Abstract
Introduction
The aim of the study was to identify the sociodemographic and clinical factors associated with death after the first lower-extremity amputation (LEA), minor and major separately, using data from regional health administrative databases.
Research design and methods
We carried out a population-based cohort study including patients with diabetes residing in the Lazio region and undergoing a primary amputation in the period 2012–2015. Each individual was followed up for at least 2 years. Kaplan-Meier analysis was used to evaluate long-term survival; Cox proportional regression models were applied to identify factors associated with all-cause mortality.
Results
The cohort included 1053 patients, 72% were male, 63% aged ≥65 years, and 519 (49%) died by the end of follow-up. Mortality rates at 1 and 4 years were, respectively, 33% and 65% for major LEA and 18% and 45% for minor LEA. Significant risk factors for mortality were age ≥65, diabetes-related cardiovascular complications, and chronic renal disease for patients with minor LEA, and age ≥75 years, chronic renal disease and antidepressant drug consumption for subjects with major LEA.
Conclusions
The present study confirms the high mortality rates described in patients with diabetes after non-traumatic LEA. It shows differences between minor and major LEA in terms of mortality rates and related risk factors. The study highlights the role of depression as specific risk factor for death in patients with diabetes after major LEA and suggests including its definition and management in strategies to reduce the high mortality rate observed in this group of patients.
Keywords: foot ulcer, mortality, adult diabetes
Significance of this study.
What is already known about this subject?
Patients with diabetes who undergo lower-extremity amputation have a high mortality rate.
Available evidence suggests that mortality excess is not fully explained by diabetes complications.
What are the new findings?
Mortality rates and risk factors differ between minor and major lower-extremity amputation.
Depression is a risk factor for death after major lower-extremity amputation.
How might these results change the focus of research or clinical practice?
Specific predictive factors should be considered in risk assessment before major and minor lower-extremity amputation.
Management of depression should be included in prevention strategies to reduce mortality after major lower-extremity amputation.
Introduction
Diabetic foot is an important long-term complication among patients with diabetes and represents the most frequent cause of non-traumatic lower-extremity amputation (LEA), with diabetic foot ulcers preceding more than 80% of amputations in people with diabetes.1 Diabetic foot is a rising health problem due to increasing prevalence of diabetes worldwide2; it is estimated that 15%–25% of people with diabetes will be affected by a foot ulcer at some point in their lives.3 After a first amputation, patients with diabetes are at high risk to undergo other amputations, with a major impact on quality of life and an increase in illness-related costs. Algorithms to manage diabetic foot and different revascularization techniques have become available, contributing to the observed reduction in the incidence of diabetes-related major limb amputations.4–7 However, amputation rates in the diabetic population remain relatively high even with a significant regional variation, suggesting variability in availability and standard of care.7 8 Late referral to vascular specialist and lack of agreement on factors to consider when choosing intervention strategies have been suggested as possible causes of the still high amputation rates.8 In spite of improvements in perioperative risk assessment and preoperative and postoperative medical care, robust evidence is available on the extremely high mortality after amputation in patients with diabetes.9 10 The 30-day mortality risk among patients with diabetes with primary LEA is higher than among individuals undergoing open infrainguinal revascularization, ranging between 6% and 8%.11 12 A recent review considering long-term mortality after LEA reported an overall mortality rate of 48%, 61%, and 71%, at 1-year, 2-year, and 3-year follow-up, respectively, among patients with diabetes and peripheral vascular disease.13 Some clinical characteristics are well known as risk factors for mortality after LEA, such as coronary artery disease, cerebrovascular disease, renal dysfunction, and dyslipidemia. Anyway, few studies, and often single center-based, analyzed factors associated with mortality after LEA among individuals with diabetes.8 14 15 In particular, characteristics other than clinical features have been less extensively investigated, as well as long-term mortality. Hoffstad et al16 reported a high risk of death among patients with diabetes and LEA compared with individuals with diabetes but no LEA. Interestingly, they also found that mortality excess was not fully explained by diabetes complications, such as cardiovascular diseases and renal insufficiency, and therefore it was suggested that other individual factors might contribute to increasing mortality risk in this particularly fragile population.17 Actually, the identification of risk factors for mortality among patients with diabetes with foot ulcers is crucial to define preventive strategies to lower the risk of death after LEA and to appraise comprehensively the risk-benefit profile of the amputation.18 19
In the Lazio region (the third most populated region of Italy, including Rome, the capital and largest Italian city), health information systems (HIS) are comprehensive and contains high-quality information and therefore allow measurement of the occurrence of acute and chronic diseases and monitor quality of care and healthcare outcomes.20 21
The aims of our study were to investigate survival time after different types of LEA (major and minor) among patients with diabetes and to identify the sociodemographic and clinical factors associated with death. For this study, we used data collected by different HIS available in the Lazio region.
Research design and methods
Study design and data sources
This is a retrospective population-based cohort study including patients with diabetes and LEA residing in the Lazio region (about six million inhabitants). We retrieved individual information registered in the following HIS: the Regional Health Assistance File, collecting demographic and residence information of all residents living in the Lazio region and registered in the Regional Health Service, accounting for 95% of the overall population; the Hospital Discharge Registry (HDR), which routinely collects data from all regional hospitals, including information on patients’ sociodemographic characteristics, discharge diagnoses and procedure codes according to the International Classification of Disease, IX Revision, Clinical Modification (ICD-9-CM); and the Drug Claims Registry (PHARM), which comprises individual records for each medical prescription that is dispensed from public and private pharmacies, and the date of dispensing. The registry is limited to drugs dispensed to outpatients and reimbursed by the healthcare system. Drugs are identified by the national drug register code, which is related to the Anatomical Therapeutic Chemical (ATC) classification system. The Regional Mortality Registry registers causes of death, codified according to ICD-9, for all resident deaths in the region. All residents in the Lazio region served by the Regional Health Service are assigned a unique personal identification code recorded in all databases deriving from regional HIS. This individual identifier is the key used to link different databases to identify individuals, avoiding double counting, and to ascertain health outcomes.
Study population and inclusion criteria
A standardized algorithm was used to identify patients with diabetes (for details see online supplementary table S1) aged ≥35 years on December 31, 2011 (date of enrollment).22 23 The study population included patients with diabetes who underwent a first amputation in the period from January 1, 2012 to December 31, 2015. Inclusion criteria were discharge with primary or secondary diagnosis of diabetes (ICD-9-CM: 250.xx) associated with ICD-9-CM codes 84.10–84.19 in any field concerning surgical procedures performed during hospitalization. Individuals who died within 30 days from the amputation or who underwent traumatic (ICD-9-CM codes: 895.0, 895.1, 896.0–896.3, 897.0–897.7) or cancer-related (ICD-9-CM codes: 170.7, 170.8, 171.3, 172.7, 173.7) amputations were excluded. The intervention date for diabetes-related LEA was identified as the index date. Individuals who underwent LEA within 2 years before the index date were excluded from the analysis and only incident cases of diabetes-related amputation were selected.
bmjdrc-2020-001355supp001.pdf (249.4KB, pdf)
Follow-up, outcome and covariates
Duration of follow-up ranged from 2 years to a maximum of 6 years, from the index date until the end of study period (December 31, 2017) or death, whichever came first. The outcome of interest was all-cause mortality after primary LEA.
Different sociodemographic information and comorbidities were investigated as potential predictive factors. Data on sociodemographic characteristics and coexisting conditions were obtained from the HDR, while information on drug consumption was retrieved from the PHARM database. Specifically, patients were characterized with respect to gender, age, and education level classified into three levels according to the International Standard Classification of Education: low (0–2; 8 years of education or less) (reference category), medium (3; 13 years of education), and high (4–8; 15 years of education or more). Comorbidities (peripheral arterial disease (PAD), peripheral neuropathy, cardiovascular diseases, and cardiovascular risk factors including lipid metabolism disorders and hypertension, neoplasms, chronic renal disease) were defined on the basis of information on hospitalization episodes in the 2 years before the index date. Diseases and their ICD-9-CM codes are listed in online supplementary table S2. Finally, we considered antidepressant drug use (ATC code N06A), defined as at least two prescriptions in the 6 months before the index date.
Statistical analysis
Both univariate and multivariate analyses were performed separately for major and minor amputation. The Kaplan-Meier method was used to determine the crude survival probabilities after the first amputation, by gender and age class (35–54, 55–64, 65–74, 75–84, 85+). Survival time was calculated from the date of first LEA to death or end of study. Multivariate analyses were performed using Cox proportional hazard regression model to estimate HR and 95% CI, including all sociodemographic and comorbidities reported above. We performed a sensitivity analysis excluding from the group of patients with minor LEA those individuals with a first minor LEA that underwent a major amputation during the follow-up period. The aim of this analysis was to investigate the potential effect of a major LEA following a minor amputation on determinants of death. The SAS statistical package was used for analyses (SAS V.9.4).
Results
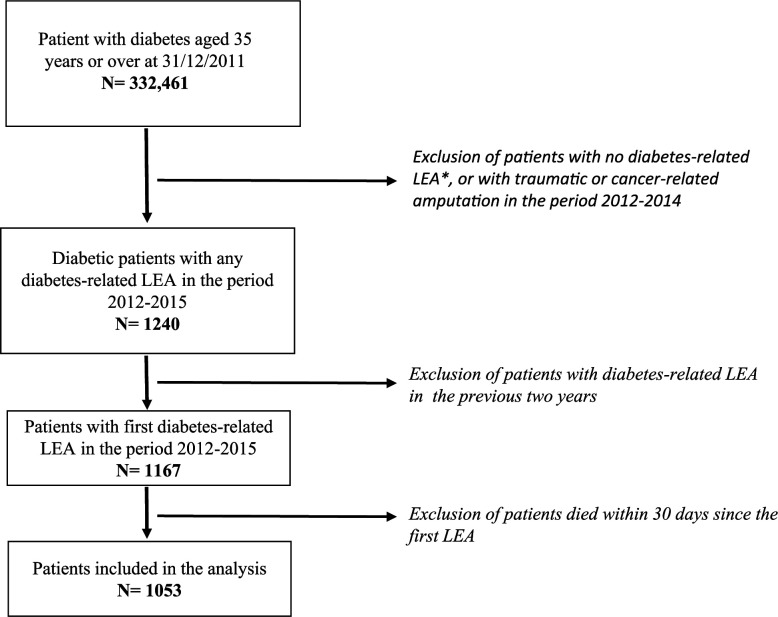
We identified 332 461 patients with diabetes aged 35 or over and residing in the Lazio region on December 31, 2011. During the period 2012–2015, 1167 individuals underwent a first minor or major LEA. After excluding patients who died within 30 days from the amputation, the study population included 1053 individuals, 317 with major LEA and the remaining (n=736) with minor LEA (figure 1).
Figure 1.
Flow diagram of the study population. *LEA, lower-extremity amputation.
The median time from enrollment (December 31, 2011) to amputation did not differ between the two groups of patients (400 days for major amputation and 415 days for minor amputation). Table 1 shows the comparison of sociodemographic and clinical characteristics in patients who underwent major or minor amputation. The proportion of men was higher among patients with a minor LEA as compared with those who had a major amputation (73% vs 69%). In both groups, more than 60% of individuals aged 65 years or over and the majority of the patients had a medium-low education level. Prevalence of comorbidities and medication use were higher among individuals with a major LEA.
Table 1.
Sociodemographic and clinical characteristics of patients with diabetes with lower-extremity amputation
| Type of amputation | |||||||
| Total (1053) | Major (317) | Minor (736) | P value | ||||
| n | % | n | % | n | % | ||
| Gender | |||||||
| Male | 756 | 71.8 | 217 | 68.5 | 539 | 73.2 | 0.114 |
| Female | 297 | 28.2 | 100 | 31.5 | 197 | 26.8 | |
| Age | |||||||
| 35–54 | 141 | 13.4 | 29 | 9.2 | 112 | 15.2 | 0.002 |
| 55–64 | 247 | 23.5 | 67 | 21.1 | 180 | 24.5 | |
| 65–74 | 351 | 33.3 | 104 | 32.8 | 247 | 33.6 | |
| 75+ | 314 | 29.8 | 117 | 36.9 | 197 | 26.8 | |
| Education level | |||||||
| Low | 415 | 39.4 | 137 | 43.2 | 278 | 37.9 | 0.266 |
| Medium | 418 | 39.7 | 118 | 37.2 | 300 | 40.9 | |
| High | 218 | 20.7 | 62 | 19.6 | 156 | 21.3 | |
| Comorbidities* | |||||||
| Vasculopathy | 398 | 37.8 | 130 | 41.0 | 268 | 36.4 | 0.158 |
| Neuropathy | 70 | 6.6 | 25 | 7.9 | 45 | 6.1 | 0.290 |
| Cardiovascular diseases† | 621 | 59.0 | 210 | 66.2 | 411 | 55.8 | 0.009 |
| Cardiovascular risk factors‡ | 412 | 39.1 | 143 | 45.1 | 269 | 36.5 | 0.002 |
| Neoplasm | 56 | 5.3 | 19 | 5.9 | 37 | 5.0 | 0.521 |
| Chronic renal diseases | 259 | 24.6 | 83 | 26.2 | 176 | 23.9 | 0.433 |
| Drug consumption§ | |||||||
| At least two antidepressant drug prescriptions | 152 | 14.4 | 56 | 17.7 | 96 | 13.0 | 0.050 |
| Vital status | |||||||
| Alive | 534 | 50.7 | 118 | 37.2 | 416 | 56.5 | 0.643 |
| Died | 519 | 49.3 | 199 | 62.8 | 320 | 43.5 | |
*In the 24 months preceding the index date.
†Ischemic disease, heart failure, cerebrovascular disease, vascular disease, previous cardiac revascularization, and cerebrovascular revascularization.
‡Lipid metabolism disorders and hypertension.
§In the 6 months preceding the index date.
During the follow-up period, 519 (49%) patients died, 63% of those with a major LEA and 43% of patients who had undergone a minor foot amputation.
The median follow-up time was 11.9 months and 8.4 months for men and women, respectively (log-rank test χ2=1.170, p=0.279) among subjects with a major LEA, and 17.9 months and 14.9 months (log-rank test χ2=3.126, p=0.077) among those with a minor LEA.
Of the individuals 33% with major LEA died within 1 year and 65% within 4 years after the amputation. Among subjects enrolled after minor LEA, mortality rates at 1 and 4 years were 18% and 45%, respectively (data not shown). The median survival time varied significantly by age class for both groups of patients. In particular, among subjects with a major LEA, the survival time ranged from 30.6 months for the age group 35–54 to 16.8 months for those aged 85 years and older. Among subjects with a minor LEA, the median survival times were 38.4 months and 24.4 months for the age groups 35–54 and 85 years and older, respectively (online supplementary figure S1). Survival rate at 1 year after major LEA was 69% among men and 61% among women, decreasing to 35% and 31%, respectively, after 4 years. For patients who underwent minor LEA, the survival rate at 1 year was 83% among men and 79% among women, and 60% and 53%, respectively, for men and women after 4 years (online supplementary figure S2).
The results from the multivariate analysis are presented in tables 2 and 3, respectively, for subjects with major and minor LEA. Among patients who underwent a major LEA, after adjustment, we observed a significant increase in the mortality risk for the oldest age class (75 years and over) (HR: 1.91, 95% CI 1.05 to 3.48). Neuropathy was significantly associated with a lower risk of mortality (HR: 0.51, 95% CI 0.26 to 0.98). We found that chronic renal disease was the only predictor of mortality (HR: 1.68, 95% CI 1.20 to 2.36). The use of antidepressant drugs was independently associated with increased risk of mortality (HR: 1.45, 95% CI 1.01 to 2.08). Age older than 65 years (HR 65–74: 1.88, 95% CI 1.22 to 2.90; HR 75+: 3.58, 95% CI 2.31 to 5.55), cardiovascular diseases and chronic renal diseases increased the risk of mortality in patients with a minor LEA (HR: 1.51, 95% CI 1.13 to 2.00; HR: 2.03, 95% CI 1.58 to 2.61, respectively).
Table 2.
Crude and adjusted HR of mortality among patients with diabetes with major lower-extremity amputation
| % | HR | 95% CI | HRagg | 95% CI | P value | |
| Gender | ||||||
| Male | 66.3 | 1.00 | 1.00 | |||
| Female | 33.7 | 1.17 | 0.88 to 1.58 | 0.95 | 0.70 to 1.31 | 0.796 |
| Age | ||||||
| 35–54 | 7.0 | 1.00 | 1.00 | |||
| 55–64 | 16.1 | 1.00 | 0.53 to 1.87 | 1.07 | 0.56 to 2.03 | 0.845 |
| 65–74 | 34.2 | 1.58 | 0.89 to 2.82 | 1.58 | 0.87 to 2.87 | 0.134 |
| 75+ | 42.7 | 1.97 | 1.12 to 3.47 | 1.91 | 1.05 to 3.48 | 0.035 |
| Education level | ||||||
| Low | 48.2 | 1.00 | 1.00 | |||
| Medium | 35.2 | 0.81 | 0.60 to 1.11 | 0.98 | 0.70 to 1.37 | 0.902 |
| High | 16.6 | 0.70 | 0.47 to 1.04 | 0.92 | 0.61 to 1.40 | 0.711 |
| Comorbidities* | ||||||
| Vasculopathy | 41.7 | 0.91 | 0.69 to 1.22 | 0.91 | 0.65 to 1.28 | 0.580 |
| Neuropathy | 5.0 | 0.46 | 0.24 to 0.88 | 0.51 | 0.26 to 0.98 | 0.043 |
| Cardiovascular diseases† | 66.8 | 0.97 | 0.72 to 1.30 | 0.87 | 0.59 to 1.27 | 0.458 |
| Cardiovascular risk factors‡ | 45.2 | 0.94 | 0.71 to 1.24 | 0.87 | 0.63 to 1.20 | 0.398 |
| Neoplasm | 6.5 | 1.10 | 0.62 to 1.93 | 1.17 | 0.65 to 2.08 | 0.605 |
| Chronic renal diseases | 27.1 | 1.64 | 1.22 to 2.22 | 1.68 | 1.20 to 2.36 | 0.002 |
| Drug consumption§ | ||||||
| At least two antidepressant drug prescriptions | 20.1 | 1.44 | 1.01 to 2.04 | 1.45 | 1.01 to 2.08 | 0.044 |
*In the 24 months preceding the index date.
†Ischemic disease, heart failure, cerebrovascular disease, vascular disease, previous cardiac revascularization, and cerebrovascular revascularization.
‡Lipid metabolism disorders and hypertension.
§In the 6 months preceding the index date.
Table 3.
Crude and adjusted HR of mortality among patients with diabetes with minor lower-extremity amputation
| % | HR | 95% CI | HRagg | 95% CI | P value | |
| Gender | ||||||
| Male | 69.7 | 1.00 | 1.00 | |||
| Female | 30.3 | 1.24 | 0.98 to 1.57 | 1.07 | 0.83 to 1.38 | 0.609 |
| Age | ||||||
| 35–54 | 8.4 | 1.00 | 1.00 | |||
| 55–64 | 15.9 | 1.20 | 0.75 to 1.91 | 1.20 | 0.75 to 1.92 | 0.446 |
| 65–74 | 33.4 | 2.05 | 1.35 to 3.13 | 1.88 | 1.22 to 2.90 | 0.004 |
| 75+ | 42.2 | 4.25 | 2.81 to 6.42 | 3.58 | 2.31 to 5.55 | 0.000 |
| Education level | ||||||
| Low | 47.8 | 1.00 | 1.00 | |||
| Medium | 34.7 | 0.57 | 0.45 to 0.73 | 0.87 | 0.67 to 1.14 | 0.308 |
| High | 17.5 | 0.55 | 0.41 to 0.75 | 0.90 | 0.65 to 1.26 | 0.555 |
| Comorbidities* | ||||||
| Vasculopathy | 38.1 | 1.11 | 0.88 to 1.39 | 0.82 | 0.63 to 1.06 | 0.130 |
| Neuropathy | 6.6 | 0.97 | 0.62 to 1.51 | 0.79 | 0.50 to 1.26 | 0.322 |
| Cardiovascular diseases† | 68.1 | 1.96 | 1.55 to 2.48 | 1.51 | 1.13 to 2.00 | 0.005 |
| Cardiovascular risk factors‡ | 42.8 | 1.37 | 1.10 to 1.71 | 0.90 | 0.69 to 1.17 | 0.430 |
| Neoplasm | 6.9 | 1.77 | 1.14 to 2.74 | 1.28 | 0.82 to 2.00 | 0.283 |
| Chronic renal diseases | 30.9 | 2.35 | 1.87 to 2.96 | 2.03 | 1.58 to 2.61 | 0.000 |
| Drug consumption§ | ||||||
| At least two antidepressant drug prescriptions | 15.6 | 1.50 | 1.11 to 2.03 | 1.27 | 0.94 to 1.73 | 0.124 |
*In the 24 months preceding the index date.
†Ischemic disease, heart failure, cerebrovascular disease, vascular disease, previous cardiac revascularization, and cerebrovascular revascularization.
‡Lipid metabolism disorders and hypertension.
§In the 6 months preceding the index date.
The results of the sensitivity analysis agreed closely with those of the main analysis (online supplementary table S3).
Discussion
In this study, we compared patients with diabetes who died and those who survived after the first major or minor LEA, considering different sociodemographic characteristics other than a wide range of comorbidities. Our results document the extreme frailty of patients with diabetes undergoing LEA, both major and minor. Some studies have observed significant differences in mortality between patients undergoing minor or major amputations, with major amputations associated with reduced long-term survival.24–26 A recent systematic review reported an overall 5-year mortality rate ranging from 29% to 69% following minor amputations and from 52% to 80% for patients with major amputations.10 Moreover, in a recent study conducted in a large Italian region, and covering the same time period, mortality rates after minor and major LEA were quite similar to those observed in our study, and specific risk factors as well.27 Ultimately, our estimates appear congruent with those reported in the literature, although comparisons are impaired by the heterogeneity across studies in terms of proportion of patients with diabetes, study period, and type of amputation.
Consistent with other studies, age was significantly related to mortality, with higher risk of death in patients older than 65 years compared with those younger, both after major and minor amputations.8 9 15 In relative terms, individuals with diabetes undergoing a minor amputation were at particularly high risk of mortality, with patients aged ≥75 years having about four times the risk of dying than those 35–54 years of age. Not surprisingly, patients with diabetes at their first amputation had a substantial disease burden with several comorbidities adversely affecting survival. Numerous studies found similar results, with heart failure, cerebrovascular disease and chronic renal disease associated with an increased risk of death.13 15 28 29 In our study, cardiovascular diseases increased the risk of death among patients with diabetes who underwent a minor amputation but not among those with major LEA. This is a quite unexpected finding. We hypothesize that, among patients with a major LEA, conditions acting upstream in the chain of events leading to the first amputation may have less impact on the risk of death than, for example, chronic renal disease. In contrast, among patients with diabetes with a minor LEA, who experience a less severe stage of their disease, the impact of cardiovascular diseases on the risk of death may be more evident. Chronic renal diseases were associated with decreased survival in both groups of patients. Indeed, previous studies stressed the need for intensive treatment for cardiovascular risk factors along with a comprehensive foot care approach among patients with diabetes with a non-traumatic LEA.30 Hoffmann et al25 found that the median survival in patients with diabetes with chronic kidney disease was 27 months, while the median survival in those without diabetic nephropathy was 79 months. Evidence suggests that the risk of diabetic foot disease increases as renal function decreases.31 32 Since patients with diabetes with decreased renal function and a foot ulcer have a higher risk of undergoing amputation,33 it is advisable to monitor closely patients with diabetes with renal insufficiency in order to prevent diabetic foot complications.
In their review Thorud et al10 concluded that despite the strong association between LEA and long-term mortality among patients with diabetes, it remains not clear if amputation hastens death or is a marker of underlying disease severity. Recently, Hoffstad et al16 reported that individuals with diabetes undergoing LEA are at increased risk of death compared with patients with diabetes but no LEA. They considered a large spectrum of clinical risk factors and argued that differences in mortality could not be fully explained by the well-known complication of diabetes. In our study, we considered both antidepressant use and level of education among potential determinants of mortality, other than a wide range of comorbidities and cardiovascular risk factors. For subjects with a first major LEA, we observed a significant association between depression and long-term postamputation mortality after adjustment for sociodemographic characteristics and other clinical conditions. Based on the available evidence, comorbid depression is associated with an increased incidence of LEA in people with diabetes and increased mortality risk in people with a first diabetic foot ulcer.34 35 Indeed, depression negatively affects diabetes management, including medication adherence, physical exercise, blood glucose monitoring and medical visits attendance.36 According to the findings of a recent systematic review, the relationship between depression and diabetes complications is bidirectional, but the risk of developing diabetes complications in people with depression is higher than the risk of developing depression in people with diabetes complications.37 In our opinion, the role of depression as a risk factor for mortality among patients with diabetes with major LEA is worth further investigation to allow, if necessary, implementation of suitable strategies for improving clinical practice and patient outcomes.
The protective effect of neuropathy on mortality after major LEA is difficult to explain. Peripheral neuropathy is risk factor for foot ulceration, but the pathway to major amputation requires additional events like a foot infection.38 On the other hand, PAD is, by itself, a risk factor for foot amputation, and patients with PAD have significant cardiovascular comorbidities.39 40 A possible explanation is a differential under-reporting in hospital charts of peripheral neuropathy. Indeed, the diagnosis of neuropathy is a complex process and requires expertise that is not always available.
This study has some potential limitations. We used hospital discharge data to define comorbidities. Although in Lazio HIS are comprehensive, periodically audited and contain high-quality information, an underestimation of prevalence of some diseases (eg, hypertension) may have occurred. Actually, regional health administrative databases are largely used to measure the occurrence of acute and chronic diseases and to evaluate healthcare outcomes.21 22 Additionally, observational studies based on administrative data suffer from lack of information on important variables as smoking history, and biochemical and laboratory parameters. However, we believe that our results, in particular those related to some risk factors, that is, chronic renal disease and depression, provide valuable insights into this topic and require consideration and further investigation. Nevertheless, a strength of the study design we used was the population-based setting, covering a whole Italian region. We included all amputations occurring during the follow-up period and enrolled a sample of a moderate size. The use of a prevalent, well-defined cohort is a major strength since it improves the generalizability of the results to other contexts. Finally, we selected within the cohort of patients with diabetes the first amputation procedure with a concurrent diagnosis of diabetes. This approach ensured the highest accuracy in case identification, although excluding 3% of total amputations.
Conclusions
The present study provides new insights into the characterization of patients with an increased risk of mortality after non-traumatic major and minor LEA. It highlights differences between risk factors for minor LEA that include chronic cardio-cerebrovascular diseases and chronic renal disease, and risk factors for major LEA including only chronic renal disease and depression.
Depression has never been indicated as a risk factor for death in patients with major LEA. Our findings suggest including definition and management of depression in prevention strategies needed to reduce mortality after major LEA in patients with diabetes. Further studies are required to confirm our observation and the role of depression comorbidity in the very high mortality rate observed after major LEA in patients with diabetes.
Footnotes
Contributors: AMB, SC, NA, MD and LU contributed to conception and design of the study. SC, AMB, and CM wrote the protocol. SC, AMB, LU, MM and LG managed the literature searches and analyses. SC performed the statistical analysis. All authors contributed to the interpretation of the results. SC and AMB wrote the first draft of the manuscript. All authors took part in revising the article critically for important intellectual content; gave final approval of the version to be published; and agree to be accountable for all aspects of the work. NA is the guarantor of this work and as such had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: The Department of Epidemiology, Regional Health Service Lazio Region, is the regional referral center for epidemiological research and has full access to anonymized health information systems. Consent was not necessary because the authors used data already collected at the beginning of the study and the data were analyzed anonymously through a standardized methodology according to the national privacy law (national legislative decree on privacy policy n. 196/30 June 2003). Individuals cannot be identified directly or through identifiers and results are shown in aggregate form.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available upon reasonable request. Data related to the findings reported in our manuscript are available to all interested researchers upon request due to stringent legal restrictions regarding privacy policy on personal information in Italy (national legislative decree on privacy policy n. 196/30 June 2003). For these reasons our data set cannot be made available on public data deposition. All interested researchers can contact the following persons to request the data: Nera Agabiti, Department of Epidemiology, Lazio Regional Health Service, Rome, Italy (email: n.agabiti@deplazio.it); Damiano Lanzi, Department of Epidemiology, Lazio Regional Health Service, Rome, Italy (email: d.lanzi@deplazio.it).
References
- 1.NICE guideline Diabetic foot problems: prevention and management, 2016. [Google Scholar]
- 2.World Health Organization Who global report on diabetes, 2016. [Google Scholar]
- 3.Singh N, Armstrong DG, Lipsky BA. Preventing foot ulcers in patients with diabetes. JAMA 2005;293:217–28. 10.1001/jama.293.2.217 [DOI] [PubMed] [Google Scholar]
- 4.Carinci F, Uccioli L, Massi Benedetti M, et al. An in-depth assessment of diabetes-related lower extremity amputation rates 2000-2013 delivered by twenty-one countries for the data collection 2015 of the organization for economic cooperation and development (OECD). Acta Diabetol 2020;57:347–57. 10.1007/s00592-019-01423-5 [DOI] [PubMed] [Google Scholar]
- 5.Narres M, Kvitkina T, Claessen H, et al. Incidence of lower extremity amputations in the diabetic compared with the non-diabetic population: a systematic review. PLoS One 2017;12:e0182081. 10.1371/journal.pone.0182081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carinci F, Massi Benedetti M, Klazinga NS, et al. Lower extremity amputation rates in people with diabetes as an indicator of health systems performance. A critical appraisal of the data collection 2000-2011 by the organization for economic cooperation and development (OECD). Acta Diabetol 2016;53:825–32. 10.1007/s00592-016-0879-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Holman N, Young RJ, Jeffcoate WJ. Variation in the recorded incidence of amputation of the lower limb in England. Diabetologia 2012;55:1919–25. 10.1007/s00125-012-2468-6 [DOI] [PubMed] [Google Scholar]
- 8.Klaphake S, de Leur K, Mulder PG, et al. Mortality after major amputation in elderly patients with critical limb ischemia. Clin Interv Aging 2017;12:1985–92. 10.2147/CIA.S137570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gurney JK, Stanley J, York S, et al. Risk of lower limb amputation in a national prevalent cohort of patients with diabetes Diabetologia 2018;61:626–63. [DOI] [PubMed] [Google Scholar]
- 10.Thorud JC, Plemmons B, Buckley CJ, et al. Mortality After Nontraumatic Major Amputation Among Patients With Diabetes and Peripheral Vascular Disease: A Systematic Review. J Foot Ankle Surg 2016;55:591–9. 10.1053/j.jfas.2016.01.012 [DOI] [PubMed] [Google Scholar]
- 11.Barshes NR, Menard MT, Nguyen LL, et al. Infrainguinal bypass is associated with lower perioperative mortality than major amputation in high-risk surgical candidates. J Vasc Surg 2011;53:1251–9. 10.1016/j.jvs.2010.11.099 [DOI] [PubMed] [Google Scholar]
- 12.Nowygrod R, Egorova N, Greco G, et al. Trends, complications, and mortality in peripheral vascular surgery. J Vasc Surg 2006;43:205–16. 10.1016/j.jvs.2005.11.002 [DOI] [PubMed] [Google Scholar]
- 13.Stern JR, Wong CK, Yerovinkina M, et al. A meta-analysis of long-term mortality and associated risk factors following lower extremity amputation. Ann Vasc Surg 2017;42:322–7. 10.1016/j.avsg.2016.12.015 [DOI] [PubMed] [Google Scholar]
- 14.Schofield CJ, Libby G, Brennan GM, et al. Mortality and hospitalization in patients after amputation: a comparison between patients with and without diabetes. Diabetes Care 2006;29:2252–6. 10.2337/dc06-0926 [DOI] [PubMed] [Google Scholar]
- 15.López-Valverde ME, Aragón-Sánchez J, López-de-Andrés A, et al. Perioperative and long-term all-cause mortality in patients with diabetes who underwent a lower extremity amputation. Diabetes Res Clin Pract 2018;141:175–80. 10.1016/j.diabres.2018.05.004 [DOI] [PubMed] [Google Scholar]
- 16.Hoffstad O, Mitra N, Walsh J, et al. Diabetes, lower-extremity amputation, and death. Diabetes Care 2015;38:1852–7. 10.2337/dc15-0536 [DOI] [PubMed] [Google Scholar]
- 17.Uccioli L, Giurato L, Meloni M, et al. Diabetes, lower-extremity amputation, and death. Diabetes Care 2016;39:e7. [DOI] [PubMed] [Google Scholar]
- 18.Kota SK, Kota SK, Meher LK, et al. Surgical revascularization techniques for diabetic foot. J Cardiovasc Dis Res 2013;4:79–83. 10.1016/j.jcdr.2012.10.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hingorani A, LaMuraglia GM, Henke P, et al. Surgical revascularization techniques for diabetic foot. Vasc Surg 2016;63:3S–21. [Google Scholar]
- 20.Cascini S, Agabiti N, Incalzi RA, et al. Pneumonia burden in elderly patients: a classification algorithm using administrative data. BMC Infect Dis 2013;13:559–67. 10.1186/1471-2334-13-559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cascini S, Kirchmayer U, Belleudi V, et al. Inhaled Corticosteroid Use in Chronic Obstructive Pulmonary Disease and Risk of Pneumonia: A Nested Case-Control Population-based Study in Lazio (Italy)-The OUTPUL Study. COPD 2017;14:311–7. 10.1080/15412555.2016.1254172 [DOI] [PubMed] [Google Scholar]
- 22.Gnavi R, Karaghiosoff L, Balzi D, et al. [Diabetes prevalence estimated using a standard algorithm based on electronic health data in various areas of Italy]. Epidemiol Prev 2008;32:15–21. [PubMed] [Google Scholar]
- 23.Gini R, Francesconi P, Mazzaglia G, et al. Chronic disease prevalence from Italian administrative databases in the VALORE project: a validation through comparison of population estimates with general practice databases and national survey. BMC Public Health 2013;13:15. 10.1186/1471-2458-13-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Faglia E, Favales F, Morabito A. New ulceration, new major amputation, and survival rates in diabetic subjects hospitalized for foot ulceration from 1990 to 1993: a 6.5-year follow-up. Diabetes Care 2001;24:78–83. 10.2337/diacare.24.1.78 [DOI] [PubMed] [Google Scholar]
- 25.Hoffmann M, Kujath P, Flemming A, et al. Survival of diabetes patients with major amputation is comparable to malignant disease. Diab Vasc Dis Res 2015;12:265–71. 10.1177/1479164115579005 [DOI] [PubMed] [Google Scholar]
- 26.Brown ML, Tang W, Patel A, et al. Partial foot amputation in patients with diabetic foot ulcers. Foot Ankle Int 2012;33:707–16. 10.3113/FAI.2012.0707 [DOI] [PubMed] [Google Scholar]
- 27.Monge L, Gnavi R, Carnà P, et al. Incidence of hospitalization and mortality in patients with diabetic foot regardless of amputation: a population study. Acta Diabetol 2020;57:221–8. 10.1007/s00592-019-01412-8 [DOI] [PubMed] [Google Scholar]
- 28.López-de-Andrés A, Jiménez-García R, Esteban-Vasallo MD, et al. Time trends in the incidence of long-term mortality in T2DM patients who have undergone a lower extremity amputation. Results of a descriptive and retrospective cohort study. J Clin Med 2019;8:1597. 10.3390/jcm8101597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Assi R, Al Azzi Y, Protack CD, et al. Chronic kidney disease predicts long-term mortality after major lower extremity amputation. N Am J Med Sci 2014;6:321–7. 10.4103/1947-2714.136910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schofield CJ, Libby G, Brennan GM, et al. Mortality and hospitalization in patients after amputation. Diabetes Care 2006;29:2252–6. [DOI] [PubMed] [Google Scholar]
- 31.Margolis DJ, Hofstad O, Feldman HI. Association between renal failure and foot ulcer or lower-extremity amputation in patients with diabetes. Diabetes Care 2008;31:1331–6. 10.2337/dc07-2244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wolf G, Müller N, Busch M, et al. Diabetic foot syndrome and renal function in type 1 and 2 diabetes mellitus show close association. Nephrol Dial Transplant 2009;24:1896–901. 10.1093/ndt/gfn724 [DOI] [PubMed] [Google Scholar]
- 33.Meloni M, Izzo V, Giurato L, et al. Impact of heart failure and dialysis in the prognosis of diabetic patients with ischemic foot ulcers. J Clin Transl Endocrinol 2018;11:31–5. 10.1016/j.jcte.2018.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.O'Neill SM, Kabir Z, McNamara G, et al. Comorbid depression and risk of lower extremity amputation in people with diabetes: systematic review and meta-analysis. BMJ Open Diabetes Res Care 2017;5:1–10. 10.1136/bmjdrc-2016-000366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ismail K, Winkley K, Stahl D, et al. A cohort study of people with diabetes and their first foot ulcer: the role of depression on mortality. Diabetes Care 2007;30:1473–9. 10.2337/dc06-2313 [DOI] [PubMed] [Google Scholar]
- 36.Gonzalez JS, Peyrot M, McCarl LA, et al. Depression and diabetes treatment nonadherence: a meta-analysis. Diabetes Care 2008;31:2398–403. 10.2337/dc08-1341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nouwen A, Adriaanse MC, van Dam K, et al. Longitudinal associations between depression and diabetes complications: a systematic review and meta-analysis. Diabet Med 2019;36:1562–72. 10.1111/dme.14054 [DOI] [PubMed] [Google Scholar]
- 38.Volmer-Thole M, Lobmann R. Neuropathy and diabetic foot syndrome. Int J Mol Sci 2016;17:917 10.3390/ijms17060917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Prompers L, Schaper N, Apelqvist J, et al. Prediction of outcome in individuals with diabetic foot ulcers: focus on the differences between individuals with and without peripheral arterial disease. The EURODIALE study. Diabetologia 2008;51:747–55. 10.1007/s00125-008-0940-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Meloni M, Izzo V, Giurato L, et al. A Complication of the Complications: The Complexity of Pathogenesis and the Role of Co-Morbidities in the Diabetic Foot Syndrome 2018 : Piaggesi A, Apelqvist J, The diabetic foot syndrome. Basel, Karger: Front Diabetes, 2018: 19–32. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjdrc-2020-001355supp001.pdf (249.4KB, pdf)