Abstract
Background
Patient satisfaction is a common measure of the success of an orthopaedic intervention. However, there is poor understanding of what satisfaction means to patients or what influences it.
Questions/purposes
Using qualitative study methodology in patients undergoing TKA, we asked: (1) What does it mean to be satisfied after TKA? (2) What factors influence satisfaction levels after TKA?
Methods
People in a hospital registry who had completed 12-month follow-up questionnaires and were not more than 18 months post-TKA at the time of sampling were eligible (n = 121). To recruit a sample that provided insight into a range of TKA experiences, we divided eligible candidates on the registry into quadrants based on their responder status and satisfaction level. A responder was an individual who experienced a clinically meaningful change in pain and/or function on the WOMAC according to the Outcome Measures in Rheumatology-Osteoarthritis Research Society International (OMERACT-OARSI) responder criteria. Individuals were considered satisfied unless they indicated somewhat dissatisfied or very dissatisfied for one or more of the four items on the Self-Administered Patient Satisfaction Scale. From the resulting quadrants: responder satisfied, nonresponder satisfied, nonresponder dissatisfied, responder dissatisfied, we identified men and women with a range of ages and invited them to participate (n = 85). The final sample (n = 40), consisted of 10 responder satisfied, nine nonresponder satisfied, eight nonresponder dissatisfied, and 13 responder dissatisfied; 71% were women, with a mean age of 71 ± 7 years and a mean time since TKA surgery of 17 ± 2 months (range 13 to 25 months). Interview transcripts were analyzed by looking for factors in the participants' narrative that appeared to underscore their level of satisfaction and attaching inductive (data-derived, rather than a priori derived) codes to relevant sections of text. Coded data from participants who reported high and low levels of satisfaction were compared/contrasted and emerging patterns were mapped into a conceptual model. Recruitment continued until no new information was uncovered in data analysis of subsequent interviews, signalling to the researchers that further interviews would not change the key themes identified and data collection could cease.
Results
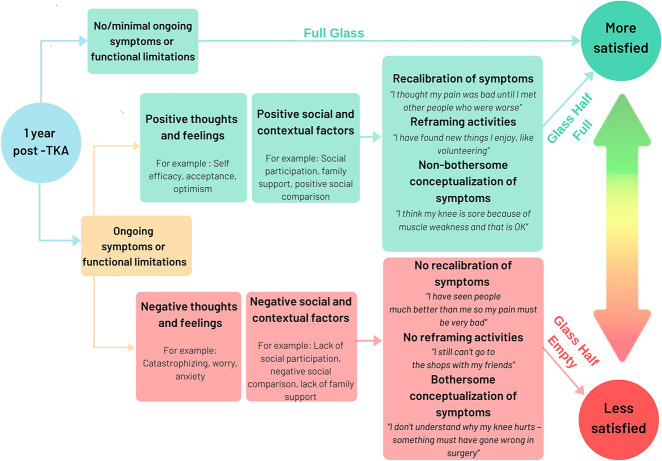
In those with high satisfaction levels, satisfaction was conceptualized as an improvement in pain and function. In those with low satisfaction levels, rather than an improvement, satisfaction was conceptualized as completely resolving all symptoms and functional limitations. In addition, we identified three pathways through which participants reached different levels of low and high satisfaction: (1) The full-glass pathway, characterized by no or minimal ongoing symptoms and functional deficits, which consistently led to high levels of satisfaction; (2) the glass-half-full pathway, characterized by ongoing symptoms and functional limitations, which led to high satisfaction; and (3) the glass-half-empty pathway, also characterized by ongoing symptoms and functional limitations, which led to low satisfaction levels. The latter two pathways were mediated by three core mechanisms (recalibration, reframing valued activities, and reconceptualization) influenced either positively or negatively by (1) a persons’ thoughts and feelings such as optimism, self-efficacy, pain catastrophizing, external locus of control; and (2) social and contextual factors such as fulfilment of social roles, therapeutic alliance, lack of family/social support.
Conclusions
This qualitative study suggests that for preoperative patients in whom unrealistically high hopes for complete symptom resolution and restoration of functional capacity persists, it may be appropriate to direct them away from TKA due to the risk of low satisfaction. For postoperative patients troubled by ongoing symptoms or functional limitations, clinicians may improve levels of satisfaction by targeting the three core mechanisms (recalibration, reframing valued activities, and reconceptualization) through addressing modifiable negative thoughts and feelings in interventions such as psychology or psychotherapy; and negative social and contextual factors by promoting a strong therapeutic alliance and engagement in community activities. Given that these factors may be identifiable preoperatively, future research is needed to explore if and how addressing them preoperatively may improve satisfaction post-TKA.
Level of Evidence
Level IV, therapeutic study.
Introduction
The effect of TKA is best measured from the patient’s perspective. Alongside other patient-reported outcome measures, such as pain and disability, satisfaction is commonly used to evaluate patients’ perceptions of surgical success [8, 9]. Reflecting the growing usage of measuring patient satisfaction, it has been included as a core outcome post-TKA according to a Delphi study by the Outcome Measures in Rheumatology initiative [34]. However, concerns have been raised regarding the meaningfulness of this measurement [33]. Satisfaction is likely to be influenced by various factors, such as patient expectations for TKA and how well they are addressed [4, 5, 22], levels of distress (symptoms of anxiety and depression) [5, 22, 25], and the hospital experience and interactions with the surgeon [4, 5]. Each factor may vary from patient to patient, such that the same surgical outcome may result in discrepant satisfaction levels [33]. As a result, current attempts to measure patient satisfaction are limited in their ability to be meaningfully interpreted because the available measures lack the ability to capture the depth or nuance associated with a patient appraisal of surgical outcome [33], and suffer strong ceiling effects. Driving these validity issues is a lack of important theoretical grounding, specifically the patient’s perspective of satisfaction after TKA, to inform questionnaire development [24]. Thus, research approaches such as qualitative inquiries that elicit the patient’s perspective on their satisfaction after TKA are needed to improve understanding of how to measure this construct.
Creating meaning from satisfaction scores is further clouded by a lack of consensus regarding question design. Tools purporting to measure satisfaction have used single items with various foci (such as satisfaction with pain, overall satisfaction, function, surgery); some have used amalgamated scales of different components of satisfaction, while others have attributed satisfaction to other constructs such as fulfilment of expectations [22]. Given that the design of the question influences satisfaction scores [12], certainty of what is being captured from one type of question to the next remains unclear.
These issues are not surprising given how rarely the patient’s perspective has been explored during the development of tools to measure satisfaction after TKA. As the meaning of satisfaction or dissatisfaction after TKA is unclear, efforts to interpret quantified satisfaction outcomes to this point have been speculative at best. To address these deficiencies in our understanding of patient satisfaction after TKA, and to identify potential targets for improving satisfaction, we undertook a qualitative study. Through interviews with patients who experienced a range of outcomes from TKA, the aim of this qualitative study was to shed light on how people arrive at different levels of satisfaction.
The specific questions governing this study were: (1) What does it mean to be satisfied after TKA? (2) What factors influence satisfaction levels after TKA?
Patients and Methods
Study Design and Setting
We conducted a cross-sectional qualitative study in the orthopaedic clinic of a large tertiary hospital in metropolitan Australia. This clinic receives state-wide referrals, performs a large volume of TKAs, and routinely collects 12-month registry data on all patients who undergo a lower limb joint replacement and records patients’ outcomes longitudinally.
This study was conducted in accordance with the ethical standards in the 1964 Declaration of Helsinki. Ethics approval was granted by St Vincent’s Hospital (Melbourne) Human Research Ethics Committee (HREC/17/SVHM/251).
Participants
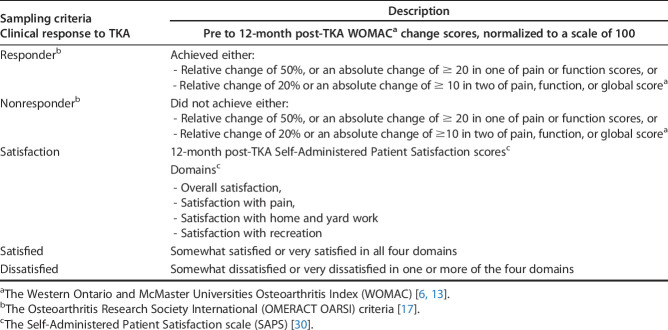
Patients who were 12 to 25 months post-TKA for knee osteoarthritis with completed 12- month registry data were eligible. The time frame of 12 to 25 months post-TKA was considered an appropriate follow-up as this study was concerned with identifying the factors and processes that shape satisfaction, which might then be targeted to improve satisfaction at later time points. Patients more than 18 months post-TKA at the time of sampling were included in this study as data collection spanned over 6 months. Patients who spoke a language other than English were eligible to participate through a qualified interpreter. Patients were ineligible if they had a cognitive impairment that prevented them from providing meaningful responses to interview questions. We sought to include people with a range of TKA outcomes and experiences in our study. To do this, we divided eligible patients into quadrants based on their Osteoarthritis Research Society International responder status and satisfaction levels: responder satisfied, responder dissatisfied, nonresponder satisfied, and nonresponder dissatisfied [6, 13, 17, 30]. A responder was defined as someone who had experienced a clinically meaningful change in pain and/or function after TKA [6, 13, 17] (Table 1). We emphasize that grouping people this way was simply a tool to assist purposive sampling, which enabled us to identify individuals with a range of experiences. The grouping of patients this way held no weight on the analytic process, nor was there any intention to suggest who should be satisfied or dissatisfied based on these metrics. Within each quadrant, we identified men and women with a range of ages to ensure a variety of voices were represented in our final sample.
Table 1.
Criteria for the four sampling quadrants
Consistent with the qualitative framework, data collection and analysis were conducted concurrently. This enabled emerging patterns in the data to be tested in subsequent interviews. We continued to recruit individuals from each sampling quadrant until there was consensus agreement among authors that the data collected could answer our research question and that the themes identified were unlikely to change through interviews with additional participants. This consensus process took place over multiple meetings in which raw data and emerging themes were presented to the authorship team and these emerging themes were discussed, refined and challenged in the context of existing theory and clinical practice (see data analysis below).
Of the 121 people from the hospital registry who were eligible, 85 were invited to participate as a result of this purposive sampling strategy, and 41 consented and were interviewed. One interview was lost due to equipment malfunction. The proportions of each sampling quadrant from the 40 interviews were: 10 responder satisfied, nine nonresponder satisfied, eight nonresponder dissatisfied, and 13 responder dissatisfied. Of the remaining 44 people, 28 declined, 12 did not respond to letter or phone contact, and four were identified as inappropriate (two cognitive impairment, one undergoing treatment for surgical complication and one declined use of professional interpreter) (Table 2).
Table 2.
Participant characteristics
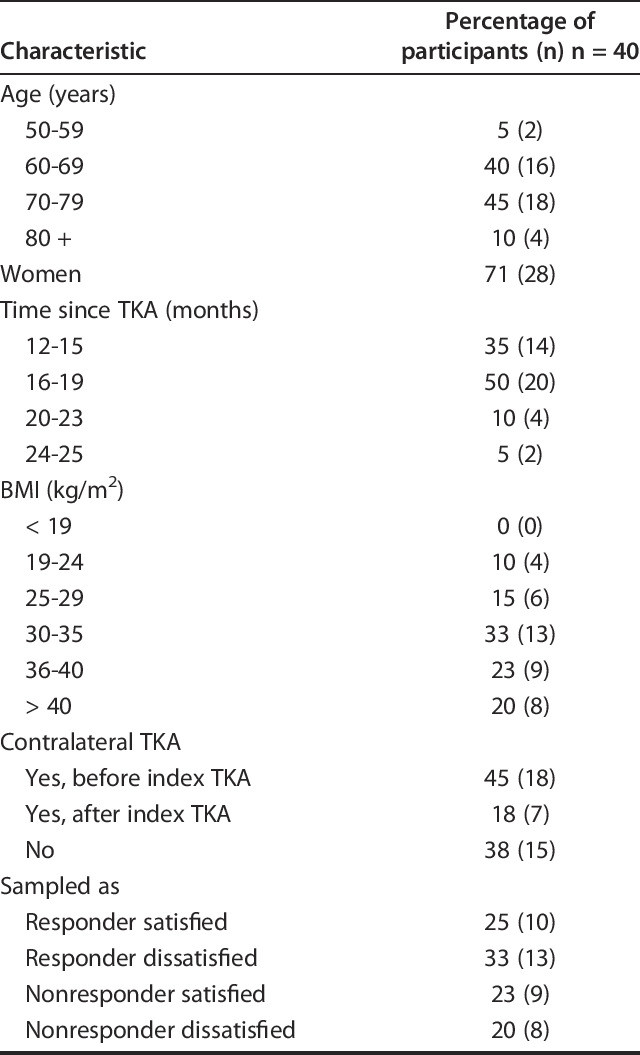
During the interviews, 29 participants reported high satisfaction levels during their interviews. Of these, 11 had no or minimal symptoms or functional limitations, while 18 had some degree of ongoing symptoms or functional limitations. Eleven participants reported low satisfaction levels during their interviews, and all had ongoing symptoms or functional limitation. Our sample did not include anyone who experienced a major surgical complication.
Data Collection
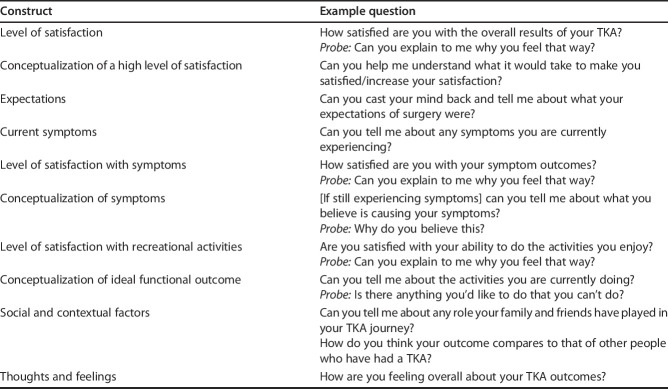
Both face-to-face (n = 12) and phone interviews (n = 28) were conducted in a private room in the hospital’s orthopaedic research department. There were no differences in the length, quality, or content between the two modes of interview. Interviews were conducted by a woman physiotherapist and PhD student (NRK) who received training from an experienced qualitative researcher (SB) and had no pre-existing relationship with any of the participants. In the interviews, participants were asked how satisfied they were with their TKA outcome and why. In addition, those reporting low levels of satisfaction were asked what it would take to be more satisfied. Participants were also encouraged to reflect on their TKA journey, including their expectations for surgery and postoperative experiences, and how they conceptualized (understood) the current symptoms they were experiencing. Interview questions remained flexible to explore/test new concepts as they arose (Table 3). Interviews lasted 50 minutes on average, were audio recorded, and transcribed before analysis.
Table 3.
The example interview schedule
Data Analysis
The present study followed a constructivist grounded theory methodology [10]. This methodology is an inductive (data derived, rather than a priori derived) approach to analyzing primary qualitative data that facilitates the development of theory grounded in participants' voices [11]. Constructivist grounded theory acknowledges the researchers’ prior knowledge and experience in the data analysis and aims to understand the processes and patterns of a given phenomenon, rather than offer descriptions or narrative accounts [11]. The development of theory in this way can offer useful clinical information, which can later be tested using quantitative research approaches in larger, generalizable samples. This method has successfully been applied to develop theory and guide clinical practice in the broader health literature. For example, Law et al. [26] used constructivist grounded theory to understand how patient-practitioner mistrust hinders effective tuberculosis management and developed a clinically useful model to address mistrust and encourage treatment adherence [26].
Data analysis in this study involved the full research team, which consisted of clinical and research physiotherapists (AS, PO, PK, NRK), an orthopaedic research nurse (MMD), an orthopaedic surgeon and researcher (PFC), a clinical and research psychologist (RS), and a qualitative expert (SB). The team had common research interests in improving treatment outcomes for people with chronic musculoskeletal pain.
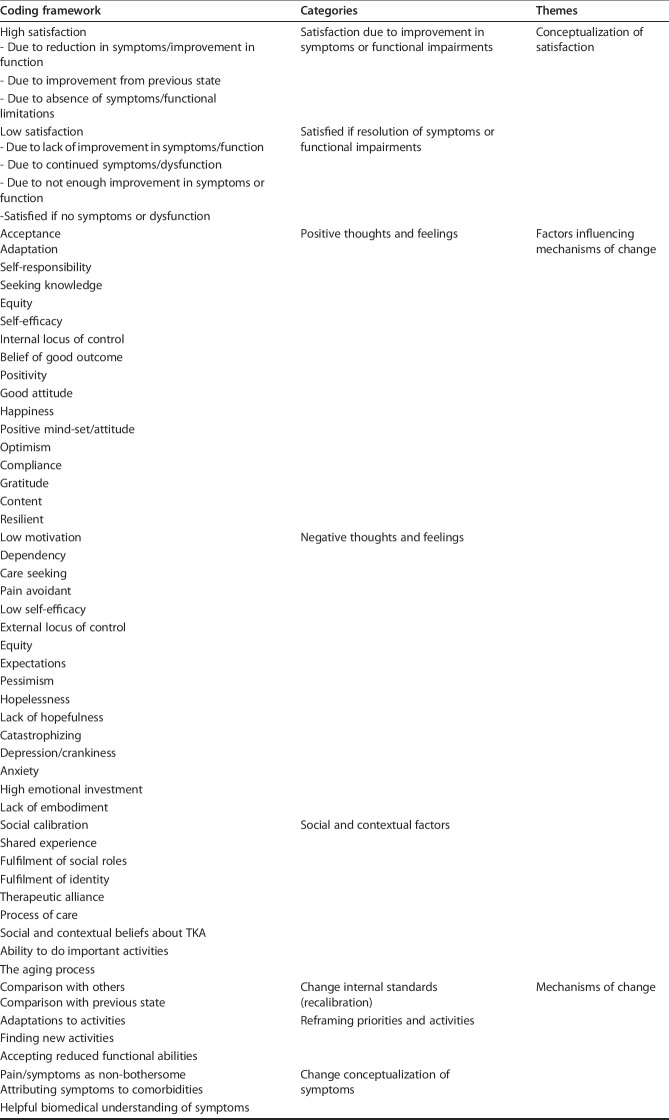
Data analysis involved the following stages: (1) Reading and re-reading the transcripts for familiarization by two authors (NRK, SB). (2) Coding of transcripts by two authors independently (NRK, SB). In this process, relevant sections of text related to the questions, “What does being satisfied mean to this person?” and “What influences the level of satisfaction in this person?” were given a code. For example, when a person described support they received from their family or friends the text fragment was coded family or social support. Although the authors were aware of pre-existing variables known to affect satisfaction levels, such as narcotic use, workplace compensation or litigation, anxiety, and depression, the purpose of this analysis was to reflect the participants’ perspectives on satisfaction after TKA rather than to validate existing knowledge. Therefore, we did not decide on any codes a priori; coding was an inductive (data-derived) process based on what we identified in the participants narratives. (3) Codes from each author were merged into a comprehensive coding framework (Table 4, left hand column), which consisted of clearly defined codes that covered all relevant raw data so that it could be consistently applied to all transcripts. (4) Coded data from participants who reported high and low levels of satisfaction were compared/contrasted. (5) Emerging patterns were mapped into a conceptual model through round table discussion involving the multidisciplinary authorship team. To test aspects of the model, additional participants were recruited. For example, to test the emerging theory that social support was important in the pathway to satisfaction, we recruited additional participants from the dissatisfied quadrants and asked them about the involvement of friends and family along their TKA journey. (6) We continued to refine the model until the research team perceived that it captured the experiences of all the participants in the study and provided a robust description of satisfaction, and the processes resulting in satisfaction. At this point, we considered that we had reached data saturation (no new information was discovered in data analysis, signalling to the researchers that data collection may cease).
Table 4.
The coding framework and process of data reduction
Study Outcomes
Our primary study outcome was to understand what it meant to be satisfied after TKA from the patient’s perspective. Through our process of data analysis, we specifically coded for the participant’s reasoning of why they had either high or lower levels of satisfaction. These codes were collated within participants, then between participants to identify patterns and common stories driving the conceptualization of satisfaction. After this back and forth process of testing patterns and themes, two key concepts were identified: In those with high satisfaction levels, satisfaction was conceptualized as an improvement in pain and function; whereas, in patients with low satisfaction levels, rather than an improvement, satisfaction was conceptualized as completely resolving all symptoms and functional limitations.
Our secondary study outcome was to identify what factors influenced patient satisfaction after TKA. Like our primary outcome, codes were given to fragments of the raw interview data that appeared influential in levels of satisfaction. Themes for those with reports of high satisfaction levels were compared with those with low satisfaction levels. Patterns and discrepancies were discussed within the authorship team until consensus was reached. We identified two key concepts: For patients with minimal or no ongoing symptoms or functional limitations, they experienced a direct pathway to high satisfaction levels; in those with ongoing symptoms or functional limitations, their satisfaction level was a result of three core mechanisms (recalibration, reframing valued activities, and reconceptualization), affected by either positive or negative thoughts and feelings, and social and contextual factors.
Study outcomes 1 and 2 are described in more detail below. Each key theme is supported with a quote from a participant indexed by the participants’ identification number, their gender, age, and time since their TKA, for example: (Participant 1, Man, 65, 15 months).
Results
What Does it Mean to be Satisfied After TKA?
Among the participants who reported high satisfaction levels, being satisfied meant being better off than before the operation, that is, improvement in symptoms or functional limitations (not suggesting the need to be completely pain free, or free of functional limitations). For example, Participant 01 reported being very satisfied with his TKA outcome because he had experienced an improvement in his pain, rather than a complete resolution in pain: “[I’m satisfied] because I’ve got more movement and less pain ... I can do all the activities without as much pain as I used to have.” (Participant 01, Man, 73 years, 24 months).
In contrast to those with high satisfaction levels, for participants who reported low satisfaction levels, it was not enough to be better off than before the operation; for them, to be satisfied would require a complete resolution of symptoms and functional limitations. For example, Participant 34 explained that she would have been satisfied if she did not have any pain or functional problems engaging in the activities she enjoyed: “[I’d be satisfied if] I could ride a bike without pain. I could camp without any problems. I could get in and out my four-wheel drive without pain. I could get down on the floor with my granddaughter.” (Participant 34, Woman, 60 years, 19 months).
Participant 20, who experienced persistent pain and required a walking aid, said that to be satisfied she would like her pain to have gone and her functional abilities restored: “Well I expected the pain to go away and you know just being able to walk, you know without hanging onto – or even with a walker would be alright but just to walk would be a good idea.” (Participant 20, Woman, 77 years, 16 months).
What Factors Influence Satisfaction After TKA?
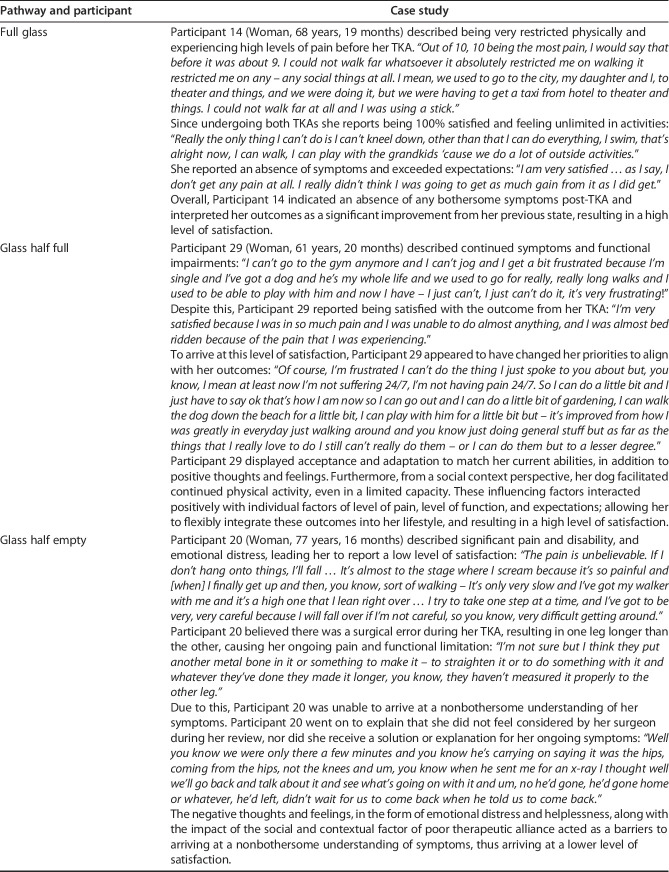
We identified three pathways to satisfaction outcomes (Fig. 1). The first pathway (full glass), which involved no or minimal ongoing symptoms or functional limitations, consistently led to reports of high satisfaction levels. The other two pathways (glass half full and glass half empty), which involved the presence of ongoing symptoms and functional limitations, consistently led to differing levels of low and high satisfaction, depending on the participants’ understanding of any ongoing symptoms and their perception of symptom severity; their level of participation in daily/social life; and their thoughts, feelings, social support and interactions with their surgeon. Each pathway is described in detail below and illustrated with a case study (Table 5).
Fig. 1.
Framework of patient satisfaction post-TKA is shown here.
Table 5.
Case studies
Full Glass
The full glass pathway (n = 11) was characterized by minimal or no ongoing symptoms or functional limitations, resulting in an increased capacity to participate in a range of activities and a direct pathway to high satisfaction (Fig. 1). The following quote is an example of a participant who expressed a lack of functional limitations and very minimal pain. He experienced a direct pathway to satisfaction: “I’m running around the ring showing me dogs again now I’ve got mobility; it’s fantastic it really, really, brings you right out you know, compared to what it was before. Me grand kids had to show me dogs before, so now I can show them me self.” (Participant 16, Man, 67 years, 20 months).
Glass Half Full
The glass half full pathway (n = 18) was characterized by high satisfaction levels despite ongoing symptoms and functional limitations. These participants arrived at a high satisfaction level through one or more of three mechanisms of change: recalibration, reframing valued activities, or reconceptualization.
The first mechanism of change involved recalibrating how severely they perceived their ongoing symptoms or function limitations. Participants did this by comparing themselves with others their age, or others who had undergone a TKA, with similar or worse outcomes. For example, after being exposed to others with a broad range of TKA outcomes through an online forum, Participant 34 recalibrated her symptoms to a lower severity: “I've spoken to numerous different people who have had the same surgery prior to me having it, in fact, prior to even me making the decision to have it. Some have said they’ve never looked back. Since then, I’m on different forums and there’s a lot of people that are a lot, lot worse off than me, yet again, that are still having substantial pain 12 months down the track and don’t have the mobility or range of movement.” (Participant 34, Woman, 60 years, 19 months).
Another mechanism of change was reframing valued activities, where participants shifted their priorities in life to align with their TKA outcomes. This could take the form of letting go of or adjusting enjoyable activities or finding new activities. For example, Participant 28 was no longer able to do the things she really enjoyed but had reframed her valued activities to a modified version of what she could previously achieve and thereby reported high satisfaction: “I mean at least now I’m not suffering 24/7, I’m not having pain 24/7. It’s improved from how I was greatly in everyday, just walking around and you know just doing general stuff but as far as the things that I really love to do I still can’t really do them. Or I can do them but to a lesser degree.” (Participant 29, Woman, 61 years, 20 months).
A third mechanism of change was reconceptualization; participants attributed their ongoing symptoms to their age and/or the aging process, a continued healing process, or other comorbidities, rather than a threatening defect with their joint replacement. For example, Participant 30 attributed the ongoing pain she experienced in her knee to her long-standing back pain. As a result of this reconceptualization, the pain in her knee was not threatening, and she was satisfied with her TKA outcome: “There’s still pain, it’s more like pins and needles or a little twinge now and again, like if I move it sudden, or some sort of exercise. The back of the leg up here, into the buttocks area. Don’t know if it’s [the] leg causing it or my spine. But I would say it’s my spine, ‘cause I've got my discs L3 and all that are out. And they’ve prolapsed.” (Participant 30, Woman, 63 years, 20 months).
Each of these change mechanisms were facilitated by positive thoughts and feelings, such as self-efficacy, optimism, and compliance. Participant 14 demonstrates how she took an active, self-efficacious approach to receiving a TKA, and how she was going to be as compliant as possible with rehabilitation: “Well, the mind tells me that you’re having it done and there’s no point having it, going through all this for you; and you’ve got to make the most of it. And try do exactly what you’re told to do with the physiotherapy.” (Participant 14, Woman, 68 years, 19 months).
Positive social and contextual factors, including family support, social participation, and positive therapeutic encounters, particularly with their surgeon, were also facilitators. For example, Participant 27 had much support from his family, including his grandson who encouraged him to keep active: “I didn’t try the dancing yet, but I try to walk as much as possible with our grandson and with my doggy. Yeah but I can feel, I can see is a much better than before, when I walk and yeah is much better.” (Participant 27, Man, 60 years, 15 months).
Participant 34 experienced a strong therapeutic alliance with a clinician who she perceived was supportive and reassuring along her TKA journey: “Same surgeon for both, but he was awesome. He was really good. Open, encouraged questions, showed me the x-rays up on the screen, didn’t hurry me through a consultation. Some just push, push, push and then get you out. He said on a number of occasions, ‘Anymore questions?’ Yeah, I found him very efficient but, yet, he had a really good bedside manner.” (Participant 34, Woman, 60 years, 19 months).
Glass Half Empty
The glass half empty pathway (n = 11) was characterized by low satisfaction levels in the presence of ongoing symptoms and functional limitations. Unlike participants in the glass half full pathway, these participants did not experience any of the change mechanisms described above. In approaching the analysis for this group of participants, the authors wish to emphasize the key themes identified were grounded in the participant’s stories. Due to this, some factors known to affect satisfaction levels from quantitative research, such as narcotic use, did not emerge as an important factor affecting satisfaction levels from the perspectives of the participants in this sample. Further, due to the public hospital setting of our study, workers compensation or litigation cases were not relevant to our study population and, therefore, would not be expected to emerge as a key theme.
Participants did not appear to recalibrate internal standards of symptoms or function due to either a lack of exposure to others with poorer outcomes or exposure to others with better outcomes. For example, compared with her husband’s outcome from TKA, Participant 40 believed her outcomes should have been better and therefore reported being dissatisfied: “Compared to my husband, I'm dissatisfied. My husband had two knee replacements, and he is walking normally, jumping up and down in bed, completely mobile, and I'm completely dependent on him. And I thought I would've been able to dress myself and just be completely mobile, just in the normal things.” (Participant 40, Woman, 71 years, 15 months).
A reframing of valued activities was not apparent from interviews with participants in this pathway. Some participants in this pathway reported being unable to engage in their valued activities due to either a lack of social participation and/or emotional distress due to continued symptoms and impairments. For example, Participant 20, was unable to adjust or reframe her valued activities and, as a result, felt dissatisfied that she could not participate in social activities: “[If I was confident] I’d be going on the trips and you know sort of when they have concerts and things here down in the main lounge room, you know singers come and things like that I can’t go and sit there for a couple of hours. You know half an hour would be the longest I could sit and trying to get up the pain is so bad you know I can’t do anything like that now.” (Participant 20, Woman, 77 years, 16 months).
The process of reconceptualization also appeared to be absent for participants in this pathway. Some participants in this pathway attributed their ongoing symptoms to a problem with the joint replacement, often blaming this on surgical incompetence. For example, Participant 39 was troubled by a lack of explanation for her persistent symptoms. As a result, she felt something was not done correctly in the surgery: “To me I still feel there’s something they didn’t do properly, or (the surgeon) hasn’t done it properly or there’s something wrong with the actual knee. The kneecap gets really sore. I shouldn’t be getting sore, and I am still getting the pain that I used to get before I had the operation.” (Participant 39, Woman, 74 years, 13 months).
This perception appeared to be reinforced by negative encounters with their surgeon. Participant 34 felt dismissed by her surgeon, who did not assist in her understanding of her persistent symptoms or functional limitations: “I saw a particular doctor who, after a 4-and-a-half-hour trip down there, said, ‘Let me look at the scar. It's healed nicely. Thank you very much. Goodbye.’ You know? So, I was most dissatisfied with that after an 11-hour trip by the time that we got home that day.” (Participant 36, Woman, 70 years, 16 months).
Other negative social and contextual factors, such as an inability to fulfil social roles and a lack of family support, as well as negative thoughts and feelings such as emotional distress, catastrophic thoughts, and anxiety all appeared to play a role in this glass half empty pathway, which led to low levels of satisfaction. Participant 20 displayed thoughts and feelings consistent with pain catastrophising and high levels of distress: “Well, the pain and the whole thing I just wish I was dead, that’s how I’m feeling, you know I’d just rather not be here. [I’m] quite distressed about it because I can’t go anywhere you know. Here they have bus trips and things like that, and I can’t go on them because I can’t walk.” (Participant 20, Woman, 77 years, 16 months).
Discussion
Patient satisfaction is important when assessing the success of orthopaedic interventions. However, a lack of understanding of what satisfaction means to patients makes it difficult to interpret satisfaction scores [32]. Through qualitative interviews with patients post-TKA, we found that satisfaction after TKA was a function of the presence or absence of ongoing symptoms and/or functional limitations. In the absence of ongoing symptoms or functional limitations, patients reported high satisfaction levels. In the presence of ongoing symptoms or functional limitations, a range of factors, some modifiable (such as, pain catastrophizing, low self-efficacy, poor therapeutic alliance, and social isolation), appeared to influence a patient’s pathway to higher or lower satisfaction levels.
Limitations
Consistent with our qualitative approach, we sought to capture a wide range of experiences and perspectives in our sample, so we purposely recruited people with a range of TKA outcomes. This enabled us to capture the voices of people with not only high, but also low levels of satisfaction who are often difficult to engage in research. However, readers should be cognizant that our sample is not representative of the TKA population and does not provide an estimate of the proportion dissatisfied after TKA. Unlike quantitative studies, qualitative studies are not seeking to estimate the likely range of a parameter (such as, prevalence, odds ratio, risk ratio) from their sample that can be extrapolated to the population of interest. Instead, qualitative research seeks to gain rich descriptions from a small sample of people who have experienced the phenomenon of interest. In doing this, qualitative research is interested in diversity and understanding a range of experiences. It is important to note that qualitative research is hypothesis-generating and does not seek to definitively produce generalizable results [27]. Thus, the issue of selection bias is not a consideration for qualitative research; however, each reader should carefully consider our sample to see if our findings are applicable to his or her setting or context, as the participants in this study may differ from the wider population in important ways. For example, it is possible that the participants here had higher health literacy than the wider population, as patients with lower health literacy may have been less likely to accept our invitation to participate. We recruited from a single site, and thus the experiences of the participants in this study will reflect aspects of the pre- and post-TKA care that is typical to this service. Additionally, this study was set in an Australian public hospital where TKAs are government-funded procedures. Incurring a financial cost may influence expectations of care, particularly given the role that process variables, such as surgeon interactions, played in reports of satisfaction among our sample. Future studies are needed to explore if and how our model captures the experiences of patients in other settings [4].
Although our model describes a process that unfolds over time, data were collected retrospectively at one time point and thus relied on the participants’ recall of the TKA journey. Additionally, the scope of this study was to explore patients’ conceptualization of, and pathways to, satisfaction 12 to 25 months after TKA. Although exploration of these factors before surgery would have been an interesting and potentially useful addition to this study, it does not detract from the utility of the results to assist clinicians in improving satisfaction levels in patients who are troubled by ongoing symptoms or functional limitations. Coding was conducted by two authors (NRK, SB) and, in accordance with the qualitative approach, was not tested for intra- or interobserver reliability. By providing an audit trail that describes the logical process of arriving at codes, themes, and theory through our own world view, we are confident that someone independent of the authorship team would be able to read the transcripts and identify similar codes in relation to our research question. Although other interpretations of our data are possible, for example, a thematic description of the lived experience after TKA, our aim was to develop a clinically useful framework to assist clinicians to improve patient satisfaction with TKA. Insights into the lived experience after TKA have been reported elsewhere [3, 19, 21].
Although previous research has identified depression, anxiety, antecedent narcotic use, or workers compensation as predictors of patient satisfaction [14, 18, 25], we did not have access to this information in our registry data to describe our sample. We emphasize that the aim of the study was to elicit the participant’s perception of what contributed to their level of satisfaction, and our identification of depression, anxiety and self-efficacy in the participants’ narratives lends support to previous quantitative findings. Although we endeavored to create a comfortable judgement-free environment for each interview, social desirability forces may have prevented participants from describing their experiences with narcotic use or workers compensation. Our results further suggest that this ability to adapt is influenced by a myriad of factors, including mental health and issues relating to social support or the therapeutic process. However, understanding whether satisfaction is a standalone construct, or merely a proxy for assessing the adaptability of patients (or other factors like anxiety and depression), requires further quantitative investigation. Future research should consider empirically testing the assumptions of our theoretical model and exploring its intersection with the previously known factors associated with patient satisfaction to advance orthopaedic knowledge of the utility in measuring this construct.
What Does it Mean to be Satisfied After TKA?
Participants in this study who reported high satisfaction levels, regardless of the presence of any ongoing symptoms or functional limitation, considered satisfaction to mean some improvement in symptoms and/or functional limitations. This finding is supported by two systematic reviews, which have documented the influence of improvements in pain and function outcomes in reports of satisfaction [20, 22]. A novel finding from our study was that all those who reported low satisfaction levels felt that to be satisfied would have called for a complete resolution of symptoms and/or functional limitations, rather than only an improvement. Our findings illustrate the need for surgeons to be more specific in their preoperative patient education pertaining to the likelihood of persistent symptoms and functional limitation after TKA. For example, surgeons can explain that a resolution of symptoms and restoration in function is unrealistic for most patients and they should reconsider the procedure if these are their expectations.
What Factors Influence Satisfaction After TKA?
The pathways to high or low satisfaction levels in the presence of ongoing symptoms or functional limitations were influenced by a range of modifiable factors such as lack of social exposure to others with TKA, lack of participation in social activities, low self-efficacy, pain catastrophizing, and poor understanding of persistent symptoms. However, those without ongoing symptoms or functional limitations experienced a direct pathway to high satisfaction levels. Contrary to what surgeons may believe [10], our findings demonstrate how satisfaction may have little to do with more tangible outcomes, such as complications or biomechanical factors. Instead, satisfaction likely has more to do with the patient’s world view and individual traits. Previous evidence has identified the association of negative thoughts and feelings (such as anxiety and depression) [1, 22], and low levels of social support [22, 23] with lower satisfaction levels. Our study demonstrates how thoughts, feelings, social and contextual factors interact with ongoing symptoms or functional limitations on the pathways to different satisfaction levels. For example, people with lower levels of satisfaction may present with negative thoughts and feelings, such as hopelessness or pain catastrophizing, in combination with negative social and contextual factors including the inability to do socially enjoyable activities and poor therapeutic alliance. These factors can affect how they understand or manage their symptoms or functional limitations, thus affecting their satisfaction level. Our findings are consistent with the response shift observed in the quality-of-life evidence. Response shift describes how quality-of-life assessments can change despite no alteration in objective circumstances, as a result of recalibrating (for example, comparing one’s situation to that of others who are less well off), reprioritizing (such as, finding new activities to enjoy), or reconceptualizing (including no longer considering health symptoms to be a threat) [2, 7]. Despite many studies attributing patient satisfaction to fulfilment of expectations [29, 32], the findings of this study suggest that expectations are only one part of the satisfaction puzzle; the other parts include the presence or absence of ongoing symptoms or function limitations, and in the presence of them, how the individual adapts and accepts them. Our findings agree with research suggesting patients calibrate their expectations to pain and function outcomes [28], and that expectations alone cannot predict satisfaction [31].
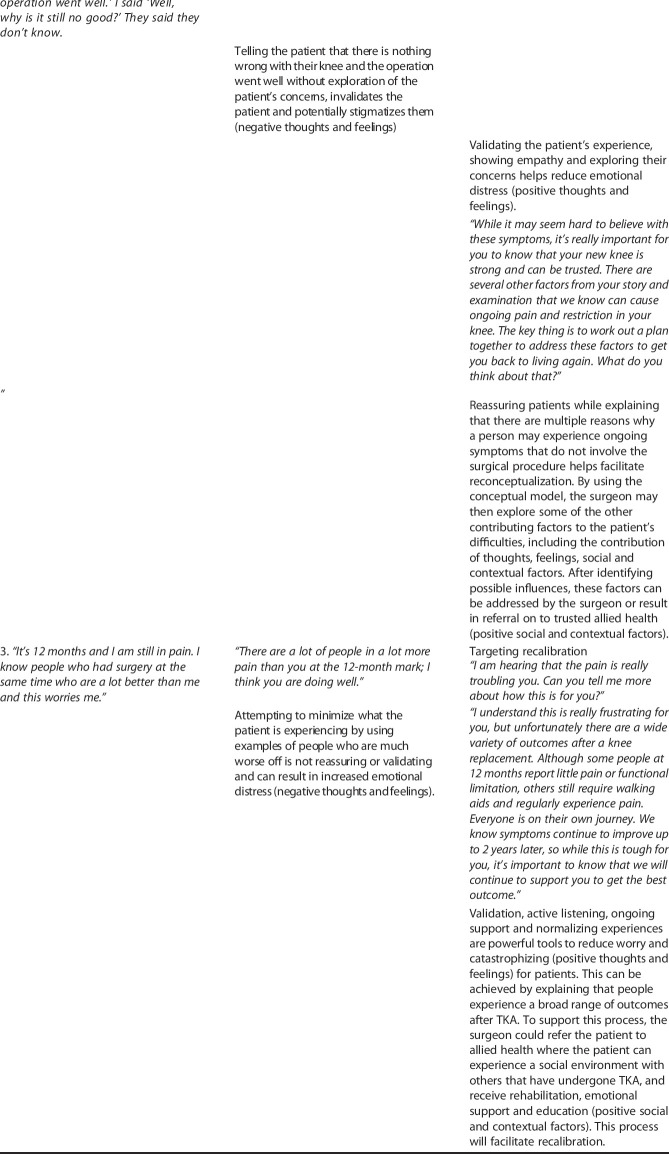
The results of this work illustrate how patients can arrive at high satisfaction levels through the three core mechanisms (recalibration, reframing valued activities, and reconceptualization), often without therapeutic intervention. However, with knowledge of these mechanisms, our findings suggest that clinicians can play an important role in facilitating higher levels of satisfaction when patients are troubled by ongoing symptoms and functional limitations. This could occur through: (1) Asking patients about any ongoing symptoms/functional limitations, what they believe is causing them, the effect they are having on their lives, and how severe they believe they are; and (2) identifying and targeting modifiable barriers to satisfaction (understanding of ongoing symptoms, social participation, confidence, self-efficacy, pain catastrophizing, depression) in the context of the individual patient. Based on our conceptual model and supported by subjective reports of therapeutic encounters from the participants in our sample, we have provided example strategies to facilitate the three mechanisms of change and address negative thoughts, feelings, social and contextual factors (Table 6). Other key areas the surgeon can target include positive communication techniques, active listening, and being available for patient follow-up appointments, rather than leaving patient follow-up in the hands of junior doctors or other allied health professionals. Clinicians may also consider applying pre-TKA screening tools that can identify patients with negative thoughts and feelings, which may predict low satisfaction levels [16]. We emphasize that patients are likely to present with more than one modifiable barrier to satisfaction and it is unlikely that these can all be addressed in a single consultation. For patients presenting with multiple barriers, such as negative thoughts, feelings, social and contextual factors, we recommend focusing on communication strategies that are validating, reassuring, patient-centered and that build confidence, acceptance, and self-efficacy. It may be that these factors are best targeted pre-TKA to improve patient outcomes, however, further research is needed to test the efficacy of this. Following this, and a review of whether rehabilitation has been adequate, it may be appropriate to refer the patient to allied health for further support to improve the patient’s satisfaction levels. Consulting services such as psychiatry and colleagues in the allied health professions like physiotherapy, occupational therapy, social work, psychology provide patients with access to a range of evidence-based interventions may be able to target the modifiable factors identified in this study, including mindfulness, which has shown to be effective in the TKA population [15].
Table 6.
Helpful communication
Conclusions
This qualitative study has demonstrated the importance of educating patients about the likely outcomes after TKA, especially the possibility of continued symptoms and functional limitations. In patients who continue to believe that their symptoms will be resolved, and their functional capacity completely restored, it may be appropriate to advise them away from TKA due to the risk of being dissatisfied postoperatively. In patients who are troubled by ongoing symptoms or functional limitations after TKA, the results of this study have described three core mechanisms (recalibration, reframing valued activities, and reconceptualization), which clinicians may use as a road map to improve patient satisfaction. In patients with low satisfaction, it is important to consider the influence of negative thoughts and feelings, such as symptoms of depression, feelings of hopelessness, and poor self-efficacy, and address them through interventions such as psychology and psychiatry. Additionally, negative social and contextual factors, such as poor social support or inability to fulfil social roles, should be considered and addressed through focusing on a strong therapeutic alliance, social work referral, and seeking ways to engage patients in meaningful activities in their communities. It may be feasible to target the modifiable thoughts and feelings, as well as social and contextual factors pre-TKA, to reduce the likelihood of a patient becoming dissatisfied postoperatively. However, future empirical research is required to test the efficacy of intervening on these factors before surgery.
Footnotes
The institution of one or more of the authors (PFC, AS, PO, MMD) has received, during the study period, funding from the Australian National Health and Medical Research Council Centre of Research Excellence in Joint Replacement Surgery (APP1116325).
Each author certifies that neither he or she, nor any member of his or her immediate family, has funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was conducted in both St Vincent’s Hospital (Melbourne), Australia, and Curtin University, Perth, Australia.
References
- 1.Ali A, Lindstrand A, Sundberg M, Flivik G. Preoperative Anxiety and Depression Correlate With Dissatisfaction After Total Knee Arthroplasty: A Prospective Longitudinal Cohort Study of 186 Patients, With 4-Year Follow-Up. J Arthroplasty. 2017;32:767-770. [DOI] [PubMed] [Google Scholar]
- 2.Barclay-Goddard R, Epstein JD, Mayo NE. Response shift: a brief overview and proposed research priorities. Qual Life Res. 2009;18:335-346. [DOI] [PubMed] [Google Scholar]
- 3.Bardgett M, Lally J, Malviya A, Deehan D. Return to work after knee replacement: a qualitative study of patient experiences. BMJ Open. 2016;6:e007912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Batbaatar E, Dorjdagva J, Luvsannyam A, Amenta P. Conceptualisation of patient satisfaction: a systematic narrative literature review. Perspect Public Health. 2015;135:243-250. [DOI] [PubMed] [Google Scholar]
- 5.Batbaatar E, Dorjdagva J, Luvsannyam A, Savino MM, Amenta P. Determinants of patient satisfaction: a systematic review. Perspect Public Health. 2017;137:89-101. [DOI] [PubMed] [Google Scholar]
- 6.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833-1840. [PubMed] [Google Scholar]
- 7.Blome C, Augustin M. Measuring change in quality of life: bias in prospective and retrospective evaluation. Value Health. 2015;18:110-115. [DOI] [PubMed] [Google Scholar]
- 8.Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res. 2010;468:57-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bullens PH, van Loon CJ, de Waal Malefijt MC, Laan RF, Veth RP. Patient satisfaction after total knee arthroplasty: a comparison between subjective and objective outcome assessments. J Arthroplasty. 2001;16:740-747. [DOI] [PubMed] [Google Scholar]
- 10.Bunzli S, Nelson E, Scott A, French S, Choong P, Dowsey M. Barriers and facilitators to orthopaedic surgeons' uptake of decision aids for total knee arthroplasty: a qualitative study. BMJ Open. 2017;7:e018614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Charmaz K. Grounded Theory: Methodology and Theory Construction. In: Wright JD, ed. International Encyclopedia of the Social & Behavioral Sciences 2nd ed. Oxford: Elsevier; 2015:402-407. [Google Scholar]
- 12.Clement ND, Bardgett M, Weir D, Holland J, Gerrand C, Deehan DJ. The rate and predictors of patient satisfaction after total knee arthroplasty are influenced by the focus of the question. Bone Joint J. 2018;100:740-748. [DOI] [PubMed] [Google Scholar]
- 13.Collins NJ, Misra D, Felson DT, Crossley KM, Roos EM. Measures of knee function: International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form, Knee Injury and Osteoarthritis Outcome Score (KOOS), Knee Injury and Osteoarthritis Outcome Score Physical Function Short Form (KOOS-PS), Knee Outcome Survey Activities of Daily Living Scale (KOS-ADL), Lysholm Knee Scoring Scale, Oxford Knee Score (OKS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Activity Rating Scale (ARS), and Tegner Activity Score (TAS). Arthritis Care Res (Hoboken). 2011;63(Suppl 11):S208-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.de Beer J, Petruccelli D, Gandhi R, Winemaker M. Primary total knee arthroplasty in patients receiving workers' compensation benefits. Can J Surg. 2005;48:100-105. [PMC free article] [PubMed] [Google Scholar]
- 15.Dowsey M, Castle D, Knowles S, Monshat K, Salzberg M, Nelson E, Dunin A, Dunin J, Spelman T, Choong P. The effect of mindfulness training prior to total joint arthroplasty on post-operative pain and physical function: A randomised controlled trial. Complement Ther Med. 2019;46:195-201. [DOI] [PubMed] [Google Scholar]
- 16.Dowsey MM, Spelman T, Choong PF. Development of a Prognostic Nomogram for Predicting the Probability of Nonresponse to Total Knee Arthroplasty 1 Year After Surgery. J Arthroplasty. 2016;31:1654-1660. [DOI] [PubMed] [Google Scholar]
- 17.Escobar A, Gonzalez M, Quintana JM, Vrotsou K, Bilbao A, Herrera-Espineira C, Garcia-Perez L, Aizpuru F, Sarasqueta C. Patient acceptable symptom state and OMERACT-OARSI set of responder criteria in joint replacement. Identification of cut-off values. Osteoarthritis Cartilage. 2012;20:87-92. [DOI] [PubMed] [Google Scholar]
- 18.Franklin PD, Karbassi JA, Li W, Yang W, Ayers DC. Reduction in narcotic use after primary total knee arthroplasty and association with patient pain relief and satisfaction. J Arthroplasty. 2010;25(6 Suppl):12-16. [DOI] [PubMed] [Google Scholar]
- 19.Goldsmith LJ, Suryaprakash N, Randall E, Shum J, MacDonald V, Sawatzky R, Hejazi S, Davis JC, McAllister P, Bryan S. The importance of informational, clinical and personal support in patient experience with total knee replacement: a qualitative investigation. BMC Musculoskelet Disord [Research Support, Non-U.S. Gov't] 2017;18:127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gunaratne R, Pratt DN, Banda J, Fick DP, Khan RJK, Robertson BW. Patient Dissatisfaction Following Total Knee Arthroplasty: A Systematic Review of the Literature. J Arthroplasty. 2017;32:3854-3860. [DOI] [PubMed] [Google Scholar]
- 21.Jeffery AE, Wylde V, Blom AW, Horwood JP. "It's there and I'm stuck with it": patients' experiences of chronic pain following total knee replacement surgery. Arthritis Care Res (Hoboken). 2011;63:286-292. [DOI] [PubMed] [Google Scholar]
- 22.Kahlenberg CA, Nwachukwu BU, McLawhorn AS, Cross MB, Cornell CN, Padgett DE. Patient Satisfaction After Total Knee Replacement: A Systematic Review. HSS J [Review]. 2018;14:192-201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kim TK, Chang CB, Kang YG, Kim SJ, Seong SC. Causes and predictors of patient's dissatisfaction after uncomplicated total knee arthroplasty. J Arthroplasty. 2009;24:263-271. [DOI] [PubMed] [Google Scholar]
- 24.Klem N-R, Kent P, Smith A, Dowsey M, Fary R, Schütze R, O'Sullivan P, Choong P, Bunzli S. Satisfaction after total knee replacement for osteoarthritis is usually high, but what are we measuring? A systematic review. Osteoarthritis and Cartilage Open; 2020:100032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lavernia CJ, Villa JM, Iacobelli DA. What is the role of mental health in primary total knee arthroplasty? Clin Orthop Relat Res. 2015;473:159-163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Law S, Daftary A, Mitnick CD, Dheda K, Menzies D. Disrupting a cycle of mistrust: A constructivist grounded theory study on patient-provider trust in TB care. Soc Sci Med. 2019;240:112578. [DOI] [PubMed] [Google Scholar]
- 27.Leopold SS. Editor's Spotlight/Take 5: Misconceptions and the Acceptance of Evidence-based Nonsurgical Interventions for Knee Osteoarthritis. A Qualitative Study. Clin Orthop Relat Res 2019;477:1970-1974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Levinger P, Bartlett JR, Bergman NR, McMahon S, Menz HB, Hill KD. The discrepancy between patient expectations and actual outcome reduces at the first 6 months following total knee replacement surgery. Knee Surg Sports Traumatol Arthrosc. 2019;27:2042-2050. [DOI] [PubMed] [Google Scholar]
- 29.Linder-Pelz S. Social psychological determinants of patient satisfaction: a test of five hypothesis. Soc Sci Med. 1982;16:583-589. [DOI] [PubMed] [Google Scholar]
- 30.Mahomed N, Gandhi R, Daltroy L, Katz JN. The self-administered patient satisfaction scale for primary hip and knee arthroplasty. Arthritis. 2011;2011:591253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mannion AF, Kampfen S, Munzinger U, Kramers-de Quervain I. The role of patient expectations in predicting outcome after total knee arthroplasty. Arthritis Res Ther. 2009;11:R139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Noble PC, Conditt MA, Cook KF, Mathis KB. The John Insall Award: Patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res. 2006;452:35-43. [DOI] [PubMed] [Google Scholar]
- 33.Ring D, Leopold SS. Editorial-Measuring Satisfaction: Can It Be Done? Clin Orthop Relat Res. 2015;473:3071-3703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Singh J, Dowsey M, Choong P. Patient Endorsement of the Outcome Measures in Rheumatology (OMERACT) Total Joint Replacement (TJR) clinical trial draft core domain set. BMC Musculoskeleta Disord. 2017;18:111. [DOI] [PMC free article] [PubMed] [Google Scholar]