Abstract
The Moderating Roles of Psychological Flexibility and Inflexibility on the Mental Health Impacts of COVID-19 Pandemic and Lockdown in Italy.
Preliminary data suggest the COVID-19 pandemic has adverse effects on mental health in approximately a quarter of the general population. Few prior studies have identified contextual risk factors and no published study has explored factors that might moderate their adverse effects on mental health. Psychological flexibility is the cornerstone of psychological health and resiliency. This study investigated the roles of psychological flexibility and inflexibility in moderating the effects of COVID-19 risk factors on three mental health outcomes: COVID-19 peritraumatic distress, anxiety, depression. We hypothesized that psychological flexibility would mitigate and psychological inflexibility would exacerbate the adverse effects of COVID-19 risk factors on mental health. During the Italian national lockdown (M = 39.29 days, SD = 11.26), 1035 adults (79% female, M = 37.5 years, SD = 12.3) completed an online survey. Twelve COVID-19 risk factors were identified (e.g. lockdown duration, family infected by COVID-19, increase in domestic violence and in unhealthy lifestyle behaviours) and constituted a COVID-19 Lockdown Index. As predicted, results showed that after controlling for sociodemographic variables, global psychological flexibility and four of its sub-processes (self-as context, defusion, values, committed action), mitigated the detrimental impacts of COVID-19 risk factors on mental health. In contrast and as expected, global psychological inflexibility and four of its sub-processes (lack of contact with present moment, fusion, self-as-content, lack of contact with personal values) exacerbated the detrimental impacts of COVID-19 risk factors on mental health. Findings converge with those from the broader psychological flexibility literature providing robust support for the use of ACT-based interventions to promote psychological flexibility and mental health during the COVID-19 pandemic.
Keywords: COVID-19 pandemic, Peritraumatic distress, Depression, Anxiety, Psychological flexibility, Psychological inflexibility, Lockdown
Highlights
-
•
Psychological flexibility mitigated COVID-19 impacts on mental health outcomes.
-
•
Psychological inflexibility intensified COVID-19 pandemic lockdown risk factors.
-
•
Psychological flexibility increases resilience during COVID-19 mandatory lockdown.
-
•
Psychological flexibility interventions can promote mental health during a pandemic.
1. Introduction
The Coronavirus disease 2019 (COVID-19) outbreak caused by SARS-CoV-2 was officially labelled a pandemic on March 12th, 2020 by Word Health Organization. Due to the disease being transmitted via close contact between persons, extreme social distancing measures have been used to curb its spread. Lengthy lockdowns have been imposed in many countries to reduce the exponential spread of the virus and to alleviate pressures on healthcare systems.
Both the pandemic and the lockdown measures have the potential to cause considerable anguish. The pandemic itself is likely to evoke fear of contagion, concerns about disease and death, and anxiety about future health and economic uncertainties (Asmundson & Taylor, 2020). This distress is further fueled by conflicting information about the virus, the absence of a medical cure, and media saturation about the deaths, infection rates, overcrowded hospitals and other negative information about the pandemic (Garfin, Silver, & Holman, 2020; Ren, Gao, & Chen, 2020). Severe pandemic lockdowns are a further source of discomfort due to inherent stressors such as confinement, social isolation, loss of income, activity restrictions and boredom (Brooks et al., 2020).
Alarming mental health impacts of the current pandemic and severe social distancing restrictions are beginning to emerge. Preliminary data from the Chinese national lockdown indicated that 35% reported mild to severe COVID-19 peritraumatic distress (N = 52,730; Qiu et al., 2020), 54% rated the psychological impact of the outbreak as moderate to severe, 16.5% endorsed moderate to severe depressive symptoms and 28.8% moderate to severe anxiety symptoms (N = 1210; Wang, Zhang, Zhao, Zhang, & Jiang, 2020). An Italian study found that 37% of participants reported post-traumatic stress and 21–23% reported high anxiety, perceived stress, insomnia and adjustment disorders (N = 18,147; Rossi et al., 2020). It is therefore critical that we identify factors that reduce or exacerbate the adverse mental health impacts of the pandemic and associated lockdowns (Holmes et al., 2020). Hence, the purpose of the present study is to explore the role of psychological flexibility (a psychological resource) and its inverse, inflexibility (a risk factor), in moderating the effects of the pandemic and lockdown context on mental health outcomes.
Italy was severely affected by COVID-19 and was subjected to mandatory lockdown for almost two months (Remuzzi & Remuzzi, 2020). The Italian Government on March 9th implemented a level one national lockdown requiring all Italians to stay home, and refrain from any social contact with friends and relatives outside their household (Lazzerini & Putoto, 2020). Schools and universities and all “non essential” industries and retail stores had to remain closed until May 4th, and travelling was only permitted for work (where work from home was not possible), health care or other basic necessities (e.g., obtaining groceries) (Government of Italy, 2020). During the mandatory lockdown, Italy registered over 28,884 deaths due to COVID-19 (Italian Ministry of Health, 2020).
1.1. COVID-19 and lockdown risk factors
Research examining risks factors for mental health outcomes from previous pandemics such as the 2002 severe acute respiratory syndrome (SARS), and the 2012 Middle East respiratory syndrome (MERS) indicates that social distancing and quarantine, being a health-care worker, unemployment and financial difficulties were related to poorer mental health outcomes (Brooks et al., 2020). Having a history of psychiatric illness prior to the quarantine and higher quarantine duration were also linked with increased anxiety and post-traumatic stress symptoms (Brooks et al., 2020; Hawryluck et al., 2004; Jeong et al., 2016).
Few published studies have examined the mental health impacts of COVID-19 and mandatory lockdown contextual factors. The following summary of risk factors is based on findings from this body of research and should be considered preliminary given the recency of the pandemic. However, all of the abovementioned risk factors identified in prior pandemics have also emerged as risk factors in the COVID-19 research, in addition to other factors. During lockdown, pre-existing medical conditions, mental illnesses, as well as learning and physical disabilities have been identified as high risk factors for loneliness, anxiety and depression (Razai, Oakeshott, Kankam, Galea, & Stokes-Lampard, 2020; Vindegaard & Benros, 2020). Older and younger people report more adverse mental health impacts from lockdown-related socializing restrictions (e.g., unable to receive visitors if living alone or hospitalized, and closure of schools and entertainment facilities) (Girdhar, Srivastava, & Sethi, 2020; Razai et al., 2020; Wang at el., 2020). Furthermore, limited social capital, decreased income during the pandemic or being a refugee or an undocumented migrant are associated with greater negative mental health outcomes (Razai et al., 2020). Having a family member infected with COVID-19 is related to higher anxiety (Cao et al., 2020). Additionally, being an informal (e.g., parent) or formal (e.g., healthcare worker) caregiver, or a victim of domestic violence, are strong risk factors for adverse mental health outcomes during lockdown (Bradbury‐Jones & Isham, 2020; Pappa et al., 2020; Razai et al., 2020; Vindegaard & Benros, 2020). Lastly, an Italian study found that lower self-discipline and perceptions of the lockdown measures as a limitation on personal freedom, were related to higher stress and a greater likelihood of violating governmental social isolation rules (Flesia, Fietta, Colicino, Segatto, & Monaro, 2020).
1.2. psychological flexibility and inflexibility
Psychological flexibility is a transdiagnostic concept that entails a range of inter- and intra-personal skills, and is considered the cornerstone of mental health as it is closely related to resiliency (Kashdan & Rottenberg, 2010). According to the psychological flexibility model that underpins acceptance and commitment therapy (ACT), psychological flexibility involves being open to inner experiencing in the present, and adjusting behaviors in response to changing situational demands that are also aligned with personal values (Hayes, Luoma, Bond, Masuda, & Lillis, 2006). As such, psychological flexibility enables an individual to shift behavioral repertoires when they compromise pursuit of personal values, while also adapting to changing circumstances (Kashdan & Rottenberg, 2010). Psychological flexibility is fostered by six therapeutic processes: (1) acceptance – openness to inner experiencing, (2) defusion – observing feelings and thoughts without attachment, (3) present moment awareness – mindful awareness of the present, (4) self-as-context – flexible self-awareness and perspective taking, (5) values – connection to personal values, (6) committed action – values-guided effective action (Hayes, Strosahl, & Wilson, 2012).
The inverse of the ACT psychological flexibility model posits that the opposite of these six processes foster psychological inflexibility, which involves rigid and reactionary behavioral responses to uncomfortable and unwanted stimuli. The corresponding six psychological inflexibility processes are: (1) experiential avoidance – avoidance of unwanted inner experiencing, (2) lack of present moment awareness, (3) self-as-content – rigid attachment to concepts of self, (4) fusion – absorption in unwanted thoughts and feelings rather than observing them and allowing them to flow freely, (5) lack of contact with values, (6) inaction and impulsiveness – derailment of functional behavior in response to unwanted inner experiencing (Hayes et al., 2012).
Higher psychological flexibility is related to better mental health outcomes across a wide range of contexts (Gloster, Meyer, & Lieb, 2017; Hayes et al., 2006; Kashdan & Rottenberg, 2010; Marshall & Brockman, 2016; Stabbe, Rolffs, & Rogge, 2019). For example, psychological flexibility was found to moderate the relationship between daily stress and physical and mental health and wellbeing outcomes in the general population (Gloster et al., 2017). Psychological flexibility has also been shown to moderate the adverse effects of major life events on depressive symptoms (Fonseca, Trindade, Mendes, & Ferreira, 2019). In contrast, higher psychological inflexibility is related to psychopathology (Hayes et al., 2006; Kashdan & Rottenberg, 2010; Stabbe et al., 2019). In particular, higher psychological inflexibility has been found to predict trauma and mental health problems in the context of violent crimes (Gold, Marx, & Lexington, 2007), school shootings (Kumpula, Orcutt, Bardeen, & Varkovitzky, 2011), and death of a loved one, motor vehicle accidents and witnessing violence in the home or natural disasters (Kashdan & Kane, 2011).
ACT is as an empirically supported treatment for a range of mental health problems that has as a primary goal, the promotion of psychological flexibility (see reviews, A-tjak et al., 2015; Hayes et al., 2006; Powers, Zum Vorde Sive Vording, & Emmelkamp, 2009; Ruiz, 2010; Spijkerman, Pots, & Bohlmeijer, 2016; Swain, Hancock, Hainsworth, & Bowman, 2013). ACT has also been effective in the context of community disasters. For example, an ACT-based self-help program effectively reduced psychological distress among war refugees (Tol et al., 2020). Hence, clarifying the roles of psychological flexibility and inflexibility in modifying the effects of COVID-19 risk factors on mental health is likely to inform intervention pathways that target these malleable processes and promote mental health in the context of a pandemic.
1.3. The present study
The purpose of this study was to investigate the roles of psychological flexibility and inflexibility in moderating the effects of COVID-19 contextual risk factors on mental health in Italy. Specifically, we hypothesized that global psychological flexibility and its six processes would mitigate the adverse effects of COVID-19 contextual risk factors on mental health outcomes, operationalized as COVID-19 peritraumatic distress, anxiety and depression. In contrast, we hypothesized that global psychological inflexibility and its six processes would exacerbate the adverse effects of COVID-19 contextual risk factors on mental health outcomes.
2. Methods
2.1. Participants and recruitment procedure
The sample consisted of 1035 participants who completed an online survey during the Italian mandatory lockdown. All Italian citizens ≥18 years of age were eligible. Recruitment was conducted through social media and a snowballing procedure, whereby participants invited friends and acquaintances to participate in the study. The survey was advertised as research designed to investigate the psychological impacts of the COVID-19 pandemic. The survey was developed on Qualtrics software and took approximately 15–20 min to complete. An accurate response rate was not possible to obtain, as recruitment was primary conducted through social networks. The study was approved by an Italian University human research ethics committee.
2.2. Measures
Demographics. Participants indicated their age, gender, education, employment, and ethnicity. To gauge socio-economic status (SES), participants were asked to indicate whether they were below, average or above the mean income of the population.
COVID-19 and Lockdown Context Variables. The following information was obtained on COVID-19 and lockdown experiences: number of days in lockdown, number of people in the household, and whether living in Northern Italy, the region most adversely affected by COVID-19. Participants also indicated whether they worked in direct contact with COVID-19 patients or if they lost work or were receiving a lockdown redundancy payment. Participants reported if they were single (i.e., currently not in a relationship), if they had existing mental or physical health problems, and whether they were on psychological or psychopharmacological treatments during lockdown. Participants also indicated whether they were infected by COVID-19 and the severity of their symptoms if infected (rated on a 5-point Likert scale; 1 = not at all serious to 5 = very serious), and whether family members were infected, hospitalized, or deceased due to COVID-19.
To gauge participant's perceptions of the adequacy of home space, and increases in domestic violence and in unhealthy lifestyle behaviors, the following items were rated on a 5-point scale (1 = not at all to 5 = very much): “Is the size of your home insufficient to guarantee your personal space, despite the mandatory lockdown, such as number of rooms in relation to the people you live with?“; “Have verbal and/or physical violent behaviours increased at home during the current mandatory lockdown?“; “Have you noticed increases in the frequency of certain behaviors such as – (1) alcohol use, (2) drug use, (3) use of tobacco or electronic cigarettes, (4) gambling, (5) taking more medications than prescribed, (6) consumption of sweets and/or salty snacks between main meals, (7) average daily time on the internet except for work or education”. A total unhealthy lifestyle behaviors score was calculated by averaging responses to the seven health behavior items.
Psychological Flexibility and Inflexibility. The Multidimensional Psychological Flexibility Inventory (MPFI; Rolffs, Rogge, & Wilson, 2018) was used to assess global psychological flexibility and inflexibility, and their core processes (psychological flexibility: acceptance, present moment awareness, self-as-context, defusion, values, committed action; psychological inflexibility: experiential avoidance, lack of contact with present moment, self-as-content, fusion, lack of contact with values, inaction). Participants rated the extent to which they agreed with each item on a 6-point scale (1 = never true to 6 = always true). Scores were averaged and higher scores on the respective global and sub-processes indicate greater psychological flexibility and inflexibility. The Italian version of this scale is currently under validation. First, two independent forward translations of the original version of the MPFI were produced (one by three authors of this report and one by a bilingual translator whose mother tongue is Italian and who is fluent with US English). Second, the forward translations were reviewed by a translation panel consisting of three authors of this report, the translator, two ACT researchers and a lay person. Ambiguities of these versions were identified, and a reconciled forward version was created. This version was submitted to 30 participants from the general population to evaluate the clarity of items. Modifications were made in response to participant feedback. A final version was created and back-translated by one bilingual translator whose native language is US English and who is fluent in Italian. The MPFI has demonstrated good reliability and validity in clinical and nonclinical samples (Lin, Rogge, & Swanson 2020; Rogge, Daks, Dubler, & Saint, 2019; Seidler, Stone, Clark, Koran, & Drake, 2020; Stabbe et al., 2019). The observed Cronbach's alphas for the global scales and subscales are summarized in Table 2. The observed range (0.86–0.95) was similar to that obtained in the derivation study (0.87–0.97).
Table 2.
Descriptive Data and Correlations between Study Predictors and Mental Health Outcomes (N = 1035).
|
Variable |
M (SD) | Range | α | COVID -19 Lockdown Index |
COVID-19 Peritraumatic Distress |
Anxiety |
Depression |
|---|---|---|---|---|---|---|---|
| r | r | r | r | ||||
| COVID-19 Lockdown Index | 7.74 (1.53) | 4–13 | – | .46** | .47** | .50** | |
| Global Psychological Flexibility | 3.69 (.85) | 1.67–6 | .95 | -.26** | -.37** | -.39** | -.39** |
| Acceptance | 2.83 (1.05) | 1–6 | .85 | .04 | .02 | .02 | .05 |
| Present Moment Awareness | 3.65 (1.17) | 1–6 | .93 | -.09** | -.14** | -.14** | -.13** |
| Self-as-context | 3.74 (1.14) | 1–6 | .92 | −22** | -.34** | -.37** | -.35** |
| Defusion | 3.44 (1.15) | 1–6 | .90 | -.30** | -.46** | -.52** | -.46** |
| Values | 4.32 (1.13) | 1–6 | .92 | -.27** | -.33** | -.34** | -.37** |
| Committed Action | 4.13 (1.19) | 1–6 | .94 | -.28** | -.40** | -.40** | -.45** |
| Global Psychological Inflexibility | 2.22 (.69) | 1–5.03 | .91 | .38** | .59** | .61** | .63** |
| Experiential avoidance | 3.40 (1.18) | 1–6 | .92 | -.08** | -.09** | -.09** | -.09** |
| Lack of Contact with Present Moment | 2.03 (1.03) | 1–6 | .92 | .30** | .39** | .36** | .45** |
| Self-as-content | 2.12 (1.14) | 1–6 | .94 | .33** | .44** | .52** | .51** |
| Fusion | 2.15 (1.11) | 1–6 | .94 | .39** | .61** | .67** | .62** |
| Lack of Contact with Values | 1.83 (.84) | 1–6 | .86 | .24** | .46** | .44** | .46** |
| Inaction | 1.80 (.93) | 1–6 | .92 | .40** | .62** | .62** | .64** |
Notes. α = Cronbach's alpha, r = Person's correlations for continuous variables and Spearman's correlations for categorical variables. ∗p < .05, ∗∗ p < .01.
COVID-19 Peritraumatic Distress. We used the COVID-19 Peritraumatic Distress Index (CPDI; Qiu et al., 2020) to measure distress due to the COVID-19 lockdown. The 18-item CPDI questionnaire was developed in China to assess COVID-19 peritraumatic distress symptoms. The English version was translated into Italian by a bilingual translator and two authors of this manuscript. The CPDI assesses the frequency of anxiety, depression, specific phobias, cognitive change, avoidance, compulsive behaviour, physical symptoms and loss of social functioning in the past week (e.g., “I feel empty and helpless no matter what I do”; “During this COVID-19 period, I often feel dizzy or have back pain and chest distress”). Items are rated on a 5-point Likert scale (0 = never to 4 = most of the time). A total score (0–100) is calculated by summing all item scores, with higher scores indicating higher COVID-19 peritraumatic distress. The Chinese normative data provided the following ranges for the total score: 28 to 51 mild to moderate distress, ≥52 severe distress. The CPDI demonstrated good reliability and content validity in the derivation study (Qiu et al., 2020). The observed Cronbach's alpha was .89.
Anxiety. Anxiety was assessed with the General Anxiety Disorder Scale (GAD-7; Spitzer, Kroenke, Williams, & Lö; we, 2006). The GAD-7 questionnaire measures anxiety symptoms over the past two weeks. Items are rated on a 4-point Likert scale (0 = not at all to 3 = nearly every day). Item scores are summed, with higher scores reflecting higher anxiety. We used the Italian version of the GAD-7 (Kroenke & Spitzer, 2010). The instrument has been shown to be psychometrically sound (Löwe et al., 2008; Plummer, Manea, Trepel, & McMillan, 2016). The observed Cronbach's alpha was .90. Normative data provide the following ranges for the total score: minimal (0–4), mild (5–9), moderate (10–14), and severe (15–21) anxiety symptoms (Spitzer, Kroenke, Williams, & Löwe, 2006).
Depression. The Patient Health Questionnaire (PHQ-9; Spitzer, Kroenke, & Williams, 1999) was used to measure depressive symptomatology over the past two weeks. Items are rated on a 4-point Likert scale (0 = not at all to 3 = nearly every day). All item scores are summed, with higher scores indicating higher depression. Normative data provide the following ranges for the total score: normal (0–4), mild (5–9), moderate (10–14), moderately severe (15–19), and severe (20–27) depressive symptoms. We used the Italian validated version of the PHQ-9 (Mazzotti et al., 2003). The measure has demonstrated sound psychometric properties (Manea, Gilbody, & McMillan, 2012). The observed Cronbach's alpha was .84.
2.3. Data analysis
All analyses were performed in IBM SPSS 24 using the Process macro v.3.4. First, correlations were conducted between all demographics and COVID-19 and lockdown context variables, and the three mental health outcomes. COVID-19 and lockdown context variables that were related to all mental health outcomes constituted a COVID-19 lockdown risk factor index that was used as the predictor in subsequent moderation analyses. Demographics significantly correlated with a mental health outcome were controlled for in the corresponding moderation analysis. To interpret the significance of correlations, we referred to Cohen's (1988) criteria: small (0.10), moderate (0.30) and large (0.50). To test the moderating role of global psychological flexibility (W) in the link between the COVID-19 and lockdown risk factor index and mental health outcomes, three simple moderation analyses were performed with Process Model 1 (Hayes, 2018), one for each dependent variable. The same three simple moderation analyses were also conducted with global psychological inflexibility as the moderator (W). Process Model 1 enables testing the conditional effect (i.e., the effect of one variable on another, conditioned on a third or interaction), by estimating the effect of X on Y at a certain point (or points) along the moderator, and testing whether this effect is significant. Statistical significance of simple moderations was established when the 95% confidence intervals (CIs) for the interaction (COVID-19 lockdown index × moderator) did not include zero (Hayes, 2018). As both the predictor and the moderator of an interaction are continuous in this study, the Johnson-Neyman procedure was used to further investigate the pattern of effects (Hayes, 2018; Hayes & Rockwood, 2017). This method clarifies the pattern of significance across the entire range of the moderator by using a regression equation which estimates Y for various combinations of X and W and their associated 95% CIs. Significance in a Johnson-Neyman plot is established when the 95% CIs are both positive or negative (i.e., they do not cross zero) (Hayes, 2018; Hayes & Rockwood, 2017).
Simple moderation models in which global psychological flexibility emerged as a significant moderator, were further examined using its six processes as single moderators, instead of the global psychological flexibility score. The same procedure was used with global psychological inflexibility and its six processes.
3. Results
3.1. Sample characteristics
We collected data from 1035 Italian adults, 79.1% of which were female. The age range was 18–81 (M = 37.5, SD = 12.3). Nearly all participants (98.4%) were of Italian nationality. Approximately half of the sample (48.4%) had a bachelor's degree, 27.2% completed high school and 20.3% postgraduate courses. Almost half (45.4%) of the sample were either married or living with a partner, while 54.6% were single, widowed or divorced. Most (65.6%) participants were employed, 13.2% were students and 6.7% unemployed. Regarding SES, 10.4% endorsed a mean income below average, 82.5% reported being in the middle socioeconomic class, and 7.1% wealthier than the average.
Table 1 summarizes descriptive data on demographics, the COVID-19 lockdown contextual variables, and their correlations with the mental health outcomes. Regarding the COVID-19 lockdown context, participants spent on average 39.29 days in lockdown, with a mean of 2.62 cohabitants. A total of 61.1% were living in the Northern region, while 23.1% lived in the Center, and 15.8% in the South. Just over half (54.6%) of the participants were single during lockdown. A total of 177 participants (17.1%) reported being infected by COVID-19, with an average symptom severity of 1.82. A total of 7.6% reported having a family member infected by COVID-19, 2.9% had family members who were hospitalized and 2.0% had family members who died due to COVID-19. A total of 4.3% of participants worked in direct contact with COVID-19 patients, while 10.9% lost work or were put on a lockdown redundancy fund. A total of 9.4% declared having mental health problems, 13.7% physical health problems, and 13.8% were engaged in psychological or psychopharmacological treatments during lockdown. The mean rating for adequacy of home personal space was 2.32, indicating on average participants had insufficient personal space in their house. Specifically, 39.6% of participants reported moderate to high agreement regarding having insufficient home personal space. The mean domestic violence rating was 1.27, denoting that on average participants did not report an increase in domestic violence. However, 5.3% of participants reported a moderate to high increase in domestic violence. Finally, the mean rating for unhealthy lifestyle behaviours during lockdown was 1.64, indicating that on average participants did not report an increase in unhealthy lifestyle behaviors, although 28.8% had moderate to high increases in specific unhealthy lifestyle behaviors as follows: 7.9% alcohol use (M = 1.36, SD = 0.67), 1.1% drug use (M = 1.05, SD = 0.30), 14.9% use of tobacco or electronic cigarettes (M = 1.47, SD = 0.90), 0.1% gambling (M = 1.01, SD = 0.13), 1.9% taking more medications than prescribed (M = 1.13, SD = 0.41), 38.9% consumption of sweets and/or salty snacks between main meals (M = 2.24, SD = 1.02), and 76.6% daily time on the internet and social media, except for work or education (M = 3.22, SD = 1.02).
Table 1.
Descriptive Data on Demographics, COVID-19 and Lockdown Context Variables, and Correlations with Mental Health Outcomes (N = 1035).
|
Variable |
% (n) | M (SD) | Range | COVID-19 Peritraumatic Distress |
Anxiety |
Depression |
|---|---|---|---|---|---|---|
| r | r | r | ||||
| Demographics | ||||||
| Age years | 37.51 (12.32) | 18.70–73.34 | -.06* | -.19** | -.18** | |
| Gender: female | 79.1 (819) | -.20** | -.20** | −18** | ||
| Low Educationa | 31.3 (323) | .08 | .03 | -.02 | ||
| Low SESb | 10.4 (108) | .06* | .05 | .09** | ||
| Currently unemployedc | 6.7 (69) | .05 | .05 | .11** | ||
| Retiredc | 3.5 (36) | -.06 | -.11** | -.15** | ||
| Italian nationalityc | 98.4 (1018) | -.04 | -.02 | .00 | ||
| COVID-19 and Lockdown Context Variables | ||||||
| Days in lockdown | 39.29 (11.26) | 0–100 | .07* | .08* | .08** | |
| Number of cohabitants during lockdown | 2.62 (1.22) | 1–6 | .07* | .08** | .05 | |
| Living in a Northern region during lockdownc | 61.1 (632) | -.07* | -.08* | -.08* | ||
| COVID-19 infectedc | 17.1 (177) | .06* | .07* | .09** | ||
| Severity of COVID-19 symptomsd | 1.8 (.92) | 1–5 | .10 | .13 | .09 | |
| Family member infectedc | 7.6 (79) | .09** | .09** | .07* | ||
| Family member hospitalizedc | 2.9 (30) | -.04 | -.05 | -.04 | ||
| Family member deceasedc | 2.0 (21) | -.01 | -.02 | .01 | ||
| Insufficient home personal spaced | 2.32 (1.00) | 1–5 | .13* | .11** | .08* | |
| Increase in violence at homed | 1.27 (.60) | 1–5 | .28** | .29** | .22** | |
| Increase in unhealthy lifestyle behavioursd | 1.64 (.34) | 1–3.43 | .44** | .41** | .47** | |
| Direct contact with COVID-19 patients at workc | 4.3 (45) | .08** | .11** | .07* | ||
| Lost work or receiving redundancy fundc | 10.9 (113) | .08* | .07* | .09** | ||
| Single during lockdownc | 54.6 (565) | .07* | .10** | .18** | ||
| Mental health problems during lockdownc | 9.4 (97) | .27** | .28** | .29** | ||
| Psychological or psychopharmacological treatmentsc | 13.8 (143) | .16** | .18** | .18** | ||
| Physical health problems during lockdownc | 13.7 (142) | -.08** | -.05 | -.03 | ||
Notes. a 1 = high school or below, 0 = bachelor's degree or above; b 1 = SES below the average, 0 = medium or above the average SES. c 1 = yes, 0 = no; d Rated on a 5-point Likert scale from 1(not at all), 5 (very much). r = Person's correlation for continuous variables and Spearman's correlations for categorical variables. ∗ p < .05, ∗∗ p < .01.
3.2. Preliminary analyses
Mental Health Descriptive Data. The COVID-19 peritraumatic distress mean was 22.19 (SD = 12.04). A total of 27.0% of participants reported mild to moderate COVID-19-related peritraumatic distress and 1.6% reached severe symptomatology (M = 22.19, SD = 12.04). Regarding anxiety symptoms, the mean was 5.51 (SD = 3.90), with 12.3% and 3.0% of the sample endorsing moderate and severe levels of anxiety, respectively. The mean for depressive symptomatology was 6.63 (SD = 4.49), with 15.5% reporting moderate levels and 6.2% severe depressive symptomatology.
COVID-19 Lockdown Index. We used the COVID-19 and lockdown context variables to form an index of mental health risk factors associated with the COVID-19 pandemic and lockdown, from here-on referred to as the COVID-19 Lockdown Index. The procedure we used to develop the COVID-19 Lockdown Index is similar to that used in the development of a psychosocial stress index, which consisted of items that had categorical and Likert scale ratings (Sonino & Fava, 1998). First, we inspected correlations between all COVID-19 context variables and the three mental health outcomes. The results of these correlations are summarized in Table 1. Twelve COVID-19 context items were significantly correlated with all three mental health outcomes. These 12 items constituted the COVID-19 Lockdown Index. Responses to nine of the forced-choice and open-ended items were converted to dichotomous categories as follows: lockdown duration (0 = <1 month, 1 = ≥ 1 month); living in the Northern region (0 = no, 1 = yes); COVID-19 infected (0 = no, 1 = yes); family member infected (0 = no, 1 = yes); work in direct contact with COVID-19 patients (0 = no, 1 = yes); lost work or receiving redundancy fund due to lockdown (0 = no, 1 = yes); single (0 = no, 1 = yes); mental health problems (0 = no, 1 = yes); and psychological or psychopharmacological treatments (0 = no, 1 = yes). An additional three items were rated on the same 5-point Likert scale (1 = not at all, to 5 = very much) as follows: increase in home violence, insufficient household space, and total increase in frequency of unhealthy lifestyle behaviours. The nine dichotomous items were scored as 0 (no, indicative of lower distress) and 1 (yes, indicative of higher distress), whereas the three items with Likert scale ratings were scored by computing the mean. Therefore, the final index was calculated by adding the mean score of the three continuous items to the total summed score of the dichotomous items. Higher index scores reflect greater risk for distress during lockdown (range 1–14).
Correlations between Study Predictors and Mental Health Outcomes. Correlations between the study predictors (COVID-19 Lockdown Index, psychological flexibility, psychological inflexibly and demographics), and the mental health outcomes are displayed in Table 2 . Higher scores on the COVID-19 Lockdown Index were significantly correlated with poorer mental health across all outcomes with the magnitude of coefficients ranging from medium to large. The global psychological flexibility and subscale scores were significantly negatively correlated with the COVID-19 Lockdown Index with the exception of acceptance, which was unrelated to the COVID-19 Lockdown Index. The global psychological inflexibility and subscale scores were significantly positively correlated with the COVID-19 Lockdown Index, except for experiential avoidance, which was weakly positively associated with the COVID-19 Lockdown Index. The global psychological flexibility and subscale scores were significantly correlated with lower COVID-19 peritraumatic distress, anxiety and depression apart from for acceptance, which was unrelated to all mental health outcomes. The global psychological inflexibility and subscale scores were significantly related to higher COVID-19 peritraumatic distress, anxiety and depression except for experiential avoidance, which was significantly but weakly correlated with lower COVID-19 peritraumatic distress, anxiety and depression. Of the demographics, gender and age were significantly but weakly associated with all mental health outcomes. Specifically, being female and younger was related to poorer mental health.
3.3. Moderation analyses
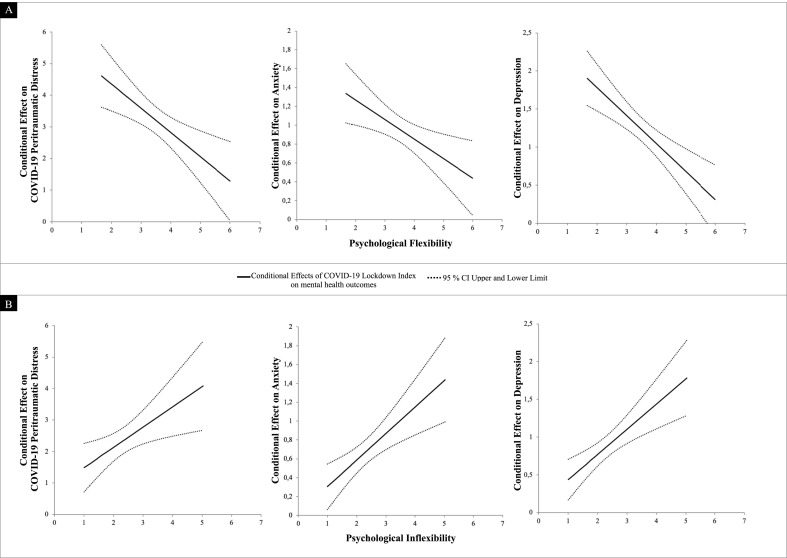
Psychological Flexibility. To investigate the hypothesis that global psychological flexibility moderates the relationship between COVID-19 lockdown risk factors and all three mental health outcomes, three simple moderation analyses were conducted. Results indicated that the interaction between the COVID-19 Lockdown Index and psychological flexibility was significant on all mental health outcomes. Each model explained between 32.3% (COVID-19 peritraumatic distress) and 36.0% (depression) of the variance while the interactions uniquely explained between 0.5% (anxiety) and 1% (depression) of the variance. Data from these three moderation models are summarized in Table 3 and in Fig. 1 A. In each model higher psychological flexibility mitigated the adverse effects of COVID-19 lockdown risk factors on all mental health outcomes. Examination of the Johnson-Neyman plots in Fig. 1A, shows that all levels of the COVID-19 Lockdown Index (low, average and high) are significantly related to all mental health outcomes at all levels of psychological flexibility (low, average and high). Specifically, people with higher COVID-19 lockdown risk factors and lower psychological flexibility reported the poorest levels of mental health. In contrast, participants with higher COVID-19 lockdown risk factors and higher psychological flexibility reported better mental health on all three outcomes.
Table 3.
Simple Moderations of Psychological Flexibility and Inflexibility in the Relationship between the COVID-19 Lockdown Index and Mental Health Outcomes.
| COVID-19 Peritraumatic Distress |
Anxiety |
Depression |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Coeff | SE | 95% CI | R2/ΔR2 | Coeff | SE | 95% CI | R2/ΔR2 | Coeff | SE | 95% CI | R2/ΔR2 | |
| Global Psychological Flexibility | -.762** | .242 | −1.237, −.286 | .323/.007 | -.206** | .077 | -.357, −.055 | .345/.005 | -.353** | .088 | -.525, −.181 | .365/.010 |
| Acceptance | .228 | .215 | -.184, .660 | .243/.001 | .094 | .069 | -.041, .230 | .259/.001 | .097 | .078 | -.056, .251 | .284/.001 |
| Present Moment Awareness | -.084 | .182 | -.442, .273 | .253/.000 | -.016 | .059 | -.130, .099 | .266/.000 | .035 | .066 | -.095, .166 | .289/.000 |
| Self-as-context | -.645** | .178 | -.995, −.294 | .310/.009 | -.148** | .057 | -.260, −.037 | .331/.004 | -.267** | .065 | -.394, −.140 | .352/.011 |
| Defusion | -.717** | .176 | −1.062, −.372 | .366/.010 | -.240** | .055 | -.347, −.133 | .415/.011 | -.322** | .064 | -.458, −.205 | .395/.016 |
| Values | -.412* | .179 | -.764, −.061 | .300/.004 | -.129* | .057 | -.242, −.016 | .313/.003 | -.230** | .064 | -.356, −.103 | .354/.008 |
| Committed Action | -.356* | .165 | -.681, −.031 | .326/.003 | -.089 | .053 | -.194, .016 | .332/.002 | -.229** | .059 | -.345, −.113 | .389/.009 |
| Global Psychological Inflexibility | .655** | .253 | .158, 1.152 | .442/.004 | .282** | .080 | .125, .438 | .474/.007 | .339** | .089 | .164, .513 | .506/.008 |
| Experiential Avoidance | -.224 | .187 | -.591, .143 | .246/.001 | .065 | .060 | -.053, .183 | .258/.001 | -.066 | .068 | -.198, .067 | .288/.001 |
| Lack of Contact with Present Moment | .322 | .197 | -.064, .709 | .323/.002 | .113 | .064 | -.013, .239 | .313/.002 | .173* | .070 | .036, .309 | .390/.004 |
| Self-as-content | .210 | .174 | -.130, .551 | .339/.001 | .118* | .054 | -.013, .223 | .399/.003 | .125* | .061 | .006, .244 | .418/.003 |
| Fusion | .317* | .157 | .009, .625 | .456/.002 | .107* | .048 | .013, .200 | .522/.003 | .187** | .057 | .075, .298 | .491/.006 |
| Lack of Contact with Values | .650** | .221 | .217, 1.084 | .371/.006 | .135 | .072 | -.006, .276 | .368/.002 | .249** | .080 | .091, .406 | .402/.006 |
| Inaction | .094 | .182 | -.263, .451 | .462/.000 | .049 | .059 | -.066, .164 | .463/.000 | .106 | .065 | -.022, .234 | .503/.001 |
Notes. Coeff = unstandardized coefficient of the interaction, SE = standard error, CI = 95% confidence interval. Significant moderations are displayed in bold. R2 = total variance explained by the model, ΔR2 = unique variance explained by the interaction. *p < .05. **p < .01.
Fig. 1A–B.
Johnson-Neyman plots representing the relationships between The COVID-19 Lockdown Index and COVID-19 peritraumatic distress, anxiety and depression as moderated through global psychological flexibility and inflexibility.
Results of analyses that explored each of the six psychological flexibility processes as single moderators (see Table 3) indicated that self-as-context, defusion, and values significantly moderated the relationship between the COVID-19 Lockdown Index and all mental health outcomes. Committed action also emerged as a significant moderator in the link between the COVID-19 Lockdown Index and both COVID-19 peritraumatic distress and depression. For each significant moderation effect, self-as-context, defusion, values and committed action mitigated the detrimental impacts of COVID-19 lockdown risk factors on mental health outcomes at all levels of each significant moderator.
Psychological Inflexibility. To investigate the hypothesis that global psychological inflexibility moderates the relationship between COVID-19 lockdown risk factors and all three mental health outcomes, three simple moderation analyses were conducted. Results indicated that the interaction between the COVID-19 Lockdown Index and psychological inflexibility was significant on all three mental health outcomes. Each model explained between 44.2% (COVID-19 peritraumatic distress) and 50.1% (depression) of the variance while the interaction uniquely explained between 0.4% (COVID-19 peritraumatic distress) and 0.08% (depression) of the variance. Data from these three moderation models are summarized in Table 3 and in Fig. 1B. In each model higher psychological inflexibility increased the adverse effects of COVID-19 lockdown risk factors on all mental health outcomes. Examination of the Johnson-Neyman plots in Fig. 1B shows that all levels of the COVID-19 Lockdown Index (low, average and high) are significantly related to all mental health outcomes at all levels of psychological inflexibility (low, average and high). In particular, participants with lower COVID-19 lockdown risk factors and lower psychological inflexibility reported higher levels of mental health. In contrast, participants with higher COVID-19 lockdown risk factors and higher psychological inflexibility reported poorer mental health on all three outcomes.
Results of analyses that explored each of the six psychological inflexibility processes as single moderators (see Table 3) showed that fusion significantly moderated the relationship between the COVID-19 Lockdown Index and all mental health outcomes. Self-as-content also emerged as a significant moderator in the link between the COVID-19 Lockdown Index and both anxiety and depression. Lack of contact with values significantly moderated the relationship between the COVID-19 Lockdown Index and both COVID-19 peritraumatic distress and depression. Finally, lack of contact with present moment moderated the relationship between COVID-19 Lockdown Index and depression. For each significant moderation effect, lack of contact with present moment, self-as-content, fusion and lack of contact with values exacerbated the detrimental impacts of COVID-19 lockdown risk factors on mental health outcomes at all levels of each significant moderator.
4. Discussion
This study investigated the roles of psychological flexibility and inflexibility in moderating the effects of COVID-19 pandemic and lockdown contextual risk factors on mental health. As predicted, global psychological flexibility and four of its sub-processes, self-as-context, defusion, values and committed action, mitigated the detrimental impacts of COVID-19 lockdown risk factors on mental health. In contrast and as expected, global psychological inflexibility and four of its sub-processes, lack of contact with present moment, fusion, self-as-content, and lack of contact with values exacerbated the detrimental impacts of COVID-19 lockdown risk factors on mental health.
The role of psychological flexibility as a protective psychological resource during a pandemic and associated social restrictions is consistent with prior research showing that psychological flexibility is related to better mental health in a wide range of contexts (Gloster et al., 2017; Hayes et al., 2006; Kashdan & Rottenberg, 2010; Stabbe et al., 2019). Results of this study that show psychological flexibility moderates the relationship between risk factors associated with the COVID-19 lockdown and mental health are consistent with prior research, which demonstrates similar moderation effects of daily stress (Gloster et al., 2017), learned helplessness Trindade, Mendes, & Ferreira, 2020) and major life events (Fonseca et al., 2019) on mental health in the general population.
Results from the present study that show higher psychological inflexibility exacerbates the adverse effects of COVID-19 pandemic and lockdown risk factors on mental health are aligned with findings from research indicating that higher psychological inflexibility predicts psychopathology in a variety of contexts including community disasters (e.g., Gold et al., 2007; Kashdan & Kane, 2011; Kumpula et al., 2011).
Of the six psychological flexibility processes, self-as-context, defusion and values emerged as the most protective, whereas the opposite of these (self-as-content, lack of contact with present moment, fusion and lack of contact with values) emerged as significant psychological inflexibility processes that intensified the detrimental effects of the COVID-19 pandemic and lockdown risk factors on mental health. The six psychological flexibility processes can be grouped into three psychological flexibility pillars: open (defusion and acceptance), centred (self-as-context and present moment awareness) and engaged (values and committed action) (Hayes et al., 2012). The opposite of these three pillars and their respective processes constitute psychological inflexibility paths to poorer mental health. It is noteworthy that at least one process from each flexibility and inflexibility pillar emerged as a significant moderator of the relationship between COVID-19 pandemic and lockdown risk factors and mental health.
Acceptance was the only psychological flexibility process that was unrelated to the COVID-19 Lockdown Index and the mental health outcomes. Unexpectedly, the psychological inflexibility counterpart of this process, experiential avoidance, was related to lower COVID-19 Lockdown Index scores and better mental health, although the correlations were weak (r = <0.10). In contrast, unhealthy lifestyle behaviors, which may function as a means of avoiding inner discomfort, were related to poorer mental health outcomes. However, post hoc analyses showed that an increase in unhealthy behaviors was not significantly correlated with the acceptance and experiential avoidances subscales. It is possible that the function of the unhealthy lifestyle behaviors altered during the lockdown and at times they functioned as effective mechanisms for managing the angst associated with lockdown. For example, increases in eating snacks may have been due to an increased interest in cooking. In Italy, cooking is strongly associated with social and cultural factors, and often functions as a means of socializing and caring for family members.
Of the six psychological flexibility processes, acceptance is likely to be the most challenging in the context of a pandemic and lockdown because it entails embracing potentially intense distress associated with a fear provoking pandemic and restrictive social isolation measures. The workability of openness to such inner discomfort in these circumstances is likely to be determined by an array of contextual factors, and for some, avoidance may be more effective in the short-term. For example, a longitudinal study of women who had been recalled because of an abnormal mammography screen showed that participants who relied on avoidant coping while they awaited their follow-up breast screen results were less distressed than women who relied on active-behavioral coping (Clutton, Pakenham, & Buckley, 1999). In an acute health crisis, avoidance of inner discomfort seemed to be effective in the short-term. In similar research, a study of couples where one partner had multiple sclerosis showed that when one partner relied on acceptance coping more than the other, the dyad was likely to report lower depressive symptoms, whereas if both partners relied on acceptance, one of the partners was likely to report elevated depressive symptoms (Pakenham & Samios, 2013). Both these studies reflect the intra- and inter-personal contextual sensitivity of acceptance and experiential avoidance with respect to health threatening contexts, similar to that of the current pandemic.
Overall, the contextually sensitive dynamic counterbalancing that occurs among the six overlapping psychological flexibility processes yields beneficial mental health effects, as demonstrated in the present study. The present findings regarding acceptance and experiential avoidance support the proposal that the effectiveness of a coping strategy depends on context and therefore no coping strategy is categorically ‘good’ or ‘bad’. This view is consistent with the functional contextual philosophy of science that underpins the ACT psychological flexibility model (Hayes et al., 2012) and stress and coping theory (Lazarus & Folkman, 1984). As is typical of the majority of psychology research, the present study was designed to examine the effects of specific variables across all individuals in the sample and is therefore limited in gauging the effects of psychological flexibility and inflexibility processes at the dynamic individual contextual level.
This study examined a wide range of contextual factors that pose mental health risks for the general community during a pandemic. Twelve risk factors were identified which formed the COVID-19 Lockdown Index. The COVID-19 pandemic and lockdown variables identified in this study as risk factors for mental health problems are consistent with those found in prior research including: pre-existing physical and mental health conditions (Razai et al., 2020), younger age (Razai et al., 2020), loss of work and reduced income (Razai et al., 2020), having a family member infected with COVID-19 (Cao et al., 2020), being a healthcare worker in contact with COVID-19 infected patients (Pappa et al., 2020) and domestic violence (Bradbury‐Jones & Isham, 2020; Razai et al., 2020). The contextual variables most strongly associated with poorer mental health in the present study were increases in unhealthy lifestyle behaviours, domestic violence and pre-existing mental health problems. These pandemic and lockdown mental health risk factors should inform the development of targeted public health interventions and support services during such emergencies.
Interestingly, family member hospitalized or deceased, and severity of the respondent's COVID-19 symptoms if infected were not associated with the mental health outcomes. Some hospitalized COVID-19 positive family members might have had relatively mild COVID-19 symptoms and were therefore placed under medical monitoring rather than in an intensive care-unit, which may explain why this factor was unrelated to the mental health outcomes. Only 21 participants reported the death of a family member due to COVID-19. Hence, the lack of variability on this variable might account for the non-significant correlations between it and the mental health outcomes. The mean severity rating of COVID-19 symptoms was low (1.8 on a 5-point scale; 1 = not at all serious to 5 = very serious) and may account for the non-significant correlations with mental health outcomes.
Data on the mental health problems in the present sample are aligned with those of other studies that have examined the mental health impacts of the COVID-19 pandemic and lockdowns using the same measures employed in this study. This body of literature shows that 32–54% of the general population report moderate to severe traumatic distress, 18–29% anxiety symptoms, and 17–23% depressive symptoms (China: Wang et al., 2020; Ireland: Hyland et al., 2020; Italy: Rossi et al., 2020).
Due to the large sample size, this study is high powered and hence, relatively weak associations emerged as significant. For example, several COVID-19 risk factors evidenced small but significant correlations with the mental health outcomes (e.g., 0.07 and 0.09), although the combination of all significant risk factors in the COVID-19 Lockdown Index yielded moderately high correlations with the outcomes (range 0.46–0.50). Similarly, relatively small amounts of variance were explained by some of the significant interaction effects (range 0.5–1%). However, following Kelley and Preacher's (2012) recommendations, the magnitude of the interactions between COVID-19 Lockdown Index and both psychological flexibility and inflexibility is likely to be clinically meaningful as the total moderation models explained between 32% and 50% of the variance in mental health outcomes.
Findings from the present study should be interpreted in the context of the following study limitations. First, all data were collected via an online survey and self-report measures, which increases the risk of common method variance. Second, the study used a cross-sectional design and hence, the causal directions among COVID-19 and lockdown context variables, psychological flexibility and inflexibility, and mental health outcomes remain ambiguous. Longitudinal research is required to examine causal links among these variables over time. Third, convenience sampling and the bias towards female participants limits the generalizability of findings. Fourth, the three mental health outcome measures were highly inter-correlated (range 0.76–0.78), which may account for the similarity in findings across outcomes. Finally, we did not examine the wellbeing dimension of mental health or the potential personal growth that may be triggered by health-related adversities (Pakenham, 2011). Future research should examine risk and protective factors for wellbeing and benefit finding in the context of the COVID-19 pandemic. Notwithstanding these limitations, this study is the first to evaluate the protective role of psychological flexibility in the link between COVID-19 and lockdown context variables and COVID-19 peritraumatic distress, anxiety, and depression.
5. Conclusion
Results from this study showed that psychological flexibility and inflexibility moderated the effects of COVID-19 and lockdown risk factors on mental health. As expected, psychological flexibility mitigated and psychological inflexibility exacerbated the detrimental impacts of COVID-19 lockdown risk factors on mental health outcomes. Three psychological flexibility processes (self-as-context, defusion and values) and their opposite counterparts (self-as-content, fusion and lack of contact with values) had the most beneficial and detrimental impacts on mental health, respectively. Each of the significant psychological flexibility processes reflects one of the three flexibility pillars, while each of the psychological inflexibility processes mirrors one of the inflexibility pillars. Consistent with the ACT framework, findings suggest that engaging in the psychological flexibility processes increases resilience during adversity. These results indicate that public health interventions targeting psychological flexibility are likely to mitigate some of the adverse effects of COVID-19 pandemic and lockdown risk factors have on mental health. Furthermore, targeting psychological flexibility with ACT-based public health interventions has been shown to be a viable means of improving a wide range of health outcomes in the general community (e.g., Fledderus, Bohlmeijer, Smit, & Westerhof, 2010) and in those with serious medical conditions (e.g., Hawkes et al., 2013). Given that research into the longer-term mental health impacts of prior pandemics show lingering elevated trauma, anxiety and depressive symptoms (e.g., after SARS quarantine; Hawryluck et al., 2004; Taylor, 2019, pp. 49–56), it is anticipated that when this pandemic abates, mental health services will face significant demands. Findings from the present study converge with those from the broader literature on psychological flexibility providing robust support for the use of ACT-based interventions to promote psychological flexibility and mental health during the COVID-19 pandemic (Polizzi, Lynn, & Perry, 2020; Presti, Mchugh, Gloster, Karekla, & Hayes, 2020).
Declaration of competing interest
The authors declare no conflict of interest.
References
- A-tjak J.G., Davis M.L., Morina N., Powers M.B., Smits J.A., Emmelkamp P.M. A meta-analysis of the efficacy of acceptance and commitment therapy for clinically relevant mental and physical health problems. Psychotherapy and Psychosomatics. 2015;84(1):30–36. doi: 10.1159/000365764. [DOI] [PubMed] [Google Scholar]
- Asmundson G.J., Taylor S. How health anxiety influences responses to viral outbreaks like COVID-19: What all decision-makers, health authorities, and health care professionals need to know. Journal of Anxiety Disorders. 2020;71 doi: 10.1016/j.janxdis.2020.102211. 102211 –102211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradbury‐Jones C., Isham L. The pandemic paradox: The consequences of COVID‐19 on domestic violence. Journal of Clinical Nursing. 2020 doi: 10.1111/jocn.15296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet. 2020;395(10227):912–920. doi: 10.1016/s0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao W., Fang Z., Hou G., Han M., Xu X., Dong J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Research. 2020;287:112934. doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clutton S., Pakenham K.I., Buckley B. Predictors of emotional well-being following a 'false-positive' breast cancer screening result. Psychology and Health. 1999;14(2):263–275. doi: 10.1080/08870449908407327. [DOI] [Google Scholar]
- Cohen J. 2nd ed. Lawrence Erlbaum; Hillsdale, NJ: 1988. Statistical power analyses for the behavioral sciences. [Google Scholar]
- Fledderus M., Bohlmeijer E.T., Smit F., Westerhof G.J. Mental health promotion as a new goal in public mental health care: A randomized controlled trial of an intervention enhancing psychological flexibility. American Journal of Public Health. 2010;100(12) doi: 10.2105/AJPH.2010.196196. 2372–2372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flesia L., Fietta V., Colicino E., Segatto B., Monaro M. Stable psychological traits predict perceived stress related to the COVID-19 outbreak. 2020. PsyArXiv. [DOI] [PMC free article] [PubMed]
- Fonseca S., Trindade I.A., Mendes A.L., Ferreira C. The buffer role of psychological flexibility against the impact of major life events on depression symptoms. Clinical Psychologist. 2020;24(1):82–90. doi: 10.1111/cp.12194. [DOI] [Google Scholar]
- Garfin D.R., Silver R.C., Holman E.A. The novel coronavirus (COVID-2019) outbreak: Amplification of public health consequences by media exposure. Health Psychology. 2020;39(5):355–357. doi: 10.1037/hea0000875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Girdhar R., Srivastava V., Sethi S. Managing mental health issues among elderly during COVID-19 pandemic. Journal of Geriatric Care and Research. 2020;7(1):29–32. doi: 10.1056/NEJMp2008017. [DOI] [Google Scholar]
- Gloster A.T., Meyer A.H., Lieb R. Psychological flexibility as a malleable public health target: Evidence from a representative sample. Journal of Contextual Behavioral Science. 2017;6(2):166–171. doi: 10.1016/j.jcbs.2017.02.003. [DOI] [Google Scholar]
- Gold S.D., Marx B.P., Lexington J.M. Gay male sexual assault survivors: The relations among internalized homophobia, experiential avoidance, and psychological symptom severity. Behaviour Research and Therapy. 2007;45(3):549–562. doi: 10.1016/j.brat.2006.05.006. [DOI] [PubMed] [Google Scholar]
- Government of Italy . 2020. Decree of the president of the council of ministers 11 March 2020.https://www.gazzettaufficiale.it/eli/id/2020/03/11/20A01605/sg March 11. Retrieved from. [Google Scholar]
- Hawkes A.L., Chambers S.K., Pakenham K.I., Patrao T.A., Baade P.D., Lynch B.M., Courneya K.S. Effects of a telephone-delivered multiple health behavior change intervention (CanChange) on health and behavioral outcomes in survivors of colorectal cancer: A randomized controlled trial. Journal of Clinical Oncology. 2013;31(18):2313–2321. doi: 10.1200/JCO.2012.45.5873. [DOI] [PubMed] [Google Scholar]
- Hawryluck L., Gold W.L., Robinson S., Pogorski S., Galea S., Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerging Infectious Diseases. 2004;10(7):1206–1212. doi: 10.3201/eid1007.030703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes A.F. The Guildford Press; New York: 2018. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. [Google Scholar]
- Hayes S.C., Luoma J.B., Bond F.W., Masuda A., Lillis J. Acceptance and commitment therapy: Model, processes and outcomes. Behaviour Research and Therapy. 2006;44(1):1–25. doi: 10.1016/j.brat.2005.06.006. [DOI] [PubMed] [Google Scholar]
- Hayes A.F., Rockwood N.J. Regression-based statistical mediation and moderation analysis in clinical research: Observations, recommendations, and implementation. Behaviour Research and Therapy. 2017;98:39–57. doi: 10.1016/j.brat.2016.11.001. [DOI] [PubMed] [Google Scholar]
- Hayes S.C., Strosahl K.D., Wilson K.G. An experiential approach to behavior change. 2nd ed. The Guildford Press; New York: 2012. Acceptance and commitment therapy. [Google Scholar]
- Holmes E.A., O'Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Ford T. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. The Lancet Psychiatry. 2020;7(6):547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyland, P., Shevlin, M, McBride O., Murphy J., Karatzias, T., Bentall R. P., et al Anxiety and depression in the Republic of Ireland during the COVID-19 pandemic. under review. PsyArXiv. https://doi.org10.31234/osf.io/8yqxr. [DOI] [PubMed]
- Italian Ministry of Health . 2020. Covid-19, cases in Italy on April 25 at 18.00 hours.http://www.salute.gov.it/portale/nuovocoronavirus/dettaglioNotizieNuovoCoronavirus.jsp?lingua=italiano&menu=notizie&p=dalministero&id=4605 April 25. Retrieved from. [Google Scholar]
- Jeong H., Yim H.W., Song Y.J., Ki M., Min J.A., Cho J. Mental health status of people isolated due to Middle East Respiratory Syndrome. Epidemiology and Health. 2016;38 doi: 10.4178/epih.e2016048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kashdan T.B., Kane J.Q. Post-traumatic distress and the presence of post-traumatic growth and meaning in life: Experiential avoidance as a moderator. Personality and Individual Differences. 2011;50(1):84–89. doi: 10.1016/j.paid.2010.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kashdan T.B., Rottenberg J. Psychological flexibility as a fundamental aspect of health. Clinical Psychology Review. 2010;30(7):865–878. doi: 10.1016/j.cpr.2010.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelley K., Preacher K.J. On effect size. Psychological Methods. 2012;17(2):137–152. doi: 10.1037/a0028086. [DOI] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L. Instruction manual: Instructions for patient health questionnaire (PHQ) and GAD-7 measures. 2010. www.phqscreeners.com Retrived from.
- Kumpula M.J., Orcutt H.K., Bardeen J.R., Varkovitzky R.L. Peritraumatic dissociation and experiential avoidance as prospective predictors of posttraumatic stress symptoms. Journal of Abnormal Psychology. 2011;120(3):617–627. doi: 10.1037/a0023927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus R.S., Folkman S. Springer Publishing Company; New York: 1984. Stress, appraisal, and coping. [Google Scholar]
- Lazzerini M., Putoto G. COVID-19 in Italy: Momentous decisions and many uncertainties. The Lancet Global Health. 2020;8:e641–e642. doi: 10.1016/S2214-109X(20)30110-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin Y.Y., Rogge R.D., Swanson D.P. Cross-cultural flexibility: Validation of the traditional Mandarin, simplified Mandarin, and Japanese translations of the multidimensional psychological flexibility inventory. Journal of Contextual Behavioral Science. 2020;15:73–84. doi: 10.1016/j.jcbs.2019.11.008. [DOI] [Google Scholar]
- Löwe B., Decker O., Müller S., Brähler E., Schellberg D., Herzog W. Validation and standardization of the generalized anxiety disorder screener (GAD-7) in the general population. Medical Care. 2008;46(3):266–274. doi: 10.1097/MLR.0b013e318160d093. [DOI] [PubMed] [Google Scholar]
- Manea L., Gilbody S., McMillan D. Optimal cut-off score for diagnosing depression with the patient health questionnaire (PHQ-9): A meta-analysis. Canadian Medical Association Journal. 2012;184(3):E191–E196. doi: 10.1503/cmaj.110829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall E.-J., Brockman R.N. The relationships between psychological flexibility, self-compassion, and emotional well-being. Journal of Cognitive Psychotherapy. 2016;30(1):60–72. doi: 10.1891/0889-8391.30.1.60. [DOI] [PubMed] [Google Scholar]
- Mazzotti E., Fassone G., Picardi A., Sagoni E., Ramieri L., Lega I., Pasquini P. The patient health questionnaire (PHQ) for the screening of psychiatric disorders: A validation study versus the structured clinical interview for DSM-IV axis I (SCID-I) Italian Journal of Psychopathology. 2003;9:235–242. [Google Scholar]
- Pakenham K.I. Benefit finding and sense making in chronic illness. In: Folkman S., editor. Oxford handbook on stress, coping, and health. Oxford University Press; New York: 2011. pp. 242–268. [Google Scholar]
- Pakenham K.I., Samios C. Couples coping with multiple sclerosis: A dyadic perspective on the roles of mindfulness and acceptance. Journal of Behavioral Medicine. 2013;36:389–400. doi: 10.1007/s10865-012-9434-0. [DOI] [PubMed] [Google Scholar]
- Pappa S., Ntella V., Giannakas T., Giannakoulis V.G., Papoutsi E., Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain, Behavior, and Immunity. 2020 doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plummer F., Manea L., Trepel D., McMillan D. Screening for anxiety disorders with the GAD-7 and GAD-2: A systematic review and diagnostic metaanalysis. General Hospital Psychiatry. 2016;39:24–31. doi: 10.1016/j.genhosppsych.2015.11.005. [DOI] [PubMed] [Google Scholar]
- Polizzi C., Lynn S.J., Perry A. Stress and coping in the time of covid-19: Pathways to resilience and recovery. Clininical Neuropsychiatry. 2020;17:59–62. doi: 10.36131/CN20200204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powers M.B., Vörding M.B.Z.V.S., Emmelkamp P.M. Acceptance and commitment therapy: A meta-analytic review. Psychotherapy and Psychosomatics. 2009;78(2):73–80. doi: 10.1159/000190790. [DOI] [PubMed] [Google Scholar]
- Presti G., Mchugh L., Gloster A., Karekla M., Hayes S.C. The dynamics of fear at the time of covid-19: A contextual behavioral science perspective. Clinical Neuropsychiatry. 2020;17(2):65–71. doi: 10.36131/CN20200206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu J., Shen B., Zhao M., Wang Z., Xie B., Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. General Psychiatry. 2020;33 doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Razai M., Oakeshott P., Kankam H., Galea S., Stokes-Lampard H. Mitigating the psychological effects of social isolation during the covid-19 pandemic. BMJ. 2020;369 doi: 10.1136/bmj.m1904. [DOI] [PubMed] [Google Scholar]
- Remuzzi A., Remuzzi G. COVID-19 and Italy: What next? The Lancet. 2020;395:1225–1228. doi: 10.1016/S0140-6736(20)30627-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren S.Y., Gao R.D., Chen Y.L. Fear can be more harmful than the severe acute respiratory syndrome coronavirus 2 in controlling the corona virus disease 2019 epidemic. World Journal of Clinical Cases. 2020;8(4):652–657. doi: 10.12998/wjcc.v8.i4.652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogge R.D., Daks J.S., Dubler B.A., Saint K.J. It's all about the process: Examining the convergent validity, conceptual coverage, unique predictive validity, and clinical utility of ACT process measures. Journal of Contextual Behavioral Science. 2019;14:90–102. doi: 10.1016/j.jcbs.2019.10.001. [DOI] [Google Scholar]
- Rolffs J.L., Rogge R.D., Wilson K.G. Disentangling components of flexibility via the hexaflex model: Development and validation of the multidimensional psychological flexibility inventory (MPFI) Assessment. 2018;25(4):458–482. doi: 10.1177/1073191116645905. [DOI] [PubMed] [Google Scholar]
- Rossi R., Socci V., Talevi D., Mensi S., Niolu C., Pacitti F. COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. An N= 18147 web-based survey. 2020. April 14) G. MedRxiv. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruiz F.J. A review of Acceptance and Commitment Therapy (ACT) empirical evidence: Correlational, experimental psychopathology, component and outcome studies. International Journal of Psychology and Psychological Therapy. 2010;10(1):125–162. [Google Scholar]
- Seidler D., Stone B., Clark B.E., Koran J., Drake C.E. Evaluating the factor structure of the Multidimensional Psychological Flexibility Inventory: An independent replication and extension. Journal of Contextual Behavioral Science. 2020;17:23–31. doi: 10.1016/j.jcbs.2020.04.007. [DOI] [Google Scholar]
- Sonino N., Fava G.A. A simple instrument for assessing stress in clinical practice. Postgraduate Medical Journal. 1998;74(873):408–410. doi: 10.1136/pgmj.74.873.408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spijkerman M.P.J., Pots W.T.M., Bohlmeijer E.T. Effectiveness of online mindfulness-based interventions in improving mental health: A review and meta-analysis an randomizedsed controlled trials. Clinical Psychology Review. 2016;45:102–114. doi: 10.1016/j.cpr.2016.03.009. [DOI] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B. Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. Jama. 1999;282(18):1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B., Löwe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Stabbe O.K., Rolffs J.L., Rogge R.D. Flexibly and/or inflexibly embracing life: Identifying fundamental approaches to life with latent profile analyses on the dimensions of the Hexaflex model. Journal of Contextual Behavioral Science. 2019;12:106–118. doi: 10.1016/j.jcbs.2019.03.003. [DOI] [Google Scholar]
- Swain J., Hancock K., Hainsworth C., Bowman J. Acceptance and commitment therapy in the treatment of anxiety: A systematic review. Clinical Psychology Review. 2013;33(8):965–978. doi: 10.1016/j.cpr.2013.07.002. [DOI] [PubMed] [Google Scholar]
- Taylor S. Scholar Publishing; Cambridge: 2019. The psychology of pandemics: Preparing for the next global outbreak of infectious disease. [Google Scholar]
- Tol W.A., Leku M.R., Lakin D.P., Carswell K., Augustinavicius J., Adaku A., Musci R.J. Guided self-help to reduce psychological distress in south Sudanese female refugees in Uganda: A cluster randomised trial. The Lancet Global Health. 2020;8(2):e254–e263. doi: 10.1016/S2214-109X(19)30504-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trindade I.A., Mendes A.L., Ferreira N.B. The moderating effect of psychological flexibility on the link between learned helplessness and depression symptomatology: A preliminary study. Journal of Contextual Behavioral Science. 2020;15:68–72. doi: 10.1016/j.jcbs.2019.12.001. [DOI] [Google Scholar]
- Vindegaard N., Benros M.E. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain, Behavior, and Immunity. 2020 doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang G., Zhang Y., Zhao J., Zhang J., Jiang F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. The Lancet. 2020;395(10228):945–947. doi: 10.1016/S0140-6736(20)30547-X. [DOI] [PMC free article] [PubMed] [Google Scholar]