Abstract
Background
Many U.S. health systems are grappling with how to safely resume elective surgery amid the COVID-19 pandemic. We used online crowdsourcing to explore public perceptions and concerns toward resuming elective surgery during the pandemic, and to determine factors associated with the preferred timing of surgery after health systems reopen.
Methods
A 21-question survey was completed by 722 members of the public using Amazon Mechanical Turk. Multivariable logistic regression analysis was performed to determine factors associated with the timing of preferred surgery after health systems reopen.
Results
Most (61%) participants were concerned with contracting COVID-19 during the surgical process, primarily during check-in and in waiting room areas, as well as through excessive interactions with staff. Overall, 57% would choose to have their surgery at a hospital over an outpatient surgery center. About 1 in 4 (27%) would feel comfortable undergoing elective surgery in the first month of health systems reopening. After multivariable adjustment, native English speaking (OR, 2.6; 95% CI, 1.04-6.4; P = .042), male sex (OR, 1.9; 95% CI, 1.3-2.7; P < .001), and Veterans Affairs insurance (OR, 4.5; 95% CI, 1.1-18.7; P = .036) were independent predictors of preferring earlier surgery.
Conclusion
Women and non-native English speakers may be more hesitant to undergo elective surgery amid the COVID-19 pandemic. Despite concerns of contagion, more than half of the public favors a hospital setting over an outpatient surgery center for their elective surgery. Concerted efforts to minimize patient congestion and unnecessary face-to-face interactions may prove most effective in reducing public anxiety and concerns over the safety of resuming elective care.
Keywords: COVID-19, elective surgery, public perceptions, elective care, patient concerns
Although the U.S. health care system has united to meet the challenges of the coronavirus disease 2019 (COVID-19) pandemic, this effort has placed many hospitals and health systems under significant financial pressure [[1], [2], [3], [4], [5]]. A recent report estimated that this pandemic has resulted in over $202 billion in losses to U.S. health systems and hospitals [1], much of which is due to the cessation of elective surgery [1,3]. As the COVID-19 burden decreases, many health systems are increasingly eager to resume margin producing elective surgery in a safe and controlled manner [[6], [7], [8]]. A new set of challenges, however, present themselves with the resumption of elective care [5,9]. Health systems may be at a crossroads between the public health obligation to keep the population healthy and safe, and the financial solvency concerns about withstanding this pandemic [1,6,10].
It is unclear how patients will react to the resumption of elective surgery. Although early reports have demonstrated that most patients seem eager to have their procedures carried out, others are hesitant [11]. Resuming elective surgery safely and at a responsible time may still result in financial losses and suboptimal patient outcomes if the public’s perceptions and subsequent treatment choices are not considered. Patients preferring to undergo surgery soon after health systems reopen may be at a higher risk of postoperative morbidity and mortality. Alternatively, unaddressed concerns leading to delayed presentations may further accentuate health care disparities in disadvantaged and vulnerable populations [[12], [13], [14], [15]].
Currently, there are limited data to guide health systems in the resumption of elective surgeries [7]. Without a true understanding of the public’s beliefs and concerns over the safety of resuming elective care, health care organizations may be flying blind in deciding how to optimize processes to reduce the fear of infection. In this context, we used an online crowdsourcing platform to explore public perceptions and concerns toward resuming elective surgery during the COVID-19 pandemic, and to determine factors associated with the timing of preferred surgery after health systems reopen.
Methods
This study was reviewed by our institutional review board and was granted an exempt research status.
Study Design
Our research team developed an electronic survey addressing public perceptions and concerns regarding resuming elective surgery during the COVID-19 pandemic. The survey was created using Qualtrics XM (Qualtrics, Provo, UT) and consisted of 21 multiple-choice questions. Before beginning the survey, responders read a brief description of our study aim as well as a definition of elective surgery. We defined elective surgery as a “nonurgent, quality of life–related surgery.” Demographic information included age, sex, race, native language, marital status, annual income, location (U.S. region), primary health insurance, and perceived overall health status.
We determined the rate of major depressive disorder with the Patient Health Questionnaire (PHQ-2) [16], and assessed health literacy using the single health literacy screening question [17]. Furthermore, patient engagement was gauged using the single health confidence question [18].
Specific questions used to assess public perceptions of resuming elective surgery were created. These questions were either binary or included four multiple-choice responses. Questions utilizing a Likert scale [19] were constructed to optimize symmetry and balance. The final survey was created by the full study team and utilized an iterative consensus process. The full survey can be found in Appendix A.
Data Source
The study population for our study was composed of participants on Amazon Mechanical Turk (MTurk; Amazon.com, Inc). Amazon Mechanical Turk (MTurk) is an international online crowdsourcing marketplace where workers are compensated for completing virtual tasks [20]. The MTurk workforce includes over 500,000 unique users worldwide, many of which are from the United States [21]. MTurk has emerged as a respected platform to perform medical research due to its generalizability to the overall U.S. population, high-scale reliability, concurrent and convergent validity, and internal consistency [22]. Furthermore, MTurk has been shown to be an efficient, reliable, and cost-effective tool for generating survey responses for medical research that are largely comparable with those collected through conventional means [20,[23], [24], [25]].
Study participants were limited to adults (≥18 years) with valid social security numbers currently residing in the United States. Each participant was awarded $0.12 for completing the survey. Personal funds were used to award participants. Incomplete surveys were excluded from the analysis. The survey was administered over a two-day period during May 2020. A sensitivity analysis was performed for participants over the age of 60 years, as they represent a considerable portion of the population undergoing elective orthopedic surgery.
Statistical Analysis
We performed a bivariate analysis to identify population characteristics associated with preferring early elective surgery (within one month of health systems resuming elective surgery). A Pearson’s chi-squared test (or Fisher’s exact test when appropriate) was used for each variable.
We then placed all variables with P < .1 from the bivariate analysis into a multivariable regression model to identify which population characteristics were independently associated with preferring early surgery. Variables were considered using an enter selection method. The results are presented as adjusted odds ratios (ORs) with 95% confidence intervals (CIs). A threshold of P < .05 was used to delineate statistical significance.
Results
Overall, 776 participants completed our survey. After excluding surveys with incomplete data, 722 responses remained for final analysis. Demographic data of our sample population is reported in Table 1 .
Table 1.
Survey Participant Characteristics (n = 722).
| Variable, n (%) | Respondents |
|---|---|
| Age in years | |
| ≤40 | 479 (66.3) |
| 41-60 | 173 (24.0) |
| >60 | 70 (9.7) |
| Sex | |
| Female | 387 (53.6) |
| Male | 335 (46.4) |
| Race | |
| White | 520 (72.0) |
| Black | 44 (6.1) |
| Asian | 119 (16.5) |
| Other | 39 (5.4) |
| Native English speaker | |
| Yes | 675 (93.5) |
| No | 47 (6.5) |
| Marital status | |
| Single | 294 (40.7) |
| Separated/divorced | 58 (8.0) |
| Married | 353 (48.9) |
| Widowed | 17 (2.4) |
| Annual income in US$ | |
| <30,000 | 200 (27.7) |
| 30,000-60,000 | 285 (39.5) |
| >60,000 | 237 (32.8) |
| United States region | |
| Northeast | 169 (23.4) |
| Midwest | 180 (24.9) |
| South | 257 (35.6) |
| West | 116 (16.1) |
| Primary health insurance | |
| Medicare | 146 (20.2) |
| Medicaid | 71 (9.8) |
| Private | 433 (60.0) |
| Veterans Affairs | 11 (1.5) |
| Uninsured | 61 (8.4) |
| Perceived overall health status | |
| Poor or fair | 55 (7.6) |
| Good | 308 (42.7) |
| Very good or excellent | 359 (49.7) |
| Major depressive disordera | 155 (21.5) |
| Limited health literacyb | 128 (17.7) |
| Low patient engagementc | 79 (10.9) |
Defined as Patient Health Questionnaire-2 (PHQ-2) score of 3 or greater.
Defined as answers of “somewhat/a little/not at all” to the single health literacy screening question.
Defined as an answer of “not very confident” to the single health confidence question.
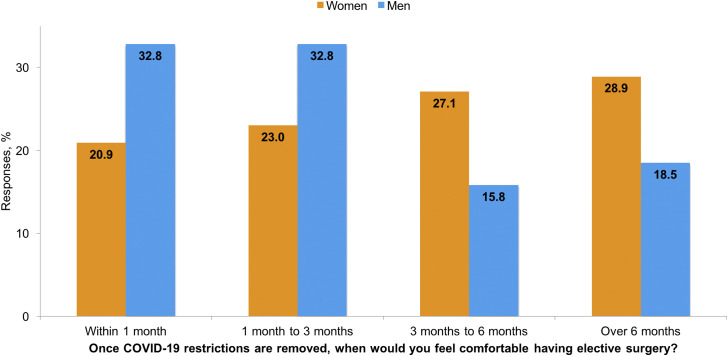
Most (61.1%) participants were concerned (answered “somewhat” or “to a great extent”) with contracting COVID-19 during the surgical process, whereas 58.6% were worried that they would expose family members (Table 2 ). Concern centered around the check-in process and waiting room areas (39.9%), as well as excessive interactions with staff (25.5%). Overall, 56.6% of participants preferred to have their procedure performed at a hospital rather than at an outpatient surgery center. Twenty-eight percent of participants would pay an extra fee to have their procedure performed sooner if placed on a long wait list, whereas 37.7% would change surgeons in this scenario. Just under half (49.6%) reported a preference toward a virtual telehealth visit over an in-person visit for their first postoperative appointment. Women more commonly preferred to delay surgery compared with men (Figure 1 ). A sensitivity analysis was performed for participants over the age of 60 years, which demonstrated similar trends (Appendix B).
Table 2.
Public Perceptions of Resuming Elective Surgery During the COVID-19 Pandemic (n = 722).
| Question/Statement | Respondents, n (%) |
|||
|---|---|---|---|---|
| Not at all | Very Little | Somewhat | To a Great Extent | |
| How worried would you be about becoming infected with COVID-19 if you were in the hospital getting surgery? | 86 (11.9) | 195 (27.0) | 273 (37.8) | 168 (23.3) |
| How worried would you be about the risk of exposing your family to COVID-19 after your surgery? |
81 (11.2) |
218 (30.2) |
264 (36.6) |
159 (22.0) |
| Within 1 mo |
1 mo to 3 mo |
3 mo to 6 mo |
Greater than 6 mo |
|
| Once COVID-19 restrictions are removed, when would you feel comfortable having elective (nonurgent) surgery? | 191 (26.5) | 199 (27.6) | 158 (21.9) | 174 (24.1) |
| Hospital |
Outpatient Surgery Center |
|||
| If given the choice, where would you prefer to have elective (nonurgent) surgery post-COVID-19? | 409 (56.6) | 313 (43.4) | ||
| No | Yes | |||
| There may be a long wait list for elective surgery post-COVID-19. Would you pay an extra fee to have your surgery done sooner? | 517 (71.6) | 205 (28.4) | ||
| There may be a long wait list for elective surgery post-COVID-19. Would you change surgeons if you had to wait too long? |
450 (62.3) |
272 (37.7) |
||
| Check-in and waiting room |
Operating room |
Interactions with staff |
Postsurgery recovery area |
|
| What part of the surgical process would worry you the most about getting COVID-19? | 288 (39.9) | 129 (17.9) | 184 (25.5) | 121 (16.8) |
| In-person visit |
Telehealth visit |
|||
| For your first visit after surgery, would you prefer to see your surgeon in-person or with a video call (telehealth)? | 364 (50.4) | 358 (49.6) | ||
Fig. 1.
Figure showing preferred timing of elective surgery following the reopening of health systems.
A bivariate analysis was performed to determine population characteristics associated with feeling comfortable undergoing early elective surgery (within one month) after health systems resume elective surgery. Just over 1 in 4 (27%) felt comfortable undergoing early elective surgery. These respondents were more likely to be male (57.6% vs 42.4%; P < .001), native English speakers (96.9% vs 92.3%; P = .028), earn less than $30,000 annually (34.6% vs 25.2%; P = .047), and have Veterans Affairs as their primary health insurance (4.2% vs 0.6%; P < .001) (Table 3 ).
Table 3.
Population Characteristics Associated With Preferring Early Surgery (Within 1 Month) After Health Systems Resume Elective Care.
| Variable, n (%) | Decision for Early Surgery |
P | Adjusted OR (95% CI) | Pd | |
|---|---|---|---|---|---|
| No | Yes | ||||
| Total | 531 (73.5) | 191 (26.5) | |||
| Age in years | |||||
| ≤40 | 345 (65.0) | 134 (70.2) | .086 | 1.0 (0.55-1.8) | .999 |
| 41-60 | 138 (26.0) | 35 (18.3) | 0.71 (0.36-1.4) | .334 | |
| >60 | 48 (9.0) | 22 (11.5) | Ref. | ||
| Sex | |||||
| Female | 306 (57.6) | 81 (42.4) | <.001 | Ref. | |
| Male | 225 (42.4) | 110 (57.6) | 1.9 (1.3-2.7) | <.001 | |
| Race | |||||
| White | 377 (71.0) | 143 (74.9) | .637 | - | |
| Black | 33 (6.2) | 11 (5.8) | - | ||
| Asian | 93 (17.5) | 26 (13.6) | - | ||
| Other | 28 (5.3) | 11 (5.8) | - | ||
| Native English speaker | |||||
| Yes | 490 (92.3) | 185 (96.9) | .028 | 2.6 (1.04-6.4) | .042 |
| No | 41 (7.7) | 6 (3.1) | Ref. | ||
| Marital status | |||||
| Single | 211 (39.7) | 83 (43.5) | .722 | - | |
| Separated/divorced | 43 (8.1) | 15 (7.9) | - | ||
| Married | 263 (49.5) | 90 (47.1) | - | ||
| Widowed | 14 (2.6) | 3 (1.6) | - | ||
| Annual income in US$ | |||||
| <30,000 | 134 (25.2) | 66 (34.6) | .047 | 1.4 (0.88-2.3) | .151 |
| 30,000-60,000 | 216 (40.7) | 69 (36.1) | 0.91 (0.59-1.4) | .647 | |
| >60,000 | 181 (34.1) | 56 (29.3) | Ref. | ||
| United States region | |||||
| Northeast | 125 (23.5) | 44 (23.0) | .057 | Ref. | |
| Midwest | 119 (22.4) | 61 (31.9) | 1.5 (0.91-2.4) | .111 | |
| South | 196 (36.9) | 61 (31.9) | 0.89 (0.55-1.4) | .625 | |
| West | 91 (17.1) | 25 (13.1) | 0.76 (0.42-1.4) | .352 | |
| Primary health insurance | |||||
| Medicare | 98 (18.5) | 48 (25.1) | <.001 | Ref. | |
| Medicaid | 51 (9.6) | 20 (10.5) | 0.82 (0.42-1.6) | .545 | |
| Private | 341 (64.2) | 92 (48.2) | 0.66 (0.42-1.03) | .066 | |
| Veterans Affairs | 3 (0.6) | 8 (4.2) | 4.5 (1.1-18.7) | .036 | |
| Uninsured | 38 (7.2) | 23 (12.0) | 1.3 (0.69-2.5) | .401 | |
| Perceived overall health status | |||||
| Poor or fair | 42 (7.9) | 13 (6.8) | .344 | - | |
| Good | 218 (41.1) | 90 (47.1) | - | ||
| Very good or excellent | 271 (51.0) | 88 (46.1) | - | ||
| Major depressive disordera | 110 (20.7) | 45 (23.6) | .412 | - | |
| Limited health literacyb | 91 (17.1) | 37 (19.4) | .488 | - | |
| Low patient engagementc | 60 (11.3) | 19 (9.9) | .608 | - | |
Defined as Patient Health Questionnaire-2 (PHQ-2) score of 3 or greater.
Defined as answers of “somewhat/a little/not at all” to the single health literacy screening question.
Defined as an answer of “not very confident” to the single health confidence question.
Bold denotes significant result (P < .05) in multivariable regression.
After controlling for potential confounding effects in the multivariable regression model (Table 3), the population characteristics independently associated with feeling comfortable undergoing early elective surgery included male sex (OR, 1.9; 95% CI, 1.3-2.7; P < .001), native English speaking (OR, 2.6; 95% CI, 1.04-6.4; P = .042), and Veterans Affairs insurance (OR, 4.5 reference: Medicare; 95% CI, 1.1-18.7; P = .036).
Of note, there was no association between a preference toward early surgery and age (P = .086), geographic region of residence (P = .057), perceived overall health status (P = .344), or marital status (P = .722). Furthermore, race (P = .637), a history of major depressive disorder (P = .412), health literacy (P = .488), and patient engagement (P = .608) were not predictive of the timing of preferred surgery.
Discussion
As the COVID-19 burden declines and society slowly reopens, health systems are beginning to resume elective procedures. A clear understanding of the public’s beliefs regarding the resumption of elective surgery may help guide health systems in providing patients with equitable, efficient, and safe care while also optimizing financial stability through this transition period. In this context, we used an online crowdsourcing platform to explore public perceptions and concerns toward resuming elective surgery during the COVID-19 pandemic, and to determine factors associated with the timing of preferred surgery after health systems reopen.
The primary strengths of this study include its large sample size and the novel use of an online crowdsourcing platform to obtain survey responses. The rapid evolution and daily changes occurring throughout the COVID-19 pandemic has created an information lag in the medical community [26]. The nature of the pandemic has resulted in many clinical decisions being made with a dearth of quality evidence [[27], [28], [29]]. Clinical trials cannot be conducted fast enough to maintain pace with the rate of change. The ability of MTurk to obtain reliable, consistent, and generalizable survey responses significantly faster and with decreased costs compared with traditional methods makes its use for data collection during the COVID-19 pandemic and beyond opportune [20,22].
Despite its strengths, our study was not without limitations. The primary weakness of this study is the lack of preexisting symptomatic pathology in our study population. An expectant approach toward surgery may be less likely in patients coping with disabling musculoskeletal conditions. However, the beliefs of our cohort are a reasonable proxy to use in this case for several reasons. Multiple prior survey studies have used the general public as a proxy to understand the perceptions of patients choosing to undergo elective surgery [30,31]. Furthermore, the MTurk platform has been extensively evaluated and is thought to have arguably closer generalizability to the US population than results derived using traditional survey methods [20,32]. Another weakness of the study is that certain MTurk users may have chosen to not participate in the study. It is unknown whether the demographics of this group differed from our sample population. Finally, the higher computer literacy of our sample population may have biased their responses toward favoring telehealth for their postoperative care.
We found that men strongly favored early surgery, whereas women demonstrated a preference toward delaying surgery. Interestingly, this same trend has been reported in regard to patients undergoing total joint arthroplasty (TJA) before the COVID-19 pandemic [33]. Gender bias, specifically in the form of surgeons being less likely to recommend TJA and including fewer shared decision-making elements to women [34,35], may play a role in this phenomenon. However, other studies have demonstrated that the values influencing the decision to undergo surgery may also differ between sexes and contribute to this trend [33]. Specifically, a study by Karlson et al. described that the women with knee osteoarthritis overwhelmingly chose to delay undergoing total knee arthroplasty longer than men because of more concerns of a bad outcome, the hope for improved future technology, and their perceived caregiver responsibilities [33]. Men conversely preferred earlier surgery as they wanted to return to a high functional level sooner, were more trusting of their surgeons, and less fearful of a bad outcome [33].
Interestingly, there may be risks unique to undergoing both early and late surgery after health systems reopen. Surgery soon after the reintroduction of elective procedures might place patients an increased risk of contracting COVID-19, as hospitals will have had less time to optimize their protocols. On the other hand, choosing to delay surgery may result in excessive postponement as long wait lists and a possible “second-wave” may occur. A shared decision-making process including a discussion of the risks and benefits of each option should be undertaken with each patient. Nevertheless, deliberate and strategic efforts must be undertaken to ensure equitable treatment to both sexes throughout the surgical process.
Our study also demonstrated that non-English speakers preferred to delay elective surgery. Reports in the lower limb arthroplasty literature have previously described a similar trend in non-native English speakers [36]. Many of the communities hit hardest by the COVID-19 pandemic have been largely comprised of non-English speakers [15]. It might be possible that the worldview non-native English speakers have developed during this pandemic has shifted their preference toward delaying elective surgery even further to limit interactions with the health care system. Mistrust and fear of the health care system may last well past the peak of the pandemic in this community. Furthermore, communication hurdles, specifically in regard to obtaining up-to-date COVID-19 information, and cultural differences are other factors that might influence non-native English speakers regardless of their socioeconomic status or residence location. Certainly, dedicated outreach programs geared toward minimizing language barriers through the surgical process are warranted.
Participants who listed Veterans Affairs as their primary insurance type showed a predilection toward preferring early surgery in our study. Patients utilizing veterans affairs services often are subject to long wait lists and institutional inefficiencies [37]. Given these baseline factors, it may be reasonable to assume that these patients would prefer to have their elective procedures completed as soon as possible once health systems reopen. Furthermore, fears of future budget cuts given the economic implications of the COVID-19 pandemic on the U.S. government may also predispose this population toward preferring early surgery [38].
Notably, our analysis did not find an association between age, perceived overall health status, or geographic region of residence with the timing of preferred surgery. Given the increased risk of a more severe form of COVID-19 in older patients [39,40] and patients with certain comorbidities [[41], [42], [43]], it may be anticipated that these patients would take an expectant approach toward the timing of elective surgery given the possibility of contracting the virus during the surgical process. This same trend may also be expected among patients residing in regions of the United States that have been hit hardest during the pandemic [44]. Interestingly, this was not the case in our analysis, as these populations did not show a predilection toward delaying surgery. Providers should be aware of the fact that “higher risk” patients may be just as willing to undergo early elective surgery as the general population. Because of the unknown risk of contracting COVID-19 during the surgical process, careful consideration and discussion should be undertaken with each patient before surgical booking.
Another interesting theme that emerged in our study was the relatively large proportion of participants who would prefer to have their procedure performed at a hospital (56.6%) instead of an outpatient surgery center. Despite the theoretical higher risk of contracting COVID-19 at an inpatient facility, where infected patients are presumably receiving treatment, much of the public paradoxically would still prefer to have surgery in a hospital setting. While it should be noted that patients would likely be more amenable to having surgery at an outpatient center for certain procedures over others, previous reports have cited concerns over pain control, falling, and not having enough help at home as reasons patients are hesitant to have surgery at outpatient facilities [45]. As health systems will inevitably transition many elective cases to outpatient facilities throughout this pandemic [46], providers should be aware of patient concerns and preferences in this shift and adjust on a patient-to-patient basis.
Finally, our study demonstrated that the most concerning aspects of the surgical process to the public were the check-in and waiting room areas, as well as interactions with staff. Minimizing crowding in the waiting room, proper availability of personal protective equipment for staff and patients, and minimizing unnecessary face-to-face interactions with patients during the surgical process might help optimize the patient experience and minimize the spread of COVID-19 [7]. This is especially relevant as payers are increasingly linking financial incentives to the patient experience [47]. Furthermore, transitioning to telehealth postoperative visits and home-based virtual physical therapy programs to minimize public interactions may improve patient compliance, optimize costs, and regain public confidence in the safety of restarting elective care during this pandemic [46].
Conclusion
Women and non-native English speakers may be more hesitant than others to proceed with elective surgery amid the COVID-19 pandemic, and should receive careful discussion through the surgical decision-making process. Despite concerns of contagion, more than half of the public favors a hospital setting over an outpatient surgery center for their elective surgery. Concerted efforts to minimize patient congestion and unnecessary face-to-face interactions may prove to be most effective in reducing public anxiety and concerns over the safety of resuming elective care.
Footnotes
Investigation performed at New England Baptist Hospital, Boston, Massachusetts.
One or more of the authors of this paper have disclosed potential or pertinent conflicts of interest, which may include receipt of payment, either direct or indirect, institutional support, or association with an entity in the biomedical field which may be perceived to have potential conflict of interest with this work. For full disclosure statements refer to https://doi.org/10.1016/j.arth.2020.07.037.
Appendix A. Supplementary Data
Appendix
Appendix A: Public Perceptions of Resuming Elective Surgery During the COVID-19 Pandemic
1. Age
A: <40 B: 41-60 C: >60
2. Sex
A: Male B: Female
3. Is English your native language?
A: Yes B: No
4. Where do you live in the United States?
A: Northeast B: Midwest C: South D: West.
5. Marital status
A: Single B: Married C: Separated/Divorced D: Widowed
6. Annual income
A: <$30,000 B: $30,000 - $60,000 C: >$60,000
7. Race
A: White B: Black C: Asian D: Other
8. Health insurance
A: Private or commercial B: Medicare C: Medicaid D: Military or Veterans Administration E: None
9. How often do you need to have someone help read or interpret instructions, pamphlets, or other written material from your doctor or pharmacy?
A: Never B: Rarely C: Sometimes D: Most of the time E: Always
10. Over the last 2 weeks, how often have you had little interest or pleasure in doing things?
A: Not at all B: Several days C: More than half the days D: Nearly every day
11. Over the last 2 weeks, how often have you felt down, depressed, or hopeless?
A: Not at all B: Several days C: More than half the days D: Nearly every day
12. How is your overall health status?
A: Poor or fair B: Good C: Very good D: Excellent
13. How worried are you about becoming infected with COVID-19 if you were in the hospital getting surgery?
A: Not at all B: Very little C: Somewhat D: To a great extent
14. Once state COVID-19 restrictions are removed, when would you feel comfortable having elective (nonurgent) surgery?
A: ≤1 month B: 1 month to 3 months C: 3 months to 6 months D: >6 months
15. If given the choice, where would you prefer to have elective (nonurgent) surgery post-COVID-19?
A: Hospital B: Free-standing ambulatory surgery center
16. There may be a long wait list for elective (nonurgent) surgery after COVID-19. Would you pay an extra fee to have your elective (nonurgent) surgery done sooner?
A: Yes B: No
17. There may be a long wait list for elective (nonurgent) surgery after COVID-19. Would you change surgeons if you had to wait too long?
A: Yes B: No.
18. How worried would you be about the risk of exposing your family to COVID-19 after your surgery?
A: Not at all B: Very little C: Somewhat D: To a great extent
19. What part of the surgical process would worry you the most about getting COVID-19?
A: Check-in and waiting room B: Operating room C: Postsurgery recovery area D: Interactions with staff
20. For your first visit after surgery, would you prefer to see your surgeon in-person or with a video call (telehealth)?
A: In-person appointment B: Video call (telehealth)
21. How confident are you that you can control and manage most of your health problems?
A: Very confident B: Somewhat confident C: Not very confident D: I don’t not have any health problems
Appendix B.
Sensitivity Analysis in the Public >60 years Old (n = 70).
| Question/Statement | Respondents, n (%) |
|||
|---|---|---|---|---|
| Not at all | Very Little | Somewhat | To a Great Extent | |
| How worried would you be about becoming infected with COVID-19 if you were in the hospital getting surgery? | 10 (14.3) | 14 (20.0) | 23 (32.9) | 23 (32.9) |
| How worried would you be about the risk of exposing your family to COVID-19 after your surgery? |
11 (15.7) |
22 (31.4) |
21 (30.0) |
16 (22.9) |
| Within 1 mo |
1 mo to 3 mo |
3 mo to 6 mo |
Greater than 6 mo |
|
| Once COVID-19 restrictions are removed, when would you feel comfortable having elective (nonurgent) surgery? |
22 (31.4) |
15 (21.4) |
20 (28.6) |
13 (18.6) |
| Hospital |
Outpatient Surgery Center |
|||
| If given the choice, where would you prefer to have elective (nonurgent) surgery post-COVID-19? | 37 (52.9) | 33 (47.1) | ||
| No | Yes | |||
| There may be a long wait list for elective surgery post-COVID-19. Would you pay an extra fee to have your surgery done sooner? | 48 (68.6) | 22 (31.4) | ||
| There may be a long wait list for elective surgery post-COVID-19. Would you change surgeons if you had to wait too long? |
52 (74.3) |
18 (25.7) |
||
| Check-in and waiting room |
Operating room |
Interactions with staff |
Postsurgery recovery area |
|
| What part of the surgical process would worry you the most about getting COVID-19? |
26 (37.1) |
12 (17.1) |
23 (32.9) |
9 (12.9) |
| In-person visit |
Telehealth visit |
|||
| For your first visit after surgery, would you prefer to see your surgeon in-person or with a video call (telehealth)? | 35 (50.0) | 35 (50.0) | ||
References
- 1.Association A.H. Hospitals and Health Systems Face Unprecedented Financial Pressures Due to COVID-19. 2020. https://www.aha.org/system/files/media/file/2020/05/aha-covid19-financial-impact-0520-FINAL.pdf [accessed 05.11.2020]
- 2.Services C.f.M.M. Non-Emergent, Elective Medical Services, and Treatment Recommendations. cms.gov. 2020. https://www.cms.gov/files/document/cms-non-emergent-elective-medical-recommendations.pdf [accessed 05.11.2020]
- 3.Health F. The Projected Economic Impact of the COVID-19 Pandemic on the US Healthcare System. 2020. https://s3.amazonaws.com/media2.fairhealth.org/brief/asset/COVID-19%20-%20The%20Projected%20Economic%20Impact%20of%20the%20COVID-19%20Pandemic%20on%20the%20US%20Healthcare%20System.pdf [accessed 05.11.2020]
- 4.Anoushiravani A.A., O’Connor C.M., DiCaprio M.R., Iorio R. Economic impacts of the COVID-19 crisis: an orthopaedic perspective. J Bone Joint Surg Am. 2020;102:937–941. doi: 10.2106/JBJS.20.00557. 9000;Latest Articles. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cutler D.M., Nikpay S., Huckman R.S. The business of medicine in the Era of COVID-19. JAMA. 2020;323:2003–2004. doi: 10.1001/jama.2020.7242. [DOI] [PubMed] [Google Scholar]
- 6.Abelson R. New York Times; New York City, NY: 2020. Hospitals struggle to restart lucrative elective care after coronavirus. [Google Scholar]
- 7.Parvizi J., Gehrke T., Krueger C.A., Chisari E., Citak M., Van Onsem S. MBBS. Current concepts review resuming elective orthopaedic surgery during the COVID-19 pandemic. J Bone Joint Surg. 2020;102:1205–1212. doi: 10.2106/JBJS.20.00844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Surgeons ACo Joint Statement: Roadmap for Resuming Elective Surgery after COVID-19 Pandemic. 2020. https://www.facs.org/covid-19/clinical-guidance/roadmap-elective-surgery [accessed 05.11.2020]
- 9.Rosenbaum L. The Untold Toll — the Pandemic’s effects on patients without Covid-19. N Engl J Med. 2020;382:2368–2371. doi: 10.1056/NEJMms2009984. [DOI] [PubMed] [Google Scholar]
- 10.Carroll C.I., Aziz K.T., Humbyrd C.J. Elective Reconstructive Surgery During a Pandemic: A Moral Dilemma. J Bone Joint Surg Am. 2020;102(e51):1–4. doi: 10.2106/JBJS.20.00524. 9000;Latest Articles. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brown T.S., Bedard N.A., Rojas E.O., Anthony C.A., Schwarzkopf R., Barnes C.L. The effect of the COVID-19 pandemic on electively scheduled hip and knee arthroplasty patients in the United States. J Arthroplasty. 2020;35:S49–S55. doi: 10.1016/j.arth.2020.04.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hoffmann D.E., Tarzian A.J. The girl who cried pain: a bias against women in the treatment of pain. J Law Med Ethics. 2001;29(Spring):13–27. doi: 10.1111/j.1748-720x.2001.tb00037.x. [DOI] [PubMed] [Google Scholar]
- 13.Organization W.H. World Health Organization; Geneva, Switzerland: 2009. Women and health: today’s evidence tomorrow’s agenda. [Google Scholar]
- 14.Chowkwanyun M., Reed A.L. Racial health disparities and Covid-19 — Caution and context. N Engl J Med. 2020;383:201–203. doi: 10.1056/NEJMp2012910. [DOI] [PubMed] [Google Scholar]
- 15.Ross J., Diaz C.M., Starrels J.L. The disproportionate burden of COVID-19 for immigrants in the Bronx, New York. JAMA Intern Med. 2020;180:1043–1044. doi: 10.1001/jamainternmed.2020.2131. [DOI] [PubMed] [Google Scholar]
- 16.Arroll B., Goodyear-Smith F., Crengle S., Gunn J., Kerse N., Fishman T. Validation of PHQ-2 and PHQ-9 to screen for major depression in the primary care population. Ann Fam Med. 2010;8:348–353. doi: 10.1370/afm.1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Keene Woods N., Chesser A.K. Validation of a Single question health literacy Screening tool for older adults. Gerontol Geriatr Med. 2017;3 doi: 10.1177/2333721417713095. 2333721417713095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wasson J., Coleman E.A. Health confidence: a simple, essential measure for patient engagement and better practice. Fam Pract Manag. 2014;21:8–12. [PubMed] [Google Scholar]
- 19.Albaum G. The Likert scale revisited. Market Res Soc J. 1997;39:1–21. [Google Scholar]
- 20.Mortensen K., Hughes T.L. Comparing Amazon's mechanical Turk platform to conventional data collection methods in the health and medical research literature. J Gen Intern Med. 2018;33:533–538. doi: 10.1007/s11606-017-4246-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stewart N., Ungemach C., Harris A.J., Bartels D.M., Newell B.R., Paolacci G. The average laboratory samples a population of 7,300 Amazon Mechanical Turk workers. Judgment Decis Making. 2015;10:479–491. [Google Scholar]
- 22.Chandler J., Shapiro D. Conducting clinical research using crowdsourced convenience samples. Annu Rev Clin Psychol. 2016;12:53–81. doi: 10.1146/annurev-clinpsy-021815-093623. [DOI] [PubMed] [Google Scholar]
- 23.Perman S.M., Shelton S.K., Knoepke C., Rappaport K., Matlock D.D., Adelgais K. Public perceptions on why women receive less bystander cardiopulmonary resuscitation than men in out-of-hospital cardiac arrest. Circulation. 2019;139:1060–1068. doi: 10.1161/CIRCULATIONAHA.118.037692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Paolacci G., Chandler J., Ipeirotis P.G. Running experiments on amazon mechanical turk. Judgment Decis Making. 2010;5:411–419. [Google Scholar]
- 25.Berinsky A.J., Huber G.A., Lenz G.S. Evaluating online labor markets for experimental research: amazon. com's Mechanical Turk. Polit Anal. 2012;20:351–368. [Google Scholar]
- 26.nick. white@covid19crc. org C-CRCEa Global coalition to accelerate COVID-19 clinical research in resource-limited settings. Lancet. 2020;395:1322–1325. doi: 10.1016/S0140-6736(20)30798-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang W., Qian B.Y. Making decisions to mitigate COVID-19 with limited knowledge. Lancet Infect Dis. 2020;3099:30280–30282. doi: 10.1016/S1473-3099(20)30280-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gautret P., Lagier J.C., Parola P., Hoang V.T., Meddeb L., Mailhe M. Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. Int J Antimicrob Agents. 2020:105949. doi: 10.1016/j.ijantimicag.2020.105949. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 29.Geleris J., Sun Y., Platt J., Zucker J., Baldwin M., Hripcsak G. Observational study of hydroxychloroquine in hospitalized patients with Covid-19. N Engl J Med. 2020;382:2411–2418. doi: 10.1056/NEJMoa2012410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Edgington J.P., Petravick M.E., Idowu O.A., Lee M.J., Shi L.L. Preferably not my surgery: a survey of patient and family member comfort with concurrent and overlapping surgeries. J Bone Joint Surg Am. 2017;99:1883–1887. doi: 10.2106/JBJS.17.00414. [DOI] [PubMed] [Google Scholar]
- 31.Kent M., Whyte R., Fleishman A., Tomich D., Forrow L., Rodrigue J. Public perceptions of overlapping surgery. J Am Coll Surg. 2017;224:771–778.e4. doi: 10.1016/j.jamcollsurg.2017.01.059. [DOI] [PubMed] [Google Scholar]
- 32.Casler K., Bickel L., Hackett E. Separate but equal? A comparison of participants and data gathered via Amazon’s MTurk, social media, and face-to-face behavioral testing. Comput Hum Behav. 2013;29:2156–2160. [Google Scholar]
- 33.Karlson E.W., Daltroy L.H., Liang M.H., Eaton H.E., Katz J.N. Gender differences in patient preferences may underlie differential utilization of elective surgery. Am J Med. 1997;102:524–530. doi: 10.1016/s0002-9343(97)00050-8. [DOI] [PubMed] [Google Scholar]
- 34.Borkhoff C.M., Hawker G.A., Kreder H.J., Glazier R.H., Mahomed N.N., Wright J.G. The effect of patients' sex on physicians' recommendations for total knee arthroplasty. CMAJ. 2008;178:681–687. doi: 10.1503/cmaj.071168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Borkhoff C.M., Hawker G.A., Wright J.G. Patient gender affects the referral and recommendation for total joint arthroplasty. Clin Orthop Relat Res. 2011;469:1829–1837. doi: 10.1007/s11999-011-1879-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Alley M.C., Mason A.S., Tybor D.J., Pevear M.E., Baratz M.D., Smith E.L. Ethnic barriers to utilization of total joint arthroplasty among Chinese immigrants in the United States. J Arthroplasty. 2016;31:1873–1877.e2. doi: 10.1016/j.arth.2016.02.046. [DOI] [PubMed] [Google Scholar]
- 37.Argo J.L., Vick C.C., Graham L.A., Itani K.M., Bishop M.J., Hawn M.T. Elective surgical case cancellation in the Veterans Health Administration system: identifying areas for improvement. Am J Surg. 2009;198:600–606. doi: 10.1016/j.amjsurg.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 38.Company M. McKinsey & Company; 2020. COVID-19: Briefing Materials.https://www.mckinsey.com/∼/media/McKinsey/Business%20Functions/Risk/Our%20Insights/COVID%2019%20Implications%20for%20business/COVID%2019%20May%2027/COVID-19-Facts-and-Insights-June-1-vF.pdf [accessed 01.06.20] [Google Scholar]
- 39.Deng G., Yin M., Chen X., Zeng F. Clinical determinants for fatality of 44,672 patients with COVID-19. Crit Care. 2020;24:179. doi: 10.1186/s13054-020-02902-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Organization W.H. World Health Organization; 2020. Coronavirus Disease 2019 Situation Reports - 89.https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200418-sitrep-89-covid-19.pdf?sfvrsn=3643dd38_2 [accessed 01.06.20] [Google Scholar]
- 41.Fadini G.P., Morieri M.L., Longato E., Avogaro A. Prevalence and impact of diabetes among people infected with SARS-CoV-2. J Endocrinol Invest. 2020;43:867–869. doi: 10.1007/s40618-020-01236-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yang J., Zheng Y., Gou X., Pu K., Chen Z., Guo Q. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis. 2020;94:91–95. doi: 10.1016/j.ijid.2020.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lighter J., Phillips M., Hochman S., Sterling S., Johnson D., Francois F. Obesity in patients younger than 60 years is a risk factor for Covid-19 hospital admission. Clin Infect Dis. 2020;71:896–897. doi: 10.1093/cid/ciaa415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Control CfD. Centers for Disease Control and Prevention; 2020. Geographic differences in COVID-19 cases, deaths, and incidence — United States, February 12–April 7, 2020.https://www.cdc.gov/mmwr/volumes/69/wr/mm6915e4.htm [accessed 01.06.20] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Adelani M.A., Barrack R.L. Patient perceptions of the safety of outpatient total knee arthroplasty. J Arthroplasty. 2019;34:462–464. doi: 10.1016/j.arth.2018.11.030. [DOI] [PubMed] [Google Scholar]
- 46.Menendez M.E., Jawa A., Haas D.A., Warner J.J.P., Codman Shoulder S. Orthopedic surgery post COVID-19: an opportunity for innovation and transformation. J Shoulder Elbow Surg. 2020;29:1083–1086. doi: 10.1016/j.jse.2020.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Centers for M., Medicaid Services H.H.S. Medicare program; hospital outpatient prospective payment system and CY 2007 payment rates; CY 2007 update to the ambulatory surgical center covered procedures list; Medicare administrative contractors; and reporting hospital quality data for FY 2008 inpatient prospective payment system annual payment update program--HCAHPS survey, SCIP, and mortality. Final rule with comment period and final rule. Fed Regist. 2006;71:67959–68401. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.