Abstract
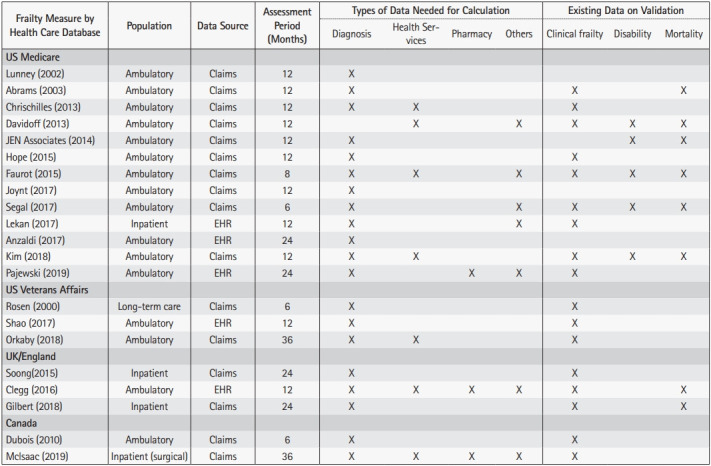
Considering the increasing burden and serious consequences of frailty in aging populations, there is increasing interest in measuring frailty in health care databases for clinical care and research. This review synthesizes the latest research on the development and application of 21 frailty measures for health care databases. Frailty measures varied widely in terms of target population (16 ambulatory, 1 long-term care, and 4 inpatient), data source (16 claims-based and 5 electronic health records [EHR]-based measures), assessment period (6 months to 36 months), data types (diagnosis codes required for 17 measures, health service codes for 7 measures, pharmacy data for 4 measures, and other information for 9 measures), and outcomes for validation (clinical frailty for 7 measures, disability for 7 measures, and mortality for 16 measures). These frailty measures may be useful to facilitate frailty screening in clinical care and quantify frailty for large database research in which clinical assessment is not feasible.
Keywords: Frailty, Healthcare administrative claims, Electronic health records
INTRODUCTION
Frailty is a clinical state resulting from age-related changes in multiple physiologic systems and accumulation of diseases that reduces patient ability to maintain homeostasis in response to stressors.1) Frailty is common in older adults, affecting one in every 10 community-dwellers2,3) and one in every two nursing home residents,4) and is associated with increased risks of death (relative risk [RR], 1.6–6.0), disability (RR, 1.8–2.8), institutionalization (RR, 2.6–24.0), and falls (RR, 1.2–2.4).1) Health care costs for older adults with frailty increase by up to 2-fold compared to those in their non-frail counterparts,5,6) mainly due to inpatient care, post-acute care, and care for potentially preventable conditions.7,8) Given the considerable clinical and societal consequences of frailty in the ever-growing aging population, assessment of frailty in clinical and population settings offers valuable opportunities for prevention and treatment through efficient use of evidence-based interventions and resources.9-11)
Several validated tools are available to measure frailty,12-15) which can be selected based on the purpose (screening, diagnosis, or monitoring response to interventions), setting (emergency department, inpatient, outpatient, or public health), and available resources (trained staff to perform self-report vs. objective assessment).16) Although simple clinical assessment tools17-19) and online calculators are available,20) frailty assessment typically requires clinical assessment in the form of a survey21-23) or objective assessments of physical performance24-27) conducted by a clinician (e.g., geriatrician) or trained health care professional. However, routine adoption of the frailty concept for clinical care or public health practice is variably slow across health systems in different countries,11) in part due to a lack of time and resources for assessment.28,29) To overcome these barriers, there is a growing interest in the measurement of frailty using ubiquitous health care databases such as administrative claims data and electronic health records (EHRs), which are by-products of health care encounters and transactions between health care providers and health plans. Administrative claims data contain diagnosis codes, health service codes, and prescription drug data obtained from a large population of health plan members but lack detailed clinical information such as vital signs, physical examination findings, and diagnostic test results. In contrast, EHR provide clinical information not available in administrative claims data; however, much of the information is unstructured (e.g., narrative clinical notes) and may be discontinuous due to patients receiving care at multiple health systems using different EHR systems.30) Nonetheless, frailty scores derived from health care databases (“database-derived frailty measures”) hold promise for population-level frailty screening as well as health services and outcomes research in frail older adults who are under-represented in clinical trials.31)
This review summarizes the latest advances in frailty measurement in health care databases, mainly administrative claims data and EHR, as well as the potential applications for clinical care and research. Frailty measures requiring in-person surveys or evaluations are beyond the scope of this review. The outline is as follows: (1) literature search; (2) general approaches to frailty measurement in health care data; (3) frailty measurement in administrative claims data; (4) frailty measurement in EHR; (5) considerations in developing a database-derived frailty measure; (6) potential applications of database-derived frailty measures; (7) areas of uncertainty; and (8) conclusions.
LITERATURE SEARCH
A literature search was conducted in PubMed using the Medical Subject Headings, “frailty” AND (“administrative claims, healthcare” OR “electronic health records” OR “Medicare”), and their variations in the title field. Additional filters were applied, including publication date, January 1, 2001, to December 31, 2019, and “aged, 65+ years”. This search yielded 50 articles. Risk scores derived from health care databases that aimed to predict mortality or hospitalization were not considered as frailty measures, although they may also be correlated with frailty.32,33) From the search results, 10 reviews or commentaries; 9 articles using frailty measures not derived from health care databases; and 8 articles not reporting development, validation, or application of database-derived frailty measures were excluded. The initial search was supplemented by an additional 29 articles from the references of the included articles. Finally, 52 articles informed this review.
GENERAL APPROACHES TO FRAILTY MEASUREMENT IN HEALTH CARE DATA
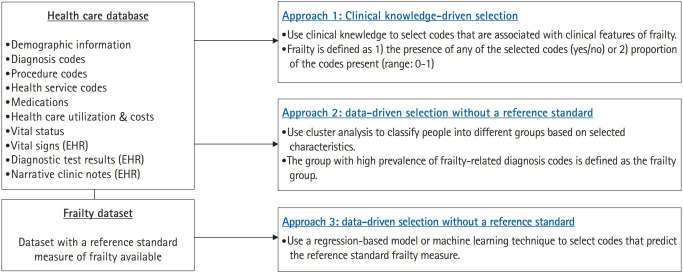
Health care databases generated primarily for health care service administration, care quality assessment, and clinical care delivery generally do not contain sufficient information to derive clinically validated measures of frailty.12-15) Therefore, frailty measures24-27) requiring clinical assessment (e.g., gait speed, grip strength, physical activity, or cognitive function) cannot be directly calculated. In the absence of sufficient clinical information, researchers attempted to measure frailty using demographic information, diagnosis codes, or health service codes available in health care databases. The approach to developing a frailty measure depended on the availability of a dataset containing a reference standard measure of frailty and methods to select diagnosis and health service codes in health care databases (Fig. 1).
Fig. 1.
Approaches to developing a frailty measure in health care databases. The literature applied three general approaches to develop a frailty measure for health care databases. When a dataset containing information on a reference standard measure of frailty was not available, frailty was measured using diagnosis and health service codes selected based on clinical knowledge (approach 1) or cluster analysis using diagnosis codes, hospital days, and total costs (approach 2). When a dataset with a reference standard measure of frailty was available, a variable selection method (e.g., penalized regression or machine learning technique) was used to select diagnosis and health service codes to measure frailty (approach 3). EHR, electronic health records.
Clinical Knowledge-Driven Selection
Health care providers and researchers with expertise in aging and frailty select diagnosis codes or health service codes based on prior research and clinical knowledge. These codes may include diseases (e.g., pressure ulcer, failure to thrive, or history of falls), symptoms or signs (e.g., fatigue, muscle weakness, abnormality of gait), and health services (e.g., hospital beds, walking aids, or transportation services) commonly reported or used by older adults with frailty.31) Frailty has been defined as the presence of any code within a pre-specified period (e.g., 12 months), while its absence assumes that the condition does not exist. This approach is straightforward and does not require a dataset containing a reference standard measure of frailty. It generally offers high specificity and low sensitivity but underestimates frailty prevalence. Alternatively, researchers have quantified frailty by counting the number of different codes in a pre-specified period and deriving a deficit-accumulation frailty index34) using these codes as health deficits. For example, a person with 10 of 40 pre-specified codes within a 12-month period is assigned a frailty index of 0.25 (=10/40). The deficit-accumulation approach allows measurement of severity rather than all-or-none classification and choice of a threshold to achieve high sensitivity or high specificity depending on the purpose. Notably, a deficit-accumulation frailty index calculated mainly from diagnosis codes seems to have a narrower range of values (99th percentile 0.4–0.5)35) than that for a frailty index calculated from clinical assessment (99th percentile 0.6–0.7).36)
Data-Driven Selection without a Reference Standard
When a dataset with a reference standard frailty measure is not available, researchers have tried to define frail individuals in the dataset by cluster analysis.37) Cluster analysis is an unsupervised learning technique that classifies individuals into groups of similar nature in terms of measured characteristics in the dataset such as diagnosis codes, hospital days, and total costs during a pre-specified period. After examining the characteristics of the groups derived from cluster analysis, one of the groups (i.e., the group with a high number of diagnoses indicative of frailty) can be designated as the frailty group. However, cluster analysis can be computing-intensive for large datasets and may not yield the same grouping in different datasets. Gilbert et al.37) tried to overcome this limitation by conducting cluster analysis in a subset of a large hospital administrative dataset and developing a logistic regression model to predict frailty group membership based on diagnosis codes. The predicted probability from this logistic model can be used to assign individuals to the frailty group from the entire dataset. While this approach identifies frail individuals without requiring a dataset with a reference standard frailty measure, determining the number of groups in the cluster analysis and designating a single frailty group may be subject to interpretation. Moreover, frail individuals may not be classified exclusively into a single group (e.g., frail people with cancer and frail people with heart disease may be classified into different groups despite similar levels of frailty).38)
Data-Driven Selection with a Reference Standard
If a population-based dataset exists that contains information on a reference standard frailty measure (e.g., frailty phenotype or deficit-accumulation frailty index) and administrative claims data, specific codes can be selected against the reference frailty measure (also known as supervised learning). Several variable selection algorithms have been applied—e.g., stepwise regression,39,40) penalized regression,39,41) or tree-based algorithms.39) More flexible “black-box” machine learning algorithms such as random forest and gradient boosting, provide limited or marginal advantages over regression-based algorithms in predictive performance.39) Under this approach, the first step is variable selection and estimation of weights (in regression models) to optimize predictive performance against a reference standard measure of frailty in a training dataset. The model derived from the training dataset is evaluated in a hold-out testing dataset or via cross-validation. This method can select codes that are positively (e.g., degenerative disease of the central nervous system) or negatively (e.g., vaccination) associated with frailty. It provides better predictive performance of frailty and adverse health outcomes than counting the number of codes or calculating a deficit-accumulation frailty index directly from the codes.41)
FRAILTY MEASUREMENT IN ADMINISTRATIVE CLAIMS DATA
Table 1 summarizes 16 frailty measures for administrative claims data. Of these, 12 measures were developed for the United States Medicare8,39-48) or Veterans Affairs49,50) claims databases, including two proprietary measures; namely, the Johns Hopkins Adjusted Clinical Groups Frailty Indicators43) and JEN-Frailty Index,45,46) two were developed for the Canadian claims databases,51,52) and two were developed for the United Kingdom hospital claims database.37,53) Database-derived frailty measures varied widely in terms of development approaches (clinical knowledge in nine measures, cluster analysis in one measure, and reference standard measures in six measures), number of variables included (nine to 109 variables), target populations (general vs. specific disease populations), and validation outcomes (clinical frailty assessment, functional status, mortality, health care utilization, or costs). Only seven of 16 measures have been compared against a clinical frailty assessment37,54-59) and seven measures have been tested for disability50,52,56,57,60) or nursing home admission.45,52,57,60)
Table 1.
Frailty measures for administrative claims data
| Author (y) | Database/population (study year) | Outcomes | Predictors | ||
|---|---|---|---|---|---|
| Development | Validation | ||||
| Clinical knowledge-driven selection | Lunney et al.42) (2002) | Medicare database (USA)42) | Not applicable | None | Presence (yes/no) of any of 11 conditions based on ICD diagnosis codes |
| - Medicare 0.1% sample (1993–1998)42) | |||||
| Abrams et al.43) (2003) | Medicare database (USA) | Not applicable | Vulnerable Elders Survey | Presence (yes/no) of any of 10 conditions based on ICD diagnosis codes (Johns Hopkins Adjusted Clinical Groups) | |
| - HMO in Israel (2008)54) | Mortality | ||||
| - Major non-cardiac surgery, emergency general surgery, orthopedic surgery patients in Canada (2002–2014)80-83) | Complications | ||||
| Discharge disposition | |||||
| Costs | |||||
| Chrischilles et al.44) (2014) | Medicare database (USA) | Not applicable | Mortality | Presence (yes/no) of any or ≥2 of 16 conditions based on ICD diagnosis and HCPCS codes | |
| - Acute MI patients (2007–2008)44) | Cardiac catheterization | ||||
| - Kidney cancer patients (2000–2009)84) | Complications | ||||
| Costs | |||||
| JEN Associates45,46) (2008) | Medicare database (USA)45,86) | Not applicable | Mortality | Count of the number of 13 conditions present based on ICD diagnosis codes (JEN-Frailty Index) | |
| - Spouses of AD patients (2001–2005)85) | NH admission | ||||
| - National Long-Term Care Survey (2004)60) | Costs | ||||
| - Medicare 5% sample (2011–2014) | Disability | ||||
| Hope et al.47) (2015) | Medicare database (USA) | Not applicable | Mortality | Presence (yes/no) of nursing facility claims or 11 conditions based on ICD diagnosis codes | |
| - ICU patients (2004–2008)47) | |||||
| Soong et al.53,87) (2015) | Inpatient claims database, England | Not applicable | Mortality | Presence (yes/no) of any of 9 conditions based on ICD diagnosis codes | |
| - HES database (2005–2013)53,87) | Discharge disposition | ||||
| Readmission | |||||
| Medicare database (USA) | Not applicable | Costs | Presence (yes/no) of ≥2 of 12 conditions based on ICD diagnosis codes and HCPCS codes (specified by Kim and Schneeweiss)31) | ||
| Joynt et al.8) (2017) | - Medicare 20% sample (2011–2012)7,8) | ||||
| Orkaby et al.49) (2018) | VA claims database (USA) | Not applicable | Mortality | Proportion of 31 health deficits present based on ICD diagnosis, CPT, and HCPCS codes | |
| - National sample (2002–2012)49) | |||||
| McIsaac et al.51) (2019) | Administrative claims database (Canada) | Not applicable | Mortality | Proportion of 30 health deficits present based on ICD diagnosis codes, drugs, assistive device codes, and living environment (preoperative Frailty Index) | |
| - Major non-cardiac surgery (2002–2015)51,88 | Discharge disposition | ||||
| Data-driven selection without a reference standard | Gilbert et al.37) (2018) | Inpatient claims database, England | Frailty cluster (from cluster analysis) | Mortality | Includes 109 ICD diagnosis variables |
| - HES database (2005–2013)37) | Prolonged hospitalization | ||||
| - Hospital cohorts37) | Readmission | ||||
| Frailty phenotype | |||||
| Deficit-accumulation FI | |||||
| Data-driven selection with a reference standard | Rosen et al.50) (2000) | VA claims database (USA) | Disability | Disability | Includes 13 conditions based on ICD diagnosis codes |
| - Long-term care (1996–1997)50,89) | |||||
| Dubois et al.52) (2010) | Prescription claims database (Canada) | Functional status score | Mortality | Includes 11 prescription drug categories | |
| - PRISMA cohort (2001–2005)52 | Disability | ||||
| Hospitalization | |||||
| NH admission | |||||
| Davidoff et al.40) (2013) | Medicare database (USA) | Disability | Mortality | Includes sex, Medicaid enrollment, number of office visits, 8 health care visit types, 3 health care services, 9 procedures, 6 DMEs, and 2 imaging tests based on CPT and HCPCS codes, and geographical regions | |
| - MCBS cohort (2001–2005)40) | Disability | ||||
| - HRS cohort (2008-2010)56) | Frailty phenotype | ||||
| - SEER-Medicare cohort (1999–2007)90,91) | Deficit-accumulation FI | ||||
| Faurot et al.48) (2015) | Medicare database (USA) | Disability | Mortality | Includes age, sex, race, and 23 conditions based on ICD diagnosis, CPT, or HCPCS codes | |
| - MCBS cohort (2006)48) | Disability | ||||
| - Medicare beneficiaries with or without influenza vaccination (2007–2008)62) | Falls | ||||
| - ARIC cohort (2011–2013)58) | Mobility impairment | ||||
| - MarketScan Medicare (2013)63) | Frailty phenotype | ||||
| - HRS cohort (2008-2010)56) | Deficit-accumulation FI | ||||
| Costs | |||||
| Segal et al.39,55) (2017) | Medicare database (USA) | Frailty phenotype | Mortality | Includes age, sex, race, Charlson Comorbidity Index, past hospitalization, and 16 conditions based on ICD diagnosis codes | |
| - CHS cohort (1992–1993/1997)39) | Disability | ||||
| - NHATS cohort (2000)55) | Hospitalization | ||||
| - Medicare TAVR cohort (2011–2015)64) | Fracture | ||||
| - HRS cohort (2008-2010)56) | NH admission | ||||
| Frailty phenotype | |||||
| Deficit-accumulation FI | |||||
| Kim et al.41) (2018) | Medicare database (USA) | Deficit-accumulation FI | Mortality | Includes 52 ICD diagnosis variables, 25 CPT variables, and 16 HCPCS variables | |
| - MCBS cohort (2006–2007/2011–2012)41) | Disability | ||||
| - HRS cohort (2008–2010)56,57) | Hospitalization | ||||
| SNF stay | |||||
| NH admission | |||||
| Falls | |||||
| Frailty phenotype | |||||
| Deficit-accumulation FI | |||||
AD, Alzheimer disease; ARIC, Atherosclerosis Risk in Communities; CHS, Cardiovascular Health Study; CPT, Current Procedural Terminology; DME, durable medical equipment; FI, frailty index; HCPCS, Healthcare Common Procedure Coding System; HES, Hospital Episode Statistics; HMO, health maintenance organization; HRS, Health and Retirement Study; ICD, International Classification of Diseases; ICU, intensive care unit; MCBS, Medicare Current Beneficiary Survey; MI, myocardial infarction; NH, nursing home; NHATS, National Health and Aging Trends Study; PRISMA, Program of Research to Integrate Services for the Maintenance of Autonomy; SEER, Surveillance, Epidemiology, and End Results; TAVR, transcatheter aortic valve replacement; VA, Veterans Affairs.
The comparative performance of database-derived frailty measures has not been well studied. In an analysis of Medicare Current Beneficiary Survey data, implementation of a deficit-accumulation frailty index using commonly used diagnosis codes or health service codes showed lower correlation with a reference standard frailty index and was less predictive of mortality than a frailty measure developed using a least absolute shrinkage and selection operator (LASSO) regression.41) A recent study compared four Medicare claims-based frailty measures—Davidoff index,40) Faurot index,48) Segal index,39) and Kim index41)—for the ability to measure frailty phenotype, deficit-accumulation frailty index, and activities-of-daily-living dependency (requiring another person’s help to perform daily activities). Of the four measures, the Kim index showed higher C statistic for frailty phenotype (0.78 vs. 0.73–0.74) after age and sex adjustment, as well as age and sex-adjusted partial correlation with a deficit-accumulation frailty index from clinical assessment (0.55 vs. 0.18–0.32).56)
These frailty measures have been applied to define population subgroups by frailty levels,61) reduce confounding by frailty in examining the association between influenza vaccination and mortality,62) estimate health care costs attributed to frailty,63) and improve mortality prediction after transcatheter aortic valve replacement.64)
FRAILTY MEASUREMENT IN EHR
Table 2 summarizes five frailty measures for EHR. Four measures were developed for three United States regional EHR systems65-68) or the Veterans Affairs EHR database,69) while the e-Frailty Index was developed for the United Kingdom primary care practices,35) which was later implemented in a primary care EHR system in Australia.59) Clinical knowledge-based selection was used for four measures while data-driven selection without a reference standard was used for one measure. A natural language processing method to explore unstructured clinic notes was applied for two measures.67,69)
Table 2.
Frailty measures for electronic health records
| Author (y) | Database/population (study year) | Outcomes | Predictors | ||
|---|---|---|---|---|---|
| Development | Validation | ||||
| Clinical knowledge-driven selection | Clegg et al.35) (2016) | Primary care EHR database (UK) | Not applicable | Mortality | Proportion of 36 health deficits present based on Read codes (codes for diagnosis, procedure, disability, and social circumstances) and polypharmacy |
| - ResearchOne database (2008–2016)35,70,75) | Hospitalization | ||||
| - THIN database (2008–2013)35,73) | NH admission | ||||
| - CPRD database (2001–2009)71,72 | Fracture | ||||
| Primary care EHR database, Australia | Frailty phenotype | ||||
| - A primary care clinic59) | |||||
| Lekan et al.65) (2017) | A tertiary-care hospital EHR database (USA) | Not applicable | Mortality | Includes 16 biopsychosocial factors including 4 laboratory tests | |
| - Inpatients (2010–2011)65,66) | Readmission | ||||
| SNF stay | |||||
| Anzaldi et al.67) (2017) | A regional health system EHR database (USA) | Not applicable | Geriatric syndromes identified using diagnosis codes and text phrases | Mention of “frailty” in clinical notes | |
| - Medicare ACO enrollees (2011–2013)67) | |||||
| Pajewski et al.68) (2019) | A regional health system EHR database (USA) | Not applicable | Mortality | Includes 54 health deficits based on diagnosis codes, smoking status, vital signs, laboratory tests, and functional status | |
| - Medicare ACO enrollees (2014–2016)68) | Falls | ||||
| Health care utilization | |||||
| Data-driven selection without a reference standard | Shao et al.69) (2017) | VA EHR database (USA) | Topics generated from clinical notes | Mortality | Includes 53 topics generated from clinical notes |
| - Heart failure patients (2010)69) | Hospitalization | ||||
ACO, accountable care organization; CPRD, Clinical Practice Research Datalink; EHR, electronic health records; NH, nursing home; SNF, skilled nursing facility; THIN, The Health Improvement Network; VA, Veterans Affairs.
Of these measures, the e-Frailty Index has been most widely used in the United Kingdom primary care EHR database to describe frailty trajectories before dying,70) examine the effect measure modification of systolic blood pressure and mortality relationship by frailty,71) predict fractures and mortality after fractures,72) and assess de-intensification for diabetes and hypertension treatment regimens among older adults with frailty.73)
CONSIDERATIONS IN DEVELOPING A DATABASE-DERIVED FRAILTY MEASURE
Database-derived frailty measures use different types of data (e.g., diagnosis, procedure, and health service codes) collected over a pre-specified period, ranging from 639) to 3649) months. Because some claims datasets record information according to a unique coding system specific to each country (e.g., Current Procedural Terminology codes and Healthcare Common Procedure Coding System codes in the United States and Read codes in the United Kingdom), the choice of datasets can affect the transportability of the frailty measures. The length of the assessment period during which codes are measured may affect the accuracy of capturing certain chronic conditions. Chronic conditions that are less likely recognized or coded by general practitioners (e.g., dementia and incontinence) may require a longer assessment period than acute conditions (e.g., acute myocardial infarction) or well recognized chronic conditions (e.g., hypertension and diabetes). A longer assessment period to calculate a frailty measure reduces the amount of follow-up data available for the main analysis.
Frailty measures developed from health care databases tend to rely on diagnoses, whereas clinical frailty assessment relies more on functional status and physical performance, factors rarely available in health care databases. Health service codes indicating clinical encounter types (e.g., home visits) and use of durable medical equipment (e.g., hospital beds or wheelchairs) seem to be important to capture functional impairment or poor physical performance, which differentiates frailty measures from comorbidity indices.57) However, including demographic characteristics in the frailty model lessens its ability to explain variation in frailty beyond demographic variables.56)
Once a frailty measure is developed, the key step is its validation against a reference standard measure of frailty. Given the lack of consensus on frailty definitions,12) prevalent activities-of-daily-living dependency can be used as an alternative outcome for validation.40,48,56,60) However, information on a reference standard frailty measure or activities-of-daily-living dependency is not always available. Many database-derived frailty measures were tested for mortality prediction rather than for frailty itself. Although frailty is associated with mortality, it is unclear how these frailty measures can be differentiated from mortality prediction models.
Another consideration is that coding systems or coding practices may change over time or vary across geographical regions. In the United States, the International Classification of Disease system transitioned from the 9th to 10th revisions in October 2015. New billing codes are generated for new procedures and health care services and some codes are retired each year. Coding practice may be influenced by the likelihood of reimbursement for health care services, which may differ across health care systems or countries. Therefore, the performance of claims-based frailty measures should be evaluated periodically in more contemporary datasets and before application to a different health care system or country.
Lastly, the development of a frailty measure from EHR may require restricting the population to those with high rates of data completeness within an EHR system to avoid bias due to health information outside the EHR system.30) A predictive algorithm is available to identify those with high rates of completeness.74)
POTENTIAL APPLICATIONS OF DATABASE-DERIVED FRAILTY MEASURES
Frailty measures calculated from health care databases can be useful to measure frailty and study health outcomes of older adults with frailty in clinical care and research (Table 3).
Table 3.
Potential applications of database-derived frailty measures and areas for future research
| Areas | Applications | Caveats/areas for future research |
|---|---|---|
| Clinical care | Screen for frail individuals requiring detailed evaluation and care management in a health care system or health plan | Database-derived frailty measures are acceptable yet imperfect; thus, they are unlikely to replace clinical assessment. |
| Predict the risk of adverse health outcomes (frailty measures are more useful than comorbidity measures for the prediction of disability, mobility impairment, falls, and SNF days). | Seeking health care during acute illness or functional decline may lead to overestimation of the frailty level (informed presence bias). | |
| Further improvement in frailty measurement may be possible by including clinical assessment datasets (e.g., MDS or OASIS in the United States Medicare database) or EHR clinic notes. | ||
| Research | Efficiently screen for frail individuals to enroll in a clinical trial | Responsiveness and MCID of database-derived frailty measures remain to be investigated. |
| Adjust for case-mix (confounding) by frailty in evaluating the effect of medical treatment or outcomes among health care systems | The assessment period used to calculate a frailty measure ranges from 6 to 36 months. The optimal period is not known. | |
| Evaluate the treatment effect heterogeneity by frailty in analysis of health care databases or clinical trial datasets (by linking clinical trial data to claims data for estimation of frailty level) | Residual confounding may exist even after adjusting for case-mix by using a database-derived frailty measure. | |
| Usefulness of EHR data may depend on the health information technology infrastructure and completeness of documentation. |
EHR, electronic health records; MCID, minimal clinically important difference; MDS, Minimum Data Set; OASIS, Outcome and Assessment Information Set; SNF, skilled nursing facility.
Clinical Care
Database-derived frailty measures can be used to screen older adults for frailty in a health care system or a health plan. Because database-derived frailty scores generally have C statistics ranging from 0.65 to 0.75 for frailty phenotype and correlation coefficients of 0.2 to 0.6 against a deficit-accumulation frailty index,37,39,56) they are unlikely to replace bed-side clinical frailty assessments. Frailty measures are useful to predict adverse health outcomes. In particular, the Kim index performed better than a comorbidity index for the prediction of disability, mobility impairment, recurrent falls, and skilled nursing facility days in the Medicare population.41,57) However, an e-Frailty Index >0.19, a threshold for frailty, had a positive predictive value of 0.11 for death in the next 3 months among primary care patients in the United Kingdom. These results suggest that, although a database-derived frailty measure may be a strong predictor in a population, it cannot be interpreted deterministically for an individual (this issue also exists for a clinical frailty assessment).75) Nonetheless, they can be useful as a routine screening test to identify individuals requiring additional detailed assessment and individualized care management.76) A cut-off point for positive screening can be determined according to percentile distributions (e.g., top 5% percent), sensitivity and specificity for frailty state (e.g., 90% sensitivity to detect frailty phenotype), or pre-defined clinically relevant thresholds (e.g., ≥0.20 according to a deficit-accumulation frailty index) after considering clinical contexts (e.g., outpatient, inpatient, or preoperative screening) and available resources for detailed assessment and care management.
Research
Database-derived frailty measures provide vast opportunities for clinical research in older populations. These measures can be used to efficiently screen individuals for enrollment in a clinical trial of interventions for frailty. In database studies to evaluate treatment effects in older adults, treated individuals may differ in frailty levels from untreated individuals, which leads to confounding. Such bias can be reduced by adjusting for a frailty measure, although residual confounding may persist.62) In choosing a frailty measure for confounding adjustment, a measure that does not include demographic variables may be more effective than a measure that includes them.56) Moreover, frailty can be an effect measure modifier. The benefits and risks of a treatment may vary by frailty status—e.g., a hypnotic drug increases the risk of hip fracture more in less frail older adults than frailer ones who are totally dependent.77) Evaluation of treatment effect heterogeneity by frailty in health care databases may provide real-world evidence to guide individualized treatment choice based on frailty assessment in older adults who are typically excluded from clinical trials. In some clinical trials that enrolled frail individuals yet lacked frailty assessment, frailty levels at trial baseline can be estimated by linking trial data to administrative claims data or EHR and applying database-derived frailty measures. Such secondary analyses of existing clinical trial data may generate hypotheses for future trials.
AREAS OF UNCERTAINTY
Few studies to date used a database-derived frailty measure as an outcome (i.e., change in frailty level over time) to evaluate the treatment effect. The responsiveness of a frailty measure to improvement or deterioration of health status and the minimal clinically important change have not been well studied. Diagnosis codes, which comprise a large proportion of the database-derived frailty measures, tend to be carried over visits and accumulate over time in administrative claims data or EHR, causing increased frailty score. Since older adults are more likely to seek medical care during acute illness or functional decline (informed presence bias78)), the estimated frailty level may be affected by the effect of acute illness and frailty progression may be recorded more often than improvement. Furthermore, in health care databases, the information needed to estimate frailty is obtained over time as opposed to clinical trials wherein information is obtained from a discrete assessment visit (e.g., baseline or follow-up visit). Therefore, the assessment periods may overlap between outcome frailty and baseline frailty, making the two measures highly collinear. For these reasons, the utility of a database-derived frailty measure as a treatment outcome remains uncertain.
Information on functional status or physical performance is often recorded in health care databases. In United States Medicare data, the Minimum Data Set records clinicians’ assessments of functional status among nursing home patients. The Outcome and Assessment Information Set contains information on patient outcomes for individuals receiving home care. In EHR, cognitive function and physical function are documented in clinical notes by primary care physicians, specialists (e.g., geriatricians, neurologists, and psychiatrists), physical therapists, or occupational therapists. In the absence of routine assessment, these documentations tend to be inconsistently available or for a subset of patients in specific clinical contexts (e.g., after a fall event, hospitalization, or major surgery), which may not represent an individual’s usual state of health. A recent study by Kharrazi et al.79) showed that the prevalence of geriatric syndromes was underestimated when only claims and structured EHR data were analyzed; natural language processing of unstructured EHR data substantially improved detection by 1.5-fold for dementia, 3.2-fold for falls, 18.0-fold for malnutrition, and 455.9-fold for lack of social support. While these findings are promising, the contribution of unstructured EHR data for case identification depends on the health information technology infrastructure and completeness of documentation by health care providers.79) How to best combine clinical information with administrative claims data or structured EHR data requires further investigation.
CONCLUSIONS
The use of a database-derived frailty measure offers new opportunities to facilitate frailty screening in clinical care and quantify frailty for large population-based database research in which clinical assessment is not feasible. Several database-derived frailty measures have been validated for use in administrative claims data and EHR, with some key differences (Fig. 2): target population (16 ambulatory, 1 long-term care, and 4 inpatient), data source (16 claims-based and 5 EHR-based measures), length of the assessment period (6 to 36 months), data types required for calculation (diagnosis codes required for 17 measures, health service codes for 7 measures, pharmacy data for 4 measures, and other additional information for 9 measures), and outcomes against which a frailty measure was validated (clinical frailty assessment for 7 measures, disability for 7 measures, and mortality for 16 measures). This summary can serve as a guide to choosing a database-derived frailty measure that suits specific objectives and databases at hand.
Fig. 2.
Considerations in choosing a database-derived frailty measure. EHR, electronic health records.
Footnotes
CONFLICT OF INTEREST
The author provides paid consultative services to Alosa Health, a nonprofit educational organization with no relationship to any drug or device manufacturers.
FUNDING
The author is supported by R01AG062713 from the National Institute on Aging (NIA). The funding sources had no role in the data design, collection, analysis, or interpretation or the decision to submit the manuscript for publication.
REFERENCES
- 1.Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. 2013;381:752–62. doi: 10.1016/S0140-6736(12)62167-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Collard RM, Boter H, Schoevers RA, Oude Voshaar RC. Prevalence of frailty in community-dwelling older persons: a systematic review. J Am Geriatr Soc. 2012;60:1487–92. doi: 10.1111/j.1532-5415.2012.04054.x. [DOI] [PubMed] [Google Scholar]
- 3.Kim KJ, Shin J, Choi J, Won CW. Discrepancies in the prevalence of known frailty scales: Korean Frailty and Aging Cohort Study. Ann Geriatr Med Res. 2018;22:137–44. doi: 10.4235/agmr.2018.22.3.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kojima G. Prevalence of frailty in nursing homes: a systematic review and meta-analysis. J Am Med Dir Assoc. 2015;16:940–5. doi: 10.1016/j.jamda.2015.06.025. [DOI] [PubMed] [Google Scholar]
- 5.Hajek A, Bock JO, Saum KU, Matschinger H, Brenner H, Holleczek B, et al. Frailty and healthcare costs-longitudinal results of a prospective cohort study. Age Ageing. 2018;47:233–41. doi: 10.1093/ageing/afx157. [DOI] [PubMed] [Google Scholar]
- 6.Comans TA, Peel NM, Hubbard RE, Mulligan AD, Gray LC, Scuffham PA. The increase in healthcare costs associated with frailty in older people discharged to a post-acute transition care program. Age Ageing. 2016;45:317–20. doi: 10.1093/ageing/afv196. [DOI] [PubMed] [Google Scholar]
- 7.Figueroa JF, Joynt Maddox KE, Beaulieu N, Wild RC, Jha AK. Concentration of potentially preventable spending among high-cost medicare subpopulations: an observational study. Ann Intern Med. 2017;167:706–13. doi: 10.7326/M17-0767. [DOI] [PubMed] [Google Scholar]
- 8.Joynt KE, Figueroa JF, Beaulieu N, Wild RC, Orav EJ, Jha AK. Segmenting high-cost Medicare patients into potentially actionable cohorts. Healthc (Amst) 2017;5:62–7. doi: 10.1016/j.hjdsi.2016.11.002. [DOI] [PubMed] [Google Scholar]
- 9.Buckinx F, Rolland Y, Reginster JY, Ricour C, Petermans J, Bruyere O. Burden of frailty in the elderly population: perspectives for a public health challenge. Arch Public Health. 2015;73:19. doi: 10.1186/s13690-015-0068-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hoogendijk EO, Afilalo J, Ensrud KE, Kowal P, Onder G, Fried LP. Frailty: implications for clinical practice and public health. Lancet. 2019;394:1365–75. doi: 10.1016/S0140-6736(19)31786-6. [DOI] [PubMed] [Google Scholar]
- 11.Dent E, Martin FC, Bergman H, Woo J, Romero-Ortuno R, Walston JD. Management of frailty: opportunities, challenges, and future directions. Lancet. 2019;394:1376–86. doi: 10.1016/S0140-6736(19)31785-4. [DOI] [PubMed] [Google Scholar]
- 12.Morley JE, Vellas B, van Kan GA, Anker SD, Bauer JM, Bernabei R, et al. Frailty consensus: a call to action. J Am Med Dir Assoc. 2013;14:392–7. doi: 10.1016/j.jamda.2013.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Buta BJ, Walston JD, Godino JG, Park M, Kalyani RR, Xue QL, et al. Frailty assessment instruments: systematic characterization of the uses and contexts of highly-cited instruments. Ageing Res Rev. 2016;26:53–61. doi: 10.1016/j.arr.2015.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aguayo GA, Donneau AF, Vaillant MT, Schritz A, Franco OH, Stranges S, et al. Agreement between 35 published frailty scores in the general population. Am J Epidemiol. 2017;186:420–34. doi: 10.1093/aje/kwx061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Theou O, Squires E, Mallery K, Lee JS, Fay S, Goldstein J, et al. What do we know about frailty in the acute care setting? A scoping review. BMC Geriatr. 2018;18:139. doi: 10.1186/s12877-018-0823-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dent E, Morley JE, Cruz-Jentoft AJ, Woodhouse L, Rodriguez-Manas L, Fried LP, Woo J, et al. Physical frailty: ICFSR international clinical practice guidelines for identification and management. J Nutr Health Aging. 2019;23:771–87. doi: 10.1007/s12603-019-1273-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173:489–95. doi: 10.1503/cmaj.050051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Morley JE, Malmstrom TK, Miller DK. A simple frailty questionnaire (FRAIL) predicts outcomes in middle aged African Americans. J Nutr Health Aging. 2012;16:601–8. doi: 10.1007/s12603-012-0084-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Theou O, Andrew M, Ahip SS, Squires E, McGarrigle L, Blodgett JM, et al. The pictorial fit-frail scale: developing a visual scale to assess frailty. Can Geriatr J. 2019;22:64–74. doi: 10.5770/cgj.22.357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Beth Israel Deaconess Medical Center . Boston, MA: Beth Israel Deaconess Medical Center; c2020. Senior health calculator: for providers - online tool to calculate Frailty Index (FI) [Internet] [cited 2020 Feb 1]. Available from: https://www.bidmc.org/research/research-by-department/medicine/gerontology/calculator. [Google Scholar]
- 21.Saliba D, Elliott M, Rubenstein LZ, Solomon DH, Young RT, Kamberg CJ, et al. The Vulnerable Elders Survey: a tool for identifying vulnerable older people in the community. J Am Geriatr Soc. 2001;49:1691–9. doi: 10.1046/j.1532-5415.2001.49281.x. [DOI] [PubMed] [Google Scholar]
- 22.Mitnitski AB, Song X, Rockwood K. The estimation of relative fitness and frailty in community-dwelling older adults using self-report data. J Gerontol A Biol Sci Med Sci. 2004;59:M627–32. doi: 10.1093/gerona/59.6.m627. [DOI] [PubMed] [Google Scholar]
- 23.Schuurmans H, Steverink N, Lindenberg S, Frieswijk N, Slaets JP. Old or frail: what tells us more? J Gerontol A Biol Sci Med Sci. 2004;59:M962–5. doi: 10.1093/gerona/59.9.m962. [DOI] [PubMed] [Google Scholar]
- 24.Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56:M146–56. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- 25.Jones DM, Song X, Rockwood K. Operationalizing a frailty index from a standardized comprehensive geriatric assessment. J Am Geriatr Soc. 2004;52:1929–33. doi: 10.1111/j.1532-5415.2004.52521.x. [DOI] [PubMed] [Google Scholar]
- 26.Rolfson DB, Majumdar SR, Tsuyuki RT, Tahir A, Rockwood K. Validity and reliability of the Edmonton Frail Scale. Age Ageing. 2006;35:526–9. doi: 10.1093/ageing/afl041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gobbens RJ, van Assen MA, Luijkx KG, Wijnen-Sponselee MT, Schols JM. The Tilburg Frailty Indicator: psychometric properties. J Am Med Dir Assoc. 2010;11:344–55. doi: 10.1016/j.jamda.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 28.Nicosia FM, Spar MJ, Steinman MA, Lee SJ, Brown RT. Making function part of the conversation: clinician perspectives on measuring functional status in primary care. J Am Geriatr Soc. 2019;67:493–502. doi: 10.1111/jgs.15677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Walston J, Bandeen-Roche K, Buta B, Bergman H, Gill TM, Morley JE, et al. Moving frailty toward clinical practice: NIA intramural frailty science symposium summary. J Am Geriatr Soc. 2019;67:1559–64. doi: 10.1111/jgs.15928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lin KJ, Schneeweiss S. Considerations for the analysis of longitudinal electronic health records linked to claims data to study the effectiveness and safety of drugs. Clin Pharmacol Ther. 2016;100:147–59. doi: 10.1002/cpt.359. [DOI] [PubMed] [Google Scholar]
- 31.Kim DH, Schneeweiss S. Measuring frailty using claims data for pharmacoepidemiologic studies of mortality in older adults: evidence and recommendations. Pharmacoepidemiol Drug Saf. 2014;23:891–901. doi: 10.1002/pds.3674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ruiz JG, Priyadarshni S, Rahaman Z, Cabrera K, Dang S, Valencia WM, Mintzer MJ. Validation of an automatically generated screening score for frailty: the care assessment need (CAN) score. BMC Geriatr. 2018;18:106. doi: 10.1186/s12877-018-0802-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ruiz JG, Rahaman Z, Dang S, Anam R, Valencia WM, Mintzer MJ. Association of the CAN score with the FRAIL scale in community dwelling older adults. Aging Clin Exp Res. 2018;30:1241–5. doi: 10.1007/s40520-018-0910-4. [DOI] [PubMed] [Google Scholar]
- 34.Searle SD, Mitnitski A, Gahbauer EA, Gill TM, Rockwood K. A standard procedure for creating a frailty index. BMC Geriatr. 2008;8:24. doi: 10.1186/1471-2318-8-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Clegg A, Bates C, Young J, Ryan R, Nichols L, Ann Teale E, et al. Development and validation of an electronic frailty index using routine primary care electronic health record data. Age Ageing. 2016;45:353–60. doi: 10.1093/ageing/afw039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rockwood K, Mitnitski A. Limits to deficit accumulation in elderly people. Mech Ageing Dev. 2006;127:494–6. doi: 10.1016/j.mad.2006.01.002. [DOI] [PubMed] [Google Scholar]
- 37.Gilbert T, Neuburger J, Kraindler J, Keeble E, Smith P, Ariti C, et al. Development and validation of a Hospital Frailty Risk Score focusing on older people in acute care settings using electronic hospital records: an observational study. Lancet. 2018;391:1775–82. doi: 10.1016/S0140-6736(18)30668-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shi SM, Kim DH. The challenges of using the Hospital Frailty Risk Score. Lancet. 2019;392:2692. doi: 10.1016/S0140-6736(18)32426-7. [DOI] [PubMed] [Google Scholar]
- 39.Segal JB, Chang H-Y, Du Y, Walston JD, Carlson MC, Varadhan R. Development of a claims-based frailty indicator anchored to a well-established frailty phenotype. Med Care. 2017;55:716–22. doi: 10.1097/MLR.0000000000000729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Davidoff AJ, Zuckerman IH, Pandya N, Hendrick F, Ke X, Hurria A, et al. A novel approach to improve health status measurement in observational claims-based studies of cancer treatment and outcomes. J Geriatr Oncol. 2013;4:157–65. doi: 10.1016/j.jgo.2012.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kim DH, Schneeweiss S, Glynn RJ, Lipsitz LA, Rockwood K, Avorn J. Measuring frailty in medicare data: development and validation of a claims-based frailty index. J Gerontol A Biol Sci Med Sci. 2018;73:980–7. doi: 10.1093/gerona/glx229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lunney JR, Lynn J, Hogan C. Profiles of older medicare decedents. J Am Geriatr Soc. 2002;50:1108–12. doi: 10.1046/j.1532-5415.2002.50268.x. [DOI] [PubMed] [Google Scholar]
- 43.Abrams C, Lieberman R, Weiner JP. Development and evaluation of the Johns Hopkins University Risk adjustment models for Medicare+Choice plan payment. Baltimore, MD: Johns Hopkins University Press; 2003. [Google Scholar]
- 44.Chrischilles E, Schneider K, Wilwert J, Lessman G, O'Donnell B, Gryzlak B, et al. Beyond comorbidity: expanding the definition and measurement of complexity among older adults using administrative claims data. Med Care. 2014;52 Suppl 3:S75–84. doi: 10.1097/MLR.0000000000000026. [DOI] [PubMed] [Google Scholar]
- 45.JEN Associates Inc . MassHealth SCO program evaluation pre-SCO enrollment period CY2004 and post-SCO enrollment period CY2005 nursing home entry rate and frailty level comparisons. Cambridge, MA: JEN Associates Inc; 2008. [Google Scholar]
- 46.JEN Associates Inc . Cambridge, MA: JEN Associates Inc.; c2019. JEN Frailty Index (JFI) [Internet] [cited 2020 Feb 1]. Available from: https://www.jen.com/jfi2. [Google Scholar]
- 47.Hope AA, Gong MN, Guerra C, Wunsch H. Frailty before critical illness and mortality for elderly medicare beneficiaries. J Am Geriatr Soc. 2015;63:1121–8. doi: 10.1111/jgs.13436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Faurot KR, Jonsson Funk M, Pate V, Brookhart MA, Patrick A, Hanson LC, et al. Using claims data to predict dependency in activities of daily living as a proxy for frailty. Pharmacoepidemiol Drug Saf. 2015;24:59–66. doi: 10.1002/pds.3719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Orkaby AR, Nussbaum L, Ho YL, Gagnon D, Quach L, Ward R, et al. The burden of frailty among U.S. veterans and its association with mortality, 2002-2012. J Gerontol A Biol Sci Med Sci. 2019;74:1257–64. doi: 10.1093/gerona/gly232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rosen A, Wu J, Chang BH, Berlowitz D, Ash A, Moskowitz M. Does diagnostic information contribute to predicting functional decline in long-term care? Med Care. 2000;38:647–59. doi: 10.1097/00005650-200006000-00006. [DOI] [PubMed] [Google Scholar]
- 51.McIsaac DI, Wong CA, Huang A, Moloo H, van Walraven C. Derivation and validation of a generalizable preoperative frailty index using population-based health administrative data. Ann Surg. 2019;270:102–8. doi: 10.1097/SLA.0000000000002769. [DOI] [PubMed] [Google Scholar]
- 52.Dubois MF, Dubuc N, Kroger E, Girard R, Hebert R. Assessing comorbidity in older adults using prescription claims data. J Pharm Health Serv Res. 2010;1:157–65. [Google Scholar]
- 53.Soong J, Poots AJ, Scott S, Donald K, Woodcock T, Lovett D, et al. Quantifying the prevalence of frailty in English hospitals. BMJ Open. 2015;5:e008456. doi: 10.1136/bmjopen-2015-008456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sternberg SA, Bentur N, Abrams C, Spalter T, Karpati T, Lemberger J, et al. Identifying frail older people using predictive modeling. Am J Manag Care. 2012;18:e392–7. [PubMed] [Google Scholar]
- 55.Segal JB, Huang J, Roth DL, Varadhan R. External validation of the claims-based frailty index in the national health and aging trends study cohort. Am J Epidemiol. 2017;186:745–7. doi: 10.1093/aje/kwx257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kim DH, Patorno E, Pawar A, Lee H, Schneeweiss S, Glynn RJ. Measuring frailty in administrative claims data: comparative performance of four claims-based frailty measures in the united states medicare data. J Gerontol A Biol Sci Med Sci. 2019 doi: 10.1093/gerona/glz224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kim DH, Glynn RJ, Avorn J, Lipsitz LA, Rockwood K, Pawar A, et al. Validation of a claims-based frailty index against physical performance and adverse health outcomes in the health and retirement study. J Gerontol A Biol Sci Med Sci. 2019;74:1271–6. doi: 10.1093/gerona/gly197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Cuthbertson CC, Kucharska-Newton A, Faurot KR, Sturmer T, Jonsson Funk M, Palta P, et al. Controlling for frailty in pharmacoepidemiologic studies of older adults: validation of an existing medicare claims-based algorithm. Epidemiology. 2018;29:556–61. doi: 10.1097/EDE.0000000000000833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ambagtsheer RC, Beilby J, Dabravolskaj J, Abbasi M, Archibald MM, Dent E. Application of an electronic Frailty Index in Australian primary care: data quality and feasibility assessment. Aging Clin Exp Res. 2019;31:653–60. doi: 10.1007/s40520-018-1023-9. [DOI] [PubMed] [Google Scholar]
- 60.Kinosian B, Wieland D, Gu X, Stallard E, Phibbs CS, Intrator O. Validation of the JEN frailty index in the National Long-Term Care Survey community population: identifying functionally impaired older adults from claims data. BMC Health Serv Res. 2018;18:908. doi: 10.1186/s12913-018-3689-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Yao NA, Ritchie C, Cornwell T, Leff B. Use of home-based medical care and disparities. J Am Geriatr Soc. 2018;66:1716–20. doi: 10.1111/jgs.15444. [DOI] [PubMed] [Google Scholar]
- 62.Zhang HT, McGrath LJ, Wyss R, Ellis AR, Stürmer T. Controlling confounding by frailty when estimating influenza vaccine effectiveness using predictors of dependency in activities of daily living. Pharmacoepidemiol Drug Saf. 2017;26:1500–6. doi: 10.1002/pds.4298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Simpson KN, Seamon BA, Hand BN, Roldan CO, Taber DJ, Moran WP, et al. Effect of frailty on resource use and cost for Medicare patients. J Comp Eff Res. 2018;7:817–25. doi: 10.2217/cer-2018-0029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kundi H, Valsdottir LR, Popma JJ, Cohen DJ, Strom JB, Pinto DS, et al. Impact of a claims-based frailty indicator on the prediction of long-term mortality after transcatheter aortic valve replacement in medicare beneficiaries. Circ Cardiovasc Qual Outcomes. 2018;11:e005048. doi: 10.1161/CIRCOUTCOMES.118.005048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lekan DA, Wallace DC, McCoy TP, Hu J, Silva SG, Whitson HE. Frailty assessment in hospitalized older adults using the electronic health record. Biol Res Nurs. 2017;19:213–28. doi: 10.1177/1099800416679730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lekan DA, McCoy TP. Frailty risk in hospitalised older adults with and without diabetes mellitus. J Clin Nurs. 2018;27:3510–21. doi: 10.1111/jocn.14529. [DOI] [PubMed] [Google Scholar]
- 67.Anzaldi LJ, Davison A, Boyd CM, Leff B, Kharrazi H. Comparing clinician descriptions of frailty and geriatric syndromes using electronic health records: a retrospective cohort study. BMC Geriatr. 2017;17:248. doi: 10.1186/s12877-017-0645-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Pajewski NM, Lenoir K, Wells BJ, Williamson JD, Callahan KE. Frailty screening using the electronic health record within a medicare accountable care organization. J Gerontol A Biol Sci Med Sci. 2019;74:1771–7. doi: 10.1093/gerona/glz017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Shao Y, Mohanty AF, Ahmed A, Weir CR, Bray BE, Shah RU, et al. Identification and use of frailty indicators from text to examine associations with clinical outcomes among patients with heart failure. AMIA Annu Symp Proc. 2017;2016:1110–8. [PMC free article] [PubMed] [Google Scholar]
- 70.Stow D, Matthews FE, Hanratty B. Frailty trajectories to identify end of life: a longitudinal population-based study. BMC Med. 2018;16:171. doi: 10.1186/s12916-018-1148-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ravindrarajah R, Hazra NC, Hamada S, Charlton J, Jackson SHD, Dregan A, et al. Systolic blood pressure trajectory, frailty, and all-cause mortality >80 years of age: cohort study using electronic health records. Circulation. 2017;135:2357–68. doi: 10.1161/CIRCULATIONAHA.116.026687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ravindrarajah R, Hazra NC, Charlton J, Jackson SHD, Dregan A, Gulliford MC. Incidence and mortality of fractures by frailty level over 80 years of age: cohort study using UK electronic health records. BMJ Open. 2018;8:e018836. doi: 10.1136/bmjopen-2017-018836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.McAlister FA, Lethebe BC, Lambe C, Williamson T, Lowerison M. Control of glycemia and blood pressure in British adults with diabetes mellitus and subsequent therapy choices: a comparison across health states. Cardiovasc Diabetol. 2018;17:27. doi: 10.1186/s12933-018-0673-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lin KJ, Singer DE, Glynn RJ, Murphy SN, Lii J, Schneeweiss S. Identifying patients with high data completeness to improve validity of comparative effectiveness research in electronic health records data. Clin Pharmacol Ther. 2018;103:899–905. doi: 10.1002/cpt.861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Stow D, Matthews FE, Barclay S, Iliffe S, Clegg A, De Biase S, et al. Evaluating frailty scores to predict mortality in older adults using data from population based electronic health records: case control study. Age Ageing. 2018;47:564–9. doi: 10.1093/ageing/afy022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Rockwood K. Screening for grades of frailty using electronic health records: where do we go from here? Age Ageing. 2016;45:328–9. doi: 10.1093/ageing/afw057. [DOI] [PubMed] [Google Scholar]
- 77.Berry SD, Lee Y, Cai S, Dore DD. Nonbenzodiazepine sleep medication use and hip fractures in nursing home residents. JAMA Intern Med. 2013;173:754–61. doi: 10.1001/jamainternmed.2013.3795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Weiskopf NG, Rusanov A, Weng C. Sick patients have more data: the non-random completeness of electronic health records. AMIA Annu Symp Proc. 2013;2013:1472–7. [PMC free article] [PubMed] [Google Scholar]
- 79.Kharrazi H, Anzaldi LJ, Hernandez L, Davison A, Boyd CM, Leff B, et al. The value of unstructured electronic health record data in geriatric syndrome case identification. J Am Geriatr Soc. 2018;66:1499–507. doi: 10.1111/jgs.15411. [DOI] [PubMed] [Google Scholar]
- 80.McIsaac DI, Bryson GL, van Walraven C. Association of frailty and 1-year postoperative mortality following major elective noncardiac surgery: a population-based cohort study. JAMA Surg. 2016;151:538–45. doi: 10.1001/jamasurg.2015.5085. [DOI] [PubMed] [Google Scholar]
- 81.McIsaac DI, Beaule PE, Bryson GL, Van Walraven C. The impact of frailty on outcomes and healthcare resource usage after total joint arthroplasty: a population-based cohort study. Bone Joint J. 2016;98-B:799–805. doi: 10.1302/0301-620X.98B6.37124. [DOI] [PubMed] [Google Scholar]
- 82.McIsaac DI, Moloo H, Bryson GL, van Walraven C. The association of frailty with outcomes and resource use after emergency general surgery: a population-based cohort study. Anesth Analg. 2017;124:1653–61. doi: 10.1213/ANE.0000000000001960. [DOI] [PubMed] [Google Scholar]
- 83.McIsaac DI, Wijeysundera DN, Huang A, Bryson GL, van Walraven C. Association of the hospital volume of frail surgical patients cared for with outcomes after elective, major noncardiac surgery: a retrospective population-based cohort study. Anesthesiology. 2017;126:602–13. doi: 10.1097/ALN.0000000000001536. [DOI] [PubMed] [Google Scholar]
- 84.Tan HJ, Shirk JD, Chamie K, Litwin MS, Hu JC. Patient function and the value of surgical care for kidney cancer. J Urol. 2017;197:1200–7. doi: 10.1016/j.juro.2016.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Gilden DM, Kubisiak JM, Kahle-Wrobleski K, Ball DE, Bowman L. Using U.S. Medicare records to evaluate the indirect health effects on spouses: a case study in Alzheimer's disease patients. BMC Health Serv Res. 2014;14:291. doi: 10.1186/1472-6963-14-291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.De Jonge KE, Jamshed N, Gilden D, Kubisiak J, Bruce SR, Taler G. Effects of home-based primary care on Medicare costs in high-risk elders. J Am Geriatr Soc. 2014;62:1825–31. doi: 10.1111/jgs.12974. [DOI] [PubMed] [Google Scholar]
- 87.Soong J, Poots AJ, Scott S, Donald K, Bell D. Developing and validating a risk prediction model for acute care based on frailty syndromes. BMJ Open. 2015;5:e008457. doi: 10.1136/bmjopen-2015-008457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Hui Y, van Walraven C, McIsaac DI. How do common comorbidities modify the association of frailty with survival after elective noncardiac surgery? A Population-Based Cohort Study. Anesth Analg. 2019;129:1699–706. doi: 10.1213/ANE.0000000000004387. [DOI] [PubMed] [Google Scholar]
- 89.Rosen A, Wu J, Chang BH, Berlowitz D, Rakovski C, Ash A, et al. Risk adjustment for measuring health outcomes: an application in VA long-term care. Am J Med Qual. 2001;16:118–27. doi: 10.1177/106286060101600403. [DOI] [PubMed] [Google Scholar]
- 90.Davidoff AJ, Gardner LD, Zuckerman IH, Hendrick F, Ke X, Edelman MJ. Validation of disability status, a claims-based measure of functional status for cancer treatment and outcomes studies. Med Care. 2014;52:500–10. doi: 10.1097/MLR.0000000000000122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Feliciano J, Gardner L, Hendrick F, Edelman MJ, Davidoff A. Assessing functional status and the survival benefit of chemotherapy for advanced non-small cell lung cancer using administrative claims data. Lung Cancer. 2015;87:59–64. doi: 10.1016/j.lungcan.2014.10.011. [DOI] [PubMed] [Google Scholar]