as Option B+, has contributed to significant progress in lowering HIV incidence and improving access to antiretroviral therapy (ART)(Organization, 2017; UNAIDS, 2016; WHO, 2013). Despite these gains, disengagement from HIV care, high rates of mobility, and transferring between clinics have all emerged as challenges (Clouse et al., 2017; Knettel et al., 2018; Tweya et al., 2014). For Option B+ to be successful, supporting women’s ongoing engagement in HIV care is essential.
Sustained engagement in HIV care requires the ability to monitor transfers between clinics(Bengtson, Go, et al., 2019; Rice et al., 2018). In Malawi and South Africa, up to 30% of women who default from Option B+ programs have self-transferred and are receiving care elsewhere (Clouse, et al., 2017; Tweya, et al., 2014). Technologies, such as mobile phones and biometric fingerprint scanning could provide a simple and reliable way to identify women transferring HIV clinics (Bengtson, Kumwenda, et al., 2019; Catalani, Philbrick, Fraser, Mechael, & Israelski, 2013; McNairy et al., 2017; Odei-Lartey et al., 2016; van der Kop et al., 2018; Wall et al., 2015). However, barriers and facilitators to implementing these technologies to monitor engagement in HIV care have not been evaluated. To fill this gap, we conducted a mixed-method study evaluating barriers and facilitators towards using three different types of technology to monitor engagement in care for HIV-infected women in Option B+.
Methods
Study design and sample
We conducted a formative mixed-methods study among HIV-infected pregnant women initiating ART through Option B+ and healthcare workers (HCWs) at two large urban ART clinics in Lilongwe, Malawi. We included HIV-infected women initiating or re-initiating ART through Option B+ and HCWs from a range of roles. All participants had to be at least 18 years of age and reside in Lilongwe District to participate. HCWs included were nurses, tracers responsible for locating patients defaulting from HIV care, and a range of other healthcare support positions.
For the survey, a convenience sample of HCWs and HIV-infected women presenting for antenatal who met inclusion criteria were asked to participate. A separate convenience sample of HCWs and women were recruited for FGDs. Women and HCWs eligible for inclusion were sensitized to the aims of study; those who consented to participate filled out a survey or were contacted by a research assistant to schedule their participation in a FGD or IDI. All participants provided written informed consent to participate and ethical approval was provided by The University of [removed for peer review] and the National Health Science Research Committee in Malawi.
Data collection and analysis
We conducted a quantitative survey, eight focus group discussions (FGDs; four among women and four among HCWs), and five in-depth interviews (IDIs; all among HCWs). The survey and FGDs were designed to assess barriers and facilitators to using technology to monitor engagement in HIV. IDIs were conducted among HCWs only to understand current practices to support engagement in HIV care. Survey and FGD questions explored three potential technologies to monitor HIV visits: 1) mobile phone text messaging, 2) mobile phone SIM card scanning, and 3) biometric fingerprint scanning.
Data collection tools were prepared in English and translated into Chichewa. Survey data were analyzed descriptively using Stata version 15 (StataCorp, College Station, TX). Qualitative interviews were audio recorded in Chichewa, transcribed and translated into English by a research assistant, and entered into Nvivo v.11 (Nvivo qualitative data analysis Software; QSR International Pty Ltd.). Transcripts were read for content and coded using first deductive and then inductive coding and key themes were identified (Bernard, 1995).
Results
We included 104 HIV-infected women initiating ART in Option B+ and 50 HCWs in the survey. Among surveyed women, the median age was 25 (IQR 25, 30), 80% lived in an urban area, 68% were married, 48% had completed secondary school or higher (Table 1) and 35% reported owning their own mobile phone (Table 3). Among HCWs surveyed, 54% were providers and 22% were administrative staff, tracers, or HIV testing counselors (Table 2). An additional 19 HIV-infected women participated in FGDs and 30 HCWs participated in FGDs and IDIs.
Table 1.
Demographic and clinical characteristics of 104 HIV-infected, pregnant women initiating antiretroviral therapy in Lilongwe, Malawi.
| Women | |
|---|---|
| Characteristic | N=104 |
| Median (IQR) | |
| Age (median, IQR) | 25 (22, 30) |
| Age at first marriage | 19 (18, 21) |
| Number of weeks pregnant | 24 (20, 26) |
| Number of living children | 1 (0,2) |
| Religion | N (%) |
| Christian | 91 (88%) |
| Muslim | 12 (11%) |
| None | 1 (1%) |
| Residence | |
| Urban | 82 (80%) |
| Rural | 19 (18%) |
| Don’t know | 2 (2%) |
| Occupation | |
| Peasant farmer | 4 (4%) |
| Housewife/caretaker | 58 (56%) |
| Small business owner | 33 (31%) |
| Casual laborer | 5 (5%) |
| Other | 4 (4%) |
| Education | |
| None | 4 (4%) |
| Standard 1–7 | 27 (26%) |
| Standard 8 | 21 (20%) |
| Secondary or more | 50 (48%) |
| Don’t know | 2 (2%) |
| Marital Status | |
| Single or never married | 32 (31%) |
| Married | 71 (68%) |
| Separated | 1 (1%) |
| Living arrangement | |
| Alone | 26 (25%) |
| With husband | 65 (62%) |
| With family or friends | 13 (13%) |
| Is this your first pregnancy? | |
| No | 78 (75%) |
| Yes | 26 (25%) |
| Among women living with a partner | N=65 |
| Is your partner HIV-infected | |
| No | 27 (42%) |
| Yes | 10 (15%) |
| Don’t know | 28 (43%) |
| Have you disclosed your status to your partner? | |
| No | 49 (77%) |
| Yes | 13 (20%) |
| Don’t know | 2 (3%) |
Table 3.
Characteristic of mobile phone use among 104 HIV-infected women initiating antiretroviral therapy.
| Women (n, %) | |
|---|---|
| N=104 | |
| Mobile phone ownership | |
| Does not own her own phone | 68 (65%) |
| Does own her own phone | 36 (35%) |
| Among with women a mobile phone | N=36 |
| Primary mobile phone use | |
| Phone calls | 28 (78%) |
| Text messages | 4 (11%) |
| Other | 4 (11%) |
| Hours per day the phone is charged | |
| All day | 28 (78%) |
| About half the day | 6 (17%) |
| Less than half the day | 2 (5%) |
| Last time you ran out of phone credit | |
| Yesterday or today | 26 (72%) |
| Sometime last week | 7 (19%) |
| Sometime last month | 2 (6%) |
| Don’t know | 1 (3%) |
Table 2.
Characteristics of 50 HIV Healthcare Workers (HCWs) in Lilongwe, Malawi.
| HCWs | |
|---|---|
| N=50 | |
| Median (IQR) | |
| Age (median, IQR) | 36.5 (33, 38) |
| Yeas in position (median, IQR) | 5 (2, 11) |
| Position | N (%) |
| Administrative | 3 (6%) |
| Data clerk/coordinator | 2 (4%) |
| Health services associate | 8 (16%) |
| Mentor mother | 4 (8%) |
| Nurse/Matron | 23 (46%) |
| Clinical Officer | 4 (8%) |
| Tracer | 2 (4%) |
| HIV testing counsellor | 4 (8%) |
| Frequency of patients transfer to another HIV clinic without letting this clinic know they are transferring | |
| Not very frequently | 16 (32%) |
| Somewhat frequently | 16 (32%) |
| Frequently | 4 (8%) |
| Very frequently | 10 (20%) |
| Don’t know | 4 (8%) |
| Difficulty of finding patients who transfer clinics using the current EMR system | |
| Not very difficult | 12 (25%) |
| Somewhat difficult | 14 (29%) |
| Difficult | 11 (22%) |
| Very difficult | 11 (22%) |
| Don’t know | 1 (2%) |
Attitudes toward using technology to monitor engagement in HIV care
In both quantitative and qualitative data, there was strong support among women and HCWs for using technology to monitor engagement in HIV care. Women expressed few concerns about sharing their mobile phone or fingerprint information with clinic staff. Nearly half (45%) of all surveyed HCWs reported that it was difficult or very difficult to know when a patient had transferred to another clinic and that technology could help to identify transfers.
[Using technology to monitor engagement in HIV care across clinics] would be very helpful because it would reduce defaulting and movements across clinics because the people at [one HIV clinic] would know that if a client did not collect drugs from there then she collected them at [a different HIV clinic]. - FGD, mentor mother
In the survey, nearly 80% of HCWs felt biometric fingerprint scanning would be very useful and 70% felt it was very feasible, compared to 48% for both text messaging and SIM card scanning (Figure 1). Among women, 72% reported they would be very comfortable using biometrics to register at HIV clinics, compared to 52% for SIM card scanning and 55% for text messaging.
Figure 1.
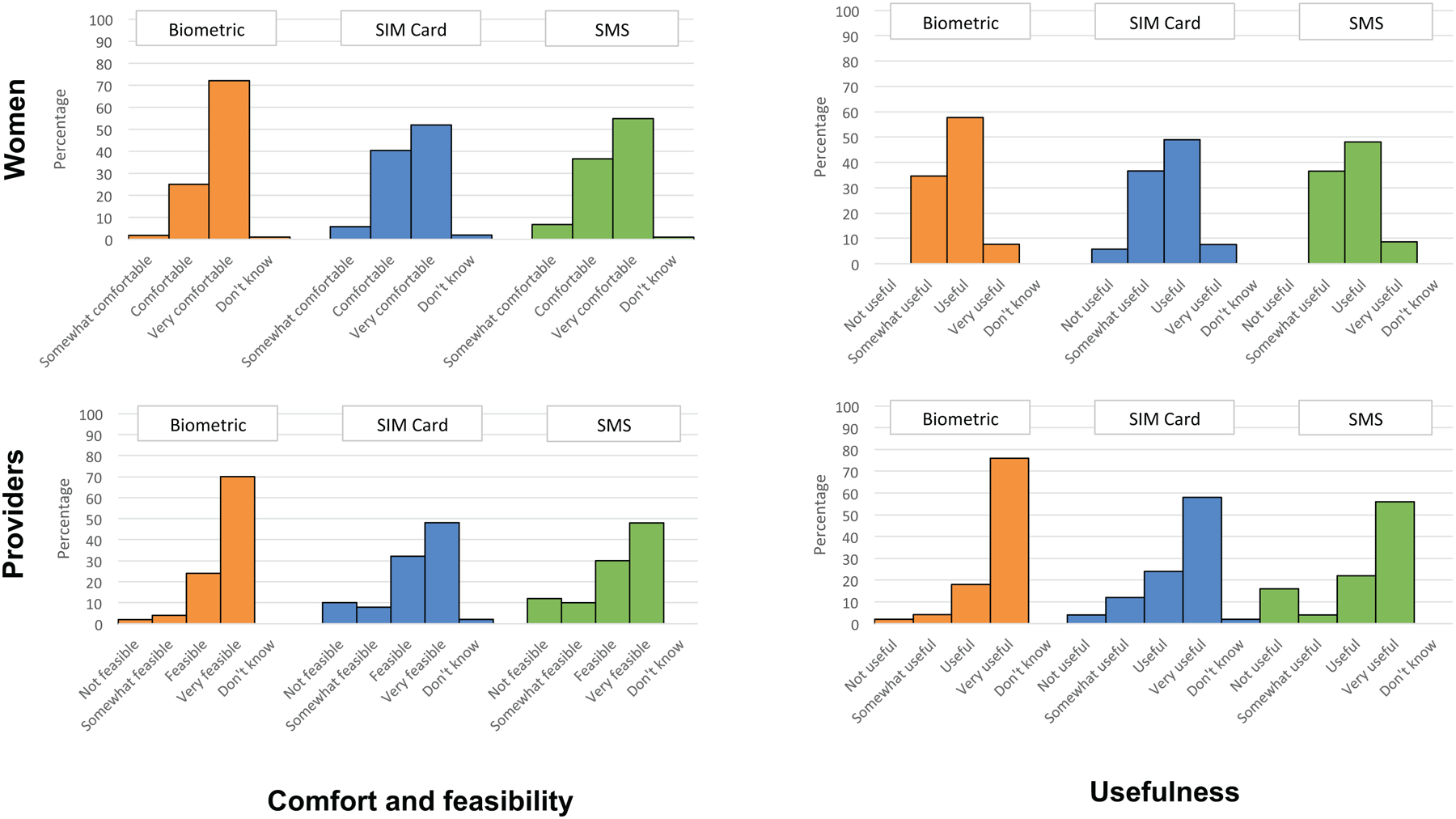
Attitudes towards using technology to monitor engagement in HIV care for HIV-infected women initiating antiretroviral therapy.
Barriers and facilitators to mobile phone-based strategies
Familiarity and the availability of mobile phones were important facilitators to using mobile phone-based strategies to monitor engagement in HIV care (Figure 2). However, participants also identified several important barriers. Only 35% of surveyed women owned their own phone and 72% reported running out of airtime credit within the last day (Table 3). In addition, nearly a quarter of HCWs surveyed raised concerns about text messages going to the wrong recipient due to women providing incorrect phone numbers or human error.
Figure 2.
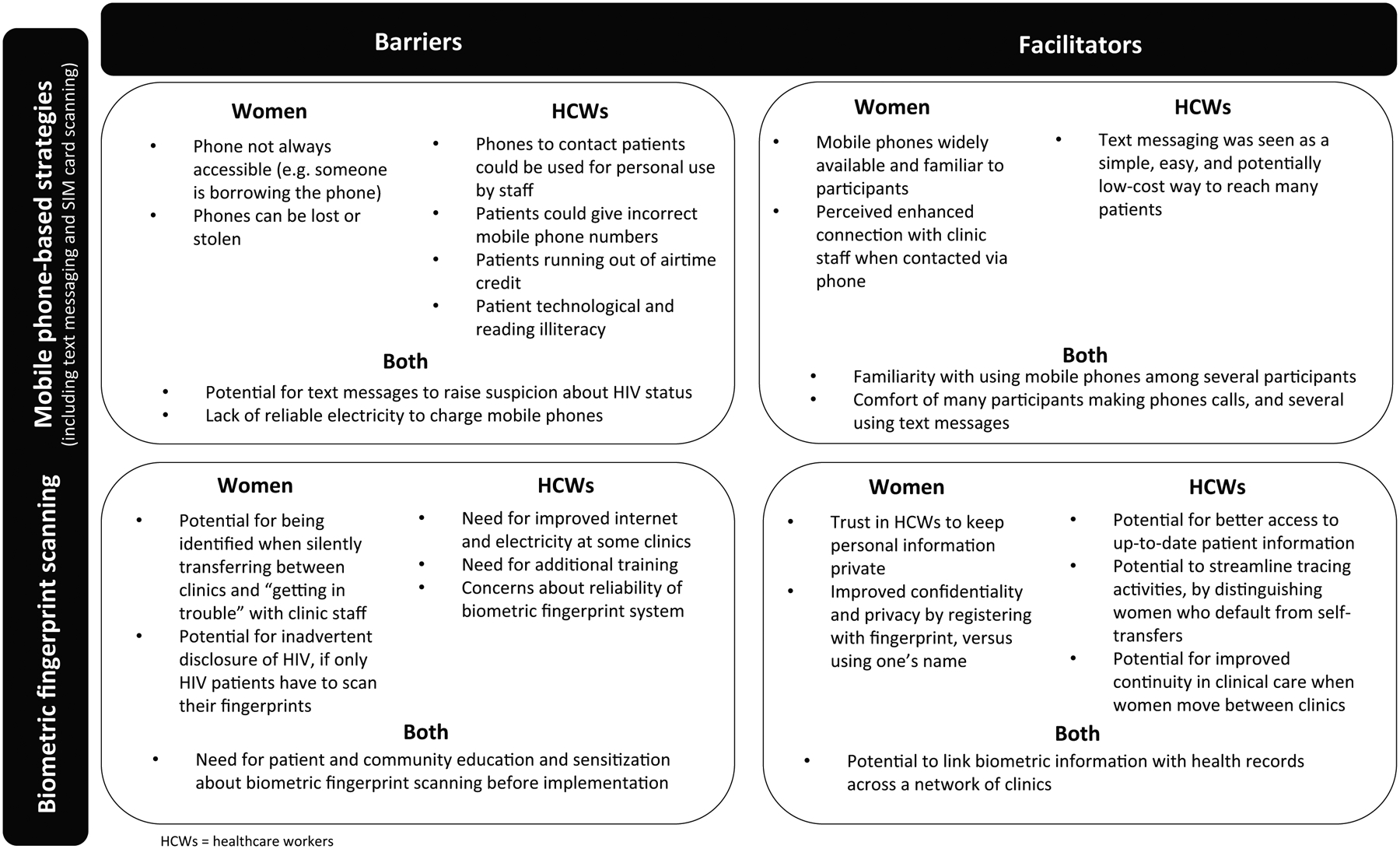
Barriers and facilitators of using technology to monitor engagement in care for HIV-infected women initiating antiretroviral therapy.
In qualitative interviews, patient privacy emerged as an important concern when using mobile phone-based strategies to monitor engagement in care. Particularly for text messages, both HCWs and women raised concerns about the potential for inadvertent disclosure of one’s HIV status or raising concerns with partners. As one woman shared “My husband always checks the missed calls and the received calls on my phone, even [text] messages.”
Barriers and Facilitators to Biometric Fingerprint Scanning
Women and HCWs reported few concerns about patient privacy or HIV status disclosure related to biometric fingerprint scanning. In fact, for some biometric fingerprint scanning was seen as providing improved privacy (Figure 2).
I would prefer the fingerprint scanning to the SIM card scanning because the SIM card would be seen by everyone but no one would know whose finger it is. It’s private. – FGD, woman re-initiating ART
Other important facilitators to using biometric fingerprint scanning included the ability to reliably and uniquely identify women. As one new ART initiator said, “I think the fingerprint scanning is better. You may lose your phone and the SIM card goes with it, but you can’t lose your finger.” For HCWs, the potential to uniquely identify patients and access their health information across a network of clinics was an important facilitator of improved clinical care.
Implementing this [biometric] system would be helpful … because it would help us to link up with our clients to know if they have been coming to make sure that they are still on treatment. Even if they do not come to our clinic…we know that they have collected their ARVS. We won’t include such clients among the defaulters or the list of missed appointments. - FGD, health services associate
To successfully implement biometric fingerprint scanning at HIV clinics, participants identified sensitization among patients, providers, and community members as essential. Barriers to implementing biometric fingerprint scanning included: 44% of surveyed HCWs identified the need for additional financial resources, 32% for training, and 12% the need for additional staff.
Discussion
In this mixed methods study of HIV-infected women initiating ART and HCWs in Lilongwe, Malawi we evaluated barriers and facilitators towards using technology to monitor engagement in HIV care. Compared to mobile phone-based strategies, biometric fingerprint scanning emerged as the preferred strategy among both women and HCWs. Barriers to using mobile phone-based strategies included low phone ownership, illiteracy concerns, frequent selling or changing of phones, and concerns about privacy and confidentiality (Figure 2). Facilitators to using biometric fingerprint scanning included minimal privacy concerns among women or HCWs and the perceived improved ability by HCWs to identify when patients transferred clinics. Investments in training, community sensitization, and infrastructure were noted as essential to support successful implementation of biometrics across HIV clinics.
As universal test and treat for HIV-infected pregnant women and adults rapidly becomes standard of care, reliable and comprehensive monitoring of engagement in HIV care is essential. In our study of women and HCWs in Option B+ programs, use of technology in general to support monitoring engagement in HIV care was highly acceptable, with biometric fingerprint scanning considered the most feasible strategy. Future work is needed to explore the feasibly of implementing biometric fingerprint scanning, alone or in combination with other technologies, to monitor women’s engagement in HIV care across HIV clinics.
Acknowledgements:
We thank the women and healthcare workers who participated in this study. We also thank the National Institute of Mental health and University of North Carolina Center for AIDS Research for funding support.
Funding: This work was supported by the National Institute of Mental Health [grant number R00MH112413] and the University of North Carolina Center for AIDS Research [grant number P30 AI50410].
Footnotes
Declaration of interest: The authors report no conflicts of interest.
Presentation: A version of this work was presented at the 22nd International AIDS Conference in Amsterdam, Netherlands, July 23–27, 2018.
Data availability statement: The data that support the findings of this study are available from the corresponding author, AMB, upon reasonable request.
References:
- Bengtson AM, Go V, Kumwenda W, Lurie M, Kutengule A, Owino M, & Hosseinipour M (2019). “A way of escaping”: a qualitative study exploring reasons for clinic transferring and its impact on engagement in care among women in Option B+(). AIDS Care, pp. 1–4. doi: 10.1080/09540121.2019.1614521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bengtson AM, Kumwenda W, Lurie M, Klyn B, Owino M, Miller WC, … Hosseinipour MC (2019). Improving Monitoring of Engagement in HIV Care for Women in Option B+: A Pilot Test of Biometric Fingerprint Scanning in Lilongwe, Malawi. AIDS Behav doi: 10.1007/s10461-019-02748-6 [doi]. 10.1007/s10461–019-02748–6 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernard HR (1995). Research Methods in Anthropology (2nd ed) Walnut Creek: Altamira Press. [Google Scholar]
- Catalani C, Philbrick W, Fraser H, Mechael P, & Israelski DM (2013). mHealth for HIV Treatment & Prevention: A Systematic Review of the Literature. Open AIDS J, 7, pp. 17–41. doi: 10.2174/1874613620130812003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clouse K, Vermund SH, Maskew M, Lurie MN, MacLeod W, Malete G, … Fox MP (2017). Mobility and Clinic Switching Among Postpartum Women Considered Lost to HIV Care in South Africa. J Acquir Immune Defic Syndr, 74(4), pp. 383–389. doi: 10.1097/qai.0000000000001284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knettel BA, Cichowitz C, Ngocho JS, Knippler ET, Chumba LN, Mmbaga BT, & Watt MH (2018). Retention in HIV Care During Pregnancy and the Postpartum Period in the Option B+ Era: Systematic Review and Meta-Analysis of Studies in Africa. J Acquir Immune Defic Syndr, 77(5), pp. 427–438. doi: 10.1097/qai.0000000000001616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNairy ML, Lamb MR, Gachuhi AB, Nuwagaba-Biribonwoha H, Burke S, Mazibuko S, … El-Sadr WM (2017). Effectiveness of a combination strategy for linkage and retention in adult HIV care in Swaziland: The Link4Health cluster randomized trial. PLoS Med, 14(11), p e1002420. doi: 10.1371/journal.pmed.1002420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Odei-Lartey EO, Boateng D, Danso S, Kwarteng A, Abokyi L, Amenga-Etego S, … Owusu-Agyei S (2016). The application of a biometric identification technique for linking community and hospital data in rural Ghana. Glob Health Action, 9, p 29854. doi: 10.3402/gha.v9.29854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization, (2017). HIV/AIDS Data and Statistics. WHO; Geneva, Switzerland: Retrieved Date Accessed, 4 September 2018 from http://www.who.int/hiv/data/en/. [Google Scholar]
- Rice B, Boulle A, Baral S, Egger M, Mee P, Fearon E, … Hargreaves J (2018). Strengthening Routine Data Systems to Track the HIV Epidemic and Guide the Response in Sub-Saharan Africa. JMIR Public Health Surveill, 4(2), p e36. doi: 10.2196/publichealth.9344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tweya H, Gugsa S, Hosseinipour M, Speight C, Ng’ambi W, Bokosi M, … Phiri S (2014). Understanding factors, outcomes and reasons for loss to follow-up among women in Option B+ PMTCT programme in Lilongwe, Malawi. Trop Med Int Health, 19(11), pp. 1360–1366. doi: 10.1111/tmi.12369 [DOI] [PubMed] [Google Scholar]
- UNAIDS. (2016). Prevention Gap Report. UNAIDS; Geneva, Switzerland: Retrieved Date Accessed, 4 September 2018 from http://www.unaids.org/sites/default/files/media_asset/2016-prevention-gap-report_en.pdf. [Google Scholar]
- van der Kop ML, Muhula S, Nagide PI, Thabane L, Gelmon L, Awiti PO, … Lester RT (2018). Effect of an interactive text-messaging service on patient retention during the first year of HIV care in Kenya (WelTel Retain): an open-label, randomised parallel-group study. Lancet Public Health, 3(3), pp. e143–e152. doi: 10.1016/s2468-2667(17)30239-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wall KM, Kilembe W, Inambao M, Chen YN, McHoongo M, Kimaru L, … Allen SA (2015). Implementation of an electronic fingerprint-linked data collection system: a feasibility and acceptability study among Zambian female sex workers. Global Health, 11, p 27. doi: 10.1186/s12992-015-0114-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO. (2013). Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: recommendations for a public health approach. . WHO; Geneva, Switzerland: Date Accessed, 4 September 2018 from http://apps.who.int/iris/bitstream/10665/85321/1/9789241505727_eng.pdf [PubMed] [Google Scholar]


