Abstract
Introduction: Sexual dysfunction is a complex problem in postmenopausal women with a prevalence rate of 68%-86%. This study aimed to evaluate the effect of a fractional CO2 laser or vaginal cream on the improvement of sexual function in menopausal women.
Methods: This is a two-group clinical trial study. Postmenopausal women with the inclusion criterion were enrolled and randomly divided into 2 groups of intervention (n=25) and control group (n=25). In the intervention group, CO2 laser therapy was performed every month for three months, and in the control group, Premarin vaginal cream was applied (0.625 mg, 3 nights a week for 3 months. Vaginal health index (VHI) scoring and Female Sexual Function Index (FSFI) questionnaires were completed before and three months after the treatment.
Results: The effects of the laser treatment were greater than the Premarin group with respect to improvement in sexual desire, orgasms, sexual satisfaction, less pain during sexual relations, and overall sexual function (P <0.05).
Conclusion: It seems that the fractional CO2 laser may be more effective than hormonal therapy in improving sexual function in postmenopausal women.
Keywords: CO2 laser, Premarin, Sexual function index, Menopause
Introduction
The most controversial discussions about menopause are related to the menstrual cessation at the end of women’s fertile life. There are short and medium-term effects of menopause, including vasomotor disorders, urinary symptoms, atrophic vaginitis, and sexual disorders, as well as long-term effects such as osteoporosis and cardiac and vascular disorders.1
Menopausal problems and the severity of symptoms which arise during this period can have a significant impact on the sexual function of postmenopausal women.
Sexual dysfunction is defined as a persistent or recurring decline in sexual desire, a persistent or recurrent decrease in sexual stimulation, pain during intercourse, and the presence of a problem or disability to reach orgasm.2,3 According to community-based studies, the prevalence of sexual dysfunction among menopausal women is 68%-86 %.4 Hormonal changes, especially hypoestrogenism, have been reported in more than half of the postmenopausal women characterized by a variety of symptoms in the form of vaginal atrophy which is reported in 45% of postmenopausal women.5-7
Vaginal dryness, pain during sex, bleeding during intercourse or contact, itching, burning, irritability, secretion, and also various urinary problems are the symptoms of this disease.8,9 Therefore, more attention must be paid to relieve these symptoms in order to provide better sexual health for postmenopausal women.
When these treatments are not effective, treatment with topical estrogen is recommended in the absence of contraindications.10 But it should be noted that the long-term information on the safety of the drug is not available (more than one year).11
A randomized comparative study of the oral steroid effects on sexual function in hysterectomized postmenopausal women has shown that topical estrogen alone improves blood flow and some sexual issues, but it is ineffective in providing sexual satisfaction. Systemic estrogen has fewer effects on sexual function.12,13
Furthermore, many women, due to side effects such as the worsening of urinary incontinence, prefer not to use hormonal therapy.14
Several studies have been conducted on the effects of the use of a CO2 laser on the treatment of vulvovaginal atrophy (VVA). It has been shown that the CO2 fractional laser is effective in treating symptoms associated with atrophy and leads to a significant improvement. According to these studies, the CO2 laser has been effective in treating menopausal women and in patients whose breast cancer has improved.15-20
However, there is no study on the effect of the laser on the improvement of sexual function in postmenopausal women in Iran; therefore, the present study compared the effect of the CO2 fractional laser and vaginal cream on the improvement of sexual performance and sexual satisfaction.
Materials and Methods
Study Design and Population
The present study is a clinical trial comparing 2 groups, which was performed at the pelvic disorders clinic of Imam Khomeini Hospital affiliated to Tehran University of Medical Sciences. The population under study are postmenopausal women who were referred to the clinic.
Study Participants
Presented to the clinic, study participants included menopausal women whose ages ranged from 45 to 65 years. They were sexually active,single-sex and monogamous, and had symptoms of VVA (vaginal dryness, irritation, soreness, or dyspareunia) between November 2017 and January 2018.
We excluded the following patients from the study: smokers; those who had used any type of topical or systemic hormone replacement therapy and vaginal-lubrication within 6 months and during 30 days before participating in the study respectively; those who had any acute or chronic urinary tract infections, active genital infections, prolapse stage II or more based on examination based on the Pelvic Organ Prolapse Quantification (POP-Q) system, psychiatric disorders, and undiagnosed vaginal bleeding; and those suffering from hormonal imbalance or any serious disease or chronic condition that could interfere with study compliance.
Sampling was done randomly in the 2 groups. The samples were randomly divided into 2 groups of intervention (n = 25) and control (n = 25). The sample size was calculated based on the Sokol and Karram study in 2017.6 They had found a significant improvement in sexual function in menopausal women. FSFI after 12 weeks using the CO2 laser fraction was 20.1 ± 11.0 vs 11.5 7.8 in the control group. So to follow up the estimation with a 95% significance level, 80% power, and 15% loss, we had to study 23 cases in each group.
Based on randomized blocks with size 4 (AABB, ABBA, ABAB, BBAA, BABA, BAAB, etc), the first sample was assigned to group A, the second sample was included in group A, the third and the fourth samples were placed in group B, and a similar random division continued in the following order until all 50 samples were divided. Healthcare therapists and staff were not aware of the groups they were assigned to and they were only given specific codes that were entirely blind.
In the intervention group, the CO2 laser therapy was performed every month for 3 months, and in the control group, Premarin vaginal cream (0.625 mg) was used with a third of the applicator being used 3 nights a week for 3 months.
The control group received a series of 3 treatments using the fractional CO2 laser system (SmartXide2, Monalisa Touch, DEKA, Florence, Italy) in an outpatient setting without analgesia or anesthesia. In this treatment, the device settings are as follows: Dot power r 40 W, dwell time 1000 µs, Dot spacing 1000 µm, Smart stack settings of 1 for the first treatment, and 3 for the third treatments.
The speculum cage was introduced into the introitus, and the handpiece was inserted into the interior edge of the treatment site (up to 11 cm in the vaginal canal). Several drops of baby oil were used for more comfortable insertion into the introits. The handpiece was positioned in contact with the vaginal wall and was rotated to apply up to 16 pulses at each 1 cm marking up to a 4 to 5 cm depth. The vaginal canal was treated with 2 to 3 passes.
The procedure was performed in the outpatient clinic and did not require analgesia/anesthesia. The patients were recommended to avoid coital sexual activity and tampon use for at least 7 days after the treatment.
Data Collection
The primary outcome was the assessment of changes in the FSFI at 12 weeks after the treatment in the 2 groups. The secondary outcome was the VHI assessment.
The data gathering tools in this study were the demographic information questionnaire (including age, body mass index [BMI], smoking, education level, number of deliveries, delivery type, history of previous genital surgery, hysterectomy and problems with the husband) and other questionnaires that were used. This questionnaire contains 8 items for vaginal examination. These 8 items include elasticity, type and concentration of discharge, PH, epithelial mucus and humidity in which each one receives a score of 1 to 3. In total, the minimum score is 3 and a maximum one is 24 and the higher score of the vaginal examination is better. The following evaluation method for VIH was used.21 By examining the vagina, the researchers evaluated and numbered the clinical signs of atrophy by completing a descriptive assessment table of vaginal mucus.
PH was noted by a litmus paper kept in the vagina for 1 minute and the color was compared to standardized colors.
The moisture/consistency of fluid was evaluated by putting the vaginal fluid on a clean slide for grading.
Rugosity and elasticity were assessed by the inspection and palpation of vaginal mucosa by the index finger.
The length of the vagina was measured by the index finger and Ayres Spatula from the highest point in the vagina to the vulvar outlet. The mean of the 2 measurements was taken as an average length.
Epithelial integrity was assessed by the presence of petechia on the vaginal wall by the pressure of the index finger.
Vascularity was assessed by the inspection of the color of the vagina.
Vaginal wall thickness was assessed by the technic of 2 balloons using the logic 500 MDGE Ultrasound Machine. It was measured by inserting 2 sterile No.18 Foley catheters, one in the vagina and the other in the anal canal.
Sexual dysfunction was assessed using the Persian version of the Female Sexual Function Index (FSFI) scale, previously translated and validated.21 FSFI and VIH questionnaires were filled in at the beginning of the study and at the end of week 12.
FSFI is a 19-item questionnaire, developed as a multidimensional self-report instrument for the assessment of the key dimensions of sexual functioning in women in the last month. The items of the scale are divided into 6 domains which include desire (2 questions), subjective arousal (4 questions), lubrication (4 questions), orgasm (3 questions), satisfaction (3 questions), and pain (3 questions). Libido (sexual desire) or interest is a feeling that includes wanting to have a sexual experience, feeling receptive to a partner’s sexual initiation, and thinking or fantasizing about having sex, arousal (desire for sexual activity with sexual stimulations), orgasm (to reach orgasm after adequate sexual arousal and stimulation), and dyspareunia (pain in the pelvis or vagina during any normal sexual stage).
In the FSFI questionnaire, since the questions are not equal to each other, the scores of questions in each area are added together and then multiplied by the number of factors. The sexual desire domain scores were considered (1-5), orgasm, lubrication, pain (0-5) and sexual satisfaction (5 or 0, 1). A score of zero indicates that during the past 4 weeks the participant has not had sexual activity.
Based on the weight of the domains, the maximum score for each area is 2, and 36 will be for the total scale. The cut-off scores are in the field of sexual desire (3.3), sexual orgasm (3.4), lubrication (3.7), pain, and satisfaction (3.8), and for the total scale, the minimum score is equal to 28.
The total FSFI score, which was 36, is the sum of all scores obtained in each of the 6 domains. The higher the score, the better the sexuality function is. A score lower than 27 was considered as the cut-off value for the diagnosis of female sexual dysfunction.21
The patients before the intervention and after 12 weeks were evaluated using the VHI and FSFI questionnaires in terms of their responses to the laser or vaginal cream. All patients underwent VHIS and FSFI evaluations, performed by the same gynecologist unaware of the type of treatment in order to avoid inter-observer variability.
Statistical Analyses
Statistical analyses were performed using SPSS software (SPSS, version 16, SPSS, Inc., IL, USA). Data are expressed as arithmetic and geometric mean ± standard deviation (SD) and number (percentile). According to the Kolmogorov-Smirnov test, the distribution of all data was normal. In order to obtain the primary outcomes andthecomparison between the 2 groups, the chi-square test and the independent-samples t test were used. The paired-samples t test was used in each group to compare the mean changes of the VHI after the intervention (P value < 0.05 considered significant).
Results
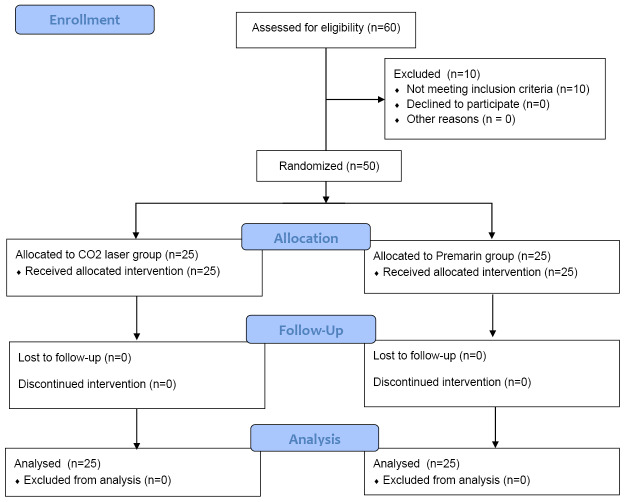
The present randomized clinical trial study was conducted at Vali-Asr Clinic in Imam Khomeini Hospital, Tehran between November 2017 and January 2018. A total of 60 female candidates participated in the study and were divided into intervention and control groups. Of these, 10 subjects were excluded due to not meeting the inclusion criteria. A total of 50 patients suffering from menopausal symptoms were studied in 2 groups of intervention with the fractional CO2 laser (n = 25) and control or Premarin (n = 25) (see Figure 1).
Figure 1.
The Consort Flowchart.
The patients were assessed before the treatment and at the 12-week follow-up after the final treatment. All 50 participants completed the study and their collected information was included in the analysis (see Figure 1).
The participants in both groups were comparable with respect to age, BMI, and other baseline parameters (see Table 1). The mean age in both groups of laser and Premarin was 57 and 54.6 years and furthermore, the BMI was 28.32 (± 4.6) and 28.06 (± 3.45) kg/m2 respectively.
Table 1. Modified Vaginal Health Index .
| Parameter | 1 | 2 | 3 |
| pH | > 6.5 | 5-6.5 | <5 |
| Moisture | No moisture | Minimal moisture/superficial layer of scanty thin white mucus | |
| Rugosity | None | Minimal | Good |
| Elasticity | Poor | Fair | Elasticity |
| Length of vagina | <4 cm | 4-6 cm | > 6 cm |
| Thickness | Papery thin | Thin | Normal |
| Epithelial integrity | Petechiae | Petechiae after scraping | Normal friable |
| Vascularity | Minimal | Fair | Good |
According to an independent-samples t test and a chi-square test, there were no significant differences in demographic characteristics between the 2 groups (see Table 2).
Table 2. Baseline Characteristics of 2 Groups .
| Variable |
Control Group
(Premarin), n=25 |
Intervention Group (CO 2 Laser), n=25 | P Value a |
| Age (y) | 57±6.42 | 54.6±8.23 | 0.25 |
| BMI | 28.32±4.6 | 28.06±3.45 | 0.82 |
| Duration of marriage (y) | 37.28±9.82 | 34.4±10.8 | 0.33 |
| Para (n) | 4.92±2.72 | 3.4±3.22 | 0.07 |
| Gravid (n) | 5.44±2.58 | 4.16±3.37 | 0.14 |
| Child (n) | 4.76±2.66 | 3.4±3.22 | 0.11 |
| Delivery type, No. (%) | 0.18 | ||
| Normal vaginal delivery | 20 (80) | 20 (80) | |
| Cesarean section | 1 (4) | 1 (4) | |
| Both | 4 (16) | 1 (4) | |
| No | 0 (0) | 3 (12) | |
| Education, No. (%) | 0.66 | ||
| Illiterate | 7 (28) | 4 (16) | |
| Elementary | 9 (36) | 8 (32) | |
| Diploma | 6 (24) | 8 (32) | |
| >Diploma | 3 (12) | 5 (11) | |
| History of previous genital surgery, No. (%) | 10(40) | 6(24) | 0.22 |
| Hysterectomy, No. (%) | 0.55 | ||
| Yes | 8(32) | 10(40) | |
| Problem with husband, No. (%) | 0.12 | ||
| Yes | 15 (60) | 20 (80) | |
| No | 10 (40) | 5 (20) | |
| VHI (Mean ± SD) | 14.96±3.72 | 14.16±2.35 | 0.37 |
| FSFI (Mean ± SD) | 14.76±6.06 | 17.17±6.44 | 0.18 |
a t test.
After the treatment, 4 FSFI domains, including those of desire (P < 0.001), arousal (P = 0.016), sexual satisfaction (P = 0.008) and dyspareunia (P = 0.007), showed significant differences between the 2 groups, but there were no significant differences observed in terms of lubrication (P = 0.73) and orgasm (P = 0.99) in sexual relationships between the 2 groups. In other words, the effect of the laser on desire, orgasms, sexual satisfaction, pain sensation in sexual relations, and overall sexual function was greater than the Premarin intervention group ( P < 0.05) (see Table 3).
Table 3. Comparison of the sexual function domains and vaginal health index (VHI) in two groups of laser treatment and Premarin pre- and post-treatments .
| Variable |
Control Group (Premarin),
n=25 |
Intervention Group (CO2 Laser),
n=25 |
P Value a |
| Sexual function in 2 groups of laser and Premarin Pre-treatment | |||
| Desire | 2.01±0.81 | 2.4±1.05 | 0.15 |
| Arousal | 2.17±1.39 | 2.35±1.14 | 0.62 |
| Lubrication | 2.29±1.27 | 3.1±1.43 | 0.03 |
| Orgasm | 2.57±1.44 | 3.28±1.5 | 0.3 |
| Satisfaction | 3.13±1.1 | 3.48±1.28 | 0.3 |
| Dyspareunia | 2.57±1.81 | 2.54±1. 63 | 0.94 |
| FSFI | 14.76±6.06 | 17.17±6.44 | 0.18 |
| VHI | 14.96±3.72 | 14.16±2. 35 | 0.37 |
| Sexual function in 2 groups of laser and Premarin post-treatment | |||
| Desire | 2.59±0.7 | 3.48±0.94 | <0.001 |
| Arousal | 2.86±1.12 | 3.62±1.02 | 0.016 |
| Lubrication | 3±0.83 | 3.09±0.61 | 0.73 |
| Orgasm | 4.68±0.86 | 4.67±0.82 | 0.99 |
| Satisfaction | 3.36±0.98 | 4.2±1.15 | 0.008 |
| Dyspareunia | 3.69±0. 86 | 4.4±0.88 | 0.007 |
| FSFI | 18.97±4. 54 | 23.16±4.87 | 0.003 |
| VHI | 17.96±4.05 | 17.36±2.61 | 0.53 |
aIndependent-samples t test.
In the 2 groups of laser and Premarin, the score of VHI did not indicate differences before and at the end of the treatment (P = 0.53). But in each group, VHI improved after the treatment. In other words, VHI in the laser and Premarin groups improved after the treatment (see Tables 3 and 4). No serious adverse effects were observed in participants. No abnormal vaginal bleeding or vaginal discharge was observed in either group.
Table 4. Comparison of Vaginal Health Index (VHI) Pre- and Post-treatment Between the 2 Groups of Laser and Premarin .
| Group | Before Treatment | After Treatment | P Value a |
| Intervention group (CO2 laser) |
14.16±2. 35 | 17.36±2. 61 | <0.001 |
| Control group (Premarin) |
14.96±3.72 | 17.96±4/05 | <0.001 |
aPaired samples t test.
Discussion
The results of the present study showed that there was a significant difference between sexual function in the 2 groups of laser or Premarin after the treatment in the field of desire, arousal, satisfaction, dyspareunia, and overall sexual function. It seems that the laser had a greater effect than the Premarin, but there was no significant difference in the degree of lubrication and orgasm in a sexual relationship.
In general, both treatments of laser CO2 and Premarin improved sexual function. However, the overall effect of laser therapy was better than Premarin. In each of the groups, the VHI improved after the treatment. In other words, VHI in both the laser-treated group and the Premarin group was better after the treatment. In this study, fractional CO2 laser treatment and Premarin were associated with the improvement of vaginal health and the amelioration of symptoms of VVA, but in the laser group, the treatment resulted in improved sexual function in menopausal women.
A study by Salvatore et al showed that Fractional microablative CO2 laser treatment improved sexual function and satisfaction in postmenopausal women with Volvo vaginal atrophy symptoms.22 Also, Pieralli et al and Pearson et al suggested that the fractional CO2 laser is an effective treatment for dyspareunia in breast cancer survivors with contraindications to hormonal treatments.19,20 Also, the results from a study conducted by Eder showed that CO2 laser therapy for post-menopausal women can be considered an effective therapeutic choice providing the relief of symptoms already noted after one laser treatment.23
The present study is consistent with the results of these studies.19,20,22,23,25 Also, similar to other studies in postmenopausal women,22,23,24,25 the clinical data support the use of pulsed CO2 lasers in the treatment of sexual dysfunction.25
Siliquini et al suggest that CO2 laser treatment induces a significant and long-term improvement of VHI symptoms.26 The effect of laser waves on the vaginal tissue leads to the rejuvenation of the vaginal cells and their stimulation to produce collagen, a substance essential for the health of vaginal cells.27 It is also used to improve the skin condition of the reproductive system and mucosal tissue in women with lichen sclerosis.28,29
In the present study, improvement in VHI scores was reported in the 2 treatment groups in menopausal women who underwent 3 sessions of fractional CO2 laser vaginal treatment. Heat-induced thermal regeneration with new collagen deposition improves the tissue quality of the vaginal canal, while ablation to the outer external labia leads to tissue regeneration.30 “The available clinical studies do not present convincing data regarding the efficacy of LASER for the treatment of vaginal atrophy or urinary incontinence”.31
But the clinical trial data of laser therapy for VVA suggest that it is safe, with no significant side effects. Thus, they suggested that it is a practicable treatment choice for women who cannot or do not want to be treated with hormone-based therapies.32
According to the results of this study, the laser can be used to improve the sexual function of menopausal women. However, with regard to the higher expenses of the laser compared to Premarin, it is recommended that laser therapy be used as a therapeutic method in the contraindications of estrogen use.
The main limitation of the present study was the small and limited number of participants in each group. Furthermore, as the study was conducted in Asian women with sexual dysfunction, it may not be applicable in women with other ethnicities or less troublesome symptoms. Consequently, further studies are warranted with a larger sample of women, other ethnicities, and other troublesome symptoms. The strength of the current study is its prospective design and how the effects of the treatment after the initial treatment were investigated and continued for 3 months.
Overall, the present study suggests a potentially significant application for the administration of CO2 laser treatment for improving sexual function.
Ethical Considerations
The ethics board of Tehran University of Medical Sciences with the code number (IR.TUMS.IKHC.REC.1396.2552) approved this clinical trial study (Identifier: IRCT20160916029835N3; https://www.irct.ir/trial/23883). Informed consent was obtained from all participants. They were informed that participation included an intervention, pelvic and clinical examination, and transvaginal ultrasound evaluation. The research purpose was described and the willingness to participate was evaluated.
Conflict of Interests
The authors declare no conflict of interest.
Acknowledgement
This article was an extracted residential thesis conducted in Tehran University of Medical Sciences and the authors express their gratitude and appreciation to the Urogynecology Clinic for their kind cooperation in the project.
Please cite this article as follows: Eftekhar T, Forooghifar T, Khalili T, Shariat M, Haghollahi F. The effect of the CO2 fractional laser or Premarin vaginal cream on improving sexual function in menopausal women: a randomized controlled trial. J Lasers Med Sci. 2020;11(3):292-298. doi:10.34172/jlms.2020.49.
References
- 1. Lobo RA, Kelsey J, Marcus R, editors. Menopause: Biology and Pathobiology. San Francisco: Academic Press; 2000.
- 2.Nappi RE, Lachowsky M. Menopause and sexuality: prevalence of symptoms and impact on quality of life. Maturitas. 2009;63(2):138–41. doi: 10.1016/j.maturitas.2009.03.021. [DOI] [PubMed] [Google Scholar]
- 3.Basson R, Berman J, Burnett A, Derogatis L, Ferguson D, Fourcroy J. et al. Report of the international consensus development conference on female sexual dysfunction: definitions and classifications. J Urol. 2000;163(3):888–93. doi: 10.1016/s0022-5347(05)67828-7. [DOI] [PubMed] [Google Scholar]
- 4.Addis IB, Van Den Eeden SK, Wassel-Fyr CL, Vittinghoff E, Brown JS, Thom DH. Sexual activity and function in middle-aged and older women. Obstet Gynecol. 2006;107(4):755–64. doi: 10.1097/01.AOG.0000202398.27428.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Naumova I, Castelo-Branco C. Current treatment options for postmenopausal vaginal atrophy. Int J Womens Health. 2018;10:387–395. doi: 10.2147/IJWH.S158913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sokol ER, Karram MM. Use of a novel fractional CO2 laser for the treatment of genitourinary syndrome of menopause: 1-year outcomes. Menopause. 2017;24(7):810–814. doi: 10.1097/GME.0000000000000839. [DOI] [PubMed] [Google Scholar]
- 7.Nappi RE, Kokot-Kierepa M. Women’s voices in the menopause: results from an international survey on vaginal atrophy. Maturitas. 2010;67(3):233–8. doi: 10.1016/j.maturitas.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 8.Stika CS. Atrophic vaginitis. Dermatol Ther. 2010;23(5):514–22. doi: 10.1111/j.1529-8019.2010.01354.x. [DOI] [PubMed] [Google Scholar]
- 9.American Menopause Society. Management of symptomatic vulvovaginal atrophy: 2013 position statement of The North American Menopause Society. Menopause. 2013;20(9):888–902. doi: 10.1097/GME.0b013e3182a122c2. [DOI] [PubMed] [Google Scholar]
- 10.Basson R, Leiblum S, Brotto L, Derogatis L, Fourcroy J, Fugl-Meyer K. et al. Definitions of women’s sexual dysfunction reconsidered: advocating expansion and revision. J Psychosom Obstet Gynaecol. 2003;24(4):221–9. doi: 10.3109/01674820309074686. [DOI] [PubMed] [Google Scholar]
- 11.Calleja-Agius J, Brincat MP. Urogenital atrophy. Climacteric. 2009;12(4):279–85. doi: 10.1080/13697130902814751. [DOI] [PubMed] [Google Scholar]
- 12.Long CY. A randomized comparative study of the effects of oral and topical estrogen therapy on the vaginal vascularization and sexual function in hysterectomized postmenopausal women. Menopause. 2006;13(5):737–43. doi: 10.1097/01.gme.0000227401.98933.0b. [DOI] [PubMed] [Google Scholar]
- 13.Goldstein I. Practical aspects in the management of vaginal atrophy and sexual dysfunction in perimenopausal and postmenopausal women. J Sex Med. 2005;2(Suppl 3):154–65. doi: 10.1111/j.1743-6109.2005.00131.x. [DOI] [PubMed] [Google Scholar]
- 14.Steinauer JE, Waetjen LE, Vittinghoff E, Subak LL, Hulley SB, Grady D. et al. Postmenopausal hormone therapy: does it cause incontinence? Obstet Gynecol. 2005;106(5 Pt 1):940–945. doi: 10.1097/01.AOG.0000180394.08406.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Salvatore S, Nappi RE, Parma M, Chionna R, Lagona F, Zerbinati N. et al. Sexual function after fractional microablative CO2 laser in women with vulvovaginal atrophy. Climacteric. 2015;18(2):219–25. doi: 10.3109/13697137.2014.975197. [DOI] [PubMed] [Google Scholar]
- 16.Salvatore S, Nappi RE, Zerbinati N, Calligaro A, Ferrero S, Origoni M. et al. A 12-week treatment with fractional CO2 laser for vulvovaginal atrophy: a pilot study. Climacteric. 2014;17(4):363–369. doi: 10.3109/13697137.2014.899347. [DOI] [PubMed] [Google Scholar]
- 17.Salvatore S, Maggiore ULR, Origoni M, Parma M, Quaranta L, Sileo F. et al. Microablative fractional CO2 laser improves dyspareunia related to vulvovaginal atrophy: a pilot study. J Endometr Pelvic Pain Disord. 2014;6(3):150–6. [Google Scholar]
- 18.Perino A, Calligaro A, Forlani F, Tiberio C, Cucinella G, Svelato A. et al. Vulvo-vaginal atrophy: A new treatment modality using thermo-ablative fractional CO2 laser. Maturitas. 2015;80(3):296–301. doi: 10.1016/j.maturitas.2014.12.006. [DOI] [PubMed] [Google Scholar]
- 19.Pieralli A, Fallani MG, Becorpi A, Bianchi C, Corioni S, Longinotti M. et al. Fractional CO2 laser for vulvovaginal atrophy (VVA) dyspareunia relief in breast cancer survivors. Arch Gynecol Obstet. 2016;294(4):841–6. doi: 10.1007/s00404-016-4118-6. [DOI] [PubMed] [Google Scholar]
- 20.Pearson A, Booker A, Tio M, Marx G. Vaginal CO2 laser for the treatment of vulvovaginal atrophy in women with breast cancer: LAAVA pilot study. Breast Cancer Res Treat. 2019;178(1):135–140. doi: 10.1007/s10549-019-05384-9. [DOI] [PubMed] [Google Scholar]
- 21.Fakhri A, Pakpour AH, Burri A, Morshedi H, Zeidi IM. The Female Sexual Function Index: translation and validation of an Iranian version. J Sex Med. 2012;9(2):514–23. doi: 10.1111/j.1743-6109.2011.02553.x. [DOI] [PubMed] [Google Scholar]
- 22.Salvatore S, Nappi RE, Parma M, Chionna R, Lagona F, Zerbinati N. et al. Sexual function after fractional microablative CO 2 laser in women with vulvovaginal atrophy. Climacteric. 2015;18:219–225. doi: 10.3109/13697137.2014.975197. [DOI] [PubMed] [Google Scholar]
- 23.Eder SE. Early effect of fractional CO2 laser treatment in Post-menopausal women with vaginal atrophy. Laser Ther. 2018;27(1):41–47. doi: 10.5978/islsm.18-OR-04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Salvatore S, Athanasiou S, Candiani M. The use of pulsed CO2 lasers for the treatment of vulvovaginal atrophy. Curr Opin Obstet Gynecol. 2015;27(6):504–8. doi: 10.1097/GCO.0000000000000230. [DOI] [PubMed] [Google Scholar]
- 25.Siliquini GP, Tuninetti V, Bounous VE, Bert F, Biglia N. Fractional CO2 laser therapy: a new challenge for vulvovaginal atrophy in postmenopausal women. Climacteric. 2017;20(4):379–384. doi: 10.1080/13697137.2017.1319815. [DOI] [PubMed] [Google Scholar]
- 26.Manstein D, Herron GS, Sink RK, Tanner H, Anderson RR. Fractional photothermolysis: a new concept for cutaneous remodeling using microscopic patterns of thermal injury. Lasers Surg Med. 2004;34(5):426–438. doi: 10.1002/lsm.20048. [DOI] [PubMed] [Google Scholar]
- 27.Peterson CM, Lane JE, Ratz JL. Successful carbon dioxide laser therapy for refractory anogenital lichen sclerosus. Dermatol Surg. 2004;30(8):1148–51. doi: 10.1111/j.1524-4725.2004.30343.x. [DOI] [PubMed] [Google Scholar]
- 28.Lee A, Lim A, Fischer G. Fractional carbon dioxide laser in recalcitrant vulval lichen sclerosus. Australas J Dermatol. 2016;57(1):39–43. doi: 10.1111/ajd.12305. [DOI] [PubMed] [Google Scholar]
- 29.Arroyo C. Fractional CO2 laser treatment for vulvovaginal atrophy symptoms and vaginal rejuvenation in perimenopausal women. Int J Womens Health. 2017;9:591–595. doi: 10.2147/IJWH.S136857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Preti M, Vieira-Baptista P, Digesu GA, Bretschneider CE, Damaser M, Demirkesen.
- 31.O O. et al. The clinical role of LASER for vulvar and vaginal treatments in gynecology and female urology: An ICS/ISSVD best practice consensus document. J Low Genit Tract Dis. 2019;23(2):151–160. doi: 10.1097/LGT.0000000000000462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gambacciani M, Palacios S. Laser therapy for the restoration of vaginal function. Maturitas. 2017;99:10–5. doi: 10.1016/j.maturitas.2017.01.012. [DOI] [PubMed] [Google Scholar]