Abstract
COVID-19 is an active pandemic that likely poses an existential threat to humanity. Frequent handwashing, social distancing, and partial or total lockdowns are among the suite of measures prescribed by the World Health Organization (WHO) and being implemented across the world to contain the pandemic. However, existing inequalities in access to certain basic necessities of life (water, sanitation facility, and food storage) create layered vulnerabilities to COVID-19 and can render the preventive measures ineffective or simply counterproductive. We hypothesized that individuals in households without any of the named basic necessities of life are more likely to violate the preventive (especially lockdown) measures and thereby increase the risk of infection or aid the spread of COVID-19. Based on nationally-representative data for 25 sub-Saharan African (SSA) countries, multivariate statistical and geospatial analyses were used to investigate whether, and to what extent, household family structure is associated with in-house access to basic needs which, in turn, could reflect on a higher risk of COVID-19 infection. The results indicate that approximately 46% of the sampled households in these countries (except South Africa) did not have in-house access to any of the three basic needs and about 8% had access to all the three basic needs. Five countries had less than 2% of their households with in-house access to all three basic needs. Ten countries had over 50% of their households with no in-house access to all the three basic needs. There is a social gradient in in-house access between the rich and the poor, urban and rural richest, male- and female-headed households, among others. We conclude that SSA governments would need to infuse innovative gender- and age-sensitive support services (such as water supply, portable sanitation) to augment the preventive measures prescribed by the WHO. Short-, medium- and long-term interventions within and across countries should necessarily address the upstream, midstream and downstream determinants of in-house access and the full spectrum of layers of inequalities including individual, interpersonal, institutional, and population levels.
Keywords: Pandemic, COVID-19 response, Water and sanitation, Food access, Infectious disease, Preventive measures, Public health
Highlights
-
•
About 46% of the sampled households in 24 sub-Saharan African countries did not have in-house access to basic necessities.
-
•
The most vulnerable are practically missing from policy responses to limit the spread of COVID-19.
-
•
Individuals in households without water, sanitation and food storage are more likely to violate lockdown regulations.
-
•
Pre-existing inequalities in access to water, sanitation and food preservation compound layered vulnerabilities to COVID-19.
-
•
Transdisciplinary research and multi-sectoral policy responses are required to address the societal impacts of COVID-19.
1. Introduction
Since December 2019 the world has been afflicted by the coronavirus disease (COVID-19), and its causative virus severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). According to the World Health Organisation (WHO, 2020), most people infected with the COVID-19 will experience mild to moderate respiratory illness and recover without requiring special treatment. However, older people, and those with underlying medical problems such as cardiovascular disease, diabetes, chronic respiratory disease, and cancer are more likely to develop serious illness (Emami et al., 2020; Jordan et al., 2020). Notwithstanding this, the scale of infections and mortality make COVID-19 an existential threat to humankind. It has taken a heavy toll on all facets of the global economy and human life, including commerce and trade, health, livelihoods of populations, education, gender (Wenham et al., 2020), mobility (more than 100 countries have imposed travel restrictions and others in partial/total lockdown), lifestyle choices, environment (lower atmosphere nitrogen dioxide levels have dropped sharply in France, Spain, Italy and China) and interpersonal relationships, among others. It is therefore unsurprising that a plethora of measures have been proffered to curb the spread and adverse outcomes of the disease on economies and human life. Obviously, policy responses have been uneven, often delayed, and there have been missteps.
From a systems perspective, dealing with COVID-19 is a complex issue or wicked problem. It requires multi-sector, multi-disciplinary, interdisciplinary, trans-disciplinary and multi-stakeholder responses. This is reflected, in part, by the range of measures being proposed or implemented by different countries worldwide. The measures typically involve specific actions at various levels—individual, interpersonal, household, community, national, international, and global. Prominent actions that have been suggested so far include social/physical distancing, personal hygiene protocols, quarantine, isolation, environmental cleaning and ventilation, and partial/total lockdown. Most of these actions are community-based measures taken by planners, administrators, and employers to protect groups, employees and the population. While these measures are appropriate and laudable, they are often incognizant of existing intra-country and inter-country inequalities that could amplify vulnerabilities and potentially undermine well-intentioned interventions. Multidimensional inequality is a defining characteristic of all societies (Chakravarty and Lugo, 2019). A key aspect of these inequalities relates to access to water and sanitation facility.
According to the WHO, in 2017, 71% of the global population (5.3 billion people) used a safely managed drinking-water service – that is, one located on premises, available when needed, and free from contamination. Approximately 90% of the global population (6.8 billion people) used at least a basic service; that is an improved drinking-water source within a round trip of 30 min to collect water. About 785 million people lack even a basic drinking-water service, including 144 million people who are dependent on surface water (WHO/UNICEF, 2017). In least developed countries, 22% of health care facilities have no water service, 21% no sanitation service, and 22% no waste management service (WHO, 2017). In 2015, 844 million people had no access to safe drinking water, and 2.3 billion people did not have ready access to basic sanitation services (WHO/UNICEF, 2017). These issues are most severe in sub-Saharan Africa and central and southern Asia. In sub-Saharan Africa, people in urban areas are twice as likely as people in rural areas to have clean and safe water. Another way that we visualise the urban-rural divide is in sanitation. While rural areas often have less access to sanitation facilities, in sub-Saharan Africa the situation is very poor (Armah et al., 2018). Only 24% of the rural population and 44% of the urban population have access to sanitation facilities (WHO/UNICEF, 2017).
Access to safe water, sanitation and hygienic conditions play an essential role in protecting human health during all infectious disease outbreaks, including the current COVID-19 outbreak (UNICEF, 2020). When we consider the fact that personal hygiene features prominently in most of the community-based measures to curb the spread of COVID-19 and is inextricably linked to access to improved water and sanitation, it is pertinent to underscore why sub-Saharan Africa may be greatly impacted by the disease even though the region has so far recorded the lowest number of COVID-19 cases. Pandemics such as COVID-19 require data-driven decisions. Hitherto research on the pandemic has focused almost exclusively on the clinical, virology and epidemiological dimensions (see Lipsitch et al., 2020). This is understandable as COVID-19 is relatively new and active. Apart from the emerging insight that old persons and those with certain pre-existing health conditions are high risk group, there are gaps in our understanding of the human dimensions and behavioural responses of populations and groups to the implementation of community-based measures.
Currently, most SSA countries are implementing partial or full lockdowns with varied enforcement mechanisms such as enactment of movement restrictions acts and deployment of low enforcement agencies to ensure compliance. However, it is not clear how existing inequalities in access to water, sanitation and food storage at the household level will attenuate, moderate or enhance the spread of infections in the population. We hypothesize that individuals in households with constrained access to water, sanitation, and food are more likely to violate lockdown, social distancing and personal hygiene measures and thereby stand a higher risk of COVID-19 infection. We use data on 25 countries in sub-Saharan Africa to investigate how vulnerability to COVID-19 is layered and heightened and how this might compromise the intended policy outcome of curbing the spread of the disease. In the context of this paper, vulnerability is defined as the degree to which a population, individual or group is unable to anticipate, cope with, resist and recover from the impacts of disease (including pandemics as COVID-19). This study holds tremendous implications for theory (conceptualization of complexity and feedback relationships between policy intervention and human behaviour during pandemics), practice (intervention design) and policy (partial/total lockdowns). In particular, this study underscores the need for water, sanitation and hygiene services and products to be made available for confined households or areas with large vulnerable groups, exposed collective sites and public spaces.
2. Methods
2.1. Data source
Demographic and Health Surveys (DHS) data for 25 SSA countries were used in this study. DHS provide data for comparative quantitative assessment of several important indicators in the areas of health, nutrition, population, and household energy across developing countries. Demographic and Health Surveys are nationally representative population-based surveys with large sample sizes. The determination of optimal sample size of the surveys is usually a trade-off between available budget and the desired survey precision (Aliaga and Ren, 2006). A two-stage probabilistic sampling design was employed to select clusters to estimate important indicators at national level. In the first stage, primary sampling units (PSUs) are selected from a frame list with probability proportional to a size measure and in the second stage, a fixed number of households are selected from a list of households obtained from the selected PSUs. Probability sampling provides unbiased estimation and enables evaluation of sampling errors (ICF International, 2012). DHS data are open source and can be accessed on DHS website (www.dhsprogram.com). The inclusion criteria for a country in this study were as follows: (i) the country should be located in SSA; (ii) should have standardized/recoded DHS household datasets on location of sources of drinking water, type of sanitation facility and access to refrigerator; (iii) the year in which the data were collected should be between 2015 and present. Based on the criteria, 25 countries in SSA were included in the study. In a situation where a country had multiple datasets within the time frame, the most recent data were used. The countries included in this study and cluster locations are shown in Fig. 1 .
Fig. 1.
The selected study countries in sub-Saharan Africa. (South Africa clusters were not geo-located).
3. Measures
3.1. Response variable
The dependent variable considered in this study was in-house access to basic needs. In this study, basic needs include water, sanitation facility and food storage. Emphasis was placed on the location of these three basic needs. When these basic needs are found in the house or on the compound, the propensity of members of a household flouting lockdown regulations and the risk of getting infected by COVID-19 could be low. In-house in the study context connotes inside a house or on the immediate compound of a house. It is worthy to note that the importance of these three basic needs with regards to adhering to lockdown regulations are not the same. For instance, the likelihood of a household without in-house sanitation facility violating the lockdown regulations is not the same as that of a household without refrigerator to store food. Other means of preservation can be used to store food for some few days but one cannot cope with living in a house without a sanitation facility for a day or two under total lockdown situation. In this regard, we gave the highest priority to sanitation facility followed by water (since some households have access to water sachets) and refrigerator (food storage) was given the least priority. In-house access to sanitation facility was generated from the “type of toilet facility” variable in DHS datasets. In-house access to water was derived from the “location of source of water”. In-house access to refrigerator was derived from “has refrigerator”. The three variables were combined to generate the outcome variable called “in-house access to basic needs” with eight (8) categories, ranked and recoded in order of importance. In-house access to all the three basic needs was recoded “0”, representing least propensity of flouting lockdown regulations and in-house access to none of the basic needs was recorded “7”, which represents the group with the highest propensity of violating lockdown regulations. The dependent variable “in-house access to basic needs” was treated as an ordinal variable with the following groupings: “0”Access to all, “1” Sanitation facility and water only “2” Sanitation facility and refrigerator only, “3” Sanitation facility only “4” Water and refrigerator, “5” Water only “6” Refrigerator only, “7” No access.
3.2. Key predictor variable
Both theoretically and practically, access to basic necessities within a household is a function of empowerment, which in turn depends on relationship structure. The explanatory variable was derived from the “relationship structure” variable and “sex of household member” in the DHS datasets. The two variables were combined to generate the key explanatory variable “household family structure” with the following groupings: “1” up to a single adult household, “2” two opposite sex adults household, “3” two female adults household, “4” two male adults household, “5” more than two related adults household and “6” more than two unrelated adults household.
3.3. Compositional and contextual factors
We controlled for compositional and contextual factors in assessing the relationship between household family structure and in-house access to basic needs. Compositional factor is related to the socio-demographic characteristics of an individual or a group (Collins et al., 2017; Pol and Thomas, 2001). It is categorized into biosocial and sociocultural factors. Biosocial factors are underlying biological or physical characteristics of individuals that are present at birth and not amenable to change (Pol and Thomas, 2001). Socio-cultural factors refer to lifestyles, economy, beliefs, values and customs (see Armah et al., 2018). The biosocial factors considered in this study included “sex of household member” (male or female), and “household age distribution”. Household age distribution was derived from age and number of household members variables. The age variable was recoded into three age groups; young adult (18–40), middle-age adult (41–64) and old-age adult (65 and above). Household size which is a continuous variable in DHS datasets was converted to a categorical variable by grouping the “number of household members”; small (less equal to 2), medium (3–5) and large (6 and above). The two recoded variables were then combined to produce household age distribution with 9 groups—“1” young adult in a small household, “2”young adult in a medium-size household, “3” young adult in a large-size household, “4”middle-aged adult in a small household, “5”middle-aged adult in a medium-size household, “6” middle-aged adult in a large-size household, “7” old-aged adult in a small household, “8” old-aged adult in a medium-size household and “9” old-aged adult in a large-size household. The socio-cultural variables included in the study were the wealth index (poorest, poorer, middle, richer and richest quintile) and highest educational level attained (no school/preschool, primary, secondary and higher).
Factors that define the broader neighbourhood characteristics or location-specific opportunities in a region are referred to as contextual factors (Collins et al., 2017; Ross and Mirowsky, 2008). The contextual factors included in the study were type of place of residence “urbanicity” (urban/rural) and country. Twenty four countries were included in the multivariate analysis. South Africa was dropped because preliminary analysis revealed that it is an outlier.
3.4. Data analysis
The statistical analyses were carried out in STATA 13 MP (StataCorp, College Station, TX, USA). Descriptive analysis was used to examine the distribution of in-house access to basic needs in the 25 study countries. Univariate and multivariate statistical techniques were employed to assess associations between the dependent variable (in-house access to basic needs) and the explanatory variables. Spatial heterogeneity analysis of in-house access to basic needs was also carried out. With the exception of the descriptive, all other analyses (univariate, multivariate and spatial) were carried out on 24 countries excluding South Africa. South Africa was removed from the analyses because it had by far the highest rate of in-house access to all the basic needs (50%, others being below 30%), and also households were not geolocated. Environmental Systems Research Institute (ESRI) ArcGIS 10.3 was used to produce the maps.
3.5. Univariate analysis
Pearson's Chi-square test was employed to determine the association between outcome variable (in-house access to basic needs) and the key predictor (household family structure) as well as the compositional and contextual factors. Cramer's V statistic was used to estimate the strength of the association between the variables. An association is considered strong when Cramer's V is equal or greater than 0.3 whereas an association is weak when Cramer's V is less than 0.3.
3.6. Multivariate regression
Ordered logistic regression was employed to model the relationship between in-house access to basic needs and household family structure. Ordered logistic regression was used because, it takes into account the order or ranking in the dependent categorical variable. In-house access to basic needs was ranked with regards to the propensity to flout lockdown regulations due to lack of in-house access to basic needs. Covariates such as compositional (sex of household member, household age distribution, wealth index and highest educational level attained) and contextual (urbanicity and country) factors were controlled or accounted for in the model. The effect size of the relationship was estimated using odds ratio (OR). An OR of 1 implies that the explanatory variable does not affect the odds of in-house access to basic needs; OR >1 means that the explanatory variable is related with higher odds of belonging to a group with higher order of worse outcomes in terms of in-house access to basic needs; OR <1 means that the explanatory variable is related with lower odds of belonging to a group with higher order of worse outcomes in terms of in-house access to basic needs. Robust estimates of variance was employed to correct any statistical outliers in the estimation of standard errors. Four models were run; household family structure (model 1), household family structure and biosocial factors (model 2) household family structure, biosocial factors and socio-cultural factors (model 3), household family structure, biosocial, sociocultural and contextual factors (model 4).
3.7. Spatial heterogeneity analysis
Recent datasets from DHS surveys have Global Positioning System (GPS) coordinates of the centroid point of enumeration clusters which enable spatial analysis and mapping. In order to protect the identity of respondents who participate in the surveys, the exact coordinates of the cluster locations are geomasked. Geomasking provides an approximate location of each households (Wilson et al., 2020) however, geolocations of households can still be used to assess spatial variations in DHS datasets (Kandala et al., 2011).
The spatial variations, with regards to in-house access to basic needs in the study countries, were mapped and assessed through categorical spatial interpolation in R using the Weighted K-Nearest Neighbor Classifier (kknn) (Hechenbichler and Schliep, 2004). The DHS household data were joined to the cluster locations spatial point data using cluster number as the common field. A regular grid of the dissolve boundary of the study countries was created. The geometric point data which contain the in-house access to basic needs as a factor variable was converted to a regular data frame. The common group in the in-house access to basic needs were retained in the process to avoid “noise” in the map. The “kknn” classifier was then employed to interpolate the point data on the grid cells created from the dissolved boundary layer of the study countries. The “k” was set to 50 in order to examine the lower level disparities within countries. The “k” specifies the number of neighboring points that is used in classifying point dataset into different categories on the grid cells.
3.8. Ethical statement
The DHS datasets used in the study were collected through standardised procedures and questionnaires reviewed and approved by the International Classification of Functioning, Disability and Health (ICF) Institutional Review Board (IRB). Moreover, the survey protocols for countries were also subjected to the host country laws.
4. Results
4.1. In-house access to basic needs
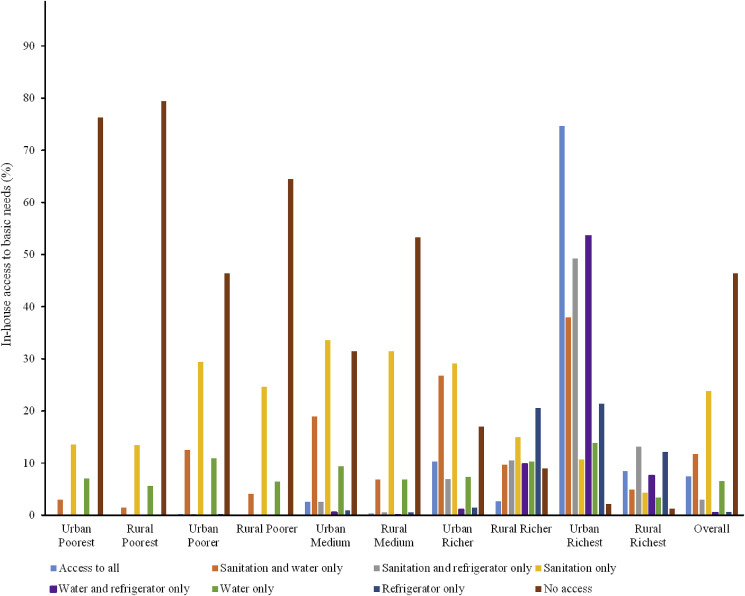
Fig. 2 shows that 7.5% of households in the 24 SSA countries (South Africa excluded) had in-house access to all the three basic needs and 46.4 had no in-house access to any of the basic needs. South Africa, which was not included in the analysis because it was considered an outlier, had 52.8% of its households having in-house access to all the basic needs and 5.8% had no in-house access to any of the basic needs. Rural poorest group recorded the highest proportion (79.4%) of households without in-house access to all the three basic needs even though there was no substantial difference compared to that of urban poorest (76.3%). Urban richest group had the highest proportion (74.7%) of households with in-house access to all the basic needs. No in-house access to any of the three necessities and sanitation only were dominant in poor categories irrespective of the type of residence whereas dominance in the richer and richest categories depended on the type of residence.
Fig. 2.
Percentage distribution of in-house access to basic needs in 24 countries based on urbanicity and wealth.
Table 1 presents the distribution of in-house access to all the three basic needs in the 25 study countries in SSA. The results show large disparities across the study countries. Five countries (Burundi, Chad, Democratic Republic of Congo, Madagascar and Rwanda) had less than 2% of their sampled households with in-house access to all the three basic needs. Apart from South Africa with over 50% of its households having in-house access to all the basic needs, Zimbabwe was the only country which had in-house access to all basic needs above 20%. Ten countries had over 50% of their households with no in-house access to all the three basic needs.
Table 1.
Percentage in-house access to water, sanitation facility and refrigerator in 25 countries in SSA.
| Country | DHS Dataset | Number of Households Sampled | Access to All Three (%) | Water and Sanitation (%) | Sanitation and Refrigerator (%) | Sanitation Only (%) | Water and Refrigerator (%) | Water Only (%) | Refrigerator Only (%) | None (%) | COVID-19 Confirmed Cases as at 09/07/2020 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Angola | DHS 2015–2016 | 15,817 | 15.33 | 10.33 | 9.26 | 24.34 | 0.92 | 3.77 | 1.26 | 34.79 | 396 |
| Burkina Faso | MIS 2017–2018 | 6282 | 3.61 | 8.91 | 1.29 | 37.36 | 0.05 | 2.04 | 0.22 | 46.51 | 1005 |
| Benin | DHS 2017–2018 | 13,932 | 4.08 | 19.66 | 0.37 | 10.38 | 0.21 | 13.4 | 0.28 | 51.62 | 1199 |
| Burundi | DHS 2016–2017 | 15,966 | 1.53 | 9.22 | 0.28 | 43.84 | 0.01 | 2.00 | 0.05 | 43.07 | 191 |
| Chad | DHS 2014–2015 | 18,157 | 1.92 | 2.51 | 1.28 | 32.04 | 0.10 | 1.33 | 0.37 | 60.44 | 873 |
| Congo Democratic Republic | DHS 2014–2015 | 17,117 | 1.42 | 3.89 | 0.32 | 7.09 | 0.26 | 5.71 | 0.1 | 81.22 | 7846 |
| Ethiopia | MIS 2016 | 16,649 | 8.60 | 11.19 | 0.41 | 5.69 | 1.35 | 8.18 | 0.4 | 64.18 | 6774 |
| Ghana | MIS 2016 | 5841 | 17.14 | 13.64 | 9.11 | 26.76 | 1.04 | 2.96 | 1.97 | 27.38 | 22,822 |
| Guinea | DHS 2018 | 7871 | 10.35 | 12.88 | 4.09 | 23.69 | 0.62 | 6.24 | 0.29 | 41.82 | 5697 |
| Kenya | MIS 2015 | 6481 | 4.71 | 27.87 | 0.99 | 22.51 | 0.26 | 12.62 | 0.14 | 30.91 | 8975 |
| Liberia | MIS 2016 | 4206 | 2.28 | 7.16 | 2.92 | 25.11 | 0.19 | 6.32 | 0.59 | 55.42 | 926 |
| Madagascar | MIS 2016 | 11,284 | 1.69 | 4.69 | 0.41 | 7.44 | 0.62 | 20.41 | 0.54 | 64.21 | 3782 |
| Mali | DHS 2018 | 9510 | 7.70 | 15.47 | 3.35 | 26.93 | 0.52 | 7.78 | 0.41 | 37.84 | 2358 |
| Malawi | MIS 2017 | 3729 | 7.83 | 8.66 | 0.72 | 9.81 | 1.96 | 11.24 | 0.62 | 59.16 | 1942 |
| Mozambique | MIS 2018 | 6196 | 19.54 | 10.43 | 1.50 | 13.61 | 2.00 | 8.33 | 0.68 | 43.92 | 1071 |
| Nigeria | DHS 2018 | 40,403 | 9.68 | 12.19 | 8.14 | 24.05 | 0.59 | 7.77 | 1.93 | 35.64 | 30,249 |
| Rwanda | DHS 2014–2015 | 12,684 | 1.66 | 10.06 | 0.31 | 60.05 | 0.01 | 0.59 | 0.02 | 27.30 | 1194 |
| Sierra Leone | MIS 2016 | 6719 | 3.77 | 9.45 | 3.20 | 26.43 | 0.09 | 6.07 | 0.31 | 50.68 | 1, 584 |
| Senegal | DHS 2016 | 4302 | 15.27 | 43.42 | 2.49 | 20.20 | 0.14 | 10.39 | 0 | 8.09 | 7784 |
| South Africa | DHS 2016 | 11,083 | 52.78 | 9.81 | 6.23 | 5.80 | 8.90 | 4.11 | 6.58 | 5.80 | 224,665 |
| Togo | MIS 2017 | 4909 | 4.32 | 12.94 | 1.47 | 22.69 | 0.04 | 6.48 | 0.14 | 51.93 | 695 |
| Tanzania | MIS 2017 | 9328 | 6.21 | 24.34 | 1.05 | 28.95 | 0.08 | 7.00 | 0.06 | 32.32 | 509 |
| Uganda | DHS 2016 | 19,340 | 3.49 | 8.54 | 1.04 | 21.16 | 0.09 | 3.80 | 0.22 | 61.65 | 1000 |
| Zambia | DHS 2018 | 12,588 | 14.27 | 10.29 | 3.02 | 23.54 | 1.18 | 7.38 | 0.6 | 39.74 | 1895 |
| Zimbabwe | DHS 2015 | 10,435 | 24.12 | 18.07 | 4.92 | 23.80 | 0.17 | 2.83 | 0.46 | 25.63 | 885 |
Chi-square results of in-house access to basic needs by country: χ2 = 7.8e+04 (P-value = 0.000; Cramér's V = 0.1994).
COVID-19 cases for study countries were obtained from John Hopkins University & Medicine website (https://coronavirus.jhu.edu/map.html).
4.2. Measures of association
The Pearson chi-square and Cramer's V statistics results of the association between in-house access to basic needs and household family structure and the compositional and contextual variables are provided in the Supplementary material (Table S1). The results rejected the null hypothesis that in-house access to basic needs was independent of household family structure. The results indicated a weak association (P<0.0001, Cramer's V = 0.076) between in-house access to basic needs and household family structure. Regarding the compositional and contextual factors, the results showed that there was a strong association between the outcome variable and wealth index (P<0.023, Cramer's V = 0.345), highest educational level attained (P<0.0001, Cramer's V = 0.260) and urbanicity (P<0.0001, Cramer's V = 0.520) whereas there was a weak association between the outcome variable and sex of household member (P<0.0001, Cramer's V = 0.029), household age distribution (P<0.0001, Cramer's V = 0.049) and country (P<0.0001, Cramer's V = 0.1994).
4.3. Relationship between household family structure and in-house assess to basic needs
In the multivariate analyses, four models: household family structure (model 1), biosocial (model 2), sociocultural (model 3), and contextual (model 4), were employed to assess their relationship with in-house access to basic needs. Table 2 shows the proportional odds ratios, robust standard errors, probability values and confidence intervals associated with the key predictor (household family structure) as well as the compositional and contextual factors. Model 1 indicates that households with two opposite sex adults were 28% more likely to belong to a group with worse outcomes in terms of in-house access to basic needs compared to households with up to a single adult. Households with two female adults and more than two unrelated adults were 35% and 65% respectively less likely to have worse outcomes compared to households with up to a single adult.
Table 2.
Ordered logistic regression model showing the relationship between household family structure and in-house access to basic needs.
| Model 1: Relationship Structure (N = 279731) |
Model 2: Relationship Structure + Biosocial Factors (N = 279731) |
Model 3: Relationship Structure + Biosocial + Sociocultural Factors (N = 233903) |
Model 4: Relationship Structure + Biosocial + Sociocultural + Contextural Factors (N = 233903) |
|||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variables | OR | Robust SE | P- Value | Confidence Interval | OR | Robust SE | P- Value | Confidence Interval | OR | Robust SE | P- Value | Confidence Interval | OR | Robust SE | P- Value | Confidence Interval | ||||
| Relationship structure (ref:up to single adult) | ||||||||||||||||||||
| 2 opposite sex adults, | 1.276 | 0.012 | 0.000 | 1.252 | 1.300 | 0.981 | 0.012 | 0.121 | 0.956 | 1.005 | 0.984 | 0.015 | 0.295 | 0.954 | 1.014 | 0.963 | 0.016 | 0.021 | 0.932 | 0.994 |
| 2 female adults | 0.651 | 0.022 | 0.000 | 0.610 | 0.695 | 0.655 | 0.022 | 0.000 | 0.614 | 0.700 | 0.912 | 0.038 | 0.028 | 0.840 | 0.990 | 1.006 | 0.044 | 0.901 | 0.922 | 1.096 |
| 2 male adults | 0.975 | 0.020 | 0.215 | 0.938 | 1.015 | 0.787 | 0.017 | 0.000 | 0.755 | 0.820 | 0.914 | 0.023 | 0.000 | 0.870 | 0.959 | 0.937 | 0.025 | 0.013 | 0.890 | 0.986 |
| More than 2 related adults | 0.994 | 0.010 | 0.537 | 0.975 | 1.013 | 0.650 | 0.009 | 0.000 | 0.632 | 0.669 | 0.838 | 0.015 | 0.000 | 0.810 | 0.867 | 0.921 | 0.017 | 0.000 | 0.889 | 0.955 |
| More than 2 unrelated adults | 0.350 | 0.007 | 0.000 | 0.337 | 0.364 | 0.246 | 0.005 | 0.000 | 0.236 | 0.256 | 0.689 | 0.016 | 0.000 | 0.657 | 0.722 | 0.817 | 0.021 | 0.000 | 0.777 | 0.859 |
| Sex (ref: male) | ||||||||||||||||||||
| Female | 0.939 | 0.009 | 0.000 | 0.921 | 0.957 | 0.776 | 0.009 | 0.000 | 0.759 | 0.794 | 0.885 | 0.011 | 0.000 | 0.864 | 0.906 | |||||
| Household age distribution(ref: Young Small) | ||||||||||||||||||||
| Young Medium | 1.620 | 0.023 | 0.000 | 1.576 | 1.666 | 1.150 | 0.020 | 0.000 | 1.111 | 1.190 | 1.053 | 0.020 | 0.006 | 1.015 | 1.093 | |||||
| Young Large | 2.421 | 0.040 | 0.000 | 2.345 | 2.501 | 1.303 | 0.026 | 0.000 | 1.253 | 1.356 | 1.060 | 0.023 | 0.007 | 1.016 | 1.106 | |||||
| Middle Small | 1.338 | 0.024 | 0.000 | 1.292 | 1.386 | 0.806 | 0.018 | 0.000 | 0.772 | 0.841 | 0.877 | 0.021 | 0.000 | 0.838 | 0.918 | |||||
| Middle Medium | 1.654 | 0.027 | 0.000 | 1.602 | 1.708 | 0.977 | 0.020 | 0.252 | 0.940 | 1.016 | 0.967 | 0.021 | 0.118 | 0.928 | 1.008 | |||||
| Middle Large | 2.132 | 0.035 | 0.000 | 2.064 | 2.202 | 1.090 | 0.022 | 0.000 | 1.047 | 1.134 | 0.989 | 0.022 | 0.603 | 0.947 | 1.032 | |||||
| Old Small | 1.975 | 0.041 | 0.000 | 1.896 | 2.057 | 0.737 | 0.019 | 0.000 | 0.700 | 0.776 | 0.808 | 0.023 | 0.000 | 0.765 | 0.854 | |||||
| Old Medium | 2.222 | 0.046 | 0.000 | 2.134 | 2.314 | 0.913 | 0.024 | 0.001 | 0.867 | 0.962 | 0.914 | 0.025 | 0.001 | 0.866 | 0.966 | |||||
| Old Large | 2.033 | 0.047 | 0.000 | 1.943 | 2.127 | 0.823 | 0.024 | 0.000 | 0.778 | 0.871 | 0.886 | 0.026 | 0.000 | 0.837 | 0.939 | |||||
| Wealth Index (ref: poorest) | ||||||||||||||||||||
| Poorer | 0.455 | 0.006 | 0.000 | 0.442 | 0.467 | 0.439 | 0.007 | 0.000 | 0.426 | 0.453 | ||||||||||
| Middle | 0.266 | 0.004 | 0.000 | 0.259 | 0.274 | 0.240 | 0.004 | 0.000 | 0.233 | 0.248 | ||||||||||
| Richer | 0.122 | 0.002 | 0.000 | 0.119 | 0.126 | 0.103 | 0.002 | 0.000 | 0.100 | 0.107 | ||||||||||
| Richest | 0.029 | 0.000 | 0.000 | 0.028 | 0.030 | 0.021 | 0.000 | 0.000 | 0.020 | 0.022 | ||||||||||
| Education (ref: no education) | ||||||||||||||||||||
| Primary | 0.814 | 0.009 | 0.000 | 0.798 | 0.831 | 0.957 | 0.012 | 0.000 | 0.935 | 0.980 | ||||||||||
| Secondary | 0.552 | 0.007 | 0.000 | 0.539 | 0.565 | 0.758 | 0.011 | 0.000 | 0.738 | 0.780 | ||||||||||
| Higher | 0.290 | 0.005 | 0.000 | 0.280 | 0.300 | 0.414 | 0.009 | 0.000 | 0.397 | 0.431 | ||||||||||
| Urbanicity (ref: Rural) | ||||||||||||||||||||
| Urban | 0.5312079 | 0.0058566 | 0.000 | 0.5198523 | 0.5428116 | |||||||||||||||
| Country (ref: Rwanda) | ||||||||||||||||||||
| Angola | 0.628 | 0.014 | 0.000 | 0.600 | 0.657 | |||||||||||||||
| Burkina Faso | 1.752 | 0.062 | 0.000 | 1.635 | 1.877 | |||||||||||||||
| Benin | 2.857 | 0.067 | 0.000 | 2.728 | 2.992 | |||||||||||||||
| Burundi | 1.813 | 0.040 | 0.000 | 1.736 | 1.894 | |||||||||||||||
| Chad | 3.647 | 0.096 | 0.000 | 3.463 | 3.841 | |||||||||||||||
| Ethiopia | 6.835 | 0.281 | 0.000 | 6.306 | 7.408 | |||||||||||||||
| Ghana | 0.611 | 0.027 | 0.000 | 0.561 | 0.665 | |||||||||||||||
| Guinea | 1.160 | 0.032 | 0.000 | 1.100 | 1.224 | |||||||||||||||
| Kenya | 1.026 | 0.031 | 0.406 | 0.966 | 1.088 | |||||||||||||||
| Liberia | 2.934 | 0.159 | 0.000 | 2.638 | 3.264 | |||||||||||||||
| Madagascar | 6.314 | 0.280 | 0.000 | 5.788 | 6.887 | |||||||||||||||
| Mali | 1.138 | 0.036 | 0.000 | 1.070 | 1.210 | |||||||||||||||
| Malawi | 9.653 | 0.661 | 0.000 | 8.441 | 11.040 | |||||||||||||||
| Mozambigue | 1.599 | 0.073 | 0.000 | 1.462 | 1.748 | |||||||||||||||
| Nigeria | 1.331 | 0.026 | 0.000 | 1.281 | 1.383 | |||||||||||||||
| Sierra Leone | 1.869 | 0.072 | 0.000 | 1.734 | 2.015 | |||||||||||||||
| Senegal | 0.127 | 0.004 | 0.000 | 0.120 | 0.136 | |||||||||||||||
| Congo Democratic Republic | 16.341 | 0.493 | 0.000 | 15.402 | 17.338 | |||||||||||||||
| Togo | 2.468 | 0.115 | 0.000 | 2.253 | 2.705 | |||||||||||||||
| Tazania | 0.799 | 0.026 | 0.000 | 0.750 | 0.851 | |||||||||||||||
| Uganda | 3.950 | 0.089 | 0.000 | 3.780 | 4.127 | |||||||||||||||
| Zambia | 1.004 | 0.025 | 0.866 | 0.957 | 1.054 | |||||||||||||||
| Zimbabwe | 0.510 | 0.012 | 0.000 | 0.486 | 0.535 | |||||||||||||||
In model 2 when biosocial factors (sex of household member and household age distribution) were controlled, the relationship between household family structure and in-house access to basic needs changed in magnitude. Households with two opposite sex adults became statistically insignificant indicating complete mediation of the relationship. Households with two male adults and more than two related adults which were not statistically significant in model 1 became significant in model 2. They were 21% and 35% respectively less likely to belong to a group with worse outcomes in terms of in-house access to basic needs compared to households with up to a single adult. The odds of households with more than two unrelated adults increased by 30% in model 2. Females were 7% less likely to belong to a group with worse outcomes in terms of in-house access to basic needs compared to males. Regarding household age distribution, all groups were more likely to belong to a group with higher level of worse outcomes in terms of in-house access to basic needs compared to the reference group, young adults in small households.
In the sociocultural model, the direction of the relationship between in-house access to basic needs and household family structure did not change compared to the model 2 but, there were changes in the magnitudes of some sub-groups. The proportional odds ratios for households with two female adults, two male adults, with more than two related adults and more than two unrelated adults decreased by 39%, 16%, 30% and 180%, respectively. Besides, the level of significance for households with two female adults reduced indicating partial mediation of the relationship. The direction of the relationship between sex of household member and in-house access to basic needs did not change but the magnitude increased by 17%. Regarding the effect of sociocultural factors on the relationship between in-house access to basic needs and household age distribution, three main things were observed. There was complete mediation of the relationship between middle-aged adults in medium-sized households and in-house access to basic needs. Middle-aged adults, old adults in small households, old adults in medium-sized households and old adults in large households became 19%, 26%, 9%, and 18% less likely to belong to a group with higher order of worse outcomes in terms of in-house access to basic needs compared to young adults in small households. In addition, there was decrease in magnitude for young adults in medium-sized households (8%), young adults (46%) and middle-aged adults (49%) in large households when sociocultural factors were controlled in model 3. Individuals in poorer, middle, richer and richest wealth quintile were 55%, 73%, 88%, and 97% were less likely to belong to a group with worse outcomes in terms of in-house access to basic needs compared to poorest households. Individuals educated to the primary level (19%), secondary level (45%) and higher level (71%) were less likely to belong to a group with higher order of worse outcomes in terms of in-house access to basic needs compared to individuals with no education or educated to the preschool level.
When contextual factors (urbanicity and country) were accounted for in model 4, suppression, partial and complete mediation were observed in the relationship between household family structure and the outcome variable. Households with two opposite sex adults group was not significant in the sociocultural model (model 3) but became marginally less likely to belong to a group with higher level of worse outcomes with regards to in-house access to basic needs compared to households with a single adult in model 4. There was complete mediation effect on households with two female adults which was statistically significant in model 3 became insignificant in model 4. There was also a partial mediation effect on household with two male adults. The proportional odds ratios for households with more than two related adults and households with more than two unrelated adults reduced by 10% and 19%, respectively. The direction of the relationship between sex of household member and in-house access to basic needs did not change but the magnitude reduced by 14%. The relationship between age distribution of household and the dependent variable was mediated, nonetheless, the direction of the association did not change. The level of significance for young adults in medium-sized households and young adults in large households reduced (partial mediation). Parameter estimates for middle-aged adults in large households became statistically insignificant indicating complete mediation by the contextual factors. With regards to wealth index, the direction of the relationship with in-house access to basic needs remained the same and there was no substantial change in magnitude of the proportional odds ratios. Contextual factors did not affect the direction of the effect of highest educational attainment but there were substantial changes in magnitude. The magnitude of the relationship for individuals educated to the primary, secondary and higher level decreased by 18%, 37% and 43%, respectively. Regarding urbanicity, households in urban areas were 47% less likely to have worse outcomes in terms of in-house access to basic needs compared to households in rural areas. Households in Angola, Ghana, Senegal, Tanzania and Zimbabwe were less likely to belong to a group with higher order of worse outcomes in terms of in-house access to basic needs compared to households in Rwanda. With the exception of Kenya and Zambia, which were not statistically significant, households in the remaining 16 countries were more likely to belong to a group with higher level of worse outcomes with regards to in-house access to basic needs compared to households in Rwanda.
4.4. Spatial mapping of in-house access to basic needs
Fig. 3 presents the interpolated map of in-house access to basic needs across 24 countries in SSA. The map shows a high spatial heterogeneity in terms of in-house access to basic needs in SSA. The most dominant category, as indicated by the map, is no access which corroborates the findings in Table 1 and Fig. 1. This category is conspicuous and well distributed throughout all the countries. Less dominant categories shown on the map include sanitation facility only, access to all as well as sanitation and water only. Three categories were almost masked out and were hard to find on the map—sanitation facility and refrigerator only, refrigerator only and water and refrigerator only. It implies that very few households belong to these three categories. Geographically, access to sanitation only clusters in the Central to Southern African countries whereas access to all, or access to toilet and water are concentrated in the Western and Eastern African countries.
Fig. 3.
Spatial variation of in-house access to basic needs in sub-Saharan Africa. Access to all means in-house access to all the three basic needs; water, sanitation facility and food storage. No access means no in-house access to any of the three bascic needs. The colour of each pixel is determined by the dominant category.
5. Discussion
This study employed DHS data on 25 countries in SSA to assess how vulnerability to COVID-19 is layered and heightened by existing inequalities in access to basic necessities of life, and how this might compromise the intended policy outcome of curbing the spread of the disease. We considered in-house access to three basic needs (sanitation facility, water and food storage) as critical things that households require in order to comply with lockdown measures and become less vulnerable to contracting COVID-19. The strength of using these as a proxy lies in the fact that without them, the propensity of individuals in households violating the lockdown measures (out of necessity) is inevitable and puts them at high risk to COVID-19.
The lack of in-house access to any of these basic necessities was prevalent and fairly distributed throughout the study countries (Fig. 3). This makes it extremely difficult for these SSA countries to adhere to some of the COVID-19 mitigation measures, prescribed by WHO, such as regular washing of hands, social distancing and lockdown. This suggests that some of the WHO prescriptions may be merely aspirational for millions at risk of exposure to the virus in lower- and middle-income countries (LMICs) due to existing inequalities. These realities must be considered when developing country or context-specific strategies for reducing COVID-19 transmission. So far, it is not clear how these vulnerable populations or existing inequalities have been visibly considered in either the provision or the implementation of the COVID-19 mitigation prescriptions in vulnerable LMICs.
Many people in SSA live in communities where vulnerable conditions persist and are limited by access to water and sanitation. Individuals without in-house access to source of water, and incapable of storing water for days, cannot implement the required sanitation practices at home. The only option is to resort to sources outside their houses which violate the lockdown regulations and social distancing measures that are vital in curbing the spread of COVID-19 (Colbourn, 2020). Having close to half of the population without in-house access to these basic necessities implies that the broad preventive measures by WHO might not be entirely effective in SSA, making the SSA highly vulnerable to rapid intra-country spread of COVID-19. It is predicted by WHO that Africa will be the next epicenter and with these worrying realities, there is a need for WHO and African leaders to devise context-specific interventions that accommodate the observed inequalities. Ghana, perhaps, as part of measures to mitigate the impacts of the preventive measures has offered free three months (April, May and June) supply of water but the implementation of this relief package has been fraught with some challenges due to poor distribution systems and extensive private ownership of water storage facilities. The underlying inequalities make long total lockdown, like what is happening in Europe, unfit for SSA and it is not surprising that there had been pockets of agitations and violent confrontations in some SSA countries that are just under partial lockdown.
The results of the study suggest a compelling need for SSA countries to swiftly address these inequalities as part of measures to strengthen their resilience and security to future pandemics or other crises of this nature. This is also in the interest of the advanced countries and global security, as by so doing, SSA countries would be able to hold themselves in readiness to comply fully with global prescriptions for slowing future pandemics. Parallel lessons can be drawn from the high COVID-19 death toll in the USA believed to be due to existing, long-standing inequalities.
Another important observation from the study is inequality induced by urbanicity. Poor households in both urban and rural areas lack in-house access to basic needs. Several studies have reported the plights of urban poor regarding access to essential services such as improved water and sanitation facilities, health care and clean cooking energy (Armah et al., 2018, 2019; Makonese et al., 2018; Mulenga et al., 2017; Tuyet-Hanh et al., 2016; Yang et al., 2013). However, the findings show that majority of households (75%) belonging to urban richest category had in-house access to all the three basic needs whereas that of rural richest was only 8%, suggesting that urbanicity can moderate the influence of wealth in having in-house access to the basic necessities.
The results from the inferential statistics indicate that household family structure influences in-house access to basic needs. Households with more adults are more likely to have in-house access to basic needs compared to households with no or a single adult. Adults are able to work and pool resources together to provide the basic necessities in a household. However, if there is only one adult in the household, the resources of this person may be overstretched, resulting in inability to provide all the required necessities. The relationship between in-house access to basic needs and household family structure was influenced by the compositional and contextual factors that were controlled for in the multivariate model. It means that the relationship between the two variables is not direct. Gender and household age distribution were found to influence the relationship between in-house access to basic needs and household family structure. Females were marginally more likely to have in-house access to basic needs compared to males. In most households in SSA, females are responsible for managing these basic needs and feel more vulnerable without these facilities compared to men, making females pay more attention to these especially when they are the household heads. This finding is consistent with Armah et al. (2018), Mulenga et al. (2017) and Osei et al. (2015). It implies that females are more likely to cope with social distancing and locked down measures, making them less exposed or vulnerable to COVID-19. Where this is not the case, females could be more vulnerable to COVID-19 infection than males as they are likely to be responsible for fetching water, buying and preparing food and seeking sanitary facilities in high risk places. Emerging studies point to the fact that men are more vulnerable to COVID-19 than females however, that has more to do with mortality than confirmed cases (Wenham, 2020).
Regarding household age distribution, older people irrespective of their household size, were marginally more likely to have in-house access to basic needs compared to young adults in a small household. It is known that household size has inverse correlation with wealth (Fotuè, 2013) but age might have moderated the influence of household size in this study. Young people usually have liquidity constraint (Muller and Yan, 2018) and may not be able to afford in-house access to basic needs. Armah et al. (2018) found that households headed by middle-aged and older-aged adults had higher odds of access to improved sanitation facilities compared to households with young adult heads. Perhaps, older people can afford basic services than young people due to material accumulation over time. Educated individuals were better off in having in-house access to basic needs compared to individuals with no education. Educated people have a better appreciation of the benefits and cost of having in-house access to the basic needs (Abubakar, 2017; Okurut et al., 2015). According to Kema et al. (2012), awareness enhances an individual's prospect of having access to improved sanitation facilities.
There are several policy implications inherent in the findings of this study in the context of COVID-19. First, households tend to adjust their behaviour and attempt to deal with external shocks unilaterally. Often it is effective (and households in developing countries are very inventive), but regularly adverse coping is observed. In this study, we find potential adverse coping strategies (such as travelling out of cities to avoid lockdown, or cutting back on water use due to lockdown) of many households in sub-Saharan Africa. In the current economic conditions, following the COVID-19 outbreak, a real threat is that households’ coping responses will include adverse coping, which will not leave permanent scars on only the household members but raise the risk of COVID-19 infections for the general community and nation. Where non-in-house access is also constrained, fatalities might occur because of COVID-19 measures but not infections. Therefore, such vulnerable households need to be assisted by community, government as well as international measures. In particular, the impact of shocks often overwhelms individual households. Also, many of the goods needed to strengthen household resilience are public goods. The continued provision and expansion of basic goods and services, including education, health services, public infrastructure and protection of property rights, are essential in times of the COVID-19 crisis. Here, continued and scaled up foreign assistance can make a huge difference in cash-strapped developing countries with large vulnerable households.
The second policy implication is that since poverty is a multi-dimensional dynamic and forward-looking concept, performance indicators should ideally relate the success of poverty reduction strategies and policies to their impact on risk and resilience to COVID-19. This is important given that the steeper the social gradient and poverty, the more the effect of the pandemic is likely to be widespread within a population.
Third, as this study clearly shows, the nature of vulnerability varies significantly among households and countries. Local knowledge is therefore vital in addressing vulnerability to COVID-19 and associated behavioural responses. For instance, as observed in the key predictor (household family structure), a ‘gendered’ approach to vulnerability is important. Women often comprise a disproportionate share of the poor, and their traditional role as caregivers, and often more extensive social networks, makes them important agents in the identification and mitigation of disease risks, and in post-pandemic assistance. In most of the countries included in this study, women predominate as frontline health workers, which heightens their likelihood of exposure and vulnerability.
Fourth, the proper and useful measurement of vulnerability and resilience will require much better data than is currently available. Often in the most vulnerable countries, in sub-Saharan Africa for instance, data constraints are most serious. Investing in sound, reliable, timely and regular data to capture disease-poverty-inequality-vulnerability-resilience will improve efforts at strengthening resilience. Finally, the most plausible approach towards dealing with the impact of disease-related shocks is one that aims to reduce or mitigate disease risks and assist risk coping, through three broad classes of interventions: strengthening resilience, building community immunity and safeguarding excellent institutions (see Naude et al., 2008).
The key issue of the spread of COVID-19 infections is not that many old/susceptible people are in Africa. In South Africa for instance, it is not concern for the wealthy aged in the middle class suburbs that has driven the rapid and extreme lockdown but rather the terrifying prospect of the disease tearing through informal settlements already ravaged by disease and poverty. Another key issue is that the social distancing measures that work in the urban environments of industrialised formal economies do not work at all in the conditions of urban informality, overcrowding and poor infrastructure that persist in the Global South. In such environments, it is impossible to ‘shelter in place’, conditions are overcrowded; there is not adequate sanitation, governmental authority is weak and contested, and the media landscape is saturated with misinformation, rumours and fake news. Those conditions make lockdown impossible—whether your population is mostly young, or whether it contains a large cohort of over 75 year olds. This also means that we need to go beyond the permanent notion that ‘one size fits all’ solutions are not enough. We have known that for decades. In this context, we need to deliberate more on public health systems since it is increasingly dawning on us that it is not medical science that flatten curves, it is social organization and behavioural responses. There are some important lessons from history. First, the last great European cholera epidemic, for instance, was not simply eradicated by medical science. What made the difference was workers' public health movements led by local organisations, working house to house in poor neighbourhoods, teaching people about hygiene, washing hands, and boiling water before use. Secondly, HIV/AIDS was largely contained in sub-Saharan Africa not simply by the roll out of anti-retrovirals. It was achieved by social movements de-stigmatising the disease and normalising the use of preventive measures. Without a broad-based social health movement changing the practices of ordinary citizens in poor communities, we will not be able to contain spread of COVID-19.
Demographic and health survey data are subject to recall and reporting biases. This may affect some of the variables (household size, age, relationship structure and highest educational level attained) used in this study. However, a review of DHS data has shown that the data are largely well reported and have made an enormous contribution to the public health studies in developing countries (Fabic et al., 2012). DHS are conducted on an ongoing basis and independently within countries, meaning that the majority of participating countries are not measured at the same time, limiting the contemporaneous cross-national comparisons (Corsi et al., 2012).
6. Conclusion
This study was premised on the hypothesis that individuals in households without basic necessities of life (water, sanitation and food storage) are more likely to violate lockdown regulations, move out of the home to meet their needs, and by extension stand a higher risk of aiding the spread of COVID-19 infections. Proceeding from this hypothesis, data on 25 countries in sub-Saharan Africa (SSA) were used to investigate how vulnerability to COVID-19 is layered and heightened by inequalities in in-house access to these basic necessities, and how this might compromise the intended policy outcome of curbing the spread of the disease. The results showed that approximately 46% of the sampled households in the studied countries (except South Africa) in SSA did not have in-house access to any of the three basic needs and about 8% had access to all the three basic needs. Only South Africa had over 50% of the households with in-house access to all the three basic needs. These findings portray large disparities across SSA with regards to in-house access to the basic necessities of life that permit full compliance with the COVID-19 preventive measures prescribed by the WHO. Without these, households will, out of necessity, risk breaching COVID-19 preventive measures, venturing out to access these resources and by so doing aid the spread of COVID-19 or render the preventive measures ineffective. The effect of this vulnerability and risk on the dynamics of COVID-19 transcends the households to the community, national and international scales. This adds clarity to why COVID-19 can spread so rapidly and have fatal consequences for SSA. It is important, therefore, that the response to COVID-19 captures the layered vulnerabilities and contextual specificities of nations and communities. Hence, SSA leaders should augment the recommendations by the WHO with innovative and cost-effective support services to such vulnerable households. The financial and administrative requirements of this layered response will likely overwhelm SSA governments and timely international assistance will be critical for successfully containing the pandemic.
Progress has been made in recent years in understanding and expanding the notion of vulnerability, and the advances have important implications for the efforts towards reducing poverty. But, much remains to be done in terms of refining, measuring, and applying the notion of vulnerability to research and policy analysis on disease distribution. Importantly, tackling vulnerability through strengthening household resilience, building appropriate bulwarks against disease risk, and creating and maintaining quality institutions remains a challenge. The findings of the current study add to the imperative for swiftly addressing these inequalities after the pandemic to strengthen resilience to multiple hazards across multiple spatial and temporal scales.
Credit author statement
Bernard Ekumah was involved in conception of ideas, data processing and analysis, writing, review and editing, and final approval of manuscript. Frederick Ato Armah was involved in conception of ideas, data processing and analysis, writing, review and editing, and final approval of manuscript. David Oscar Yawson was involved in data processing and analysis, writing, review and editing, and final approval of manuscript. Reginald Quansah was involved in data processing and analysis, writing, review and editing, and final approval of manuscript. Florence Esi Nyieku was involved in data processing and analysis, writing, review and editing, and final approval of manuscript. Samuel Asiedu Owusu was involved in data analysis, writing, review and editing, and final approval of manuscript. Justice Odoiquaye Odoi was involved in data analysis, writing, review and editing, and final approval of manuscript. Abdul-Rahaman Afitiri was involved in data analysis, writing, review and editing, and final approval of manuscript.
Declaration of competing interest
The authors declare that they have no known conflicts of interest to disclose.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.envres.2020.109936.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Abubakar I.R. Access to sanitation facilities among Nigerian households: determinants and sustainability implications. Sustainability. 2017;9(4):547. [Google Scholar]
- Aliaga A., Ren R. ORC Macro; Calverton, MD: 2006. Optimal Sample Sizes for Two-Stage Cluster Sampling in Demographic and Health Surveys: Working Paper 30. [Google Scholar]
- Armah F.A., Ekumah B., Yawson D.O., Odoi J.O., Afitiri A.R., Nyieku F.E. Access to improved water and sanitation in sub-Saharan Africa in a quarter century. Heliyon. 2018;4(11) doi: 10.1016/j.heliyon.2018.e00931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armah F.A., Ekumah B., Yawson D.O., Odoi J.O., Afitiri A.R., Nyieku F.E. Predictive probabilities of access to clean cooking: evidence from the demographic and health surveys in 31 countries in sub-saharan Africa. Environ. Justice. 2019;12(3):118–131. [Google Scholar]
- Chakravarty S.R., Lugo M.A. Poverty, Social Exclusion and Stochastic Dominance. Springer; Singapore: 2019. Multidimensional indicators of inequality and poverty; pp. 223–259. [Google Scholar]
- Colbourn T. COVID-19: extending or relaxing distancing control measures. Lancet Publ. Health. 2020;5(5) doi: 10.1016/S2468-2667(20)30072-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins J., Ward B.M., Snow P., Kippen S., Judd F. Compositional, contextual, and collective community factors in mental health and well-being in Australian rural communities. Qual. Health Res. 2017;27(5):677–687. doi: 10.1177/1049732315625195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corsi D.J., Neuman M., Finlay J.E., Subramanian S.V. Demographic and health surveys: a profile. Int. J. Epidemiol. 2012;41(6):1602–1613. doi: 10.1093/ije/dys184. [DOI] [PubMed] [Google Scholar]
- Emami A., Javanmardi F., Pirbonyeh N., Akbari A. Prevalence of underlying diseases in hospitalized patients with COVID-19: a systematic review and meta-analysis. Archives of Academic Emergency Medicine. 2020;8(1) [PMC free article] [PubMed] [Google Scholar]
- Fabic M.S., Choi Y., Bird S. A systematic review of Demographic and Health Surveys: data availability and utilization for research. Bull. World Health Organ. 2012;90:604–612. doi: 10.2471/BLT.11.095513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fotuè L.A.T. Awareness and the demand for improved drinking water source in Cameroon. Int. J. Econ. Pract. Theor. 2013;3(1):50–59. [Google Scholar]
- Hechenbichler K., Schliep K. 2004. Weighted K-Nearest-Neighbor Techniques and Ordinal Classification. [Google Scholar]
- ICF International . ICF International; Calverton, Maryland, U.S.A.: 2012. Demographic and Health Survey Sampling and Household Listing Manual. MEASURE DHS. [Google Scholar]
- Jordan R.E., Adab P., Cheng K.K. Covid-19: risk factors for severe disease and death. BMJ. 2020;368 doi: 10.1136/bmj.m1198. [DOI] [PubMed] [Google Scholar]
- Kandala N.B., Madungu T.P., Emina J.B., Nzita K.P., Cappuccio F.P. Malnutrition among children under the age of five in the Democratic Republic of Congo (DRC): does geographic location matter? BMC Publ. Health. 2011;11(1):261. doi: 10.1186/1471-2458-11-261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kema K., Semali I., Mkuwa S., Kagonji I., Temu F., Ilako F., Mkuye M. Factors affecting the utilisation of improved ventilated latrines among communities in Mtwara Rural District, Tanzania. The Pan African medical journal. 2012;13(Suppl. 1) [PMC free article] [PubMed] [Google Scholar]
- Lipsitch M., Swerdlow D.L., Finelli L. Defining the epidemiology of Covid-19—studies needed. N. Engl. J. Med. 2020;382:1194–1196. doi: 10.1056/NEJMp2002125. [DOI] [PubMed] [Google Scholar]
- Makonese T., Ifegbesan A.P., Rampedi I.T. Household cooking fuel use patterns and determinants across southern Africa: evidence from the demographic and health survey data. Energy Environ. 2018;29(1):29–48. [Google Scholar]
- Mulenga J.N., Bwalya B.B., Kaliba-Chishimba K. Determinants and inequalities in access to improved water sources and sanitation among the Zambian households. Int. J. Dev. Sustain. 2017;6(8):746–762. [Google Scholar]
- Muller C., Yan H. Household fuel use in developing countries: review of theory and evidence. Energy Econ. 2018;70:429–439. [Google Scholar]
- Naudé W., Santos-Paulino A.U., McGillivray M. 2008. Vulnerability in Developing Countries. [Google Scholar]
- Okurut K., Kulabako R.N., Abbott P., Adogo J.M., Chenoweth J., Pedley S. Access to improved sanitation facilities in low-income informal settlements of East African cities. J. Water, Sanit. Hyg. Dev. 2015;5(1):89–99. [Google Scholar]
- Osei L., Amoyaw J., Boateng G.O., Boamah S., Luginaah I. The paradox of water accessibility: understanding the temporal and spatial dimensions of access to improved water sources in Rwanda. J. Water, Sanit. Hyg. Dev. 2015;5(4):553–564. [Google Scholar]
- Pol L.G., Thomas R.K. Springer Science & Business Media; 2001. The Demography of Health and Health Care. [Google Scholar]
- Ross C.E., Mirowsky J. Neighborhood socioeconomic status and health: context or composition? City Community. 2008;7(2):163–179. [Google Scholar]
- Tuyet-Hanh T.T., Lee J.K., Oh J., Van Minh H., Ou Lee C., Hoan L.T. Household trends in access to improved water sources and sanitation facilities in Vietnam and associated factors: findings from the Multiple Indicator Cluster Surveys, 2000–2011. Glob. Health Action. 2016;9(1):29434. doi: 10.3402/gha.v9.29434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNICEF UNICEF WASH Programme contribution to COVID- 19 prevention and response. 2020. https://www.unicef.org/media/66091/file/UNICEF-WASH-COVID-19-prevention-response-overarching.pdf
- Wenham C., Smith J., Morgan R. COVID-19: the gendered impacts of the outbreak. Lancet. 2020;395(10227):846–848. doi: 10.1016/S0140-6736(20)30526-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson E., Hazel E., Park L., Carter E., Moulton L.H., Heidkamp R., Perin J. Obtaining district-level health estimates using geographically masked location from Demographic and Health Survey data. Int. J. Health Geogr. 2020;19(1):2. doi: 10.1186/s12942-020-0198-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . World Health Organization; 2020. Clinical Care for Severe Acute Respiratory Infection: Toolkit: COVID-19 Adaptation (No. WHO/2019-nCoV/SARI_toolkit/2020.1) [Google Scholar]
- World Health Organization and United Nations Children’s Fund . WHO and UNICEF; Geneva: 2017. Progress on Drinking Water, Sanitation and Hygiene: Update and SGD Baselines. [Google Scholar]
- Yang H., Bain R., Bartram J., Gundry S., Pedley S., Wright J. Water safety and inequality in access to drinking-water between rich and poor households. Environ. Sci. Technol. 2013;47(3):1222–1230. doi: 10.1021/es303345p. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.