Abstract
The COronaVIrus Disease-19 (COVID-19) pandemic has highlighted the critical need to focus on its impact on the mental health of Healthcare Workers (HCWs) involved in the response to this emergency. It has been consistently shown that a high proportion of HCWs is at greater risk for developing Posttraumatic Stress Disorder (PTSD) and Posttraumatic Stress Symptoms (PTSS). The present study systematic reviewed studies conducted in the context of the three major Coronavirus outbreaks of the last two decades to investigate risk and resilience factors for PTSD and PTSS in HCWs. Nineteen studies on the SARS 2003 outbreak, two on the MERS 2012 outbreak and three on the COVID-19 ongoing outbreak were included. Some variables were found to be of particular relevance as risk factors as well as resilience factors, including exposure level, working role, years of work experience, social and work support, job organization, quarantine, age, gender, marital status, and coping styles. It will be critical to account for these factors when planning effective intervention strategies, to enhance the resilience and reduce the risk of adverse mental health outcomes among HCWs facing the current COVID-19 pandemic.
Keywords: Corona, Mental health, Nurses, Physicians, Psychological distress, Stress
1. Introduction
The outbreak of Corona Virus Disease-19 (COVID) that emerged in December 2019 in Wuhan (China), quickly spread outside of China, leading the World Health Organization (WHO) Emergency Committee to declare a Public Health Emergency of International Concern (PHEIC) on January 30th 2020 (Nishiura, 2020), and a pandemic on March 11, 2020. The SARS-CoV2 – the virus responsible for COVID-19 – was isolated by 7th January 2020, and belongs to the same viral family as the coronavirus syndrome (SARS-CoV) and the Middle East respiratory coronavirus syndrome (MERS-CoV). Both of these coronavirus-based respiratory syndromes infected over 10,000 cases in the past two decades, with overall mortality rates as high as 11% and 35%, respectively (Peeri et al., al.,2020; de Wit et al., 2016; Leung et al., 2004; WHO, 2004). Compared to the Severe Acute Respiratory Syndrome (SARS) and the Middle East Respiratory Syndrome (MERS), the Corona Virus Disease-19 (COVID-19) has a greater transmission rate but a lower, though still significant, fatality rate (Peeri et al., 2020; Huang et al., 2020). To date, with more than 14 million infected worldwide and a spread that is far from being contained, investigating the psychological impact of this pandemic on healthcare workers (HCWs) including physicians and nurses, has become increasingly important.
In the last two decades, first responders’ mental health outcomes has been the focus of increasing attention, particularly in the aftermath of September 11 2001, terrorist attacks that shed light on the risks they are exposed to when operating in emergency settings, as they may be affected by physical and mental disorders, such as burnout and posttraumatic stress disorder (PTSD) (Perlman et al., 2011; Carmassi et al., 2016, 2018; Martin et al., 2017). The DSM-5 (APA, 2013) indicates that "experiencing repeated or extreme exposure to aversive details of the traumatic event(s)" can be considered as potentially traumatic events (criterion A4: e.g. first responders collecting human remains, police officers repeatedly exposed to details of child abuse).
Healthcare Workers (HCWs) in emergency care settings are particularly at risk for PTSD because of the highly stressful work-related situations they are exposed to, that include: management of critical medical situations, caring for severely traumatized people, frequent witnessing of death and trauma, operating in crowded settings, interrupted circadian rhythms due to shift work) (Figley, 1995; Crabbe et al., 2004; Cieslak et al., 2014; Berger et al., 2012; Hegg-Deloye et al., 2013; Garbern et al., 2016). PTSD rates have been reported to range from 10 to about 20% (Grevin, 1996; Clohessy and Ehlers, 1999; Robertson and Perry, 2010; DeLucia et al., 2019), with even higher PTSD rates (8% to 30%) among Intensive Care Unit (ICU) staff, (Mealer et al., 2009; Karanikola et al., 2015; Machado et al., 2018).
Although most individuals prove to be resilient after being exposed to a traumatic event (Bonanno et al., 2007), several risk factors may compromise the effectiveness of adaptation, including prior psychiatric history, female sex, lack of social support (Brewin et al., 1999; Ozer et al., 2003; Carmassi et al., 2020a, 2020b), having young children (Yehuda et al., 2015; Bryant 2019); experiencing feelings of helplessness during the trauma or intensity of emotions when exposed (i.e., anger, peritraumatic distress) (Vance et al., 2018; Carmassi et al., 2017). On the other hand, resilience, defined as the capacity to react to stress in a healthy way through which goals are achieved at a minimal psychological and physical cost (Epstein and Krasner, 2013), plays a key role in mitigating the impact of traumatic events and hence reducing PTSS, enhancing at the same time the quality of care (Wrenn et al., 2011; Ager et al., 2012; Haber et al., 2013; McGarry et al., 2013; Craun and Bourke, 2014; Hamid and Musa, 2017; Colville et al., 2017; Cleary et al., 2018; Winkel et al., 2019).
This interplay of risk and resilience factors becomes even more complex and challenging when applied in the context of an infectious epidemic. This statement is first supported by the fact that, as previous studies outlined, during epidemics a high percentage of HCWs, (up to 1 in 6 of those providing care to affected patients), develops significant stress symptoms (Lu et al., 2006; McAlonan et al., 2007) It is worth considering that in epidemic contexts HCWs are first in line facing the clinical challenges intrinsically linked to the course of the disease while under the constant personal threat of being infected or representing a source of infection.
The current COVID-19 pandemic is characterized by some relevant features that increase the risk for PTSD among HCWs addressing the emergency, such as the unprecedented numbers of critically ill patients, with an often unpredictable course of the disease, high mortality rates and lack of effective treatment, or treatment guidelines (Wang, 2020; Peeri et al., 2020). Thus, the burden of the current outbreak on healthcare providers deserves the closest attention, as it is extremely likely that health care workers involved in the diagnosis, treatment and care of patients with COVID-19 are at risk of developing psychological distress and other mental health symptoms (Bao et al., 2020; Lai et al., 2020; Carmassi et al., 2020c)
The aim of the present paper is therefore to systematically review the studies investigating the potential risk and resilience factors for the development of PTSD symptoms in HCWs who faced the two major Coronavirus outbreaks that occurred worldwide in the last two decades, namely the SARS and the MERS, as well as the ongoing COVID-19 pandemic, in order to outline effective measures to reduce the HCWs’ psychiatric burden during the current crisis affecting healthcare systems all over the world.
2. Methods
2.1. Search strategy
We reviewed articles indexed in the electronic database PubMed until 20th April 2020. No time limit was set in regard to the year of publication. The search terms were combined with the Boolean operator as follows: “(Post-traumatic stress OR Post-traumatic stress disorder OR Post-traumatic stress symptoms OR PTSD OR PTSS) AND (Severe Acute Respiratory Syndrome OR SARS OR Middle East Respiratory Syndrome OR MERS OR Corona Virus Disease 19 OR COVID-19 OR Coronavirus)”. Furthermore, relevant articles were extracted from the references section of the manuscripts found in the initial search, to complete our search.
2.2. Eligibility criteria
We included articles that met the following inclusion criteria: original studies on humans investigating possible risk and/or resilience factors for PTSD symptoms in HCWs facing the coronavirus outbreaks of SARS, MERS and COVID-19. Articles in print or published ahead of print were accepted. The exclusion criteria were: (a) studies involving general population samples that did not consider a sub-sample of HCWs; (b) studies examining other mental health symptoms but not PTSS; (c) studies assessing PTSS but not considering potential risk and resilience factors; (d) literature reviews; (e) full text not available; (f) not available in English.
2.3. Study selection
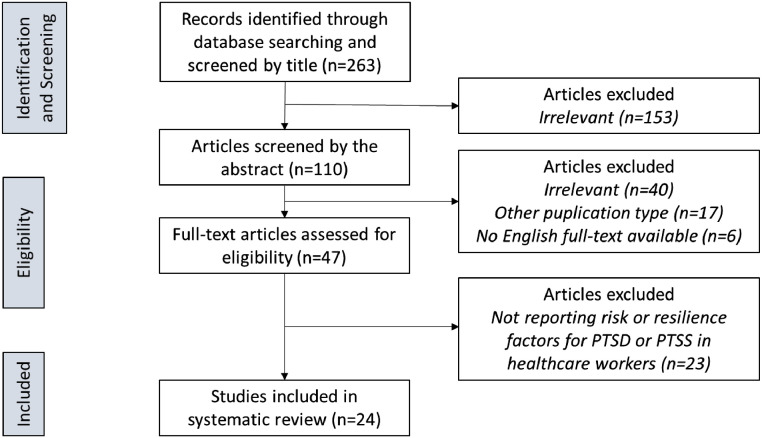
The first author screened each study for eligibility by reading the title and abstract. Any uncertainties about eligibility were clarified through discussion among all authors. Decisions for inclusion or exclusion are summarized in a flowchart according to PRISMA recommendations, usually used to conduct meta-analyses and systematic reviews of randomized clinical trials, but that have also been used for other types of systematic reviews such as our present one (Moher et al., 2009).
3. Results
3.1. Process of study selection
The study selection process is outlined in a flow-chart (Fig. 1 ). The electronic database search returned 263 publications. Following a preliminary screening of the titles and abstracts, 47 articles were considered of potential relevance, their eligibility was assessed by means of a full text examination. Twenty-four of these studies, published between 2004 and 2020, were included in this review. The main reasons for study exclusion were: the absence of a HCW sample or sub-sample, the lack of data regarding PTSS and/or about possible risk or resilience factors related to psychopathology.
Fig. 1.
PRISMA flowchart of studies selection process.
3.2. Characteristics of included studies
The key characteristics of the studies included are summarized in Table 1 . All retrieved studies were published between January 2004 and April 2020. Nineteen studies were on the SARS 2003 outbreak, two on the MERS 2012 outbreak, and three on the ongoing Covid-19 outbreak. Nine studies were on a mixed population in which HCWs represented a sub-sample (Bai et al., 2004; Chong et al., 2004; Kwek et al., 2006; Reynolds et al., 2007; Lancee et al., 2008; Wu et al., 2009; Mak et al., 2010; Wing and Leung, 2012; Li et al., 2020) while all other studies included HCWs only. Finally, five studies included specifically survivors from the infection (Kwek et al., 2006; Lee et al., 2007; Mak et al., 2010; Wing and Leung, 2012; Ho et al., 2005).
Table 1.
Main characteristics of included studies.
| Study | Outbreak | Type | Sample | PTSS/PTSD measures | Main general findings | Main risk and resilience factors |
|---|---|---|---|---|---|---|
| Bai et al. (2004) | SARS | Cross-sectional study | 557 hospital staff members (HCWs n = 402; administrative personnel n = 155) |
SARS-related stress reactions questionnaire | 5% acute stress disorder; 20% stigmatized; and 9% reluctance to work or considered resignation |
Risk factor: quarantine |
| Chan and Huak (2004) | SARS | Cross-sectional study | 661 HCWs (doctors and nurses) | Impact of Events Scale | 20% IES score >30; 27% psychiatric symptoms (35% of doctors and 25% of nurses) |
Resilience factors: Support from family/supervisors/colleagues; work organization (clear directives/precautionary measures from management) |
| Chong et al. (2004) | SARS | naturalistic, observational study |
1257 hospital staff members (nurses n = 676; doctors n = 139; health administrative workers n = 140; others n = 302) |
Impact of Event Scale | IES mean score= 34.8; 75.3% psychiatric symptoms (anxiety and worrying, depression and interpersonal difficulties, somatic problems) in the initial phase of the outbreak |
Risk factors: male; technicians; ≤2 years work experience; level of exposure |
| Maunder et al. (2004) | SARS | cross-sectional study | 1557 HCWs | Impact of Events Scale | Higher Impact of Event Scale scores are found in nurses and HCWs having contact with SARS patients. | Risk factors: level of exposure; nurses; perceived threat for their health; social isolation |
| Sim et al. (2004) | SARS | cross-sectional study | 277 HCWs (doctors n = 91; nurses n = 186) |
Impact of Events Scale | 9.4% PTSS; 20.6% psychiatric morbidity |
Risk factors: younger age, being married, psychiatric morbidity, less venting, less humor, and less acceptance. |
| Tham et al. (2004) | SARS | cross-sectional study | Emergency HCWs (doctors n = 38; nurses n = 58) |
Impact of Events Scale | IES score ≥26 in 13.2% doctors and 20.7% nurses; General Health Questionnaire-28 ≥ 5 in 15.8% doctors and 20.7% nurses |
Risk factors: nurses |
| Ho et al. (2005) | SARS | cross-sectional study | 82 HCWs not infected and 97 HCWs who recovered from SARS |
Impact of Events Scale (Chinese version) |
HCWs recovered reported high PTSS intrusion symptoms and more concerns about other health problems and discrimination. HCWs not infected had stronger fear related to infection than HCWs recovered; equal concern about infecting others (especially family members) than being self-infected emerged |
Risk factors: being HCWs survivors |
| Phua et al. (2005) | SARS | cross-sectional study | 99 HCVs (doctors n = 41; nurse n = 58) |
Impact of Events Scale | 17.7% IES >26; | Risk Factor: nurses Resilience factors: positive coping styles (humor and planning) |
| Kwek et al. (2006) | SARS | cross-sectional study | 63 HCWs SARS survivors | Impact of Events Scale | 41% scored indicative of PTSD; 30% likely anxiety and depression. | Risk factor: being HCW survivors |
| Maunder et al. (2006) | SARS | cross-sectional study | 769 HCWs (SARS and no-SARS units) |
Impact of Events Scale |
SARS unit HCWs reported higher PTSS, burnout, and psychological distress rather than no-SARS unit HCWs. SARS unit HCWs more reduced patient contact and work hours. |
Risk factors: maladaptive coping strategies (avoidance, hostile confrontation, and self-blame). Resilience factors: training, Support from family/supervisors/colleagues, work organization |
| Lee et al. (2007) | SARS | cohort study | SARS survivors (non–HCWs n = 49; HCWs n = 30) | Impact of Event Scale–Revised | Participants with at least moderate PTSS reported 32.2% Intrusion, 20.0% Avoidance, and 22.2% Hyperarousal. HCW SARS survivors were more distressed than non–HCW one year after the outbreak . |
Risk factors: being HCW survivors. |
| Lin et al. (2007) | SARS | cross-sectional study | 66 emergency HCWs and 26 no-emergency HCWs | Davidson Trauma Scale-Chinese version (DTS-C) | Emergency HCWs reported > DTS-C scores than no-emergency HCWs; 21,7% emergency HCWs and 13% no-emergency HCWs reported DTS-C >40 (suspected PTSD). | Risk factor: level of exposure |
| Reynolds et al. (2007) | SARS | cross-sectional study | 1057 quarantined subjects (HCWs n = 269) |
Impact of Events Scale – Revised | 14.6% IES-R ≥ 20; quarantined HCWs experienced greater PTSS than quarantined no-HCWs | Risk factors: quarantine |
| Su et al. (2007) | SARS | prospective and periodic follow-up study | 102 HCWs (70 SARS and 32 no-SARS HCWs) | Davidson Trauma Scale-Chinese version (DTS-C) | SARS unit HCWs reported higher Depression (38.5% vs. 3.1%) insomnia (37% vs. 9.7%) and PTSS (33% vs. 18.7%, but not significant). | Risk factors: level of exposure |
| Lancee et al. (2008) | SARS | cross-sectional study | 139 hospital staff (HCWs n = 103; clerical staff n = 13; Other n = 21) | Structured Clinical Interview for DSM-IV; Clinician-Administered PTSD Scale | 30% lifetime prevalence of depressive, anxiety, or substance use diagnosis. 5% new psychiatric disorders after outbreak |
Risk factors: previous psychiatric disorder, < years of work experience Resilience factors: training and supervisor/colleagues support. |
| Styra et al. (2008) | SARS | cross-sectional study | SARS units HCWs (n = 160) and no-SARS units HCWs (n = 88) | Impact of Event Scale—Revised | HCWs taking care of only one SARS patient had higher PTSS levels than those taking care of none or more than two SARS patients | Risk factor: level of exposure |
| Wu et al. (2009) | SARS | cross-sectional study | 549 hospital staff (21% doctors, 38% nurses, 22% technicians; 20% administrative and others) | Impact of Event Scale—Revised | About 10% IES-R ≥ 20. | Risk factors: level of exposure; younger age; quarantine/isolation (quarantine, having friends or close relatives infected). Resilience factor: coping strategies (altruistic acceptance of work-related risks) |
| Mak et al. (2010) | SARS | retrospective cohort study | 90 SARS survivors (30% HCWs) | Structured Clinical Interview for the DSM-IV; Impact of Events Scale–Revised |
47.8% PTSD in the aftermath of SARS. 25.6% still suffers PTSD 30-months post-SARS | Risk factors: being HCWs survivors (but large proportion of the HCWs were female, and this could affect results). |
| Wing and Leung (2012) | SARS | case-control study | 233 SARS survivors | Chinese bilingual version of the Semi-Structured Clinical Interview (SCID-I) Impact of Event Scale-revised |
50% SARS survivors a lifetime psychiatric disorder (depression, PTSD, somatoform pain disorder, panic disorder) | Risk factor: being HCWs survivors |
| Lee et al. (2018) | MERS | cohort study | 359 HCWs (MERS and no-MERS unit) |
Impact of Events Scale–Revised | 51% HCWs reported IES>25 (MERS units > no-MERS units) in the first month of MERS outbreak. After one month: quarantined MERS units HCWs showed higher sleep and numbness scores; MERS units HCWs showed higher intrusion symptoms |
Risk factors: level of exposure, quarantine |
| Jung et al. (2020) | MERS | cross-sectional study | 147 HCWs (nurses of MERS units) | Impact of Event Scale–Revised Korean version | 57.1% PTSD (25.1% full PTSD and 32.0% partial PTSD). PTSD was associated with turnover intention |
Risk factors: level of exposure (emergency HCWs > no-emegency HCWs), previous psychiatric disorders Resilience factor: supervisor support |
| Kang et al. (2020) | COVID-19 | cross-sectional study | 994 Wuhan HCWs (doctors and nurses) | Impact of Event Scale-Revised | Regarding mental health problem (including PTSS), 36.9% had sub-threshold disturbances, 34.4% mild disturbances, 22.4% moderate disturbances, and 6.2% severe disturbance. | Risk factors: level of exposure (to people around them who were infected, including family/collegues/friends). Resilience factors: coping strategies (being motivated to learn the necessary skills to respond to diverse challenges) |
| Lai et al. (2020) | COVID-19 | cross-sectional study | 1257 HCWs (doctors n = 493, nurses n = 764) | Impact of Event Scale–Revised | 71.5% reported mild to severe PTSS (36.5% mild, 24.5% moderate, 10.5 severe). | Risk factors: level of exposure, nurses, female, fewer years of work experience. |
| Li et al. (2020) | COVID-19 | case-control study | 214 general public and 526 HCWs (234 front-line nurses, 292 non-front-line nurses) | Vicarious traumatization questionnaire (based on several questionnaires, including IES-R) | Vicarious traumatization was significantly lower in front-line nurses than non-front-line ones and general public (no difference between non-front-line nurses and general public) | Risk factors: level of exposure, marital status. |
HCWs: healthcare workers.
3.3. PTSD and PTSS risk factors in HCWs facing the coronavirus outbreaks
3.3.1. Level of exposure
Ten studies (Chong et al., 2004; Maunder et al., 2004; Lin et al., 2007; Su et al., 2007; Styra et al., 2008; Wu et al., 2009; Lee et al., 2018; Lai et al., 2020; Kang et al., 2020; Jung et al., 2020) highlighted the role of exposure level, such as working in high-risk wards or in front-line settings during the Coronavirus outbreaks, as the major risk factor for developing PTSS and PTSD. Particularly, they pointed out the relevance of perceived threat for health and life and the experienced feelings of vulnerability as mediating factors. Most of these studies reported on the 2003 SARS outbreak. Lin et al. (2007) showed higher rates of PTSD (21,7%) among 66 emergency department staff compared to 26 HCWs of non-emergency departments (i.e., psychiatric ward, 13%). Wu et al. (2009) investigated a sample of 549 HCWs in Beijing (China), including administrative staff, finding 2 to 3 times higher PTSS rates among respondents who worked in high-risk locations and perceived high SARS-related risks, beside an increased risk for subsequent alcohol abuse/dependence. This latter resulted significantly related with hyper-arousal symptoms. A further study in Toronto (Styra et al., 2008) confirmed the impact of operating in a high-risk unit, and first reported that caring for only one SARS patient was related to a higher risk than caring for multiple SARS patients. A recent study on 147 nurses who worked in MERS units during the outbreak found higher PTSD rates among emergency HCWs than among non-emergency ones (Jung et al., 2020). To date, two studies have explored this issue in the COVID-19 pandemic. Li et al. (2020) found among 526 nurses, that those who worked on the frontline appeared to be less prone to developing PTSS compared to second-line ones; conversely Kang et al. (2020) in a large study on 994 HCWs in Wuhan reported the exposure level to infected people, more broadly including colleagues, relatives or friends, to be a risk factor for mental health problems, including PTSS.
3.3.2. Occupational role
Five studies, four on the SARS epidemic and one on the COVID-19 pandemic, highlighted the occupational role as a major risk factor for PTSD or PTSS in Coronavirus outbreaks. Maunder et al. (2004) found on a sample of 1557 HCWs collected in Toronto, higher PTSS rates among nurses and explained this finding by means of the longer contact and higher exposure to patients of the nursing staff. A study on 96 emergency HCWs, assessed six months after the 2003 SARS outbreak, revealed a greater burden of PTSS among nurses than among physicians (Tham et al., 2004). A further study by Phua et al. (2005) confirmed this finding in a sample of 99 HCWs. Finally, a most recent study on 1257 hospital physicians and nurses caring for COVID-19 patients reached the same conclusion (Lai et al., 2020).
3.3.3. Age and gender
Three studies on the SARS outbreak and one on the COVID-19 pandemic reported that younger HCWs had a greater risk of developing PTSS (Sim et al., 2004; Su et al., 2007; Wu et al., 2009). From a wider perspective, further studies pointed out an association between fewer years of work experience and an increased PTSS risk in HCWs, as described in two SARS studies (Chong et al., 2004; Lancee et al., 2008) and in one COVID-19 study (Lai et al., 2020). As far as gender is concerned, while one recent study on COVID-19 reported a higher risk for the female HCWs, a previous study involving 1257 HCWs in a tertiary hospital affected by SARS found an increased risk of PTSS among males (Chong et al., 2004).
3.3.4. Marital status
Three studies focused on the relevance of marital status, two of which referred to the SARS outbreaks and one to the current COVID-19 pandemic. Chan and Huak (2004) in a study on 661 HCWs in Singapore showed that those who were not married were more adversely affected than married ones. In contrast, a further study in Singapore (Sim et al., 2004) found a positive association between post-traumatic morbidities and being married. Likewise, a recent case control study on HCWs facing the COVID-19 pandemic showed that married, divorced or widowed operators reported higher scores in vicarious traumatization symptoms compared to unmarried HCWs (Li et al., 2020).
3.3.5. Quarantine, isolation and stigma
Three SARS studies on Chinese hospital staff members (Bai et al., 2004; Reynolds et al., 2007; Wu et al., 2009) and one on the MERS outbreak (Lee et al., 2018) consistently reported high levels of PTSS among HCWs who had been quarantined. More specifically, Bai et al. (2004) examining 338 HCWs in an East Taiwan hospital found that 5% of them suffered from acute stress disorder, with quarantine being the most frequently associated factor, and a further 20% felt stigmatized and rejected in their neighborhood because of their hospital work, with also 9% reporting reluctance to work and/or considering quitting their job. Similar findings emerged from a Canadian SARS study on 1057 subjects (Reynolds et al., 2007), in which quarantined HCWs reported more PTSS than non-HCWs quarantined individuals. Moreover, in a study on MERS outbreak, Lee et al. (2018) assessed PTSS experienced by 359 university HCWs who cared for infected patients, observing that quarantined HCWs had a higher risk of developing PTSS which persisted over time, particularly sleep and numbness-related symptoms. More in general, social isolation and separation from family was found to be associated with higher rates of PTSS in SARS outbreak, as well as having friends or close relatives with the infection (Maunder et al., 2004; Chong et al., 2004; Wu et al., 2009).
3.3.6. Previous psychiatric disorders
Three studies on SARS have stressed the presence of previous psychiatric disorders as a risk factor for the development of PTSS (Sim et al., 2004; Su et al., 2007; Lancee et al., 2008). Accordingly, Su et al. (2007) on a sample of 70 nurses from two SARS units and 32 nurses from two non-SARS units found highlighted a previous history of mood disorders as a major risk factor for PTSS. One study on MERS outbreak confirmed this finding (Jung et al., 2020).
3.4. PTSD and PTSS resilience factors of in HCWs facing the three coronavirus outbreaks
3.4.1. Family and social support
Two studies on the SARS outbreak highlighted the support of family and friends as having a major role in protecting from PTSS development (Chan and Huak, 2004; Su et al., 2007). In particular, Su et al. (2007) investigating 102 nurses found that strong social and family support protected against acute stress, with a positive impact on their global functioning as a function of time.
3.4.2. Supervisors and colleagues support
Three researches concerning the SARS outbreak (Chan and Huak, 2004; Maunder et al., 2006; Lancee et al., 2008) and one on the MERS (Jung et al., 2020), reported a protective role of the support from supervisors/colleagues. Particularly, Lancee et al. (2008), in 139 HCWs in Canada, showed feeling well supported while working as a resilience factor also in the long-term. Jung et al. (2020) noticed that management strategies based on supervisors’ support proved helpful in order to reduce PTSS in 147 nurses in three isolation hospitals in South Korea during the MERS outbreak.
3.4.3. Training
The perception of being adequately trained was identified as a potentially protective factor in two studies on the SARS (Maunder et al., 2006; Lancee et al., 2008)., Comparing 769 Canadian HCWs displaced in 9 hospitals that treated SARS patients and 4 hospitals that did not, from 13 to 26 months after the outbreak, Maunder et al. (2006) suggested the importance of supportive interventions in preventing PTSD and PTSS with particular impact on maladaptive coping styles.
3.4.4. Work organization
The same authors reported that working in structured units and the perceived safety of the working environment are further factors which seem to enhance the resilience of HCWs, in line with findings of another study by Su et al., 2007). Moreover, it has also been observed that a clear communication of directives and precautionary measures to be adopted was related to a better outcome with regard to PTSS (Chan and Huak, 2004).
3.4.5. Coping strategies
In five studies on the SARS outbreak (Chan and Huak 2004; Sim et al., 2004; Phua et al., 2005; Su et al., 2007; Wu et al., 2009), positive coping strategies were reported to be a protective factor against the development of PTSD psychopathology. Particularly, in a study carried out in Singapore on 41 physicians and 58 nurses, Phua et al. (2005) reported an association between the use of humor and planning as coping strategies, and lower rates of PTSD. Other protective coping styles included: the altruistic acceptance of work-related risks (Wu et al., 2009), the ability to talk to someone about their experiences, and the presence of religious beliefs (Chan and Huak 2004). Accordingly, Maunder et al. (2006) found that maladaptive coping strategies, such as avoidance, hostile confrontation and self-blame, resulted in worse outcomes in terms of PTSS and Sim et al. (2004) reported that less venting, humor and acceptance were associated to higher levels of PTSS. Consistently, positive coping strategies, such as motivation to learning different skills, have been indicated as resilience factors also in HMWs dealing with the current COVID-19 pandemic (Kang et al., 2020).
3.5. HCWs survivors to coronavirus outbreaks
Five studies focusing on HCWs who survived the SARS infection highlighted this population as particularly “at risk” for PTSD. Kwek et al. (2006) in a sample of SARS survivors at 3 months post-discharge found that HCWs were more affected by PTSS than non-HCWs. Lee et al. (2007) examined a sample of 96 Hong Kong SARS survivors divided into sub-samples of HCWs and non-HCWs, found that while PTSS levels were similar in the two sub-samples at the peak of the outbreak, HCWs compared to non-HCWs, reported significantly higher PTSS one year after discharge, suggesting a lack of recovery as a function of time, among HCW SARS survivors. In line with this, a later study among 233 Chinese SARS survivors also reported a higher risk of PTSD among HCW compared to non-HCW (Wing and Leung, 2012). Furthermore, a study conducted on a sample of 90 Hong Kong SARS survivors at 30 months after the outbreak (Mak et al., 2010) showed that being a HCW was significantly associated with PTSD development, despite the authors hypothesizing that this finding could be gender-biased because the majority of the sample was made up of female HCWs. Finally, Ho et al. (2005) in 97 HCWs in Hong Kong found a positive correlation between the presence of pronounced SARS-related fears and PTSS burden, particularly intrusion symptoms; in addition HCWs who had recovered from SARS appeared to be more concerned about death, discrimination and quarantine than those who had not been infected.
4. Discussion
To the best of our knowledge we conducted the first review addressing PTSD and PTSS risk and resilience factors in HCWs who were involved in the three major recent Coronavirus outbreaks, namely the SARS, the MERS and the current COVID-19, which have affected the worldwide population in the last two decades. Converging data suggest a high risk for PTSD development among emergency HCWs, with studies consistently outlining several risk factors that are enhanced in the case of these highly lethal outbreaks, such as: the frequent unpredictability of daily caseloads, having to frequently manage patients and their families’ expectations in unexpected critical cases/situations (Mealer et al., 2009; Czaja et al., 2012; Iranmanesh et al., 2013; Fjeldheim et al., 2014). In the context of an outbreak emergency such as the COVID-19 crisis, difficulties are further heightened by the rapidly increasing flow of critical patients requiring increased medical attention, the decision-making burden and high daily fatality rates, and the constant updates of hospital procedures following advances in knowledge about the disease, that creates another burden for HCWs who need to keep up to date. Further, patients medical management requires tight physical isolation, to protect patients and HCWs because of the extremely high risk of contamination (Petrie et al., 2018; Berger et al., 2012; Brooks et al., 2019). Occupational role, marital status, age and gender, quarantine, stigma, previous psychiatric disorders, isolation and being survivors of the same outbreak also emerged as robust risk factors for PTSS. In parallel, the literature highlighted a number of resilience factors, such as support, training, prompt work organization and good coping strategies.
The majority of studies included in our review focused on the 2003 SARS outbreak; fewer data were available on the MERS, and the studies on COVID-19 are only emerging at the time of writing. All these studies reported a high risk for adverse psychological reactions, particularly PTSS and PTSD among HCWs, suggesting the proximity to “ground zero” as a primary risk factor (Kwek et al., 2006; Lee et al., 2018). HCWs’ fear of contagion and infection of their family, friends and colleagues, feelings of uncertainty, stigmatization and rejection in their neighborhood because of their hospital work were also reported. Studies also reported the reluctance to work and/or considering quitting their job, as well as high levels of stress, anxiety and depression symptoms, which could have long-term psychological implications (Maunder et al., 2003; Bai et al., 2004; Lee et al., 2007; Wu et al., 2009). The self-perceived high risk for contagion might be the most important aspect related to the front-line activities, with for example Su et al. (2007), failing to find any significant difference between HCWs in SARS vs. non-SARS units in PTSD prevalence rate. This suggests that not only HCWs working within the SARS units, but also those working outside them and facing uncertainty because of the displacement, might develop PTSS during the outbreak. In this regard, in the ongoing COVID-19 pandemic, the lack of personal protection devices represents a critical issue.
Interestingly, however, some authors found first-line exposure to have a protective effect. Styra et al. (2008) reported that HCWs working in SARS high risk units, as expected, experienced greater distress than HCWs displaced in other departments such as the psychiatric one, but contrary to expectations HCWs caring for many SARS patients while working in high-risk units emerged as being less distressed. This finding suggests that experience in treating SARS patients may be a mediating factor that could be amenable to intervention in future outbreaks. This is in line with more recent findings from a COVID-19 study, according to which PTSS severity of non-front-line nurses was greater than that of front-line nurses, who showed stronger psychological endurance. The authors argue that this finding may be explained considering that front-line nurses were voluntarily selected and provided with sufficient psychological preparation. Moreover, the selected front-line nurses were mainly middle-level backbone staff with working experience and psychological capacity (Li et al., 2020).
Hence, there is evidence that perceived adequacy of training represents a protective factor against adverse outcomes of traumatic exposure (Maunder et al., 2006; Lancee et al., 2008). Similarly, other factors concerning positive working organization, such as working in structured units, a sense of protection of environment (Maunder et al., 2006; Su et al., 2007) and clear communication of directives and of precautionary measures (Chan and Huak, 2004), have proven to be protective factors against the development of PTSS in HCWs. In particular, Chan and Huak (2004) explored the important role in preventing PTSS of clear and prompt communication of directives and information about the disease, of providing precautionary measures, such as Personal Protective Equipment (PPE), and of the support of a supervisor/head of department, colleagues and family. The support from family and friends as well as that from supervisors and colleagues has been shown to represent an important resilience factor against the development of PTSS, as widely demonstrated in the literature (Chan and Huak, 2004; Maunder et al., 2006; Su et al., 2007; Lancee et al., 2008). Nevertheless, this matter deserves further consideration since in this peculiar clinical setting the implications of the contagion risk often lead to self-isolation, with subsequent decreased social support.
Some important individual risk and resilience factors for PTSS have also been reported among HCWs facing a coronavirus outbreak. First, female gender. Despite the fact that the majority of the studies corroborate the preventive role of professional training as to PTSD onset up to the point of flattening of the gender gap which is commonly observed in PTSD reports, most of the studies on HCWs dealing with Coronavirus outbreaks tend to show a higher incidence of PTSD among women. Females, in fact, were shown to be most affected by PTSS in three SARS studies (Lee et al., 2007; Reynolds et al., 2007; Lai et al., 2020), as well as younger HCWs or HCWs with fewer years of work experience (Reynolds et al., 2007; Lancee et al., 2008). Moreover, nurses proved to be more affected by PTSS than other HCWs (Tham et al., 2004; Maunder et al., 2004). Although this has been explained as related to closer contact with infected patients, we may also argue that often the nurse staff are mostly women. Further studies in this regard are thus warranted. Outbreaks threatening family members’ well-being or affecting children's care, in fact, may constitute a burden for women (Carmassi et al., 2019). It is worthy of note that all these factors could be influenced by coping styles adopted by the HCWs to address the psychic burden of the outbreak. Some studies focused on positive coping styles that were associated to a better outcome (Phua et al., 2005; Wu et al., 2009). Among these, Phua et al. (2005) found that physicians chose humor as a coping strategy more frequently than nurses, and this resulted in lower post-traumatic stress morbidity. Other authors stressed the effect of maladaptive coping styles in predicting PTSS, such as avoidance, hostile confrontation and self-blame (Maunder et al., 2006).
As previously highlighted, the sense of isolation was found to be an important factor related to PTSS. Consequently, HCWs who had been quarantined were shown to be at higher risk (Bai et al., 2004) as well as HCW survivors from the infection. These latter constitute a special population in which the impact of infectious disease, along with related fears for one's health and for the contagion of loved ones and the sense of isolation and the rejection due to the stigma, lead to a greater PTSS burden (Wing and Leung, 2012).
More recently, scientists, clinicians and the general public, in fact, have been increasingly referring to the current COVID-19 emergency and its subsequent impact on health care systems, as the “9/11 of health care systems”. First studies reported high levels of psychopathological burden in HCWs dealing with the COVID-19 pandemic in China, including depression, anxiety, insomnia and PTSS (Huang et al., 2020; Kang et al., 2020; Lai et al., 2020). In particular, anxiety and PTSS symptoms resulted higher in females, nurses and in HCWs with fewer years of work experience (Lai et al., 2020; Huang et al., 2020). HCWs are called to confront this new scenario under widespread media coverage and in a context of a persisting imbalance between needs and resources, increasing the decisional burden and the feelings of hopelessness; they are also forced to deal with challenging expectations of the patients and their relatives in a framework characterized by unusual communicative constraints. Moreover, the fear of contagion is amplified by the lack of personal protective equipment (PPE) and the high number of infected or deceased colleagues, and is associated to the concern of representing a threat to family members: this often leads to self-isolation. As a consequence, loneliness, along with the risk of a growing trend towards social stigmatization of HCWs as potential carriers of infection (WHO, 2020) results in deprivation of social support, which is listed among the main factors of resilience.
Despite the slight decrease in the COVID-19 contagion rate, the impact on HCWs mental health may produce enduring effects. Finally, some evidence revealed a significant time-effect on reducing PTSD symptom ratings, as observed in a SARS study by Su et al. (2007), reporting a 50% decrease after one month, no-one meeting the criteria for PTSD. Conversely, a MERS study by Lee et al. (2018) reported that HCWs performing one month before MERS-related tasks were at higher risk for symptoms of PTSD even after time had passed, and the risk was increased in sleep and numbness-related symptoms, in particular if home quarantine was implemented.
For all these reasons, providing a timely response to psychological pressure on HCWs in order to prevent negative mental health outcomes requires the development of specific intervention strategies (Carmassi et al., 2020c). Such strategies cannot but be based on a careful survey of both risk and resilience factors that may be playing a role in this special working population and should take into account what the studies conducted in the aftermath of the previous outbreaks reported.
When discussing our results some limitations should be considered. First, the lack of a quality assessment of the studies. Second, we consulted only one database for our search (PubMed). Third, most of the included articles (N = 16) adopted the Impact of Event Scale scores, which is a well-known rating scale that provides a subjective measure of perceived stress (Horowitz et al., 1979; Marziali and Pilkonis, 1986; Weiss et al., 1984), to detect PTSD or PTSS. Fourth, surveys give us a limited glimpse into a complex psychological dynamic that happens with healthcare providers in isolation wards, because they rely on voluntary responses by the subjects, who may choose not to revisit a traumatic experience by participating in the survey, thus leading to under-reporting the incidence of traumatic sequelae (Li et al., 2020). This is in line with Chen et al. (2020) who reported how the implementation of psychological intervention services in the COVID-19 pandemic proved to be problematic, because medical staff were reluctant to participate in the group or individual psychology interventions provided to them. Fifth, some studies reported that while quarantined HCWs consistently showed more frequent adverse psychological impacts than non-HCWs, their experience was probably influenced by their job-related experiences with SARS and not unique to their HCW status (Reynolds et al., 2007). Finally, no information was available on HCW family members, particularly on the possible impact of the presence of children as a possible PTSS risk factor (Carmassi et al., 2019).
We have examined studies carried out in the context of the three Coronavirus outbreaks in order to outline PTSD and PTSS risk and resilience factors impacting on HCWs and to consistently enhance the effectiveness of intervention strategies. While the COVID-19 pandemic is straining healthcare systems all over the world, awareness of the impact of the emergency on the HCWs’ mental health is rising, consistently with evidence of the high risk of them developing psychological distress, such as PTSD and PTSS, under similar circumstances. To date, despite some recommendations released by international organizations (WHO, 2020; Inter-Agency Standing Committee (IASC) 2020; IFRC, 2020) and a variety of action proposals, a systematic approach is not yet in place. Efficacious treatments for PTSD and PTSS exist (Lee and Bowles, 2020; Charney et al., 2018; Dell'Osso et al., 2015), and healthcare systems should also focus on prepare to roll out these treatments among HCWs should prevention strategies fail to prevent the development of these conditions.
CRediT authorship contribution statement
Claudia Carmassi: Conceptualization, Methodology, Investigation, Writing - original draft, Writing - review & editing, Supervision. Claudia Foghi: Methodology, Investigation, Writing - original draft, Writing - review & editing. Valerio Dell'Oste: Conceptualization, Methodology, Investigation, Writing - original draft, Writing - review & editing. Annalisa Cordone: Investigation, Writing - original draft. Carlo Antonio Bertelloni: Investigation, Writing - original draft. Eric Bui: Conceptualization, Methodology, Writing - original draft, Writing - review & editing, Supervision. Liliana Dell'Osso: Conceptualization, Methodology, Writing - original draft, Supervision.
Declaration of Competing Interest
No conflict of interest. No disclosures to declare of any relationship with a commercial company that has a direct financial interest in subject matter or materials discussed in article or with a company making a competing product.
Acknowledgments
Financial support
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Ethical standards
Not applicable.
Acknowledgments
Dr. Julia Antonia Elizabeth Gray, native English speaker, revised the entire article.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.psychres.2020.113312.
Appendix. Supplementary materials
References
- Ager A., Pasha E., Yu G., Duke T., Eriksson C., Cardozo B.L. Stress, mental health, and burnout in national humanitarian aid workers in Gulu, Northern Uganda. J. Trauma Stress. 2012;25:713–720. doi: 10.1002/jts.21764. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association (APA) DSM-5. American Psychiatric Press; Washington DC: 2013. Diagnostic and statistical manual of mental disorders. [Google Scholar]
- Bai Y., Lin C.C., Lin C.Y., Chen J.Y., Chue C.M., Chou P. Survey of stress reactions among health care workers involved with the SARS outbreak. Psychiatr. Serv. 2004;55(9):1055–1057. doi: 10.1176/appi.ps.55.9.1055. [DOI] [PubMed] [Google Scholar]
- Bao Y., Sun Y., Meng S., Shi J., Lu L. 2019-nCoV epidemic: address mental health care to empower society. Lancet. 2020;395(10224):e37–e38. doi: 10.1016/S0140-6736(20)30309-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berger W., Coutinho E.S., Figueira I., Marques-Portella C., Luz M.P., Neylan T.C., Marmar C.R., Mendlowicz M.V. Rescuers at risk: a systematic review and meta-regression analysis of the worldwide current prevalence and correlates of PTSD in rescue workers. Soc. Psychiatry Psychiatr. Epidemiol. 2012;47(6):1001–1011. doi: 10.1007/s00127-011-0408-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonanno G.A., Galea S., Bucciarelli A., Vlahov D. What predicts psychological resilience after disaster? The role of demographics, resources, and life stress. J. Consult. Clin. Psychol. 2007;75(5):671–682. doi: 10.1037/0022-006X.75.5.671. [DOI] [PubMed] [Google Scholar]
- Brewin C.R., Andrews B., Rose S., Kirk M. Acute stress disorder and posttraumatic stress disorder in victims of violent crime. Am. J. Psychiatry. 1999;156:360–366. doi: 10.1176/ajp.156.3.360. [DOI] [PubMed] [Google Scholar]
- Brooks S.K., Rubin G.J., Greenberg N. Traumatic stress within disaster-exposed occupations: overview of the literature and suggestions for the management of traumatic stress in the workplace. Br. Med. Bull. 2019;129(1):25–34. doi: 10.1093/bmb/ldy040. [DOI] [PubMed] [Google Scholar]
- Bryant R.A. Post-traumatic stress disorder: a state-of-the-art review of evidence and challenges. World Psychiatry. 2019;18(3):259–269. doi: 10.1002/wps.20656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmassi C., Barberi F.M., Cordone A., Maglio A., Dell’Oste V., Dell’Osso L. Trauma, PTSD and post-traumatic stress spectrum: 15 years’ experience on a multidimensional approach to trauma related psychopathology. Journal of Psychopathology. 2020;26(1):4–11. doi: 10.36148/2284-0249-376. [DOI] [Google Scholar]
- Carmassi C., Bertelloni C.A., Gesi C., Conversano C., Stratta P., Massimetti G., Rossi R., Dell’Osso L. New DSM-5 PTSD guilt and shame symptoms among Italian earthquake survivors: Impact on maladaptive behaviors. Psychiatry Research. 2017;251:142–147. doi: 10.1016/j.psychres.2016.11.026. [DOI] [PubMed] [Google Scholar]
- Carmassi C., Cerveri G., Bui E., Gesi C., Dell’Osso L. Defining Effective Strategies to Prevent Post-Traumatic Stress in Healthcare Emergency Workers Facing the COVID-19 Pandemic in Italy. CNS Spectrums. 2020:1–5. doi: 10.1017/S1092852920001637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmassi C., Corsi M., Bertelloni C.A., Pedrinelli V., Massimetti G., Peroni D.G., Bonuccelli A., Orsini A., Dell'Osso L. Post-traumatic stress and major depressive disorder in parent caregivers of children with a chronic disorder. Psychiatry Res. 2019;279:195–200. doi: 10.1016/j.psychres.2019.02.062. [DOI] [PubMed] [Google Scholar]
- Carmassi C., Gesi C., Corsi C., Cremone I.M., Bertelloni C.A., Massimetti E., Olivieri M.C., Conversano C., Santini M., Dell’Osso L. Exploring PTSD in emergency operators of a major University Hospital in Italy: a preliminary report on the role of gender, age, and education. Ann Gen Psychiatry. 2018;17:17. doi: 10.1186/s12991-018-0184-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmassi C., Gesi C., Simoncini M., Favilla L., Massimetti G., Olivieri M.C., Conversano C., Santini M., Dell'Osso L. DSM-5 PTSD and posttraumatic stress spectrum in Italian emergency personnel: correlations with work and social adjustment. Neuropsychiatr. Dis. Treat. 2016;12:375–381. doi: 10.2147/NDT.S97171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmassi C., Rossi A., Pedrinelli V., Cremone I.M., Dell’Oste V., Stratta P., Bertelloni C.A., Dell’Osso L. PTSD in the aftermath of a natural disaster: what we learned from the Pisa-L’Aquila Collaboration Project. J. Psychopathol. 2020;26(1):99–106. doi: 10.36148/2284-0249-377. [DOI] [Google Scholar]
- Chan A.O., Huak C.Y. Psychological impact of the 2003 severe acute respiratory syndrome outbreak on health care workers in a medium size regional general hospital in Singapore. Occup. Med. 2004;54(3):190–196. doi: 10.1093/occmed/kqh027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charney M.E., Hellberg S.N., Bui E., Simon N.M. Evidenced-based treatment of posttraumatic stress disorder: an updated review of validated psychotherapeutic and pharmacological approaches. Harv. Rev. Psychiatry. 2018;26(3):99–115. doi: 10.1097/HRP.0000000000000186. [DOI] [PubMed] [Google Scholar]
- Chen Q., Liang M., Li Y., Guo J., Fei D., Wang L., He L., Sheng C., Cai Y., Li X., Wang J., Zhang Z. Mental health care for medical staff in China during the COVID-19 outbreak. The Lancet Psychiatry. 2020;7(4):e15–e16. doi: 10.1016/S2215-0366(20)30078-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chong M.Y., Wang W.C., Hsieh W.C., Lee C.Y., Chiu N.M., Yeh W.C., Huang O.L., Wen J.K., Chen C.L. Psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. Br. J. Psychiatry. 2004;185:127–133. doi: 10.1192/bjp.185.2.127. [DOI] [PubMed] [Google Scholar]
- Cieslak R., Shoji K., Douglas A., Melville E., Luszezynska A., Benight C.C. A meta-analysis of the relationship between job bournout and secondary traumatic stress among workers with indirect exposure to trauma. Psychol. Serv. 2014;11(1):75. doi: 10.1037/a0033798. [DOI] [PubMed] [Google Scholar]
- Cleary M., Kornhaber R., Thapa D.K., West S., Visentin D. The effectiveness of interventions to improve resilience among health professionals: a systematic review. Nurse Educ. Today. 2018;71:247–263. doi: 10.1016/j.nedt.2018.10.002. [DOI] [PubMed] [Google Scholar]
- Clohessy S., Ehlers A. PTSD symptoms, response to intrusive memories and coping in ambulance service workers. Br. J. Clin. Psychol. 1999;38(3):251–265. doi: 10.1348/014466599162836. [DOI] [PubMed] [Google Scholar]
- Colville G., Smith J., Brierley J., Citron K., Nguru N.M., Shaunak P.D., Tam O., Perkins-Porras L. Coping with staff burnout and work-related posttraumatic stress in intensive care. Pediatric Crit. Care Med. 2017;18:e267–e273. doi: 10.1097/PCC.0000000000001179. [DOI] [PubMed] [Google Scholar]
- Crabbe J.M., Bowley D.M., Boffard K.D., Alexander D.A., Klein S. Are health professionals getting caught crossfire? The personal implications of caring for trauma victims. Emerg. Med. J. 2004;21(5):568–572. doi: 10.1136/emj.2003.008540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craun S., Bourke M. The use of humor to cope with secondary traumatic stress. J. Child Sex Abuse. 2014;23:840–852. doi: 10.1080/10538712.2014.949395. [DOI] [PubMed] [Google Scholar]
- Czaja A., Moss M., Mealer M. Symptoms of post-traumatic stress disorder among pediatric acute care nurses. J. Pediatr. Nurs. 2012;27(4):357–365. doi: 10.1016/j.pedn.2011.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Wit E., van Doremalen N., Falzarano D., Munster V.J. SARS and MERS: recent insights into emerging coronaviruses. Nat. Rev. Microbiol. 2016;14:523–534. doi: 10.1038/nrmicro.2016.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dell'Osso B., Albert U., Atti A.R., Carmassi C., Carrà G., Cosci F., Del Vecchio V., Di Nicola M., Ferrari S., Goracci A., Iasevoli F., Luciano M., Martinotti G., Nanni M.G., Nivoli A., Pinna F., Poloni N., Pompili M., Sampogna G., Tarricone I., …, Fiorillo A. Bridging the gap between education and appropriate use of benzodiazepines in psychiatric clinical practice. Neuropsychiatr. Dis. Treat. 2015;11:1885–1909. doi: 10.2147/NDT.S83130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeLucia J.A., Bitter C., Fitzgerald J., Greenberg M., Dalwari P., Buchanan P. Prevalence of post-traumatic stress disorder in emergency physicians in the United States. West J. Emerg. Med. 2019;20(5):740–746. doi: 10.5811/westjem.2019.7.42671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein R.M., Krasner M.S. Physician resilience: what it means, why it matters, and how to promote it. Acad. Med. 2013;88(3):301–303. doi: 10.1097/acm.0b013e318280cff0. [DOI] [PubMed] [Google Scholar]
- Figley, C.R., 1995. Compassion fatigue: coping with secondary traumatic stress disorder in those who treat the traumatized. New York: Brunner-Mazel.
- Fjeldheim C.B., Nöthling J., Pretorius K., Basson M., Ganasen K., Heneke R., Cloete K.J., Seedat S. Trauma exposure, posttraumatic stress disorder and the effect of explanatory variables in paramedic trainees. BMC Emerg. Med. 2014;14:11. doi: 10.1186/1471-227X-14-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garbern S.C., Ebbeling L.G., Bartels S.A. A systematic review of health outcomes among disaster and humanitarian responders. Prehosp. Disaster Med. 2016;31(6):635–642. doi: 10.1017/S1049023X16000832. [DOI] [PubMed] [Google Scholar]
- Grevin F. Posttraumatic stress disorder, ego defense mechanisms, and empathy among urban paramedics. Psychol. Rep. 1996;79:483–495. doi: 10.2466/pr0.1996.79.2.483. [DOI] [PubMed] [Google Scholar]
- Haber Y., Palgi Y., Hamama-Raz Y., Shrira A., Ben-Ezra M. Predictors of professional quality of life among physicians in a conflict setting: the role of risk and protective factors. Isr. J. Psychiatry Relat. Sci. 2013;50:174–181. [PubMed] [Google Scholar]
- Hamid A., Musa S. The mediating effects of coping strategies on the relationship between secondary traumatic stress and burnout in professional caregivers in the UAE. J. Ment. Health. 2017;26:28–35. doi: 10.1080/09638237.2016.1244714. [DOI] [PubMed] [Google Scholar]
- Hegg-Deloye S., Brassard P., Jauvin N., Prairie J., Larouche D., Poirier P., Tremblay A., Corbeil P. Current state of knowledge of post-traumatic stress, sleeping problems, obesity and cardiovascular disease in paramedics. Emerg. Med. J. 2013;31(3):242–247. doi: 10.1136/emermed-2012-201672. [DOI] [PubMed] [Google Scholar]
- Ho S.M., Kwong-Lo R.S., Mak C.W., Wong J.S. Fear of severe acute respiratory syndrome (SARS) among health care workers. J. Consult. Clin. Psychol. 2005;73(2):344–349. doi: 10.1037/0022-006X.73.2.344. [DOI] [PubMed] [Google Scholar]
- Horowitz M., Wilner N., Alvarez W. Impact of event scale: a measure of subjective stress. Psychosom. Med. 1979;41(3):209–218. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- Inter-Agency Standing Committee (IASC), 2020. Briefing note on addressing mental health and psychosocial aspects of COVID-19 Outbreak-Version 1.1. https://interagencystandingcommittee.org/iasc-reference-group-mental-health-and-psychosocial-support-emergency-settings/interim-briefing.
- International Federation of Red Cross and Red Crescent Societies (IFRC), 2020. Mental health and psychosocial support for staff, volunteers and communities in anoutbreakof novel Coronavirus. https://pscentre.org/wp-content/uploads/2020/02/MHPSS-in-nCoV-2020_ENG-1.pdf.
- Huang J.Z., Han M.F., Luo T.D., Ren A.K., Zhou X.P. [Mental health survey of medical staff in a tertiary infectious disease hospital for COVID-19] Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi. 2020;38(3):192–195. doi: 10.3760/cma.j.cn121094-20200219-00063. [DOI] [PubMed] [Google Scholar]
- Iranmanesh S., Tirgari B., Sheikh H. Post-traumatic stress disorder among paramedic and hospital emergency personnel in south-east. World J. Emerg. Med. 2013;4(1):26–31. doi: 10.5847/wjem.j.issn.1920-8642.2013.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jung H., Jung S.Y., Lee M.H., Kim M.S. Assessing the presence of post-traumatic stress and turnover intention among nurses post-Middle East respiratory syndrome outbreak: the importance of supervisor support. Workplace Health Saf. 2020;68(7):337–345. doi: 10.1177/2165079919897693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang L., Ma S., Chen M., Yang J., Wang Y., Li R., Yao L., bai H., Cai Z., Xiang Yang B., Hu S., Zhang K., Wang G., Ma C., Liu Z. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: a cross-sectional study. Brain Behav. Immun. 2020;87:11–17. doi: 10.1016/j.bbi.2020.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karanikola M., Giannakopoulou M., Mpouzika M., Kaite C.P., Tsiaousis G.Z., Papathanassoglou E.D. Dysfunctional psychological responses among Intensive Care Unit nurses: asystematic review of the literature. Rev. Esc. Enferm. USP. 2015;49(5):847–857. doi: 10.1590/S0080-623420150000500020. [DOI] [PubMed] [Google Scholar]
- Kwek S.K., Chew W.M., Ong K.C., Ng A.W., Lee L.S., Kaw G., Leow M.K. Quality of life and psychological status in survivors of severe acute respiratory syndrome at 3 months postdischarge. J. Psychosom. Res. 2006;60(5):513–519. doi: 10.1016/j.jpsychores.2005.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai J., Ma S., Wang Y., Cai Z., Hu J., Wu J., Du H., Chen T., Li R., Tan H., Kang L., Yao L., Huang M., Wang H., Wang G., Liu Z., Hu S. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw. Open. 2020;3(3) doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lancee W.J., Maunder R.G., Goldbloom D.S. Coauthors for the impact of SARS study, 2008. Prevalence of psychiatric disorders among Toronto hospital workers one to two years after the SARS outbreak. Psychiatr. Serv. 2008;59(1):91–95. doi: 10.1176/ps.2008.59.1.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee A.M., Wong J.G., McAlonan G.M., Cheung V., Cheung C., Sham P.C., Chu C.-M., Wong P.-C., Tsang K.W.T., Chua S.E. Stress and psychological distress among SARS survivors 1 year after the outbreak. Can. J. Psychiatry. 2007;52(4):233–240. doi: 10.1177/070674370705200405. [DOI] [PubMed] [Google Scholar]
- Lee E., Bowles K. Navigating treatment recommendations for PTSD: a rapid review. Int. J. Ment. Health. 2020:1–41. doi: 10.1080/00207411.2020.1781407. [DOI] [Google Scholar]
- Lee S.M., Kang W.S., Cho A.R., Kim T., Park J.K. Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Compr. Psychiatry. 2018;87:123–127. doi: 10.1016/j.comppsych.2018.10.003. 10.1016/j.comppsych.2018.10.003 PMCID: PMC7094631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung G.M., Hedley A.J., Ho L.M., Chau P., Wong I.O., Thach T.Q., Ghani A.C., Donnelly C.:.A., Fraser C., Riley S., Ferguson N.M., Anderson R.M., Tsang T., Leung P.Y., Wong V., Chan J.C., Tsui E., Lo S.V., Lam T.H. The epidemiology of severe acute respiratory syndrome in the 2003 Hong Kong epidemic: an analysis of all 1755 patients. Ann. Intern. Med. 2004;141(9):662–673. doi: 10.7326/0003-4819-141-9-200411020-00006. [DOI] [PubMed] [Google Scholar]
- Li Z., Ge J., Yang M., Feng J., Qiao M., Jiang R., Bi J., Zhan G., Xu X., Wang L., Zhou Q., Zhou C., Pan Y., Liu S., Zhang H., Yang J., Zhu B., Hu Y., Hashimoto K., Jia Y., Wang H., Wang R., Liu C., Yang C. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain Behav. Immun. S. 2020;0889-1591(20) doi: 10.1016/j.bbi.2020.03.007. 30309-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin C.Y., Peng Y.C., Wu Y., Chang J., Chan C.H., Yang D.Y. The psychological effect of severe acute respiratory syndrome on emergency department staff. Emerg. Med. J. 2007;24(1):12–17. doi: 10.1136/emj.2006.035089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu Y.C., Shu B.C., Chang Y.Y., Lung F.W. The mental health of hospital workers dealing with severe acute respiratory syndrome. Psychother. Psychosom. 2006;75(6):370–375. doi: 10.1159/000095443. [DOI] [PubMed] [Google Scholar]
- Machado D.A., Figueiredo N.M.A., Velasques L.S., Bento C.A.M., Machado W.C.A., Vianna L.A.M. Cognitive changes in nurses working in intensive care units. Rev. Bras. Enferm. 2018;71(1):73–79. doi: 10.1590/0034-7167-2016-0513. [DOI] [PubMed] [Google Scholar]
- Mak I.W., Chu C.M., Pan P.C., Yiu M.G., Ho S.C., Chan V.L. Risk factors for chronic post-traumatic stress disorder (PTSD) in SARS survivors. Gen. Hosp. Psychiatry. 2010;32(6):590–598. doi: 10.1016/j.genhosppsych.2010.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin C.E., Vujanovic A.A., Paulus D.J., Bartlett B., Gallagher M.W., Tran J.K. Alcohol use and suicidality in firefighters: associations with depressive symptoms and posttraumatic stress. Comp. Psych. 2017;74:44–52. doi: 10.1016/j.comppsych.2017.01.002. [DOI] [PubMed] [Google Scholar]
- Marziali E.A., Pilkonis P.A. The measurement of subjective response to stressful life events. J. Human Stress. Spring. 1986;12(1):5–12. doi: 10.1080/0097840X.1986.9936760. [DOI] [PubMed] [Google Scholar]
- Maunder R.G., Hunter J., Vincent L., Bennett J., Peladeau N., Leszcz M., Sadavoy J., Verhaeghe L.M., Steinberg R., Mazzulli T. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ. 2003;168(10):1245‐51. [PMC free article] [PubMed] [Google Scholar]
- Maunder R.G., Lancee W.J., Balderson K.E., Bennett J.P., Borgundvaag B., Evans S., Fernandes C.M.B., Goldbloom D.S., Gupta M., Hunter J.J., McGillis Hall L., Nagle L.M., Pain C., Peczeniuk S.S., Raymond G., Read N., Rourke S.B., Steinberg R.J., Stewart T.E., VanDeVelde-Coke S., Veldhorst G.G., Wasylenki D.A. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg. Infect. Dis. 2006;12(12):1924–1932. doi: 10.3201/eid1212.060584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maunder R.G., Rourke S., Hunter J.J., Goldbloom D., Balderson K., Petryshen P., Steinberg R., Wasylenki D., Koh D., Fones C.S. Factors associated with the psychological impact of severe acute respiratory syndrome on nurses and other hospital workers in Toronto. Psychosom. Med. 2004;66(6):938–942. doi: 10.1097/01.psy.0000145673.84698.18. [DOI] [PubMed] [Google Scholar]
- McAlonan G.M., Lee A.M., Cheung V., Cheung C., Tsang K.W.T., Sham P.C., Chua S.E., Wong J.G.W.S. Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Can. J. Psychiatry. 2007;52(4):241–247. doi: 10.1177/070674370705200406. [DOI] [PubMed] [Google Scholar]
- McGarry S., Girdler S., McDonald A., Valentine J., Lee S.L., Blair E., Wood F., Elliott C. Paediatric health-care professionals: relationships between psychological distress, resilience and coping skills. J. Paediatr. Child. Health. 2013;49:725–732. doi: 10.1111/jpc.12260. [DOI] [PubMed] [Google Scholar]
- Mealer M., Burnham E.L., Goode C.J., Rothbaum B., Moss M. The prevalence and impact of post traumatic stress disorder and burnout syndrome in nurses. Depress. Anxiety. 2009;26(12):1118–1126. doi: 10.1002/da.20631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzla J., Altman D.G. The PRISMA Group preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS. Med. 2009;6 [PMC free article] [PubMed] [Google Scholar]
- Nishiura H. The extent of transmission of novel coronavirus in Wuhan. China. J. Clin. Med. 2020;9:330. doi: 10.3390/jcm9020330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozer E.J., Best S.R, Lipsey T.L., Weiss D.S. Predictors of posttraumatic stress disorder and symptoms in adults: a meta-analysis. Psychol. Bull. 2003;129(1):52–73. doi: 10.1037/0033-2909.129.1.52. [DOI] [PubMed] [Google Scholar]
- Peeri N.C., Shrestha N., Rahman M.S., Zaki R., Tan Z., Bibi S., Baghbanzadeh M., Aghamohammadi N., Zhang W., Haque U. The SARS, MERS and novel coronavirus (COVID-19) epidemics, the newest and biggest global health threats: what lessons have we learned. Int. J. Epidemiology. 2020 doi: 10.1093/ije/dyaa033. Int J Epidemiol. dyaa033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perlman S.E., Friedman S., Galea S., Nair H.P., Eros-Samyal M., Stellman S.D., Hon J., Greene C.M. Short-term and medium-term health effects of 9/11. Lancet. 2011;378(9794):925–934. doi: 10.1016/S0140-6736(11)60967-7. [DOI] [PubMed] [Google Scholar]
- Petrie K., Milligan-Saville J., Gayed A., Deady M., Phelps A., Dell L., Forbes D., Bryant R.A., Calvo R.A., Glozier N., Harvey S.B. Prevalence of PTSD and common mental disorders amongst ambulance personnel: a systematic review and meta-analysis. Soc. Psychiatry Psychiatr. Epidemiol. 2018;53(9):897–909. doi: 10.1007/s00127-018-1539-5. [DOI] [PubMed] [Google Scholar]
- Phua D.H., Tang H.K., Tham K.Y. Coping responses of emergency physicians and nurses to the 2003 severe acute respiratory syndrome outbreak. Acad. Emerg. Med. 2005;12(4):322–328. doi: 10.1197/j.aem.2004.11.015. [DOI] [PubMed] [Google Scholar]
- Reynolds D.L., Garay J.R., Deamond S.L., Moran M.K., Gold W., Styra R. Understanding, compliance and psychological impact of the SARS quarantine experience. Epidemiol. Infect. 2007;136(7):997–1007. doi: 10.1017/S0950268807009156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson N., Perry A. Institutionally based health care workers' exposure to traumatogenic events:systematic review of PTSD presentation. J. Trauma Stress. 2010;23(3):417–420. doi: 10.1002/jts.20537. [DOI] [PubMed] [Google Scholar]
- Sim K., Chong P.N., Chan Y.H., Soon W.S. Severe acute respiratory syndrome-related psychiatric and posttraumatic morbidities and coping responses in medical staff within a primary health care setting in Singapore. J. Clin. Psychiatry. 2004;65(8):1120–1127. doi: 10.4088/jcp.v65n0815. [DOI] [PubMed] [Google Scholar]
- Styra R., Hawryluck L., Robinson S., Kasapinovic S., Fones C., Gold W.L. Impact on health care workers employed in high-risk areas during the Toronto SARS outbreak. J. Psychosom. Res. 2008;64(2):177–183. doi: 10.1016/j.jpsychores.2007.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Su T.P., Lien T.C., Yang C.Y., Su Y.L., Wang J.H., Tsai S.L., Yin J.C. Prevalence of psychiatric morbidity and psychological adaptation of the nurses in a structured SARS caring unit during outbreak: a prospective and periodic assessment study in Taiwan. J. Psychiatr. Res. 2007;41(1–2):119–130. doi: 10.1016/j.jpsychires.2005.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tham K.Y., Tan Y.H., Tang H.K. Psychological morbidity among emergency department doctors and nurses after the SARS outbreak. Hong Kong J. Emerg. Med. 2004;12(4):215–223. doi: 10.1177/102490790501200404. [DOI] [PubMed] [Google Scholar]
- Vance M.C., Kovachy B., Dong M., Bui E. Peritraumatic distress: a review and synthesis of 15 years of research. J. Clin. Psychol. 2018;74(9):1457–1484. doi: 10.1002/jclp.22612. [DOI] [PubMed] [Google Scholar]
- Wang C. A novel coronavirus outbreak of global health concern. Lancet. 2020;395:470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss D.S., Horowitz M.J., Wilner N. The stress response rating scale: a clinician's measure for rating the response to serious life-events. Br. J. Clin. Psychol. 1984;23(Pt 3):202–215. [PubMed] [Google Scholar]
- Wing Y.K., Leung C.M. Mental health impact of severe acute respiratory syndrome: a prospective study. Hong Kong Med. J. 2012;18(Suppl 3):24–27. [PubMed] [Google Scholar]
- Winkel A.F., Robinson A., Jones A.A., Squires A.P. Physician resilience: a grounded theory study of obstetrics and gynaecology residents. Med. Educ. 2019;53:184–194. doi: 10.1111/medu.13737. [DOI] [PubMed] [Google Scholar]
- World Health Organization, 2004. Summary of probable SARS cases with onset of illness from 1 November 2002 to 31 July 2003. http://www.who.int/csr/sars/country/table2004_04_21/en/.
- World Health Organization. 2020. Mental health and psychosocial considerations during the COVID-19 outbreak, 18 March 2020. https://apps.who.int/iris/handle/10665/331490.
- Wrenn G.L., Wingo A.P., Moore R., Pelletier T., Gutman A.R., Bradley B., Ressler K.J. Dr. Glenda L. Wrenn, The effect of resilience on posttraumatic stress disorder in trauma-exposed inner-city primary care patients. J. Natl. Med. Assoc. 2011;103(7):560–566. doi: 10.1016/s0027-9684(15)30381-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu P., Fang Y., Guan Z., Fan B., Kong J., Yao Z., Liu X., Fuller C.J., Susser E., Lu J., Hoven C.W. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can. J. Psychiatry. 2009;54(5):302–311. doi: 10.1177/070674370905400504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yehuda R., Hoge C., McFarlane A., Vermetten E., Lanius R.A., Nievergelt C.M., Hobfoll S.E., Koenen K.C., Neylan T.C., Hyman S.E. Post-traumatic stress disorder. Nat. Rev. Dis. Primers. 2015;1:150–157. doi: 10.1038/nrdp.2015.57. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.