Dear Editor,
In China, the epidemic of COVID-19 has been temporarily brought under control due to strong measures, while there are few new cases except some imported ones (https://static.wecity.qq.com/wuhan-haiwai-pre/dist/index.html#/). The PCR-based test result combined with clinical symptoms has widely been used for the detection and confirmation of COVID-19.1 However, the prevalence of asymptomatic or subclinical SARS-CoV-2 infection in China remained unknown.
Serological investigation can comprehensively identify the infected people in community, especially those asymptomatic. Presence of positive IgM antibody in serum indicates an early infection, while positivity in IgG antibody, which persists for a long time after disease, indicates a prior infection. A recent study demonstrated that 100% of COVID-19 patients were tested positive for antiviral immunoglobulin.2 Although the antibody test has a false rate of 10%–15% (false negative and false positive), it can detect the former asymptomatic infections and be used to estimate the true infection rate of the population. A serosurvey in Santa Clara county at California indicated that the infection rate of SARS-CoV-2 may be 30–50 times of that in official reports based on nucleic-acid diagnoses.3
Here, we studied the seroprevalence of IgM/IgG antibodies to SARS-CoV-2 of hospital visitors from the First Affiliated Hospital of Guangzhou Medical University in Guangzhou, the largest city in Southern China, and the Hubei Cancer Hospital in Wuhan, the epicenter of the outbreak, respectively. These visitors, including inpatients and their healthy companions, represented a population with a common social exposure and without COVID-19-related symptoms.
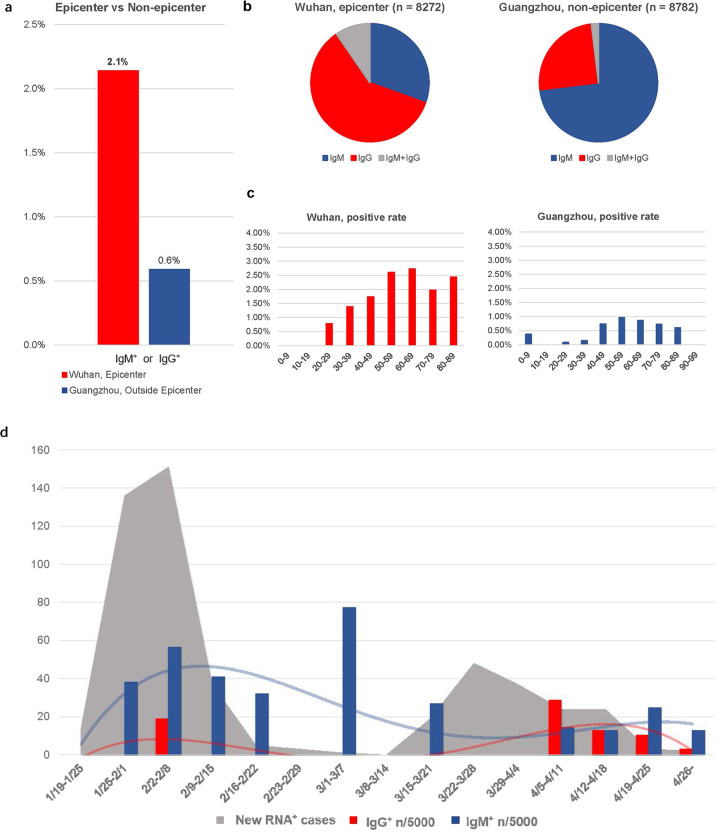
Up to April 30th, a total of 8272 individuals in the Wuhan cohort (epicenter) and 8782 individuals in the Guangzhou cohort (non-epicenter) were included (Supplementary information, Table S1); the median age was 54 (IQR (interquartile range), 44–62) and 55 (IQR, 38–67), respectively. All these individuals were tested negative for SARS-CoV-2 RNA, and most of them had no COVID-19-related symptoms within the past three months. The seroprevalence of IgM/IgG was 2.1% in Wuhan and 0.6% in Guangzhou, respectively (Fig. 1a). In Wuhan, the seroprevalence against SARS-CoV-2 of IgG is higher than that of IgM (Fig. 1b). There was no significant difference of seroprevalence in sex and age subgroups (Fig. 1c; Supplementary information, Table S2). The time trend of IgM and IgG prevalence among hospital visitors in Guangzhou cohort was illustrated in Fig. 1d, which matched with ‘two peaks’ of the total RNA-positive (RNA+) case number in Guangzhou with a slight delay in time.
Fig. 1. Summary of SARS-CoV-2 seroprevalance among hospital visitors.
a Positive rate of SARS-CoV-2 IgM/IgG in Wuhan and Guangzhou. b Proportion of IgM positive, IgG positive and IgM+IgG double positive in Wuhan and Guangzhou. c Positive rate of IgM/IgG in different age groups. x-axis, age ranges; y-axis, positive rate. d IgM (blue bars and fitted line) and IgG (red bars and fitted line) prevalence in cases tested in Guangzhou hospital cohort, and total RNA-confirmed cases (gray areas) in Guangzhou city, in each week since outbreak. x-axis, date ranges; y-axis, positivity burden. n, number of positivity (b, d).
This serosurvey of hospital visitors detected individuals positive for antibodies against SARS-CoV-2. These individuals had no history of COVID-19 symptoms, and therefore regarded as asymptomatic or mild. There was no consensus on whether individuals with asymptomatic patients are infectious or not. On this basis, public health interventions are still required to avoid the second wave of outbreak. In addition, serosurveys might partially reflect the disease prevalence.3 In this survey, the seroprevalence of epicenter Wuhan was higher than that in Guangzhou, which is outside the epicenter, and the trends of RNA+ cases in Guangzhou and antibody positive rates of hospital visitors in Guangzhou were well matched with each other. Admittedly, the current seroprevalence might be underestimated due to the sensitivity of assays and biased by the comorbidity burden among patients requiring hospitalization. There might be also a bias for the investigated population (patients with other disease and without significant COVID-19 symptoms), as most RNA+ cases has been detected and isolated due to the comprehensive screening strategy in China. On this basis, this study did not provide an exact number of infection prevalence and of the comparison between the two cities. Still, the relatively low seropositivity suggests that prevention and control measures in China are effective.4 On the other hand, this study showed that in Wuhan and Guangzhou, whether inside or outside the epicenter of outbreak, the population immunity is still at a low level. Therefore, there is an urgent need for an effective vaccine against SARS-CoV-2, and strict isolation and community measures should be continued until such a vaccine is available.
Supplementary information
Acknowledgements
This study is supported by the National Natural Science Foundation of China National (No. 81871893), Key Project of Guangzhou Scientific Research Project (No. 201804020030), High-level university construction project of Guangzhou Medical University (No. 20182737, 201721007, 201715907, 2017160107); National key Research and Development Program (No. 2017YFC0907903, 2017YFC0112704) and the Guangdong high level hospital construction “reaching peak” plan.
Author contributions
N.S.Z., J.X.H., G.H. and D.S.H conceived the study and supervised the project. W.H.L., Y.P.L., J.P.B. and J.F.L. cleaned and analyzed data. Y.L., G.W.J. and Z.F.Y. collected the data. All authors contributed to writing and editing the manuscript.
Competing interests
The authors declare no competing interests.
Footnotes
These authors contributed equally: Wenhua Liang, Yongping Lin, Jianping Bi, Jianfu Li
Contributor Information
Guang Han, Email: hg7913@hotmail.com.
Desheng Hu, Email: hds_005@163.com.
Jianxing He, Email: drjianxing.he@gmail.com.
Supplementary information
Supplementary information accompanies this paper at 10.1038/s41422-020-0371-0.
References
- 1.Guan, W. J. et al. N. Engl. J. Med.382, 1708–1720 (2020). [DOI] [PMC free article] [PubMed]
- 2.Long, Q. X., et al. Nat. Med. 26, 845–848 (2020). [DOI] [PubMed]
- 3.Bendavid E., et al. medrxiv.org. 10.1101/2020.04.14.20062463.
- 4.Yang, Z. et al. J. Thorac. Dis.12, 165–174 (2020). [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.