Highlights
-
•
BAI score of respondents here is higher than those in previous studies with Chinese.
-
•
Quarantined people presented the highest BAI score and incidence of anxiety.
-
•
People in high epidemic area showed higher BAI score and incidence of anxiety.
-
•
All factors impacted respondents’ anxiety level significantly, except gender.
Keywords: COVID-19, Epidemic, Anxiety, General public, Psychosocial factors
Abstract
Background
COVID-19 outbreak happened last December in China and is still continuing. Here, we reported effects of COVID-19 outbreak on the mood of general public and ascertained impacts of psychosocial factors on the plague-related emotional measures.
Methods
During Feb. 4-6, 2020, a self-reported questionnaire Beck Anxiety Inventory (BAI) was disseminated to general public via Wechat, along with a sociodemographic information sheet. BAI score and incidences of moderate and severe anxiety in subgroups of respondents were compared. Multiple linear and logistic regressions were done for correlation analysis and to identify factors predictive of anxiety.
Results
Averaged BAI score of all respondents is higher than those of general public in two previous studies. The people quarantined for probable COVID-19 infection presented higher BAI score and incidences of moderate and severe anxiety relative to non-quarantined respondents. People in high epidemic area showed higher BAI score and incidences of moderate and severe anxiety compared to those in low epidemic area. Significant associations existed between anxiety level of the respondents and each of the investigated factors, except for gender. Quarantine was the predictor with a highest OR, followed by divorced/widow. The other factors showed smaller but significant effects on the anxiety level of respondents.
Limitations
This cross-sectional study was unable to track the emotional changes in the respondents over time. It had a relatively small sample and involved some of emotional measures only.
Conclusion
These data are of help in planning psychological interventions for the different subpopulations in general public during and after COVID-19 outbreak.
1. Introduction
In December 2019, clusters of patients with pneumonia of unknown pathogen were reported in Wuhan, China (Huang et al., 2020; Hui et al., 2020; Liu et al., 2020). The patients presented acute respiratory infection symptoms in early stages, and some of them rapidly developed acute respiratory distress syndrome, even respiratory failure, and other serious complications (Huang et al., 2020). The pathogen of the patients, however, was not identified until Jan 7, 2020, one week after an epidemiologic and etiologic investigation by an expert team from the Chinese Center for Disease Control and Prevention (China CDC). The team experts obtained throat swab samples from the patients and subsequently identified the pathogen of a novel coronavirus (Lu et al., 2020; Wu et al., 2020), which is named COVID-19 now.
Unfortunately, the COVID infection was spreading rapidly across the city and the other areas of Hubei province. Hundreds of people, including fifteen health workers in a tertiary hospital, had been infected and hospitalized for COVID-19 infection till the arrival of the second expert team from China CDC (Li et al., 2020). And what's worse, there were many more people who had been infected but showed no clinical symptoms. These people may transmit the viruses to many others thus led to wide spread of the infection in population (Special Expert Group for Control of the Epidemic of Novel Coronavirus Pneumonia of the Chinese Preventive Medicine Association, 2020). On Jan 23, therefore, the local bureaucracy of Wuhan sealed off the city from all outside contact to stop the spread of the plague, the highest response measure to curb outbreak and save lives.
Sealing off Wuhan city is an unprecedented event in the 70-years history of P. R. China. It changed all things in the city. Except for those relevant to the prevention and treatment of COVID-19 infection and daily supplies of people, no other things were allowed to be done. The vast majority of people were asked to stay at home. The entire metropolitan area was silence in the absence of working people and moving vehicles. Furthermore, the same stringent constraints were applied to all the other areas of Hubei province and the whole country a few days later. And these constraints are remaining in effect till now when the manuscript is being prepared.
While effectively blocking the spread of a plague, sealing off a whole metropolitan area may induce a lot of negative consequences. In addition to the catastrophic damage to local and national economy, sealing off a city would lead to panic in general public. In line with this notion, people showed feelings of extreme vulnerability, uncertainty and threat to life indicated by somatic and cognitive symptoms of anxiety in the initial phase of an outbreak, when the infection was spreading rapidly (Chong et al., 2004). In addition, general public were anxious due to implementation of a quarantine policy and the fear of infection. Some people were concerned with the demand for health care service which may overwhelm health resources (Bartholomew and Wessely, 2002). Moreover, some people in severe epidemic areas presented psychological problems because of perceiving life threat and low emotional support (Wu et al., 2005). During SARS outbreak in 2003, higher levels of anxiety was found to be related to the increased use of precautionary measures against SARS (severe acute respiratory syndrome), but not associated with a greater use of health services, in much of the general population (Blendon et al., 2004; Leung et al., 2003; Quah and Hin-Peng, 2004). More relevantly, Wang and colleagues (Wang et al., 2020) reported that 53.8% of the general public rated the psychological impact of the outbreak as moderate or severe and that 28.8% reported moderate to severe anxiety symptoms during the initial COVID-19 outbreak in China. Here, we reported the effect of COVID-19 outbreak on the mood of general public in China. The data were collected during Feb. 2-6, 2000, when people were asked to follow the stringent constraints set up by central and local governments during the epidemic period. We explored the involved mechanisms and ascertained psychosocial factors that influenced the COVID-19 outbreak-induced emotional consequences in general public.
2. Materials and methods
2.1. Participants
During Feb. 4-6, 2020, we disseminated a self-reported questionnaire Beck Anxiety Inventory (BAI) to general public in mainland, China, via Wechat. In addition, we asked participants to provide demographic information including gender, age, education level, marital status, living region, occupation (whether or not work at a hospital or receive medical education), quarantined or non-quarantined at the surveying time. No exclusion criteria were applied to participants except for one prerequisite of being ≥ 13 years old. Each participant was allowed to return one finished questionnaire only. All personal information provided by participants has been kept confidential and will not be used for any other purpose as stated in the study protocol, which was reviewed and approved by the Institutional Review Board of Mental Health Center, Shantou University Medical College, China. Six of all 2009 returns were invalid thus excluded from data analysis.
2.2. Subsamples of respondents
With the 2003 valid returns, respondents were classified into various subsamples according to the demographic information including gender (male and female), age (13-30, 31-50, and > 50 years old), education (high school or lower, college or higher), marital status (unmarried, married, and divorced/widow), location of residence (Hubei where first patients with COVID-19 infection were reported; high epidemic area including Guangdong, Henan, and Zhejiang provinces with more than 800 patients identified till midnight Feb. 6, 2020; and low epidemic area, i.e. the other areas in mainland, China), occupation (if work at hospital or study in medical school), and if quarantined during the survey time.
2.3. Assessment of anxiety level
To evaluate anxiety level of the participants in this study, the Chinese version of BAI, a structured self-reported questionnaire, was used. This version was successfully applied in previous studies with Chinese population (Huang et al., 2016a, 2016b). The BAI is comprised of 21 questions, each of which describes a common symptom of anxiety. The respondent was asked to rate how much he or she had been bothered by each symptom over the past week on a 4-point Likert-type (0-3). The total score has a range of 0–63 (Beck et al., 1988). By referring to a previous study, the BAI scores of respondents were categorized into four levels of none or normal (0-9), mild to moderate (10-18), moderate to severe (19-29), and severe anxiety (30-63) (Cheng et al., 2004).
2.4. Statistical analysis
Data were analyzed with the SPSS Version 15.0 (SPSS Inc, Chicago, Il, 2006). Descriptive statistics were used to characterize the sample's demographic profile and BAI scores of respondents. Normality was tested by the Kolmogorov-Smirnov test. Chi-square analyses (for categorical data) and two-tailed t-tests (for continuous data) were carried out. Multiple linear regression analysis was done for correlation analysis. Multivariate logistic regression analysis was performed to identify factors predictive of moderate and severe anxiety. The level of statistical significance was set to 0.05.
3. Results
3.1. Demographic characteristics of respondents
As shown in Table 1 , all respondents were divided into various subsamples in terms of gender, age, education level, marital status, occupation, location of residence, and if quarantined for probable COVID-19 infection. Each of subsamples accounted for different percentages in the whole sample.
Table 1.
Demographic characteristics of the respondents (N = 2003).
| Demographic factors | n | % |
|---|---|---|
| Gender: | ||
| Male | 719 | 35.90 |
| Female | 1284 | 64.10 |
| Age: years old | ||
| 13-30 | 1275 | 63.68 |
| 31-50 | 651 | 32.50 |
| type="Other">50 | 77 | 3.84 |
| Education level: | ||
| High school or below | 282 | 14.08 |
| College or above | 1721 | 85.92 |
| Marital status: | ||
| Unmarried | 1000 | 49.93 |
| Married | 961 | 47.98 |
| Divorced/widow | 42 | 2.10 |
| Occupation: | ||
| Health professional | 369 | 18.42 |
| The others | 1634 | 81.58 |
| Location of residence: | ||
| Hubei* | 83 | 4.14 |
| High epidemic area⁎⁎ | 611 | 30.50 |
| Low epidemic area⁎⁎⁎ | 1309 | 63.35 |
| If quarantined | ||
| No | 1982 | 98.95 |
| Yes | 21 | 1.05 |
Note:
Hubei is the infection focus where first patients with COVID-19 infection were reported.
high epidemic area refers to Guangdong, Henan, and Zhejiang provinces where more than 800 COVID-19 infected cases had been reported till midnight Feb. 6, 2020 when the data of this study were collected.
low epidemic area refers to the other regions of mainland, China, where relatively fewer patients were reported.
3.2. COVID-19 outbreak increased public anxiety level
First of all, we wondered if COVID-19 outbreak increased public anxiety during the survey period. For this purpose, we compared the averaged BAI score of all respondents in this study to that of healthy Chinese living in a non-epidemic area. We found this comparer in two previous studies (Huang et al., 2016a, 2016b) of 6.06 ± 7.15 (n =146) and 5.67 ± 6.82 (n = 179), respectively. The averaged BAI score of all respondents in this study is 7.10 ± 9.38 (n = 2003), which seems to be higher than those of general public reported in the aforementioned previous studies. The BAI scores of all respondents are shown in Table 2 , in which the respondents were classified into various subsamples as mentioned above.
Table 2.
BAI scores of respondents classified into various subsamples.
| BAI scores | ||||||
|---|---|---|---|---|---|---|
| Subsamples | 0 – 9 n (%) | 10 – 18 n (%) | 19 – 29 n (%) | 30 – 63 n (%) | X2 | p |
| Gender: | 5.936 | 0.115 | ||||
| Male (n = 719) | 563 (78.63) | 86 (11.96) | 23 (3.20) | 47 (6.54) | ||
| Female (n = 1284) | 998 (77.73) | 178 (13.86) | 51 (3.97) | 67 (4.44) | ||
| Age: years old | 14.226 | 0.027 | ||||
| 13 – 30 (n = 1275) | 991 (77.73) | 179 (14.04) | 47 (3.69) | 58 (4.55) | ||
| 31 – 50 (n = 651) | 500 (76.81) | 83 (12.75) | 24 (3.69) | 44 (6.76) | ||
| >50 (n = 77) | 70 (90.90) | 2 (2.60) | 3 (3.90) | 2 (2.60) | ||
| Education level: | 43.760 | <0.001 | ||||
| High school or below (n = 282) | 202 (71.63) | 30 (10.64) | 13 (4.61) | 37 (13.12) | ||
| College or above (n = 1721) | 1359 (78.97) | 234 (13.60) | 61 (3.55) | 67 (3.89) | ||
| Marital status: | 177.935 | <0.001 | ||||
| Unmarried (n = 1000) | 816 (81.86) | 144 (14.40) | 30 (3.00) | 10 (1.00) | ||
| Married (n = 961) | 726 (75.55) | 118 (12.28) | 41 (4.27) | 76 (7.91) | ||
| Divorced/widow (n = 42) | 19 (45.24) | 2 (4.76) | 3 (7.14) | 18 (42.86) | ||
| Occupation: | 20.434 | <0.001 | ||||
| Health professional (n = 369) | 266 (72.09) | 48 (13.01) | 23 (6.23) | 32 (8.67) | ||
| The others (n = 1634) | 1295 (79.25) | 216 (13.22) | 51 (3.12) | 72 (4.41) | ||
| Location of residence: | 40.811 | <0.001 | ||||
| Hubei (n = 83) | 63 (75.90) | 12 (14.46) | 4 (4.82) | 4 (4.82) | ||
| High epidemic area (n = 611) | 442 (72.34) | 80 (13.09) | 31 (5.07) | 58 (9.49) | ||
| Low epidemic area (n = 1309) | 1056 (80.67) | 172 (13.14) | 39 (2.98) | 42 (3.21) | ||
| If quarantined: | 101.483 | <0.001 | ||||
| No (n = 1982) | 1561 (78.76) | 260 (13.32) | 71 (3.58) | 90 (4.54) | ||
| Yes (n = 21) | 0 (0.00) | 4 (19.05) | 3 (14.29) | 14 (66.67) | ||
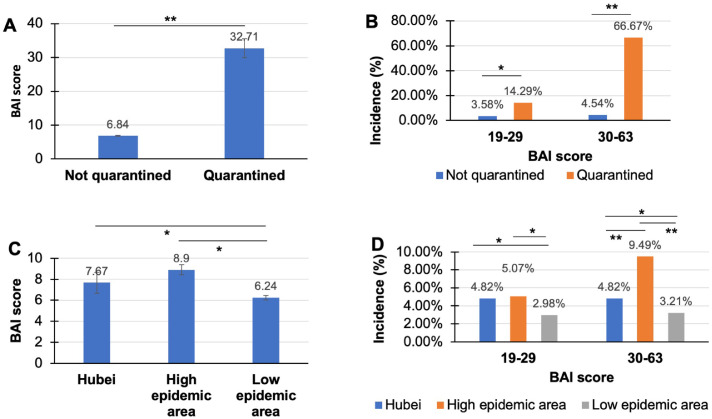
We expected that quarantine for probable COVID-19 infection would be a major contributor to the higher BAI score in the respondents of this study relative to those reported in the previous studies. As such, we compared the averaged BAI score of respondents who were quarantined to that of the others not-quarantined. As expected, people who were being quarantined presented a significantly higher BAI score relative to those not quarantined at the survey time (32.71 ± 12.51 vs 6.84 ± 8.60, p<0.01; Fig. 1 A). Furthermore, we compared the incidences of moderate (BAI = 19-29) and severe anxiety (BAI = 30-63) in people quarantined to the same indices in the respondents not quarantined. Obviously, people in the quarantine subsample presented significantly higher incidences of moderate and severe anxiety relative to the respondents who were not quarantined at the survey time (Fig. 1B).
Fig. 1.
COVID-19 outbreak increased anxiety level of general public. (A) Averaged BAI scores of quarantined and not quarantined subsamples. (B) Incidences of moderate and severe anxiety in quarantined and not quarantined subsamples. (C) Averaged BAI scores of respondents living in Hubei, high epidemic area, and low epidemic area. (D) Incidences of moderate and severe anxiety of respondents living in Hubei, high epidemic area, and low epidemic area. BAI scores were expressed as mean ± SEM and analyzed by two-tailed t-tests. Incidences of anxiety were analyzed by Chi-square. *p<0.05, **p<0.01.
Following the same rationale, we expected that people living in Hubei province and high epidemic area would have higher anxiety level relative to those living in low epidemic area. To test this assumption, we did comparisons among the three subsamples and found: (1) people in Hubei and the high epidemic area presented significantly higher BAI scores compared to that of people in low epidemic area (Fig. 1C); (2) people in Hubei and the high epidemic area presented significantly higher incidences of moderate and severe anxiety compared to those of people in low epidemic area (Fig. 1D).
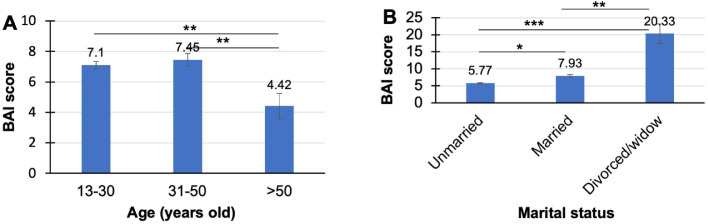
3.3. Psychosocial factors mediating the COVID-19 outbreak-induced anxiety in public
The next purpose of this study was to ascertain psychosocial factors that may mediate the COVID-19 infection-induced anxiety in public. To achieve this aim, we first compared the averaged BAI scores of different subsamples of all respondents in terms of the variables on the basis of which the classification was done. Of the five variables, only age and marital status showed significant effects on BAI score of the respondents. Specifically, people over 50 years showed significantly lower BAI score compared to people between 31-50 years and those between 13-30 years (Fig. 2 A). As for marital status, divorced individuals or widows showed the highest BAI score compared to unmarried and married people. Married people presented higher BAI score relative to unmarried persons (Fig. 2B).
Fig. 2.
Effects of age and marital status on averaged BAI score of the respondents. (A) Effect of age on averaged BAI score of respondents. (B) Effect of marital status on averaged BAI score of the respondents. BAI scores were expressed as mean ± SEM and analyzed by two-tailed t-tests. *p<0.05, **p<0.01, ***p<0.001.
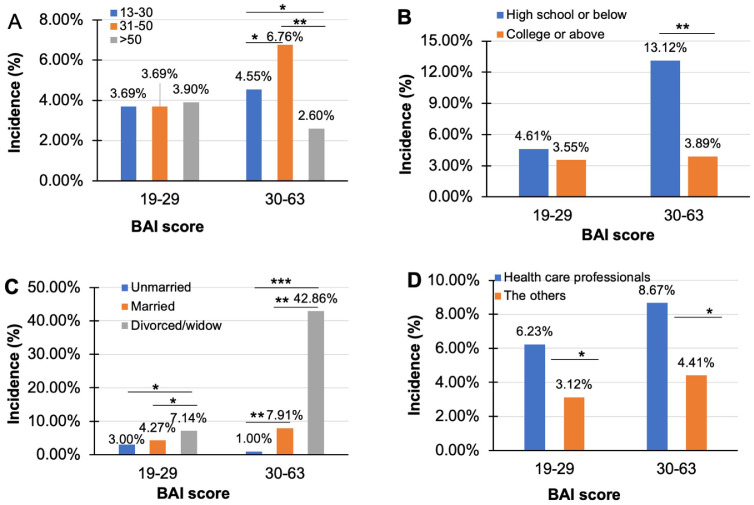
Furthermore, we checked if the demographic factors influence incidences of moderate and severe anxiety of the respondents. Except for gender, all the other demographic factors did influence the incidences. In details, people in the 31-50 subsample showed the highest incidence of severe anxiety (BAI score = 30-63) among the three age subsamples, whereas people elder than 50 presented the lowest incidence of severe anxiety over the other two groups. The three subsamples were comparable in terms of the incidence of moderate anxiety (Fig. 3 A). As for education level, people at college or higher levels had significantly lower incidence of severe anxiety compared to those at high school or lower levels. The two subsamples were comparable in terms of moderate anxiety (Fig. 3B). Like described above, divorced individuals or widows showed the highest incidences of both moderate and severe anxiety compared to unmarried and married people. Married people presented higher incidence of severe anxiety relative to unmarried persons (Fig. 3C). Interestingly, people worked at hospitals or studied in medical schools showed higher incidences of both moderate and severe anxiety compared to the other respondents (Fig. 3D).
Fig. 3.
Effects of some demographic factors on the COVID-19 outbreak induced anxiety in general public. (A) Comparisons of moderate and severe anxiety incidences among the three age subsamples of respondents. (B) Comparisons of moderate and severe anxiety incidences between the two education subsamples of respondents. (C) Comparisons of moderate and severe anxiety incidences among the three marital status subsamples of respondents. (D) Comparisons of moderate and severe anxiety incidences between the two occupation subsamples of respondents. Data were analyzed by Chi-square. *p<0.05, **p<0.01, ***p<0.001.
3.4. Association between anxiety level and demographic and COVID-19 relevant factors
The correlation and multiple linear regression analysis disclosed the predictive factors for the BAI score of all respondents. Except for gender, all the other variables were shown to be important factors influencing BAI score of respondents. Specifically, quarantine, living in Hubei and high epidemic area, divorced/widow, and medical background (health care professionals and medical students) seemed to upregulate anxiety level of respondents; whereas married, being senior and with higher education level showed protective effect (Table 3 ). Also, multivariate logistic regression analysis revealed that all the factors, except for gender, were significantly associated with anxiety level of the respondents. The highest OR was seen in people who were quarantined at the survey time (OR = 22.397, 95 % CI = 6.959 – 72.077), followed by divorced/widow group (OR = 4.170, 95 % CI = 3.022 – 5.755). The other factors showed smaller but significant effects on the anxiety level of respondents (Table 4 ).
Table 3.
The predictors of BAI score using multiple linear regression analysis.
| R2 = 0.146 | Beta | p-value |
|---|---|---|
| Gender | - 0.197 | 0.632 |
| Age | - 2.918 | <0.001 |
| Education level | - 1.898 | <0.001 |
| Marital status | 4.635 | <0.001 |
| Location of residence | - 1.505 | <0.001 |
| Occupation | - 1.867 | <0.001 |
| If quarantined | 22.723 | <0.001 |
Note: The predictors were assigned specific values as follows:
Gender: male = 1, female = 2.
Age: 13-30 = 1, 31-50 = 2, >50 = 3.
Education level: high school or below = 1, college or above = 2.
Marital status: unmarried = 1, married = 2, divorced/widow = 3.
Location of residence: Hubei = 1, high epidemic area = 2, low epidemic area = 3.
Occupation: health professional =1, the others = 2.
If quarantined: not =1, yes = 2.
Table 4.
Multivariate logic regression analysis of factors affecting anxiety level.
| Variables | OR | 95 % CI | p-value |
|---|---|---|---|
| Gender | 0.996 | 0.724 -1.370 | 0.979 |
| Age | 0.552 | 0.402 - 0.757 | <0.001 |
| Education level | 0.456 | 0.313 - 0.665 | <0.001 |
| Marital status | 4.170 | 3.022 - 5.755 | <0.001 |
| Location of residence | 0.641 | 0.500 - 0.823 | <0.001 |
| Occupation | 0.429 | 0.298 - 0.619 | <0.001 |
| If quarantined | 22.397 | 6.959 - 72.077 | <0.001 |
4. Discussion
This study has demonstrated that COVID-19 outbreak increased public anxiety level in China. Supporting evidence for this conclusion includes: 1) the averaged BAI score of all respondents in this study is higher than those of same ethnic Chinese who were healthy and lived in a non-epidemic area a few years ago (Huang et al., 2016a, 2016b); 2) people living in Hubei province (the infection focus) and the high epidemic area showed significantly higher averaged BAI score and incidences of moderate and severe anxiety relative to people living in low epidemic area; 3) being quarantined at the survey time was the most significant contributor to the increased public anxiety level. These data add evidence for the claim that outbreak of an infectious disease can have profound impact on the human psyche (Tucci et al., 2017). Indeed, over the course of the epidemic of the West African Ebola virus disease (EVD) from 2013 to 2016, health professionals reported that mental health services were overwhelmed due to extreme anxiety experienced by patients, family members, and health-care professionals, in addition to loss of life and grief (Reardon, 2015). And more than half of health care workers (56.7%) reported moderately high degree of anxiety as they worried about the A/H1N1 influenza pandemic (Goulia et al., 2010).
Of the 2003 respondents, 21 (1.05%) persons were being quarantined at the survey time for probable infection with COVID-19. They showed the highest averaged BAI compared to the others in this study who were not quarantined. Also, they had a very high combined incidence of moderate and severe anxiety compared to the non-quarantined people. Finding the major causes leading to this high anxiety level at terribly high incidence and analyzing effects of psychosocial factors on the emotional measures would be very important and practically significant. The data at our hands are of great help to us.
First of all, the major causes leading to a high BAI score must be something directly related to COVID-19 infection that made people to be quarantined for probable infection, like fever, cough, malaise, or other nonspecific symptoms. In support of this notion, a recent study reported that chills, myalgia, cough, dizziness, coryza, and sore throat were significantly associated with higher DASS (Depression, Anxiety and Stress Scale) anxiety and depression subscale scores (Wang et al., 2020). Certainly, the clinical symptoms must be of biological origin, such as a pathogenic microorganism, including virus, infection. In other words, a pathogenic microorganism infection was the major factor leading to high anxiety level in at least some of quarantined individuals, i.e. those who were to be identified as patients with COVID-19 infection. In line with this interpretation, sporadic infectious diseases have been associated with various neuropsychiatric disorders, exemplified by Borna virus, which had some human associations with neuropsychiatric disease (Tucci et al., 2017). More relevantly, patients with severe acute respiratory syndrome (SARS) experienced anxiety and reported fear, loneliness, boredom and anger (Maunder et al., 2003). In another study, patients with SARS were deemed to have psychiatric problems such as anger, anxiety, suicidal ideas and depressive reaction during the period of the outbreak (Cheng et al., 2004). Similar to SARS, EVD was reported to cause vulnerabilities, social stigma, distress, and isolation at an individual level (World Health Organization, 2014).
In addition, having family member(s) infected with the virus or closely contacting identified patient(s) can also make a person to be quarantined. These non-biological factors would be likely to aggravate the anxiety symptoms resulted from pathogenic infection or result in anxiety symptoms independent of the biological factors. A perfect illustration pertinent to this interpretation is the emotional and behavioral responses of healthcare professionals in response to the SARS epidemic in Hong Kong and Toronto. They showed higher levels of emotional distress than that of the general public (Maunder et al., 2003; Wong et al., 2004). Another study reported that the infected healthcare workers in the hospital felt extreme vulnerability, uncertainty and threat to life, with significantly high psychiatric morbidity of acute stress syndrome (Chong et al., 2004). Another hospital survey carried out during the SARS outbreak reported that 29% of respondents (healthcare professionals) experienced emotional distress, much higher than that seen in a general population survey (Nickell et al., 2004). In a more recent study, 14.5% healthcare workers suffered from moderate to severe anxiety in Singapore, which was higher compared to their peers in the other countries that were not attacked by COVID-19 during the survey time (Tan et al., 2020). In line with these previous studies, health professionals in the present study showed significantly higher incidences of moderate (6.23% vs 3.12%) and severe (8.67% vs 4.41%) anxiety relative to the non-healthcare workers. Certainly, the higher anxiety levels in this subsample were related to what they were doing, what they were witnessing and/or knew relevant to COVID-19 infection. Relevant to the same interpretation, people living in high epidemic area presented significantly higher incidence of severe anxiety compared to those in low epidemic area (9.49% vs 3.21%).
Interestingly, the marital status, age, and educational level of respondents also significantly impacted the emotional measures of them, in response to COVID-19 outbreak. Specifically, divorced people and widows presented higher anxiety level then unmarried and married people. This effect may be due to the loneliness of the divorced people and widows and lack of emotional support to them. As for effect of age, youngers (people in 13-30 and 30-50 years old) presented significantly higher anxiety levels than seniors (>50 years old). This difference may be relevant to multiple socio-economic issues. Of possible ones, youngers may have heavier burden of life than seniors examined in this study. For example, people in 13-30 years old subsample are generally occupied with heavy academic burden which may be intensified by Chinese culture. They were likely to worry about for how long the plague would continue. In addition, this subpopulation, especially the adolescents of them, are less tolerable to constraints and were being enforced to stay at home day after day. Overall, those in 31-50 years old subsample have much heavier burden in life and work than the other subsamples. He/she is the backbone of a family and concerned with much more issues than the other subsamples. As such, they are more sensitive but less tolerable to increased use of precautionary measures against COVID-19 and thus being more anxious. Last but not least, people at college or above levels showed significantly lower anxiety level than those at high school or below, indicating a protective effect of education on the COVID-19 related anxiety. This is not unexpected as people at lower education level or with less knowledge are more likely to trust in what they hear and/or read on we-media, which is the main platform creating and propagating unscientific information, even rumors. As such, the emotion of this group people is more likely to be influenced by unjustified information, which ran rampant during the outbreak of COVID-19 infection.
Overall, this study provided evidence that COVID-19 outbreak did extensively and intensively impact the mood of general public in China and ascertained some of psychosocial factors that influenced the plague-induced emotional measures. These data along with those from the other studies (Tan et al., 2020; Wang et al., 2020) warrant propagation of scientific information about COVID-19 to general population and offering relevant psychological consultation service to specific subpopulation. Acknowledging the importance of psychological services, as early as the late of January 2020, the National Health Commission of China issued the first comprehensive guideline on emergency psychological crisis intervention in individuals who were affected by COVID-19 (National Health Committee, People's Republic of China, 2020). Although this survey was performed after the issuance of the guideline, the data of this study is unlikely affected by the implementation of the guideline as the emphasis of it was on delivery of mental health support services to patients and healthcare workers. More services should be provided to general population to relieve their anxiety and improve their psychological health. In this regard, a very recent article deserves to be highlighted. It suggested 6 strategies that local and overseas authorities could consider for improving their current psychological intervention plan, in addition to summarizing the impacts of COVID-19 on mental health of general population, healthcare professionals, and infected patients. As expected by the authors of this article, countries will be equipped to succeed in their battle against COVID-19 and secure their future after their psychological defense is bolstered (Ho et al., 2020).
The limitations of this study should not be ignored. First, it is a cross-sectional study unable to track the emotional changes over time in the respondents. Second, sample size is relatively small thus did not allow further analyses on the data from some subsamples such as divorced/widow (n = 42) and quarantined people (n = 21). Third, the survey should include more self-reported measures like the Impact of Event Scale (Horowitz et al., 1979), which has been used to assess the frequency of intrusive and avoidant phenomena in response to a specific stressful life event (Hsu et al., 2002), severe pollution (Ho et al., 2014), and COVID-19 outbreak (Wang et al., 2020). Last but not least, this study, like many other internet surveys, was not based on probability sampling. The survey questionnaire was simply released via WeChat. Respondents were those people who had a cell phone with access to WeChat and decided to participate in the survey. Therefore, this survey may suffer from the problems of under-coverage and self-selection (Bethlehem, 2010; Greenacre, 2016). Under-coverage is because of the exclusion of some elements of the general population from sample selection. For instance, some elders have no cell phone or do not play WeChat at all thus were unlikely selected. Indeed, there were only 77 participants over 50-years-old among a total of 2003 respondents in this study. Self-selection means that it is completely left to individuals to select themselves for the survey (Bethlehem, 2010). Therefore, this survey may have a potential of high non-response rates. Both of under-coverage and self-selection may lead to biased estimates. As such, caution should be exercised when generalizing the conclusions of this study.
In summary, the outbreak of COVID-19 infection led to higher anxiety levels in general public in mainland, China. The virus infection was the chief culprit for the severe anxiety in some of quarantined people, while non-biological factors, such as having family member(s) infected with the virus or closely contacting identified patient(s), could aggravate the anxiety symptoms resulted from pathogenic infection or result in anxiety symptoms independently. Of the psychosocial factors, working as a healthcare professional and lack of emotional support (divorced/widow) upregulated anxiety level of the respondents, whereas high education level protected respondents against the COVID-19 outbreak-related anxiety. People at different age groups showed distinct psychological anxiety levels due to their own socio-economic conditions. On the basis of all these information, distinct psychological consultation services should be provided to different subpopulations in general public during and after the outbreak of COVID-19 infection.
Contributors
HZ, LL, QH, and HX designed the study. HZ, QQ, ZK, TD, LH, and LD disseminated the questionnaire and analyzed the data. HZ, XH, GF, LL, QH, and HX interpreted the data. HZ and HX wrote the manuscript. QH and HX revised the manuscript. All authors read the manuscript and approved for the submission of it to Journal of Affective Disorders.
Declaration of Competing Interest
The authors declare no conflict of interest.
Acknowledgments
Role of funding source
None
Acknowledgments
None
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jad.2020.07.085.
Appendix. Supplementary materials
References
- Bartholomew R.E., Wessely S. Protean nature of mass sociogenic illness: from possessed nuns to chemical and biological terrorism fears. Br. J. Psychiatry. 2002;180:300–306. doi: 10.1192/bjp.180.4.300. [DOI] [PubMed] [Google Scholar]
- Beck A.T., Epstein N., Brown G., Steer R.A. An inventory for measuring clinical anxiety: psychometric properties. J. Consult. Clin. Psychol. 1988;56(6):893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- Bethlehem J. Selection bias in web surveys. Int. Statist. Rev. 2010;78(2):161–188. [Google Scholar]
- Blendon R.J., Benson J.M., DesRoches C.M., Raleigh E., Taylor-Clark K. The public's response to severe acute respiratory syndrome in Toronto and the United States. Clin. Infect. Dis. 2004;38(7):925–931. doi: 10.1086/382355. [DOI] [PubMed] [Google Scholar]
- Cheng S.K., Tsang J.S., Ku K.H., Wong C.W., Ng Y.K. Psychiatric complications in patients with severe acute respiratory syndrome (SARS) during the acute treatment phase: a series of 10 cases. Br. J. Psychiatry. 2004;184:359–360. doi: 10.1192/bjp.184.4.359. [DOI] [PubMed] [Google Scholar]
- Chong M.Y., Wang W.C., Hsieh W.C., Lee C.Y., Chiu N.M., Yeh W.C. Psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. Br. J. Psychiatry. 2004;185:127–133. doi: 10.1192/bjp.185.2.127. [DOI] [PubMed] [Google Scholar]
- Greenacre Z.A. The importance of selection bias in internet surveys. Open J. Statist. 2016;6:397–404. [Google Scholar]
- Goulia P., Mantas C., Dimitroula D., Mantis D., Hyphantis T. General hospital staff worries, perceived sufficiency of information and associated psychological distress during the A/H1N1 influenza pandemic. BMC Infect. Dis. 2010;10:322. doi: 10.1186/1471-2334-10-322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho C.S., Chee C.Y., Ho R.C. Mental health strategies to combat the psychological impact of COVID-19 beyond paranoia and panic. Ann. Acad. Med. Singapore. 2020;49(1):155–160. [PubMed] [Google Scholar]
- Ho R.C., Zhang M.W., Ho C.S., Pan F., Lu Y., Sharma V.K. Impact of 2013 south Asian haze crisis: study of physical and psychological symptoms and perceived dangerousness of pollution level. BMC Psychiatry. 2014;14:81. doi: 10.1186/1471-244X-14-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horowitz M., Wilner N., Alvarez W. Impact of event scale: a measure of subjective stress. Psychosom. Med. 1979;41(3):209–218. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- Hsu C.C., Chong M.Y., Yang P., Yen C.F. Posttraumatic stress disorder among adolescent earthquake victims in Taiwan. J. Am. Acad. Child. Adolesc. Psychiatry. 2002;41(7):875–881. doi: 10.1097/00004583-200207000-00022. [DOI] [PubMed] [Google Scholar]
- Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang W.L., Chen T.T., Chen I.M., Chang L.R., Lin Y.H., Liao S.C. Harm avoidance and persistence are associated with somatoform disorder psychopathology: a study in Taiwan. J. Affect. Disord. 2016;196:83–86. doi: 10.1016/j.jad.2016.02.009. [DOI] [PubMed] [Google Scholar]
- Huang W.L., Chen T.T., Chen I.M., Ma H.M., Lee M.T., Liao S.C. Depression and anxiety among patients with somatoform disorders, panic disorder, and other depressive/anxiety disorders in Taiwan. Psychiatry Res. 2016;241:165–171. doi: 10.1016/j.psychres.2016.05.008. [DOI] [PubMed] [Google Scholar]
- Hui D.S., Azhar I., Madani E., Ntoumi T.A., Kock F., Dar R.O. . The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health - the latest 2019 novel coronavirus outbreak in Wuhan, China. Int. J. Infect. Dis. 2020;91:264–266. doi: 10.1016/j.ijid.2020.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung G.M., Lam T.H., Ho L.M., Ho S.Y., Chan B.H., Wong I.O. . The impact of community psychological responses on outbreak control for severe acute respiratory syndrome in Hong Kong. J. Epidemiol. Community Health. 2003;57(11):857–863. doi: 10.1136/jech.57.11.857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N. Engl. J. Med. 2020;2020 doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu H., Stratton C.W., Tang Y.W. Outbreak of pneumonia of unknown etiology in Wuhan China: the mystery and the miracle. J. Med. Virol. 2020;92(4):401–402. doi: 10.1002/jmv.25678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maunder R., Hunter J., Vincent L., Bennett J., Peladeau N., Leszcz M. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ. 2003;168(10):1245–1251. [PMC free article] [PubMed] [Google Scholar]
- National Health Committee, People's Republic of China. 2020. Guidelines of psychological crisis intervention for COVID-19 pneumonia. Available at:http://www.nhc.gov.cn/jkj/s3577/202001/6adc08b966594253b2b791be5c3b9467.
- Nickell L.A., Crighton E.J., Tracy C.S., Al-Enazy H., Bolaji Y., Hanjrah S. . Psychosocial effects of SARS on hospital staff: survey of a large tertiary care institution. CMAJ. 2004;170(5):793–798. doi: 10.1503/cmaj.1031077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quah S.R., Hin-Peng L. Crisis prevention and management during SARS outbreak. Singapore. Emerg. Infect. Dis. 2004;10(2):364–368. doi: 10.3201/eid1002.030418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reardon S. Ebola's mental-health wounds linger in Africa. Nature. 2015;519(7541):13–14. doi: 10.1038/519013a. [DOI] [PubMed] [Google Scholar]
- Special Expert Group for Control of the Epidemic of Novel Coronavirus Pneumonia of the Chinese Preventive Medicine Association An update on the epidemiological characteristics of novel coronavirus pneumonia (COVID-19) Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41(2):139–144. doi: 10.3760/cma.j.issn.0254-6450.2020.02.002. [DOI] [PubMed] [Google Scholar]
- Tan B.Y.Q., Chew N.W.S., Lee G.K.H., Jing M., Goh Y., Yeo L.L.L. Psychological impact of the COVID-19 pandemic on healthcare workers in Singapore. Ann. Intern. Med. 2020 doi: 10.7326/M20-1083. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucci V., Moukaddam N., Meadows J., Shah S., Galwankar S.C., Kapur G.B. The forgotten plague: psychiatric manifestations of Ebola, Zika, and emerging infectious diseases. J. Glob. Infect. Dis. 2017;9(4):151–156. doi: 10.4103/jgid.jgid_66_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong W.C., Lee A., Tsang K.K., Wong S.Y. How did general practitioners protect themselves, their family, and staff during the SARS epidemic in Hong Kong? J. Epidemiol. Commun. Health. 2004;58(3):180–185. doi: 10.1136/jech.2003.015594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . WHO Library Cataloguing-in-Publication Data; 2014. Psychological First aid During Ebola Virus Disease Outbreaks. [Google Scholar]
- Wu F., Zhao S., Yu B., Chen Y.M., Wang W., Song Z.G. A new coronavirus associated with human respiratory disease in China. Nature. 2020 doi: 10.1038/s41586-020-2008-3. [published Online First: 2020/02/06] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu K.K., Chan S.K., Ma T.M. Posttraumatic stress, anxiety, and depression in survivors of severe acute respiratory syndrome (SARS) J. Trauma. Stress. 2005;18(1):39–42. doi: 10.1002/jts.20004. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.