Abstract
Objectives:
To report experience with a global multidisciplinary tracheostomy e-learning initiative.
Methods:
An international multidisciplinary panel of experts convened to build a virtual learning community for tracheostomy care, comprising a web-based platform, five distance learning (interactive webinar) sessions, and professional discourse over 12 months. Structured pre- and post-webinar surveys were disseminated to global participants including otolaryngologists, intensivists, nurses, allied health professionals, and patients/caregivers. Data were collected on audio-visual fidelity, demographics, and pre- and post-tutorial assessments regarding experience and skill acquisition. Participants reported confidence levels for NICU, pediatric, adult, and family care, as well as technical skills, communication, learning, assessment, and subdomains.
Results:
Participants from 197 institutions in 22 countries engaged in the virtual education platform, including otolaryngologists, speech pathologists, respiratory therapists, specialist nurses, patients, and caregivers. Significant improvements were reported in communication (P < .0001), clinical assessments (P < .0001), and clinical governance (P < .0001), with positive impact on pediatric decannulation (P = .0008), adult decannulation (P = .04), and quality improvement (P < .0001). Respondents reported enhanced readiness to integrate knowledge into practice. Barriers included time zones, internet bandwidth, and perceived difficulty of direct clinical translation of highly technical skills. Participants rated the implementation highly in terms of length, ability for discussion, satisfaction, applicability to professional practice, and expertise of discussants (median scores: 4, 4, 4, 4 and 5 out of 5).
Conclusions:
Virtual learning has dominated the education landscape during COVID-19 pandemic, but few data are available on its effectiveness. This study demonstrated feasibility of virtual learning for disseminating best practices in tracheostomy, engaging a diverse, multidisciplinary audience. Learning of complex technical skills proved a hurdle, however, suggesting need for hands-on experience for technical mastery. While interactive videoconferencing via webinar affords an engaging and scalable strategy for sharing knowledge, further investigation is needed on clinical outcomes to define effective strategies for experiential online learning and virtual in-service simulations.
Keywords: e-Learning, medical education, tracheostomy, patient safety/quality improvement, distance learning, webinar
Introduction
Patients with tracheostomies have complex needs, and when these patients suffer airway-related adverse events, they can deteriorate rapidly, risking life-threatening complications. Slow dissemination of best practices has been a major barrier to high quality tracheostomy care, despite the notable successes of multidisciplinary tracheostomy care.1-4 A critical knowledge gap in the United States and abroad5 is how to drive large-scale improvement in care. These data are critically important for quality improvement and clinical education.6-10 The Global Tracheostomy Collaborative (GTC), whose mission is to improve lives of individuals with tracheostomy,4 has spearheaded data collection efforts and dissemination of best practice.11,12 Yet, little is known about effectiveness of virtual approaches for engaging professionals of different disciplines. In the era of COVID-19, the stakes are greatly increased, as healthcare workers have risk of infectious transmission from aerosol generating procedures and routine care related to tracheostomy.
The COVID-19 pandemic has created massive upheaval in societal, economic, and medical systems, and in doing so it has catalyzed change in medical education and training on a scale that would have been unimaginable only several weeks ago. These changes are far-reaching and have immediate relevance to both the safety and education of frontline healthcare professionals, who range from otolaryngologist—head & neck surgeons to critical care specialists, nurses, and allied health professionals. While virtual learning in early forms dates back decades, the pandemic has led to a veritable renaissance of virtual learning—the implications of which remain largely unstudied. In the quality improvement realm, technology-enabled learning—often asynchronous in time or space—has held particular appeal, due to its promise of scalable learning that spans continents and cultures. The quality improvement efforts around tracheostomy therefore provide a compelling system for understanding the capabilities and limitations inherent in virtual learning.
In the era prior to COVID-19, we developed a virtual learning community for tracheostomy care. This article describes our experiences building a webinar series to promote interactive learning and to reach diverse audiences, with attention to the vital role of patients and family in quality improvement efforts.13,14 We report on a patient-centered global multidisciplinary approach to tracheostomy virtual learning. We hope that it will serve as a proof of concept to inform similar education projects in related fields, particularly with the proliferation of such methods since the onset of the global pandemic.
Methods
Study Design and Intervention
This prospective cohort study was conducted anonymously and in strict accordance with institutional procedures. The protocol was registered with the Institutional Review Board in accordance with the Code of Federal Regulation in compliance with University of Michigan institutional policy for conducting quality improvement projects (Study eResearch ID: HUM00171636; 45 CFR 46, 21 CFR 56). Participants were recruited via the GTC mailing list and social media venues for patient and family recruitment, inviting individuals to attend the virtual tutorials free-of-charge. There was no limit on numbers of attendees or on the study size. The GTC hosted five one-hour virtual tutorials. Table 1 details the background of the presenters and the learning objectives. The tutorials were broadcast using GoToWebinar software. After webinars, participants were able to pose questions to discussants or to the larger forum via message boards or email, as a strategy to foster the learning community.
Table 1.
Details of Virtual Session, Including Presenter Locations, Content, and Times.
| Topic | Presenters | Content and Skills |
|---|---|---|
|
Neonatal intensive care unit (NICU) 1 pm CT / 6 pm GMT / 5 am AEDT |
• Chief of Neonatology (MD), Massachusetts, USA • Head/Neck Surgeons, Boston and Florida, USA • Nursing Director NICU, Florida, USA |
• Multidisciplinary education • Ex-utero intrapartum treatment • Neonates with congenital and acquired upper airway obstruction • Lower airway conditions |
|
Pediatric decannulation 4 pm CT / 9 pm GMT / 8 am AEDT |
• Head/Neck Surgeon, Michigan, USA • Nursing Clinical Care Coordinator, Michigan, USA |
• Clinical readiness for decannulation • Review capping protocol • Describe the decannulation process • Prepare child and family • Post decannulation follow up |
|
Adult decannulation 4 pm CT / 9 pm GMT / 8 am AEDT |
• Head/Neck Surgeons, London, UK; Baltimore, USA; Washington, USA • Registered Nurse, Johns Hopkins, USA; Manchester, UK • Speech Pathologist, Australia |
• Indications and contraindications • Practices as in- and out-patient • Failure and success factors • Role of multidisciplinary approach • The patients’ role • Post-decannulation education |
|
Patient & family perspective 5 pm CT / 10 pm BST / 8 am AEDT |
• Patient and family members • Chair of patient and family committee, GTC • Head and Neck Surgeons, Wisconsin, USA; Boston, USA |
• Incorporating patients and families • Results of patient-family survey • Strategies to increase patient engagement • Opportunities with the GTC |
|
Quality improvement initiatives 5 pm CT / 10 pm BST / 8 am AEDT |
• Intensive Care Consultant, Manchester, UK • Head / Neck Surgeon, Manchester, UK • Nurse, Manchester, UK • Patients and family, UK |
• QI at multiple levels: local department, hospital, national, international • Patient perspective |
Abbreviations: AEDT, Australian Eastern Daylight Time; CT, Central Time; GMT, Greenwich Mean Time; BST, British Summer time.
Analysis
Pre- and post-tutorial surveys were designed. Prior to dissemination, multiple healthcare professionals evaluated the survey to reduce bias in language and content. In order to optimize stakeholder representation, physician, allied health professional, and patient and family input was obtained. Participants completed the anonymized surveys voluntarily via email. Lack of evaluation did not affect eligibility to participate in future sessions. There were no financial incentives.
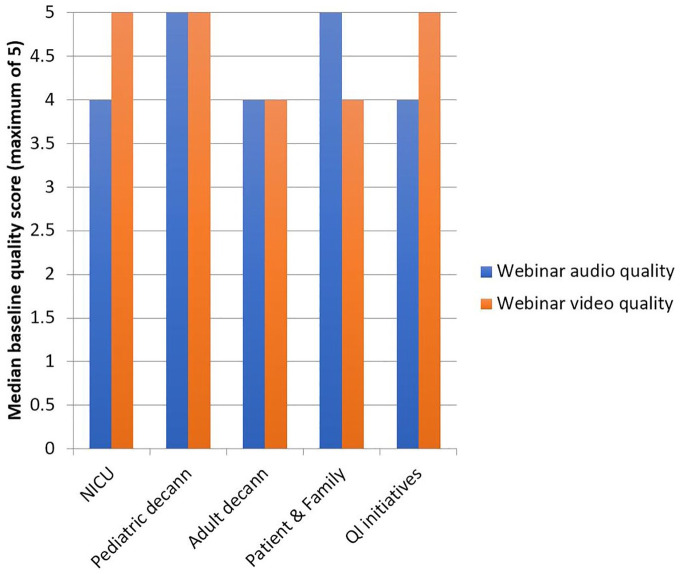
Survey participants scored audio and visual fideltiy using a 1 to 5 Likert scale. Anchors at 1 and 5 corresponded to “strongly disagree” and “strongly agree,” respectively. An overall average baseline quality score of 4, on a 5-point Likert scale, was set a priori as the minimum score for inclusion.
Participants reported confidence level before and after each virtual session. Impact was evaluated by assessing confidence of participants regarding their tracheostomy-related knowledge and ability to apply that knowledge for the content covered in each tutorial. Assessments were conducted before and after the tutorials using a 5-point Likert scale. Anchors at 1 and 5 corresponded to “not very confident” and “very confident,” respectively. Multiple questions on each topic were posed to participants covering a variety of different themes. For the purpose of this article, a theme was identified as an overarching area of particular importance or concern, such as communication or practical skills. Topics were defined as the subject matter of the webinar, such as neonatal tracheostomy. This “overlapping wedge” concept, utilizing horizontal (topics) and vertical (themes) integration, is often used in medical education to improve learning experiences for students.
Median values were calculated. Immediate participant reaction and satisfaction with the program were also evaluated using a 5-point Likert scale. Participants were asked to provide free-response answers regarding specific plans for their future practice as a surrogate for long-term impact of the program.
Data Analysis
Descriptive statistics were summarized for course evaluation. Overall confidence score was calculated. Values were interpreted as being independent, as pre- and post-survey responses were anonymized. A Mann-Whitney U-test was used to compare differences in confidence values between pre- and post-tutorial scores. Values were calculated for each tutorial and for key themes (technical skills, communication, lifelong learning, clinical assessments, clinical governance). Statistical significance was set at P-values less than 0.05. To account for missing data, a non-matched statistical analysis method was employed. The statistical package GraphPad Prism 7.0 was used for data analysis. Interquartile ranges (IQR), reported for assessments of educational impact, correspond to the difference between the largest and smallest values in the middle 50% of each data set.
Results
Demographics
Table 2 illustrates participation in virtual tutorials, detailing data on individuals who pre-registered, attended the live tutorial, or watched the recording at a later date (asynchronous viewing). A total of 328 surveys were completed: 225 before and 103 after the tutorials. Survey response rates of those attending the live tutorial were 51% before and 23% afterwards. Table 3 illustrates the demographic characteristics of survey respondents. Participants from 197 different institutions responded to the surveys; the majority were from North America. A total of 22 countries were represented. Individuals from multi-disciplinary team frequently attended.
Table 2.
Registrants and Attendees. The live attendees number is determined automatically by the webinar platform software and does not account for those who viewed the webinar as a group (extracted in January 2018).
| Topic | Date | Number of Registrants | Number of Attendees (live) | Number Viewed the Recording at Later Date |
|---|---|---|---|---|
| Neonatal intensive care unit | November 2016 | 135 | 67 | 111 |
| Pediatric decannulation | January 2017 | 157 | 89 | 173 |
| Adult decannulation | March 2017 | 304 | 156 | 285 |
| Patient and family perspective | May 2017 | 199 | 86 | 94 |
| Quality improvement initiatives | July 2017 | 121 | 43 | 109 |
Table 3.
Demographic Characteristics of Survey Responders.
| Before Webinar | After Webinar | |
|---|---|---|
| Participants, n | 225 | 103 |
| NICU | 34 | 23 |
| Pediatric | 40 | 19 |
| Adult | 86 | 34 |
| Patient and family | 49 | 20 |
| Quality improvement | 16 | 7 |
| Age, mean (range) | 42.4 (24-77) | 43.4 (27-71) |
| Female: Male | 167:31 | 84:18 |
| Number of institutions | 136 | 61 |
| Profession, n (%) | ||
| Nurse | 35 (15.6) | 17 (16.5) |
| Speech & language pathologist | 55 (24.4) | 20 (19.4) |
| Physiotherapist & Respiratory therapist | 33 (14.7) | 17 (16.5) |
| Doctor | 40 (17.8) | 27 (26.2) |
| Social worker | 5 (2.2) | 2 (1.9) |
| Non-clinical | 26 (11.6) | 10 (9.7) |
| Other | 31 (13.8) | 10 (9.7) |
| Country, n (%) | ||
| USA, Canada | 115 (51) | 61 (59.2) |
| Australia, New Zealand | 47 (20.9) | 22 (21.4) |
| UK | 42 (18.7) | 14 (13.6) |
| Other European | 10 (4.4) | 3 (2.9) |
| South America | 1 (0.4) | 1 (0.9) |
| Asia | 10 (4.4) | 2 (1.9) |
Audio-Visual Quality
All tutorials met the minimum baseline score for inclusion in analysis (Figure 1).
Figure 1.
Audio and video quality. An overall median score of 4 out of 5 was set a priori as the minimum score for inclusion.
Abbreviations: decann, decannulation; NICU, neonatal intensive care unit; QI, quality improvement.
Overall Response to Virtual Learning
Participants rated the course highly in terms of length, opportunity for discussion, overall satisfaction, applicability to professional practice, and expertise of discussants (median scores: 4, 4, 4, 4 and 5). Participants provided suggestions regarding areas that they enjoyed or felt could be improved (detailed below). In terms of content, participants requested additional time for discussion and utilization of case scenarios. Queries were collated and addressed by discussants and other experts in tracheostomy care, making regular use of GTC forums to facilitate additional discourse on practical aspects of tracheostomy-related care.
Educational Impact
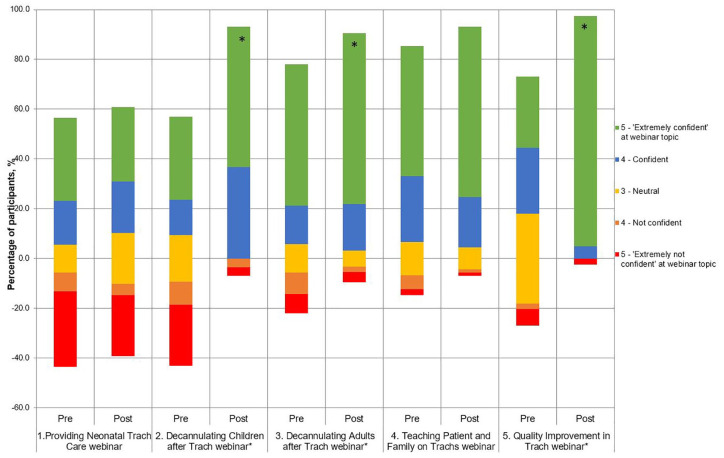
Impact by tutorial
A shift in participant’s responses towards being “confident” and “extremely confident” was observed in all five tutorials (Figure 2). The median values of Likert responses are presented; multiple domains were assessed to reflect different aspects. Significant improvements were demonstrated following the pediatric decannulation tutorial (pre-course median 3.25 [IQR3.125] vs post-course median 4.5 [IQR1]; P = .0008), adult decannulation tutorial (median 4.5 [IQR2] vs 5 [IQR0.5]; P = .04), and quality improvement tutorial (median 3.5 [IQR1] vs 5 [IQR0]; P < .0001).
Figure 2.
Participant confidence regarding mastery of education content covered, measured before and after the five virtual tutorials: Diverging stacked bar chart.
*Those tutorials with statistically significant improvement in confidence before and after (P < .05).
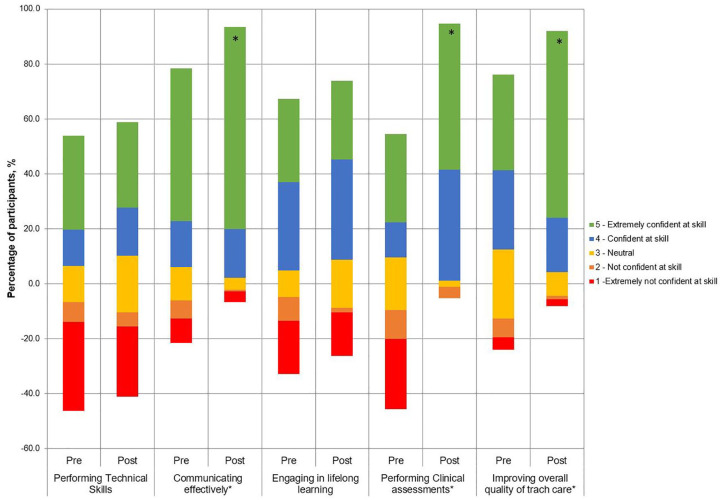
Impact by themes
A shift in participant’s responses towards being “confident” and “extremely confident” was seen in the five themes (Figure 3). Significant improvements were observed for communication (pre-course median 4 [IQR2] vs post-course median 5 [IQR1]; P < .0001), clinical assessments (median 3 [IQR4] vs 5 [IQR1]; P < .0001), and clinical governance (median 4 [IQR2] vs 5 [IQR1]; P < .0001).
Figure 3.
Participant confidences in core competency areas of education were measured before and after the five virtual tutorials: Diverging stacked bar chart.
*Those tutorials with statistically significant improvement in confidence before and after (P < .05).
Change in Behavior of Daily Clinical Practice
Several participants identified specific changes in behavior relating to daily practice. Respondents conveyed thinking more in terms of the multidisciplinary team and of sharing information with others. Most respondents reported enthusiasm to engage in quality improvement initiatives at their hospital. While some participants felt that they would be more confident in carrying out practical skills, some respondents indicated residual reservations about assisting in technical procedures and ability to carry out the algorithm recommended for achieving decannulation.
Evolution of the Series
A number of metrics were analyzed to facilitate ongoing progress of the sessions and learning community. Early feedback from participants noted concerns of poor audio-visual content, which cut out several times. Following that first session, a debriefing meeting was conducted. The committee concluded that, in addition to rehearsing presentation content, it was equally important to rehearse the technology. This measure enabled all presenters to ensure compatibility of audio-visual systems with the software. Audio-visual interruptions were also minimized by hardwiring the internet and using phones for audio instead of computer microphones.
Further ongoing assessments revealed that participants who registered on the day of the session were more likely to attend than those who registered in advance. Partly this trend was associated with likelihood of viewing the session at a later time. Nonetheless, this insight enabled the planning team to increase the live attendance rates by focusing advertisements in days before presentations and providing targeted reminder emails to those registered in advance (1 week, 5 days, 1 day, 1 hour before), leading to a pronounced spike in attendees at the following session.
Timing was another significant factor. The first session was held at 2 pm EST, corresponding to presenters’ availability. However, participants from Australia signaled that this corresponded to a 5 am meeting in Sydney. Following discussions with the education committee, 5 pm EST, 9 pm Greenwich Mean Time and 8 am Australian Eastern Daylight Time was agreed. As Western Australia, Queensland and Northern Territory do not observe daylight saving, this corresponded to 10 pm British Summer Time from March to October. It was decided that 10 pm in the United Kingdom was preferable to 7 am in Australia. Reports from participants in Australia indicated that attending sessions as a group breakfast meeting was well received.
Discussion
Our data, spanning 22 countries and 197 institutions, reflects experiences across a spectrum of professionals involved in providing multidisciplinary tracheostomy care. The significant improvements around perceived knowledge and skills support virtual education in otolaryngology, with the caveat that a lack of impact was observed in technical skills. This finding highlights the importance of hands-on and experiential learning. The finding of pre- and post- webinar improvement is in keeping with prior studies evaluating virtual learning, where healthcare professionals had gain in knowledge comparable to learners receiving traditional teaching (Stain p = 0.65; Joshi p = 0.6; Bertsch p = 0.66).15-17 Black et al performed post-tutorial survey polls, which demonstrated that most survey respondents (71%, n = 89) believed that virtual learning was effective for information sharing and knowledge acquisition.18
Preparing surgeons and other healthcare professionals adequately enhances patient safety and operational efficiencies.4 The global engagement in these efforts to improve tracheostomy care is heartening. Since completion of the current data series, the interest in these virtual forums has increased an order of magnitude, with over 1500 registrants in a recent session. Otolaryngologists, as leaders in airway surgery, can have more impact if they embrace technology. The current COVID-19 pandemic is placing a worldwide strain on healthcare, and it becomes increasingly important to encourage global collaborative learning and sharing of information. The number of tracheostomies performed in critically ill patients will likely increase during the pandemic. There are new considerations such as airway safety and timing of the procedure,19,20 as well as ensuring healthcare worker safety.21 Virtual learning is a valuable medium for rapidly sharing clinician expertise around global strategies to reduce aerosolisation as well as timely topics regarding healthcare disparities.22 During this period, the GTC has run six webinars involving thousands of attendees with broad engagement on timely topics ranging from healthcare worker safety and public health to healthcare disparities. The work described above acted as the stepping-stone to enable this accomplishment.
Advantages of Virtual Learning
Participants in this tutorial series demonstrated high satisfaction with the program, and this finding is significant for a couple of reasons. First, individuals who have a positive experience are more likely to return for future sessions, as demonstrated by the growing engagement in these sessions in recent weeks. A more nuanced reason relates to our goal of cultivating a learning community. To do so, participants must develop a sense of camaraderie and trust. Anecdotally, we can report instances where bonds have formed or strengthened spanning continents, between fellow otolaryngologists and other specialists who see common problems and find common solutions.
Medical education, whether in-person or virtual format, ideally involves bidirectional sharing of ideas. Live virtual learning is highly conducive to this goal. The “question and answer” period at the end of each session allowed participants to share their own ideas and pose questions to the speakers, enabling interactive participant engagement. A collaborative, team-based approach to e-learning facilitates sustainable, responsive and multidisciplinary developments within a field that is constantly changing and evolving.23
Medicine is collaborative,24 and increasingly focused on experiential learning.25 Virtual learning has tremendous potential for collaborative multidisciplinary efforts. The needs of patients with tracheostomies frequently traverse traditional cross-specialty boundaries, requiring collaboration and communication between multiple teams. The series was attended and taught by various specialties, as well as caregivers and community teams. The background of speakers for each session included representation from a minimum of two countries, so as to facilitate an international perspective. Virtual tutorials, such as those conducted in this study, afford participants an opportunity to interact with worldwide experts in a variety of professions as well as patients. Interprofessional education has been shown to improve students’ knowledge of tracheostomy care and professional roles.26,27 Patient involvement in interprofessional education may be beneficial in fostering person-centeredness, particularly in undergraduate students.28,29 The importance of interprofessional education in health professions training is increasingly recognized through new accreditation guidelines,30 and is being implemented in medical curricula as an effective learning method.31 A recent systematic review highlighted positive results in students’ attitudes towards learning and interprofessional collaboration; but highlighted concerns related to difficulties of implementation.31 More insight is required into the design of effective interprofessional education curricula, particularly in the context of virtual training.
Limitations Inherent in Virtual Learning
When technical skills are critical, as in tracheostomy care, virtual learning is ideally combined with in-person simulation, in-services, or other practical training.32 A randomized controlled trial (n = 168) evaluated different versions of a training program for physician-patient or teacher-parent communication.33 The results indicated that a combined method of both e-learning and role play showed the greatest effect; interestingly e-learning proved more effective than role play alone in this particular study.33 A large number of individuals viewed the tutorials in recorded format, rather than the intended live version. This highlights versatility but also difficulties inherent in learning across continents. Survey responses were only requested from individuals who participated in the live activity.
A final limitation relates to fidelity. Satisfactory hardware is crucial for audio and video quality.34,35 There were rare instances of frustrations attributed to loss of audio-visual display, similar to other studies.16,36 In patients with tracheostomies using speaking valves, audibility was also sometimes degraded. Further difficulties may arise from suboptimal device settings. It is advisable to check equipment beforehand and to use mute functions to minimize distractions. Older devices are prone to difficulty. Such issues may be more likely to occur in resource-limited settings. Other initiatives have addressed methods to improve tracheostomy care in such settings, including publishing an electronic open-access online database of tracheostomy care.37
When possible, a fixed/wired Internet connection is preferable to Wi-Fi and mobile networks, which have fluctuating bandwidth. Headsets with USB plugs are beneficial, as high quality inbuilt microphones are uncommon. Echo-suppressing microphones are required when using speakers. Less technologically savvy users may not realize that computers usually default to lower fidelity built-in microphones.
Evaluation of the Series
Future work is needed to assess how virtual tutorials can be combined with direct skills training to drive improvements in outcomes, perhaps by running a tandem standardized practical skills tracheostomy training program for participants following tutorials and addressing relevant skills. Table 4 illustrates candidate outcomes for monitoring. Accredited individuals could run sessions in each country. Additionally, more readily achieved future directions involve refining strategies that allow custom tailoring content to a culturally, geographically, and professionally diverse audience.
Table 4.
Outcomes Monitoring Requirements.
| Suggestion | Comment |
|---|---|
| Demographics | Information regarding study population should be used to contextualize presentation and responses. |
| Educational impact | Pre and post-webinar quizzes is desirable, ultimately with long-term evaluation of impact on professional practice. |
| Audio and visual quality | Fidelity of technology is crucial, as participants can readily disengage if there are unnecessary distractions. |
| Participant satisfaction | Positive responses reflect learning outcomes and can be measured using, for example, 5-point Likert scale. |
It is important that outcomes are evaluated in a structured fashion to ensure monitoring of the learning session. A systematic review of technology-enhanced learning for healthcare professionals found that only 64% of 417 studies presented any form of validity evidence.26 These limitations restrict conclusions, and so from the outset we sought to build rigor into analysis for the present study by adopting the Kirkpatrick methodology. This validation process was developed in industry and is supported by the Best Evidence Medical Education initative.27 The four-part model comprises a series of evaluation levels, to appraise increasingly complex outcomes. However, our experience with this model for outcome monitoring for webinars was challenging, and despite demonstrating improvements in confidence and participant assigned intent to change behaviors in response to the webinars, any such impact is speculative. We therefore have only been able to conclusively demonstrate a benefit in Kirkpatrick level 1.
Further studies are required to determine which aspects of healthcare education are most conducive to virtual learning. There is a need for clear reporting of methodology to ensure reproducibility, to validate outcomes, and to demonstrate sustained impact. The improvement in confidence across many domains and topics found in this study is an encouraging result, as there is a growing body of evidence documenting the importance of self-efficacy and its relation to agency and performance.38 Such work on self-efficacy has been applied to surgical skill acquisition,39 and the significance of nursing comfort level as a barrier to tracheostomy care has also been reported.40
Study Limitations Relating to Data Collection
The number of participants in each session is unknown and easily underestimated. For example, participants from Austin Health, the major health system in Melbourne, Australia, shared that many of its clinicians viewed webinars in a large theater, which is counted as a single registrant with one survey response. Furthermore, the 23% response rate for the follow-up voluntary questionnaire indicates that a preponderance of post-tutorial data was un-captured and introduces a selection bias. One encouraging finding regarding representative sampling is that the proportion of participants completing the survey was uniform across dimensions of country, profession, age, gender, and parent versus adult. These data compare favorably to other electronic survey data in the otolaryngology quality improvement literature, which typically report response rates below 20%.41,42
Conclusion
The COVID-19 pandemic has changed the world permanently, including modifying the fabric of medical education and clinical care. The pervasive use of technology for virtual communication that has been a necessity in a time of social distancing will have a lasting effect across the continuum of medical education, residency, and continuing medical education. Instructional lectures aiming to improve tracheostomy and airway knowledge deficits43 that were previously delivered face-to-face are one such option that could be converted to virtual learning. The Association of American Medical Colleges (AAMC) has created a free and open resource repository to facilitate sharing and disseminating educational approaches. Even once the pandemic subsides, many of the innovations that were effectively shoehorned into our daily lives are here to stay, with hopefully salutary effects on otolaryngology’s educational, clinical, and quality improvement operations. While the experience presented herein with virtual learning was initiated before the pandemic, it nonetheless affords a window into innovations ranging from resident education to virtual care to virtual clinical learning.
Virtual learning allows broader reach than local forums and offers interaction not available in independent online learning. Today’s millennial medical students and practitioners are highly receptive to incorporating technology in learning.44 Literature on mentoring of millennials emphasizes benefits of less hierarchical interactions and flexible approaches, such as micro-mentoring, reverse-mentoring, and adaptable engagement.45 Many aspects of otolaryngology require embracing multidisciplinary approaches, and engagement with technology positions otolaryngologists as innovators who can lead in promoting collaborative learning. The lessons garnered from this endeavor are not only of practical value in preparing for tracheostomy during the COVID-19 outbreak, but also can enhance forward looking quality improvement and educational initiatives.
Acknowledgments
The authors would like to acknowledge the input and support of all the clinicians, healthcare staff, and patients who taught on or attended this educational series.
Footnotes
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: The authors have no financial conflicts of interest. Michael J. Brenner is on the Board of Directors and is president for The Global Tracheostomy Quality Improvement Collaborative (GTC), a 501(c)(3) nonprofit charitable organization with mission of improving tracheostomy care standards.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The authors have received no funding or revenue for this work. The GTC sponsors webinar programming as part of its educational mission and has received unrestricted educational grants from both Medtronic and Smiths Medical.
ORCID iD: Michael J. Brenner  https://orcid.org/0000-0003-4926-0957
https://orcid.org/0000-0003-4926-0957
References
- 1. Arora A, Hettige R, Ifeacho S, Narula A. Driving standards in tracheostomy care: a preliminary communication of the St Mary’s ENT-led multi disciplinary team approach. Clin Otolaryngol. 2008;33(6):596-599. [DOI] [PubMed] [Google Scholar]
- 2. Bedwell JR, Pandian V, Roberson DW, McGrath BA, Cameron TS, Brenner MJ. Multidisciplinary tracheostomy care: how collaboratives drive quality improvement. Otolaryngol Clin North Am. 2019;52(1):135-147. [DOI] [PubMed] [Google Scholar]
- 3. McGrath B, Wilkinson K, Shah RK. Notes from a small island: lessons from the UK NCEPOD tracheotomy report. Otolaryngol Head Neck Surg. 2015;153(2):167-169. [DOI] [PubMed] [Google Scholar]
- 4. McGrath BA, Lynch J, Bonvento B, et al. Evaluating the quality improvement impact of the Global Tracheostomy Collaborative in four diverse NHS hospitals. BMJ Qual Improv Rep. 2017;6(1). doi: 10.1136/bmjquality.u220636.w7996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. McGrath BA, Wallace S, Lynch J, et al. Improving tracheostomy care in the United Kingdom: results of a guided quality improvement programme in 20 diverse hospitals. Br J Anaesth. 2020;125(1):e119-e129. doi: 10.1016/j.bja.2020.04.064 [DOI] [PubMed] [Google Scholar]
- 6. Jenkins KJ, Castañeda AR, Cherian KM, et al. Reducing mortality and infections after congenital heart surgery in the developing world. Pediatrics. 2014;134(5):e1422-e1430. [DOI] [PubMed] [Google Scholar]
- 7. John T, Morton M, Weissman M, et al. Feasibility of a virtual learning collaborative to implement an obesity QI project in 29 pediatric practices. Int J Qual Health Care. 2014;26(2):205-213. [DOI] [PubMed] [Google Scholar]
- 8. Mussman GM, Lossius M, Wasif F, et al. Multisite emergency department inpatient collaborative to reduce unnecessary bronchiolitis care. Pediatrics. 2018;141(2):e20170830. [DOI] [PubMed] [Google Scholar]
- 9. Zocchi MS, McClelland MS, Pines JM. Increasing throughput: results from a 42-hospital collaborative to improve emergency department flow. Jt Comm J Qual Patient Saf. 2015;41(12):532-542. [DOI] [PubMed] [Google Scholar]
- 10. Simpson KR, Knox GE, Martin M, George C, Watson SR. Michigan Health & Hospital Association Keystone Obstetrics: A statewide collaborative for perinatal patient safety in Michigan. Jt Comm J Qual Patient Saf. 2011;37(12):544-552. [DOI] [PubMed] [Google Scholar]
- 11. Zhu H, Das P, Woodhouse R, Kubba H. Improving the quality of tracheostomy care. Breathe. 2014;10(4):286-294. [Google Scholar]
- 12. Brenner MJ, Pandian V, Milliren CE, et al. Global tracheostomy collaborative: data-driven improvements in patient safety through multidisciplinary teamwork, standardisation, education, and patient partnership. Br J Anaesth. 2020;125(1):e104-e118 doi: 10.1016/j.bja.2020.04.054 [DOI] [PubMed] [Google Scholar]
- 13. McCormick ME, Ward E, Roberson DW, Shah RK, Stachler RJ, Brenner MJ. Life after tracheostomy: patient and family perspectives on teaching, transitions, and multidisciplinary teams. Otolaryngol Head Neck Surg. 2015. ;153(6):914-920. [DOI] [PubMed] [Google Scholar]
- 14. Ward E, Pandian V, Brenner MJ. The primacy of patient-centered outcomes in tracheostomy care. Patient. 2018;11(2):143-145. [DOI] [PubMed] [Google Scholar]
- 15. Stain SC, Mitchell M, Belue R, et al. Objective assessment of videoconferenced lectures in a surgical clerkship. Am J Surg 2005;189(1):81-84. [DOI] [PubMed] [Google Scholar]
- 16. Joshi P, Thukral A, Joshi M, Deorari AK, Vatsa M. Comparing the effectiveness of webinars and participatory learning on essential newborn care (ENBC) in the class room in terms of acquisition of knowledge and skills of student nurses: a randomized controlled trial. Indian J Pediatr. 2013;80(2):168-170. [DOI] [PubMed] [Google Scholar]
- 17. Bertsch TF, Callas PW, Rubin A, Caputo MP, Ricci MA. Effectiveness of lectures attended via interactive video conferencing versus in-person in preparing third-year internal medicine clerkship students for Clinical Practice Examinations (CPX). Teach Learn Med 2007;19(1):4-8. [DOI] [PubMed] [Google Scholar]
- 18. Black AT, Clauson M, Fraser S. Nursing education and research rounds: evaluation of a webinar-based education strategy to engage nurses and support practice. J Nurses Prof Dev. 2013;29(5):249-254. [DOI] [PubMed] [Google Scholar]
- 19. McGrath BA, Brenner MJ, Warrillow SJ, et al. Tracheostomy in the COVID-19 era: global and multidisciplinary guidance. Lancet Respir Med. 2020:S2213-2600(20)30230-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Balakrishnan K, Schechtman S, Hogikyan ND, Teoh AYB, McGrath B, Brenner MJ. COVID-19 pandemic: what every otolaryngologist–head and neck surgeon needs to know for safe airway management. Otolaryngol Head Neck Surg. 2020;162:804-808. [DOI] [PubMed] [Google Scholar]
- 21. Zaga CJ, Pandian V, Brodsky MB, et al. Speech-language pathology guidance for tracheostomy during the COVID-19 pandemic: an international multidisciplinary perspective. Am J Speech Lang Pathol. 2020;29(3):1320-1334. doi: 10.1044/2020_AJSLP-20-00089 [DOI] [PubMed] [Google Scholar]
- 22. Graboyes E, Cramer J, Balakrishnan K, et al. COVID-19 pandemic and healthcare disparities in head and neck cancer_ scanning the horizon. Authorea. 2020;42(7):1555-1559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kiteley RJ, Ormrod G. Towards a team-based, collaborative approach to embedding e-learning within undergraduate nursing programmes. Nurse Educ Today. 2009;29(6):623-629. [DOI] [PubMed] [Google Scholar]
- 24. Jamal N, Bowe SN, Brenner MJ, Balakrishnan K, Bent JP. Impact of a formal patient safety and quality improvement curriculum: a prospective, controlled trial. Laryngoscope. 2019;129(5):1100-1106. [DOI] [PubMed] [Google Scholar]
- 25. Morrison RJ, Bowe SN, Brenner MJ. Teaching quality improvement and patient safety in residency education: strategies for meaningful resident quality and safety initiatives. JAMA Otolaryngol Head Neck Surg. 2017;143(11):1069-1070. [DOI] [PubMed] [Google Scholar]
- 26. Darr A, Mughal Z, Siddiq S, Spinou C. Development and evaluation of an interprofessional simulation workshop on assessment and management of tracheostomy and laryngectomy emergencies. J Surg Simul 2016;3:13-22 [Google Scholar]
- 27. Estis JM, Rudd AB, Pruitt B, Wright T. Interprofessional simulation-based education enhances student knowledge of health professional roles and care of patients with tracheostomies and Passy-Muir® Valves. J Nurs Educ Pract. 2015;5:123-128. [Google Scholar]
- 28. Romme S, Bosveld MH, Van Bokhoven MA, De Nooijer J, Van den Besselaar H, Van Dongen JJJ. Patient involvement in interprofessional education: a qualitative study yielding recommendations on incorporating the patient’s perspective. Health Expect. 2020;23(4):943-957. doi: 10.1111/hex.13073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Cherney RL, Pandian V, Ninan A, et al. The trach trail: a systems-based pathway to improve quality of tracheostomy care and interdisciplinary collaboration. Otolaryngol Head Neck Surg. 2020;163(2):232-243. doi: 10.1177/0194599820917427 [DOI] [PubMed] [Google Scholar]
- 30. Lie DA, Forest CP, Kysh L, Sinclair L. Interprofessional education and practice guide No. 5: interprofessional teaching for prequalification students in clinical settings. J Interprof Care. 2016;30(3):324-330. [DOI] [PubMed] [Google Scholar]
- 31. Vuurberg G, Vos JAM, Christoph LH, de Vos R. The effectiveness of interprofessional classroom-based education in medical curricula: a systematic review. J Interprofessional Educ Pract. 2019;15:157-167. [Google Scholar]
- 32. Desimone LM. Improving impact studies of teachers’ professional development: toward better conceptualizations and measures. Educ Res. 2009;38(3):181-199. [Google Scholar]
- 33. Gartmeier M, Bauer J, Fischer MR, et al. Fostering professional communication skills of future physicians and teachers: effects of e-learning with video cases and role-play. Instr Sci. 2015;43(4):443-462. [Google Scholar]
- 34. Carriero A, Beomonte Zobel B, Bonomo L, et al. E-learning in radiology: Italian multicentre experience. Radiol Med. 2011;116(7):989-999. [DOI] [PubMed] [Google Scholar]
- 35. Reid MJ, Flam R, Tsiouris F. New models for medical education: Web-based conferencing to support HIV training in Sub-Saharan Africa. Telemed J E Health 2012;18(7):565-569. [DOI] [PubMed] [Google Scholar]
- 36. Gilkey MB, Moss JL, Roberts AJ, Dayton AM, Grimshaw AH, Brewer NT. Comparing in-person and webinar delivery of an immunization quality improvement program: a process evaluation of the adolescent AFIX trial. Implement Sci. 2014;9(1):1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Sandler ML, Ayele N, Ncogoza I, et al. Improving tracheostomy care in resource-limited settings. Ann Otol Rhinol Laryngol. 2019;129(2):181-190. [DOI] [PubMed] [Google Scholar]
- 38. Bandura A. Self-efficacy mechanism in human agency. Am Psychol. 1982;37:122-147. [Google Scholar]
- 39. Nishisaki A, Keren R, Nadkarni V. Does simulation improve patient safety?: self-efficacy, competence, operational performance, and patient safety. Anesthesiol Clin. 2007;25(2):225-236. [DOI] [PubMed] [Google Scholar]
- 40. Pritchett CV, Rietz MF, Ray A, Brenner MJ, Brown D. Inpatient nursing and parental comfort in managing pediatric tracheostomy care and emergencies. JAMA Otolaryngol Head Neck Surg. 2016;142(2):132-137. [DOI] [PubMed] [Google Scholar]
- 41. Shah RK, Nussenbaum B, Kienstra M, et al. Wrong-site sinus surgery in otolaryngology. Otolaryngol Head Neck Surg. 2010;143(1):37-41. [DOI] [PubMed] [Google Scholar]
- 42. Lavin JM, Boss EF, Brereton J, Roberson DW, Shah RK. Responses to errors and adverse events: the need for a systems approach in otolaryngology. Laryngoscope. 2016;126(9):1999-2002. [DOI] [PubMed] [Google Scholar]
- 43. Hsieh T, Timbang L, Kuhn M, Brodie H, Squires L. Assessment of tracheostomy and laryngectomy knowledge among non-otolaryngology physicians. Ann Otol Rhinol Laryngol. 2019;129(2):115-121. [DOI] [PubMed] [Google Scholar]
- 44. Chu LF, Erlendson MJ, Sun JS, Clemenson AM, Martin P, Eng RL. Information technology and its role in anaesthesia training and continuing medical education. Best Pract Res Clin Anaesthesiol. 2012;26(1):33-53. [DOI] [PubMed] [Google Scholar]
- 45. Waljee JF, Chopra V, Saint S. Mentoring millennials. JAMA. 2018;319(15):1547-1548. [DOI] [PubMed] [Google Scholar]