Abstract
In the field of endodontics, lasers have been used for a long time for the optimization of Endodontic irrigation in particular. The laser-activated irrigation (LAI) technique is based on the photomechanical effects of the lasers at low settings. They create specific cavitation phenomena and acoustic streaming in intracanal fluids. More recently, a new technique with a Er:YAG laser has been used with sub-ablative energy (20 mJ, 15 Hz) and ultra-short pulses (50 µs). This leads to intracanal cavitation and shockwaves as a result of photoacoustic and photomechanical effects. This phenomenon is called photon-induced photoacoustic streaming (PIPS). PIPS and Laser activated irrigation are described in the literature as a revolutionary and powerful method to activate the irrigant; however, systematic literature on this topic is missing. This review compares the literature on Er:YAG LAI and PIPS on endodontic irrigation with other irrigation methods. An article search was performed on the PubMed database using a series of keywords related to endodontic irrigation, including Er:YAG LAI and PIPS; 59 articles were selected for the review according to the inclusion and exclusion criteria. No in vivo study was found. The Er:YAG LAI and PIPS outperformed other methods in 33 of the 59 articles. There was a great variety in the study designs including bacterial incubation time, laser parameters, irrigation protocols, and irrigating solution used. The evidence suggests that the Er:YAG LAI and PIPS are promising in canal disinfection as well as debris and smear layer removal. However, the large variety in the study methods makes the results less significant. Further studies are needed to better evaluate the efficiency of these techniques, especially in vivo studies.
Keywords: Endodontic irrigation, Er:YAG laser, Laser activated irrigation, Photon-induced photoacoustic streaming
Introduction
Endodontics preserves pathologic teeth and restores their functions. A successful endodontic treatment should accomplish the triad of endodontics: shaping, cleaning, and filling of the root canal systems in three dimensions. Although a combination of those three factors needs to be achieved, it is widely accepted that root canal disinfection is central to the outcome of root canal treatment.1,2 This procedure involves removing pulp tissue, bacteria, and related irritants from the root canal systems as well as the smear layer produced during the shaping step.3
Many irrigants, devices, and methods have been introduced for efficient disinfection. Sodium hypochlorite (NaOCl) is considered the gold standard for root canal irrigation thanks to its wide-spectrum, nonspecific antimicrobial efficacy, and great tissue-dissolving capacity.4 NaOCl remains the best primary irrigant versus other traditional antimicrobial agents such as hydrogen peroxide, iodine, and chlorhexidine (CHX) as well as novel agents like MTAD (a mixture of doxycycline, citric acid, and detergent) and QMix (a mixture of ethylenediaminetetraacetic acid (EDTA), CHX, and detergent).5
While powerful as an efficient irrigant, NaOCl cannot accomplish another important aim of root canal irrigation—dissolving inorganic debris and removing and preventing the formation of the smear layer on the root canal walls during instrumentation.6 In addition, root canal calcifications restricting mechanical preparation are common. Therefore, the use of chelator solutions such as EDTA7 and citric acid8,9 at the end of mechanical instrumentation is recommended. The demineralizing agents allow the removal of the smear layer, which consists of dentine debris, pulpal residues, bacteria, and endotoxins. This offers better cleaning and achieves a closer interface between obturation materials and root canal walls.10,11 While the antiseptic effect of chelators is very limited, an alternating irrigating protocol of NaOCl and EDTA may be more efficient than NaOCl alone.12 A final rinse with a disinfecting solution after the smear layer removal is often required because EDTA and citric acid can reduce the antimicrobial properties of NaOCl.13,14
Classically, the irrigation solutions are dispensed from a handheld syringe utilizing a gauge needle with various vent designs. However, this conventional method has several disadvantages due to the complexity of the root canal system and the limitations of the syringe/needle irrigation technique.15 Many disinfection methods have been developed to presumably acquire better intracanal cleaning. Different irrigant agitation techniques have been introduced, including pumping a gutta percha master cone in a fluid-filled canal, activating irrigants with ultrasonic metal tips or sonic nonmetal tips, and energizing irrigants with lasers.
Several laser wavelengths have been investigated for root canal cleaning and disinfecting: erbium:yttrium aluminum garnet (Er:YAG), 2940 nm; erbium, chromium:yttrium scandium gallium garnet (Er,Cr:YSGG), 2780 nm; neodymium:yttrium aluminium garnet (Nd:YAG), 1064 nm; diode, 635 to 980 nm; potassium titanyl phosphate (KTP), 532 nm; carbon dioxide (CO2), 9600 and 10 600 nm. The wavelengths of erbium lasers (Er:YAG, Er,Cr:YSGG) are well absorbed in water and hydroxyapatite; thus, they may have value in agitating irrigation solutions.16
The laser-activated irrigation (LAI) technique is based on the creation of cavitation phenomena and acoustic streaming in intracanal fluids related to the photomechanical effects of the lasers at low settings.17 The strong absorption of the Erbium laser energy in water and NaOCl causes vaporization and formation of vapour bubbles. These large elliptical bubbles implode after 100 to 200 µs, inducing the secondary cavitation effect. More recently, a new technique with a Er:YAG laser has been used with sub-ablative energy (20 mJ, 15 Hz) and ultra-short pulses (50 µs). This leads to intracanal cavitation and shockwaves as a result of photoacoustic and photomechanical effects.18 This phenomenon is called photon-induced photoacoustic streaming (PIPS). In contrast to LAI in which the tips are positioned 5 mm from the apex, PIPS specific tips are kept at the entrance of the root canal, reducing the need for large file instrumentation.19,20 The aim of this study was to review previously published studies and evaluate the effectiveness of Er:YAG LAI with PIPS versus other currently used methods and techniques in endodontic irrigation.
Literature Search Methodology
Data Sources and the Search Strategy
The review was performed as determined by the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) protocols.21 The structured research question was developed by using the population, intervention, comparison, and outcome (PICO) framework: Do PIPS and Er:YAG LAI: (I) perform better (O) than other irrigation methods (C) in in vitro experiments based on extracted tooth samples (P)? A comprehensive literature search was conducted on PubMed (MEDLINE), Ovid (MEDLINE), Web of Science (all databases), SCOPUS, and the Cochrane library from 2008 to 2018. The search strategy used to explore the database was as follows: ((((((((Photon induced photoacoustic streaming) OR Photon initiated photoacoustic streaming) OR Laser activated irrigation) OR Er: YAG laser) OR Sodium hypochlorite irrigation) OR Irrigation solution) OR Photoacoustic streaming) OR Hypochlorite sodium Er YAG). Articles that resulted from the above search strategy were first screened based on the title and abstract. In the second screening, whole articles were read, and articles were excluded based on predetermined exclusion criteria.
Screening and Selection of the Studies
The titles identified by the searches were screened first. If the title indicated possible inclusion, then the abstract was evaluated. In case of any doubt, the full text of the article was read. Following the evaluation of the abstracts, the articles considered eligible for the review were identified, and all of the full-text articles were assessed. Two independent reviewers assessed all the citations. Studies were selected for inclusion if they fulfilled all of the following criteria: a study about endodontic irrigation, a study about the LAI technique, and a study about PIPS. The exclusion criteria of this review were as follows:
1. Study on a plastic bloc simulating the root canal system;
2. Study on non-human teeth;
3. Study on an Er:YAG laser without using PIPS or LAI techniques;
4. Study on Er,Cr:YSGG, diode and neodymium lasers without comparison with an Er:YAG laser;
5. Article not in English.
Data Extraction
Data extraction for the included studies used a data extraction form designed to summarize each study. Data were extracted by one reviewer directly from the full text, and a second reviewer independently verified the extracted data. The following variables were recorded: author information, year of publication, type of teeth, type of laser, number of teeth employed, master apical file, type of laser tip, laser settings, activation time, and concentration of irrigant solutions. Each study was analyzed in terms of similarities so that a meta-analysis could be performed. However, a meta-analysis was not indicated because of the considerable methodological heterogeneity. Rather, a descriptive analysis of the results of the individual studies was undertaken.
Quality Assessment (Risk of Bias)
The quality of each selected study was evaluated based on the following criteria:
(1) Was the calculation of an adequate sample size performed before starting the experiments?
(2) Were the teeth preparations performed by one operator?
(3) Was the teeth preparation procedure standardized?
(4) Were the teeth randomly divided into groups?
(5) Was the irrigating procedure performed by one operator?
(6) Were the same irrigants used in the control groups and test groups?
(7) Was the experience of the operator on the PIPS and LAI techniques reported?
(8) Were the analyses performed by evaluators blinded to the groups?
After collecting these items, the studies were classified with a high, moderate, or low risk of bias. Studies that failed to report five or more of the above items were classified as high risk, studies that failed to report three or four items were classified as moderate risk, and studies that failed to report two items or less were classified as low risk.
Results
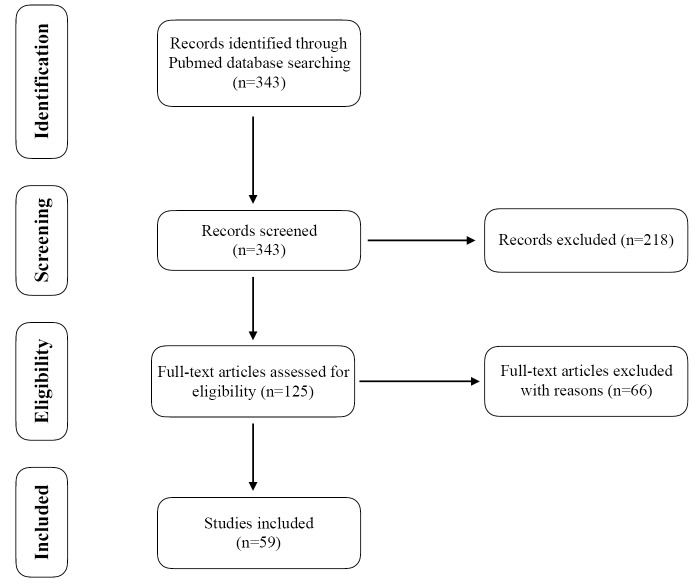
The PubMed database yielded 343 citations in the first screening (title and abstract reviewing) process; 218 articles were selected according to the exclusion criteria, and 125 articles were subjected to full text review for eligibility assessment with 66 additional articles excluded during that process. The final result was the inclusion of 59 articles for this review (Figure 1).
Figure 1.
Articles Selection Flow Chart.
Outcomes and Interests
The 59 articles included in this review were published between 2008 and 2018. Teeth used in the studies are extracted monoradicular human teeth that are generally decoronated to have the same working length. They are instrumented by different file systems and are particularly prepared for each study, including creating artificial intracanal irregularities, incubating microorganisms, cutting in half, and so on. They received different irrigation protocols before being analyzed by optical, confocal, or electronic microscopy. To evaluate the results of these articles, we established the analysis criteria for this review as follows:
Root canal disinfection and debris removal
Smear layer removal
Root canal medication and sealer removal
Resin sealer bond strength
Dentinal tubule penetration
Apical extrusion
Risk of Bias
All 59 included studies were assessed for the risk of bias (Table 1), and only 4 (7%) showed a low risk of bias. Ten (17%) had a high risk. Most studies, 45 (76%), had a medium risk.
Table 1. Quality of Assessment of Reviewed Articles .
| Sample size calculation | Single operator in teeth preparation | Teeth preparation standardization | Teeth randomization | Single operator in teeth irrigation | Same irrigants for control and test groups | Operator experience | Blinding of the evaluator | Classification | |
| George et al, 2008 (75) | N | N | Y | Y | N | Y | N | N | High |
| George et al, 2008 (60) | N | N | N | N | N | Y | N | N | High |
| de Groot et al, 2009 (22) | N | N | Y | N | N | Y | N | Y | High |
| De Moor et al,2010 (23) | N | N | Y | Y | N | Y | N | N | High |
| DiVito et al, 2011 (20) | N | N | Y | Y | N | N | N | N | High |
| Peters et al, 2011 (31) | N | N | Y | N | N | Y | N | N | High |
| DiVito et al, 2012 (19) | N | N | Y | Y | N | N | N | Y | High |
| Jaramillo et al, 2012 (41) | N | N | Y | N | N | Y | N | N | High |
| Pedullà et al, 2012 (42) | N | N | Y | Y | N | Y | N | N | High |
| Sahar-Helft et al, 2013 (50) | N | N | Y | Y | N | Y | N | N | High |
| Zhu et al, 2013 (43) | N | N | Y | N | N | Y | N | Y | High |
| Al Shahrani et al, 2014 (33) | N | N | Y | N | N | Y | N | N | High |
| Arslan et al, 2014 (24) | N | N | Y | N | N | Y | N | Y | High |
| Guidotti et al, 2014 (54) | N | N | Y | N | N | N | N | Y | High |
| Mathew et al, 2014 (45) | N | N | Y | Y | N | Y | N | N | High |
| Olivi et al, 2014 (34) | N | N | Y | Y | N | Y | N | N | High |
| Sathe et al, 2014 (49) | N | N | Y | N | N | Y | N | N | High |
| Akcay et al, 2015 (65) | N | N | Y | Y | N | Y | N | N | High |
| Akyuz Ekim et al, 2015 (52) | N | N | N | N | N | Y | N | Y | High |
| Akyuz Ekim et al, 2015 (66) | N | N | Y | N | N | Y | N | N | High |
| Arslan et al, 2015 (63) | N | N | Y | Y | N | Y | N | N | High |
| Arslan et al, 2015 (67) | N | N | Y | Y | N | Y | N | N | High |
| Arslan et al, 2015 (81) | N | N | Y | Y | N | Y | N | N | High |
| Deleu et al, 2015 (25) | N | N | N | N | N | Y | N | Y | High |
| Li et al, 2015 (61) | N | N | Y | N | N | Y | N | N | High |
| Neelakantan et al, 2015 (35) | N | N | Y | Y | Y | Y | Y | N | Moderate |
| Sahar-Helft et al, 2015 (50) | N | N | Y | Y | N | Y | N | N | High |
| Yost et al, 2015 (72) | N | N | Y | N | N | Y | N | N | High |
| Balić et al, 2016 (44) | N | N | Y | Y | N | Y | N | N | High |
| Akcay et al, 2016 (69) | N | N | Y | Y | N | Y | N | N | High |
| Arslan et al, 2016 (55) | N | N | Y | Y | N | Y | N | N | High |
| Ayranci et al, 2016 (51) | N | N | Y | Y | N | Y | N | N | High |
| Azim et al, 2016 (37) | N | N | Y | N | N | Y | Y | N | High |
| Cheng et al, 2016 (38) | N | N | N | N | N | Y | N | N | High |
| Jaramillo et al, 2016 (36) | N | N | Y | Y | N | Y | N | N | High |
| Keles et al, 2016 (30) | N | N | Y | Y | N | Y | N | N | High |
| Lloyd et al, 2016 (64) | N | N | Y | Y | N | Y | N | Y | Moderate |
| Miletic et al, 2016 (70) | N | N | Y | N | N | Y | N | N | High |
| Nasher et al, 2016 (59) | N | N | N | N | N | Y | N | Y | High |
| Vangala et al, 2016 (71) | N | N | N | Y | N | N | N | N | High |
| Akcay et al, 2017 (68) | N | N | Y | N | N | Y | N | N | High |
| Cheng et al, 2017 (40) | N | N | Y | Y | N | Y | N | N | High |
| Cheng et al, 2017 (46) | N | N | Y | Y | N | Y | N | N | High |
| Gokturk et al, 2017 (62) | N | N | Y | Y | N | Y | N | Y | Moderate |
| Golob et al, 2017 (48) | N | N | Y | N | N | N | N | N | High |
| Kamaci et al, 2017 (27) | N | N | Y | Y | N | Y | N | Y | Moderate |
| Kasić et al, 2017 (47) | N | N | Y | Y | N | Y | N | N | High |
| Mancini et al, 2017 (56) | N | N | Y | Y | N | Y | N | Y | Moderate |
| Ozses Ozkaya et al, 2017 (39) | N | N | Y | Y | N | Y | N | Y | Moderate |
| Suman et al, 2017 (57) | N | N | Y | Y | N | Y | N | Y | Moderate |
| Turkel et al, 2017 (26) | N | N | Y | Y | N | Y | N | Y | Moderate |
| Verstraeten et al, 2017 (28) | N | N | Y | Y | N | Y | N | N | High |
| Arslan et al, 2018 (74) | Y | N | Y | Y | N | Y | N | N | Moderate |
| Azim et al, 2018 (73) | N | N | Y | N | N | Y | Y | N | High |
| Gorus et al, 2018 (53) | N | N | Y | Y | N | Y | N | N | High |
| Ozbay et al, 2018 (58) | N | N | Y | N | N | Y | N | N | High |
| Passalidou et al, 2018 (29) | N | N | Y | Y | N | Y | N | N | High |
Y, reported in the article; N, not reported in the article.
Debris Removal
There were 11 studies that discussed debris removal. Four of them concluded that LAI was more effective than other methods in removing dentine debris from root canals. All four studies found that the PIPS and LAI techniques are significantly more efficient to eliminate debris than conventional syringe irrigation (CSI) alone. Three studies also concluded that the PIPS and LAI techniques remove significantly more apical dentinal debris than passive ultrasonic irrigation (PUI).22-24 Arslan et al24 showed that PIPS is significantly more efficient than EndoActivator.
The authors of the other seven studies found no significantly greater debridement efficacy of PIPS versus Er: YAG LAI or other techniques. They concluded that there is no difference between the LAI technique and/or PIPS groups and PUI,25 EndoVac,26 ultrasonically-activated irrigation (UAI),27-29 manual-activated irrigation (MAI),29 or CSI.26,27 Two articles reported that LAI with an Er: YAG laser eliminated significantly more debris than PIPS (Table 2).25,30
Table 2. Descriptive Data Related to Disinfection and Debris Removal Effect .
| Author/Year | Study Objects | Number of Teeth | MAF | Laser Tip | Laser Settings (Pulse Energy, Repetition Rate, Power, Pulse Widths) | Activation Time | NaOCl | Main Findings |
| de Groot22 (2009) | LAI, PUI, CI | 60 | 35/0.06 | 280 μm, 30 mm | 100 mJ, n/a, n/a, n/a | 50 s | 2% | LAI removed more debris than CI |
| De Moor23 (2010) | LAI, PUI, CI | 100 | 40/0.06 | 200 μm, n/a | 75 mJ, 20 Hz, n/a, n/a | 20 s | 2.5% | LAI removed more debris than CI |
| Peters31 (2011) | PIPS, PUI, CI | 70 | 20/0.07 | 400 μm, 21 mm | 50 mJ, 10 Hz, n/a, n/a | 30 s | 6% | PIPS killed E. faecalis most effectively |
| Jaramillo41 (2012) | PIPS | 24 | 20/0.07 | 400 μm, 14 mm | 20 mJ, 15 Hz, 0.3 W, 50 μs | 20 s | 6% | PIPS inhibited 100% the development of E. faecalis |
| Pedullà42 (2012) | PIPS, CI | 148 | 25/0.06 | 400 μm, 12 mm | 20 mJ, 15 Hz, n/a, 50 μs | 30 s | 5% | No difference in bacterial reduction between groups |
| Sahar-Helft50 (2013) | LAI (Er:YAG), CI | 60 | 30/0.09 | 0.4 μm, n/a | 500 mJ, 12 Hz, n/a, n/a | 4x15 s CHX, 4x15 s EDTA |
2% CHX 17% EDTA |
LAI killed more E. faecalis than CI |
| Zhu43 (2013) | PIPS, CI | 48 | 40/0.06 | 400 μm, 12 mm | 20 mJ, 15 Hz, 0.3 W, 50 μs | 60 s | 3% | No difference in bacterial reduction between groups |
| Al Shahrani33 (2014) | PIPS, CI | 60 | 25/0.08 | 600 μm, 9 mm | 20 mJ, 15 Hz, 0.3 W, 50 μs | 90 s | 6% | PIPS killed more E. faecalis than CI |
| Arslan24 (2014) | PIPS, SI, UAI, CI | 48 | 40/0.06 | 300 μm, 14 mm | 20 mJ, 15 Hz, 0.3 W, 50 μs | 60 s | 1% | PIPS removed debris most effectively |
| Mathew45 (2014) | PIPS, SI, diode laser, CI | 130 | 20/0.07 | 200 μm, n/a | 75 mJ, 20 Hz, n/a, n/a | 60 s NaOCl + 60 s EDTA | 5% NaOCl 17% EDTA |
Diode laser killed E. faecalis most effectively |
| Olivi34 (2014) | PIPS, CI | 26 | 25/0.06 | 600 μm, 9 mm | 20 mJ, 15 Hz, 0.3 W, 50 μs | 60 s | 5% | PIPS inhibited 100% the development of E. faecalis, unlike CI |
| Deleu25 (2015) | PIPS, LAI, PUI, CI, MAI, diode laser | 25 | 30/0.06 | PIPS, LAI: 300 μm, 14 mm | PIPS: 40 mJ, 20 Hz, n/a, 50 μs LAI: 60 mJ, 20 Hz, n/a, 50 μs |
20 s | 2.5% | LAI performed similar to PUI and more effectively than the rest in debris removal |
| Neelakantan35 (2015) | PIPS, UAI, diode laser, CI | 280 | 25/0.06 | 400 μm, 21 mm | 50 mJ, 10 Hz, n/a, 50 ms | 30 s, 60 s, 90 s | 3%, 6% | PIPS performed similarly to the diode laser, both killed more E. faecalis than the rest |
| Balić44(2016) | PIPS, SI, CI | 91 | 30/0.07 | 600 μm, n/a | 20 mJ, 15 Hz, n/a, 50 μs | 60 s | 2.5%, Qmix | No difference in bacterial reduction between groups |
| Lloyd64 (2016) | PIPS, CI | 14 | 30/0.06 | 600 μm, 9 mm | 20 mJ, 15 Hz, 0.3 W, n/a | 240 s | 6% | PIPS removed more debris than CI |
| Jaramillo36 (2016) | PIPS, CI | 48 | 30/0.09 | n/a | n/a | 3x30 s | Buffered 0.5% | PIPS killed more E. faecalis than CI |
| Keleş30 (2016) | PIPS, Er:YAG, Nd:YAG | 42 | 45/ n/a | 300 μm, 14 mm | 50 mJ, 20 Hz, 1 W, 50 μs | 60 s | 5% | Er:YAG LAI removed debris most effectively |
| Azim37 (2016) | PIPS, XP Finisher, SI, CI | 18 | 25/0.04 | n/a | 20 mJ, 15 Hz, n/a, n/a | 3x30 s | 6% | PIPS killed E. faecalis most effectively |
| Cheng38 (2016) | PIPS, CSI | 155 | n/a | 300 μm, n/a | 20 mJ, 15 Hz, 0.3/0.5/1 W, 50 μs | 20/30 s | 5.25% | PIPS killed more E. faecalis than CI |
| Keles30 (2016) | PIPS, LAI (Er:YAG, Nd:YAG), PUI, SAF, CI | 90 | 45/n/a | PIPS, Er:YAG: 300 μm, 14 mm Nd:YAG: 320 μm, n/a |
PIPS: 45 mJ, 20 Hz, 0.9 W, 50 µs LAI: 50 mJ, 20 Hz, 1 W, 50 µs |
PIPS, LAI: 3x10 s PUI, SAF: 60 s |
5% | All other methods removed more debris than CI. The Er:YAG LAI group had the least amount of residual debris |
| Ozses Ozkaya3 (2017) | PIPS, Nd:YAG, CI | 110 | 50/n/a | PIPS: 400 μm, 14 mm Nd:YAG: 200 μm, n/a |
PIPS: 35 mJ, 15 Hz, n/a, 50 μs Nd:YAG: n/a, 15 Hz, 1.5 W, n/a |
PIPS: 20 s LAI: 4x5 s |
1% | PIPS killed more E. faecalis than Nd:YAG when using saline, but similarly when using NaOCl |
| Cheng40 (2017) | PIPS, UAI, CI | 115 | 40/0.04 | 300 μm, n/a | 20 mJ, 25 Hz, 0.5 W, 50 μs | PIPS: 30 s, UI: 60 s | 5.25% | PIPS killed more E. faecalis than CI, but similarly to UAI |
| Kasić47 (2017) | PIPS, LAI (Er,Cr:YSGG), Nd:YAG laser | 30 | 30/0.09 | PIPS: 400 μm, 14 mm LAI, Nd:YAG: 200 μm, n/a |
PIPS: 20 mJ, 15 Hz, 0.3 W, 50 μs LAI: n/a, 15 Hz, 1.25 W, 150 μs Nd:YAG: n/a, 15 Hz, 1.5 W, 100 μs |
PIPS: 40 s LAI: n/a | 0.9% saline | Er,Cr:YSGG killed E. faecalis most effectively, followed by PIPS |
| Cheng46 (2017) | PIPS, CI | 355 | 15/0.04 20/0.04 25/0.04 30/0.04 40/0.04 |
300 μm, n/a | 20 mJ, 15/25/50 Hz, 0.3/0.5/1 W, 50 μs | 20 s, 40 s, 60 s | 5.25% | PIPS improved disinfection efficiency of NaOCl at each apical terminal working width |
| Turkel26 (2017) | PIPS, ANP, CI | 142 | 40/0.06 | 300 μm, 14 mm |
20 mJ, 15 Hz, 0.3 W, 50 μs | 30 s | 5% | PIPS removed debris similarly to ANP, CI |
| Kamaci27 (2017) | PIPS, LAI (diode laser), UAI, CI | 75 | 50/0.05 | PIPS: 300 nm, n/a LAI: 200 μm, n/a |
PIPS: 20 mJ, 15 Hz, 0.3 W, n/a LAI: n/a, n/a, 2 W, n/a |
20 s | 2.5% | UAI removed more debris than CI. No difference between other groups |
| Verstraeten28 (2017) | PIPS, LAI (Er:YAG), UAI | 69 | 30/0.07 | PIPS: 400 μm, 14 mm, LAI: 300 μm, 14 mm |
PIPS: 20 mJ, 20 Hz, n/a, 50 μs LAI: 20 mJ, 20 Hz, n/a, 50 μs |
3x20 s | 2.5% | No difference in debris removal between groups |
| Golob48 (2017) | PIPS | 86 | 30/0.06 | 600 μm, 9 mm | 10/20 mJ, n/a, 0.15/0.3 W, n/a | 30 s NaOCl + 30 s EDTA + 2x30 s NaOCl + 30 s water | 1%, 3%, 5% NaOCl 17% EDTA |
Decontamination was only efficient when using 5% NaOCl |
| Passalidou29 (2018) | LAI (Er:YAG), UAI, MAI, CI | 50 | 25/0.08 | 400/600 μm, n/a | 20 mJ, 20 Hz, n/a, 50 μs | 3x20 s | 2.5% | LAI removed more debris than CI, but similarly to UAI, MAI |
CI, conventional irrigation; LAI, laser-activated irrigation; MAF, master apical file; MAI, manual activated irrigation; n/a, not available; ANP, apical negative pressure; PIPS, photon-induced photoacoustic streaming; PUI, passive ultrasonic irrigation; SAF, self-adjusting file; SI, sonic irrigation; UAI, ultrasonically activated irrigation.
Canal Disinfection
Eighteen studies addressed canal disinfection. Two-thirds of them (11/18) concluded that PIPS had high bacterial killing efficacy, which was significantly more effective than CSI.31-40 This was also more effective than several other activation techniques including PUI,31,35 Nd:YAG irradiation,39 EndoActivator, and XP-endo Finisher file.37 One study found that PIPS coupled with 6% NaOCl inhibited 100% of E. faecalis but did not compare it to other techniques.41
Seven other studies showed no significant improvement in bacterial eradication following the activation by PIPS. The results were tested and compared to CSI,42-44 diode laser irradiation,45 PUI,44 UAI,46 and Er,Cr:YSGG LAI.47 One study varied the laser settings and NaOCl concentration and concluded that the decontamination was only efficient with 5% NaOCl and no irrigation protocol other than PIPS (Table 2).48
Smear Layer Removal
Seventeen studies were included in the analysis of smear layer removal. Seven remarked on better smear layer removal following Er:YAG laser treatment. The authors noticed that Er:YAG lasers were significantly more effective than Nd:YAG LAI and MAI,49 PUI,50,51 diode lasers,52 and CSI.30,50,52,53 They also had better results than ANP (EndoVac), Nd:YAG LAI, and self-adjusting file (SAF) 30,52 but this improvement was not statistically significant. Irrigation with NaOCl and EDTA activated by lasers was significantly better versus NaOCl activated alone, EDTA activated alone, and unactivated EDTA alone.54
The remaining studies showed no superiority of the Er:YAG laser in removing smear layers from root canals versus other techniques including the EndoActivator,55,56 EndoVac,26,56,57 LAI (Nd:YAG, Er,Cr:YSGG),58 and CSI.26,43,59 Despite this, three studies still found that PIPS was better than CSI.55,57,58 The rest only tested PIPS or LAI and did not compare them with other techniques (Table 3).19,20,60
Table 3. Descriptive Data Related to Smear Layer Removal Effect .
| Author | Study objects | Ni. of teeth | MAF | Laser tip | Laser settings (pulse energy, repetition rate, power, pulse widths) | Activation time | EDTA | Main findings |
| George60 (2008) | LAI (Er:YAG, Er,Cr:YSGG) | 150 | 50/0.05 | Er:YAG, Er,Cr:YSGG: 400 μm, n/a | Er:YAG: 200 mJ, 20 Hz, 4 W, n/a Er,Cr:YSGG: 62.5 mJ, 20 Hz, 1.25 W, n/a |
50 s | 15% EDTAC | Conical fibers performed better than plain fibers, no difference between 2 laser systems |
| DiVito20 (2011) | PIPS | 50 | K-file #30 30/0.06 |
400 μm, 14 mm | 20 mJ, 10 Hz, 0.2 W, 50 μs | 20 s, 40 s | 17% | PIPS removed more smear layer with EDTA than with saline and saline alone |
| DiVito19 (2012) | PIPS | 80 | 30/0.06 | 400 μm, 12 mm | 20 mJ, 15 Hz, 0.3 W, 50 μs | 30 s | 17% | PIPS removed more smear layer with EDTA than with saline and saline alone |
| Zhu43 (2013) | PIPS, CI | 48 | 40/0.06 | 400 μm, 12 mm | 20 mJ, 15 Hz, 0.3 W, 50 μs | 60 s | PIPS: 3% NaOCl, CI: 3% NaOCl +17% EDTA | PIPS removed the smear layer similarly to CI |
| Sathe49 (2014) | PIPS, LAI (Nd:YAG), MAI | 30 | 30/0.09 | PIPS: 400 μm, 12 mm LAI: 200 μm,n/a |
PIPS: 40 mJ, 20 Hz, n/a, 50 μs LAI: n/a, 15 Hz, 1.5 W, 50 μs |
PIPS: n/a LAI: 3x5 s NaOCl, 3x5 s EDTA |
17% EDTA 5.25% NaOCl |
PIPS removed more smear layer than LAI, MAI |
| Guidotti54 (2014) | LAI, CI | 48 | 30/0.09 | 300 μm, n/a | 50 mJ, 20 Hz, 1 W, n/a | 3x5 s NaOCl; 3x5 s NaOCl + 3x5 s EDTA; 3x5 s EDTA | 2.5% NaOCl 17% EDTA |
The LAI with NaOCl+EDTA group gave better results than NaOCl alone activated, EDTA alone activated and EDTA alone non-activated groups |
| Akyuz Ekim52(2015) | PIPS, LAI (diode laser, Nd:YAG, Er:YAG), ANP, PUI, CI | 80 | 40/0.06 | PIPS, LAI: 300 μm, 17 mm |
LAI: diode laser (n/a, 15 Hz, 1.5 W, n/a), Nd:YAG (100 mJ, 15 Hz, 1.5 W, n/a), Er:YAG (50 mJ, 10 Hz, 0.5 W, n/a) PIPS: 20 mJ, 15 Hz, 0.3 W, 50 μs |
20 s | 17% | PIPS removed more smear layer than CI and the diode laser, similarly to the rest |
| Sahar-Helft50 (2015) | LAI (Er:YAG), PUI, CI | 60 | 30/0.09 | 400 μm, 17 mm |
50 mJ, 10 Hz, 0.5 W, n/a | 60 s | 17% | LAI removed more smear layer than PUI and CI |
| Arslan55 (2016) | PIPS, LAI (Er:YAG), SI, CI | 64 | 40/0.06 | LAI: 300 μm, n/a PIPS: 400 μm, n/a |
LAI: 50 mJ, 20 Hz, 1 W, n/a PIPS: 20 mJ, 15 Hz, 0.3 W, n/a |
3x20 s | QMix | PIPS performed similarly to SI, both were better than CI |
| Ayranci51 (2016) | LAI (Er:YAG), PUI | 48 | 40/0.06 | 300 μm, 14 mm | n/a, n/a, n/a, 50 ms | 60 s | 17% | LAI removed more smear layer than PUI |
| Nasher59 (2016) | PIPS, CI | 64 | 40/n/a | 600 μm, 9 mm | 20 mJ, 50 Hz, 0.3 W, 50 μs | 2x30 s | 20% | PIPS performed similarly to CI |
| Keles30 (2016) | PIPS, LAI (Er:YAG, Nd:YAG), PUI, SAF, CI | 90 | 45/n/a | PIPS, Er:YAG: 300 μm, 14 mm Nd:YAG: 320 μm, n/a |
PIPS: 45 mJ, 20 Hz, 0.9 W, 50 µs LAI: 50 mJ, 20 Hz, 1 W, 50 µs |
PIPS, LAI: 3x10 s NaOCl + 3x10 s EDTA PUI, SAF: 60 s EDTA + 60 s NaOCl |
5% NaOCl 17% EDTA |
All other methods were more effective than CI. The Er:YAG LAI group had the least amount of residual smear layer |
| Suman57 (2017) | LAI (Er:YAG), SI, ANP, CI | 40 | 40/0.06 | 300 μm, n/a | 50 mJ, 10 Hz, 0.5 W, n/a | LAI: 3x15 s EDTA + 3x15 s NaOCl SI: 60 s EDTA + 60 s NaOCl |
5.25% NaOCl 17% EDTA |
ANP was significantly more effective than all other groups in the apical third. |
| Turkel26 (2017) | PIPS, ANP, CI | 142 | 40/0.06 | 300 μm, 14 mm |
20 mJ, 15 Hz, 0.3 W, 50 μs | 30 s NaOCl + 30 s EDTA | 5% NaOCl 17% EDTA |
PIPS performed similarly to ANP and CI |
| Mancini56 (2017) | LAI (Er:YAG), PUI, ANP, SI | 80 | 40/0.06 | 300 μm, 14 mm |
60 mJ, 20 Hz, n/a, 50 μs | LAI: 4x5 s NaOCl PUI, SI: 60 s NaOCl |
5.25% NaOCl | ANP was the most effective at 1 mm from apex; SI was more effective than PUI, LAI at 3, 5, and 8 mm from apex |
| Gorus53 (2018) | LAI (Er:YAG), CI | 60 | 30/0.09 | n/a | 20/40 mJ, 15 Hz, 0.3/0.6 W, n/a | LAI: 2x3 s NaOCl SI: 60 s NaOCl |
5% NaOCl | LAI removed more smear layer than CI; no difference between parameters |
| Ozbay58 (2018) | PIPS, LAI (Nd:YAG, Er,Cr:YSGG), CI | 96 | 40/0.06 | PIPS: 300 μm, n/a Nd:YAG: 320 μm, n/a Er,Cr:YSGG: 300 μm, n/a |
PIPS: 20 mJ, 15 Hz, 0.3 W, n/a Nd:YAG: 60 mJ, 15 Hz, 1.5 W, n/a Er,Cr:YSGG: n/a, 20 Hz, 1.5 W, 140 ms |
8x5 s distilled water 4x5 s NaOCl + 4x5 s EDTA |
2.5% NaOCl 17% EDTA |
Lasers were more effective than CI; no difference between laser systems |
CI, conventional irrigation; LAI, laser-activated irrigation; MAF, master apical file; n/a, not available; MAI, manual activated irrigation; ANP, apical negative pressure; PIPS, photon-induced photoacoustic streaming; PUI, passive ultrasonic irrigation; SAF, self-adjusting file; SI, sonic irrigation; UAI, ultrasonically activated irrigation.
Root Canal Medication and Sealer Removal
All four studies involving this subject remarked that the use of Er:YAG as PIPS or LAI improved the results. LAI or PIPS produced similar results to PUI in two studies61,62 and better ones in two other studies.63,64 They also performed better than EndoActivator,61,63 XP-endo Finisher file, and CanalBrush.62 They gave better results than CSI in all four studies (Table 4).
Table 4. Descriptive Data Related to Calcium Hydroxide Removal Effect .
| Author | Study Objects | No. of Teeth | MAF | Laser Tip | Laser Settings (Pulse Energy, Repetition Rate, Power, Pulse Widths) | Activation Time | Irrigant | Main Findings |
| Arslan63 (2015) | PIPS, UAI, SI, CI | 48 | 40/0.06 | 300 μm, 14 mm |
30 mJ, 30 Hz, 0.9 W, n/a | PIIPS, UAI: 3x20 s SI: 60 s |
17% EDTA | PIPS performed most effectively |
| Li61 (2015) | PIPS, UAI, SI, CI | 24 | 25/0.08 | 300 μm, 14 mm |
20 mJ, 15 Hz, 0.3 W, n/a | 3x20 s | 3% NaOCl | PIPS and PUI performed similarly, better than the rest |
| Lloyd64 (2016) | PIPS, PUI, CI | 30 | 25/0.06 | 600 μm, 9 mm |
20 mJ, 15 Hz, n/a, n/a | 3x30 s NaOCl + 30 s EDTA | 8.25% NaOCl 17% EDTA |
PIPS performed most effectively |
| Gokturk62 (2017) | LAI (Er:YAG), PUI, SI, XP Finisher, CanalBrush, CI (beveled needle, double side-vented needle) | 105 | 40/0.06 | ISO 30, 28 mm |
100 mJ, 10 Hz, 1 W, n/a | LAI, PUI, XP Finisher, CanalBrush: 60 s SI: 120 s |
2.5% NaOCl | LAI and PUI performed similarly, better than the rest |
CI, conventional irrigation; LAI, laser activated irrigation; MAF, master apical file; n/a, not available; ANP, apical negative pressure; PIPS, photon-induced photoacoustic streaming; PUI, passive ultrasonic irrigation; SI, sonic irrigation; UAI, ultrasonically activated irrigation.
Root Canal Sealer Bond Strength
We included seven studies here. Four of them remarked on higher bond strength of resin sealers following PIPS. PIPS was reported to give significantly better results compared to CSI65-68 and UAI.67 It performed as effectively as PUI in two studies65,69 but better in one study.66 In the latter, PIPS outperformed LAI (Er:YAG, Nd:YAG, diode lasers), PUI, and EndoVac. Nevertheless, the three other studies did not remark on the improved penetration caused by PIPS versus CSI,26,70 MAI,71 and EndoVac (Table 5).26
Table 5. Descriptive Data Related to Resin Sealer Bond Strength .
| Author | Study Objects | No. of Teeth | MAF | Laser Tip | Laser Settings (Pulse Energy, Repetition Rate, Power, Pulse Widths) | Activation Time | Concentration of Irrigant Solutions | Main Findings |
| Akcay65 (2015) | PIPS, PUI, SI, CI | 72 | 40/0.06 | 300 μm, 14 mm |
30 mJ, 30 Hz, 0.9 W, n/a | All 30 s EDTA + 30 s NaOCl | 2.5% NaOCl 17% EDTA |
PIPS and PUI gave similar results, better than the rest |
| Akyuz Ekim66 (2015) | PIPS, LAI (diode laser, Nd:YAG, Er:YAG), ANP, PUI, CI | 32 | 40/0.06 | PIIPS, LAI: 300 μm, n/a | LAI: diode laser (n/a, n/a, 1.2 W, n/a), Nd:YAG (100 mJ, 15 Hz, 1.5 W, n/a), Er:YAG (50 mJ, 10 Hz, 0.5 W, 1000 μs), PIPS: 20 mJ, 15 Hz, 0.3 W, 50 μs | PIPS, LAI, PUI: 4x5 s NaOCl + 4x5 s EDTA, ANP: 20 s NaOCl + 20 s EDTA |
2.5% NaOCl 17% EDTA |
PIPS gave the best result |
| Arslan67 (2015) | PIPS, UAI, CI | 72 | 40/0.06 | 400 μm, 14 mm |
20 mJ, 15 Hz, 0.3 W, n/a | PIPS: 60 s NaOCl, 60 s EDTA UI: 60 s NaOCl |
5% NaOCl 17% EDTA |
PIPS with distilled water gave the best result; negative effect of NaOCl and EDTA on bond strength of RelyX U200 |
| Akcay69 (2016) | PIPS, PUI, CI | 156 | 40/0.06 | 300 μm, 14 mm |
30 mJ, 30 Hz, 0.9 W, 100 μs | All 60 s NaOCl | 5% NaOCl | PIPS and PUI gave similar results, better than CI |
| Miletic70 (2016) | PIPS, CI | 40 | 30/0.09 | 400 μm, 14 mm |
20 mJ, 15 Hz, n/a, 50 μs | 60 s | 17% EDTA | PIPS gave similar result to CI |
| Vangala71 (2016) | PIPS, MAI, CI | 30 | 30/0.09 | n/a | 40 mJ, 20 Hz, n/a, n/a | PIPS: 40 s EDTA MAI: 60 s EDTA |
17% EDTA | PIPS gave similar results to MAI, both were better than CI |
| Turkel26 (2017) | PIPS, ANP, CI | 142 | 40/0.06 | 300 μm, 14 mm |
20 mJ, 15 Hz, 0.3 W, 50 μs | 30 s NaOCl + 30 s EDTA | 5% NaOCl 17% EDTA |
PIPS gave similar results to the rest |
CI, conventional irrigation; MAF, master apical file; MAI, manual activated irrigation; n/a, not available; ANP, apical negative pressure; PIPS, photon-induced photoacoustic streaming; PUI, passive ultrasonic irrigation; UAI, ultrasonically activated irrigation.
Irrigant Penetration in Dentinal Tubules
Only one study69 was found on irrigant penetration into dentinal tubules. The authors concluded that PIPS led to a significantly improved penetration area versus PUI, EndoActivator, and CSI (Table 6).
Table 6. Descriptive Data Related to Irrigant Penetration Into the Dentinal Tubule .
| Author | Study Objects | Number of Teeth | MAF | Laser Tip | Laser Settings (Pulse Energy, Repetition Rate, Power, Pulse Widths) | Activation Time | Irrigant | Main Findings |
| Akcay69 (2017) | PIPS, LAI (Er:YAG), PUI, SI, CI | 65 | 40/0.06 | PIPS, LAI: 300 μm, 14 mm |
PIPS: 30 mJ, 30 Hz, 0.9 W, n/a LAI: 50 mJ, 20 Hz, 1 W, n/a |
60 s NaOCl | 5% NaOCl | Lasers gave the best results |
CI, conventional irrigation; LAI, laser-activated irrigation; MAF, master apical file; n/a, not available; PIPS, photon-induced photoacoustic streaming; PUI, passive ultrasonic irrigation; SI, sonic irrigation.
Apical Extrusion
Three out of five studies concluded that PIPS and Er:YAG LAI produce more extrusion than all other irrigation methods except for CSI in one study.72 Irrigation systems included EndoVac, EndoActivator, XP-endo Finisher file, and CSI.72–74 The two remaining studies concluded that laser activation produced statistically similar amounts of extrusion to UAI and CSI and more than the side-vented needle (Table 7).24,75
Table 7. Descriptive Data Related to Apical Extrusion Effect .
| Author | Study Objects | No. of Teeth | MAF | Laser Tip | Laser Settings (Pulse Energy, Repetition Rate, Power, Pulse Widths) | Activation Time | Irrigants | Main Findings |
| George75 (2008) | LAI (Er:YAG, Er,Cr:YSGG), CI | 16 | 50/0.05 | 400 μm, n/a | Er:YAG: 200 mJ, n/a, 4 W, 50 ms; Er,Cr:YSGG: 62.5 mJ, n/a, 1.25 W, 50 ms | 5 s | Dye | The volume of extruded fluid was similar to conven- tional 25-G needles, but the fluid was distributed further from the apex |
| Arslan81 (2015) | PIPS, UAI, CI | 64 | 30/0.09 | 300 μm, 14 mm | 20 mJ, 15 Hz, 0.3 W, 50 μs; 30 mJ, 30 Hz, 0.9 W, 50 μs |
30 s | 1% Na OCl | PIPS at both 0.3 W and 0.9 W resulted in similar solution extrusion to the conventional irrigation or ultrasonic irrigation |
| Yost72 (2015) | PIPS, ANP, SI, CI | 36 | 35/0.04 55/0.04 |
600 μm, 9 mm |
20 mJ, 15 Hz, n/a, 50 μs 10 mJ, 15 Hz, n/a, 50 μs |
PIPS: 3x30 s SI: 60 s |
6% NaOCl | No difference was found between the 10 mJ and 20 mJ PIPS laser groups. EndoVac demonstrated significantly less potential for apical extrusion than PIPS and Max-i-Probe |
| Arslan74 (2018) | PIPS, CI | 60 | 25/0.06 | 300 μm, 14 mm |
20 mJ, 15 Hz, 0.3 W, 50 μs | 20 s | bidistilled water | PIPS activation was associated with significantly more extrusion debris in curved canals compared with no activation |
| Azim73 (2018) | PIPS, ANP, XP Finisher, SI, CI | 20 | 40/0.04 | n/a | 20 mJ, 15 Hz, n/a, n/a | 3x30 s | 3% NaOCl | PIPS extrudes more irrigant than other systems |
CI, conventional irrigation; LAI, laser-activated irrigation; MAF, master apical file; n/a, not available; ANP, apical negative pressure; PIPS, photon-induced photoacoustic streaming; SI, sonic irrigation; UAI, ultrasonically activated irrigation.
Discussion
PIPS and LAI techniques are described in the literature as a revolutionary and powerful method to activate the irrigant. These tools use the photothermal effect of direct irradiation as well as the photoacoustic effect. The main advantage is to overcome unwanted effects on the carbonization of the root canal dentin. PIPS studies tend to replace the LAI technique. In fact, 17 of the 55 articles published since 2011 (year of the first PIPS article) cover the LAI technique.
This review shows heterogeneity in the protocols tested: laser fiber parameters, laser parameters, irrigant concentration, activation time, and the number of activation cycles. There are also differences in sample preparation: the type of the teeth, the state of the teeth (freshly extracted or coming from a collection), the teeth preparation protocol, incubation methods, bacterial counting methods, and analysis methods. Other factors such as the experience of the operators and the differences in irrigant use between test and control groups can also affect the results.
We found that 11 of 18 articles concluded that the Er:YAG laser benefited the activation procedure as judged by disinfection outcomes. However, there is little evidence in terms of evidence-based medicine because these studies were in vitro or ex vivo studies. The teeth were only infected with E. faecalis . The clinical reality is a poly-microbial infection, even including fungi. To date, no experimental in vitro model has reproduced endodontic biofilms.76 Its elimination via the PIPS or LAI technique has never been explored. In addition, some studies19,20,41,48,60 only examined the LAI technique or PIPS without comparison to other techniques. The absence of in vivo studies or clinical trials reduces the scientific power of the Er:YAG laser for the activation of irrigating solutions. Additional clinical research studies, especially in vivo studies, are required to prove the scientific efficacy of these techniques and establish a sufficient level of proof.
Another factor to be considered is the irrigating solutions. Three major irrigants were used: NaOCl, EDTA, and QMix. There is a large variety in the concentration of NaOCl: 1%, 2%, 2.5%, 3%, 5%, 5.25%, and 6%. The 2.5% NaOCl was found to be better due to its higher efficiency and lower cytotoxicity.77 However, 6% NaOCl was shown to be the most effective disinfecting solution against a 3-week-old E. faecalis biofilm.78 The articles used various incubation times to evaluate the effectiveness of E. faecalis disinfection protocols: 2 weeks, 3 weeks, and 4 weeks. Other authors found that the E. faecalis biofilm was not completely established until 3 weeks.76
We only found consensus in the results on the removal of root canal medication and sealer—all studies remarked that the use of the Er:YAG laser improved the results versus other removal methods. Many factors such as the variation in sample conditions, irrigating protocols, and irrigating solutions hamper direct comparison of the results of the studies. The lack of concrete scientific proof makes it difficult to draw broad conclusions about the effectiveness of PIPS and LAI.
Nevertheless, we conclude that irrigation is a key element of endodontic success. The PIPS technique is a time-saving tool for clinicians. An important advantage of this technique is that the irrigant is propelled throughout the entire root canal system. Thus, we should discuss the results to establish a complete operating protocol and prognosis for treated teeth.
There are no clear recommendations in the literature about irrigation or activation times.35 The duration of the application should be as short as possible but with maximum efficiency. There is no consensus on application time. We noted a wide variety of activation times from 20 seconds to 240 seconds; none of the articles reviewed worked to create a reproducible protocol.
A complete clinical protocol for the final rinse was first suggested in 2012.79 The protocol is three cycles of 30-second activation by PIPS with NaOCl followed by three rounds of 30-second off cycles. The next step is 30 seconds of irrigation using PIPS with water only. EDTA is then used with PIPS for 30 seconds, and finally, a 30-second cycle with PIPS and water is applied. One publication also tested this effectiveness and concluded that this protocol was the most effective compared to CI and PUI.64
Several laser parameters are also important. Meire et al reported that greater energy (40 mJ compared to 10 and 20 mJ) coupled with 30 Hz of frequency eliminates more root canal debris. There are more powerful photoacoustic shockwaves at higher powers.80 We note that the energy used for the LAI technique can go up to 500 mJ32 with 4 W of power.60,75 However, no other publication has reported such parameters. Moreover, recently published articles showed that this technique used parameters close to those of PIPS. The use of PIPS at the 20 mJ/0.3 W setting was reported to be effective in removing the smear layer without any damage to the dentinal tissue.19 Cheng et al also tested the Er:YAG laser at 0.3, 0.5, and 1.0 W for either 20 or 30 seconds. They concluded that the most efficient methods were activation with 0.5 and 1.0 W for 30 seconds.38 Laser activation at 0.5 W for 30 seconds combined with NaOCl is the preferable option because of the lower emission power. In addition, PIPS used at either 10 or 20 mJ and 0.3 or 0.9 W produced a similar apical extrusion volume.72,81 It would be interesting to test these parameters in clinical situations by exploring postoperative pain differences.82
Conclusion
In the field of endodontics, PIPS and Laser activated irrigation are described in the literature as a revolutionary and powerful method to activate the irrigant. The aim of this study was to review previously published studies and evaluate the effectiveness of Er:YAG LAI with PIPS versus other currently used methods and techniques in endodontic irrigation. There was a great variety in the study designs including bacterial incubation time, laser parameters, irrigation protocols, and irrigating solution used. The evidence suggests that Er:YAG LAI and PIPS are promising in canal disinfection as well as debris and smear layer removal. However, the large variety in the study methods makes the results less significant. Further studies are needed to better evaluate the efficiency of these techniques, especially in vivo studies.
Ethical Considerations
Not applicable.
Conflict of Interests
The authors declare no conflict of interest.
Please cite this article as follows: Do QL, Gaudin A. The Efficiency of the Er: YAG laser and photon-induced photoacoustic streaming (PIPS) as an activation method in endodontic irrigation: A literature review. J Lasers Med Sci. 2020;11(3):316-331. doi:10.34172/jlms.2020.53.
References
- 1.Haapasalo M, Shen Y, Wang Z, Gao Y. Irrigation in endodontics. Br Dent J. 2014;216(6):299–303. doi: 10.1038/sj.bdj.2014.204. [DOI] [PubMed] [Google Scholar]
- 2.Kandaswamy D, Venkateshbabu N. Root canal irrigants. J Conserv Dent. 2010;13(4):256–264. doi: 10.4103/0972-0707.73378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Peters OA, Laib A, Göhring TN, Barbakow F. Changes in root canal geometry after preparation assessed by high-resolution computed tomography. J Endod. 2001;27(1):1–6. doi: 10.1097/00004770-200101000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Moorer WR, Wesselink PR. Factors promoting the tissue dissolving capability of sodium hypochlorite. Int Endod J. 1982;15(4):187–196. doi: 10.1111/j.1365-2591.1982.tb01277.x. [DOI] [PubMed] [Google Scholar]
- 5.Abbott P V. Medicaments: aids to success in endodontics Part 1 A review of the literature. Aust Dent J. 1990;35(5):438–448. doi: 10.1111/j.1834-7819.1990.tb05427.x. [DOI] [PubMed] [Google Scholar]
- 6.Zehnder M. Root Canal Irrigants. J Endod. 2006;32(5):389–398. doi: 10.1016/j.joen.2005.09.014. [DOI] [PubMed] [Google Scholar]
- 7.Mohammadi Z, Shalavi S, Yaripour S, Kinoshita JI, Manabe A, Kobayashi M. et al. Smear layer removing ability of root canal irrigation solutions: a review. J Contemp Dent Pract. 2019;20(3):395–402. [PubMed] [Google Scholar]
- 8.Loel DA. Use of acid cleanser in endodontic therapy. J Am Dent Assoc. 1975;90(1):148–151. doi: 10.14219/jada.archive.1975.0010. [DOI] [PubMed] [Google Scholar]
- 9.Yamaguchi M, Yoshida K, Suzuki R, Nakamura H. Root canal irrigation with citric acid solution. J Endod. 1996;22(1):27–29. doi: 10.1016/S0099-2399(96)80232-9. [DOI] [PubMed] [Google Scholar]
- 10.Torabinejad M, Handysides R, Khademi AA, Bakland LK. Clinical implications of the smear layer in endodontics: A review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;94(6):658–666. doi: 10.1067/moe.2002.128962. [DOI] [PubMed] [Google Scholar]
- 11.Kokkas AB, Boutsioukis AC, Vassiliadis LP, Stavrianos CK. The influence of the smear layer on dentinal tubule penetration depth by three different root canal sealers: An in vitro study. J Endod. 2004;30(2):100–102. doi: 10.1097/00004770-200402000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Rossi-Fedele G, Guastalli AR, Doǧramaci EJ, Steier L, De Figueiredo JA. Influence of pH changes on chlorine-containing endodontic irrigating solutions. Int Endod J. 2011;44(9):792–799. doi: 10.1111/j.1365-2591.2011.01911.x. [DOI] [PubMed] [Google Scholar]
- 13.Baumgartner JC, Ibay AC. The chemical reactions of irrigants used for root canal debridement. J Endod. 1987;13(2):47–51. doi: 10.1016/S0099-2399(87)80153-X. [DOI] [PubMed] [Google Scholar]
- 14.Grawehr M, Sener B, Waltimo T, Zehnder M. Interactions of ethylenediamine tetraacetic acid with sodium hypochlorite in aqueous solutions. Int Endod J. 2003;36(6):411–417. doi: 10.1046/j.1365-2591.2003.00670.x. [DOI] [PubMed] [Google Scholar]
- 15.Jiang LM, Lak B, Eijsvogels LM, Wesselink P, van der Sluis LW. Comparison of the cleaning efficacy of different final irrigation techniques. J Endod. 2012;38(6):838–841. doi: 10.1016/j.joen.2012.03.002. [DOI] [PubMed] [Google Scholar]
- 16.Diaci J, Gaspirc B. Comparison of Er:YAG and Er,Cr:YSGG lasers used in dentistry. J Laser Health Acad. 2012;2012(1):1–13. [Google Scholar]
- 17.Mir M, Gutknecht N, Poprawe R, Vanweersch L, Lampert F. Visualising the procedures in the influence of water on the ablation of dental hard tissue with erbium:yttrium-aluminium-garnet and erbium, chromium:yttrium-scandium-gallium-garnet laser pulses. Lasers Med Sci. 2009;24(3):365–374. doi: 10.1007/s10103-008-0571-1. [DOI] [PubMed] [Google Scholar]
- 18.Olivi G, DiVito E. Photoacoustic endodontics using PIPS: experimental background and clinical protocol. J Laser Health Acad. 2012;2012(1):22–25. [Google Scholar]
- 19.DiVito E, Peters OA, Olivi G. Effectiveness of the erbium: YAG laser and new design radial and stripped tips in removing the smear layer after root canal instrumentation. Lasers Med Sci. 2012;27(2):273–280. doi: 10.1007/s10103-010-0858-x. [DOI] [PubMed] [Google Scholar]
- 20.DiVito EE, Colonna MP, Olivi G. The Photoacoustic Efficacy of an Er:YAG Laser with Radial and Stripped Tips on Root Canal Dentin Walls: An SEM Evaluation. J Laser Dent. 2011;19(1):156–161. [Google Scholar]
- 21.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M. et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.de Groot SD, Verhaagen B, Versluis M, Wu MK, Wesselink PR, van ders Sluis LW. Laser-activated irrigation within root canals: Cleaning efficacy and flow visualization. Int Endod J. 2009;42(12):1077–1083. doi: 10.1111/j.1365-2591.2009.01634.x. [DOI] [PubMed] [Google Scholar]
- 23.De Moor RJ, Meire M, Goharkhay K, Moritz A, Vanobbergen J. Efficacy of ultrasonic versus laser-activated irrigation to remove artificially placed dentin debris plugs. J Endod. 2010;36(9):1580–1583. doi: 10.1016/j.joen.2010.06.007. [DOI] [PubMed] [Google Scholar]
- 24.Arslan H, Capar ID, Saygili G, Gok T, Akcay M. Effect of photon-initiated photoacoustic streaming on removal of apically placed dentinal debris. Int Endod J. 2014;47(11):1072–1077. doi: 10.1111/iej.12251. [DOI] [PubMed] [Google Scholar]
- 25.Deleu E, Meire MA, De Moor RJ. Efficacy of laser-based irrigant activation methods in removing debris from simulated root canal irregularities. Lasers Med Sci. 2015;30(2):831–835. doi: 10.1007/s10103-013-1442-y. [DOI] [PubMed] [Google Scholar]
- 26.Turkel E, Onay EO, Ungor M. Comparison of three final irrigation activation techniques: effects on canal cleanness, smear layer removal, and dentinal tubule penetration of two root canal sealers. Photomed Laser Surg. 2017;35(12):672–681. doi: 10.1089/pho.2016.4234. [DOI] [PubMed] [Google Scholar]
- 27.Kamaci A, Aydin B, Erdilek N. The effect of ultrasonically activated irrigation and laser based root canal irrigation methods on debris removal. Int J Artif Organs. 2018;41(2):71–75. doi: 10.5301/ijao.5000646. [DOI] [PubMed] [Google Scholar]
- 28.Verstraeten J, Jacquet W, De Moor RJ, Meire MA. Hard tissue debris removal from the mesial root canal system of mandibular molars with ultrasonically and laser-activated irrigation: a micro-computed tomography study. Lasers Med Sci. 2017;32(9):1965–1970. doi: 10.1007/s10103-017-2297-4. [DOI] [PubMed] [Google Scholar]
- 29.Passalidou S, Calberson F, De Bruyne M, De Moor R, Meire MA. Debris removal from the mesial root canal system of mandibular molars with laser-activated irrigation. J Endod. 2018;44(11):1697–1701. doi: 10.1016/j.joen.2018.06.007. [DOI] [PubMed] [Google Scholar]
- 30.Keles A, Kamalak A, Keskin C, Akçay M, Uzun İ. The efficacy of laser, ultrasound and self-adjustable file in removing smear layer debris from oval root canals following retreatment: A scanning electron microscopy study. Aust Endod J. 2016;42(3):104–111. doi: 10.1111/aej.12145. [DOI] [PubMed] [Google Scholar]
- 31.Peters OA, Bardsley S, Fong J, Pandher G, Divito E. Disinfection of root canals with photon-initiated photoacoustic streaming. J Endod. 2011;37(7):1008–1012. doi: 10.1016/j.joen.2011.03.016. [DOI] [PubMed] [Google Scholar]
- 32.Sahar-Helft S, Stabholtz A, Moshonov J, Gutkin V, Redenski I, Steinberg D. Effect of Er:YAG laser-activated irrigation solution on Enterococcus faecalis biofilm in an ex-vivo root canal model. Photomed Laser Surg. 2013;31(7):334–341. doi: 10.1089/pho.2012.3445. [DOI] [PubMed] [Google Scholar]
- 33.Al Shahrani M, DiVito E, Hughes CV, Nathanson D, Huang GT. Enhanced removal of Enterococcus faecalis biofilms in the root canal using sodium hypochlorite plus photon-induced photoacoustic streaming: An in vitro study. Photomed Laser Surg. 2014;32(5):260–266. doi: 10.1089/pho.2014.3714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Olivi G, DiVito E, Peters O, Kaitsas V, Angiero F, Signore A. et al. Disinfection efficacy of photon-induced photoacoustic streaming on root canals infected with Enterococcus faecalis: An ex vivo study. J Am Dent Assoc. 2014;145(8):843–848. doi: 10.14219/jada.2014.46. [DOI] [PubMed] [Google Scholar]
- 35.Neelakantan P, Cheng CQ, Mohanraj R, Sriraman P, Subbarao C, Sharma S. Antibiofilm activity of three irrigation protocols activated by ultrasonic, diode laser or Er:YAG laser in vitro. Int Endod J. 2015;48(6):602–610. doi: 10.1111/iej.12354. [DOI] [PubMed] [Google Scholar]
- 36.Jaramillo DE, Aguilar E, Arias A, Ordinola-Zapata R, Aprecio RM, Ibarrola JL. Root canal disinfection comparing conventional irrigation vs photon-induced photoacoustic streaming (PIPS) using a buffered 05 % sodium hypochlorite solution. Evid Based Endod. 2016;1(1):6. doi: 10.1186/s41121-016-0006-6. [DOI] [Google Scholar]
- 37.Azim AA, Aksel H, Zhuang T, Mashtare T, Babu JP, Huang GT. Efficacy of 4 irrigation protocols in killing bacteria colonized in dentinal tubules examined by a novel confocal laser scanning microscope analysis. J Endod. 2016;42(6):928–34. doi: 10.1016/j.joen.2016.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cheng X, Chen B, Qiu J, He W, Lv H, Qu T. et al. Bactericidal effect of Er:YAG laser combined with sodium hypochlorite irrigation against Enterococcus faecalis deep inside dentinal tubules in experimentally infected root canals. J Med Microbiol. 2016;65(2):176–187. doi: 10.1099/jmm.0.000205. [DOI] [PubMed] [Google Scholar]
- 39.Ozses Ozkaya B, Gulsahi K, Ungor M, Gocmen JS. A Comparison of Er:YAG laser with photon-initiated photoacoustic streaming, Nd:YAG laser, and conventional irrigation on the eradication of root dentinal tubule infection by Enterococcus faecalis Bbofilms: A Scanning electron microscopy study. Scanning. 2017;2017:6215482. doi: 10.1155/2017/6215482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cheng X, Xiang D, He W, Qiu J, Han B, Yu Q. et al. Bactericidal Effect of Er:YAG laser-activated sodium hypochlorite irrigation against biofilms of Enterococcus faecalis isolate from canal of root-filled teeth with periapical lesions. Photomed Laser Surg. 2017;35(7):386–392. doi: 10.1089/pho.2017.4293. [DOI] [PubMed] [Google Scholar]
- 41.Jaramillo DE, Aprecio RM, Angelov N, Divito E. Efficacy of photon induced photoacoustic streaming (PIPS) on root canals infected with Enterococcus faecalis: A pilot study. Endod Prac. 2012;5(3):28–32. [Google Scholar]
- 42.Pedullà E, Genovese C, Campagna E, Tempera G, Rapisarda E. Decontamination efficacy of photon-initiated photoacoustic streaming (PIPS) of irrigants using low-energy laser settings: An ex vivo study. Int Endod J. 2012;45:865–870. doi: 10.1111/j.1365-2591.2012.02044.x. [DOI] [PubMed] [Google Scholar]
- 43.Zhu X, Yin X, Chang JW, Wang Y, Cheung GS, Zhang C. Comparison of the Antibacterial effect and smear layer removal using photon-initiated photoacoustic streaming aided irrigation versus a conventional irrigation in single-rooted canals: An in vitro study. Photomed Laser Surg. 2013;31(8):371–377. doi: 10.1089/pho.2013.3515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Balić M, Lucić R, Mehadžić K, Bago I, Anić I, Jakovljević S. et al. faecalis biofilm. Lasers Med Sci. 2016;31(2):335–342. doi: 10.1007/s10103-015-1864-9. [DOI] [PubMed] [Google Scholar]
- 45.Mathew J, Emil J, Paulaian B, John B, Raja J, Mathew J. Viability and antibacterial efficacy of four root canal disinfection techniques evaluated using confocal laser scanning microscopy. J Conserv Dent. 2014;17(5):444–448. doi: 10.4103/0972-0707.139833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cheng X, Tian T, Tian Y, Xiang D, Qiu J, Liu X. et al. Erbium:yttrium aluminum garnet laser-activated sodium hypochlorite irrigation: A promising procedure for minimally invasive Endodontics. Photomed Laser Surg. 2017;35(12):695–701. doi: 10.1089/pho.2017.4274. [DOI] [PubMed] [Google Scholar]
- 47.Kasić S, Knezović M, Beader N, Gabrić D, Malčić AI, Baraba A. Efficacy of three different lasers on eradication of Enterococcus faecalis and Candida albicans biofilms in root canal system. Photomed Laser Surg. 2017;35(7):372–377. doi: 10.1089/pho.2016.4258. [DOI] [PubMed] [Google Scholar]
- 48.Golob BS, Olivi G, Vrabec M, El Feghali R, Parker S, Benedicenti S. Efficacy of photon-induced photoacoustic streaming in the reduction of Enterococcus faecalis within the root canal: Different settings and different sodium hypochlorite concentrations. J Endod. 2017;43(10):1730–1735. doi: 10.1016/j.joen.2017.05.019. [DOI] [PubMed] [Google Scholar]
- 49.Sathe S, Hegde V, Jain PA, Ghunawat D. Effectiveness of Er: YAG (PIPS) and Nd: YAG activation on final irrigants for smear layer removal - SEM observation. J Dent Lasers. 2014;8(1):8–13. doi: 10.4103/0976-2868.134110. [DOI] [Google Scholar]
- 50.Sahar-Helft S, Sarp AS, Stabholtz A, Gutkin V, Redenski I, Steinberg D. Comparison of positive-pressure, passive ultrasonic, and laser-activated irrigations on smear-layer removal from the root canal surface. Photomed Laser Surg. 2015;33(3):129–135. doi: 10.1089/pho.2014.3788. [DOI] [PubMed] [Google Scholar]
- 51.Ayranci LB, Arslan H, Akcay M, Capar ID, Gok T, Saygili G. Effectiveness of laser-assisted irrigation and passive ultrasonic irrigation techniques on smear layer removal in middle and apical thirds. Scanning. 2016;38(2):121–127. doi: 10.1002/sca.21247. [DOI] [PubMed] [Google Scholar]
- 52.Akyuz Ekim SN, Erdemir A. Comparison of different irrigation activation techniques on smear layer removal: An in vitro study. Microsc Res Tech. 2015;78(3):230–239. doi: 10.1002/jemt.22466. [DOI] [PubMed] [Google Scholar]
- 53.Gorus Z. A comparative evaluation of smear layer removal by using different Er:YAG lasers parameters: an in-vitro scanning electron microscopic study. Niger J Clin Pract. 2018;21(12):1602–6. doi: 10.4103/njcp.njcp_317_18. [DOI] [PubMed] [Google Scholar]
- 54.Guidotti R, Merigo E, Fornaini C, Rocca JP, Medioni E, Vescovi P. Er:YAG 2,940-nm laser fiber in endodontic treatment: A help in removing smear layer. Lasers Med Sci. 2014;29(1):69–75. doi: 10.1007/s10103-012-1217-x. [DOI] [PubMed] [Google Scholar]
- 55.Arslan D, Guneser MB, Dincer AN, Kustarci A, Er K, Siso SH. Comparison of smear layer removal ability of QMix with different activation techniques. J Endod. 2016;42(8):1279–1285. doi: 10.1016/j.joen.2016.04.022. [DOI] [PubMed] [Google Scholar]
- 56.Mancini M, Cerroni L, Iorio L, Dall’Asta L, Cianconi L. FESEM evaluation of smear layer removal using different irrigant activation methods (EndoActivator, EndoVac, PUI and LAI) An in vitro study. Clin Oral Investig. 2018;22(2):993–999. doi: 10.1007/s00784-017-2179-y. [DOI] [PubMed] [Google Scholar]
- 57.Suman S, Verma P, Prakash-Tikku A, Bains R, Kumar-Shakya V. A comparative evaluation of smear layer removal using apical negative pressure (EndoVac), sonic irrigation (EndoActivator) and Er:YAG laser -An in vitro SEM study. J Clin Exp Dent. 2017;9(8):e981–e987. doi: 10.4317/jced.53881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ozbay Y, Erdemir A. Effect of several laser systems on removal of smear layer with a variety of irrigation solutions. Microsc Res Tech. 2018;81(10):1214–1222. doi: 10.1002/jemt.23122. [DOI] [PubMed] [Google Scholar]
- 59.Nasher R, Franzen R, Gutknecht N. The effectiveness of the Erbium:Yttrium aluminum garnet PIPS technique in comparison to different chemical solutions in removing the endodontic smear layer An in vitro profilometric study. Lasers Med Sci. 2016;31(9):1871–1882. doi: 10.1007/s10103-016-2063-z. [DOI] [PubMed] [Google Scholar]
- 60.George R, Meyers IA, Walsh LJ. Laser activation of endodontic irrigants with improved conical laser fiber tips for removing smear layer in the apical third of the root canal. J Endod. 2008;34(12):1524–1527. doi: 10.1016/j.joen.2008.08.029. [DOI] [PubMed] [Google Scholar]
- 61.Li D, Jiang S, Yin X, Chang JW, Ke J, Zhang C. Efficacy of needle, ultrasonic, and endoactivator irrigation and photon-induced photoacoustic streaming in removing calcium hydroxide from the main canal and isthmus: An in vitro micro-computed tomography and scanning electron microscopy study. Photomed Laser Surg. 2015;33(6):330–337. doi: 10.1089/pho.2015.3903. [DOI] [PubMed] [Google Scholar]
- 62.Gokturk H, Ozkocak I, Buyukgebiz F, Demir O. Effectiveness of various irrigation protocols for the removal of calcium hydroxide from artificial standardized grooves. J Appl Oral Sci. 2017;25(3):290–298. doi: 10.1590/1678-7757-2016-0414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Arslan H, Akcay M, Capar ID, Saygili G, Gok T, Ertas H. An in vitro comparison of irrigation using photon-initiated photoacoustic streaming, ultrasonic, sonic and needle techniques in removing calcium hydroxide. Int Endod J. 2015;48(3):246–251. doi: 10.1111/iej.12306. [DOI] [PubMed] [Google Scholar]
- 64.Lloyd A, Navarrete G, Marchesan MA, Clement D. Removal of calcium hydroxide from Weine Type II systems using photon-induced photoacoustic streaming, passive ultrasonic, and needle irrigation: a microcomputed tomography study. J Appl Oral Sci. 2016;24(6):543–548. doi: 10.1590/1678-775720160234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Akcay M, Arslan H, Mese M, Sahin NN. The effect of photon-initiated photoacoustic streaming, ultrasonically and sonically irrigation techniques on the push-out bond strength of a resin sealer to the root dentin. Clin Oral Investig. 2015;19(5):1055–1061. doi: 10.1007/s00784-014-1332-0. [DOI] [PubMed] [Google Scholar]
- 66.Akyuz Ekim SN, Erdemir A. Effect of different irrigant activation protocols on push-out bond strength. Lasers Med Sci. 2015;30(8):2143–2149. doi: 10.1007/s10103-015-1772-z. [DOI] [PubMed] [Google Scholar]
- 67.Arslan H, Akcay M, Saygili G, Keskı A, MeŞe İT, Gok A. et al. Comparison of photon-initiated photoacoustic streaming technique with needle and ultrasonic irrigation. Acta Odontol Scand. 2015;73(5):348–52. doi: 10.3109/00016357.2014.967717. [DOI] [PubMed] [Google Scholar]
- 68.Akcay M, Arslan H, Mese M, Durmus N, Capar ID. Effect of photon-initiated photoacoustic streaming, passive ultrasonic, and sonic irrigation techniques on dentinal tubule penetration of irrigation solution: a confocal microscopic study. Clin Oral Investig. 2017;21(7):2205–2212. doi: 10.1007/s00784-016-2013-y. [DOI] [PubMed] [Google Scholar]
- 69.Akcay M, Arslan H, Durmus N, Mese M, Capar ID. Dentinal tubule penetration of AH Plus, iRoot SP, MTA fillapex, and guttaflow bioseal root canal sealers after different final irrigation procedures: A confocal microscopic study. Lasers Surg Med. 2016;48(1):70–76. doi: 10.1002/lsm.22446. [DOI] [PubMed] [Google Scholar]
- 70.Miletić I, Chieffi N, Rengo C, Ferrari M, Nathanson D, Baraba A. Effect of photon induced photoacoustic streaming (PIPS) on bond strength to dentine of two root canal filling materials. Lasers Surg Med. 2016;48(10):951–954. doi: 10.1002/lsm.22536. [DOI] [PubMed] [Google Scholar]
- 71.Vangala A, Hegde V, Sathe S, Dixit M, Jain P. Effect of irrigating solutions used for postspace treatment on the push-out bond strength of glass fiber posts. J Conserv Dent. 2016;19(1):82–6. doi: 10.4103/0972-0707.173206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Yost RA, Bergeron BE, Kirkpatrick TC, Roberts MD, Roberts HW, Himel VT. et al. Evaluation of 4 different irrigating systems for apical extrusion of sodium hypochlorite. J Endod. 2015;41(9):1530–1534. doi: 10.1016/j.joen.2015.05.007. [DOI] [PubMed] [Google Scholar]
- 73.Azim AA, Aksel H, Margaret Jefferson M, Huang GT. Comparison of sodium hypochlorite extrusion by five irrigation systems using an artificial root socket model and a quantitative chemical method. Clin Oral Investig. 2018;22(2):1055–1061. doi: 10.1007/s00784-017-2187-y. [DOI] [PubMed] [Google Scholar]
- 74.Arslan D, Kustarci A. Efficacy of photon-initiated photoacoustic streaming on apically extruded debris with different preparation systems in curved canals. Int Endod J. 2018;51(Suppl 1):e65–e72. doi: 10.1111/iej.12816. [DOI] [PubMed] [Google Scholar]
- 75.George R, Walsh LJ. Apical extrusion of root canal irrigants when using Er:YAG and Er,Cr:YSGG lasers with optical fibers: An in vitro dye study. J Endod. 2008;34(6):706–708. doi: 10.1016/j.joen.2008.03.003. [DOI] [PubMed] [Google Scholar]
- 76.Kishen A, Haapasalo M. Biofilm models and methods of biofilm assessment. Endod Topics. 2012;22(1):58–78. doi: 10.1111/j.1601-1546.2012.00285.x. [DOI] [Google Scholar]
- 77.Marion JJC, Manhães FC, Bajo H, Duque TM. Efficiency of different concentrations of sodium hypochlorite during endodontic treatment. Dent Press Endod. 2012;2(4):32–37. [Google Scholar]
- 78.Wang Z, Shen Y, Haapasalo M. Effectiveness of endodontic disinfecting solutions against young and old Enterococcus faecalis biofilms in dentin canals. J Endod. 2012;38(10):1376–1379. doi: 10.1016/j.joen.2012.06.035. [DOI] [PubMed] [Google Scholar]
- 79.Koch JD, Jaramillo DE, DiVito E, Peters OA. Irrigant flow during photon-induced photoacoustic streaming (PIPS) using Particle Image Velocimetry (PIV) Clin Oral Investig. 2016;20(2):381–386. doi: 10.1007/s00784-015-1562-9. [DOI] [PubMed] [Google Scholar]
- 80.De Meyer S, Meire MA, Coenye T, De Moor RJ. Effect of laser-activated irrigation on biofilms in artificial root canals. Int Endod J. 2017;50(5):472–479. doi: 10.1111/iej.12643. [DOI] [PubMed] [Google Scholar]
- 81.Arslan H, Akcay M, Ertas H, Capar ID, Saygili G, Meşe M. Effect of PIPS technique at different power settings on irrigating solution extrusion. Lasers Med Sci. 2015;30(6):1641–1645. doi: 10.1007/s10103-014-1633-1. [DOI] [PubMed] [Google Scholar]
- 82.Huiz Peeters H, Suardita K, Mooduto L, Gutknecht N. Extrusion of irrigant in open apex teeth with periapical lesions following laser-activated irrigation and passive ultrasonic irrigation. Iran Endod J. 2018;13(2):169–175. doi: 10.22037/iej.v13i2.17150. [DOI] [PMC free article] [PubMed] [Google Scholar]