Abstract
Background: Peripheral 1B tears of the triangular fibrocartilage complex (TFCC) can result in distal radioulnar joint (DRUJ) instability. In the context of associated DRUJ instability, combined evidence supports successful outcomes for peripheral tear repair. Methods: The aim of this systematic review (SR) was to compare the surgical treatment of 1B TFCC tears via arthroscopic versus open methods of repair. The primary outcome measure was restored DRUJ stability. The secondary outcome measures included patient-reported outcomes and clinical outcome measures. An electronic database search of Ovid Embase, PubMed, and the Cochrane Central Register of Controlled Trials was performed to cover a 20-year period. Two authors independently screened records for eligibility and extracted data. Results: Only 3 studies met the strict inclusion criteria, highlighting the poor evidence base for TFCC 1B repairs. Hence, a “secondary analysis” group was developed with modified inclusion criteria which included a further 7 studies for analysis. Pooled data from the primary and secondary analysis groups demonstrated that postoperative DRUJ stability was achieved following open repair in 84% (76/90) of cases and following arthroscopic repair in 86% (129/150) of cases. Conclusions: This SR demonstrates a current lack of high-quality evidence required to draw firm conclusions on the merits of arthroscopic versus open repair of 1B TFCC tears. There is no scientific evidence to suggest superiority of one technique over the other, albeit some surgeons and authors may express a strong personal view.
Keywords: TFCC, 1B tear, DRUJ instability, arthroscopic, open, repair, systematic review
Introduction
Triangular fibrocartilage complex (TFCC) tears are a common cause of ulnar-sided wrist pain.1,2 They were originally described by Palmer3 and categorized into 2 main types. Type 1 lesions are acute traumatic tears, subdivided into 1A to 1D, and usually involve mechanisms of rotational stress with axial load-bearing from falling on an outstretched hand.4 Traumatic type 1 injuries occur more commonly at the periphery. Type 2 lesions are degenerative and central in location with increasing secondary changes.5
Palmer 1A is a central perforation tear to the TFCC disk. 1B, 1C, and 1D tears are classed as “peripheral” tears (Figure 1). 1C tears lead to ulno-carpal instability, whereas 1B and 1D tears lead to instability of the distal radioulnar joint (DRUJ). Palmer 1B tears involve an avulsion of the ulnar foveal attachment of the TFCC, whereas Palmer 1D tears, which are rare,6 involve an avulsion of the radial attachment. In Palmer 1B tears, injury to the distal limb does not itself lead to DRUJ instability; however, disruption to the proximal limb which inserts into the fovea will cause instability.7,8
Figure 1.

Peripheral TFCC tear.
Note. TFCC = triangular fibrocartilage complex.
Reproduced with permission from Elsevier, from Lindau.9
Peripheral tears are amenable to surgical repair1,10 because the peripheral TFCC11 is vascular, as opposed to the central membranous portion.1
In DRUJ instability, the evidence supports successful outcomes for peripheral repair/reattachment.7,12-14 However, the key question of whether arthroscopic techniques are superior to open repair remains unclear.15,16 A further controversy pertaining to the treatment of symptomatic peripheral 1B tears is whether surgical repair is necessary in the context of a stable DRUJ. Several studies support favorable outcomes in this setting,17-20 supported by early papers suturing the detached surface to the peripheral capsule rather than to the fovea.18,21 However, arthroscopic debridement without repair had comparable results to repair in this context.22
The main advantages of arthroscopic repair are superior visualization of the TFCC and proposed improved wrist function by avoiding further injury to surrounding soft tissue structures.23 In general, the arthroscopic techniques used are either described as “inside-out” or “outside-in” depending on how the reattachment is performed.24 The perceived limitation of arthroscopic repair of 1B tears is the inability to anatomically restore the foveal attachment.18,25
The aim of this systematic review (SR) was to compare the surgical treatment of 1B TFCC tears via arthroscopic versus open methods of repair.
Materials and Methods
Literature Search
An electronic database search of Ovid Embase, PubMed, and the Cochrane Central Register of Controlled Trials was performed in April 2017. Studies published between January 1, 1997, and December 31, 2016 were included, covering 20 years of research. The search terms were developed with the help of an information analyst (DG) to include the key concepts of TFCC, DRUJ instability, and ulnar avulsion (Supplementary Material 1).
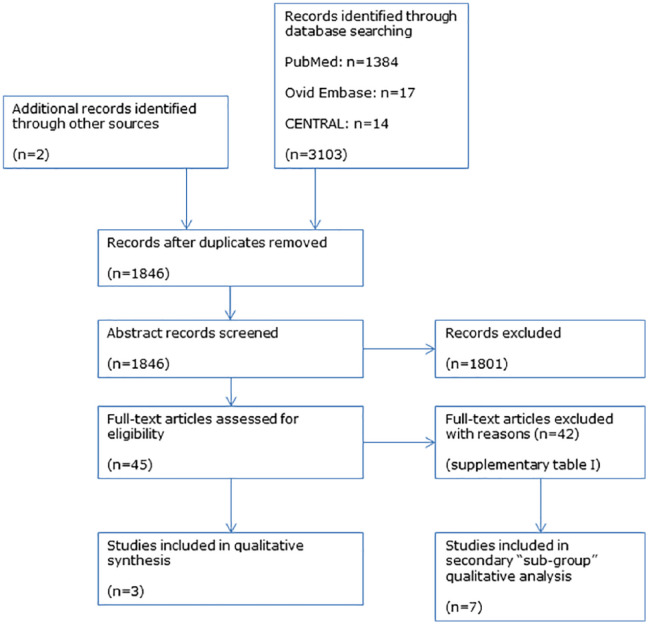
Additional articles were sourced by manually checking reference lists of articles identified via the search. Studies other than in English or Spanish language were excluded. The review protocol is registered on the international prospective register of systematic reviews (PROSPERO; ID: CRD42017033327, available via http://www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42017033327). Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed.26 The selection process is demonstrated in the study PRISMA flowchart (Figure 2).
Figure 2.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flowchart.
Note. CENTRAL = Cochrane Central Register of Controlled Trials.
Inclusion and Exclusion Criteria
The inclusion and exclusion criteria used to assess the full-text articles for eligibility are summarized below.
Inclusion criteria:
Studies of patients with 1B TFCC tears treated via arthroscopic or open surgical repair;
Age 18 to 65 years;
Reporting the preoperative and postoperative DRUJ stability status;
Reporting at least one patient-reported outcome measure (PROM) or clinical outcome measure;
Minimum follow-up of 12 months;
Randomized controlled trials, cohort studies, case-control studies, and case series.
Exclusion criteria:
Central TFCC tears;
Peripheral tears other than type 1B;
Associated injuries;
Studies including surgical procedures in addition to repair of the TFCC;
Studies published prior to January 1, 1997, or after December 31, 2016;
Abstract-only publications;
Case reports, editorials, letters, cadaveric studies, and review articles;
Full-text study reports other than in English or Spanish language.
Outcome Measures
The primary outcome measure was restored stability of the DRUJ at a minimum postoperative follow-up period of 12 months. The secondary outcome measures included patient-reported outcomes and clinical outcome measures. The patient-reported outcomes were the Modified Mayo Wrist Score, the Disabilities of the Arm, Shoulder, and Hand (DASH) score, the Patient-Rated Wrist Evaluation (PRWE) score, and the Visual Analog Score (VAS). Clinical measures reviewed were grip strength, range of movement, and treatment complications.
Data Management and Quality Assessment
Two authors (VR, AF) independently screened records for eligibility and extracted data. Quality assessment of studies was performed using the Joanna Briggs Institute critical appraisal tool checklist for case series studies27 (Supplementary Tables II and III). Disagreements were reviewed by the senior authors (TL, AK).
Results
The results of the search and selection process are presented in a PRISMA flowchart26 (Figure 2).
Three studies fully met all the strict, predefined inclusion criteria for this review.28-30 There were no comparative studies (randomized controlled trials, cohorts, or case controls). The 3 included studies were case series exclusively of arthroscopic results. These studies were entered into the “primary analysis group” (Table 1).
Table 1.
Primary Analysis Group (Demographic Details, Follow-up, and Outcome Measures).
| Open |
Arthroscopic |
|||
|---|---|---|---|---|
| N/A | Kim et al30
(n = 15) |
Iwasaki et al29
(n = 12) |
Bayoumy et al28,a
(n = 37) |
|
| Mean age (range) | 30.5 (19-54) | 31 (20-50) | 23.3 (18-34) | |
| Mean follow-up, mo | 29 | 30 | 24 | |
| Unstable preoperatively, % | 100 (15/15) | 100 (12/12) | 0 (0/37) | |
| Unstable postoperatively, % | 0 (0/15) | 0 (0/12) | N/A | |
| % remaining unstable | 0 | 0 | N/A | |
| DASH: preoperative | 28.4 | 59.5 | 29.9 | |
| DASH: postoperative | 16.6 (P = .06) | 7.7 (P < .0001) | 10.2 (P < .05) | |
| VAS: preoperative | — | 72.1 | 7.6 | |
| VAS: postoperative | — | 10 (P < .0001) | 2.9 (P < .05) | |
| Mayo: preoperative | 64 | Unknown | 62.1 | |
| Mayo: postoperative | 84 (P = .007) | 92.5 | 91.2 (P < .05) | |
| Mayo postoperative results | ||||
| Excellent and Good | n = 12 | n = 12 | — | |
| Fair and Poor | n = 3 | n = 0 | — | |
| Grip strength, % of contralateral | ||||
| Preoperative | 79.3 | 92.7 | 82.5 | |
| Postoperative | 82.9 (P = .086) | 106.3 (P = .003) | 89 | |
| Complications | ||||
| ECU tendinitis | n = 1 | n = 2 | — | |
| DSBUN neurapraxia | — | — | n = 1 | |
| EDM extensor lag | — | — | n = 1 | |
Note. DASH = Disabilities of the Arm, Shoulder, and Hand; VAS = Visual Analog Score; ECU = extensor carpi ulnaris; DSBUN = dorsal sensory branch ulna nerve; EDM = extensor digiti minimi.
1B tears with a stable distal radioulnar joint.
We further identified 5 studies,12, 19,20,31,32 which would have met the inclusion criteria bar the strict age range applied and/or reporting of certain follow-up parameters. Most importantly, these 5 studies report the DRUJ stability status (primary outcome). Therefore, we also present a separate post hoc “secondary analysis group” of studies fulfilling the modified inclusion criteria.
Modified inclusion criteria:
Studies with a mixed age population (age range <18 or >65), if the mean age of participants was within the 18 to 65 range;
Studies where the minimum follow-up for some patients was less than 12 months, provided that the mean study follow-up was at least 12 months.
Two further studies were also entered into the secondary analysis group (Table 2).16,33 Nakamura et al33 did not report PROM or clinical measurement outcomes; however, it was included because it met the modified inclusion criteria and included both arthroscopic and open techniques. The study by Luchetti et al16 was also included, despite having patients with an associated injury or additional interventional procedures, because it is the only published study in which the design was such that a direct comparison of arthroscopic versus open 1B repairs was reported.
Table 2.
Secondary Analysis Group (Demographic Details, Follow-up, and Outcome Measures).
| Open |
Arthroscopic |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Nakamura et al33
(n = 66) |
Luchetti et al16
(n = 24) |
Nakamura et al33
(n = 24) |
Luchetti et al16
(n = 25) |
Woo et al32
(n = 12) |
Jegal et al31
(n = 19) |
Atzei et al12
(n = 48) |
Wysocki et al19,a
(n = 29) 4 lost to F/U |
Yao and Lee20,a
(n = 12) |
|
| Mean follow-up, mo | 36 | 31 | 42 | 31 | 19 | 31 | 33 | 31 | 17.5 |
| Minimum follow-up | 24 | 6 | 12 | 6 | 14 | 18 | 6 | 16 | 11 |
| Mean age (range) | 31 (16-68)b | 32 (13-49) | 27 (16-53)b | 33 (13-69) | 24.7 (17-34) | 37 (16-60) | 34 (17-54) | 30 (13-61) | 42 (19-69) |
| Additional injury/surgery | 0 | 9 DR# | 0 | 16 DR# | 0 | 0 | 0 | 0 | 0 |
| 5 wafers | |||||||||
| Unstable preoperatively, % | 100 (66/66) | 100 (24/24) | 100 (24/24) | 100 (25/25) | 100 (12/12) | 74 (14/19) | 100 (48/48) | 0 (0/29) | 0 (0/12) |
| Unstable postoperatively, % | 15 (10/66) | 17 (4/24) | 29 (7/24) | 4 (1/25) | 58 (7/12) | 11 (2/19) | 8 (4/48) | 0 (0/25) | 0 (0/12) |
| % remaining unstable | 15 (10/66) | 17 (4/24) | 29 (7/24) | 4 (1/25) | 58 (7/12) | 14 (2/14) | 8 (4/48) | 0 (0/25) | 0 (0/12) |
| DASH: preoperative | — | 58 | — | 39 | 48.4 | 44 | 42 | 38 | — |
| DASH: postoperative | — | 36 (P < .001) | — | 18 | 24.6 (P = .005) | 11 | 15 | 9 (P = .003) | 11 (Quick D) |
| VAS (rest): preoperative | — | 2 | — | 2 | 5.3c | — | 3 | 5.4 c | — |
| VAS (rest): postoperative | — | 1 (NS) | — | 1 (NS) | 1.7 (P = .003) | — | 1 | 0.9 (P < .001) | — |
| VAS (active): preoperative | — | 7 | — | 7 | — | — | 8 | — | — |
| VAS (active): postoperative | — | 4 (P < .001) | — | 3 (P < .001) | — | — | 3 | — | — |
| Mayo: preoperative | — | — | — | — | — | — | 48 | — | — |
| Mayo: postoperative | — | — | — | — | — | — | 87 | — | — |
| Excellent and Good | — | — | — | — | — | n = 17 | n = 40 | — | — |
| Fair and Poor | — | — | — | — | — | n = 2 | n = 6 | — | — |
| Grip strength (% of contralateral/kg) | |||||||||
| Preoperative | — | 20 kg | — | 22 kg | 54.90% | 71% | 92.70% | — | — |
| Postoperative | — | 22 kg (NS) | — | 24 kg (NS) | 72.80% | 89% | 103.6% (P < .05) | 35 kg | 64% |
| PRWE: preoperative | — | 69 | — | 54 | 58.7 | 53 | — | — | — |
| PRWE: postoperative | — | 42 (P < .001) | — | 23 (P < .001) | 30.2 (P = .007) | 19 | — | — | 19 |
| Complications | |||||||||
| DSBUN neurapraxia | — | — | — | — | — | — | n = 5 | n = 2 | — |
| Suture knot irritation | — | — | —— | — | — | n = 9 | — | — | — |
| ECU tendinitis | — | — | — | —— | — | — | — | n = 1 | — |
| FCR tendinitis | — | — | — | —— | — | — | — | n = 1 | — |
Note. DR# = distal radius fracture; DASH = Disabilities of the Arm, Shoulder, and Hand; VAS = Visual Analog Score; NS = not significant; PRWE = Patient-Rated Wrist Evaluation; ECU = extensor carpi ulnaris; DSBUN = dorsal sensory branch ulna nerve; EDM = extensor digiti minimi; FCR = flexor carpi radialis.
1B tears with a stable distal radioulnar joint.
Cases aged <18 years were skeletally mature (confirmed with author).
Unclear whether VAS score was done at rest or when active—therefore assumed to be at rest.
A common reason for study exclusion in the primary analysis was that different TFCC tear subtypes were often grouped together in the analysis.14,15,34-38 Several studies were excluded due to ambiguity regarding which of their subjects had associated injuries or concurrent procedures.39-45 However, for one study,33 we were able to contact the senior author to clarify their methodology and include the study in the “secondary analysis group” (Table 2).
Results in the Primary Analysis Group
These 3 studies only included arthroscopic repairs.28-30
The 27 subjects included in Kim et al30 (n = 15) and Iwasaki et al29 (n = 12) had an unstable DRUJ preoperatively. In all 27 cases, DRUJ instability was restored at follow-up (Table 1). In terms of secondary outcome measures, both studies showed an improvement in DASH scores and grip strength postoperatively; however, a statistically significant difference for these outcomes was only reported in the smaller study (n = 12; Iwasaki et al29). The latter also showed a statistically significant improvement postoperatively in VAS scores, from 72.1 to 10 (P < .0001). Kim et al30 demonstrated a significant improvement in Mayo score from 64 to 84 (P = .007), and overall, both studies reported an “excellent” or “good” result in 24 of 27 cases and a “fair” or “poor” result in 3 of 27 cases for the arthroscopic procedure (Table 1).
The third study in the “primary analysis group” (Bayoumy et al28; n = 37) included patients with ulnar-sided wrist pain, which worsened on grasping or ulnar deviation, but without instability of the DRUJ preoperatively. This suggests a distal 1B peripheral tear, not a destabilizing proximal 1B tear.7,8 Hence, the primary outcome measure of regained stability could not be assessed; however, the study showed statistically significant improvements in the secondary outcome measurements—DASH, grip strength, VAS, and Mayo scores postoperatively (Table 1).
Results in the Secondary Analysis Group
Of the 7 studies entered into the “secondary analysis group” (Table 2), 2 studies included nonrandomized comparisons of arthroscopic and open treatment of 1B TFCC tears (Nakamura et al33 [n = 90] and Luchetti et al16 [n = 49]). By combining data from these studies, open repair techniques restored DRUJ stability in 76 (84%) of 90 patients and arthroscopic repair in 41 (84%) of 49 cases. The secondary outcome measures of interest were reported only by Luchetti et al16 with statistically significant improvements in DASH (P < .001), VAS during activity (P < .001), and PRWE (P < .001).
The remaining 5 studies in the “secondary analysis group” (Table 2) were case series of arthroscopic-only repair of 1B tears.12,19,20,31,32Three studies included 74 patients who presented with DRUJ instability preoperatively (Woo et al32 [12/12], Atzei et al12 [48/48], and Jegal et al31 [14/19]). In total, when combined with arthroscopic repairs in the above cohorts (Nakamura et al33 and Luchetti et al16), 102 (83%) of 123 patients regained DRUJ stability. In terms of secondary outcome measures, these authors reported an improvement (Table 2). All patients presented by Wysocki et al19 (n = 29) and Yao and Lee20 (n = 12) had a stable DRUJ preoperatively, which is similar to Bayoumi et al28 (n = 37) in the “primary analysis group,” suggesting a distal 1B tear. There were limited data available on secondary outcome scores for these studies.
Open Versus Arthroscopic Treatment in Relation to Resolving DRUJ Instability
By pooling data from the primary and secondary analysis groups (Table 3), the SR suggests that postoperative stability can be expected following open repair in 84% (76/90) of cases and following arthroscopic repair in 86% (129/150) of cases, ie, comparable results.
Table 3.
Combined Assessment of Cases With DRUJ Instability Preoperatively for Both Primary and Secondary Analysis Groups, Comparing Open and Arthroscopic Treatment.
| Preoperatively (all unstable) | Postoperatively stable | Postoperatively unstable |
|---|---|---|
| Open (n = 90) | 76 (84.4%) | 14 (15.6%) |
| Arthroscopic (n = 150) | 129 (86%) | 21 (14%) |
Complications
Documented complication rates were low and all complications were reported to resolve. The 2 studies which assessed both arthroscopic and open techniques reported no complications at all16,33 (Table 2).
Discussion
The aim of this SR was to assess the merits of arthroscopic repair versus open repair for peripheral 1B tears in the context of DRUJ instability. This SR demonstrates that the current evidence for surgical management of peripheral 1B TFCC tears consists primarily of low-level studies (retrospective case series). Our overall evidence-based conclusion is that both techniques provide similar good outcomes.
The study’s predefined inclusion and exclusion criteria reflect what we felt should be the ideal study population, aiming to eliminate confounding factors such as concomitant injuries and other surgical procedures. An age range between 18 and 65 years covers the working-age population and excludes patients with skeletally immature wrists and older patients where the presence of osteoporosis and coexisting arthritic changes is more likely.46 Also, a minimum follow-up period of 12 months was deemed important to ensure outcomes for each subject were assessed at a reasonable time postoperatively, allowing maximum recovery. Another important strength is that we only included studies that clearly defined whether the TFCC tear had caused instability to the DRUJ. It is essential to know the “stability status” of the DRUJ as instability entails a 1B peripheral tear to the proximal part of the TFCC, making a reattachment to the fovea of the ulnar head necessary,47 as opposed to a stable joint where the distal part is torn and the need for repair remains questionable.22
In accordance with these strict predefined inclusion criteria, only 3 case series of arthroscopic repair techniques were reported in our “primary analysis group,” making any comparison redundant. As described in the methods, we further identified 7 studies that marginally missed the inclusion criteria—our “secondary analysis group.” Most importantly, these 7 studies did report the DRUJ stability status (primary outcome). We felt that not considering these “suboptimal” studies altogether, despite their limitations, would consist of underreporting the existing literature.
The secondary analysis group allowed comparison of arthroscopic and open repair of type 1B peripheral TFCC tears, showing no gross differences in outcomes and complications; most cases regained postoperative stability, irrespective of technique. The complication risk may be weakly in favor of open procedures as they had no reported complications, as opposed to a number of minor transient complications after arthroscopic procedures (Tables 1 and 2). Interestingly, arthroscopic repair of TFCC tears in patients with a stable DRUJ19,20,28 resulted in statistically significant improvements in DASH and VAS scores, suggesting that all type 1B peripheral tears may merit a repair, at least regarding pain relief and overall function. However these results must be interpreted with great caution, due to the biases introduced by any nonrandomized comparison (primarily selection bias) and the poor methodological quality of the studies.
The main limitation of this study was the lack of good-quality comparative studies of open repair to arthroscopic procedures. Many TFCC lesions reported in the literature are associated with distal radius fractures. These fractures have an impact on wrist function per se, whether or not they require operative fixation.48 We identified several weaknesses of the included studies, which limit the reliability of their results (Supplementary Tables II and III): the methodology, in particular the inclusion criteria, was not always clear; the majority did not clarify whether consecutive inclusion of participants occurred, which may have led to selection bias. Furthermore, a variety of differing techniques of assessing DRUJ stability were described across studies: each study implemented one or more clinical tests combined with, in some studies, an arthroscopic assessment of instability features. Although accepted as current practice, this lack of a clear and standardized assessment of stability status is a major limitation in pooling results. Furthermore, an array of different repair techniques was described by the authors under “umbrella terms” of open or arthroscopic repair.
Conclusions
This SR demonstrates current lack of the high-quality evidence required to draw firm conclusions on the merits of arthroscopic versus open repair of 1B TFCC tears with DRUJ instability preoperatively. This is not only due to the design and methodological flaws of existing studies but also due to the fact that type 1B tears are a difficult condition to research in isolation, as they often present with associated injuries that may require concurrent surgical procedures.
The available evidence suggests that both open and arthroscopic methods of repair adequately address DRUJ instability in most of the cases (over 80%), with similar rates of persisting instability. Secondary outcome measures were also seen to improve for both techniques. In cases with no preoperative DRUJ instability, where the need for repair is controversial,22 secondary outcome scores also improved postoperatively.
It is brutally obvious, based on this SR, that we have to improve our evidence-based knowledge by setting up prospective, preferably randomized studies, where there is no bias from the researchers/surgeons in the study design. It is well known that keen “wrist arthroscopists” are mostly in favor of an arthroscopically assisted approach as opposed to “anatomists” who with excellent dissection will favor an open approach. There are obvious advantages and disadvantages with both techniques, but it is reassuring that the current literature supports the surgeon to use any of the 2 options as outcome, and complications will be very similar.
Supplemental Material
Supplemental material, Supplementary_material for Open Versus Arthroscopic Repair of 1B Ulnar-Sided Triangular Fibrocartilage Complex Tears: A Systematic Review by Vanessa Robba, Andrew Fowler, Alexia Karantana, Douglas Grindlay and Tommy Lindau in HAND
Footnotes
Supplemental material is available in the online version of the article.
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: The above work is a systematic review of literature and we did not carry out experiments on human or animal subjects.
Statement of Informed Consent: We confirm there to be no identifying information about participants in the article.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Andrew Fowler  https://orcid.org/0000-0002-6026-9496
https://orcid.org/0000-0002-6026-9496
Alexia Karantana  https://orcid.org/0000-0003-3742-5646
https://orcid.org/0000-0003-3742-5646
References
- 1. Ahn AK, Chang D, Plate AM. Triangular fibrocartilage complex tears: a review. Bull NYU Hosp Jt Dis. 2006;64:114-118. [PubMed] [Google Scholar]
- 2. Read J. Ulnar-sided wrist pain is not the only cause of TFCC injury: a clinical perspective on other diagnoses in the sport setting. Br J Sports Med. 2013;47:1061-1062. [DOI] [PubMed] [Google Scholar]
- 3. Palmer AK. Triangular fibrocartilage complex lesions: a classification. J Hand Surg Am. 1989;14:594-606. [DOI] [PubMed] [Google Scholar]
- 4. Rettig AC. Athletic injuries of the wrist and hand part I: traumatic injuries of the wrist. Am J Sports Med. 2003;31:1038-1048. [DOI] [PubMed] [Google Scholar]
- 5. Sachar K. Ulnar-sided wrist pain: evaluation and treatment of triangular fibrocartilage complex tears, ulnocarpal impaction syndrome, and lunotriquetral ligament tears. J Hand Surg Am. 2008;33:1669-1679. [DOI] [PubMed] [Google Scholar]
- 6. Dalal S, Murali SR. The distal radio-ulnar joint. Orthop Trauma. 2012;26:44-52. [Google Scholar]
- 7. Atzei A. New trends in arthroscopic management of type 1-B TFCC injuries with DRUJ instability. J Hand Surg Eur Vol. 2009;34:582-591. [DOI] [PubMed] [Google Scholar]
- 8. Skalski MR, White EA, Patel DB, et al. The traumatized TFCC: an illustrated review of the anatomy and injury patterns of the triangular fibrocartilage complex. Curr Probl Diagn Radiol. 2016;45:39-50. [DOI] [PubMed] [Google Scholar]
- 9. Lindau T. Arthroscopic evaluation of associated soft tissue injuries in distal radius fractures. Hand Clin. 2017;33:651-658. [DOI] [PubMed] [Google Scholar]
- 10. Nagle DJ. Triangular fibrocartilage complex tears in the athlete. Clin Sports Med. 2001;20:155-166. [DOI] [PubMed] [Google Scholar]
- 11. Bednar MS, Arnoczky SP, Weiland AJ. The microvasculature of the triangular fibrocartilage complex: its clinical significance. J Hand Surg Am. 1991;16:1101-1105. [DOI] [PubMed] [Google Scholar]
- 12. Atzei A, Luchetti R, Braidotti F. Arthroscopic foveal repair of the triangular fibrocartilage complex. J Wrist Surg. 2015;4:22-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Corso SJ, Savoie FH, Geissler WB, et al. Arthroscopic repair of peripheral avulsions of the triangular fibrocartilage complex of the wrist: a multicenter study. Arthroscopy. 1997;13:78-84. [DOI] [PubMed] [Google Scholar]
- 14. Shih JT, Lee HM, Tan CM. Early isolated triangular fibrocartilage complex tears: management by arthroscopic repair. J Trauma. 2002;53:922-927. [DOI] [PubMed] [Google Scholar]
- 15. Anderson ML, Larson AN, Moran SL, et al. Clinical comparison of arthroscopic versus open repair of triangular fibrocartilage complex tears. J Hand Surg Am. 2008;33:675-682. [DOI] [PubMed] [Google Scholar]
- 16. Luchetti R, Atzei A, Cozzolino R, et al. Comparison between open and arthroscopic-assisted foveal triangular fibrocartilage complex repair for post-traumatic distal radio-ulnar joint instability. J Hand Surg Eur Vol. 2014;39:845-855. [DOI] [PubMed] [Google Scholar]
- 17. Reiter A, Wolf MB, Schmid U, et al. Arthroscopic repair of Palmer 1B triangular fibrocartilage complex tears. Arthroscopy. 2008;24:1244-1250. [DOI] [PubMed] [Google Scholar]
- 18. Trumble TE, Gilbert M, Vedder N. Arthroscopic repair of the triangular fibrocartilage complex. Arthroscopy. 1996;12:588-597. [DOI] [PubMed] [Google Scholar]
- 19. Wysocki RW, Richard MJ, Crowe MM, et al. Arthroscopic treatment of peripheral triangular fibrocartilage complex tears with the deep fibers intact. J Hand Surg Am. 2012;37:509-516. [DOI] [PubMed] [Google Scholar]
- 20. Yao J, Lee AT. All-arthroscopic repair of Palmer 1B triangular fibrocartilage complex tears using the FasT-Fix device. J Hand Surg Am. 2011;36:836-842. [DOI] [PubMed] [Google Scholar]
- 21. Haugstvedt JR, Husby T. Results of repair of peripheral tears in the triangular fibrocartilage complex using an arthroscopic suture technique. Scand J Plast Reconstr Surg Hand Surg. 1999;33:439-447. [DOI] [PubMed] [Google Scholar]
- 22. Cardenas-Montemayor E, Hartl JF, Wolf MB, et al. Subjective and objective results of arthroscopic debridement of ulnar-sided TFCC (Palmer type 1B) lesions with stable distal radio-ulnar joint. Arch Orthop Trauma Surg. 2013;133:287-293. [DOI] [PubMed] [Google Scholar]
- 23. Bednar JM, Osterman AL. The role of arthroscopy in the treatment of traumatic triangular fibrocartilage injuries. Hand Clin. 1994;10:605-614. [PubMed] [Google Scholar]
- 24. Cober SR, Trumble TE. Arthroscopic repair of triangular fibrocartilage injuries. Orthop Clin North Am. 2001;32:279-294. [DOI] [PubMed] [Google Scholar]
- 25. Sagerman SD, Short W. Arthroscopic repair of radial-sided triangular fibrocartilage complex tears. Arthroscopy. 1996;12:339-342. [DOI] [PubMed] [Google Scholar]
- 26. Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Moola S, Munn Z, Tufanaru C, et al. Chapter 7: systematic reviews of etiology and risk. In: Aromataris E, Munn Z, eds. Joanna Briggs Institute Reviewer’s Manual. The Joanna Briggs Institute; 2017. https://reviewersmanual.joannabriggs.org. Accessed December 12, 2018. [Google Scholar]
- 28. Bayoumy M, Elkady HA, Said HG, et al. Short-term evaluation of arthroscopic outside-in repair of Type 1B TFCC tear with vertical mattress suture. Int J Multidiscip Res Dev. 2015;2:679-683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Iwasaki N, Nishida K, Motomiya M, et al. Arthroscopic-assisted repair of avulsed triangular fibrocartilage complex to the fovea of the ulnar head: a 2- to 4-year follow-up study. Arthroscopy. 2011;10:1371-1378. [DOI] [PubMed] [Google Scholar]
- 30. Kim B, Yoon HK, Nho JH, et al. Arthroscopically assisted reconstruction of triangular fibrocartilage complex foveal avulsion in the ulnar variance-positive patient. Arthroscopy. 2013;29:1762-1768. [DOI] [PubMed] [Google Scholar]
- 31. Jegal M, Heo K, Kim JP. Arthroscopic trans-osseous suture of peripheral triangular fibrocartilage complex tear. J Hand Surg Asian Pac Vol. 2016;21:300-306. [DOI] [PubMed] [Google Scholar]
- 32. Woo SJ, Jegal M, Park MJ. Arthroscopic-assisted repair of triangular fibrocartilage complex foveal avulsion in distal radioulnar joint injury. Indian J Orthop. 2016;50:263-268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Nakamura T, Sato K, Okazaki M, et al. Repair of foveal detachment of the triangular fibrocartilage complex: open and arthroscopic transosseous techniques. Hand Clin. 2011;27:281-290. [DOI] [PubMed] [Google Scholar]
- 34. Buterbaugh GA, Brown TR, Horn PC. Ulnar-sided wrist pain in athletes. Clin Sports Med. 1998;17:567-583. [DOI] [PubMed] [Google Scholar]
- 35. Estrella EP, Hung LK, Ho PC, et al. Arthroscopic repair of triangular fibrocartilage complex tears. Arthroscopy. 2007;23:7729-7737. [DOI] [PubMed] [Google Scholar]
- 36. Park MJ, Jagadish A, Yao J. The rate of triangular fibrocartilage injuries requiring surgical intervention. Orthopedics. 2010;33:806. [DOI] [PubMed] [Google Scholar]
- 37. Ruch DS, Papadonikolakis A. Arthroscopically assisted repair of peripheral triangular fibrocartilage complex tears: factors affecting outcome. Arthroscopy. 2005;21:1126-1130. [DOI] [PubMed] [Google Scholar]
- 38. Tang CY, Fung B, Rebecca C, et al. Another light in the dark: review of a new method for the arthroscopic repair of triangular fibrocartilage complex. J Hand Surg Am. 2012;37:1263-1268. [DOI] [PubMed] [Google Scholar]
- 39. McAdams TR, Swan J, Yao J. Arthroscopic treatment of triangular fibrocartilage wrist injuries in the athlete. Am J Sports Med. 2009;37:2291-2297. [DOI] [PubMed] [Google Scholar]
- 40. Moritomo H, Masatomi T, Murase T, et al. Open repair of foveal avulsion of the triangular fibrocartilage complex and comparison by types of injury mechanism. J Hand Surg Am. 2010;35:1955-1963. [DOI] [PubMed] [Google Scholar]
- 41. Moritomo H. Open repair of the triangular fibrocartilage complex from palmar aspect. J Wrist Surg. 2015;4:2-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Shinohara T, Tatebe M, Okui N, et al. Arthroscopically assisted repair of triangular fibrocartilage complex foveal tears. J Hand Surg Am. 2013;38:271-277. [DOI] [PubMed] [Google Scholar]
- 43. Trumble TE, Gilbert M, Vedder N. Isolated tears of the triangular fibrocartilage: management by early arthroscopic repair. J Hand Surg Am. 1997;22:57-65. [DOI] [PubMed] [Google Scholar]
- 44. Wolf MB, Kroeber MW, Reiter A, et al. Ulnar shortening after TFCC suture repair of Palmer type 1B lesions. Arch Orthop Trauma Surg. 2010;130:301-306. [DOI] [PubMed] [Google Scholar]
- 45. Wolf MB, Haas A, Dragu A, et al. Arthroscopic repair of ulnar-sided triangular fibrocartilage complex (Palmer Type 1B) tears: a comparison between short-and midterm results. J Hand Surg Am. 2012;37:2325-2330. [DOI] [PubMed] [Google Scholar]
- 46. Banks LN, Lindau TR. Epidemiology of osteoarthritis of the hand and wrist. OA Musculoskeletal Med. 2013;1:23. [Google Scholar]
- 47. Atzei A, Luchetti R. Foveal TFCC tear classification and treatment. Hand Clin. 2011;27:263-272. [DOI] [PubMed] [Google Scholar]
- 48. Gliatis JD, Plessas SJ, Davis TRC. Outcome of distal radial fractures in young adults. J Hand Surg Br. 2000;25:535-543. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Supplementary_material for Open Versus Arthroscopic Repair of 1B Ulnar-Sided Triangular Fibrocartilage Complex Tears: A Systematic Review by Vanessa Robba, Andrew Fowler, Alexia Karantana, Douglas Grindlay and Tommy Lindau in HAND