Highlights
-
•
Maternal depression and anxiety prevalence rates appear elevated during COVID-19.
-
•
Risk factors for depression and anxiety were evaluated based on child age ranges.
-
•
Prior psychopathology, poor marital quality, and financial strain affected risk.
-
•
Mothers primarily obtained mental health information through online resources.
Keywords: Depression, Anxiety, Maternal, Mental health services, COVID-19
Abstract
Background
Mental health problems are increasingly recognized as a significant and concerning secondary effect of the COVID-19 pandemic. Research on previous epidemics/pandemics suggest that families, particularly mothers, may be at increased risk, but this population has yet to be examined. The current study (1) described prevalence rates of maternal depressive and anxiety symptoms from an online convenience sample during the COVID-19 pandemic, (2) identified risk and protective factors for elevated symptoms, and (3) described current mental health service use and barriers.
Methods
Participants (N = 641) were mothers of children age 0–8 years, including expectant mothers. Mothers completed an online survey assessing mental health, sociodemographic information, and COVID-19-related variables.
Results
Clinically-relevant depression was indicated in 33.16%, 42.55%, and 43.37% of mothers of children age 0–18 months, 18 months to 4 years, and 5 to 8 years, respectively. Prevalence of anxiety was 36.27%, 32.62%, and 29.59% for mothers across age groups, respectively. Binary logistic regressions indicated significant associations between risk factors and depression/anxiety across child age groups.
Limitations
Cross-sectional data was used to describe maternal mental health problems during COVID-19 limiting the ability to make inferences about the long-term impact of maternal depression and anxiety on family well-being.
Conclusions
Maternal depression and anxiety appear to be elevated in the context of COVID-19 compared to previously reported population norms. Identified risk factors for depression and anxiety across different child age ranges can inform targeted early intervention strategies to prevent long-term impacts of the COVID-19 pandemic on family well-being and child development.
Introduction
The coronavirus disease (COVID-19) pandemic has impacted 1.38 billion children worldwide due to closures to schools, daycares, extracurricular programs, and outdoor recreational spaces (Cluver et al., 2020; World Health Organization, 2020). Parents are similarly affected, with many experiencing changes to income, employment, and childcare needs (Statistics Canada, 2020). As a result, families are facing numerous psychological and socioeconomic stressors that are commonly associated with increased parental mental health needs (Wachs et al., 2009). Maternal mental health is particularly important to consider, given that females are at increased risk for depression and anxiety (American Psychiatric Association, 2013). Similarly, suicide is a leading cause of death in mothers of young children in non-pandemic populations (Rahman et al., 2013). Thus, in addition to the physical health impacts of COVID-19, the psychological and socioeconomic impacts of the pandemic and COVID-related measures should be examined to allow for the effective development and implementation of targeted prevention and intervention strategies.
As a result of the measures implemented to halt the transmission of COVID-19, millions of families have experienced significant changes to their social functioning through self-isolation, physical distancing, or additional restrictions on social interactions. In many cases, this change in functioning has resulted in increased interactions between household family members, given many families are isolating together. Family systems have also seen an abrupt shift in daily functioning through a blending of parental work and parenting duties due to closures of schools and daycares as well as work-from-home initiatives implemented for several non-essential services/businesses. While children are no longer attending school in-person, many schools and classroom teachers have adapted the curriculum for online-delivery resulting in increased parental support for learning. These challenges are further exacerbated by the financial burden of COVID-19-related loss of employment, reduced pay, or decreased food security for some families.
COVID-19-related measures are expected to have widespread impacts on family psychosocial functioning. These measures may increase risk for maternal depression given established risk factors for depression onset, including high levels of economic stress, relationship distress and conflict, lower social support, greater number of young children, and children with increased needs (Gelaye et al., 2016; Rahman et al., 2013; Wachs et al., 2009). Maternal depression is associated with harsh or punitive parenting (Wolford et al., 2019) and disruptions in maternal-child attachment (Martins and Gaffan, 2000). Exposure to maternal depression also puts children at greater risk for internalizing and externalizing problems, cognitive and motor developmental delays, and low academic achievement (Wachs et al., 2009). Given the increase in possible exposure to maternal depression under the COVID-19 conditions, children may be at an exponential risk for these negative outcomes related to maternal depression.
The potential impacts of the COVID-19 pandemic on family mental health may be better understood by examining more recent epidemics/pandemics. Such examples include the severe acute respiratory syndrome (SARS) epidemic, the Middle East respiratory syndrome coronavirus (MERS-CoV) epidemic, and the A(H1N1)pdm09 virus (commonly known as the H1N1 influenza virus) pandemic. Self-isolation during epidemics/pandemics has been associated with fear-related adverse psychological outcomes (Brooks et al., 2020), anger and anxiety symptoms several months post-quarantine (Jeong et al., 2016; Mihashi et al., 2009), and four times the risk of post-traumatic stress symptoms in parents and their children (Sprang and Silman, 2013). Pregnant females experience an increased concern surrounding the acquisition or transmission of a virus (Braunack-Mayer et al., 2013). Similarly, preliminary research on COVID-19 indicates a significant increase in psychological distress for expectant mothers (Lebel et al., 2020). Yet, some research has also suggested that family functioning improved in some ways as a result of self-isolation, including increased social support from family members when in need, sharing of emotions within the family, and compassion for family members’ feelings (Lau et al., 2006). Moreover, having more than two children may be protective for maternal mental health during an epidemic (Hawryluck et al., 2004). Given the long-term effects untreated impaired maternal mental health has on child health and development, it is imperative that risk and resilience factors for mental distress are identified during the current pandemic to inform early intervention strategies to promote healthy family functioning (Leis et al., 2014).
Extant literature highlights the urgency to identify risk and protective factors for mothers and families during the COVID-19 pandemic. Home confinement and reduced access to schools and social services will inevitably diminish the accessibility of direct patient encounters in clinical practice resulting in increased vulnerability for families with significant mental health needs (Pfefferbaum and North, 2020). As such, risk and protective factors for maternal mental health along with the accessibility of mental health services should be investigated to promote family well-being during and following the COVID-19 pandemic.
Thus, the primary aim of the current study was to describe prevalence rates of maternal anxiety and depression and investigate factors that affect risk for clinically-relevant symptoms. The secondary aim was to describe maternal use of mental health services and the unmet needs of mothers experiencing mental health distress during the COVID-19 pandemic by evaluating barriers faced when accessing mental health services.
Methods
Participants
Between April 14, 2020 and April 28, 2020, a convenience sample was recruited through online advertisements and poster sharing on social media platforms (e.g., Twitter, Facebook, Instagram, Reddit, Craigslist, Kijiji) as well as through invitation from previous study participation with consent for future contact to uphold physical distancing measures implemented during the pandemic. Participants were also recruited indirectly through knowledge translation mediums, such as media interviews (e.g., CBC Winnipeg, New York Times) and commentary articles (e.g., Conversation Canada). Parents over the age of 18 years who were either pregnant or had a child 0–8 years old were eligible to participate. At the time of the current study, the vast majority (n = 641/728; 88.05%) of participants identified as mothers (e.g., biological mother, step-mother, adoptive mothers); thus, only maternal data was utilized to provide a cohesive understanding of maternal mental health and mental health service use during the pandemic.
Procedure
Informed consent was obtained before online survey completion using REDCap electronic data capture tools hosted at the University of Manitoba (Harris et al., 2009). All participants who completed the survey were entered into a draw to win one of five $100/CAD electronic gift certificates. The study protocol was approved by the University of Manitoba Research Ethics Board.
Measures
Sociodemographic information
Mothers were asked to specify family sociodemographic information (e.g., maternal age, marital status, maternal/partner education, annual household income, location of residence at the time of survey completion). Employment and financial information was also collected, including household employment status or changes during the COVID-19 pandemic, the likelihood of applying for federal benefits, and the extent of financial strain endured by COVID-19 measured as the ability to cover unexpected expenses during the pandemic, where higher scores indicated greater difficulty. Of note, employment status/changes and application for federal benefits was framed to encompass both the individual as well as the household more broadly (e.g., “Have you or someone in your household been laid off or lost hours due to the COVID-19 outbreak?”).
COVID-19
Participants were also asked COVID-19 specific questions including known exposure or vulnerability to COVID-19, whether members in the household were practicing physical distancing, and the extent to which members of the household were leaving to use essential/non-essential services.1
Adult mental health disorder checklist (AMHDC)
The AMHDC was created to identify the frequency of maternal mental health diagnoses through self-report. For each mental health disorder, participants indicated whether they had received a diagnosis or treatment for the disorder in the past month (=3), 2 to 12 months ago (=2), 1+ years ago (=1), or never (=0). Prior research supports the use of self-reported mental health diagnoses, such as depression, showing adequate validity compared to physician diagnosis (Sanchez-Villegas et al., 2008).
The center for epidemiologic studies depression (CESD) and - Revised (CESD-R)
Mothers of children between 1.5–8 years of age completed the 20-item CESD (n = 75) (Radloff, 1977) or the CESD-R (n = 204) (Eaton et al., 2004) to assess the presence and frequency of depressive symptoms during the past week. The first 351 surveys contained the CESD while subsequent surveys contained the CESD-R. The CESD and CESD-R have been shown to have a similar two week to one-year test-retest reliability between 0.40 and 0.70 (Eaton et al., 2004). Both measures were scored using the original CESD Likert scale and summative score ranges (Eaton et al., 2004). While the self-report measure does not equate to a clinical diagnosis, the clinical cut-off score of ≥ 16 indicates optimal specificity for identifying a depressive case (Eaton et al., 2004; Radloff, 1977). Internal consistency was good to excellent in the current study (CESD: α = 0.88; CESD-R: α = 0.94). The scales will be referred to as the CESD hereafter.
Edinburgh postnatal depression scale (EPDS)
Mothers of children age 0–1.5 years completed the 10-item EPDS (Cox et al., 1987) to identify depression during pregnancy and the postpartum period. EPDS items were scored on a four-point Likert scale with higher total scores indicating increasing depressive symptoms. A clinical cut-off score of ≥ 13 identifies scores consistent with major depressive disorder, although the self-report measure does not replace a clinical diagnosis (Cox et al., 1987). Internal consistency was good in the current study (α = 0.88).
Generalized anxiety disorder 7-item scale (GAD-7)
The seven-item GAD-7 (Spitzer et al., 2006) was used to assess symptoms of maternal anxiety in mothers of children age 1.5–8 years old. GAD-7 items were scored on a scale ranging from not at all sure to nearly every day, with higher scores indicating higher levels of anxiety. Anxiety is indicated above a clinical cut-off score of ≥ 10 on the GAD-7 (Spitzer et al., 2006). Internal consistency in the current study was excellent (α = 0.92).
Perinatal anxiety screening scale (PASS)
Mothers of children aged 0–1.5 years completed the 31-item PASS (Somerville et al., 2014). The PASS measures maternal anxiety during pregnancy and the postpartum period. Items are scored on a three-point scale ranging from not at all to almost always. Elevated anxiety on the PASS was defined using a clinical cut-off score of ≥ 26 (Somerville et al., 2014). Cronbach's alpha in the current study indicated excellent internal consistency (α = 0.95).
Multidimensional scale of perceived social support (MSPSS)
The MSPSS is a 12-item questionnaire used to measure perceived social support (Zimet et al., 1988). The scale is comprised of three social support subscales: family, friends, and significant others. Items are scored on a seven-point Likert scale ranging from very strongly disagree to very strongly agree, with higher total scores indicating higher perceived social support. Cronbach's alpha in the current study indicated excellent internal consistency (α = 0.97).
Revised dyadic adjustment scale (RDAS)
The 14-item RDAS (Busby et al., 1995) is a brief assessment of marital quality that consists of three subscales: dyadic consensus, dyadic satisfaction, and dyadic cohesion. The RDAS assesses relationship strain and adjustment with items scored on a five-point scale, with lower scores indicating greater relationship distress (Busby et al., 1995). Internal consistency for the total scale was good (α = 0.86), while the subscales demonstrated acceptable internal consistency (α = 0.78–0.80).
Recent stressful experiences (RSE)
The author-compiled RSE was developed as a result of recommendations from the JBP research network on toxic stress at the Harvard's Center on the Developing Child. The RSE was used to assess presence of recent family stressors within the past month and past two to twelve months. The current study used the term “RSE past month” to describe presence of events in the past month and “RSE past year” to describe presence of events in the past two to twelve months.
Mental health services use
Author-compiled measures were developed to evaluate families’ mental health service use in the past month in terms of the number of days per month that the services were accessed and the average time spent accessing the service. Mental health service use assessed via the author-compiled Mental Health Service Use Questionnaire included: virtual or in-person individual/group counselling, instant messaging mental health services, mental health crisis line use, seeking mental health information online, well-being phone applications, faith-based counselling services with religious leaders, or an 'other' option where participants were given the option to include any mental health services unaccounted for in the above options. If no service was accessed, mothers were asked to identify reasons why the services were not accessed from multiple choice responses (e.g., “too costly” and “do not believe services would help”).
Statistical analysis
All analyses were conducted using IBM SPSS Statistics Version 25. Little's Missing Completely at Random (MCAR) test indicated that CESD (χ2 = 206.88, p = .489), EPDS (χ2 = 31.30, p = .259), GAD-7 (χ2 = 42.48, p = .065), and PASS (χ2 = 456.00, p = .313) data were completely missing at random. Analyses were conducted across three child age ranges: pregnancy to <18 months postpartum, 18 months old to four years old, and five years old to eight years old. Mothers who identified as a parent of at least one child in an age group were included in the analyses for that age group. As such, mothers were included in at least one age group (as per study inclusion) and up to three categories if they had a child meeting each age range. Descriptive analyses were conducted to identify prevalence rates of depression (CESD, EPDS) and anxiety (GAD-7, PASS). Depressive and anxiety symptoms above and below cut-off scores on each measure were recoded into dichotomous measures indicating depression and anxiety, respectively. Bivariate correlations were conducted to identify relationships between variables. Binomial logistic regression was then conducted to examine if significant bivariate sociodemographic and COVID-19-related variables affected risk for maternal depression and anxiety. Binomial logistic regression models were also evaluated for mental health service use.
Results
Participant characteristics
On average, mothers (N = 641) were 34.27 years old (SD = 5.02; range = 21 - 48). Mothers were categorized based on having at least one child age < 18 months (n = 267), 18 months to <5 years (n = 388), and 5 to < 8 years old (n = 273). On average, households consisted of 2.02 (SD = 0.42) adults and 1.79 (SD = 0.81) children; 6.10% of mothers reported being a single-adult household. The vast majority of participants were married or common-law (91.50%), had at least a bachelor's degree (71.47%), and were residing in Canada at the time of survey completion (88.46%). Participants were primarily residing in the Canadian cities of Winnipeg (39.78%), Toronto (5.46%), and Calgary (4.84%). Participants were also from the United States (9.20%) or international countries (2.34%). The majority of mothers (56.05%) reported an annual income of > $100,000. Most participants (99.84%) had not experienced a diagnosis of COVID-19 within their immediate household; however, 21.72% indicated that they knew someone personally who had been diagnosed with COVID-19 of which 24.64% were hospitalized and 66.18% had recovered at the time of survey completion (Table 1 ).
Table 1.
Characteristics of the sample.
| Characteristic | % | Valid N |
|---|---|---|
| Maternal Education Level | 638 | |
| Some high school | 0.63 | |
| High school diploma or equivalent | 8.15 | |
| College/Technical School | 19.75 | |
| Bachelor's degree | 31.82 | |
| Above bachelor's degree | 39.66 | |
| Partner Education Level | 599 | |
| Some high school | 1.84 | |
| High school diploma or equivalent | 14.69 | |
| College/Technical School | 28.55 | |
| Bachelor's degree | 29.05 | |
| Above bachelor's degree | 25.88 | |
| Household Employment Status during COVID-19 | 597 | |
| Hours consistent | 43.05 | |
| More than half of regular hours | 10.89 | |
| Less than half of regular hours | 9.05 | |
| Laid off | 16.25 | |
| Salaried | 20.77 | |
| Total Annual Household Income | 603 | |
| ≤ $20,000 | 2.16 | |
| $20,001 - $40,000 | 5.31 | |
| $40,001 - $60,000 | 8.62 | |
| $60,001 - $80,000 | 12.27 | |
| $80,001 - $100,000 | 15.59 | |
| >$100,000 | 56.05 | |
| Marital Status | 635 | |
| Married/Common Law | 91.50 | |
| Divorced/Separated | 3.46 | |
| Single (never married) | 5.04 | |
| Number of children | 641 | |
| 0 | 0.47 | |
| 1 | 39.00 | |
| 2 | 46.33 | |
| 3+ | 14.20 | |
| Currently Pregnant | 51 | |
| First-time parent | 5.88 | |
| Experienced parent | 94.12 | |
| Pregnancy Trimester | 49 | |
| First | 12.24 | |
| Second | 46.94 | |
| Third | 40.82 | |
| Previous Maternal Mental Health Diagnosis/Treatment | 51.52 | 427 |
| Apply for Federal Insurance Benefits | 629 | |
| Extremely likely | 19.55 | |
| Likely | 9.54 | |
| Neutral | 10.33 | |
| Unlikely | 28.46 | |
| Extremely unlikely | 32.11 | |
| Mother in a Vulnerable Population | 633 | |
| Underlying medical condition | 7.11 | |
| Compromised immune system | 5.21 | |
| Partner in a Vulnerable Population | 634 | |
| Underlying medical condition | 5.68 | |
| Compromised immune system | 1.89 | |
| Child in a Vulnerable Population | 636 | |
| Underlying medical condition | 7.55 | |
| Compromised immune system | 2.83 | |
| Medical Services Impacted by COVID-19 | 43.38 | 634 |
| Racial/Ethnic Minority Background | 16.17 | 402 |
Of the mothers included in the study, 72.70% completed the mental health questionnaires (i.e., EPDS/CESD, GAD-7/PASS). A comparison of mothers who did and did not complete mental health questionnaires revealed no significant differences in maternal education (χ2 = 6.04, p = .419), partner education (χ2 = 3.63, p = .726), maternal age (t(638) = −1.29, p = .197), household income (χ2 = 15.83, p = .324), number of children in household (χ2 = 7.37, p = .288), employment loss (χ2 = 0.038, p = .845), or likelihood of applying for federal benefits (χ2 = 4.03, p = .402). Rates of depression and anxiety did not differ by country of residence (p = .550 and 0.587, respectively).
Social and economic impact of COVID-19
Nearly all mothers (99.53%) were currently practicing physical distancing. A total of 94.99% of participants reported a household member leaving for essential services, which typically occurred once per week (53.62%). Only 13.79% reported leaving their home for non-essential services. Over one-third of mothers (38.62%) indicated current financial strain, which was over-represented among those in lower income households (p < .001). A minority of mothers reported that they or someone in the household had been laid off (16.25%) or lost at least half of their regular work hours as a result of the pandemic (9.05%).
Prevalence of maternal depression
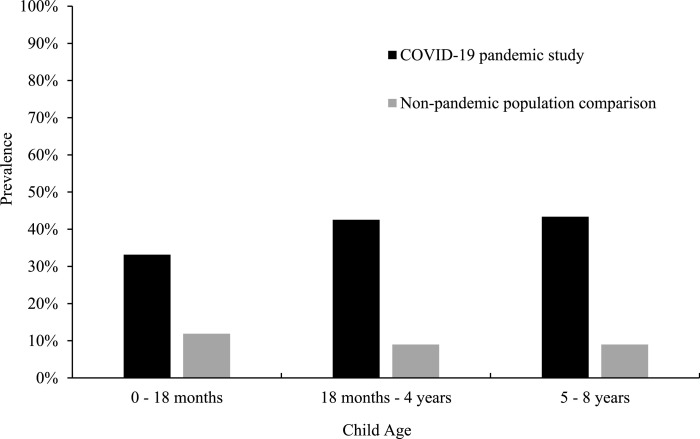
Average self-reported depressive symptoms were M = 9.79 (SD = 5.31) and M = 16.86 (SD = 12.35) on the EPDS (n = 186) and CESD (n = 279), respectively. In the full sample, 41.51% (N = 465) of mothers met the clinical cut-off scores of ≥ 13 for EPDS and ≥ 16 for CESD indicating depression. Of the mothers (n = 193) with a child aged 0 to 18 months, average scores were M = 9.79 (SD = 5.31) and M = 16.71 (SD = 20.30) on the EPDS (n = 186) and CESD (n = 7), respectively; 33.16% (n = 64) of these mothers met the cut-off scores for depression. Mothers (n = 282) of children age 18 months to 4 years reported average symptoms of M = 9.93 (SD = 5.42) on the EPDS (n = 100) and M = 16.66 (SD = 11.92) on the CESD (n = 182). Of these mothers, 42.55% (n = 120) scored above the cut-off scores for depression. Similarly, mothers (n = 196) of children aged 5 to 8 years old reported average symptoms of M = 9.89 (SD = 4.85) on the EPDS (n = 35) and M = 16.63 (SD = 12.81) on the CESD (n = 161). A total of 43.37% (n = 85) met clinical cut-off scores for depression. Study prevalence compared to pre-pandemic population norms (Letourneau et al., 2013; Woody et al., 2017) can be seen in Fig. 1 .
Fig. 1.
Prevalence rates of maternal depression stratified across child age groups with population comparisons.
Correlates of maternal depression
Associations between sociodemographic and pandemic-related variables of interest are reported in Table 2a -b by child age group. For mothers of children 0 to 18 months, depression was associated with previous mental health history, lower maternal and partner education, lower household income, presence of employment loss and/or financial strain, higher RSE past month, lower MSPSS, and lower RDAS total and subscales. For mothers of children 18 months to 4 years old, maternal depression was positively associated with mental health history, employment loss, financial strain, RSE past month, and RSE past year and negatively correlated with household income, MSPSS, RDAS total, and RDAS satisfaction and cohesion subscales. Maternal depression was associated with previous mental health history, greater RSE past month and past year, lower MSPSS, and lower RDAS total and subscales for mothers of children aged 5 to 8 years. All significant predictors of depression at the bivariate level were included in subsequent inferential analyses.
Table 2a.
Bivariate correlations of sociodemographic and predictor variables for mothers with children age 0 to 18 months and 18 months to 4 years.
| Measure | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Depression | – | .546⁎⁎ | .405⁎⁎ | −0.202⁎⁎ | −0.242⁎⁎ | −0.221⁎⁎ | −0.288⁎⁎ | −0.098 | .174⁎⁎ | .176⁎⁎ | .125* | .155⁎⁎ | −0.083 | −0.015 | −0.044 | −0.115 | −0.064 | −0.131* |
| 2. Anxiety | .633⁎⁎ | – | .354⁎⁎ | −0.080 | −0.112 | −0.048 | −0.245⁎⁎ | −0.010 | .157⁎⁎ | .090 | .103 | .190⁎⁎ | −0.137* | .065 | −0.066 | −0.077 | −0.068 | −0.007 |
| 3. Mental health history | .240⁎⁎ | .208⁎⁎ | – | −0.081 | −0.166* | −0.128 | −0.223⁎⁎ | −0.073 | .142* | .154* | .144* | .085 | −0.056 | −0.005 | .071 | −0.148* | −0.123 | −0.080 |
| 4. MSPSS | −0.210⁎⁎ | −0.182* | −0.079 | – | .198⁎⁎ | .117 | .123 | .199⁎⁎ | −0.176⁎⁎ | −0.049 | −0.069 | −0.044 | .009 | .076 | −0.035 | −0.006 | −0.001 | .084 |
| 5. RDAS total | −0.302⁎⁎ | −0.213⁎⁎ | −0.134 | .222⁎⁎ | – | .767⁎⁎ | .807⁎⁎ | .829⁎⁎ | −0.079 | −0.114 | −0.030 | −0.077 | −0.063 | .154* | .066 | .017 | .186⁎⁎ | .013 |
| 6. RDAS cohesion | −0.161* | −0.070 | −0.110 | .151 | .814⁎⁎ | – | .503⁎⁎ | .375⁎⁎ | −0.014 | −0.129 | −0.026 | .016 | −0.128 | .114 | .004 | −0.033 | .102 | −0.013 |
| 7. RDAS satisfaction | −0.312⁎⁎ | −0.340⁎⁎ | −0.207* | .218⁎⁎ | .799⁎⁎ | .470⁎⁎ | – | .532⁎⁎ | −0.141* | −0.077 | −0.032 | −0.120 | −0.003 | .196⁎⁎ | .063 | .075 | .230⁎⁎ | .118 |
| 8. RDAS consensus | −0.261⁎⁎ | −0.152 | −0.060 | .149 | .838⁎⁎ | .485⁎⁎ | .572⁎⁎ | – | −0.048 | −0.053 | −0.028 | −0.089 | −0.007 | .100 | .085 | .026 | .153* | −0.035 |
| 9. RSE past month | .237⁎⁎ | .208⁎⁎ | .212⁎⁎ | −0.157* | −0.193* | −0.094 | −0.273⁎⁎ | −0.077 | – | .472⁎⁎ | .337⁎⁎ | .207⁎⁎ | −0.156⁎⁎ | −0.272⁎⁎ | −0.034 | −0.138⁎⁎ | −0.082 | −0.233⁎⁎ |
| 10. RSE past year | .110 | .065 | .146 | −0.037 | −0.024 | −0.078 | −0.062 | .093 | .415⁎⁎ | – | .153⁎⁎ | .101* | −0.131⁎⁎ | −0.153⁎⁎ | −0.062 | −0.069 | −0.090 | −0.180⁎⁎ |
| 11. Employment Loss | .160* | .070 | .230⁎⁎ | −0.147* | −0.101 | −0.086 | −0.092 | −0.051 | .384⁎⁎ | .060 | – | .223⁎⁎ | −0.130* | −0.065 | .098 | −0.140⁎⁎ | −0.133* | −0.253⁎⁎ |
| 12. Financial Strain | .239⁎⁎ | .314⁎⁎ | .000 | −0.181⁎⁎ | −0.044 | −0.013 | −0.035 | −0.026 | .167⁎⁎ | .171⁎⁎ | .176⁎⁎ | – | −0.064 | −0.170⁎⁎ | .005 | −0.116* | −0.194⁎⁎ | −0.301⁎⁎ |
| 13. Maternal Age | −0.131 | −0.074 | −0.078 | .077 | .035 | −0.013 | .131 | −0.015 | −0.145* | −0.163⁎⁎ | −0.057 | −0.211⁎⁎ | – | .038 | −0.003 | .437⁎⁎ | .296⁎⁎ | .373⁎⁎ |
| 14. Marital Status | .001 | .046 | −0.012 | .095 | .149 | .078 | .157 | .159 | −0.228⁎⁎ | −0.202⁎⁎ | −0.064 | −0.187⁎⁎ | .103 | – | .044 | .090 | .044 | .313⁎⁎ |
| 15. Parity | .062 | .000 | .084 | −0.189⁎⁎ | −0.139 | −0.053 | −0.132 | −0.106 | .057 | −0.098 | .029 | −0.007 | .066 | .009 | – | −0.121* | −0.129* | −0.037 |
| 16. Maternal Education | −0.251⁎⁎ | −0.113 | −0.097 | .229⁎⁎ | .147 | .060 | .179* | .082 | −0.191⁎⁎ | −0.112 | −0.207⁎⁎ | −0.217⁎⁎ | .416⁎⁎ | .090 | −0.184⁎⁎ | – | .566⁎⁎ | .299⁎⁎ |
| 17. Partner Education | −0.190⁎⁎ | −0.163* | −0.138 | .159* | .247⁎⁎ | .154 | .293⁎⁎ | .185* | −0.136* | −0.080 | −0.131* | −0.263⁎⁎ | .278⁎⁎ | .006 | −0.188⁎⁎ | .596⁎⁎ | – | .272⁎⁎ |
| 18. Household Income | −0.265⁎⁎ | −0.195⁎⁎ | −0.222⁎⁎ | .216⁎⁎ | .239⁎⁎ | .100 | .305⁎⁎ | .166* | −0.347⁎⁎ | −0.195⁎⁎ | −0.218⁎⁎ | −0.440⁎⁎ | .381⁎⁎ | .290⁎⁎ | −0.100 | .371⁎⁎ | .344⁎⁎ | – |
Note. Below diagonal = age 0 to 18 months, Above diagonal = age 18 month to 4 years; *p ≤ 0.05, **p ≤ 0.01.
Abbreviations: MSPSS = Multidimensional Scale of Perceived Social Support; RDAS = Revised Dyadic Adjustment Scale; RSE = Recent Stressful Events.
Block-wise logistic regressions were conducted by each child age group with mental health history (block 1) and sociodemographic predictors (block 2). Sociodemographic predictors that contributed to depression over and above the variance accounted for by mental health history were included in the final model with pandemic-related factors (block 3; Table 3). For mothers of children age 0 to 18 months, marital quality (OR = 0.94, 95% Confidence Interval (CI) [0.89, 0.99], p = .031) was a significant protective factor from depression, while greater RSE past month (OR = 1.76, 95% CI [1.03, 2.99], p = .038) was a significant risk factor for maternal depression. Mental health history was the only significant predictor for mothers of children 18 months to 4 years old, such that previous mental health history increased risk for depression (OR = 5.16, 95% CI [2.63, 10.11], p < .001). For mothers of children age 5 to 8 years, mental health history (OR = 4.39, 95% CI [1.85, 10.44], p = .001) and marital quality (OR = 0.90, 95% CI [0.85, 0.96], p = .001) were positively and negatively associated with odds of maternal depression, respectively.
Table 3.
Binary logistic regression for maternal depression in final models (block 3).
| Predictor Variable |
0 to 18 months |
18 months to 4 years |
5 to 8 years |
||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | |
| History of mental health | 2.12 | 0.96, 4.70 | .064 | 5.16 | 2.63, 10.11 | <0.001 | 4.39 | 1.85, 10.44 | .001 |
| MSPSS | 0.98 | 0.96, 1.01 | .200 | 0.99 | 0.98, 1.01 | .565 | 1.00 | 0.98, 1.03 | .988 |
| RDAS | 0.94 | 0.89, 0.99 | .031 | 0.96 | 0.93, 1.00 | .063 | 0.90 | 0.85, 0.96 | .001 |
| RSE past month | 1.76 | 1.03, 2.99 | .038 | 1.06 | 0.64, 1.77 | .824 | 1.52 | 0.86, 2.69 | .147 |
| RSE past year | – | – | – | 1.33 | 0.96, 1.86 | .089 | 1.23 | 0.77, 1.96 | .385 |
Note. Abbreviations: MSPSS = Multidimensional Scale of Perceived Support; RDAS = Revised Dyadic Adjustment Scale; RSE = Recent Stressful Events.
Prevalence of maternal anxiety
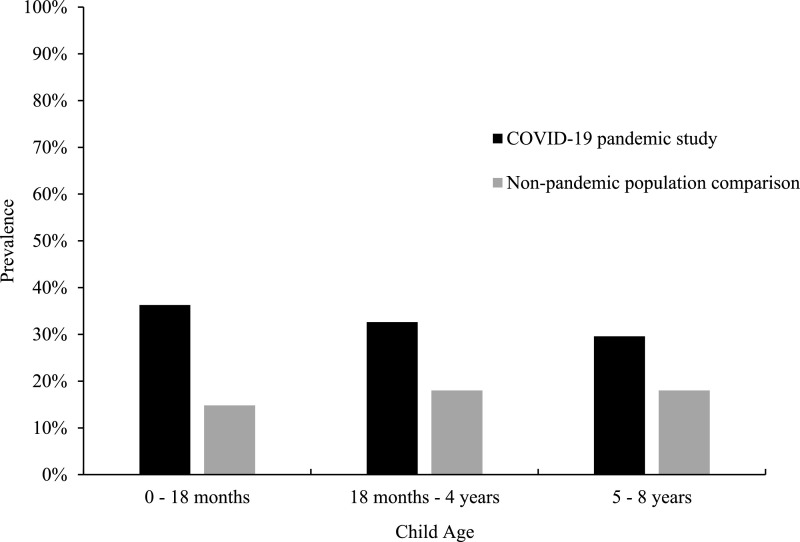
On average, anxiety symptoms were M = 7.31 (SD = 5.92) on the GAD-7 (n = 279) and M = 21.79 (SD = 15.88) on the PASS (n = 186) for all mothers. In the total sample, 32.69% (N = 465) met clinical cut-off scores of ≥ 10 for GAD-7 and ≥ 26 for PASS indicating clinically-relevant anxiety. Mothers of children age 0 to 18 months (n = 193) reported average scores of M = 8.55 (SD = 9.31) on the GAD-7 (n = 7) and M = 21.79 (SD = 15.88) on the PASS (n = 186). Over one third (36.27%, n = 70) of these mothers scored above the clinical cut-off scores for anxiety. For mothers (n = 282) of children age 18 months to 4 years, average anxiety symptoms were reported to be M = 7.45 (SD = 6.00) on the GAD-7 (n = 182) and M = 22.30 (SD = 15.88) on the PASS (n = 100). One third (32.62%; n = 92) of these mothers met clinical cut-off scores for anxiety. Similarly, mothers (n = 196) of children aged 5 to 8 years old reported average symptoms of M = 6.96 (SD = 5.84) on the GAD-7 (n = 161) and M = 20.06 (SD = 14.68) on the PASS (n = 35). A total of 29.59% (n = 58) of these mothers met clinical cut-off scores for anxiety. Study prevalence compared to pre-pandemic population norms (Clavarino et al., 2010; Dennis et al., 2017) can be seen in Fig. 2 .
Fig. 2.
Prevalence rates of maternal anxiety stratified across child age groups with population comparisons.
Correlates of maternal anxiety
For mothers of children 0 to 18 months, anxiety was significantly correlated with a significant mental health history, greater financial strain, lower partner education, lower household income, lower MSPSS, lower RDAS total and satisfaction subscale, and greater RSE past month (Table 2a). For mothers of children 18 months to 4 years old, maternal anxiety was similarly associated with mental health history, greater financial strain, younger maternal age, lower RDAS satisfaction, and greater RSE past month (Table 2a). Maternal anxiety was positively correlated with mental health history, RSE past month, RSE past year, employment loss, and financial strain, as well as negatively associated with MSPSS, RDAS total, RDAS satisfaction and consensus for mothers of children aged 5 to 8 years (Table 2b ). All significant predictors of maternal anxiety at the bivariate level were included in subsequent inferential analyses.
Table 2b.
Bivariate correlations of sociodemographic and predictor variables for mothers of children age 5 to 8 years.
| Measure | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Depression | – | |||||||||||||||||
| 2. Anxiety | .560⁎⁎ | – | ||||||||||||||||
| 3. Mental health history | .319⁎⁎ | .225⁎⁎ | – | |||||||||||||||
| 4. MSPSS | −0.146* | −0.208⁎⁎ | −0.105 | – | ||||||||||||||
| 5. RDAS total | −0.330⁎⁎ | −0.228⁎⁎ | −0.147 | .268⁎⁎ | – | |||||||||||||
| 6. RDAS cohesion | −0.227⁎⁎ | −0.111 | −0.121 | .189* | .846⁎⁎ | – | ||||||||||||
| 7. RDAS satisfaction | −0.327⁎⁎ | −0.282⁎⁎ | −0.178* | .143 | .777⁎⁎ | .503⁎⁎ | – | |||||||||||
| 8. RDAS consensus | −0.262⁎⁎ | −0.191* | −0.103 | .243⁎⁎ | .825⁎⁎ | .484⁎⁎ | .553⁎⁎ | – | ||||||||||
| 9. RSE past month | .251⁎⁎ | .239⁎⁎ | .100 | −0.193⁎⁎ | −0.141 | −0.026 | −0.099 | −0.177* | – | |||||||||
| 10. RSE past year | .231⁎⁎ | .274⁎⁎ | .240⁎⁎ | −0.123 | −0.081 | −0.008 | −0.077 | −0.072 | .483⁎⁎ | – | ||||||||
| 11. Employment Loss | .110 | .207⁎⁎ | .034 | −0.013 | −0.045 | −0.015 | −0.051 | −0.044 | .338⁎⁎ | .074 | – | |||||||
| 12. Financial Strain | .090 | .163* | .051 | −0.039 | .046 | .105 | .005 | −0.010 | .231⁎⁎ | .100 | .277⁎⁎ | – | ||||||
| 13. Maternal Age | −0.088 | −0.077 | −0.057 | .057 | −0.149 | −0.173* | −0.161 | −0.076 | −0.164⁎⁎ | −0.111 | −0.114 | −0.138* | – | |||||
| 14. Marital Status | −0.062 | −0.136 | −0.134 | .222⁎⁎ | −0.122 | −0.084 | −0.138 | −0.094 | −0.141* | −0.244⁎⁎ | −0.020 | −0.152* | .089 | – | ||||
| 15. Parity | −0.012 | −0.102 | .054 | −0.038 | .029 | .111 | −0.035 | .015 | .141* | −0.013 | .142* | −0.007 | −0.062 | .082 | – | |||
| 16. Maternal Education | −0.115 | −0.056 | −0.125 | .127 | −0.062 | −0.128 | −0.029 | −0.014 | −0.180⁎⁎ | .018 | −0.304⁎⁎ | −0.201⁎⁎ | .381⁎⁎ | .105 | −0.177⁎⁎ | – | ||
| 17. Partner Education | −0.004 | −0.003 | −0.050 | .039 | .098 | −0.010 | .104 | .179* | −0.168⁎⁎ | −0.101 | −0.202⁎⁎ | −0.193⁎⁎ | .289⁎⁎ | .138* | −0.154* | .573⁎⁎ | – | |
| 18. Household Income | −0.124 | −0.089 | −0.153* | .064 | −0.023 | −0.103 | −0.049 | .074 | −0.228⁎⁎ | −0.211⁎⁎ | −0.258⁎⁎ | −0.413⁎⁎ | .403⁎⁎ | .374⁎⁎ | −0.054 | .385⁎⁎ | .375⁎⁎ | – |
Note. Below diagonal = age 5 to 8 years; *p ≤ 0.05, **p ≤ 0.01.
Abbreviations: MSPSS = Multidimensional Scale of Perceived Social Support; RDAS = Revised Dyadic Adjustment Scale; RSE = Recent Stressful Events.
Block-wise logistic regressions were conducted as previously described (Table 4 ). For mothers of children age 0 to 18 months, financial strain (OR = 3.23, 95% CI [1.46, 7.16], p = .004) and RSE past month (OR = 2.31, 95% CI [1.32, 4.04], p = .003) significantly affected the odds of maternal anxiety, such that both variables represented significant risk factors. For mothers of children 18 months to 4 years, mental health history (OR = 3.44, 95% CI [1.70, 6.94], p = .001) and financial strain (OR = 2.12, 95% CI [1.04, 4.33], p = .039) were significant risk factors for anxiety, while maternal age (OR = 0.93, 95% CI [0.86, 0.999], p = .048) was negatively associated with odds of clinically-relevant anxiety. For mothers of children age 5 to 8 years, marital quality was a significant protective factor from maternal anxiety (OR = 0.93, 95% CI [0.88, 0.99], p = .017).
Table 4.
Binary logistic regression for maternal anxiety in final models (block 3).
| Predictor Variable |
0 to 18 months |
18 months to 4 years |
5 to 8 years |
||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | |
| History of mental health | 1.29 | 0.57, 2.91 | .541 | 3.44 | 1.70, 6.94 | .001 | 1.97 | 0.78, 5.01 | .153 |
| MSPSS | 1.00 | 0.97, 1.03 | .919 | – | – | – | 0.99 | 0.96, 1.01 | .280 |
| RDAS | 0.97 | 0.92, 1.02 | .264 | – | – | – | 0.93 | 0.88, 0.99 | .017 |
| RDAS Satisfaction | – | – | – | 0.90 | 0.80, 1.00 | .056 | – | – | – |
| RSE past month | 2.31 | 1.32, 4.04 | .003 | 1.23 | 0.76, 1.98 | .396 | 1.13 | 0.61, 2.08 | .705 |
| RSE past year | – | – | – | – | – | – | 1.14 | 0.72, 1.80 | .579 |
| Employment loss | – | – | – | – | – | – | 2.18 | 0.82, 5.76 | .117 |
| Financial strain | 3.23 | 1.46, 7.16 | .004 | 2.12 | 1.04, 4.33 | .039 | – | – | – |
| Maternal age | – | – | – | 0.93 | 0.86, 0.999 | .048 | – | – | – |
Note. Abbreviations: MSPSS = Multidimensional Scale of Perceived Support; RDAS = Revised Dyadic Adjustment Scale; RSE = Recent Stressful Events.
Mental health service use and barriers
A total of 16.99% (n = 53/312) of all included mothers who responded to mental health service use questions reported engaging in individual therapy in the past month compared to 2.03% (n = 6/296) in group therapy by means of either in-person or virtual modalities. Mothers did not utilize instant messaging mental health services or crisis line services in the past month. Additional mental health service use included: seeking mental health information online (21.84%; n = 64/293), using well-being phone apps (19.40%; n = 58/299), and accessing faith-based counseling services (3.11%; n = 9/289). Yet, mothers also reported several barriers to mental services, including not believing they needed services (23.87%), not having time or energy (17.63%), not interested in accessing services (11.08%), cost of services (8.44%), uncertainty on how to access services (5.15%), and belief it would not help (3.13%).
Of the mothers who identified clinically-relevant depression or anxiety, only 21.48% (n = 32/149) of these mothers indicated that they had accessed individual counselling in the past month, while 3.55% (n = 5/141) had accessed group counselling services. Nearly a third of mothers (30.99%; n = 44/142) sought mental health information online, while 22.14% (n = 32/140) reported using well-being phone apps. Only a few individuals (2.94%; n = 4/136) reported accessing faith-based counselling services. There was no reported access of text messaging services or crisis telephone services. Endorsed barriers to mental service use included not having time or energy (34.53%), cost of services (17.94%), not believing they needed services (15.25%), uncertainty on how to access services (11.66%), not interested in accessing services (11.21%), and belief it would not help (5.38%).
Discussion
To our knowledge, the current study is the first to evaluate depression and anxiety prevalence in mothers of children 0–8 years old during the COVID-19 pandemic. The current study identified clinically-relevant depression and anxiety in 33.16% to 43.37% and 29.59% to 36.27% of mothers, respectively, across child ages. Although the data are collected from an online convenience sample with inherent bias potential, we emphasize that these rates are dramatically elevated compared to past reports of maternal depression or anxiety from prior research with highly similar recruitment methods (e.g., Williams et al., 2016). Depression rates may have particular intergenerational mental health implications given that up to 60% of young children exposed to maternal depression go onto experience life-course psychopathology (Goodman et al., 2011; Vostanis et al., 2006).
In non-pandemic populations, prenatal and postpartum depression and anxiety prevalence has been meta-estimated to be 11.9%, 95% CI [11.4, 12.5] (Woody et al., 2017) and 14.8% to 24.6%, 95% CIs ranging from 13.6% to 28.0%, respectively (Dennis et al., 2017). As such, the prevalence of maternal prenatal and postpartum depression (33.16%) and anxiety (36.27%) in the present study appear to be elevated within the context of the COVID-19 pandemic, given that they are significantly higher than reported confidence intervals. Similarly, non-pandemic population norms for mothers with young children indicate that maternal depression rates increase steadily to 9% across the first 10 years of childhood (Letourneau et al., 2013), while maternal anxiety can occur in up to 18% of mothers (Clavarino et al., 2010). Thus, the rates reported in the current study of 42.55% to 43.37% and 29.59% to 32.62% for depression and anxiety, respectively, appear to be significantly elevated for mothers of children 18 months to 8 years old.
The prevalence rates reported in the current study are similar to previous literature that reported increased prevalence of posttraumatic stress disorder (PTSD) and depression among quarantined individuals in Canada during the SARS epidemic (Hawryluck et al., 2004). Specifically, 28.9% and 31.2% of individuals met cut-off scores for PTSD and depression, respectively (Hawryluck et al., 2004). While more than half of the study participants were not parents, prevalence rates were not affected by parent status (Hawryluck et al., 2004). Thus, the consistencies between rates reported during the COVID-19 pandemic and SARS epidemic provide significant evidence that mental health needs are increased during global health crises.
Consistent with the extant literature (Yim et al., 2015), prior psychopathology was a significant risk factor for depression in mothers of children 18 months old and older as well as anxiety in mothers of children 18 months old to four years old. The reoccurrence of depression and anxiety under the stress conditions of the pandemic is consistent with the hypothesis that epigenetics plays a key role through which environmental stressors influence genetic constitution for risk of mental illness (Nestler, 2014). Through this hypothesis, severe stress triggers a genetic change in vulnerable individuals that can lead to sustained changes in gene expression and result in chronic susceptibility to mental illness in the face of stressful life events (Gotlib et al., 2008; Nestler, 2014). Given this vulnerability, an important follow-up public health effort would be for healthcare providers and/or government service to re-contact mothers of young children with prior mental health diagnoses. This contact would serve to re-assess at-risk mothers to identify if significant problems related to COVID-19 are present and inform or refer follow-up treatment plans to ameliorate individual and family well-being.
Maternal anxiety in mothers of younger children up to four years old was particularly vulnerable to current financial strain. Stressful events in the last month was similarly related to anxiety and depression in mothers from pregnancy to 18 months postpartum. Mothers with children age 18 months to four years old demonstrated a unique predictor of maternal anxiety as well, such that younger mothers within this age range were at greater risk for clinically-relevant anxiety. Interestingly, maternal age was significantly correlated with household income within this age group, indicating that younger mothers reported lower household income. Given the sensitive period for language and cognitive development in early childhood, there is a significant need to address economic stress in young families to allow for the rich and responsive caregiving necessary for promoting child development. Poverty and poverty-related factors (e.g., household organization and stability) have been shown to impact language development in young children due to the effect of financial stress on parent well-being, parenting, and parental investment (Perkins et al., 2013; Vernon-Feagans et al., 2012). In Canada alone, within the same week comparison from 2019 to 2020, the Canada Revenue Agency reported an 18-fold increase in applications for employment insurance, underscoring the huge financial impact the COVID-19 pandemic has had on Canadian households (Statistics Canada, 2020). Given the potential detrimental effects on child development, families of infants and toddlers require assurances of basic income or additional income supplements guaranteed for a prolonged period of time (e.g., 12-months) to improve family functioning and reduce finance-related distress.
For families of school-aged children (age 5–8 years), mothers appeared to be most impacted by their marital quality, such that lower overall marital quality increased odds of depression or anxiety. Yet, marital quality was also a significant predictor of depression from pregnancy to 18 months postpartum. Exposure to marital distress in childhood has repeatedly been associated with an increased risk of internalizing and externalizing disorders in children (El-Sheikh and Whitson, 2006; Essex et al., 2003). Of great concern is more severe forms of marital distress, including domestic violence, which is associated with increased risk of children experiencing abuse and maltreatment, emotional and behavioural problems, and increased exposure to additional adversities (Holt et al., 2008). Timely and effective interventions are crucial to preventing severe and enduring effects of parental relationship distress on child psychosocial functioning.
Mental health service access
Access to and use of mental health services is crucial to prevent long-term impacts on individuals and their families. Likely as a result of COVID-19-related measures (e.g., physical distancing, shuttering of businesses), individuals primarily endorsed seeking information through online means and phone apps. In the context of the pandemic, internet-based services are a viable option for economically advantaged families. Yet, in many cases, the transition to providing telehealth alternatives to psychological intervention has been slow and costly due to the investment required for secure platforms and equipment. Additionally, most telehealth models do not concurrently treat maternal mental health concerns and parenting risks, despite the evidence for the importance of addressing both (Patel et al., 2013; Shonkoff and Fisher, 2013). There are also important considerations at a practical and policy level to ensure families are meeting basic needs (e.g., food/housing security, safe and accessible childcare) during the uncertainty of the pandemic. Further, the widespread dissemination and implementation of telehealth interventions will be crucial to target all families in need.
Interventions
Given the current study's findings, the wide-spread implementation of evidence-based treatments is crucial to support families with young children during the COVID-19 pandemic. Cognitive-behavioural therapy is a well-established and highly-researched intervention for the treatment of depression (Ekers et al., 2008) and anxiety (Hofmann and Smits, 2008). Given the high comorbidity of anxiety and depression in the current sample, a more transdiagnostic approach to intervention may also be useful to address emotional concerns simultaneously, such as the Unified Protocol for the transdiagnostic treatment of emotional disorders (Barlow et al., 2017; Farchione et al., 2012). Dialectical behavior therapy (DBT) (Linehan, 1987; Ritschel et al., 2015) for the treatment of emotion dysregulation would be a similar transdiagnostic approach; additionally, recent research has evaluated the utility of DBT as an intervention for emotion dysregulation in parents, with the added component of increasing parenting skills (Martin et al., 2017; Muzik et al., 2016; Zalewski et al., 2018). Each of these possible interventions have been shown to be effective in individual and group formats, as well as through telehealth services. Given the need to disseminate affordable services widely due to COVID-19, group-based telehealth interventions may allow for increased reach of psychological services in a time of elevated need. Should such significant levels of psychosocial distress in parents continue, which is not unlikely given the recent global surge in virus load, it would also be advised for policy makers to consider prevention-based approaches to reduce family stress. These could include investments in family supports such as paid parental leave, accessible childcare and universal basic income as well as innovative approaches to highly scalable mental health interventions such as peer-support and online platforms that can be quickly evaluated to ensure acceptable efficacy.
Strengths and limitations
The findings of the current study should be interpreted in the context of some limitations. Most notably, the results of this study are based on cross-sectional data, which provide a snapshot of the current mental health for mothers of young children. However, the study is limited in the ability to provide long-term conclusions regarding the impact of COVID-19. Similarly, participants were not limited to a particular location of residence. Due to the nature of the pandemic, experiences may be related to country or province/state-specific measures that have been implemented. To that extent, the majority of participants were living in Canada at the time of completion with a higher representation from Winnipeg, Manitoba. Similarly, the current study's population demonstrated higher household income than comparable Canadian census data, indicating that lower socioeconomic populations are likely underrepresented in the current study. In addition, the current sample demonstrated a relatively higher socioeconomic status overall. Given the negative bivariate association between depression/anxiety and household income across age groups, as well as the consideration that women with lower household income may not have access to the internet to participate in the current study, the reported prevalence rates may reflect an underestimate of depression and anxiety. Additionally, maternal income and employment were not assessed separately and thus conclusions cannot be drawn regarding mothers who work out of the home and those who identify as stay-at-home mothers. Similarly, mental health service use prior to COVID-19 restrictions was not assessed and thus conclusions regarding changes in service use were not assessed. Mothers were also included in each appropriate child age range to allow for proper consideration of mothers with multiple children. This method to the analysis allows for greater clinical utility; however, it required some mothers to be included multiple times across analyses. Individuals may also respond differently to the survey based on the stage of the COVID-19 pandemic; however, the current study utilized a short window of data collection to minimize differences and changes in restrictions due to COVID-19. Lastly, the nature of self-report mental health data implies symptom level and does not replace a clinical diagnosis.
Despite these limitations, the current study provides significant insight into the experiences of mothers during the COVID-19 pandemic. In under three weeks, the current study collected data from 728 caregivers of children under the age of nine years old across Canada and international countries. Given the sample size, the data allowed for several evaluations of risk and protective factors. The accelerated nature of the current study allows for the efficient and timely dissemination of important findings to inform policy recommendations and intervention strategies.
Future directions
There is still substantial work to be done on widespread needs of family systems. The current findings are generalizable primarily to higher income Canadian populations, while their ability to inform nuanced populations is limited. Future research should consider the findings of the current study when investigating risk and protective factors of additional populations to determine if the noted factors can be generalized to other individuals. Additionally, as previously noted, rates of depression and anxiety may be underestimated given the average socioeconomic status of the sample; future research investigating prevalence rates and factors affecting those rates in more diverse populations is crucial. Future research should also investigate broad mental health needs and continue monitoring the effects of the COVID-19 pandemic to anticipate a possible delayed effect of mental health and family needs. Similarly, changes to mental health service use should be assessed to evaluated whether specific services are more likely to be accessed under the conditions of COVID-19. A longitudinal follow-up study to describe evolving needs over the course of the pandemic would also be informative. Similarly, investigation of additional caregiver needs is warranted to better address the needs of the whole family.
Conclusions
The COVID-19 pandemic has no doubt affected families worldwide. The current study highlights the substantial increase in clinically significant depression and anxiety in mothers. Future research efforts, policy development and implementation, and mental health interventions should continue to consider and identify specific populations that may be particularly vulnerable to mental health impacts as a result of the pandemic.
Contributors
L.R., K.R., and J.P. developed the study concept and contributed to the study design in addition to E.C. Data collection were performed by L.R. and E.C. E.C. and K.J. performed the data analysis and interpretation in collaboration with L.R. E.C., K.J., and C.D. drafted the manuscript, and L.R., K.R., and J.P. provided critical revisions. All authors approved the final version of the manuscript for submission.
Role of the funding source
The funding sources mentioned in the Acknowledgements contributed to participant remuneration and resources necessary for study development. Start-up funds, Children's Hospital Research Institute of Manitoba, University of Manitoba, and Social Science and Humanities Research Council provided funding for student involvement.
Declaration of Competing Interest
None.
Acknowledgments
We thank the participating families without whom this work would not be possible. Thank you to Marlee Salisbury, Shaelyn Stienwandt, Mateja Carevic, Helen Harvie, and Irlanda Gomez for their diligent work with project development. This work was supported by the generous support of Research Manitoba (L.R.), Social Science and Humanities Research Council (L.R.), Department of Pediatrics and Child Health, University of Manitoba (J.P.) and Children's Hospital Research Institute of Manitoba (J.P.; L.R.) as well as fellowships from the Social Science and Humanities Research Council (E.C.) and University of Manitoba (K.J.).
Footnotes
Canada's National Strategy for Critical Infrastructure defines essential services as all services which are essential to maintaining Canadians health, safety, security, and economic well-being as well as an effective government (Public Safety Canada, 2009).
References
- American Psychiatric Association . 5th ed. Author; Washington, DC: 2013. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- Barlow D.H., Farchione T.J., Sauer-Zavala S., Latin H.M., Ellard K.K., Bullis J.R., Bentley K.E., Boettcher H.T., Cassiello-Robbins C. 2nd ed. Oxford University Press; 2017. The Unified Protocol for Transdiagnostic Treatment of Emotional Disorders. [DOI] [Google Scholar]
- Braunack-Mayer A., Tooher R., Collins J.E., Street J.M., Marshall H. Understanding the school community's response to school closures during the H1N1 2009 influenza pandemic. BMC Public Health. 2013;13:344. doi: 10.1186/1471-2458-13-344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Busby D., Christensen C., Crane D., Larson J. A revision of the Dyadic Adjustment Scale for use with distressed and nondistressed couples: construct hierarchy and multidimensional scales. J. Marital Fam. Ther. 1995;21:289–308. doi: 10.1111/j.1752-0606.1995.tb00163.x. [DOI] [Google Scholar]
- Clavarino A.M., Mamun A.A., O'Callaghan M., Aird R., Bor W., O'Callaghan F., Williams G.M., Marrington S., Najman J.M., Alati R. Maternal anxiety and attention problems in children at 5 and 14 years. J. Atten. Disord. 2010;13:658–667. doi: 10.1177/1087054709347203. [DOI] [PubMed] [Google Scholar]
- Cluver L., Lachman J.M., Sherr L., Wessels I., Krug E., Rakotomalala S., Blight S., Hillis S., Bachman G., Green O., Butchart A., Tomlinson M., Ward C.L., Doubt J., McDonald K. Parenting in a time of COVID-19. Lancet. 2020;395:E64. doi: 10.1016/S0140-6736(20)30736-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox J.L., Holden J.M., Sagovsky R. Detection of postnatal depression: development of the 10-item Edinburgh Postnatal Depression scale. Br. J. Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- Dennis C.L., Falah-Hassani K., Shiri R. Prevalence of antenatal and postnatal anxiety: systematic review and meta-analysis. Br. J. Psychiatry. 2017;210:315–323. doi: 10.1192/bjp.bp.116.187179. [DOI] [PubMed] [Google Scholar]
- Eaton W., Smith C., Ybarra M., Muntaner C., Tien A. Center for Epidemiologic Studies Depression Scale: review and Revision (CESD and CESD-R) In: Maruish M.E., editor. The Use of Psychological Testing for Treatment Planning and Outcomes Assessment: Instruments for Adults. Routledge; 2004. pp. 363–377. [Google Scholar]
- Ekers D., Richards D., Gilbody S. A meta-analysis of randomized trials of behavioural treatment of depression. Psychol. Med. 2008;38:611–623. doi: 10.1017/S0033291707001614. [DOI] [PubMed] [Google Scholar]
- El-Sheikh M., Whitson S.A. Longitudinal relations between marital conflict and child adjustment: vagal regulation as a protective factor. J. Fam. Psychol. 2006;20:30–39. doi: 10.1037/0893-3200.20.1.30. [DOI] [PubMed] [Google Scholar]
- Essex M.J., Klein M.H., Cho E., Kraemer H.C. Exposure to maternal depression and marital conflict: gender differences in children's later mental health symptoms. J. Am. Acad. Child Adolesc. Psychiatry. 2003;42:728–737. doi: 10.1097/01.CHI.0000046849.56865.1D. [DOI] [PubMed] [Google Scholar]
- Farchione T.J., Fairholme C.P., Ellard K.K., Boisseau C.L., Thompson-Hollands J., Carl J.R., Gallagher M.W., Barlow D.H. Unified protocol for transdiagnostic treatment of emotional disorders: a randomized controlled trial. Behav. Ther. 2012;43:666–678. doi: 10.1016/j.beth.2012.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelaye B., Rondon M.B., Araya R., Williams M.A. Epidemiology of maternal depression, risk factors, and child outcomes in low-income and middle-income countries. Lancet Psychiatry. 2016;3:973–982. doi: 10.1016/S2215-0366(16)30284-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman S.H., Rouse M.H., Connell A.M., Broth M.R., Hall C.M., Heyward D. Maternal depression and child psychopathology: a meta-analytic review. Clin. Child Fam. Psychol. Rev. 2011;14:1–27. doi: 10.1007/s10567-010-0080-1. [DOI] [PubMed] [Google Scholar]
- Gotlib I.H., Joormann J., Minor K.L., Hallmayer J. HPA axis reactivity: a mechanism underlying the associations among 5-HTTLPR, stress, and depression. Biol. Psychiatry. 2008;63:847–851. doi: 10.1016/j.biopsych.2007.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris P.A., Taylor R., Thielke R., Payne J., Gonzalez N., Conde J.G. Research electronic data capture (REDCap) - A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawryluck L., Gold W.L., Robinson S., Pogorski S., Galea S., Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg. Infect. Dis. 2004;10:1206–1212. doi: 10.3201/eid1007.030703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann S.G., Smits J.A.J. Cognitive-behavioral therapy for adult anxiety disorders: a meta-analysis of randomized placebo-controlled trials. J. Clin. Psychiatry. 2008;69:621–632. doi: 10.4088/JCP.v69n0415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt S., Buckley H., Whelan S. The impact of exposure to domestic violence on children and young people: a review of the literature. Child Abus. Negl. 2008;32:797–810. doi: 10.1016/j.chiabu.2008.02.004. [DOI] [PubMed] [Google Scholar]
- Jeong H., Yim H.W., Song Y.J., Ki M., Min J.A., Cho J., Chae J.H. Mental health status of people isolated due to Middle East Respiratory Syndrome. Epidemiol. Health. 2016;38 doi: 10.4178/epih.e2016048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau J.T.F., Yang X., Tsui H.Y., Pang E., Wing Y.K. Positive mental health-related impacts of the SARS epidemic on the general public in Hong Kong and their associations with other negative impacts. J. Infect. 2006;53:114–124. doi: 10.1016/j.jinf.2005.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lebel, C., MacKinnon, A., Bagshawe, M., Tomfohr-Madsen, L., Giesbrecht, G., 2020. Elevated depression and anxiety among pregnant individuals during the COVID-19 pandemic. 10.31234/osf.io/gdhkt. [DOI] [PMC free article] [PubMed]
- Leis J.A., Heron J., Stuart E.A., Mendelson T. Associations between maternal mental health and child emotional and behavioral problems: does prenatal mental health matter? J. Abnorm. Child Psychol. 2014;42:161–171. doi: 10.1007/s10802-013-9766-4. [DOI] [PubMed] [Google Scholar]
- Letourneau N.L., Tramonte L., Willms J.D. Maternal depression, family functioning and children's longitudinal development. J. Pediatr. Nurs. 2013;28:223–234. doi: 10.1016/j.pedn.2012.07.014. [DOI] [PubMed] [Google Scholar]
- Linehan M.M. Dialectical behavior therapy for borderline personality disorder: theory and method. Bull. Menninger Clin. 1987;51:261–276. [PubMed] [Google Scholar]
- Martin C.G., Roos L.E., Zalewski M., Cummins N. A dialectical behavior therapy skills group case study on mothers with severe emotion dysregulation. Cogn. Behav. Pract. 2017;24:405–415. doi: 10.1016/j.cbpra.2016.08.002. [DOI] [Google Scholar]
- Martins C., Gaffan E.A. Effects of early maternal depression on patterns of infant-mother attachment: a meta-analytic investigation. J. Child Psychol. Psychiatry. 2000;41:737–746. doi: 10.1111/1469-7610.00661. [DOI] [PubMed] [Google Scholar]
- Mihashi M., Otsubo Y., Yinjuan X., Nagatomi K., Hoshiko M., Ishitake T. Predictive factors of psychological disorder development during recovery following SARS outbreak. Heal. Psychol. 2009;28:91–100. doi: 10.1037/a0013674. [DOI] [PubMed] [Google Scholar]
- Muzik M., Rosenblum K., Schuster M., Kohler E.S., Alfafara E., Miller N. A mental health and parenting intervention for adolescent and young adult mothers and their infants. J. Depress. Anxiety. 2016:5. doi: 10.4172/2167-1044.1000233. [DOI] [Google Scholar]
- Nestler E.J. Epigenetic mechanisms of depression. JAMA Psychiatry. 2014;71:454–456. doi: 10.1001/jamapsychiatry.2013.4291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel V., Belkin G.S., Chockalingam A., Cooper J., Saxena S., Unützer J. Grand challenges: integrating mental health services into priority health care platforms. PLoS Med. 2013;10 doi: 10.1371/journal.pmed.1001448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perkins S.C., Finegood E.D., Swain J.E. Poverty and language development: roles of parenting and stress. Innov. Clin. Neurosci. 2013;10:10–19. [PMC free article] [PubMed] [Google Scholar]
- Pfefferbaum B., North C.S. Mental health and the Covid-19 pandemic. N. Engl. J. Med. 2020 doi: 10.1056/nejmp2008017. [DOI] [PubMed] [Google Scholar]
- Public Safety Canada, 2009. National Strategy for Critical Infrastructure [WWW Document]. URLhttps://www.publicsafety.gc.ca/cnt/rsrcs/pblctns/srtg-crtcl-nfrstrctr/srtg-crtcl-nfrstrctr-eng.pdf.
- Radloff L.S. The CES-D Scale: a self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977;1:385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- Rahman A., Surkan P.J., Cayetano C.E., Rwagatare P., Dickson K.E. Grand challenges: integrating maternal mental health into maternal and child health programmes. PLoS Med. 2013;10 doi: 10.1371/journal.pmed.1001442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritschel L.A., Lim N.E., Stewart L.M. Transdiagnostic applications of DBT for adolescents and adults. Am. J. Psychother. 2015;69:111–128. doi: 10.1176/appi.psychotherapy.2015.69.2.111. [DOI] [PubMed] [Google Scholar]
- Sanchez-Villegas A., Schlatter J., Ortuno F., Lahortiga F., Pla J., Benito S., Martinez-Gonzalez M.A. Validity of a self-reported diagnosis of depression among participants in a cohort study using the Structured Clinical Interview for DSM-IV (SCID-I) BMC Psychiatry. 2008;8:43. doi: 10.1186/1471-244X-8-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shonkoff J.P., Fisher P.A. Rethinking evidence-based practice and two-generation programs to create the future of early childhood policy. Dev. Psychopathol. 2013;25:1635–1653. doi: 10.1017/S0954579413000813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Somerville S., Dedman K., Hagan R., Oxnam E., Wettinger M., Byrne S., Coo S., Doherty D., Page A.C. The Perinatal Anxiety Screening Scale: development and preliminary validation. Arch. Womens. Ment. Health. 2014;17:443–454. doi: 10.1007/s00737-014-0425-8. [DOI] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B.W., Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Sprang G., Silman M. Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster Med. Public Health Prep. 2013;7:105–110. doi: 10.1017/dmp.2013.22. [DOI] [PubMed] [Google Scholar]
- Statistics Canada, 2020. Employment insurance claims received by province and territory, monthly, seasonally adjusted [WWW Document]. URLhttps://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1410000501.
- Vernon-Feagans L., Garrett-Peters P., Willoughby M., Mills-Koonce R., Cox M., Blair C., Burchinal P., Burton L., Crnic K., Crouter N., Garrett-Peters P., Granger D., Greenberg M., Lanza S., Miccio A., Mills-Koonce R., Skinner D., Stifter C., Werner E., Willoughby M. Chaos, poverty, and parenting: predictors of early language development. Early Child. Res. Q. 2012;27:339–351. doi: 10.1016/j.ecresq.2011.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vostanis P., Graves A., Meltzer H., Goodman R., Jenkins R., Brugha T. Relationship between parental psychopathology, parenting strategies and child mental health: findings from the GB national study. Soc. Psychiatry Psychiatr. Epidemiol. 2006;41:509–514. doi: 10.1007/s00127-006-0061-3. [DOI] [PubMed] [Google Scholar]
- Wachs T.D., Black M.M., Engle P.L. Maternal depression: a global threat to children's health, development, and behavior and to human rights. Child Dev. Perspect. 2009;3:51–59. doi: 10.1111/j.1750-8606.2008.00077.x. [DOI] [Google Scholar]
- Williams C., Taylor E.P., Schwannauer M. A web-based survey of mother-infant bond, attachment experiences, and metacognition in posttraumatic stress following childbirth. Infant Ment. Health J. 2016;37:259–273. doi: 10.1002/imhj.21564. [DOI] [PubMed] [Google Scholar]
- Wolford S.N., Cooper A.N., McWey L.M. Maternal depression, maltreatment history, and child outcomes: the role of harsh parenting. Am. J. Orthopsychiatry. 2019;89:181–191. doi: 10.1037/ort0000365. [DOI] [PubMed] [Google Scholar]
- Woody C.A., Ferrari A.J., Siskind D.J., Whiteford H.A., Harris M.G. A systematic review and meta-regression of the prevalence and incidence of perinatal depression. J. Affect. Disord. 2017;219:86–92. doi: 10.1016/j.jad.2017.05.003. [DOI] [PubMed] [Google Scholar]
- World Health Organization, 2020. WHO Novel Coronavirus (2019-nCoV) Situation Report 1.
- Yim I.S., Tanner Stapleton L.R., Guardino C.M., Hahn-Holbrook J., Dunkel Schetter C. Biological and psychosocial predictors of postpartum depression: systematic review and call for integration. Annu. Rev. Clin. Psychol. 2015;11:99–137. doi: 10.1146/annurev-clinpsy-101414-020426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zalewski M., Lewis J.K., Martin C.G. Identifying novel applications of dialectical behavior therapy: considering emotion regulation and parenting. Curr. Opin. Psychol. 2018;21:122–126. doi: 10.1016/j.copsyc.2018.02.013. [DOI] [PubMed] [Google Scholar]
- Zimet G.D., Dahlem N.W., Zimet S.G., Farley G.K. The multidimensional scale of perceived social support. J. Pers. Assess. 1988;52:30–41. doi: 10.1207/s15327752jpa5201_2. [DOI] [PubMed] [Google Scholar]