Abstract
Background: The state of West Virginia (WV) is often seen as a health care desert with a scarcity of hospitals and resources. The prevalence of cerebrovascular disease and associated comorbidities are also some of the highest in the nation.
Introduction: Ischemic stroke is a time-sensitive diagnosis. Prompt treatment in WV is difficult due to limited and isolated stroke-ready hospitals. Adoption of telestroke has helped to bypass these obstacles and improve access to care.
Materials and Methods: Retrospective analyses; using data from the American Heart Association's Get With The Guidelines Stroke Data Registry, and other statewide agencies, we looked for trends in the volume of patients treated with intravenous-tissue plasminogen activator (tPA) in WV. We also reviewed data from West Virginia University's (WVU) telestroke database to assess trends in consult volumes and quality metrics.
Results: Since the establishment of WVU telestroke, the total number of stroke patients receiving tPA across the state increased by 173% from 2015 (259 patients) to 2018 (448 patients) (p < 0.0001). Telestroke consults made up 24% (107/448) of total statewide tPA administrations for 2018. Between 2016 and 2018, the total symptomatic hemorrhage rate for tPA treated patients through telestroke was 1% (3/292). Telestroke also facilitated local care by avoiding patient transfer on average 65% of the time.
Conclusion: Not only has telestroke increased the quantity of treated acute ischemic strokes, but it has also done so safely and effectively even in resource-poor areas. These findings demonstrate that telestroke is a useful tool for treating strokes, particularly those that happen far from stroke centers.
Keywords: teleneurology, telemedicine, telehealth, emergency medicine/teletrauma
Introduction
Although advances in care have reduced the overall mortality of stroke, it remains the fifth leading cause of mortality nationally1 and in West Virginia (WV).2 Furthermore, rural populations are 1.45 times more likely to experience a stroke than urban populations.3 Compounding this disparity, rural populations are less likely to receive intravenous tissue plasminogen activator (IV-tPA) than patients at urban centers.4 This difference is likely due to decreased access to stroke centers with specialized cerebrovascular care.5 In nonstroke centers, it is often left to an emergency medicine (EM) physician to treat acute stroke; however, a survey conducted among EM physicians found that 40% would never use tPA.6 A lack of access to providers with neurological expertise was identified in a separate survey as a significant barrier to treatment.7
In the United States, only 55.5%, 43.2%, and 22.3% of the population has access to a stroke center within 60, 45, or 30 min, respectively.4 In WV, the access gap is more extreme. WV covers 24,078 square miles with a population of 1.8 million people8 who are cared for by 58 active neurologists9 with only one comprehensive stroke center.
Telestroke treatment of acute ischemic stroke (AIS) with tPA has been shown to be effective within 3 h of onset,10 but information regarding thrombolytic treatment in the 3–4.5 h window and the impact of telestroke on triage for endovascular transfer is lacking.
The purpose of this article is to demonstrate the safety and efficacy of acute stroke treatment through telestroke using a hub and spoke model in WV. This study includes the extended window (3.5–4 h) thrombolysis treatments and endovascular triage.
Materials and Methods
This study was approved by the institutional review board at West Virginia University (WVU).
All data analyzed were derived from hospitals throughout the state of WV. There are about 46 hospitals in WV (per the WV Hospital Association). Thirty of WV 55 counties have at least one hospital. Twelve counties have two or more. Thirteen counties have no hospital. There are five primary stroke centers and only one comprehensive stroke center listed in the WV Department of Health and Human Resources.
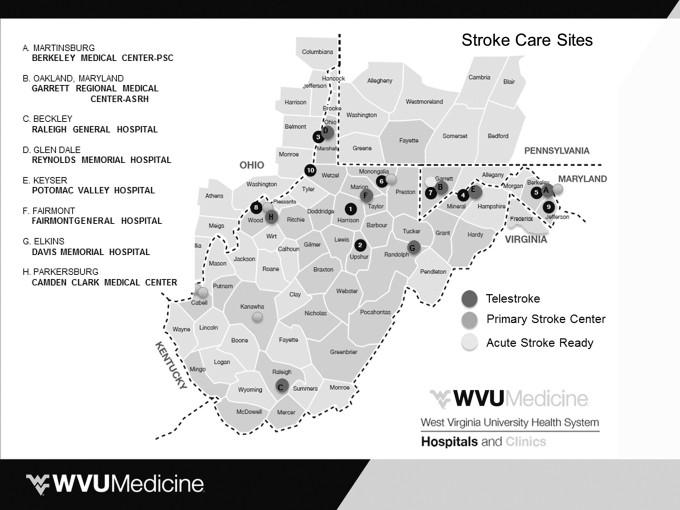
WVU has been providing telestroke consultation since 2016, with eight active sites at the end of 2018 (Fig. 1). There are currently eight neurologists in the call pool. The spoke site initiates a consult by calling a centralized phone number that connects to the on-call neurologist. Basic information is collected followed by a formal telestroke evaluation. Different variables are collected for these patients, including demographic data, location of call, relevant time metrics, National Institutes of Health Stroke Scale (NIHSS), if the patient was administered thrombolytic, or if the patient was transferred for endovascular therapy (EVT). The teleneurology coordinator maintains this database and ensures the accuracy of the data. Telestroke personnel verified diagnoses and tPA eligibility from the electronic medical record. There is a quarterly phone call with all sites where all patient-related outcomes and complications are collected and feedback is provided.
Fig. 1.
Stroke care sites and telestroke sites in West Virginia. WVU, West Virginia University.
State-level data were derived from Get With The Guidelines (GWTG)-stroke, the West Virginia Office of Vital Statistics (WVOVS), and Center for Medicare and Medicaid Services (CMS). GWTG is a national hospital-based quality improvement program developed by the American Heart Association designed to serve as a regional and national database for stroke metrics. WVOVS and CMS report stroke-related discharges and mortality.
Statistical analysis: In addition to descriptive statistics, we used the Fisher's exact test to calculate the p-values for any statistically significant findings.
Results
Statewide GWTG data show that the numbers of AIS were 2,622, 2,453, 2,936, and 2,974 from 2015 to 2018, respectively. WVU Hospital's data show that the number of AIS treated at WVU was 819, 850, 857, and 816 from 2015 to 2018, respectively (Table 1).
Table 1.
Number of Acute Ischemic Strokes by Year
| YEAR | TOTAL ACUTE ISCHEMIC STROKES IN WV | ACUTE ISCHEMIC STROKES TREATED AT WVU HOSPITALS |
|---|---|---|
| 2015 | 2,622 | 819 |
| 2016 | 2,453 | 850 |
| 2017 | 2,936 | 857 |
| 2018 | 2,974 | 816 |
WV, West Virginia; WVU, West Virginia University.
Before 2016, telestroke was not utilized in WV, as there was previously no telestroke network for the state. After the establishment of WVU telestroke services, GWTG demonstrated increases in the total number of stroke patients receiving tPA across the state, with a 173% increase from 2015 (259 patients) to 2018 (448 patients) (p < 0.0001).
Consult volume within the WVU telestroke network for its eight spoke sites grew from year to year, with a 63% increase in consults from 2016 (187) to 2017 (304), and a 31% increase in consults from 2017 (304) to 2018 (399). Through June of 2019, there have been 244 telestroke consults received.
The proportion of triaged patients receiving tPA through telestroke also increased. Only 19% (35/187) of telestroke consults were treated with tPA in 2016 compared with 27% (107/399) in 2018 (p = 0.0384).
Among spoke sites, utilization of the WVU telestroke program varied considerably based on patient and emergency department (ED) volumes. Our spoke sites with the largest patient volumes, Berkeley Medical Center and Raleigh General Hospital, generated the highest number of consults, making up 33% and 28% of our consults, respectively (Table 2).
Table 2.
Spoke Site Consult and Emergency Department Volumes
| SPOKE SITE | % OF CONSULTS | ANNUAL ED VISITS |
|---|---|---|
| Berkeley Medical Center | 33 | >50,000 |
| Raleigh General Hospital | 28 | 40–50,000 |
| Camden Clark Medical Center | 13.5 | 40–50,000 |
| Garrett Regional Medical Center | 10 | 20–30,000 |
| Reynolds Memorial Hospital | 7 | <20,000 |
| Davis Medical Center | 3 | 20–30,000 |
| Potomac Valley Hospital | 2.5 | <20,000 |
| Fairmont Regional Medical Center | 2 | <20,000 |
ED, emergency department.
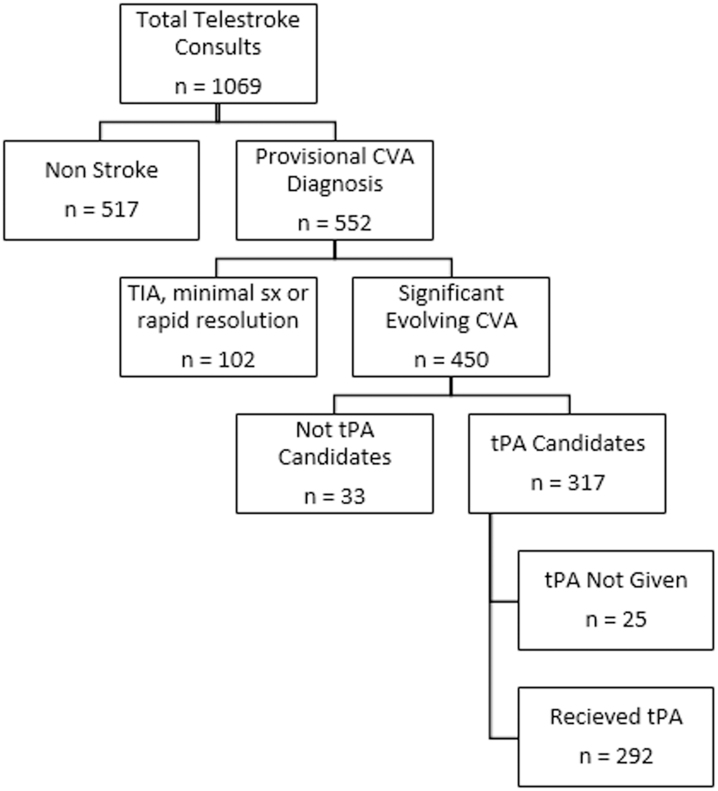
Since its inception in 2016, the WVU telestroke network has conducted a total of 1,069 audiovisual consults (Fig. 2). A total of 292 or 92% of tPA-eligible patients received IV-tPA with telestrokologist guidance. Twenty-five (7.8%) patients who were initially eligible did not receive tPA: 22 patients or families refused due to the risk of hemorrhage, and 3 patients changed their time last seen normal to outside the 4.5 h window after being counseled on the time-sensitive nature of thrombolytic therapy.
Fig. 2.
tPA eligibility of consults. CVA, cerebrovascular accident; TIA, transient ischemic attack; tPA, tissue plasminogen activator.
The primary reasons that tPA was not recommended during a consult were as follows: low likelihood of cerebrovascular ischemia (including unknown diagnoses), being outside the 4.5 h window for treatment, and mild or rapidly improving symptoms. Less common reasons included anticoagulation use, recent surgery, head trauma or stroke, confirmed intracranial or intra-abdominal bleeds upon presentation to the ED, and uncontrolled hypertension (Table 3).
Table 3.
Reasons Thrombolytic Therapy was Not Received
| REASON FOR NOT RECEIVING TPA | NO. OF PATIENTS | % OF TOTAL PATIENTS |
|---|---|---|
| Diagnosis unknown/not amenable to tPA | 517 | 48 |
| Outside of window for tPA | 110 | 10 |
| Rapidly improving symptoms | 84 | 8 |
| Anticoagulation/INR >1.7 | 18 | 1.6 |
| Recent surgery/head trauma/stroke | 10 | 0.9 |
| Bleeding upon presentation to ED | 10 | 0.9 |
| Hypertension | 3 | 0.3 |
INR, international normalized ratio; tPA, tissue plasminogen activator.
Telestroke was also shown to be effective in triaging AIS patients, potentially avoiding unwarranted transfer while expediting appropriate patients to EVT-capable centers. In 2016, 2017, and 2018, respectively, 60% (112/187), 62% (189/304), and 71% (284/399) of consulted patients remained locally through consensus between the ED provider and telestroke physician. In 2017, 37% (24/65) of EVT cases were transferred from an outside hospital. Of those, 41% (10/24) were a large vessel occlusion (LVO) patient transferred from a spoke site. In 2018, this proportion increased to 45% (13/29). Overall, the proportion of EVT cases performed in transferred patients remained the same at 41% (29/70).
A total of 292 patients received IV-tPA through telestrokologist guidance with minimal thrombolysis-related complications. Three (1%) symptomatic hemorrhagic transformations were observed, corresponding to our own hospital's low hemorrhagic transformation rate of 1%. One (0.3%) nonfatal asymptomatic intracerebral hemorrhage (ICH) was recorded in 2017. One episode of hemoptysis requiring reversal with cryoprecipitate and platelets occurred in 2017. Finally, one episode of epistaxis occurred in 2017, which was controlled with pressure. None of the patients treated with IV-tPA by telestroke expired during their subsequent admission. The overall mortality rate among AIS patients cared for at WVU in 2018 was 4.9% (40/816). Statewide mortality data were reported as 4.6% (135/2,936) in 2017 and 4.3% (129/2,974) in 2018.
Discussion
This study indicates that the adoption of telestroke in WV has improved the availability of stroke care to its rural population. Statewide data are most comprehensively tracked through GWTG. When cross-referencing GWTG data with Medicare and market sources, it represents 78% of all stroke patients cared for throughout the state. After the establishment of WVU's telestroke service in 2016, the GWTG data demonstrate a significant increase in the quantity of strokes evaluated and treated at rural hospitals in the state of WV. Statewide tPA use has increased by 173% since 2015 (259 patients to 448 in 2018, p < 0.0001). For the same time period, a parallel increase in consults received by the telestroke service was observed. Since its inception, our spoke–hub model has incorporated eight sites, and consult volume has more than doubled from 187 consults in 2016 to 399 in 2018. Telestroke consults made up 24% (107/448) of total statewide tPA administrations for 2018.
It appears that as the relationship between hub and spoke hospitals matures, AIS patients are triaged more efficiently and effectively. The proportion of telestroke patients who received tPA grew significantly, suggesting an improved ability of spoke sites to recognize a likely candidate, expedite a consult activation, and feel confident with the telestrokologist's assessments. In 2015, only 19% (35/187) of telestroke patients received tPA as compared with 27% (107/399) in 2018 (p = 0.0384). Although high-volume hospitals drove the majority of the utilization growth observed between 2016 and 2018, it is important to recognize that for many of our smaller spokes, telestroke was their main conduit to thrombolytic access. Before the telestroke partnership, tPA was not or rarely offered. As an illustration, one of our spoke sites did not carry tPA until they were incorporated into the telestroke network in 2016. This site has since generated 63 consults and administered tPA 20 times. The statistically significant increase in the proportion of consults treated with tPA for the same time course demonstrates the power of building effective relationships regardless of the consult volume at a particular spoke site.
Of the 1,069 total consults performed, 51% (552/1,069) were given a provisional diagnosis of cerebrovascular ischemia with 81% (450/552) classified as a significant evolving stroke. Seventy percent (317/450) were tPA candidates and the majority (92% or 282/317) received thrombolysis. Among tPA-eligible patients who were untreated, patient preference was most commonly cited as the reason (88% or 22/25).
Importantly, incorporating telestroke services to improve access to evaluation and treatment of AIS patients did not come at the expense of safety. No patients treated with tPA within the 4.5 h window through telestroke died during their subsequent admission. Between 2016 and 2018, only three symptomatic intracerebral hemorrhages (sICH as defined by Safe Implementation of Thrombolysis in Stroke-Monitoring Study criteria11) after tPA occurred. This corresponds to 1% (3/292) and is in line with our own hospital's low 1% rate of hemorrhagic transformation, both well below the Joint Commission's standard for comprehensive stroke centers of 5.7%. Three additional hemorrhagic complications were observed; one asymptomatic ICH and two nonfatal systemic bleeding events. Prior telestroke hemorrhagic complication rates have been difficult to interpret due to lack of standardized hemorrhagic transformation definition and paucity of prospective studies. A meta-analysis concluded that the safety of IV thrombolysis delivered through telestroke and certified stroke centers was comparable; however, the most recent referenced study was conducted in 2011, and the sICH rates varied between 1% and 8% in the tele sites.10
Rapidly improving access to a clinician with adequate training in recognizing various stroke subtleties is essential to increasing the number of AIS patients who receive appropriate acute stroke treatment. Adopting alternative strategies with standing protocols and NIHSS cutoffs are more vulnerable to inter-rater reliability when performed by providers who administer this examination infrequently.12 These challenges highlight the importance of a telestroke network beyond simply facilitating the administration of IV lytics. In addition, the telestrokologist provides another layer of patient triage. The decision to transfer a patient is a critical step in emergency care yet the factors and resources available are infrequently studied.13,14 Clinical evaluation through telestroke can assist in stratifying patients who are likely to be experiencing an LVO and can facilitate timely transfer to a center capable of EVT. The decision to transfer a patient is performed using a shared decision model between the telestrokologist, the local provider, and the patient or their families. In 2017, 10/24 (41%) of our yearly EVT cases were initially seen through teleconsultation and in 2018, 13/29 (45%) EVT patients originated from a spoke site. Typically, 60% of our EVT cases are from our in-house acute population. Inappropriate transfer of AIS patients to endovascular-capable centers is a large and costly burden on the already limited health care resources, especially when aeromedical transport is employed. Effective triage by coordinating care between strokologists and EM providers improves their ability to identify EVT candidates. Conversely, more non-EVT candidates are able to remain in their local hospital, thus reducing unnecessary transfers and associated expenses.15
Successful telestroke partnerships facilitate access for patients' families, reinforce the spoke site infrastructure, and contribute to the financial health of the community. In 2016, 2017, and 2018, our partner hospitals were able to care for their patients locally in 60% (112/187), 62% (189/304), and 71% (284/399) of consulted patients. Emphasizing telestroke's role in patient disposition based on shared decision making, treatment with IV-tPA did not translate into an automatic hub transfer. In 2016, 2017, and 2018, respectively, 62% (22/35), 64% (54/84), and 50% (54/107) of patients remained locally even after they had received thrombolysis.
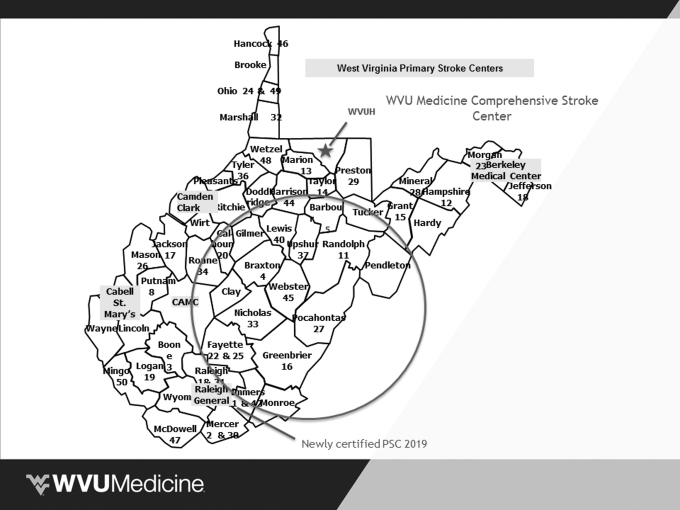
Telestroke is a key component of a successful stroke system of care and it should be a cornerstone of any future stroke network. Comprehensive stroke centers, already recognized for their expertise and dedication to stroke care, are a natural leader of such an initiative. Their purpose is multifold; not only do they increase the numbers of treated patients with AIS and allow them to stay in their communities when appropriate, but they also provide mentorship to health care providers locally. Over time, these partnerships between hub and spoke may lead to improved knowledge and care of AIS patients independent of telestrokologist input. A hub–spoke model is also an important opportunity to support affiliated hospitals in seeking and obtaining stroke center certification status. This year, one of our larger volume partners located in the heart of our state's stroke desert (Fig. 3) successfully achieved a primary stroke center designation.
Fig. 3.
West Virginia's primary stroke centers and stroke desert (stroke desert indicated by the circle). CAMC, Charleston Area Medical Center; PSC, primary stroke center; WVUH, West Virginia University Hospital.
In summary, our findings confirm that telestroke is a useful tool for evaluating and treating strokes, particularly those that happen far from stroke centers. Furthermore, it can be employed safely. As our program continues to grow, we aim to expand the network to include more overlap between WVU telestroke's area of service and the state's stroke care desert, thereby improving stroke care for our entire rural region. We are actively working with stakeholders throughout the state to develop a statewide telestroke solution; however, increasing the numbers of AIS patients treated acutely is only the first step in establishing an excellent stroke system of care. Further efforts must focus on improving individual outcomes and boosting stroke care locally.
It is important to note that this study has several limitations, including its retrospective nature and use of stroke registry data with a high risk of reporting bias. Cross-referencing the state stroke numbers with CMS data minimizes the risk of incomplete or inaccurate reporting. It is also likely that the increase in patients treated with tPA statewide is multifactorial and due to improved recognition of stroke symptoms by the public and emergency medical services as well as improved ED preparedness and quality of care with telestroke services. Lack of longer-term outcome data outside acute hospitalization or simple mortality or hemorrhagic complications after tPA hamper our ability to fully evaluate the impact of incorporating a telestroke network. Further efforts to systematically collect data regarding stroke care networks and analyze their efficacy are essential to continuing a successful system of care.
Acknowledgments
We thank Michelle Large and Kimberly Gordon for their assistance with data collection, analysis, and general efforts in supporting the telestroke center in West Virginia. We also thank Cynthia Keely for her assistance with the American Heart Association's Get With The Guidelines Stroke Database.
Disclosure Statement
No competing financial interests exist.
Funding Information
The project described was supported by the National Institute Of General Medical Sciences, U54GM104942-04. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
References
- 1. Benjamin EJ, Virani SS, Callaway CW, et al. Heart disease and stroke statistics-2018 update: A report from the American Heart Association. Circulation 2018;137:e67–e492 [DOI] [PubMed] [Google Scholar]
- 2. Stats of the State of West Virginia. 2019. Available at https://www.cdc.gov/nchs/pressroom/states/westvirginia.htm (last accessed August31, 2019).
- 3. Adams PF, Hendershot GE, Marano MA, Centers for Disease C, Prevention/National Center for Health Statistics. Current estimates from the National Health Interview Survey, 1996. Vital Health Stat 10 1999;1–203 [PubMed] [Google Scholar]
- 4. Albright KC, Branas CC, Meyer BC, et al. ACCESS: Acute cerebrovascular care in emergency stroke systems. Arch Neurol 2010;67:1210–1218 [DOI] [PubMed] [Google Scholar]
- 5. Aguiar de Sousa D, von Martial R, Abilleira S, et al. Access to and delivery of acute ischaemic stroke treatments: A survey of national scientific societies and stroke experts in 44 European countries. Eur Stroke J 2018;4:13–28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Brown DL, Barsan WG, Lisabeth LD, Gallery ME, Morgenstern LB. Survey of emergency physicians about recombinant tissue plasminogen activator for acute ischemic stroke. Ann Emerg Med 2005;46:56–60 [DOI] [PubMed] [Google Scholar]
- 7. Meurer WJ, Majersik JJ, Frederiksen SM, Kade AM, Sandretto AM, Scott PA. Provider perceptions of barriers to the emergency use of tPA for acute ischemic stroke: A qualitative study. BMC Emerg Med 2011;11:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Rural health for West Virginia Introduction—Rural Health Information Hub. 2019. Available at https://www.ruralhealthinfo.org/states/west-virginia (last accessed April2, 2019).
- 9. AAMC. West Virginia physician workforce profile. 2017. Available at https://www.aamc.org/download/484606/data/westvirginiaprofile.pdf (last accessed March14, 2019).
- 10. Kepplinger J, Barlinn K, Deckert S, Scheibe M, Bodechtel U, Schmitt J. Safety and efficacy of thrombolysis in telestroke: A systematic review and meta-analysis. Neurology 2016;87:1344–1351 [DOI] [PubMed] [Google Scholar]
- 11. Wahlgren N, Ahmed N, Davalos A, et al. Thrombolysis with alteplase for acute ischaemic stroke in the Safe Implementation of Thrombolysis in Stroke-Monitoring Study (SITS-MOST): An observational study. Lancet 2007;369:275–282 [DOI] [PubMed] [Google Scholar]
- 12. Meyer BC, Lyden PD. The modified National Institutes of Health Stroke Scale: Its time has come. Int J Stroke 2009;4:267–273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sorensen MJ, von Recklinghausen FM, Fulton G, Burchard KW. Secondary overtriage: The burden of unnecessary interfacility transfers in a rural trauma system. JAMA Surgery 2013;148:763–768 [DOI] [PubMed] [Google Scholar]
- 14. Rourke JT, Kennard M. Emergency patient transfers from rural hospitals: A regional study. CJEM 2001;3:296–301 [DOI] [PubMed] [Google Scholar]
- 15. Sequeira D, Martin-Gill C, Kesinger MR, et al. Characterizing strokes and stroke mimics transported by helicopter emergency medical services. Prehosp Emerg Care 2016;20:723–728 [DOI] [PubMed] [Google Scholar]