Abstract
Purpose
To evaluate the effect of double level osteotomy (DLO), a combination of a lateral closed distal femoral osteotomy (LCWDFO) and medial opening wedge high tibial osteotomy (MOWHTO), on patellar height and patellofemoral alignment as compared to those of isolated MOWHTO.
Methods
Twenty-six consecutive knees in 26 patients who underwent DLO (DLO group) constituted the study population. For comparative purpose, a control cohort (N: 26) matched for age, sex, and body mass index with the study group were selected from the patients who underwent isolated MOWHTO with an opening gap of more than 10 mm during the same period (MOWHTO group). Patellar height and patellofemoral alignment were assessed on radiographs preoperatively and at 2 years after surgery. For the patellar height, following parameters were measured on a lateral radiograph: Modified Insall-Salvati Index (mISI), modified Caton–Deschamps Index (mCDI), and modified Blackburne-Peel Index (mBPI). In the assessment of patellofemoral alignment, lateral patellar tilt (LPT) and lateral patellar shift (LPS) were measured on a skyline view. The measured values were statistically compared using the Student’s t-test.
Results
In the DLO group, the patellar height measured by mCDI and mPBPI significantly decreased after surgery. As regards the patellofemoral alignment, LPT significantly decreased with no significant postoperative change detected for LPS. When the amounts of postoperative changes in radiological indices were compared between the DLO and isolated MOWHTO groups, no significant differences were detected for all parameters.
Conclusion
DLO induced reduction in patellar height and decreased lateral patellar tilt. Those changes in patellar position and orientation were similarly observed in isolated MOWHTO knees. Although DLO is specifically indicated for knees with severe varus deformity, the two surgical options for correction of varus knee deformity exerted similar influences on patellofemoral biomechanics.
Keywords: Double level osteotomy (DLO), Varus deformity, Osteoarthritis of the knee, Patellar height, Patellofemoral joint alignment
Introduction
Osteotomies around the knee are widely performed procedures in surgical management of unicompartmental knee osteoarthritis with malalignment, especially in young or active patients. For the surgical correction of varus deformity, medial opening wedge high tibial osteotomy (MOWHTO) has been generally performed with good clinical results reported in literatures.1, 2, 3, 4 In correction of severe varus deformity, however, isolated MOWHTO with large wedge opening may result in non-physiologic lateral inclination of the joint line.3,5,6 Moreover, it has been reported that excessive wedge opening in MOWHTO induces a problematic reduction in patellar height and an increase in the patellofemoral contact pressure.7, 8, 9, 10, 11 Regarding the sites of deformity in severe varus knee deformity, the geometrical factors causing deformity are present on both the femoral and tibial sides.
Based on the aforementioned considerations, double level osteotomy (DLO) has been introduced as a surgical option for correction of severe varus deformity to overcome the potential shortcomings associated with correction by MOWHTO alone in this situation. There have been several studies reporting favorable surgical outcomes of DLO.12, 13, 14 Those reports have shown that DLO enables restoration of normal limb alignment without causing non-physiologic joint line inclination as observed in isolated MOWHTO knees; however, most of the previous relevant studies dealt with correction of the femoro-tibial alignment, and associated changes in the patellofemoral joint have not been addressed. Although there have been studies investigating the changes in the patellar position and orientation following MOWHTO, there is lack of information regarding the effects of DLO on patellar height or patellofemoral alignment.
The purpose of this study, therefore, is to evaluate the effect of double level osteotomy (DLO), a combination of a lateral closed distal femoral osteotomy (LCWDFO) and MOWHTO, on patellar height and patellofemoral alignment as compared to those of isolated MOWHTO.
Materials and methods
Patient population
Between January 2014 and October 2016, 26 patients (3 male, 23 female) underwent DLO comprising of LCWDFO and MOWHTO for correction of varus deformity at our institution. Follow-up results for a minimum of 2 years could be obtained for all patients and this group of patients constituted the study population (DLO group).
During the same period, 156 patients underwent isolated MOWHTO with a 2-year minimum follow-up results available, of which 62 patients exhibited severe varus deformity requiring an opening gap of more than 10 mm. Among those 62 patients, 26 patients matched for age, sex, and body mass index with the DLO group were selected and this cohort served as a control group (MOWHTO group).
The design of this study was approved by the Review Board and informed consent was obtained from all patients.
Surgical indication and planning
DLO was indicated for knees exhibiting deformity in both the femur and tibia, and for patients with high activity level who wished to retain the level of activity after surgery.13 Preoperative surgical planning was performed using digital planning software (mediCADR, Hectect, Germany) on a standing full-length anteroposterior radiograph.15 The indication for DLO was severe varus malalignment and medial compartment osteoarthritis. Based on reports by Nakayama et al. and S. Schröter et al., the surgical planning of MOWHTO was conducted first, and DLO was considered as a surgical option when the mechanical medial proximal tibial angle (mMPTA) in the simulation was more than 95° or the wedge size was more than 15 mm. DLO was subsequently performed if the mLDFA was greater than 90°. Based on the normal mechanical alignment described by Paly et al.,16 the lower limit of normal for the mechanical lateral distal femoral angle (mLDFA) was set to 85° in the same manner as previous studies13,14 for the surgical planning of DLO, and the mMPTA was adjusted so as for the HKA angle to achieve a mild valgus alignment (0–2°).
Surgical procedure
All surgeries were performed by a single surgeon (H.N.) under general anesthesia. The surgery was started with arthroscopic examination and procedures for intraarticular pathologies. Osteophytes were arthroscopically removed as much as possible, and proliferated synovium was resected. Meniscal and chondral lesions were arthroscopically addressed as needed. When the patellar mobility was deemed to be poor, arthroscopic lateral retinacular release was performed.17
Detailed description of our DLO procedure in our practice is made in our previous paper.13 Briefly, DLO was started with LCWDFO. A 4 to 5-cm longitudinal incision was made at the lateral side of the femur just above the femoral epicondyle. After the femoral osteotomy using the biplanar technique,18 fixation of the osteotomy site was accomplished using the minimally invasive plate osteosynthesis (MIPO) technique.19 The TomoFix medial distal femur (MDF) anatomical plate (DePuySynthes, Solothurn, Switzerland) originally designed for the contralateral femur was bent according to the individual’s anatomy and utilized for fixation. Secondly, the osteotomy procedure was completed with subsequent OWHTO. The OWHTO was performed using a modified technique as previously described.20, 21 A 4-cm straight vertical skin incision was made on the anteromedial aspect of the tibia. A biplanar osteotomy was performed, and the site of the osteotomy was opened with a bone spreader. Following the fluoroscopic confirmation for the degree of correction, a wedge-shaped bone substitute (ß-TCP: Osferion 60; Olympus Terumo Biomaterials, Tokyo, Japan) was inserted into the osteotomy gap. TomoFix™ medial high tibial (MHT) plate (DePuy Synthes, Solothurn, Switzerland) was placed anteromedially and the osteotomy site was fixed using lag screws.
Postoperative rehabilitation
Following DLO, knee motion was started as tolerated a day after surgery. Partial weight bearing was initiated at 3 weeks postoperatively with progression to full weight bearing at 4 weeks. For knees with isolated MOWHTO, knee motion and weight bearing were allowed as tolerated on the following day.
Radiographic assessments
Assessment of radiological parameters regarding lower extremity alignment and bony geometry were made on a full-length standing anteroposterior radiograph using the digital planning software described above. The parameters subjected to the analysis were as follows: Position of the weight-bearing axis relative to the tibial articular surface width (%WBL), hip-knee-ankle (HKA) angle, mechanical lateral distal femoral angle (mLDFA), and mechanical medial proximal tibial angle (mMPTA). In addition, the tibial posterior slope (TPS) was measured on the standing lateral view of the knee in extension (Fig. 1).
Fig. 1.
Parameters for alignment of the lower limb and posterior tibial slope
(A) Preoperative surgical planning on a weight-bearing anteroposterior radiograph. (B) Weight-bearing anteroposterior radiograph at 2 years after surgery. mLDFA, mechanical lateral distal femoral angle; mMPTA, mechanical medial proximal tibial angle; mFA-mTA, mechanical tibiofemoral angle; HKA angle, hip-knee-ankle angle. Yellow line, anatomical femoral axis; blue line, anatomical tibial axis; white line, mechanical femoral and tibial axis; sky blue line, mechanical axis. (C) Measurement of tibial posterior slope (TPS). TPS is defined as the angle between the line perpendicular to the mid-diaphyseal axis of the tibia and the tangent of the tibial plateau on a lateral radiograph. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
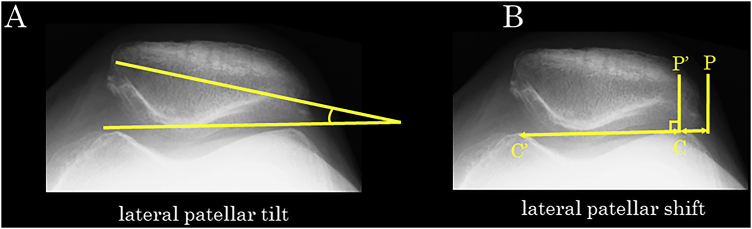
As parameters for patellar height, the modified Insall-Salvati index (mISI),22 modified Caton–Deschamps index (mCDI),23 and modified Blackburne-Peel index (mBPI) were measured on the standing lateral view of the knee in extension7,24 (Fig. 2). In assessment of patellofemoral joint alignment, lateral patellar tilt (LPT) and lateral patellar shift (LPS) were measured on a 30° skyline view (Fig. 3).
Fig. 2.
Indices of patellar height measured on a weight-bearing lateral radiograph. (A) Modified Insall-Salvati Index (b/a). Modified Insall-Salvati Index is defined as the ratio of the patellar tendon length (b, distance from the inferior pole of the patella to the tibial tuberosity) to the patellar length (a, maximum diagonal length of the patella). (B) Modified Caton Deschamps Index (d/c). odified Caton Deschamps Index is defined as the ratio of the distance between the distal end of the patellar articular surface and the angular protrusion of the tibial plateau (d) to the length of the articular surface of the patella (c). (C) Modified Blackburne-Peel Index (f/e). The Modified Blackburne-Peel Index is defined as the ratio of the perpendicular distance from the distal end of the patellar articular surface to the extension of the tibial plateau line (f) to the length of the articular surface of the patella (e).
Fig. 3.
Indices of patellofemoral alignment measured on a skyline view with the knee at 30° of flexion. (A) Lateral patellar tilt. Lateral patellar tilt is defined as the angle formed by the line connecting medial and lateral edges of the patella and the line connecting medial and lateral edges of the trochlear sulcus. (B) Lateral patellar shift (PP’/CC′). The reference line is drawn connecting medial and lateral edges of the trochlear sulcus (CC′). Perpendicular lines to the extension of the reference line are drawn from the lateral edge of the trochlear sulcus (P′) and lateral edge of the patella (P). Lateral patellar shift is defined as the ratio of the distance between P and P′ on the extended reference line to the distance between C and C’.
The radiological measurements were conducted for the preoperative and 2-year postoperative radiographs by a single orthopedic surgeon (Y. A.) who was blinded to clinical information except for radiological image data.
Analytical protocol
Operative records for the included patients were reviewed and relevant surgical information including wedge size and concomitant arthroscopic procedures was retrieved. In the comparative analysis of the obtained radiological parameters, pre- and postoperative values were compared for the change induced by surgery. For the comparison between the study (DLO) and control (MOWHTO) groups, each of the preoperative parameter values as well as the amount of postoperative change was compared between the groups.
Statistical analysis
Statistical comparison between the parameter values measured at pre- and postoperative evaluations was made using the Student’s paired t-test. The preoperative patient clinical and radiological characteristics and postoperative changes in each of the radiological parameters were statistically compared between the DLO and MOWHTO groups using the unpaired t-test. A statistical significance was defined as P < 0.05. According to a meta-analysis report8 on changes in patellar height after opening wedge osteotomy, the power calculation for the required sample size showed that a minimum of 16 knees were required for an α value of 0.05 and β value of 0.8 to detect a difference of 0.1 with a standard deviation of 0.10 for mISI, mCDI and mBPI. All analyses were performed with the commercially available software (Stat Flex version 7.0, Artech, Inc., Osaka, Japan).
Results
Patient profile
The patient demographic data in each of the two groups are presented in Table1. Since both groups were matched for age, sex, and body mass index, all data for patient characteristics in both groups were comparable without significant difference.
Table 1.
Patient demographics
| Variable | DLO† | MOWHTO† | P value |
|---|---|---|---|
| Number (male/female) | 26 (3/23) | 26 (3/23) | |
| Age (years) | 62.3 (6.8) | 62.3 (5.6) | 0.98 |
| Height (m) | 1.57 (7.6) | 1.57 (7.1) | 0.65 |
| Weight (kg) | 61.3 (10.0) | 60.6 (8.7) | 0.79 |
| BMI (kg/m2) | 24.6 (2.5) | 24.5 (2.7) | 0.93 |
| Follow up (M) | 35.5 (8.0) | 39.0 (4.9) | 0.07 |
BMI, body mass index; DLO, double level osteotomy; MOWHTO, medial open wedge high tibial osteotomy.
Data in the second and third columns are expressed as mean and standard deviation (in parenthesis) values unless otherwise indicated.
Intraoperative parameter
Surgical data derived from the patient records are presented in Table 2. In the DLO group, the amount of resected bone on the femoral side was a mean of 6.0 ± 1.5 mm. The opening width on the tibial side averaged 10.1 ± 2.4 mm which was significantly smaller than that of the isolated MOWHTO group with the width of 12.6 ± 2.1 mm (P < 0.001) (Table2).
Table 2.
Intraoperative Parameter
| Parameter | DLO† | MOWHTO† | P value |
|---|---|---|---|
| Femoral closed wedge (mm) | 6.0 (1.5) | ||
| Tibial open wedge (mm) | 10.1 (2.4) | 12.6 (2.1) | < 0.001 |
| Lateral retinacular release (number of knees) | 5/26 | 8/26 | 0.65 |
DLO, double level osteotomy; MOWHTO, medial open wedge high tibial osteotomy.
Data in the second and third rows are expressed as mean and standard deviation (in parenthesis) values unless otherwise indicated.
Lateral retinacular release was performed for 5 and 8 knees of the 26 knees in the DLO and MOWHTO groups respectively.
Knee alignment parameters
Pre- and postoperative data in both groups are shown in Table 3. Preoperatively, %WBL, HTA angle, and mLDFA values were significantly greater in the DLO group than the MOWHTO group indicating abnormalities in alignment and femoral geometry were more evident in the DLO group. In comparison of the pre- and postoperative values, all values on coronal plane parameters (%WBL, HKA angle, mLDFA, and mMPTA) were corrected with significant changes induced by the surgery. Although no significant difference was observed in the postoperative %MA and HKA angle between groups, both tended to exhibit larger values in the MOWHTO group. Moreover, the postoperative mMPTA was significantly higher in the MOWHTO group. TPS value on the sagittal plane was not changed after surgery in both groups.
Table 3.
Pre- and Postoperative Knee Alignment Parameters
| Parameter | DLO† | MOWHTO† | P value | |
|---|---|---|---|---|
| %MA | Pre-op | -13.2 (11.9) | 1.2 (9.7) | <0.001 |
| Post-op | 50.0 (12.4)∗ | 57.6 (14.6)∗ | 0.06 | |
| HKA angle (°) | Pre-op | -14.7 (2.7) | -10.7 (2.1) | <0.001 |
| Post-op | 0.46 (2.7)∗ | 1.58 (4.2) ∗ | 0.26 | |
| mLDFA (°) | Pre-op | 91.0 (1.4) | 88.2 (2.0) | <0.001 |
| Post-op | 85.6 (1.5)∗ | ― | ― | |
| mMPTA (°) | Pre-op | 82.3 (1.7) | 82.3 (1.9) | 0.94 |
| Post-op | 90.2 (2.0)∗ | 92.9 (4.1)∗ | 0.004 | |
| TPS (°) | Pre-op | 8.9 (3.7) | 9.8 (2.9) | 0.32 |
| Post-op | 7.6 (4.4) | 9.3 (3.1) | 0.11 |
DLO, double level osteotomy; MOWHTO, medial open-wedge high tibial osteotomy; %MA, mechanical alignment; HKA angle, hip-knee-ankle angle; mLDFA, mechanical lateral distal femoral angle; mMPTA, mechanical medial proximal tibial angle; TPS, tibial posterior slope.
Data in the third and fourth columns are expressed as mean and standard deviation (in parenthesis) values.
Significant difference between pre- and post-op values
Patellar height
Pre- and postoperative parameters for patellar height in the two groups are presented in Table 4. Preoperatively, there was no differences in any of the indices between the groups. After surgery, mISI was not significantly changed while mCDI and mBPI values were significantly reduced in both groups (P < 0.001) indicating that the patellar position was lowered with reference to the joint level by the osteotomy. In the comparison between the DLO and MOWHTO groups, no significant difference in the postoperative change was demonstrated.
Table 4.
Changes in Patellar Height Parameters after DLO and MOWHTO
| Patellar Height | DLO† | MOWHTO† | P value |
|---|---|---|---|
| Modified Insall-Salvati Index | |||
| Pre-op Post-op |
1.17 (0.17) | 1.14 (0.17) | 0.61 |
| 1.13 (0.18) | 1.14 (0.19) | 0.80 | |
| ΔmISI | 0.039 (0.113) | 0.001 (0.104) | 0.22 |
| Modified Caton-Deschamps Index | |||
| Pre-op Post-op |
0.95(0.15) | 1.03 (0.14) | 0.07 |
| 0.82 (0.16)∗ | 0.84 (0.15)∗ | 0.69 | |
| ΔmCDI | 0.13 (0.18) | 0.19 (0.23) | 0.32 |
| Modified Blackburne-Peel Index | |||
| Pre-op Post-op |
0.76 (0.18) | 0.72 (0.15) | 0.38 |
| 0.70 (0.17)∗ | 0.64 (0.14)∗ | 0.15 | |
| ΔmBPI | 0.063 (0.13) | 0.084 (0.09) | 0.49 |
Δ: Change from pre-op to post-op values
Data in the second and third columns are expressed as mean and standard deviation (in parenthesis) values.
Significant difference between pre- and post-op values
Patellofemoral alignment
Results of the assessment for patellofemoral congruity are presented in Table 5. After the osteotomy, LPT value was significantly reduced (P < 0.001) while no significant postoperative change was observed for LPS in both groups. In the comparison of the postoperative changes between the DLO and MOWHTO groups, no significant differences were demonstrated for the two parameters.
Table 5.
Changes in Patellofemoral Alignment Parameters after DLO and MOWHTO
| Patellofemoral Alignment | DLO† | MOWHTO† | P value |
|---|---|---|---|
| Lateral patellar tilt, | |||
| Pre-op Post-op |
5.5 (3.2) | 7.0 (3.2) | 0.11 |
| 2.6 (2.3)∗ | 4.1 (3.5)∗ | 0.08 | |
| ΔLPT | 2.88 (3.0) | 2.88 (2.4) | 1.00 |
| Lateral patellar shift | |||
| Pre-op Post-op |
0.08 (0.04) | 0.10 (0.04) | 0.11 |
| 0.08 (0.04) | 0.09 (0.04) | 0.15 | |
| ΔLPS | 0.0045 (0.043) | 0.0071 (0.040) | 0.82 |
Δ: Change from pre-op to post-op values
Data in the second and third columns are expressed as mean and standard deviation (in parenthesis) values.
Significant difference between pre- and post-op values
Discussion
The most important findings of the present study were that mCDI and mBPI, patellar height parameters with reference to the joint level, were significantly decreased after DLO. These changes were similarly noted for the knees with isolated MOWHTO and there was no significant difference between the DLO and isolated MOWHTO groups. A regards the parameters of patellofemoral congruity, DLO induced reduction in lateral tilt of the patella with no change in the shift. Similar to the effect of osteotomy on patellar height, no significant differences between the results of DLO and MOWHTO groups were detected.
There have been a number of studies examining the effect of MOWHTO performed for varus osteoarthritic knees on patellar height.7,9, 10, 11 Bin et al. conducted a metaanalysis of those studies and concluded that postoperative patellar height assessed with CDI and BPI decreased after MOWHTO with no significant change in ISI.8 The present study results for DLO and MOHTO cohorts agree with those of the previous studies. Causative factors for patellar height reduction reported in the previous literatures are distal transposition of the tibial tuberosity by wedge opening,9 shortening of the patellar tendon by postoperative scarring and contracture of peritendinous tissue,25,26 and change in the posterior slope of the tibia.27 Another finding reported in the previous studies is a correlation between the amount of patellar height reduction and correction angle (wedge width) in MOWHTO knees.28 Although the wedge size in the isolated MOWHTO group in this study was significantly greater than in the DLO group (12.6 mm vs. 10.1 mm), the inter-group difference was so small as to induce no appreciable difference between the groups for postoperative changes in the patellar height parameters.
Regarding the patellofemoral congruity, there have been studies reporting changes in patellofemoral alignment following MOWHTO.29, 30, 31 Those previous studies have shown somewhat discordant results for lateral patellar tilt, reporting postoperative reduction in some studies and no change in others. By contrast, the majority of the studies have reported no significant postoperative change in lateral patellar shift. The present study has shown both DLO and isolated MOWHTO significantly decreased lateral tilt with no change induced for the lateral shift. According to the previous relevant studies, the postoperative decrease in patellar lateral tilt has been attributed to two factors. Gaasbeek et al. examined three-dimensional patellar kinematics in a cadaveric study and reported that OWHTO induced medial patellar tilt due to the contact and compression of patellar lateral facet against the lateral wall of the femoral trochlea with resultant change in patellar orientation.30 Second possible factor leading to reduction in patellar tilt is the effect of lateral retinacular release on patellar orientation. Murayama et al. investigated the effect of concomitant lateral retinacular release on patellar position and orientation in knees undergoing MOWHTO. According to their report, lateral release concomitantly performed with MOWHTO induced reduction in lateral tilt.17 In the present study population, lateral retinacular release was added to the procedure in 5 and 8 of the 26 knees in the DLO and MOWHTO groups respectively, and this factor may have contributed to the postoperative decrease in patellar lateral tilt. Regarding patellar shift, both of the previous and the present studies demonstrated no change after surgery. Therefore, the effect of the femoral and tibial osteotomies on the patellar position on the medial/lateral axis seems minimal.
DLO has been reported to produce satisfactory outcomes12, 13, 14 indicating that this procedure is an effective surgical option for varus knees with deformities on both the femoral and tibial sides. Combined correction on both sides of the knee in DLO can effectively prevent the problem of non-physiologic joint line inclination as encountered in correction of severe varus deformity by isolated MOWHTO. However, since varus deformity of the knees undergoing DLO is severe, wedge opening of more than 10 mm is generally required for MOWHTO on the tibial side. Consequently, deformity correction by DLO is associated with similar effects on patellar position and orientation to those observed for isolated MOWHTO with large wedge opening. Although it is not clear whether the postoperative changes observed in this study induce osteoarthritic progression of the patellofemoral joint,10,11 it can be stated that correction of severe varus deformity by either DLO or isolated MOWHTO induces similar changes in the biomechanical environment of the patellofemoral joint. Since it has been reported that knees with severe varus deformity is generally combined with severe patellofemoral arthritis,32 osteotomy procedures that exert less influence on the patellar position such as distal-tuberosity osteotomy,33,34 closed wedge HTO,8,28 and hybrid HTO 35,36,37should be considered as alternative surgical options on the tibial side.
Limitation
There are several limitations included in the design and contents of this study. First, the study design is a retrospective analysis of the patient data. Although comparative analysis of two procedures (DLO versus isolated MOWHTO) was conducted for matched pair cohorts, there apparently was a selection bias in the surgical option. Second is an issue of radiological evaluation method. In this study, patellar height was assessed using three measurement methods on a standing lateral radiograph taken in an extended position, while a non-weight-bearing lateral radiograph in mild flexion (30° flexion) was subjected to the measurement in the original descriptions of those three methods.22, 23, 24 In addition, all the methods employed in this study are the measurements with reference to the tibial bony landmark. Since specific feature of DLO is a femoral osteotomy in addition to MOWHTO, use of a radiological evaluation method in relation to the femur as proposed by Miura et al.38 may have led to different results. Third, we performed a lateral retinacular release if the patellar mobility was subjectively rated as poor according to manual manipulation under general anesthesia.17 Since the assessment was not objectively based on preoperative image examination or stress examination, the results could have potentially varied across examiners. Although the patellar tilt was significantly improved in both groups compared to preoperative levels, the degree of improvement was approximately 2.9°, which may have been small enough to be a result of under-corrected (neutral) coronal alignment after surgery. Finally, this study examined changes in patellar position and orientation on 2-year postoperative radiographs. Additional data sets such as intermediate- and long-term radiological examinations as well as evaluation using clinical outcome measures are required to clarify the consequence of patellofemoral changes observed in this study.
Conclusion
DLO induced reduction in patellar height and decreased lateral patellar tilt. Those changes in patellar position and orietation were similarly observed in isolated MOWHTO knees. Although DLO is specifically indicated for knees with severe varus deformity, the two surgical options for correction of varus knee deformity exerted similar influences on patellofemoral biomechanics.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for- profit sectors, and no material support of any kind was received
Declaration of competing interest
The authors declare no conflicts of interest in association with the present study.
Acknowledgements
I would like to thank Prof. Hiroyuki Kato for useful discussions.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.asmart.2020.05.003.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Giuseffi S.A., Replogle W.H., Shelton W.R. Opening-wedge high tibial osteotomy: Review of 100 consecutive cases. Arthroscopy. 2015;31(11):2128–2137. doi: 10.1016/j.arthro.2015.04.097. [DOI] [PubMed] [Google Scholar]
- 2.Saito T., Kumagai K., Akamatsu Y., Kobayashi H., Kusayama Y. Five- to ten-year outcome following medial opening-wedge high tibial osteotomy with rigid plate fixation in combination with an artificial bone substitute. Bone Joint Lett J. 2014;96-b(3):339–344. doi: 10.1302/0301-620X.96B3.32525. [DOI] [PubMed] [Google Scholar]
- 3.Schuster P., Gesslein M., Schlumberger M. Ten-year results of medial open-wedge high tibial osteotomy and chondral resurfacing in severe medial osteoarthritis and varus malalignment. Am J Sports Med. 2018;46(6):1362–1370. doi: 10.1177/0363546518758016. [DOI] [PubMed] [Google Scholar]
- 4.Kim J.H., Kim H.J., Lee D.H. Survival of opening versus closing wedge high tibial osteotomy: a meta-analysis. Sci Rep. 2017;7(1):7296. doi: 10.1038/s41598-017-07856-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Akamatsu Y., Kumagai K., Kobayashi H., Tsuji M., Saito T. Effect of increased coronal inclination of the tibial plateau after opening-wedge high tibial osteotomy. Arthroscopy. 2018;34(7):2158–2169. doi: 10.1016/j.arthro.2018.01.055. e2152. [DOI] [PubMed] [Google Scholar]
- 6.Nakayama H., Schroter S., Yamamoto C. Large correction in opening wedge high tibial osteotomy with resultant joint-line obliquity induces excessive shear stress on the articular cartilage. Knee Surg Sports Traumatol Arthrosc. 2018;26(6):1873–1878. doi: 10.1007/s00167-017-4680-x. [DOI] [PubMed] [Google Scholar]
- 7.Bito H., Takeuchi R., Kumagai K. Opening wedge high tibial osteotomy affects both the lateral patellar tilt and patellar height. Knee Surg Sports Traumatol Arthrosc. 2010;18(7):955–960. doi: 10.1007/s00167-010-1077-5. [DOI] [PubMed] [Google Scholar]
- 8.Bin S.I., Kim H.J., Ahn H.S., Rim D.S., Lee D.H. Changes in patellar height after opening wedge and closing wedge high tibial osteotomy: a meta-analysis. Arthroscopy. 2016;32(11):2393–2400. doi: 10.1016/j.arthro.2016.06.012. [DOI] [PubMed] [Google Scholar]
- 9.El-Azab H., Glabgly P., Paul J., Imhoff A.B., Hinterwimmer S. Patellar height and posterior tibial slope after open- and closed-wedge high tibial osteotomy: a radiological study on 100 patients. Am J Sports Med. 2010;38(2):323–329. doi: 10.1177/0363546509348050. [DOI] [PubMed] [Google Scholar]
- 10.Goshima K., Sawaguchi T., Shigemoto K., Iwai S., Nakanishi A., Ueoka K. Patellofemoral osteoarthritis progression and alignment changes after open-wedge high tibial osteotomy do not affect clinical outcomes at mid-term follow-up. Arthroscopy. 2017;33(10):1832–1839. doi: 10.1016/j.arthro.2017.04.007. [DOI] [PubMed] [Google Scholar]
- 11.Kim K.I., Kim D.K., Song S.J., Lee S.H., Bae D.K. Medial open-wedge high tibial osteotomy may adversely affect the patellofemoral joint. Arthroscopy. 2017;33(4):811–816. doi: 10.1016/j.arthro.2016.09.034. [DOI] [PubMed] [Google Scholar]
- 12.Babis G.C., An K.N., Chao E.Y., Rand J.A., Sim F.H. Double level osteotomy of the knee: a method to retain joint-line obliquity. Clinical results. J Bone Joint Surg Am. 2002;84-A(8):1380–1388. doi: 10.2106/00004623-200208000-00013. [DOI] [PubMed] [Google Scholar]
- 13.Nakayama H., Iseki T., Kanto R. Physiologic knee joint alignment and orientation can be restored by the minimally invasive double level osteotomy for osteoarthritic knees with severe varus deformity. Knee Surg Sports Traumatol Arthrosc. 2020;28(3):742–750. doi: 10.1007/s00167-018-5103-3. [DOI] [PubMed] [Google Scholar]
- 14.Schroter S., Nakayama H., Yoshiya S., Stockle U., Ateschrang A., Gruhn J. Development of the double level osteotomy in severe varus osteoarthritis showed good outcome by preventing oblique joint line. Arch Orthop Trauma Surg. 2019;139(4):519–527. doi: 10.1007/s00402-018-3068-9. [DOI] [PubMed] [Google Scholar]
- 15.Schroter S., Ihle C., Mueller J., Lobenhoffer P., Stockle U., van Heerwaarden R. Digital planning of high tibial osteotomy. Interrater reliability by using two different software. Knee Surg Sports Traumatol Arthrosc. 2013;21(1):189–196. doi: 10.1007/s00167-012-2114-3. [DOI] [PubMed] [Google Scholar]
- 16.Paley D., Pfeil J. [Principles of deformity correction around the knee] Orthopä. 2000;29(1):18–38. doi: 10.1007/s001320050004. [DOI] [PubMed] [Google Scholar]
- 17.Murayama K., Nakayama H., Murakami T., Yoshiya S., Otsuki S., Tachibana T. The effect of concomitant arthroscopic lateral retinacular release on postoperative patellar position and orientation in open wedge high tibial osteotomy. Knee surgery & related research. 2018;30(3):241–246. doi: 10.5792/ksrr.18.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Freiling D., van Heerwaarden R., Staubli A., Lobenhoffer P. [The medial closed-wedge osteotomy of the distal femur for the treatment of unicompartmental lateral osteoarthritis of the knee] Operat Orthop Traumatol. 2010;22(3):317–334. doi: 10.1007/s00064-010-9006-9. [DOI] [PubMed] [Google Scholar]
- 19.Visser J., Brinkman J.M., Bleys R.L., Castelein R.M., van Heerwaarden R.J. The safety and feasibility of a less invasive distal femur closing wedge osteotomy technique: a cadaveric dissection study of the medial aspect of the distal femur. Knee Surg Sports Traumatol Arthrosc. 2013;21(1):220–227. doi: 10.1007/s00167-012-2133-0. [DOI] [PubMed] [Google Scholar]
- 20.Lobenhoffer P., Agneskirchner J.D. Improvements in surgical technique of valgus high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2003;11(3):132–138. doi: 10.1007/s00167-002-0334-7. [DOI] [PubMed] [Google Scholar]
- 21.Staubli A.E., De Simoni C., Babst R., Lobenhoffer P. TomoFix: a new LCP-concept for open wedge osteotomy of the medial proximal tibia--early results in 92 cases. Injury. 2003;34(Suppl 2):B55–B62. doi: 10.1016/j.injury.2003.09.025. [DOI] [PubMed] [Google Scholar]
- 22.Insall J., Salvati E. Patella position in the normal knee joint. Radiology. 1971;101(1):101–104. doi: 10.1148/101.1.101. [DOI] [PubMed] [Google Scholar]
- 23.Caton J., Deschamps G., Chambat P., Lerat J.L., Dejour H. [Patella infera. Apropos of 128 cases] Revue de chirurgie orthopedique et reparatrice de l’appareil moteur. 1982;68(5):317–325. [PubMed] [Google Scholar]
- 24.Blackburne J.S., Peel T.E. A new method of measuring patellar height. J Bone Joint Surg Br. 1977;59(2):241–242. doi: 10.1302/0301-620X.59B2.873986. [DOI] [PubMed] [Google Scholar]
- 25.Cullu E., Aydogdu S., Sur H. Does patellar ligament length change after dome-type high tibial osteotomy? Bulletin (Hospital for Joint Diseases (New York, NY)) 2000;59(3):140–143. [PubMed] [Google Scholar]
- 26.Okamoto R., Koshino T., Morii T. Shortening of patellar ligament and patella baja with improvement of quadriceps muscle strength after high tibial osteotomy. Bulletin (Hospital for Joint Diseases (New York, NY)) 1993;53(3):21–24. [PubMed] [Google Scholar]
- 27.LaPrade R.F., Oro F.B., Ziegler C.G., Wijdicks C.A., Walsh M.P. Patellar height and tibial slope after opening-wedge proximal tibial osteotomy: a prospective study. Am J Sports Med. 2010;38(1):160–170. doi: 10.1177/0363546509342701. [DOI] [PubMed] [Google Scholar]
- 28.Amzallag J., Pujol N., Maqdes A., Beaufils P., Judet T., Catonne Y. Patellar height modification after high tibial osteotomy by either medial opening-wedge or lateral closing-wedge osteotomies. Knee Surg Sports Traumatol Arthrosc. 2013;21(1):255–259. doi: 10.1007/s00167-012-2304-z. [DOI] [PubMed] [Google Scholar]
- 29.Agneskirchner J.D., Hurschler C., Wrann C.D., Lobenhoffer P. The effects of valgus medial opening wedge high tibial osteotomy on articular cartilage pressure of the knee: a biomechanical study. Arthroscopy. 2007;23(8):852–861. doi: 10.1016/j.arthro.2007.05.018. [DOI] [PubMed] [Google Scholar]
- 30.Gaasbeek R., Welsing R., Barink M., Verdonschot N., van Kampen A. The influence of open and closed high tibial osteotomy on dynamic patellar tracking: a biomechanical study. Knee Surg Sports Traumatol Arthrosc. 2007;15(8):978–984. doi: 10.1007/s00167-007-0305-0. [DOI] [PubMed] [Google Scholar]
- 31.Hinterwimmer S., Beitzel K., Paul J. Control of posterior tibial slope and patellar height in open-wedge valgus high tibial osteotomy. Am J Sports Med. 2011;39(4):851–856. doi: 10.1177/0363546510388929. [DOI] [PubMed] [Google Scholar]
- 32.Otsuki S., Nakajima M., Okamoto Y. Correlation between varus knee malalignment and patellofemoral osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2016;24(1):176–181. doi: 10.1007/s00167-014-3360-3. [DOI] [PubMed] [Google Scholar]
- 33.Gaasbeek R.D., Sonneveld H., van Heerwaarden R.J., Jacobs W.C., Wymenga A.B. Distal tuberosity osteotomy in open wedge high tibial osteotomy can prevent patella infera: a new technique. Knee. 2004;11(6):457–461. doi: 10.1016/j.knee.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 34.Akiyama T., Osano K., Mizu-Uchi H. Distal tibial tuberosity arc osteotomy in open-wedge proximal tibial osteotomy to prevent patella infra. Arthrosc Tech. 2019;8(6):e655–e662. doi: 10.1016/j.eats.2019.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Takeuchi R., Ishikawa H., Miyasaka Y., Sasaki Y., Kuniya T., Tsukahara S. A novel closed-wedge high tibial osteotomy procedure to treat osteoarthritis of the knee: hybrid technique and rehabilitation measures. Arthrosc Tech. 2014;3(4):e431–437. doi: 10.1016/j.eats.2014.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Otsuki S., Murakami T., Okamoto Y. Hybrid high tibial osteotomy is superior to medial opening high tibial osteotomy for the treatment of varus knee with patellofemoral osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2019;27(4):1332–1338. doi: 10.1007/s00167-018-5015-2. [DOI] [PubMed] [Google Scholar]
- 37.Ishimatsu T., Takeuchi R., Ishikawa H. Hybrid closed wedge high tibial osteotomy improves patellofemoral joint congruity compared with open wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2019;27(4):1299–1309. doi: 10.1007/s00167-019-05350-4. [DOI] [PubMed] [Google Scholar]
- 38.Miura H., Kawamura H., Nagamine R., Urabe K., Iwamoto Y. Is patellar height really lower after high tibial osteotomy? Fukuoka igaku zasshi = Hukuoka acta medica. 1997;88(6):261–266. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.