Abstract
Background
Disease severity on chest radiographs (CXR) has been associated with higher risk of disease progression and adverse outcomes from COVID-19. Few studies have evaluated COVID-19-related racial/ethnic disparities in radiology.
Purpose
To evaluate whether Non-White minority patients hospitalized with confirmed COVID-19 infection presented with increased severity on admission CXR compared with White/Non-Hispanic patients.
Methods
Single-institution, retrospective cohort study approved by the IRB. Patients hospitalized with confirmed COVID-19 infection (3/27/20-4/10/20) were identified using the electronic medical record (EMR) (n=326, mean age: 59 years (SD: 17 years), M:F (188:138). Primary outcome was severity of lung disease on admission CXR, measured by modified Radiographic Assessment of Lung Edema (mRALE) score. Secondary outcome was a composite adverse clinical outcome of intubation, ICU admission, or death. Primary exposure was racial/ethnic category: White/Non-Hispanic versus Non-White [i.e., Hispanic, Black, Asian, Other]. Multivariable linear regression analyses were performed to evaluate the association between mRALE scores and race/ethnicity.
Results
Non-White patients had significantly higher mRALE scores (median 6.1, 95% CI 5.4–6.7) compared with White/Non-Hispanic patients (median 4.2, 95% CI 3.6–4.9) (unadjusted average difference 1.8, 95% CI 0.9–2.8, p<0.01). For both White (Adjusted HR, 1.3, 95%CI 1.2-1.4, p<0.001) and Non-White patients (Adjusted HR 1.2, 95%CI 1.1-1.3, p<0.001), increasing mRALE scores were associated with a higher likelihood of experiencing composite adverse outcome with no evidence of interaction (p = 0.16). Multivariable linear regression analyses demonstrated that Non-White patients presented with higher mRALE scores on admission CXR versus White/Non-Hispanic patients (adjusted average difference 1.6, 95% CI 0.5–2.7, p<0.01). Adjustment for hypothesized mediators revealed that the association between race/ethnicity and mRALE scores was mediated by limited English proficiency (p<0.01).
Conclusion
Non-White patients hospitalized with COVID-19 infection were more likely to present with higher severity of disease on admission CXR than White/Non-Hispanic patients, and increased severity was associated with worse outcomes for all patients.
Summary
Non-White minority patients admitted with confirmed COVID-19 infection were more likely to present with increased disease severity on admission chest radiographs than White/Non-Hispanic patients, increasing the likelihood of adverse clinical outcomes.
Key Results
■ Non-White patients admitted with confirmed COVID-19 infection were more likely to present with increased disease severity on admission chest radiographs, as measured by mRALE score (adjusted average difference=1.6, p<0.01).
■ Higher mRALE scores were associated with increased likelihood of adverse composite clinical outcomes for White/Non-Hispanic (Adjusted HR=1.3, p<0.001) and Non-White patients (Adjusted HR=1.2, p<0.001).
■ Increased radiographic severity among Non-White patients was associated with delayed presentation, low English proficiency, and obesity.
Introduction:
Racial and ethnic minorities experience increased morbidity and mortality from COVID-19, likely secondary to socioeconomic factors and medical comorbidities [1,2]. Comorbidities associated with worse COVID-19 outcomes, such as obesity and hypertension, are historically more prevalent among racial/ethnic minorities.[3] In addition, racial and ethnic minority populations tend to live in multigenerational households and communities of higher population density. These environments make social distancing difficult, thereby facilitating spread of COVID-19.[4] Furthermore, racial/ethnic minorities disproportionately experience lower socioeconomic status and are more often employed in jobs not conducive to remote work with limited paid time off, such as in the service industry, thus increasing their exposure to COVID-19.[5–7] Finally, racial/ethnic minorities are more likely to have limited English proficiency (LEP), which may introduce additional barriers to care.[8] This combination of factors may lead to increased viral exposure and delays in seeking care, potentially resulting in greater severity of disease at the time of presentation with COVID-19 infection.[6] Improved understanding of these factors could promote development of risk mitigation strategies and improve outcomes among racial/ethnic minority groups.
Radiology, particularly chest radiography (CXR) and computed tomography (CT), has played a central role in triage and diagnosis during the COVID-19 pandemic.[9–11] Disease severity on chest imaging has been associated with disease progression and increased risk of adverse clinical outcomes.[11,12] Chest radiographs can help assess disease severity as part of the initial evaluation among symptomatic patients presenting with COVID-19 infection.[12] Severity of disease on CXR can be classified by the modified Radiographic Assessment of Lung Edema (mRALE) score, which has been used to predict adverse outcomes in patients with acute respiratory distress syndrome (ARDS).[13–15] Severity of radiographic findings at the time of presentation may reflect a combination of factors that include delayed presentation, high viral load, and pre-existing comorbidities leading to worse outcomes. However, few published research studies in radiology have assessed disparities in COVID-19 disease severity [1,2]. The purpose of this study was to examine if racial/ethnic minorities were more likely to present with worse disease severity on admission CXR among patients admitted with confirmed COVID-19 infection. We hypothesized that racial/ethnic minority patients would be more likely to present with increased disease severity on admission chest radiographs among patients hospitalized for COVID-19.
Methods:
Study design and setting
Single-institution, retrospective cohort study was HIPAA compliant and approved by the Institutional Review Board with waiver of patient consent. The study was performed at an urban, quaternary care, academic medical center with affiliated community health centers that serve catchment areas with relatively high proportion of individuals of Hispanic ethnicity and high-density housing based on census data.[16]
Cohort
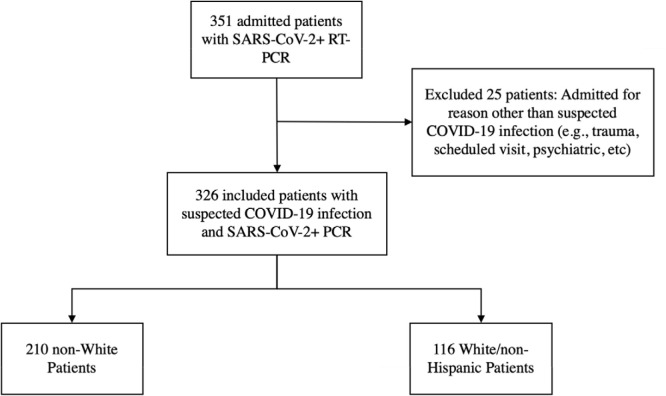
The electronic medical record [(EMR); Epic Hyperspace™; Epic Systems Corp., Verona, WI] was used to identify all adults (ages 23-98 years) hospitalized from March 14, 2020 to April 10, 2020 with suspected COVID-19 infection. Patients with SARS CoV-2 confirmed with nucleic acid testing (NAT) of a nasopharyngeal specimen who had a CXR at the time of admission were included (Figure 1). During this period, only patients with clinical symptoms consistent with COVID-19, or who required testing for admission to an inpatient psychiatric or skilled nursing facility, were tested for SARS CoV-2. Patients without a CXR on admission, admitted for an unrelated presenting medical condition (e.g. trauma after fall) or without a positive NAT were excluded. We obtained follow-up data for all patients until April 24, 2020.
Figure 1:
Patient selection cohort
Variables
Study outcomes
The primary outcome was disease severity of parenchymal lung disease on admission CXR measured by mRALE score among patients admitted with confirmed COVID-19 infection.[15] Secondary outcome was a composite adverse clinical outcome of intubation, ICU admission, or death at time of last follow-up.
Modified Radiographic Assessment of Lung Edema (mRALE) score
The severity of imaging features of COVID-19 infection on CXRs was graded based on a simplified version of the mRALE scale scoring system, which accounts for the extent and severity of lung opacities on CXRs [12]. Each individual lung was scored based on the percentage involvement of opacified lung (0 = no involvement; 1 = <25%, 2 = 25-50%, 3 = 50-75%; 4 = > 75%). For lungs with any opacity, the overall density of the opacity was also scored (1 = hazy; 2 = moderate; 3 = dense). These two scores were multiplied for each lung, and then added together for a total score for each radiograph. Compared to the original RALE score, mRALE differs in that a score is assigned for each lung, instead of four quadrants (2 per lung). The original RALE scoring system was validated in patients with ARDS, and higher scores were associated with worse disease and survival [12]. A deep learning algorithm trained using mRALE scores and applied to hospitalized patients with COVID-19 has shown that lung disease severity can predict subsequent intubation or death [15].
Frontal CXRs performed at the time of admission were independently evaluated and graded using the mRALE score by two radiologists with subspecialty training in thoracic imaging (BPL, DPM) and/or two post-graduate year 4 diagnostic radiology residents (MDL, FD). All raters were instructed with sample cases on how to use the mRALE score to reduce interrater variability. To reduce variability over time, each rater’s scores were assigned in a single rating session (i.e. ratings were not performed at different time periods). The intraclass correlation coefficients (ICC(2,1) between MDL and BPL, DPM, and FD was 0.82, 0.87 and 0.85 respectively [17]. Given these high ICC values, we averaged individual reader mRALE scores for each patient.
Primary exposure
Primary exposure of interest was self-reported race/ethnicity based on current information available in the EMR. Race/ethnicity was dichotomized as White/Non-Hispanic versus Non-White, with the Non-White category including Hispanic (any race), Black alone, Asian alone, other/unavailable, as Black alone, Asian alone and other/unavailable race categories represented a small proportion of the cohort.
Potential confounders
Potential confounders hypothesized a priori to be associated with race/ethnicity or imaging severity score included age, gender, insurance payor, zip code of home address, medical co-morbidities, and clinical symptoms(S1). We used 2015 US Census data from the patient’s home address zip code to capture median household income [18] data at the time of admission regarding comorbidities, clinical presenting symptoms, and symptom onset date was manually collected from the EMR.
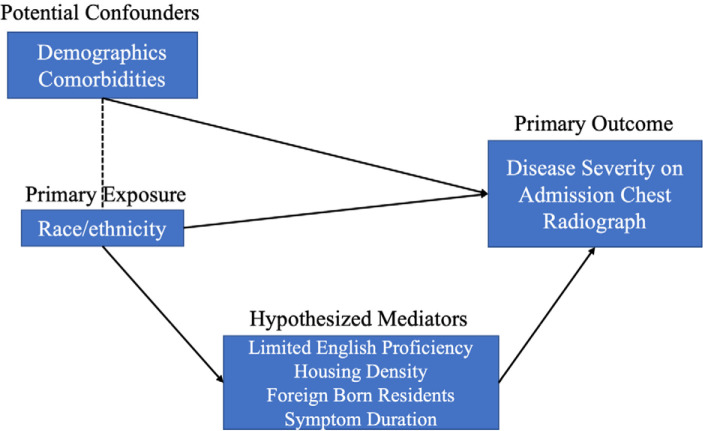
Hypothesized mediators
We hypothesized that limited English proficiency (LEP), housing density (by zip code level), symptom duration, and percentage of foreign-born residents (by zip code level) to represent mechanisms by which the main exposure of interest (race/ethnicity) would be associated with increased disease severity on admission CXR (Figure 2). LEP was defined as patients who had a non-English primary language listed within the EMR. The 2018 American Community Survey data was used to capture the proportion of foreign-born residents in a given zip code and the proportion of households with greater than one occupant per room as a measure of overcrowding [18].
Figure 2:
Causal Model and Variable Description. This causal model demonstrates the interpretation of our statistical modeling of our primary exposure and other variables of interest. Namely, that demographic variables and race/ethnicity directly lead to a portion of our observed primary outcome, but race/ethnicity also is hypothesized to potentially interact with variables such as limited English proficiency, housing density, and foreign-born population at zip code level before our primary outcome is observed.
Statistical analysis plan with sensitivity analyses
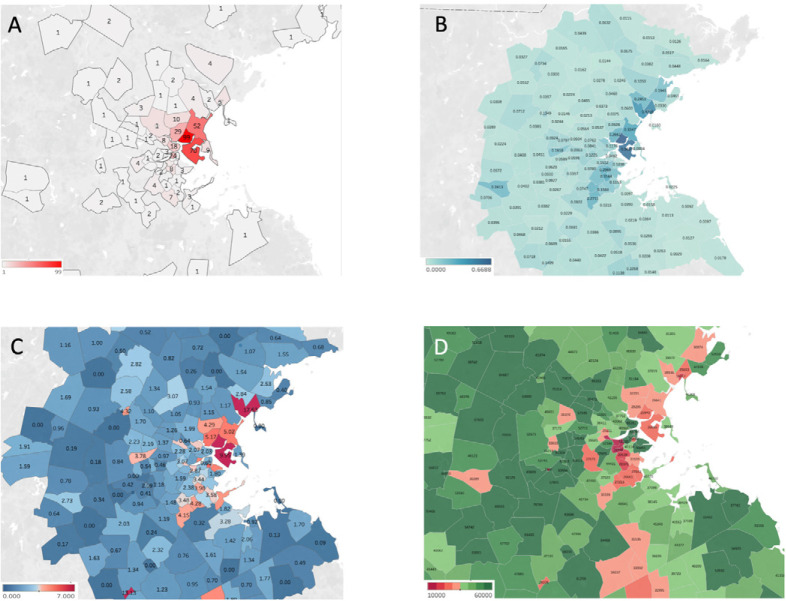
Baseline characteristics were compared between White/Non-Hispanic and Non-Whites. Demographic characteristics for all participants were summarized using means and proportions with 95% confidence intervals. Comparisons were done with student’s t-test, fisher's exact, or chi squared where appropriate. Geospatial data visualization based on the patient’s home address zip-code was compared to zip code-based census data and American Community Survey data, including median income, persons-per-room, and Hispanic population (Tableau Software, version 2020.1, Mountain View, CA).
To evaluate the association between imaging severity, race/ethnicity, and primary language, the primary study outcome (mRALE score) was analyzed in multiple fashions to reflect the differing ways that the variable can be classified. For the primary analysis, we considered mRALE as a continuous outcome variable with scores ranging between 0 – 24. We performed linear regression analyses to evaluate the association between mRALE scores, race/ethnicity, with and without adjustment for potential confounders. Linear regression assumptions about the normality of residuals were evaluated using residual plots and variance inflation factors were used to assess collinearity. Deviations from residual normality were addressed using log transformations.
As a secondary analysis, we categorized the mRALE score as an ordinal response variable. Categories were determined prior to performing the analysis based on clinical consensus from study investigators and informed by prior literature on RALE and mRALE scores.[13,14] Categories for mRALE scores were defined as follows: scores between 0-4 were considered mild, >4-10 were considered moderate, and >10 were considered severe. We performed ordinal logistic regression analyses to evaluate the association between mRALE categories and race/ethnicity with and without adjustment for potential confounders. Proportional odds assumption was tested using likelihood ratio tests. For both analyses, mediation was evaluated by comparing regression coefficients with and without addition of mediator variables into the model.
Multiple variable cox proportional hazards regression analyses were performed to evaluate association between the composite adverse outcome and categorical mRALE scores, adjusted for potential confounders. Proportional hazards assumption was tested based on Schoenfeld residuals.
As our study included readers with varying levels of experience (residents and thoracic radiologists), sensitivity analysis was conducted exclusively using mRALE scores provided by subspecialty trained thoracic radiologists (BPL, DPM). Finally, sensitivity analysis was conducted to reflect changing testing availability in communities affected by COVID-19. After April 1, testing availability was increased, particularly in one of the community health centers located in a predominantly Hispanic neighborhood. To determine if the change in testing availability may have influenced results, we performed a stratified analysis to determine if race/ethnicity was associated with increased extent of disease involvement on admission chest radiograph after April 1. P-values less than 0.05 were considered as statistically significant. Analyses were conducted using Stata 11.2 (StataCorp, College Station, TX).
Bias
Any measurement errors secondary to mRALE severity scoring were expected to be non-differential across race/ethnicity as interpretation of CXRs was blinded to name and race/ethnicity.
Study size
Sample size was based on convenience. A sample size of approximately 140 White/Non-Hispanic patients and 210 Non-White patients would have 96% statistical power assuming a difference in mRALE score of 2 (4 vs 6) with a standard deviation of 5.
Results
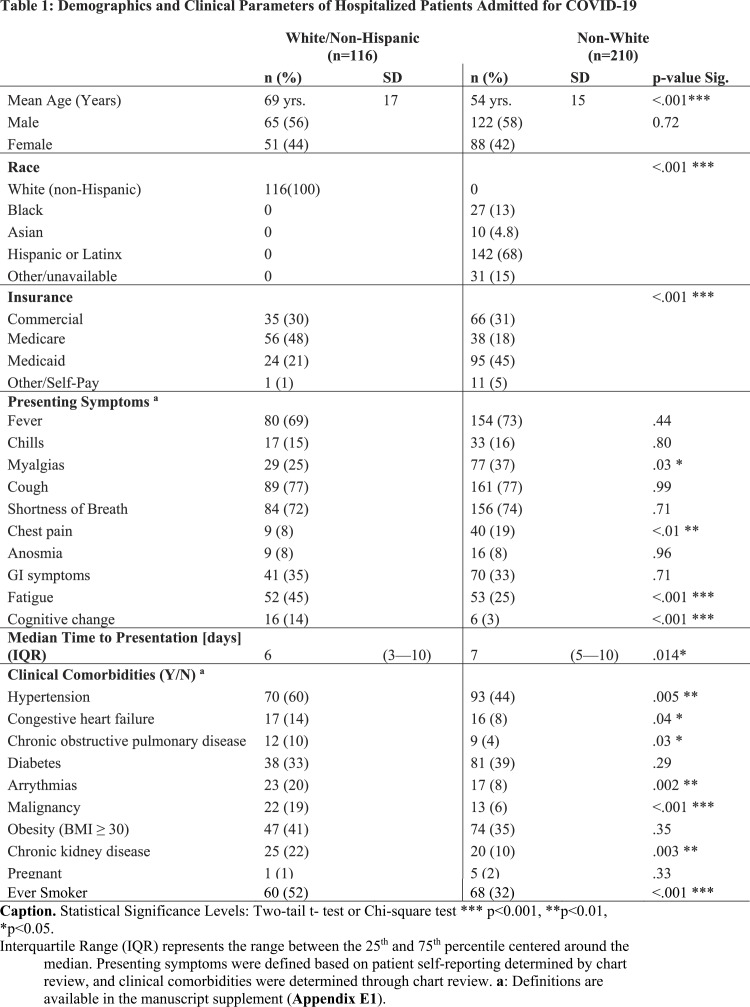
During the study period, 351 hospitalized patients had confirmed COVID-19 infection. Twenty-five (8%) patients initially admitted for other reasons (e.g., trauma) were excluded, representing a final sample size of 326 patients. The mean age of the study cohort was 59 years (SD: 17 yrs.) and the male to female gender distribution was 188:138. Patients with limited English proficiency (LEP) comprised 140 (43%) of the study cohort. Additional patient demographics and clinical presentation among White/Non-Hispanic and Non-White patients are available in Table 1. The largest proportion of admitted patients presented from zip code tabulation areas (ZCTA) with relatively higher proportions of Hispanic individuals, lower median household income, and higher number of persons per room (Figure 3).
Table 1:
Demographics and Clinical Parameters of Hospitalized Patients Admitted for COVID-19
Figure 3.
Title: Geospatial data visualization of admitted patients with COVID-19 infection per zip code and Census-based data by zip code. Figure 3 Caption: A) Number of admitted patients with confirmed COVID-19 infection by zip code, B) Hispanic or Latino Fraction by Population by Zip Code (2018 American Community Survey 5yr Survey) C) Persons-per-room by zip code expressed in percent of individuals living in overcrowded conditions (PPR > 1.01;2018 American Community Survey 5yr Survey), D) Median income by zip code expressed in U.S. Dollars. Majority of patients admitted for COVID-19 infection included in the study cohort were living in home addresses with zip codes with a relatively higher proportion of Hispanic or Latino individuals, higher persons per room and lower median household income.
Primary Outcomes
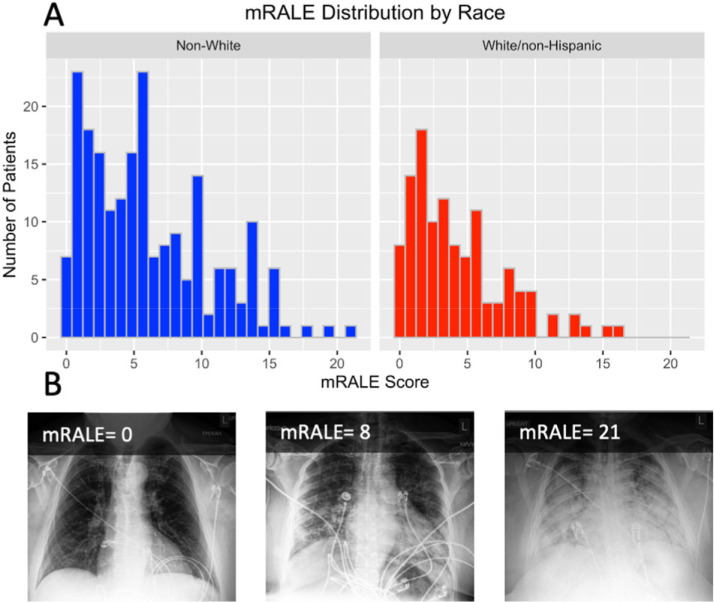
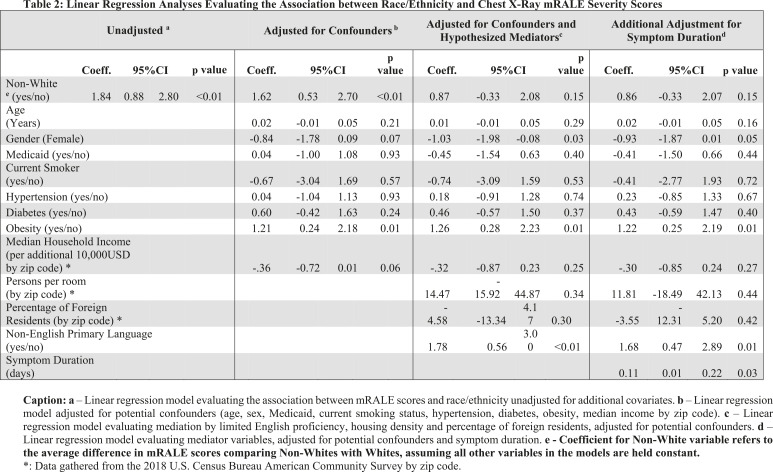
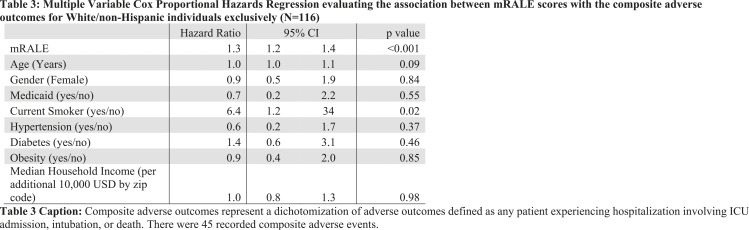
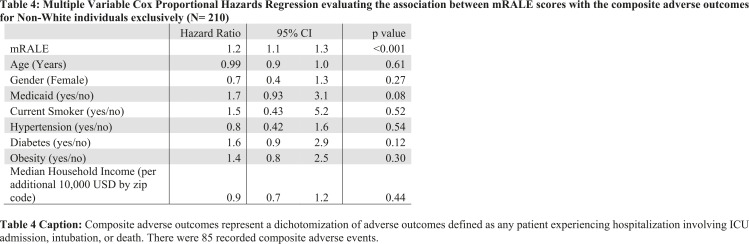
Admission CXRs revealed at least one abnormality in 318 (98%) of the 326 patients included in analysis. Comparison of mRALE scores (Figure 4) revealed that Non-White patients had higher mRALE scores (median 6.1, 95% CI 5.4–6.7) compared with White/Non-Hispanic patients (median 4.2, 95% CI 3.6–4.9) (unadjusted average difference 1.8, 95% CI 0.88–2.8, p<0.01). Multiple variable linear regression analysis (Table 2) demonstrated that Non-White patients presented with higher mRALE scores on admission CXR compared with White/Non-Hispanic patients (adjusted average difference 1.6, 95% CI 0.5–2.7, p=0.005). In adjusted analyses, for White/Non-Hispanic (Hazard Ratio (HR)=1.3, 95% CI 1.2–1.4, p < 0.001) and Non-White patients (HR=1.2, 95% CI 1.1–1.3, p<0.001), increasing mRALE scores were associated with a higher likelihood of experiencing the composite adverse outcome with no evidence of interaction (p = 0.16) (Tables 3 and 4). Additional adjustment for hypothesized mediators revealed that the association between race/ethnicity and severity scores was mediated by LEP (p=0.007), even after controlling for symptom duration prior to admission. Symptom duration was also independently associated with increased severity score (adjusted average increase in score per additional day of symptom duration= 0.11 95% CI 0.01—0.22, p=0.03). Obesity was determined to be independently associated with mRALE score (adjusted average difference comparing obese vs. non-obese patients: 1.2, 95% CI 0.2–2.2, p=0.01). Results from our sensitivity analyses yielded similar results to our primary outcome analyses.
Figure 4.
Title: Histogram of mRALE Score Distribution by Race. A) Distribution of mRALE categories on Admission Chest Radiograph by Race/Ethnicity. Non-White/Hispanic patients were more likely to have higher mRALE score categories compared with White/non-Hispanic patients (Coefficient 0.560, 95% CI 0.046 to 1.074 to, p = 0.033). On average, adjusted for potential confounders, Non-White patients presented with higher mRALE scores on admission CXR compared with White patients (average difference 1.60, 95%CI 0.50 to 2.71, p=0.005) in our multiple variable linear regression analyses (B) Examples of modified Radiograph Assessment of Lung Edema (mRALE) annotations for pulmonary disease severity in patients with COVID-19. The top left inset number for each image is the corresponding mRALE score, the average of annotations by multiple raters. A score of 0-4 was categorized as mild, 4.1-10 was moderate, and >10 was severe.
Table 2:
Linear Regression Analyses Evaluating the Association between Race/Ethnicity and Chest X-Ray mRALE Severity Scores
Table 3:
Multiple Variable Cox Proportional Hazards Regression evaluating the association between mRALE scores with the composite adverse outcomes for White/non-Hispanic individuals exclusively (N=116)
Table 4:
Multiple Variable Cox Proportional Hazards Regression evaluating the association between mRALE scores with the composite adverse outcomes for Non-White individuals exclusively (N= 210)
Secondary clinical outcomes
During the index hospitalization, 243 patients (75%) required supplemental oxygen with nasal cannula or a non-rebreather mask, 119 (34%) were admitted to the ICU, 101 (31%) were intubated (29% of those intubated died), 41 (13%) died overall, and 39 (12%) remain admitted at time of last follow up. Among White/Non-Hispanic patients (n=116), 90 (78%) required supplemental oxygen, 36 (31%) were admitted to the ICU, 29 (25%) were intubated, and 27 (23%) were deceased. Among Non-White patients (n=210), 153 (73%) required supplemental oxygen, 83 (40%) were admitted to the ICU, 72 (34%) were intubated, and 19 (9.1%) were deceased. (Tables 3 and 4).
Discussion
In this single-site retrospective cohort study, we found that racial/ethnic minority patients were more likely to present with increased disease severity from COVID-19 on admission chest radiograph (adjusted average difference 1.6, 95% CI 0.53–2.7, p=0.005. Increasing mRALE severity scores were associated with a higher likelihood of experiencing adverse clinical outcomes for both White/Non-Hispanic (Hazard Ratio (HR)=1.3, 95% CI 1.2–1.4, p < 0.001) and Non-White patients (HR=1.20, 95% CI 1.1–1.3, p<0.001). Increased radiographic severity among Non-White patients was associated with delayed presentation (adjusted average increase in score per additional day of symptom duration: 0.11 95% CI 0.01—0.22, p=0.03) and limited English proficiency (LEP) (adjusted average difference: 1.8 95% CI 0.6—3.0, p<0.01). Identification of racial/ethnic imaging disparities may help radiologists rapidly identify at-risk groups and establish collaborations with other medical specialties and community stakeholders to enhance the effectiveness of public health interventions (e.g., expanded testing) assisting vulnerable populations.
The results of this study are consistent with emerging data that show racial/ethnic minorities have been disproportionately affected by COVID-19.[19,20] The study results show that Non-White patients had significantly greater delays in presentation after onset of symptoms. This could be due to a variety of complex sociodemographic factors that disproportionately affect racial/ethnic minority patients, including employment in low-wage occupations with limited sick-leave and an inability to work remotely, such as in the service industry, living in overcrowded multigenerational households within high population-density metropolitan areas, higher dependence on public transportation, medical mistrust and racial stigma experienced in the health system, among others [5–7,21,22]. These delays in presentation likely result in missing a critical window of early treatment that may be related to the increased disease severity at the time of presentation[23,24]. Additionally, the high incidence of this highly transmissible virus in crowded metropolitan areas, higher prevalence of medical comorbidities associated with worse outcomes, such as obesity, and the association with employment that is incompatible with remote work are factors that place racial/ethnic minority patients at increased risk of infection, more severe clinical presentation, and worse outcomes.[6,25,26]
In addition to these factors, in this study we found that the relationship between race/ethnicity and radiographic severity at presentation was mediated by LEP. In our study, patients with LEP comprised nearly half of the study cohort, which coincided with the peak of the COVID-19 surge, demonstrating a greater proportion than in the surrounding population where at most 24% are reported to have LEP.[27] This likely reflects the characteristics of the surrounding communities near one of our affiliated community health centers, located in a predominantly Hispanic neighborhood. Limited English proficiency is more prevalent among racial/ethnic minority individuals and could be understood as a proxy for sociodemographic minority status and lower health literacy levels.[28,29] Furthermore, LEP can be a barrier to care in the current pandemic due to limitations in availability of multilingual actionable COVID-19 health information that could be contributing to the delayed presentation seen in these patients. Combined with the higher housing density among racial/ethnic minority patients, LEP has been associated with worse clinical outcomes and delays to care, which likely contributed to the association between race/ethnicity and severity scores mediated by LEP and worse outcomes among Non-White patients in the study.[8,30–32] Having multilingual, culturally tailored health information can be particularly important during the current highly infectious COVID-19 pandemic, as this information can be essential to minimizing spread of disease among racial/ethnic minority patients with LEP.
This study suggests that radiology can provide insight to some of the emerging disparities among racial/ethnic minority populations experiencing worse outcomes during the COVID-19 pandemic. The multifactorial combination that interacts in a complex manner and manifests as increased radiographic severity among racial/ethnic minority patients is incompletely captured within the scope of this study. However, the findings of this study could potentially assist radiologists in the development of algorithms to identify emerging disparities among vulnerable populations and rapidly identify at-risk populations. This could also provide radiologists an opportunity to establish collaborations with other medical specialties, community stakeholders, and public health initiatives to enhance the effectiveness of public health interventions that increase access to care, such as access to infectious disease clinics that include imaging and COVID-19 testing, and the development of actionable health information for LEP communities, among others[33,34]. These interventions may improve outcomes during the COVID-19 pandemic through early detection among vulnerable populations.
There are several limitations to this study. First, this study covers a relatively limited period in the scope of an ongoing pandemic, and the testing capacity of health systems and community-based public health interventions continue to rapidly evolve. Second, as a quaternary academic medical center, our patient population may be biased toward more severe disease at the time of presentation. Third, we extracted self-reported demographic data from the medical record that may underreport co-morbidities, demographics, and LEP, among other variables, which may be secondary to racial stigma and mistrust of the healthcare system among racial/ethnic minority populations.[8,21,22] Fourth, census-based zip code data contains aggregate information and may not reflect individual patient living situations and sociodemographic characteristics. Future studies can further elucidate some of these limitations.
Increased disease severity on admission CXRs among Non-White patients hospitalized with confirmed COVID-19 infection may reflect disparities in care due to a multifactorial combination that includes delayed presentation, linguistic barriers, and pre-existing comorbidities Radiographic imaging findings have implications on outcomes in patients; thus, radiology can serve as a means to identify these higher-risk patients and help address emerging disparities. Furthermore, identification of racial/ethnic imaging disparities may help radiologists develop algorithms to rapidly identify at-risk groups and establish collaborations with other medical specialties and community stakeholders to enhance the effectiveness of public health interventions to improve access to care and outcomes among racial/ethnic minority populations during the COVID-19 pandemic.
N.P.J. and N.J.R. contributed equally to the article.
Sources of funding:
No sources of funding were obtained for the preparation of this manuscript.
Institutional Review Board:
This study was approved by the Institutional Review Board, including waiver of patient consent.
Declaration of interests: Dr. Little is an academic author and textbook associate editor for Elsevier, Inc. and receives royalties for his work. Dr. Dugdale reports grants from NIH, personal fees from UNAIDS, other from Infectious Diseases Society of America, outside the submitted work. Dr. Hyle reports grants from NIH, other from UpToDate, outside the submitted work. Dr. Flores reports grants from the NIH and the ACR, outside the submitted work. The remaining authors have nothing to disclose.
Abbreviations:
- mRALE
- modified Radiographic Assessment of Lung Edema
- ICC
- intraclass correlation coefficient
- LEP
- limited English proficiency
- HR
- hazard ratio
References:
- [1].Wadhera RK, Wadhera P, Gaba P, Figueroa JF, Joynt Maddox KE, Yeh RW, et al. Variation in COVID-19 Hospitalizations and Deaths Across New York City Boroughs. JAMA 2020. 10.1001/jama.2020.7197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Webb Hooper M, Nápoles AM, Pérez-Stable EJ. COVID-19 and Racial/Ethnic Disparities. JAMA 2020. 10.1001/jama.2020.8598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Dorn A van, Cooney RE, Sabin ML. COVID-19 exacerbating inequalities in the US. Lancet 2020. 10.1016/s0140-6736(20)30893-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Rocklöv J, Sjödin H. High population densities catalyze the spread of COVID-19. J Travel Med 2020. 10.1093/jtm/taaa038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Bureau of Labor Statistiscs USD of L. No Title. 2018. [Google Scholar]
- [6].Liem A, Wang C, Wariyanti Y, Latkin CA, Hall BJ. The neglected health of international migrant workers in the COVID-19 epidemic. The Lancet Psychiatry 2020. 10.1016/S2215-0366(20)30076-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Harris JR, Huang Y, Hannon PA, Williams B. Low-socioeconomic status workers: Their health risks and how to reach them. J Occup Environ Med 2011. 10.1097/JOM.0b013e3182045f2c. [DOI] [PubMed] [Google Scholar]
- [8].Smedley BD, Stith AY, Nelson AR. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care (with CD). 2003. 10.17226/12875. [DOI] [PubMed]
- [9].Bernheim A, Mei X, Huang M, Yang Y, Fayad ZA, Zhang N, et al. Chest CT findings in coronavirus disease 2019 (COVID-19): Relationship to duration of infection. Radiology 2020. 10.1148/radiol.2020200463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Lang Min. Carey Denston, Reid Nicholas, Mendoza Dexter P., Flores Efren J., Li Matthew D., Shepard Jo-Anne O., Brent P. Little AS. Pulmonary Vascular Manifestations of COVID-19 Pneumonia. Radiol Cardiothorac Imaging 2020;2. 10.1148/ryct.2020200277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Toussie D, Voutsinas N, Finkelstein M, Cedillo MA, Manna S, Maron SZ, et al. Clinical and Chest Radiography Features Determine Patient Outcomes In Young and Middle Age Adults with COVID-19. Radiology 2020. 10.1148/radiol.2020201754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Wong HYF, Lam HYS, Fong AHT, Leung ST, Chin TWY, Lo CSY, et al. Frequency and Distribution of Chest Radiographic Findings in COVID-19 Positive Patients. Radiology 2019. 10.1148/radiol.2020201160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Warren MA, Zhao Z, Koyama T, Bastarache JA, Shaver CM, Semler MW, et al. Severity scoring of lung oedema on the chest radiograph is associated with clinical outcomes in ARDS. Thorax 2018. 10.1136/thoraxjnl-2017-211280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Zimatore C, Pisani L, Lippolis V, Calfee CS, Ware LB, Algera AG, et al. The radiographic assessment of lung edema (RALE) score has excellent diagnostic accuracy for ARDS, 2019. 10.1183/13993003.congress-2019.oa3299. [DOI] [PMC free article] [PubMed]
- [15].Li MD, Arun NT, Gidwani M, Chang K, Deng F, Little BP, et al. Automated assessment of COVID-19 pulmonary disease severity on chest radiographs using convolutional Siamese neural networks. Radiol Artif Intell, 2020, In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Demographic Data for Boston’s Neighborhoods, 1950-2017. Boston, MA: 2017. [Google Scholar]
- [17].Koo TK, Li MY. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J Chiropr Med 2016;15:155–63. 10.1016/j.jcm.2016.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Bureau USC. No Title. Am Community Survery 5 Year Estim 2018.
- [19].Chen JT, Krieger N. Working Paper Series Revealing the unequal burden of COVID-19 by income, race / ethnicity, and household crowding: US county vs. ZIP code analyses 2020;19. [DOI] [PubMed] [Google Scholar]
- [20].Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, et al. Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area. JAMA 2020. 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].De P, Pozen A, Budhwani H. Is Perceived Stigma in Clinical Settings Associated with Poor Health Status among New York City’s Residents of Color? Med Care 2019. 10.1097/MLR.0000000000001205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Stepanikova I, Oates GR. Perceived Discrimination and Privilege in Health Care: The Role of Socioeconomic Status and Race. Am J Prev Med 2017. 10.1016/j.amepre.2016.09.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Beigel JH, Tomashek KM, Dodd LE, Mehta AK, Zingman BS, Kalil AC, et al. Remdesivir for the Treatment of Covid-19 — Preliminary Report. N Engl J Med 2020. 10.1056/nejmoa2007764. [DOI] [PubMed] [Google Scholar]
- [24].Sun Q, Qiu H, Huang M, Yang Y. Lower mortality of COVID-19 by early recognition and intervention: experience from Jiangsu Province. Ann Intensive Care 2020;10:33. 10.1186/s13613-020-00650-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Burgard SA, Lin KY. Bad Jobs, Bad Health? How Work and Working Conditions Contribute to Health Disparities. Am Behav Sci 2013;57:1105–27. 10.1177/0002764213487347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Kluge HHP, Jakab Z, Bartovic J, D’Anna V, Severoni S. Refugee and migrant health in the COVID-19 response. Lancet 2020. 10.1016/S0140-6736(20)30791-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Non-English Speakers for Massachusetts | Data USA n.d. https://datausa.io/profile/geo/massachusetts/demographics/languages (accessed May 10, 2020).
- [28].Kim G, Worley CB, Allen RS, Vinson L, Crowther MR, Parmelee P, et al. Vulnerability of older latino and asian immigrants with limited english proficiency. J Am Geriatr Soc 2011. 10.1111/j.1532-5415.2011.03483.x. [DOI] [PubMed] [Google Scholar]
- [29].Kim J, Ford KL, Kim G. Geographic Disparities in the Relation between English Proficiency and Health Insurance Status among Older Latino and Asian Immigrants. J Cross Cult Gerontol 2019. 10.1007/s10823-019-09366-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Tang AS, Kruger JF, Quan J, Fernandez A. From admission to discharge: Patterns of interpreter use among resident physicians caring for hospitalized patients with limited english proficiency. J Health Care Poor Underserved 2014. 10.1353/hpu.2014.0160. [DOI] [PubMed] [Google Scholar]
- [31].Karliner LS, Pérez-Stable EJ, Gregorich SE. Convenient Access to Professional Interpreters in the Hospital Decreases Readmission Rates and Estimated Hospital Expenditures for Patients with Limited English Proficiency. Med Care 2017. 10.1097/MLR.0000000000000643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Biswas S, Dinh D, Lucas M, Duffy SJ, Brennan A, Liew D, et al. Impact of limited English proficiency on presentation and clinical outcomes of patients undergoing primary percutaneous coronary intervention. Eur Hear J - Qual Care Clin Outcomes 2019. 10.1093/ehjqcco/qcz061. [DOI] [PubMed] [Google Scholar]
- [33].Kucharski AJ, Klepac P, Conlan AJK, Kissler SM, Tang ML, Fry H, et al. Effectiveness of isolation, testing, contact tracing, and physical distancing on reducing transmission of SARS-CoV-2 in different settings: a mathematical modelling study. Lancet Infect Dis 2020;0. 10.1016/S1473-3099(20)30457-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Pan A, Liu L, Wang C, Guo H, Hao X, Wang Q, et al. Association of Public Health Interventions With the Epidemiology of the COVID-19 Outbreak in Wuhan, China. JAMA 2020;323:1915. 10.1001/jama.2020.6130. [DOI] [PMC free article] [PubMed] [Google Scholar]