Abstract
Background
Acute chloroquine and hydroxychloroquine toxicity is characterized by a combination of direct cardiovascular effects and electrolyte derangements with resultant dysrhythmias and is associated with significant morbidity and mortality.
Objective
This review describes acute chloroquine and hydroxychloroquine toxicity, outlines the complex pathophysiologic derangements, and addresses the emergency department (ED) management of this patient population.
Discussion
Chloroquine and hydroxychloroquine are aminoquinoline derivatives widely used in the treatment of rheumatologic diseases including systemic lupus erythematosus and rheumatoid arthritis as well as for malaria prophylaxis. In early 2020, anecdotal reports and preliminary data suggested utility of hydroxychloroquine in attenuating viral loads and symptoms in patients with SARS-CoV-2 infection. Aminoquinoline drugs pose unique and significant toxicological risks, both during their intended use as well as in unsupervised settings by laypersons. The therapeutic range for chloroquine is narrow. Acute severe toxicity is associated with 10–30% mortality owing to a combination of direct cardiovascular effects and electrolyte derangements with resultant dysrhythmias. Treatment in the ED is focused on decontamination, stabilization of cardiac dysrhythmias, hemodynamic support, electrolyte correction, and seizure prevention.
Conclusions
An understanding of the pathophysiology of acute chloroquine and hydroxychloroquine toxicity and available emergency treatments can assist emergency clinicians in reducing the immediate morbidity and mortality associated with this disease.
Keywords: Hydroxychloroquine, Chloroquine, Acute toxicity, Aminoquinoline
1. Introduction
Chloroquine and hydroxychloroquine are aminoquinoline derivatives widely used in the treatment of rheumatologic diseases as well as for malaria prophylaxis [1]. In early 2020, anecdotal reports and preliminary data suggested utility of chloroquine and hydroxychloroquine for attenuating viral loads and symptoms in patients with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection [[2], [3], [4], [5]]. Clinical trials are underway to determine treatment protocols, efficacy, and optimal dosing for SARS-CoV-2 infection [6]. Shortly following publication of initial reports indicating efficacy, cases of acute chloroquine toxicity including inadvertent deaths were reported in the United States (U.S.), African, and European newsmedia [[7], [8], [9]]. There were 283 chloroquine and hydroxychloroquine exposures reported to U.S. Poison Control Centers from January 1, 2020 through April 26, 2020, an increase of 42% compared to the same time period during the previous year, with a 93% increase during the month of April 2020 when compared to April 2019 [10]. Aminoquinoline drugs, including chloroquine, hydroxychloroquine, and amodiaquine, pose unique and significant toxicological risks, both in therapeutic use as well as in unsupervised settings by laypersons. For the purposes of this review, “aminoquinolines” will refer to chloroquine and hydroxychloroquine.
The therapeutic margin for chloroquine toxicity is narrow, and acute severe toxicity is associated with 10–30% mortality owing to a combination of direct cardiovascular effects and electrolyte derangements with resultant dysrhythmias [11]. In typical use, aminoquinoline toxicity is rarely reported. Fewer than 10 cases of acute severe chloroquine or hydroxychloroquine overdoses were reported to U.S. Poison Control Centers from 2012 to 2018, and approximately 70 cases of chloroquine or hydroxychloroquine overdose were reported in the literature base in the past decade [[12], [13], [14], [15], [16], [17], [18]]. While commonly prescribed for rheumatologic diseases, the novel proposed indication for SARS-CoV-2 infection represents an unprecedented expansion of aminoquinoline use in a significantly wider population [6].
As acute aminoquinoline toxicity is rare, contemporary literature on management is sparse [19]. Similar to other toxicological emergencies, randomized controlled trials and systematic reviews analyzing management approaches are absent. Prospective clinical trials evaluating treatment are also rare and date back to the 1980s and 1990s [20,21]. Updated treatment recommendations for aminoquinoline toxicity since the development of rescue modalities including intravenous lipid emulsion (ILE) and extracorporeal membrane oxygenation (ECMO) are lacking [22]. This article reviews the pathophysiology of aminoquinoline toxicity to provide guiding principles for management of acute complications. Understanding these complications and the approach to the management of electrolyte imbalances and hemodynamic instability is essential to optimizing patient care, especially following acute intoxication that may bring patients to the emergency department.
2. Methods
This review provides a focused evaluation of emergency department-based evaluation and treatment of aminoquinoline toxicity. The authors searched PubMed and Google Scholar for articles containing the key words “hydroxychloroquine” OR “aminoquinoline” OR “chloroquine” OR “quinolone” AND “toxicity” OR “poisoning” OR “adverse effects”. The PubMed search was conducted from database inception to April 5, 2020, yielding over 6300 articles. The first 200 articles in Google Scholar were also evaluated for inclusion. The literature search was restricted to studies published in English, with a focus on emergency medicine and critical care. Authors evaluated case reports and series, retrospective and prospective studies, systematic reviews and meta-analyses, and narrative reviews. Authors also reviewed guidelines and supporting citations of included articles. Articles were chosen based upon author consensus. When available, systematic reviews and meta-analyses were preferentially selected. These were followed sequentially by randomized controlled trials, prospective studies, retrospective studies, case reports, and other narrative reviews, when alternate data were not available. A total of 121 articles were selected for inclusion in this narrative review.
3. Discussion
3.1. Proposed aminoquinoline uses in coronavirus infection
Chloroquine and hydroxychloroquine are derivatives of quinine, derived from the bark of the Peruvian Cinchona tree. Chloroquine was synthesized in 1934 but shelved for years due to concerns for toxicity in human patients. Hydroxychloroquine sulfate was developed in 1946 in an effort to produce a less toxic chloroquine analog. Animal toxicological studies demonstrate hydroxychloroquine to be approximately 40% less toxic than chloroquine [23]. Initially indicated for antimalarial treatment and prophylaxis, chloroquine and analogs found new anti-inflammatory use in World War II. As millions of soldiers used it against malaria, military physicians observed improvement in inflammatory arthritis, leading to trials demonstrating aminoquinoline efficacy for rheumatologic conditions [24]. Antimalarial efficacy of chloroquine waned in the late 20th century, though it is still used for malarial prophylaxis in regions with susceptible Plasmodium strains. Chloroquine analogues have also been found to have metabolic, antithrombotic, antineoplastic, and antiviral effects, and have been hypothesized as targeted agents against coronavirus infection since the 2003 SARS outbreak [25,26].
Coronavirus disease 2019 (COVID-19), caused by SARS-CoV-2, is responsible for a major international pandemic with significant morbidity and mortality rates between 1.5 and 9% depending on the population investigated [27,28]. The pathophysiology of SARS-CoV-2 includes but is not limited to cytokine dysregulation, direct cytopathic effects on respiratory tract epitheliocytes, and down-regulation of lung protective angiotensin converting enzyme resulting in diffuse alveolar damage and hypercoagulability [29,30]. Viral entry is facilitated by cellular protease-primed spike protein binding to angiotensin-converting enzyme 2 (ACE2) receptors [31]. Efforts to repurpose or develop targeted therapeutics for SARS-CoV-2 infection have included assessment of anti-inflammatory drugs such as corticosteroids and interleukin inhibitors, macrolide antibiotics such as azithromycin, and direct-acting antivirals such as protease inhibitors and adenosine analogs [6]. The utility of aminoquinolines in attenuating infection severity is hypothesized to derive from preventing SARS-CoV-2 binding to target receptors and inhibiting viral cell entry [6]. Chloroquine and hydroxychloroquine are concentrated within the endosome, where they are thought to modulate organelle pH, inhibiting autophagosome formation and impairing cleavage of the SARS-CoV-2 spike protein [32]. Additional hypothesized immunomodulatory effects in SARS-CoV-2 infection include downregulation of T-cell response and inflammatory cytokine storm that play a role in organ injury and acute respiratory distress syndrome [32,33]. Preliminary in-vitro data and clinical trials in China and France in early 2020 using chloroquine and hydroxychloroquine suggested anti-SARS-CoV-2 activity [2,34]. These clinical trials utilized chloroquine at dosages and treatment courses greater than those prescribed for antimalarial and rheumatologic indications, raising concern for toxicological implications in susceptible patients. Following the United States Food and Drug Administration emergency use authorization for chloroquine and hydroxychloroquine in the treatment of SARS-CoV-2, many additional clinical trials with randomization, blinding, and larger sample sizes were initiated to determine the benefit and risks. The largest of these studies, enrolling over 96,000 patients, initially demonstrated increased in-hospital mortality rates in patients treated with chloroquine or hydroxychloroquine [35]. However, that study has since been retracted due to concerns regarding veracity of the data and analyses conducted and inability to conduct an independent and private peer review [36]. Additional studies have demonstrated similar findings of increased mortality or did not find any evidence of prevention of primary endpoints, such as need for mechanical ventilation or death in patients treated with aminoquinolines [[37], [38], [39]]. As of June 2020, there are over 40 ongoing clinical trials actively assessing the efficacy of chloroquine or hydroxychloroquine, demonstrating continued interest in its role as a therapeutic agent for COVID-19. Furthermore, additional trials targeting frontline healthcare workers are underway to assess for the possible preventative action of these agents. The use of chloroquine or hydroxychloroquine sulfate in combination with other novel antiviral agents has been discouraged by the United States Food and Drug Administration, as recent in-vitro data demonstrating increasing concentrations of chloroquine phosphate reduced formation of activated remdesivir triphosphate in human bronchial epithelial cells, raising concerns that it may reduce the antiviral activity of this medication [40]. Widespread non-prescription use of aminoquinolines for either prophylaxis or treatment by laypersons in response to fears of COVID-19 raises significant and continued concern for unintended toxicity from overdose and/or drug-drug interactions.
3.2. Chloroquine and hydroxychloroquine toxicology
3.2.1. Metabolism and pharmacokinetics
Despite slight differences in chemical structure, chloroquine and hydroxychloroquine are similar in regard to both metabolism and toxicity [41,42]. Both molecules are highly lipophilic, have a high volume of distribution, and have mild-to-moderate protein binding [43,44]. Following ingestion, the drugs are rapidly absorbed from the upper gastrointestinal (GI) tract and slowly redistribute to other compartments, eventually accumulating in erythrocytes, liver, lung, kidney, heart, muscle, and retinal tissue [43]. The combination of rapid absorption, high oral bioavailability, and slow redistribution prompts early peak serum levels post-ingestion which correlate with symptom severity in overdose [41].
Recent trials for COVID-19 have used regimens starting with 1 g on day one followed by 500 mg once daily for 4–7 days [6]. Median lethal doses (LD50) for chloroquine and hydroxychloroquine in humans are unknown as most available mortality data are derived from case reports and case series. As little as 2–3 g of chloroquine may be fatal in adult patients, though the most commonly reported lethal dose in adults is 3–4 g [19]. The minimum lethal dose of chloroquine is estimated at 30–50 mg/kg [45]. Whole blood concentrations of 2.5 μg/L and above are considered to be lethal [46]. Significant toxicity from hydroxychloroquine has been reported in patients with plasma levels ranging between 2.05 and 18.16 μmol/L (640 μg to 6100 μg/L) and fatalities with postmortem blood levels of 142.89 μmol/L (48,000 μg/L) and 309.62 μmol/L (104,000 μg/L) [21].
Both chloroquine and hydroxychloroquine undergo hepatic metabolism via cytochrome P450 enzymes [47]. Intrinsic liver disease, such as hepatitis, alcoholism, or those taking additional medications metabolized by the same P450 isozymes can also modify chloroquine and hydroxychloroquine metabolism [48]. Following hepatic metabolism, aminoquinolines are mainly excreted renally (Table 1 ). A small percentage of the initial ingested quantity of chloroquine or hydroxychloroquine is excreted unchanged [49]. Plasma half-life is extended in patients with renal insufficiency [50].
Table 1.
Pharmacokinetics of aminoquinolines.
| Oral Bioavailability (%) | Time to peak concentration | Volume of distribution (L/kg) | Half-life | Elimination | |
|---|---|---|---|---|---|
| Chloroquine | 80 | 2–5 h | >100 | 40–55 days | Renal |
| Hydroxychloroquine | 70 | 3–12 h | 800 | 40 days | Renal |
3.2.2. Mechanism of action
Chloroquine and hydroxychloroquine are distinct in terms of serum concentration required to produce toxicity, as chloroquine produces lethal effects at approximately 25% of the serum concentration of hydroxychloroquine [45]. However, both drugs have similar mechanisms of action. Aminoquinolines are pharmacologically diverse with activity on many distinct organ systems, cellular receptor sites, and intracellular organelles. This versatility contributes to the myriad uses of aminoquinolines from antimalarial prophylaxis to immunomodulation [51]. Most acutely lethal in cases of toxicity is the ability of aminoquinolines to inhibit myocardial sodium and potassium channels [52]. They behave as class IA antiarrhythmics with “Quinidine-like” effects, decreasing inotropy and producing characteristic electrocardiographic (ECG) changes [52]. Aminoquinolines also cause α1-adrenergic receptor blockade with loss of vascular sympathetic tone and resultant hypotension [52]. Finally, aminoquinolines have the ability to bind to and inhibit ATP-dependent potassium channels on pancreatic β-cells leading to a similar mechanism of systemic release of insulin as is observed with sulfonylureas [53].
3.2.3. Toxicity by organ system
Acute aminoquinoline toxicity affects multiple organ systems. The following sections describe effects from acute and chronic toxicity. Many of the features of aminoquinoline toxicity are pertinent to ED care, particularly serum abnormalities and cardiac, respiratory, and neurologic phenomena. Others may occur following admission or discharge from the ED and become more relevant in the context of patient history, including otologic and ophthalmic sequelae. A summary of these findings is displayed in Table 2 .
Table 2.
Organ toxicity and symptomatology of quinine and aminoquinolines.
| Organ System | Acute Toxicity | Chronic Toxicity |
|---|---|---|
| Cardiovascular | Syncope Hypotension PR, QRS- and QT-interval prolongation Atrioventricular blocks Ventricular arrhythmias Torsades de pointes |
Cardiomyopathy Biatrial and/or biventricular enlargement Concentric hypertrophy with restrictive features |
| Serum Abnormalities | Hypoglycemia Hypokalemia |
|
| Central nervous system | Headache Confusion and delirium Tonic clonic seizures Hallucinations Ataxia |
Extrapyramidal effects |
| Respiratory | Impaired respiratory drive Hypoxia Pulmonary edema |
|
| Auditory | Tinnitus Decreased hearing acuity Vestibular dysfunction |
Tinnitus Decreased hearing acuity Vestibular dysfunction |
| Ocular | Diplopia Loss of visual acuity and color perception Tunnel vision Mydriasis Scotomata Pupillary dilatation |
Retinal damage and vasospasm Maculopathy Blindness |
| Gastrointestinal | Nausea and vomiting Gastrointestinal irritation Diarrhea Drug induced liver injury |
|
| Musculoskeletal | Myopathy and weakness (proximal>distal) | Myopathy and weakness (proximal>distal) |
| Immunologic | Hypersensitivity reactions | |
| Hematologic | Thrombocytopenia Agranulocytosis Hemolysis in glucose-6-phophate dehydrogenase (G6PD) deficiency patients Disseminated intravascular coagulation |
3.2.4. Cardiotoxicity
Patient outcomes in acute toxicity depend on the degree of observed cardiovascular dysfunction [20,54]. Aminoquinolines produce multiple effects on cardiac electrical conduction via sodium and potassium channel inhibition and α1-adrenergic receptor antagonism as previously mentioned [20]. Similar to class I antiarrhythmics, aminoquinolines have a dose-dependent effect on the cardiac action potential, binding more avidly to ion channels and exerting greater sodium channel blockade [52]. The effect leads to the classic PR prolongation, QRS complex widening, and QT prolongation associated with toxicity [55]. Also similar to class IA antiarrhythmics is the dose-dependent ability of aminoquinolines to bind and inhibit the action of potassium channels. As potassium is responsible for myocyte repolarization, potassium channel blockade delays repolarization. Clinically, this produces additional QT prolongation and predisposes to torsades de pointes (TdP) [52]. Delay of repolarization is greatest at slower heart rates [52].
Acute cardiac toxicity manifests as conduction blocks involving the atrioventricular junction and His-Purkinje system and ECG changes with prolongation in PR, QRS, and QT intervals [11,52]. Following overdose, these abnormalities can be profound, with reports of corrected QT (QTc) intervals of 563 milliseconds (ms) and 600 ms in case reports detailing oral hydroxychloroquine overdoses of 36 g and 22 g, respectively [42]. Dysrhythmias are typically present in moderate to severe toxicity [52,56]. Patients with underlying prolonged QTc from structural heart disease, congenital long-QT syndromes, electrolyte disturbances, renal failure, and/or use of additional QT prolonging medications are at heightened risk for development of dysrhythmias including TdP [56,57]. Hydroxychloroquine induced conduction delay often presents as a progression from a singular fascicular block to bundle branch block, followed by third-degree AV block [58]. Secondary to α1-adrenergic blockade, acutely toxic patients present with hypotension, which in addition to dysrhythmias may cause presyncope or syncope [59].
While unlikely to occur in acute overdose, cardiomyopathy is described in case reports of patients presenting with chronic chloroquine and/or hydroxychloroquine toxicity [60,61]. Aminoquinoline-induced cardiomyopathy is believed to result from lysosomal dysfunction and toxic phospholipid accumulation in cardiomyocytes [61]. Aminoquinoline-related cardiomyopathy has been reported with findings of biatrial and/or biventricular enlargement as well as concentric hypertrophy with restrictive features [62]. Chronic exposure to cumulative doses of 1277 g and 1843 g of chloroquine and hydroxychloroquine, respectively, over an average of 13 years has been demonstrated to produce this effect [63]. Risk of development is greater in patients with underlying heart failure or structural heart defects. Sequelae of drug-induced cardiomyopathy include acute and chronic heart failure, recurrent syncopal episodes, and newly developed conduction disorders [52,55].
3.2.5. Serum abnormalities
Plasma potassium levels vary inversely with the degree of blood chloroquine concentrations [11,64,65]. Hypokalemia is invariably present in overdose, and the extent of hypokalemia is an indicator of the severity of overdose [54,64]. Treatment-refractory hypokalemia is often one of the most challenging features following acute intoxication and is associated with cardiac manifestations including dysrhythmias [64,66]. Case reports from acute overdose report serum potassium concentrations of 2.5–2.7 mEq/L despite management with up to 280 mEq of potassium chloride [66]. The mechanism underlying hypokalemia is believed to be due to an intracellular shift of potassium as opposed to total body depletion, as aminoquinolines cause blockade of potassium channels on the pancreatic β-cells [42,64,67]. Similar to the mechanism of action of sulfonylureas, hyperinsulinism can produce additional serum abnormalities of hypoglycemia, particularly in patients with underlying metabolic derangements [68,69].
3.2.6. Neurologic sequelae
Central nervous system (CNS) effects are common with quinine, though incidence is much lower in aminoquinoline derivatives [70]. A variety of neurological effects have been reported, including sensorineural hearing loss, confusion, generalized seizures, dizziness, headaches, hallucinations, CNS depression, and ataxia. Rarely, extrapyramidal effects can be observed and include trismus, coarse tremors, and involuntary movements [71].
3.2.7. Respiratory effects
Aminoquinolines can suppress the respiratory drive, causing significant hypoxemia and hypercarbia in severe toxicity [65]. The mechanism underlying respiratory depression may be related to sodium channel blockade of aminoquinolines on the respiratory control centers [72,73]. Pulmonary edema has also been observed following acute intoxication and is believed to be due to the negative inotropic effects of aminoquinolines [74,75]. Although severe respiratory depression is rare, the combination of altered mentation, nausea, and vomiting presents significant aspiration risk.
3.2.8. Ototoxicity
While aminoquinolines are less likely than quinine to cause the cinchonism toxidrome consisting of headache, tinnitus, and sensorineural hearing loss, both single doses and chronic use can produce ototoxicity [76]. Hearing loss is typically bilateral, mild to moderate, and may be accompanied by vestibular dysfunction including dizziness and vertigo. In chronic use, these adverse events have been shown to be reversible in some cases with drug cessation. In acute overdose, ototoxicity often resolves within 48 to 72 h [77]. Toxicity occurs via a multifactorial mechanism involving oxidative stress, ischemic damage, and potassium channel inhibition in outer cochlear hair cells leading to hearing loss and vertigo [70,77,78]. Loss of balance, sensorineural hearing loss, and ataxia are believed to be related to vestibular dysfunction [79,80].
3.2.9. Ocular toxicity
Ophthalmologic sequelae of acute aminoquinoline intoxication include diplopia, loss of visual acuity, tunnel vision, mydriasis, and scotomata [81]. Onset of ocular symptoms often follows other clinical presentations, such as arrhythmia or hypotension by several hours. Vision improvement may occur rapidly or have a protracted recovery course of months following exposure [81]. Retinal toxicity has been reported at higher cumulative aminoquinoline doses, most often seen with chronic use. Following cumulative doses of 1000 g, the prevalence of retinal toxicity increases to 1% and is associated with an irreversible loss of vision despite cessation of the drug [82]. In some cases, progression of vision loss is present for up to one year after discontinuation of the offending agent. Vision loss is often bilateral and is characterized as a “bull's-eye” maculopathy and depigmentation of the retinal pigment epithelium (RPE) [83]. This begins in the central visual fields, but with continued exposure leads to atrophy of the RPE and visual acuity loss. The mechanism underlying toxicity to the cells of the retina is believed to be multifactorial, including direct photoreceptor damage via alterations in metabolism and secondary effects due to the binding of aminoquinolines to the melanin cells within the RPE [83].
3.2.10. Gastrointestinal toxicity
As opposed to quinine, aminoquinoline toxicity is less commonly associated with acute onset of GI symptoms such as nausea, vomiting, and diarrhea. While these may occur in both acute toxicity and in chronic therapeutic use, there are no long-term GI sequelae [51]. Aminoquinoline-related nausea and vomiting is mediated both by direct gastric irritant effects and activation of emetic centers in the brain [84]. Symptoms are usually transient following acute intoxication or therapeutic doses [84]. Fewer than 1% of patients display an increase in transaminases following initiation of aminoquinolines [85]. Case reports of drug induced liver injury (DILI) have reported AST and ALT elevations of 399 IU/L and 285 IU/L, respectively, within eight hours of initial dosing [86,87]. However, in patients with underlying liver disease or porphyria cutanea tarda, DILI has been reported in up to 50% of cases, and observed transaminitis may be much more severe [86,87]. In the majority of cases, transaminases returned to baseline following drug discontinuation [85,86].
3.2.11. Myotoxicity
Similar to the mechanism underlying aminoquinoline-induced cardiomyopathy, lysosomal dysfunction with vacuolar accumulation of metabolic products is believed to play a role in skeletal muscle toxicity [21]. Clinically, myopathy tends to be mild when symptomatic and affects the proximal muscles to a greater degree than distal groups, presenting as weakness [88]. While the incidence of chronic aminoquinoline use-induced myopathy is reportedly as high as 12.6%, it is believed to be higher due to two factors [86,87]. First, patient underreporting is likely, as elevations in creatine phosphokinase may be seen in patients even with normal strength testing. Second, myopathy may be difficult to distinguish from baseline, as myopathy-related pain and weakness are often associated with the rheumatologic diseases that these drugs are often prescribed to treat [88]. It is unknown if myopathy is dose-dependent, although myotoxicity progression has been observed with prolonged treatment (Table 2) [89].
3.2.12. Hematologic toxicity
Thrombocytopenia, agranulocytosis, and disseminated intravascular coagulation have been reported with aminoquinoline use [90]. Hemolytic anemia has also been reported with findings including jaundice, hemoglobinuria, and renal failure [90,91]. In patients with glucose-6-phosphate dehydrogenase (G6PD) deficiency, hemolysis can occur due to free radical accumulation in erythrocytes [91,92]. Due to a lack of reduced glutathione, oxidative stress denatures heme, causing extravascular hemolysis. The extent of hemolysis depends on the drug, dose, and the degree of enzyme deficiency, leading to a range of asymptomatic to life-threatening hemolysis [93]. Primaquine is more closely associated with G6PD-mediated hemolysis. Although case report literature describes the finding in chloroquine and hydroxychloroquine use, the largest chart review to date examining these drugs in patients with G6PD noted no occurrence of hemolysis [91,92].
3.3. Management considerations in acute poisoning
Gold-standard evidence such as randomized controlled trials, systematic reviews, or meta-analyses for management of aminoquinoline toxicity do not currently exist in the literature. The following recommendations are based on published expert opinion from poison control centers and medical toxicologists, as well as frequent findings described in case report literature. Consultation with a poison control center and/or medical toxicologist is recommended early in the management of these patients in the emergency department.
Aminoquinoline overdose produces toxicity ranging from mild to severe. Unlike with chloroquine overdoses, there is no established lethal or toxic dose of hydroxychloroquine in adults, and management should be tailored to observed toxicity [22]. Mild chloroquine toxicity in adults is defined as symptomatology occurring with suspected ingested dose <2 g, normal systolic blood pressure, and normal QRS (≤120 ms) [19]. Moderate chloroquine toxicity occurs with suspected ingested dose 2–4 g, normal systolic blood pressure, and normal QRS (≤120 ms) [19]. Severe chloroquine toxicity occurs with suspected ingested dose >4 g, hypotension, and QRS prolongation (>120 ms) [54]. Doses exceeding 5 g are highly associated with mortality due to arrhythmias and hypokalemia [94]. Treatment in the ED setting is focused on high-quality symptomatic and supportive measures, decontamination, stabilization of cardiac dysrhythmias if present, hemodynamic support, and electrolyte correction as necessary [22]. Indications for intensive care unit admission include persistent systemic hypotension, QRS elongation >120 ms, ventricular arrhythmias, seizures, coma, and persistent hypoglycemia [95]. Multiple reports cite early intubation and mechanical ventilation as critical for survival. The combination of altered mentation, apnea, and vomiting present in many aminoquinoline-intoxicated patients heightens the necessity for early and aggressive airway intervention to reduce aspiration risk. Given concerns for rapid potassium shifts in toxicity and repletion, an alternative to succinylcholine should be considered for rapid sequence induction and paralysis to avoid provoking rapid onset of hyperkalemia. Additionally, clinicians should avoid barbiturates for induction, as they may precipitate sudden cardiac arrest [96].
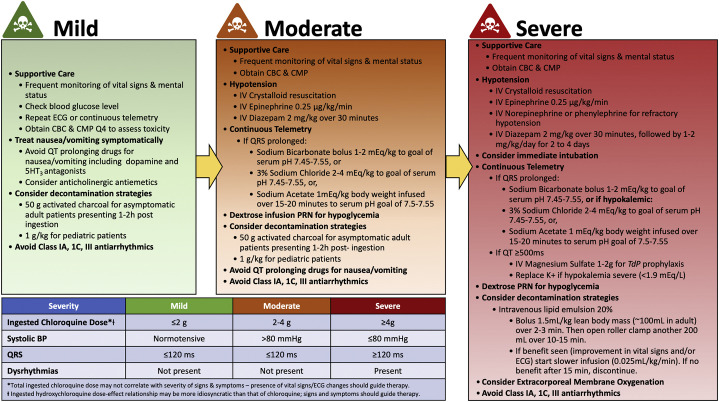
In the following sections, strategies for the emergency management of aminoquinoline intoxication will be addressed, including decontamination, pharmacotherapeutics, elimination methods, and emerging modalities (i.e. ECMO and ILE). Algorithmic application of these strategies to the categorization of mild, moderate, and severe toxicity is shown in Fig. 1 .
Fig. 1.
Adult algorithmic management of chloroquine and hydroxychloroquine overdose.
3.3.1. Decontamination
Hydroxychloroquine and chloroquine have high volumes of distribution and significant protein binding, complicating modalities for augmenting elimination [11]. Although these drugs are ingested, patients should not receive emetics such as syrup of ipecac, as toxicity sequelae of seizures, altered mentation, dysrhythmias, and hypotension heighten risks of aspiration [11]. Similarly, orogastric lavage has fallen out of favor due to the risks of aspiration. In cases of life threatening ingestion, orogastric lavage can be considered in patients presenting early following ingestion, within one hour [41,66]. Activated charcoal effectively absorbs aminoquinoline in the gastrointestinal tract with 95%–99% binding when administered in the first five minutes following ingestion [97]. As with other decontamination strategies, the use of activated charcoal will depend on patient presentation (i.e. those who are not nauseated or vomiting) and duration of intoxication [11]. While serum drug levels may be drawn, they are not readily available and therefore are not a practical measure to guide initial management of acute toxicity in the ED setting [74]. However, for inpatient treatment, early and serial measurements of blood chloroquine concentrations are more accurate compared to estimated oral ingestion for predicting cardiovascular severity of chloroquine poisonings [98]. High serum chloroquine concentrations have been reported for 8–10 days despite resolution of clinical symptoms within two days [95].
3.3.2. Pharmacotherapeutics
Addressing electrolyte abnormalities, dysrhythmias, and blood pressure are the main role of pharmacotherapeutics in the management of aminoquinoline overdose. Hypoglycemia should be managed with dextrose infusion, with careful attention paid to the serum potassium and QT interval. Refractory cases with intractable hypoglycemia (glucose <50 mg/dL) can be managed similar to sulfonylurea toxicity with 50 μg subcutaneous octreotide every 6 h [95,99]. Hypokalemia is a marker of severity of toxicity in acute poisoning and must be carefully monitored and managed as intracellular shifts can reverse as acute toxicity resolves, with rapid onset of hyperkalemia [11]. Potassium may be repleted cautiously in severe hypokalemia (<1.9 mEq/L), and monitoring of potassium levels should occur regularly. While older studies indicate that hypokalemia may prolong survival, contemporary data favor potassium repletion, generally to >4 mEq/L. [64] Dysrhythmias resulting from electrolyte derangements including potassium should be rapidly but carefully corrected [11]. Class IA, IC, and III antiarrhythmics should be avoided as they may worsen conduction delays [11]. Magnesium sulfate 2 g IV over 10 min may be used for TdP treatment, but it has an unclear role in prophylaxis for QT prolongation ≥500 ms. [100] Potassium repletion to achieve serum concentration between 4.7 and 5.2 mEq/L has demonstrated efficacy in shortening QT interval [101].
For hypotension, supportive care with appropriate crystalloid resuscitation should be used [20,74]. In severe toxicity, hypotension may be refractory to fluid bolus, and vasopressors should be utilized [20,102]. Epinephrine is the vasopressor of choice in these patients, given the intrinsic negative inotropic effect in aminoquinoline overdose (combination of a α1 and β1 adrenergic receptor blockade) [20]. The literature base supports high-dose epinephrine as the pressor of choice at a starting dose of 0.25 μg/kg/min increased by 0.25 μg/kg/min increments targeting a mean arterial pressure of 65 mmHg [20]. However, epinephrine may exacerbate pre-existing hypokalemia. A study of severely poisoned patients found the addition of high-dose epinephrine to mechanical ventilation increased survival from 9% to 91% [20]. If epinephrine fails to adequately raise mean arterial pressure, a second pressor such as norepinephrine or phenylephrine can be titrated to effect, though alpha agonists increase the effective refractory period and may increase the occurrence of arrythmias [103,104]. If hypotension is due to myocardial depression rather than arterial vasodilation, these vasoactive medications may worsen cardiac output [104]. Patients requiring additional vasopressor support beyond epinephrine and diazepam should receive close attention to hemodynamic parameters to ensure treatment efficacy.
Diazepam is used in the management of both hypotension and dysrhythmias in dosages of 2 mg/kg IV over 30 min, followed by 1 to 2 mg/kg/d for 2–4 days in severe cases [51]. The mechanism of diazepam in attenuation of cardiotoxicity is believed to be due to a central antagonistic effect, anticonvulsant effect, antidysrhythmic effect and interaction inverse to aminoquinolines, and decrease aminoquinoline induced-vasodilation [22,105,106]. Experimental use of diazepam in animal models of severe chloroquine overdose demonstrates improved systolic and diastolic arterial pressures, heart rate, urine volume, urinary excretion of chloroquine, and shortened QRS duration [102,107]. No studies have compared efficacy between different benzodiazepines for treatment of acute aminoquinoline toxicity. With medication shortages or variation in ED pharmacy stock, another benzodiazepine may be substituted for treatment of seizures and for maintenance of sedation.
Gastrointestinal symptoms, such as nausea, vomiting, and diarrhea, can be found in mildly intoxicated patients and more severe overdoses. Vomiting in early stages of intoxication may be due to direct irritant effects of aminoquinolines and may be better managed with the decontamination strategies addressed above. Nausea and vomiting can be treated symptomatically while avoiding QTc prolonging agents such as serotonin antagonists (ondansetron) and phenothiazines (promethazine, prochlorperazine) [108]. Antihistamine (meclizine) and dopamine receptor antagonist (metoclopramide) antiemetics may be safer options.
There are currently no accepted treatments for quinine-induced ocular toxicity, but fundoscopic examination, visual field examination, and color testing are appropriate to assess injury ideally by an ophthalmologist [19]. Hyperbaric oxygen has been used successfully in vision recovery, but causality was not established [109].
3.3.3. Elimination methods
To address sodium channel blockade, sodium loading with sodium bicarbonate (NaHCO3), sodium acetate, or hypertonic saline (3% NaCl) may be used [11]. Consideration should be given to the degree of cardiac toxicity and severity of hypokalemia if present, favoring use of sodium acetate or hypertonic saline to avoid worsening hypokalemia. The pH can be used as an indirect indicator of sodium load. When using NaHCO3, a bolus of 1–2 mEq/kg is recommended, repeated as needed to terminate dysrhythmias or narrow QRS complex, followed by a NaHCO3 infusion [11]. When using sodium acetate, 1 mEq/kg body weight may be infused over 15–20 min as a bolus [110]. Potassium should be closely monitored for intracellular shifting of potassium with development of clinically significant hypokalemia. Hypertonic saline contains the same quantity of sodium in 97 mEq as sodium bicarbonate in 50 mEq. When using 3% NaCl, a bolus of 2–4 mEq/kg may be considered, and sodium levels should be closely monitored [111]. Approximately 50% of chloroquine is excreted renally, and acute renal failure is possible following acute intoxication [112]. Providers should anticipate the possibility of extended toxicity course in patients with acute and/or chronic renal failure. Unfortunately, hemodialysis use has been reported as ineffective due to high protein binding and large volume of distribution intrinsic to the aminoquinolines [112]. Case report evidence suggests hemodialysis efficacy can be augmented by use of ILE [22].
3.3.4. Novel modalities for aminoquinoline toxicity management
There are multiple reports of veno-arterial ECMO to successfully treat aminoquinoline toxicity [98,[113], [114], [115], [116]]. ECMO may be considered in severe toxicity refractory to standard supportive care and other therapies (i.e. escalation of epinephrine drip rate to >3 mg/h, persistent end-organ failure). One case report describes ECMO initiation on intensive care unit admission following a 9.5 g chloroquine ingestion (initial blood chloroquine concentration 6215 μg/L). The patient presented with altered mental status, left ventricular systolic dysfunction with a dyskinetic interventricular septum, and hypotension unresponsive to crystalloid fluid resuscitation as well as 3 mg/h epinephrine infusion. The patient was weaned from vasopressors on day three, decannulated from ECMO on day four, extubated on day seven, and discharged on day ten with no neurological sequelae [117]. Another case detailing ECMO use in a patient experiencing ventricular fibrillation following 12 g hydroxychloroquine overdose noted “spectacular improvement of hemodynamic parameters and electrocardiographic normalization at day one.” [114]
Owing to the lipophilicity of aminoquinolines, there are several reports of successful outcomes following ILE use [22,46,118,119]. Recommended ILE treatment is 1.5 mL/kg lean body mass (~100 mL in adults) as bolus over two to three minutes followed by 200 mL over 10–15 min [22]. If benefit is seen in vital signs and/or ECG parameter normalization, slower continuous infusion of ~0.25 mL/kg/min can be administered until resolution of toxicity [119]. Combined ILE, NaHCO3, and vasopressor support has been reported in profound hydroxychloroquine overdose of 40 g presenting with hypokalemia and refractory ventricular fibrillation with positive outcome [22]. Protracted ILE has been associated with dysfunction of ECMO circuits, though this is unlikely in short-term ILE use (<24 h continuous infusion), and case reports have described safe concomitant use of both modalities [118,120]. Serum triglyceride levels may be monitored to guide ILE extent of infusion, with ~1000 mg/dL as a lipid volume limit of efficacy [121].
4. Conclusions
Given the wide publicity in the lay media regarding the use of aminoquinolines for COVID-19 and trends in national poison control center data, a more current exploration of the acute management of aminoquinoline toxicity is necessary. This class of drugs has a narrow therapeutic range and a large variance in toxic dose from person to person. Severe symptoms can occur with doses as small as 1.5 g with onset one to three hours post-ingestion. Management of acute toxicity often occurs in the emergency department and should focus on hemodynamic stabilization with the use of early mechanical ventilation, diazepam, epinephrine, frequent ECGs, and repeated blood glucose monitoring, with early step-up to aggressive resuscitative measures including ECMO to support vital functions until the offending agent is metabolized and cleared.
Declaration of Competing Interest
None.
Acknowledgements
All authors conceived the idea for this manuscript and contributed substantially to the writing and editing of the review. This manuscript did not utilize any grants, and it has not been presented in abstract form. This clinical review has not been published, it is not under consideration for publication elsewhere, its publication is approved by all authors and tacitly or explicitly by the responsible authorities where the work was carried out, and that, if accepted, it will not be published elsewhere in the same form, in English or in any other language, including electronically without the written consent of the copyright-holder. This review does not reflect the views or opinions of the U.S. government, Department of Defense, U.S. Army, U.S. Air Force, or SAUSHEC EM Residency Program.
References
- 1.Browning D.J. Hydroxychloroquine and chloroquine retinopathy. 2014. Pharmacology of chloroquine and hydroxychloroquine; pp. 35–63. [Google Scholar]
- 2.Cortegiani A., Ingoglia G., Ippolito M., Giarratano A., Einav S. A systematic review on the efficacy and safety of chloroquine for the treatment of COVID-19. J Crit Care. 2020;57:279–283. doi: 10.1016/j.jcrc.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen Z., Hu J., Zhang Z. Efficacy of hydroxychloroquine in patients with COVID-19: results of a randomized clinical trial. medRxiv. 2020 Pre-print article, 2020.2003.2022.20040758. [Google Scholar]
- 4.Duan Y.J., Liu Q., Zhao S.Q. The trial of chloroquine in the treatment of corona virus disease 2019 (COVID-19) and its research progress in forensic toxicology. Fa Yi Xue Za Zhi. 2020;36(2) doi: 10.12116/j.issn.1004-5619.2020.02.002. [DOI] [PubMed] [Google Scholar]
- 5.Liu J., Cao R., Xu M. Hydroxychloroquine, a less toxic derivative of chloroquine, is effective in inhibiting SARS-CoV-2 infection in vitro. Cell Discovery. 2020;6(1):16. doi: 10.1038/s41421-020-0156-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jean S.-S., Lee P.-I., Hsueh P.-R. Treatment options for COVID-19: The reality and challenges. Journal of Microbiology, Immunology and Infection. 2020;53(3):436–443. doi: 10.1016/j.jmii.2020.03.034. ISSN 1684-1182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.FDA . 2020. FDA letter to stakeholders: do not use chloroquine phosphate intended for fish as treatment for COVID-19 in humans. [Google Scholar]
- 8.Busara S. CNN. 2020. Nigeria records chloroquine poisoning after Trump endorses it for coronavirus treatment. [Google Scholar]
- 9.Communiqué de presse - Coronavirus : point de situation en Nouvelle-Aquitaine du 29/03/2020 [press release]. Nouvelle-Aquitaine, France. 2020. [Google Scholar]
- 10.National Poison Data System (NPDS) Bulletin COVID-19 (Hydroxychloroquine/Chloroquine) [press release] American Association of Poison Control Centers; 2020. [Google Scholar]
- 11.Marquardt K., Albertson T.E. Treatment of hydroxychloroquine overdose. Am J Emerg Med. 2001;19(5):420–424. doi: 10.1053/ajem.2001.25774. [DOI] [PubMed] [Google Scholar]
- 12.Gummin D.D., Mowry J.B., Spyker D.A. 2018 annual report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 36th annual report. Clin Toxicol. 2019;57(12):1220–1413. doi: 10.1080/15563650.2019.1677022. [DOI] [PubMed] [Google Scholar]
- 13.Gummin D.D., Mowry J.B., Spyker D.A., Brooks D.E., Osterthaler K.M., Banner W. 2017 annual report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 35th annual report. Clin Toxicol. 2018;56(12):1213–1415. doi: 10.1080/15563650.2018.1533727. [DOI] [PubMed] [Google Scholar]
- 14.Gummin D.D., Mowry J.B., Spyker D.A., Brooks D.E., Fraser M.O., Banner W. 2016 annual report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 34th annual report. Clin Toxicol. 2017;55(10):1072–1254. doi: 10.1080/15563650.2017.1388087. [DOI] [PubMed] [Google Scholar]
- 15.Mowry J.B., Spyker D.A., Brooks D.E., Zimmerman A., Schauben J.L. 2015 annual report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 33rd annual report. Clin Toxicol (Phila) 2016;54(10):924–1109. doi: 10.1080/15563650.2016.1245421. [DOI] [PubMed] [Google Scholar]
- 16.Mowry J.B., Spyker D.A., Brooks D.E., McMillan N., Schauben J.L. 2014 annual report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 32nd annual report. Clin Toxicol (Phila) 2015;53(10):962–1147. doi: 10.3109/15563650.2015.1102927. [DOI] [PubMed] [Google Scholar]
- 17.Mowry J.B., Spyker D.A., Cantilena L.R., Jr., McMillan N., Ford M. 2013 annual report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 31st annual report. Clin Toxicol (Phila) 2014;52(10):1032–1283. doi: 10.3109/15563650.2014.987397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mowry J.B., Spyker D.A., Cantilena L.R., Jr., Bailey J.E., Ford M. 2012 annual report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 30th annual report. Clin Toxicol (Phila) 2013;51(10):949–1229. doi: 10.3109/15563650.2013.863906. [DOI] [PubMed] [Google Scholar]
- 19.Stokkermans T.J., Trichonas G. 2020. Chloroquine and hydroxychloroquine toxicity. In: StatPearls. Treasure Island (FL) [PubMed] [Google Scholar]
- 20.Riou B., Barriot P., Rimailho A., Baud F.J. Treatment of severe chloroquine poisoning. N Engl J Med. 1988;318(1):1–6. doi: 10.1056/NEJM198801073180101. [DOI] [PubMed] [Google Scholar]
- 21.Jordan P., Brookes J.G., Nikolic G., Le Couteur D.G., Le Couteur D. Hydroxychloroquine overdose: toxicokinetics and management. J Toxicol Clin Toxicol. 1999;37(7):861–864. doi: 10.1081/clt-100102466. [DOI] [PubMed] [Google Scholar]
- 22.McBeth P.B., Missirlis P.I., Brar H., Dhingra V. Novel therapies for myocardial irritability following extreme hydroxychloroquine toxicity. Case Rep Emerg Med. 2015;2015:692948. doi: 10.1155/2015/692948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liu J., Cao R., Xu M. Hydroxychloroquine, a less toxic derivative of chloroquine, is effective in inhibiting SARS-CoV-2 infection in vitro. Cell Discovery. 2020;6(1) doi: 10.1038/s41421-020-0156-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Al-Bari M.A.A. Chloroquine analogues in drug discovery: new directions of uses, mechanisms of actions and toxic manifestations from malaria to multifarious diseases. Journal of Antimicrobial Chemotherapy. 2015;70(6):1608–1621. doi: 10.1093/jac/dkv018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Savarino A., Boelaert J.R., Cassone A., Majori G., Cauda R. Effects of chloroquine on viral infections: an old drug against today’s diseases? Lancet Infect Dis. 2003;3(11):722–727. doi: 10.1016/S1473-3099(03)00806-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vincent M.J., Bergeron E., Benjannet S. Chloroquine is a potent inhibitor of SARS coronavirus infection and spread. Virol J. 2005;2:69. doi: 10.1186/1743-422X-2-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. Jama. 2020;323(13):1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 28.Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;20(5):533–534. doi: 10.1016/S1473-3099(20)30120-1. https://pubmed.ncbi.nlm.nih.gov/32087114/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tortorici M.A., Veesler D. Chapter Four - Structural insights into coronavirus entry. In: Rey F.A., editor. Advances in Virus Research. vol 105. Academic Press; 2019. pp. 93–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hulswit R.J.G., Lang Y., Bakkers M.J.G. Human coronaviruses OC43 and HKU1 bind to 9-O-acetylated sialic acids via a conserved receptor-binding site in spike protein domain a. Proc Natl Acad Sci. 2019;116(7):2681–2690. doi: 10.1073/pnas.1809667116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hoffmann M., Kleine-Weber H., Schroeder S. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181(2):271–280.e8. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Devaux C.A., Rolain J.-M., Colson P., Raoult D. New insights on the antiviral effects of chloroquine against coronavirus: what to expect for COVID-19? Int J Antimicrob Agents. 2020;105938 doi: 10.1016/j.ijantimicag.2020.105938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Colson P., Rolain J.-M., Raoult D. Chloroquine for the 2019 novel coronavirus SARS-CoV-2. Int J Antimicrob Agents. 2020;55(3):105923. doi: 10.1016/j.ijantimicag.2020.105923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gao J., Tian Z., Yang X. Breakthrough: Chloroquine phosphate has shown apparent efficacy in treatment of COVID-19 associated pneumonia in clinical studies. Biosci Trends. 2020;14(1):72–73. doi: 10.5582/bst.2020.01047. [DOI] [PubMed] [Google Scholar]
- 35.Mehra M.R., Desai S.S., Ruschitzka F., Patel A.N. Hydroxychloroquine or chloroquine with or without a macrolide for treatment of COVID-19: a multinational registry analysis. The Lancet. 2020 doi: 10.1016/S0140-6736(20)31180-6. [published online ahead of print, 2020 May 22] [retracted in: Lancet. 2020 Jun 5;:null], S0140-6736(20)31180-6. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 36.Mehra M.R., Ruschitzka F., Patel A.N. Retraction-Hydroxychloroquine or chloroquine with or without a macrolide for treatment of COVID-19: a multinational registry analysis. Lancet (London, England) 2020;395(10240):1820. doi: 10.1016/S0140-6736(20)31324-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Geleris J., Sun Y., Platt J. Observational study of hydroxychloroquine in hospitalized patients with Covid-19. New England Journal of Medicine. 2020;382(25):2411–2418. doi: 10.1056/NEJMoa2012410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Borba M.G.S., FdA Val, Sampaio V.S. Chloroquine diphosphate in two different dosages as adjunctive therapy of hospitalized patients with severe respiratory syndrome in the context of coronavirus (SARS-CoV-2) infection: Preliminary safety results of a randomized, double-blinded, phase IIb clinical trial (CloroCovid-19 Study) medRxiv. 2020 [Pre-print], 2020.2004.2007.20056424. [Google Scholar]
- 39.Magagnoli J., Narendran S., Pereira F. Outcomes of hydroxychloroquine usage in United States veterans hospitalized with Covid-19. medRxiv. 2020 doi: 10.1016/j.medj.2020.06.001. [published online ahead of print, 2020 Jun 5], 2020.2004.2016.20065920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Food and Drug Administration . 2020. Remdesivir by Gilead Sciences: FDA Warns of Newly Discovered Potential Drug Interaction That May Reduce Effectiveness of Treatment [press release] [Google Scholar]
- 41.Yanturali S., Aksay E., Demir OF, Atilla R. Massive hydroxychloroquine overdose. Acta Anaesthesiol Scand. 2004;48(3):379–381. doi: 10.1111/j.0001-5172.2004.0302.x. [DOI] [PubMed] [Google Scholar]
- 42.de Olano J., Howland M.A., Su M.K., Hoffman R.S., Biary R. Toxicokinetics of hydroxychloroquine following a massive overdose. Am J Emerg Med. 2019;37(12) doi: 10.1016/j.ajem.2019.158387. 2264.e2265–2264.e2268. [DOI] [PubMed] [Google Scholar]
- 43.Furst D.E. Pharmacokinetics of hydroxychloroquine and chloroquine during treatment of rheumatic diseases. Lupus. 1996;5(1_suppl):11–15. [PubMed] [Google Scholar]
- 44.Warhurst D.C., Steele J.C., Adagu I.S., Craig J.C., Cullander C. Hydroxychloroquine is much less active than chloroquine against chloroquine-resistant plasmodium falciparum, in agreement with its physicochemical properties. J Antimicrob Chemother. 2003;52(2):188–193. doi: 10.1093/jac/dkg319. [DOI] [PubMed] [Google Scholar]
- 45.Chloroquine and related agents. In: POISINDEX® System (electronic version). Truven Health Analytics AA, MI. Available at. http://www.micromedexsolutions.com/ (Accessed 3/25/20)
- 46.Ten Broeke R., Mestrom E., Woo L., Kreeftenberg H. Early treatment with intravenous lipid emulsion in a potentially lethal hydroxychloroquine intoxication. Neth J Med. 2016;74(5):210–214. [PubMed] [Google Scholar]
- 47.Kim K.A., Park J.Y., Lee J.S., Lim S. Cytochrome P450 2C8 and CYP3A4/5 are involved in chloroquine metabolism in human liver microsomes. Arch Pharm Res. 2003;26(8):631–637. doi: 10.1007/BF02976712. [DOI] [PubMed] [Google Scholar]
- 48.Rainsford K.D., Parke A.L., Clifford-Rashotte M., Kean W.F. Therapy and pharmacological properties of hydroxychloroquine and chloroquine in treatment of systemic lupus erythematosus, rheumatoid arthritis and related diseases. Inflammopharmacology. 2015;23(5):231–269. doi: 10.1007/s10787-015-0239-y. [DOI] [PubMed] [Google Scholar]
- 49.Furst D.E. Pharmacokinetics of hydroxychloroquine and chloroquine during treatment of rheumatic diseases. Lupus. 1996;5(Suppl. 1):S11–S15. [PubMed] [Google Scholar]
- 50.Salako L.A., Walker O., Iyun A.O. Pharmacokinetics of chloroquine in renal insufficiency. Afr J Med Med Sci. 1984;13(3–4):177–182. [PubMed] [Google Scholar]
- 51.Plantone D., Koudriavtseva T. Current and future use of chloroquine and hydroxychloroquine in infectious, immune, neoplastic, and neurological diseases: a mini-review. Clin Drug Investig. 2018;38(8):653–671. doi: 10.1007/s40261-018-0656-y. [DOI] [PubMed] [Google Scholar]
- 52.Chatre C., Roubille F., Vernhet H., Jorgensen C., Pers Y.M. Cardiac complications attributed to chloroquine and hydroxychloroquine: a systematic review of the literature. Drug Saf. 2018;41(10):919–931. doi: 10.1007/s40264-018-0689-4. [DOI] [PubMed] [Google Scholar]
- 53.Davis T.M.E. Antimalarial drugs and glucose metabolism. Br J Clin Pharmacol. 1997;44(1):1–7. doi: 10.1046/j.1365-2125.1997.00597.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Clemessy J.L., Angel G., Borron S.W. Therapeutic trial of diazepam versus placebo in acute chloroquine intoxications of moderate gravity. Intensive Care Med. 1996;22(12):1400–1405. doi: 10.1007/BF01709558. [DOI] [PubMed] [Google Scholar]
- 55.Page R.L., O’Bryant C.L., Cheng D. Drugs that may cause or exacerbate heart failure. Circulation. 2016;134(6):e32–e69. doi: 10.1161/CIR.0000000000000426. [DOI] [PubMed] [Google Scholar]
- 56.Simpson T.F., Salazar J.W., Vittinghoff E. Association of QT-prolonging medications with risk of autopsy-defined causes of sudden death. JAMA Intern Med. 2020;180(5):1–9. doi: 10.1001/jamainternmed.2020.0148. [published online ahead of print, 2020 Mar 2] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57."The Cardiotoxicity of Antimalarials." World Health Organization- Malaria Policy Advisory Committee Meeting. 22 Mar. www.who.int/malaria/mpac/mpac-mar2017-erg-cardiotoxicity-report-session2.pdf
- 58.Tönnesmann E., Kandolf R., Lewalter T. Chloroquine cardiomyopathy-a review of the literature. Immunopharmacol Immunotoxicol. 2013;35 doi: 10.3109/08923973.2013.780078. [DOI] [PubMed] [Google Scholar]
- 59.Ajayi A.A., Adigun A.Q. Syncope following oral chloroquine administration in a hypertensive patient controlled on amlodipine. Br J Clin Pharmacol. 2002;53(4):404–405. doi: 10.1046/j.1365-2125.2002.01572-2.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Muthukrishnan P., Roukoz H., Grafton G., Jessurun J., Colvin-Adams M. Hydroxychloroquine-Induced Cardiomyopathy. Circulation: Heart Failure. 2011;4(2) doi: 10.1161/CIRCHEARTFAILURE.110.959916. [DOI] [PubMed] [Google Scholar]
- 61.Costedoat-Chalumeau N., Hulot J.-S., Amoura Z. Cardiomyopathy related to antimalarial therapy with illustrative case report. Cardiology. 2007;107(2):73–80. doi: 10.1159/000094079. [DOI] [PubMed] [Google Scholar]
- 62.Joyce E., Fabre A., Mahon N. Hydroxychloroquine cardiotoxicity presenting as a rapidly evolving biventricular cardiomyopathy: key diagnostic features and literature review. Eur Heart J Acute Cardiovasc Care. 2013;2(1):77–83. doi: 10.1177/2048872612471215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Yogasundaram H., Putko B.N., Tien J. Hydroxychloroquine-induced cardiomyopathy: case report, pathophysiology, diagnosis, and treatment. Can J Cardiol. 2014;30(12):1706–1715. doi: 10.1016/j.cjca.2014.08.016. [DOI] [PubMed] [Google Scholar]
- 64.Clemessy J.L., Favier C., Borron S.W., Hantson P.E., Vicaut E., Baud F.J. Hypokalaemia related to acute chloroquine ingestion. Lancet. 1995;346(8979):877–880. doi: 10.1016/s0140-6736(95)92711-5. [DOI] [PubMed] [Google Scholar]
- 65.Jaeger A., Sauder P., Kopferschmitt J., Flesch F. Clinical features and management of poisoning due to antimalarial drugs. Med Toxicol Adverse Drug Exp. 1987;2(4):242–273. doi: 10.1007/BF03259868. [DOI] [PubMed] [Google Scholar]
- 66.Fanelli N., Arnold J., Anwar M., Lopez G., Kazzi Z. Persistent hypokalemia despite aggressive potassium replacement following a hydroxychloroquine overdose. Clin Toxicol. 2015;53(7) 727-727. [Google Scholar]
- 67.Limburg P.J., Katz H., Grant C.S., Service FJ Quinine-induced hypoglycemia. Ann Intern Med. 1993;119(3):218–219. doi: 10.7326/0003-4819-119-3-199308010-00007. [DOI] [PubMed] [Google Scholar]
- 68.Winter E.M., Schrander-van der Meer A., Eustatia-Rutten C., Janssen M. Hydroxychloroquine as a glucose lowering drug. BMJ Case Rep. 2011;2011 doi: 10.1136/bcr.06.2011.4393. bcr0620114393. Published 2011 Oct 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Goyal V., Bordia A. The hypoglycemic effect of chloroquine. J Assoc Physicians India. 1995;43(1):17–18. [PubMed] [Google Scholar]
- 70.Parmar R.C., Valvi C.V., Kamat J.R., Vaswani R.K. Chloroquine induced parkinsonism. J Postgrad Med. 2000;46(1):29–30. [PubMed] [Google Scholar]
- 71.Phillips-Howard P.A., ter Kuile F.O. CNS adverse events associated with antimalarial agents. Fact or fiction? Drug Saf. 1995;12(6):370–383. doi: 10.2165/00002018-199512060-00003. [DOI] [PubMed] [Google Scholar]
- 72.Mapfumo Chinyanga H., Vartanian G.A. Specific influence of chloroquine on central respiratory mechanisms. Eur J Pharmacol. 1973;22(1):83–90. doi: 10.1016/0014-2999(73)90187-8. [DOI] [PubMed] [Google Scholar]
- 73.Di Grande A., Giuffrida C., Narbone G. Management of sodium-channel blocker poisoning: the role of hypertonic sodium salts. Eur Rev Med Pharmacol Sci. 2010;14(1):25–30. [PubMed] [Google Scholar]
- 74.Clemessy J.L., Taboulet P., Hoffman J.R. Treatment of acute chloroquine poisoning: a 5-year experience. Crit Care Med. 1996;24(7):1189–1195. doi: 10.1097/00003246-199607000-00021. [DOI] [PubMed] [Google Scholar]
- 75.Ndiaye N., Petrognani R., Diatta B., Seck M., Theobald X., Adnet P. Chloroquine poisoning with respiratory distress and fatal outcome. Ann Fr Anesth Reanim. 1999;18(6):683–685. doi: 10.1016/s0750-7658(99)80157-9. [DOI] [PubMed] [Google Scholar]
- 76.Hadi U., Nuwayhid N., Hasbini A.S. Chloroquine ototoxicity: an idiosyncratic phenomenon. Otolaryngol Head Neck Surg. 1996;114(3):491–493. doi: 10.1016/s0194-5998(96)70226-7. [DOI] [PubMed] [Google Scholar]
- 77.Seçkin U., Ozoran K., Ikinciogullari A., Borman P., Bostan E.E. Hydroxychloroquine ototoxicity in a patient with rheumatoid arthritis. Rheumatol Int. 2000;19(5):203–204. doi: 10.1007/s002960000054. [DOI] [PubMed] [Google Scholar]
- 78.Malcangi G., Fraticelli P., Palmieri C., Cappelli M., Danieli M.G. Hydroxychloroquine-induced seizure in a patient with systemic lupus erythematosus. Rheumatol Int. 2000;20(1):31–33. doi: 10.1007/s002960000066. [DOI] [PubMed] [Google Scholar]
- 79.Chansky P.B., Werth V.P. Accidental hydroxychloroquine overdose resulting in neurotoxic vestibulopathy. BMJ Case Rep. 2017;2017 doi: 10.1136/bcr-2016-218786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Oliveira K.R.H.M., dos Anjos L.M., Araújo A.P.S. Ascorbic acid prevents chloroquine-induced toxicity in inner glial cells. Toxicol In Vitro. 2019;56:150–155. doi: 10.1016/j.tiv.2019.01.008. [DOI] [PubMed] [Google Scholar]
- 81.Browning D.J. Hydroxychloroquine and chloroquine retinopathy: screening for drug toxicity. Am J Ophthalmol. 2002;133(5):649–656. doi: 10.1016/s0002-9394(02)01392-2. [DOI] [PubMed] [Google Scholar]
- 82.Marmor M.F., Kellner U., Lai T.Y., Lyons J.S., Mieler W.F. Revised recommendations on screening for chloroquine and hydroxychloroquine retinopathy. Ophthalmology. 2011;118(2):415–422. doi: 10.1016/j.ophtha.2010.11.017. [DOI] [PubMed] [Google Scholar]
- 83.Yusuf I.H., Sharma S., Luqmani R., Downes S.M. Hydroxychloroquine retinopathy. Eye (Lond) 2017;31(6):828–845. doi: 10.1038/eye.2016.298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Tracy J.W. LW. Drugs used in the chemotherapy of protozoal infection: malaria. In: Hardman J.G., Limbird L.E., Molinoff P.B., editors. Goodman and Gilman’s the pharmacologic basis of Therapeutics. Vol 10. New York: McGraw-Hill. 2001. pp. 1059–1095. [Google Scholar]
- 85.van Jaarsveld C.H., Jahangier Z.N., Jacobs J.W. Toxicity of anti-rheumatic drugs in a randomized clinical trial of early rheumatoid arthritis. Rheumatology (Oxford) 2000;39(12):1374–1382. doi: 10.1093/rheumatology/39.12.1374. [DOI] [PubMed] [Google Scholar]
- 86.Mok M.Y., Ng W.L., Yuen M.F., Wong R.W., Lau C.S. Safety of disease modifying anti-rheumatic agents in rheumatoid arthritis patients with chronic viral hepatitis. Clin Exp Rheumatol. 2000;18(3):363–368. [PubMed] [Google Scholar]
- 87.Sunkara B., Roofeh D., Silver S., Pearson T.L., Ettel M., McCune W.J. The devil’s in the dosing: severe drug-induced liver injury in a hydroxychloroquine-naive patient with subacute cutaneous lupus erythematosus and porphyria cutanea tarda. Lupus. 2018;27(8):1383–1386. doi: 10.1177/0961203318768884. [DOI] [PubMed] [Google Scholar]
- 88.Casado E., Gratacós J., Tolosa C. Antimalarial myopathy: an underdiagnosed complication? Prospective longitudinal study of 119 patients. Ann Rheum Dis. 2006;65(3):385–390. doi: 10.1136/ard.2004.023200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Bolaños-Meade J., Zhou L., Hoke A., Corse A., Vogelsang G., Wagner K.R. Hydroxychloroquine causes severe vacuolar myopathy in a patient with chronic graft-versus-host disease. Am J Hematol. 2005;78(4):306–309. doi: 10.1002/ajh.20294. [DOI] [PubMed] [Google Scholar]
- 90.Sames E., Paterson H., Li C. Hydroxychloroquine-induced agranulocytosis in a patient with long-term rheumatoid arthritis. Eur J Rheumatol. 2016;3(2):91–92. doi: 10.5152/eurjrheum.2015.0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Braga C.B.E., Martins A.C., Cayotopa A.D.E. Side effects of chloroquine and primaquine and symptom reduction in malaria endemic area (Mâncio Lima, Acre, Brazil) Interdiscip Perspect Infect Dis. 2015;2015:346853. doi: 10.1155/2015/346853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Mohammad S., Clowse M.E.B., Eudy A.M., Criscione-Schreiber L.G. Examination of hydroxychloroquine use and hemolytic anemia in G6PDH-deficient patients. Arthritis Care Res (Hoboken) 2018;70(3):481–485. doi: 10.1002/acr.23296. [DOI] [PubMed] [Google Scholar]
- 93.Nkhoma E.T., Poole C., Vannappagari V., Hall S.A., Beutler E. The global prevalence of glucose-6-phosphate dehydrogenase deficiency: a systematic review and meta-analysis. Blood Cells Mol Dis. 2009;42(3):267–278. doi: 10.1016/j.bcmd.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 94.Chary M.A., Barbuto A.F., Izadmehr S., Hayes B.D., Burns M.M. COVID-19: therapeutics and their toxicities. J Med Toxicol. 2020:1–11. doi: 10.1007/s13181-020-00777-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Jones A.L. Chloroquine and Quinine. In: Brent J., Burkhart K., Dargan P., Hatten B., Megarbane B., Palmer R., editors. Critical care toxicology. Springer International Publishing; Cham: 2016. pp. 1–16. [Google Scholar]
- 96.Meeran K., Jacobs M.G. Chloroquine poisoning. Rapidly fatal without treatment. Bmj. 1993;307(6895):49–50. doi: 10.1136/bmj.307.6895.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Kivisto K.T., Neuvonen P.J. Activated charcoal for chloroquine poisoning. BMJ. 1993;307(6911):1068. doi: 10.1136/bmj.307.6911.1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Mégarbane B., Bloch V., Hirt D. Blood concentrations are better predictors of chioroquine poisoning severity than plasma concentrations: a prospective study with modeling of the concentration/effect relationships. Clin Toxicol (Phila) 2010;48(9):904–915. doi: 10.3109/15563650.2010.518969. [DOI] [PubMed] [Google Scholar]
- 99.Phillips R.E., Warrell D.A., Looareesuwan S. Effectiveness of SMS 201-995, a synthetic, long-acting somatostatin analogue, in treatment of quinine-induced hyperinsulinaemia. Lancet. 1986;1(8483):713–716. doi: 10.1016/s0140-6736(86)91103-7. [DOI] [PubMed] [Google Scholar]
- 100.Drew B.J., Ackerman M.J., Funk M. Prevention of torsade de pointes in hospital settings: a scientific statement from the American Heart Association and the American College of Cardiology Foundation. Circulation. 2010;121(8):1047–1060. doi: 10.1161/CIRCULATIONAHA.109.192704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Thomas S.H.L., Behr E.R. Pharmacological treatment of acquired QT prolongation and torsades de pointes. Br J Clin Pharmacol. 2016;81(3):420–427. doi: 10.1111/bcp.12726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Riou B., Rimailho A., Galliot M., Bourdon R., Huet Y. Protective cardiovascular effects of diazepam in experimental acute chloroquine poisoning. Intensive Care Med. 1988;14(6):610–616. doi: 10.1007/BF00256764. [DOI] [PubMed] [Google Scholar]
- 103.Buckley N.A., Smith A.J., Dosen P., O’Connell D.L. Effects of catecholamines and diazepam in chloroquine poisoning in barbiturate anaesthetised rats. Hum Exp Toxicol. 1996;15(11):909–914. doi: 10.1177/096032719601501108. [DOI] [PubMed] [Google Scholar]
- 104.Tisdale J.E., Patel R.V., Webb C.R., Borzak S., Zarowitz B.J. Proarrhythmic effects of intravenous vasopressors. Ann Pharmacother. 1995;29(3):269–281. doi: 10.1177/106002809502900309. [DOI] [PubMed] [Google Scholar]
- 105.Erickson T.B., Chai P.R., Boyer E.W. Chloroquine, hydroxychloroquine and COVID-19. Toxicology Communications. 2020;4(1):40–42. doi: 10.1080/24734306.2020.1757967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Liu L., Katz Y., Weizman R., Rosenberg B., Pasternak G.W., Gavish M. Interactions of chloroquine with benzodiazepine, γ-aminobutyric acid and opiate receptors. Biochem Pharmacol. 1991;41(10):1534–1536. doi: 10.1016/0006-2952(91)90574-o. [DOI] [PubMed] [Google Scholar]
- 107.Crouzette J., Vicaut E., Palombo S., Girre C., Fournier P.E. Experimental assessment of the protective activity of diazepam on the acute toxicity of chloroquine. J Toxicol Clin Toxicol. 1983;20(3):271–279. doi: 10.3109/15563658308990070. [DOI] [PubMed] [Google Scholar]
- 108.Chary M.A., Barbuto A.F., Izadmehr S., Hayes B.D., Burns M.M. COVID-19: therapeutics and their toxicities. J Med Toxicol. 2020;16(3):284–294. doi: 10.1007/s13181-020-00777-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Wolff R.S., Wirtschafter D., Adkinson C. Ocular quinine toxicity treated with hyperbaric oxygen. Undersea Hyperb Med. 1997;24(2):131–134. [PubMed] [Google Scholar]
- 110.Neavyn M.J., Boyer E.W., Bird S.B., Babu K.M. Sodium acetate as a replacement for sodium bicarbonate in medical toxicology: a review. J Med Toxicol. 2013;9(3):250–254. doi: 10.1007/s13181-013-0304-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.McKinney P.E., Rasmussen R. Reversal of severe tricyclic antidepressant-induced cardiotoxicity with intravenous hypertonic saline solution. Ann Emerg Med. 2003;42(1):20–24. doi: 10.1067/mem.2003.233. [DOI] [PubMed] [Google Scholar]
- 112.Thorogood N., Atwal S., Mills W. The risk of antimalarials in patients with renal failure. Postgrad Med J. 2007;83(986) doi: 10.1136/pgmj.2007.063735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.de Lange D.W., Sikma M.A., Meulenbelt J. Extracorporeal membrane oxygenation in the treatment of poisoned patients. Clin Toxicol (Phila) 2013;51(5):385–393. doi: 10.3109/15563650.2013.800876. [DOI] [PubMed] [Google Scholar]
- 114.Mongenot F., Gonthier Y.T., Derderian F., Durand M., Blin D. Treatment of hydroxychloroquine poisoning with extracorporeal circulation. Ann Fr Anesth Reanim. 2007;26(2):164–167. doi: 10.1016/j.annfar.2006.09.005. [DOI] [PubMed] [Google Scholar]
- 115.Gunja N., Roberts D., McCoubrie D. Survival after massive hydroxychloroquine overdose. Anaesth Intensive Care. 2009;37(1):130–133. doi: 10.1177/0310057X0903700112. [DOI] [PubMed] [Google Scholar]
- 116.Vanzetto G., Akret C., Bach V. Assistance circulatoire extracorporelle percutanée dans les défaillances hémodynamiques aiguës graves : Expérience monocentrique chez 100 patients consécutifs. Can J Cardiol. 2009;25(6):e179–e186. doi: 10.1016/s0828-282x(09)70093-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Bagate F., Radu C., Mekontso Dessap A., de Prost N. Early extracorporeal membrane oxygenation for cardiovascular failure in a patient with massive chloroquine poisoning. The American Journal of Emergency Medicine. 2017;35(2) doi: 10.1016/j.ajem.2016.08.058. 380.e383–380.e384. [DOI] [PubMed] [Google Scholar]
- 118.Haesendonck R., de Winter S., Verelst S., Sabbe M.B. Intravenous lipid emulsion for intentional Chloroquine poisoning. Clin Toxicol (Phila) 2012;50(3):223. doi: 10.3109/15563650.2011.653488. [DOI] [PubMed] [Google Scholar]
- 119.Murphy L.R., Maskell K.F., Kmiecik K.J., Shaffer B.M. Intravenous lipid emulsion use for severe hydroxychloroquine toxicity. Am J Ther. 2018;25(2):e273–e275. doi: 10.1097/MJT.0000000000000451. [DOI] [PubMed] [Google Scholar]
- 120.Lee H.M., Archer J.R., Dargan P.I., Wood D.M. What are the adverse effects associated with the combined use of intravenous lipid emulsion and extracorporeal membrane oxygenation in the poisoned patient? Clin Toxicol (Phila) 2015;53(3):145–150. doi: 10.3109/15563650.2015.1004582. [DOI] [PubMed] [Google Scholar]
- 121.Fettiplace M.R., Akpa B.S., Rubinstein I., Weinberg G. Confusion about infusion: rational volume limits for intravenous lipid emulsion during treatment of oral overdoses. Ann Emerg Med. 2015;66(2):185–188. doi: 10.1016/j.annemergmed.2015.01.020. [DOI] [PubMed] [Google Scholar]