Abstract
Cardiopulmonary resuscitation (CPR) is widely practised by healthcare professionals to revive heart beat and breathing in a patient suffering from cardiac/ respiratory arrest. It is increasingly being recognized that in some patients with specific medical conditions, CPR does not alter the overall outcome of illness, and is likely to increase suffering and further deteriorate the quality of life. Do Not Attempt Resuscitation (DNAR) as an option has been practised in many countries for such cases to avoid futile CPR and maintain dignity of the patient. The decision of DNAR should be taken by the treating physician who is well versed with the patient's medical condition, with information to the patient or her/his surrogate. While ordering DNAR on the patient's medical case record, every effort should be made to treat the underlying disease and continue optimal medical care with compassion. This policy document describes the principles for DNAR, offers an algorithm and format for its implementation, and guidance on frequently asked questions.
Background
Cardiopulmonary resuscitation (CPR) is an emergency procedure performed in an attempt to revive patients suffering from cardiac and/or respiratory arrest. It involves either or all of the following: repeated chest compression; mouth-to-mouth or artificial breathing usually with airway tube in the trachea; electric shock/s on the chest; and injectable drugs. In certain situations however, providing CPR is likely to increase the suffering of patients who have serious often terminal illness and without the prospect of a reasonable quality of life even if they are revived. Doctors and hospitals are regularly faced with the ethical dilemma of whether or not to perform CPR in such patients. Therefore, it is important to provide patients and their relatives adequate information on the disease or medical condition, poor chances of meaningful survival or worsened quality of life enable them to understand the likely benefit or potential harm of CPR in case it is required. Do not attempt resuscitation (DNAR) is an option that may be exercised by the treating physician in such a situation in the best interests of the patient. It would pave the way for arriving at an informed decision on 'DNAR' and its implementation. DNAR relates to CPR only and its limited value in certain situations and not to other forms of treatment. Whenever the treating physician is in doubt on whether to perform DNAR or not, CPR should be performed as the default option.
A core committee of experts from various disciplines was constituted to draft the guidelines, and several other experts were consulted. The guidelines were finalized through a national web based and in person consultative meeting with a wider representative audience.
Purpose
This document aims to guide treating physician(s) on their decision concerning 'DNAR'. It would help treating physician(s) and patient/surrogate(s) in preserving dignity in death and avoid prolonged suffering to the patient through non-beneficial CPR while continuing to provide other potentially curative and supportive care. Open communication and considered decision-making would enhance mutual trust and respect between the treating physician(s) and the patient/surrogate(s).
Scope
-
(i)
DNAR would apply to a patient with a progressive debilitating/incurable/terminal illness where CPR would be inappropriate, non-beneficial and likely to prolong the suffering of the patient in the best judgement of the treating physician(s). While applying this principle, compassionate care is integral to the overall goals of medical treatment.
-
(ii)
DNAR is distinct from withdrawal or withholding of other life-supporting treatments and advance directives which do not come under the purview of this document.
Instructions
The treating physician(s) should initiate discussions with the patient/surrogate and explain in detail about (i)the patient's disease and its prognosis, and (ii)the benefits and harms of CPR under the given medical circumstances in case the patient develops cardiac or respiratory arrest.
Procedure
-
(i)
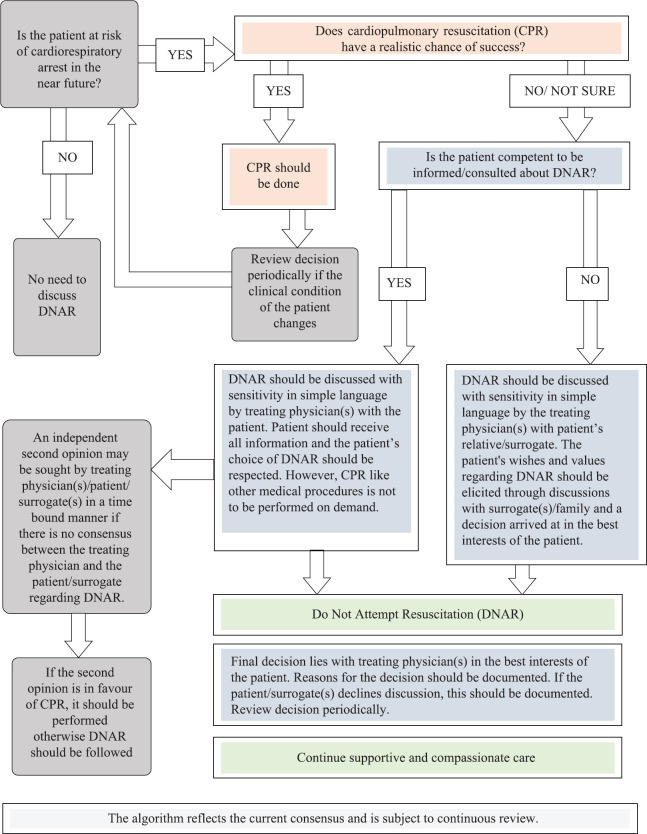
The document is intended to facilitate the process of decision-making on DNAR, which that is respectful of patient's autonomy and is in the best interests of the patient by the treating physician(s) on a case-to-case basis (Figure).
-
(ii)
There should be adequate opportunity, time and space to discuss with the patient and family in private and facilitate clear understanding of DNAR and its implications. Thus, it should be done in anticipation of an impending cardiorespiratory arrest, during the current hospitalization of the patient. This will allow better communication and understanding between the treating physician(s) and patient/surrogate(s)/caregiver.
-
(iii)
Teamwork and good communication are of crucial importance in decision-making and the delivery of care.
-
(iv)
Combined decision may be taken with the help of another physician, a psychologist or social worker or a counsellor or the hospital administrator, particularly in some settings, such as rural hospitals, where other types of personnel may not be available. This should be applicable in case the treating physician is unsure about the futility of CPR, or there is no consensus between the physician and the patient/surrogate. All such discussions must be noted in the patient's case records and the DNAR form.
-
(v)
While communicating, the treating physician(s) should explain that the patient would continue to be provided all treatments intended for potentially curable conditions or to reverse potentially reversible conditions and to provide supportive care. Moreover, DNAR does not mean withdrawal or withholding of other life-supporting treatments. The treating physician(s) should understand the social/cultural perspective of the patient.
-
(vi)
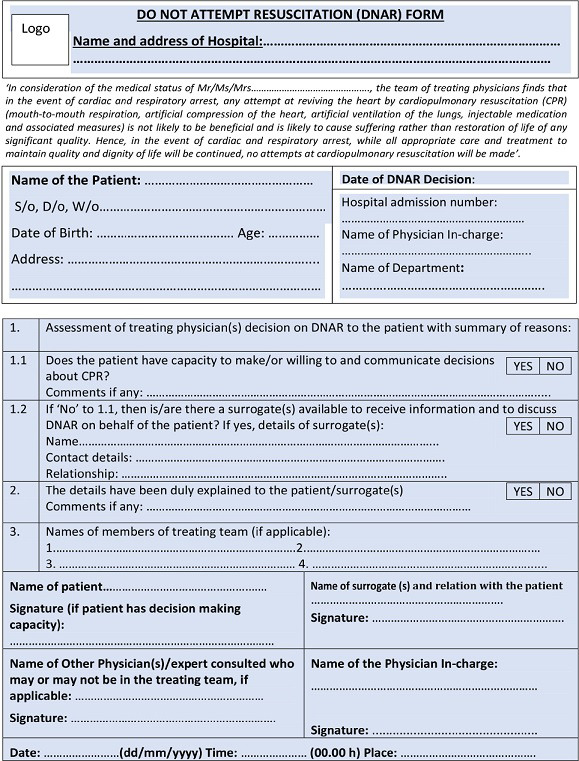
DNAR forms should be available in the language understood by the patient/surrogate(s) and should be signed, timed and dated by patient/surrogate(s) and the treating physician(s). In case the patient/surrogate(s) does/do not sign the DNAR form, the same should be recorded.
-
(vii)
Hospital administration should make efforts to sensitize their healthcare professionals on all issues related to DNAR.
Figure.
Algorithm for Do Not Attempt Resuscitation (DNAR) decision-making.
Decision and review of decisions on DNAR
-
(i)
Since CPR is a form of treatment to be provided by the treating physician the responsibility for the final decision regarding DNAR rests with the treating physician(s), which is taken in consultation with the patient/surrogate(s), empowered with the required information. Often the patient's relatives/surrogates may face an ethical dilemma to take the decision regarding DNAR. To provide them psychological support and help them overcome any feeling of guilt, the treating physician(s) should explain to them the futility of CPR and the harm it might cause to the patient.
-
(ii)
In case of conflict of opinion, an independent second opinion from a qualified medical practitioner belonging to the relevant specialty may be sought by the treating physician/patient/surrogate(s) in a timely manner.
-
(iii)
Any decision taken contrary to patient's expressed wishes should based on be robust criteria, accounted for and documented in the hospital records.
Storage of DNAR forms
-
(i)
The resuscitation plans and completed DNAR forms should be easily accessible to all the medical professionals to respond appropriately in the event of cardiorespiratory arrest of the patient concerned.
-
(ii)
It is recommended to attach a copy of the DNAR form to the patient's case records and to be integrated with the electronic health records, if available.
-
(iii)
All the case reports along with the DNAR forms should be archived for future reference.
Acknowledgment
Authors acknowledge all stakeholders who participated in the National Consultation Meeting or provided their comments during public consultation which helped in the finalization of this Consensus Guidelines.
Annexure I
Patient/Surrogate(s) Information Sheet on Do Not Attempt Resuscitation (DNAR)
(Copies of Annexure I & II to be provided to patient/surrogate(s) and also kept in hospital records)
This guidance is meant to help patients and their families to understand about cardiopulmonary resuscitation (CPR) and the decision regarding 'Do Not Attempt Resuscitation' (DNAR) if a patient's heart and/or breathing stops during treatment in the hospital setting.
What is CPR? CPR is an emergency medical procedure. It consists of one or all of the following: repeated chest compression; mouth-to-mouth and artificial breathing usually with airway tube in the windpipe (in the throat); electric shock/s on the chest; and injectable drugs. This is an emergency treatment that is initiated immediately by the physician. In most patients, this needs to be followed by intensive care unit (ICU) admission and artificial ventilation if the patient is not already in the ICU. This is because CPR does not change the reason why heart and/or breathing stopped and the main illness or condition still needs to be managed.
Are there problems with CPR in certain patients? CPR is most successful when it is done in time, in those with a reversible disease or in those with no accompanying incurable advanced chronic or acute disease(s). However, it may have serious side effects in other circumstances such as those with advanced chronic diseases or those with catastrophic or unresponsive disease(s). The most frequent potential harm is that the heart may restart, but the brain may be permanently damaged because it had no circulation for some period of time during the process of CPR. This often means that the patient becomes dependent and, in some cases, even vegetative. Most often, the patients' misery and suffering get prolonged when the primary illness or general health condition is incurable. In old and frail people, the procedure may itself may cause rib fractures and injury to the heart.
What is DNAR? It is a medical decision to not initiate or perform CPR on a patient suffering from an incurable disease/condition/terminal illness where medically meaningful survival is not expected.
When to take a decision about CPR and DNAR? Since CPR is an emergency medical procedure which needs to be done as quickly as possible, discussions on DNAR should ideally take place when the patient is in her/his full senses or if the patient is incompetent, i.e. not in a position to take such a decision, then with the family/surrogate(s) allowing reasonable time for them to understand before the physician takes the decision.
Does the decision on DNAR affect the ongoing treatment? Signing the DNAR Form would not deprive the patient of any ongoing treatment aimed at cure and other supportive medical and nursing care.
Annexure II
Annexure III
Frequently asked questions related to Do Not Attempt Resuscitation (DNAR)
-
Q.1.
Is Do Not Attempt Resuscitation (DNAR) same as an Advance Directives (Living Will)?
Ans: No, DNAR is distinct and is a physician-initiated decision, whereas advance directives or living will is a patient-initiated action.
-
Q.2.
When will a DNAR form be issued?
Ans: After the treating physician(s) assesses its need and appropriateness for a patient who is suffering with terminal condition and discusses it with the patient/surrogate(s).
-
Q.3.
What are the underlying conditions in which DNAR may be discussed?
Ans: The clinical triggers to initiate discussions regarding DNAR include (but may not be restricted to) the following:
-
(i)Where death is imminent (within a few hours or days),
-
(ii)Advanced, progressive, incurable conditions,
-
(iii)Existing conditions where sudden death may occur as an acute complication, and
-
(iv)Life-threatening acute conditions caused by sudden catastrophic events or persons in persistent vegetative state (PVS).
-
(i)
-
Q.4.
Can the DNAR form be used for a patient who is currently not diagnosed as 'terminal ill' or who is not currently in a state of permanent unconsciousness/vegetative state?
Ans: Yes, the treating physician(s) may make this assessment in view of the underlying disease and a likely cardiorespiratory arrest in the near future.
-
Q.5.
Can hospitals modify/customize the DNAR form as per their standard operating procedures?
Ans: Yes, but the essential principles described here should be followed.
-
Q.6.
Who is a surrogate?
Ans: A surrogate is a person or persons other than the healthcare providers who is/are accepted as the representatives of the patient's best interests, who will make decisions on behalf of the patient when the patient loses his/her capacity to make healthcare decisions. The surrogate of a patient can be the spouse, children, parents, siblings, a close friend or caregiver, a significant other as partner. A hierarchy of surrogates is not defined in the Indian Law.
-
Q.7.
What happens when the patient's wishes are not known and the patient has no surrogate?
Ans: In such a case, a Legally Authorized Representative (LAR) or caregiver or hospital administration authorities should be involved in the decision on DNAR.
-
Q.8.
What is the value of the communication in the DNAR process?
Ans: Good communication is the cornerstone and should have utmost priority for an empowered DNAR process. It should be done in a simplified and easy manner and in a language understood by the patient, giving enough time for discussion in privacy and with an option to seek second opinion if desired.
-
Q.9.
What happens if the patient is transferred to another hospital/ward?
Ans: DNAR decisions, though subject to review, are portable, i.e. if the patient is discharged after the decision, or shifted to another hospital, care facility, or ward, the decisions should be documented.
-
Q.10.
What should be done if the decision of DNAR is at odds with the wishes of the patient/surrogate(s)?
Ans: The doctor would make all efforts to explain and provide information. He/she should also provide the patient/ surrogate(s) an opportunity to take an independent second opinion before making the decision in the best interest of the patient. However, the final decision rests with the treating physician as in any other form of treatment.
-
Q.11.
Does DNAR ensure respect for human rights?
Ans: Yes, the patient's right to autonomy (Article 21) is the cornerstone in deciding about his/her cardiopulmonary resuscitation (CPR) status. Further, the patient's Right to Die with Dignity (Article 21) is upheld by this process. According to a recent judgement of the Supreme Court, the patient has the Right to Autonomy in opting for or refusing a medical intervention. (http://supremecourtofindia.nic.in/supremecourt/2005/9123/9123_2005_Judgement_09-Mar-2018.pdf). In addition, DNAR helps to empower patients towards their right to freedom from degrading treatment and ensuring respect for privacy and family life as per the Universal Declaration of Human Rights.
-
Q.12.
What happens when patients do not have the capacity to understand and get involved in this decision?
Ans: Discussions on DNAR should happen with a surrogate/LAR.
-
Q.13.
When should the DNAR discussion begin?
Ans: The decision on DNAR should not be taken in haste in an emergency situation. It should be discussed early while the patient is being treated in the hospital and not until death seems imminent.
-
Q.14.
What should hospitals do?
Ans: Hospitals can put policies in place to ensure that all physicians are made aware of the DNAR option and support its implementation. They can ensure adequate training of doctors and staff, improve the communications between doctors and patients, set up clinical ethics committees or multidisciplinary teams which can help guide the process and effective implementation, create educational videos, teaching material for better awareness of patients and integrate DNAR in the health records, and for review and feedback to maintain quality of care.
-
Q.15.
What are all the possible treatments that would continue while initiating DNAR?
Ans: All treatments aimed at cure and supportive care except CPR will continue. It should be noted that DNAR does not mean withdrawal or withholding of other life-supporting treatments. All compassionate care and pain relief measures will continue.
-
Q.16.
For which disease conditions should DNAR be considered?
Ans: There could be a range of disease conditions where a patient is suffering with terminal illness, incurable advanced diseases and advanced age with frailty to consider DNAR (e.g. debilitating chronic obstructive pulmonary disease, multi-organ failure, irreversible heart failure, advanced irreversible neurological disease, and advanced metastatic cancer).
Footnotes
This Policy Document is being published in the Indian Journal of Medical Research (Indian J Med Res 2020;151: 303-10) and simultaneously in the National Medical Journal of India (Natl Med J India 2020;32:e1-e8)
Disclaimer: These Consensus Guidelines are based on a review of currently available evidence and best practices. This dynamic document will undergo revisions and updation in the light of new knowledge, experience and guidelines from authorities on DNAR or public and clinicians perception and experience in the implementation of this guidance.
Conflicts of Interest: None.
References (for additional reading)
- 1.Indian Council of Medical Research. Definition of terms used in limitation of treatment and providing palliative care at the end of life. ICMR. 2018. [accessed on February 4, 2020]. Available from: http://www.ncdirindia.org/Download/EOLC.pdf . [DOI] [PMC free article] [PubMed]
- 2.Indian Council of Medical Research. National Ethical Guidelines for Biomedical and Health Research Involving Human Participants. ICMR. 2017. [accessed on February 4, 2020]. Available from: http://ethics.ncdirindia.org//asset/pdf/ICMR_National_Ethical_Guidelines.pdf .
- 3.Resuscitation Council (UK) Decisions relating to Cardiopulmonary Resuscitation (3rd edition - 1st revision) Guidance from the British Medical Association, the Resuscitation Council (UK), and the Royal College of Nursing. 2016 doi: 10.1136/jme.27.5.310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.DNACPR Form, Nottingham University Hospitals, National Health Service. [accessed on February 4, 2020]. Available from: http://dnar.co.uk/wp-content/uploads/2016/10/DNACPR-form-NUH-2014.pdf .
- 5.Etheridge Z, Gatland E. When and how to discuss “do not resuscitate” decisions with patients. BMJ. 2015;350:h2640. doi: 10.1136/bmj.h2640. [DOI] [PubMed] [Google Scholar]
- 6.Honourable Supreme Court Judgement on Advance Directives. “Writ Petition (Civil) No. 215 of 2005”. [accessed on February 4, 2020]. Available from: https://main.sci.gov.in/supremecourt/2005/9123/9123_2005_Judgement_09-Mar-2018.pdf .
- 7.Burns JP, Truog RD. The DNR order after 40 years. N Engl J Med. 2016;375:504–6. doi: 10.1056/NEJMp1605597. [DOI] [PubMed] [Google Scholar]
- 8.Salins NS, Pai SG, Vidyasagar M, Sobhana M. Ethics and medico legal aspects of “not for resuscitation”. Indian J Palliat Care. 2010;16:66–9. doi: 10.4103/0973-1075.68404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Adhikary SD, Raviraj R. Do not resuscitate orders. Indian J Med Ethics. 2006;3:100–1. doi: 10.20529/IJME.2006.039. [DOI] [PubMed] [Google Scholar]
- 10.Mani RK, Amin P, Chawla R, Divatia J, Kapadia F, Khilnani P, et al. Limiting life-prolonging interventions and providing palliative care towards the end-of-life in Indian intensive care units. Indian J Crit Care Med. 2005;2:96–107. [Google Scholar]
- 11.Mishra S, Mukhopadhyay K, Tiwari S, Bangal R, Yadav BS, Sachdeva A, et al. End-of-life care: Consensus statement by Indian Academy of Pediatrics. Indian Pediatr. 2017;54:851–9. doi: 10.1007/s13312-017-1149-4. [DOI] [PubMed] [Google Scholar]
- 12.DNR (Do Not Resuscitate) Guidelinesfor Medical ID Wearers. [accessedon February 4, 2020]. Available from: https://www.americanmedical-id.com/dnr .
- 13.The Scottish Government. Do Not Attempt CardiopulmonaryResuscitation (DNACPR) - Integrated Adult Policy: Guidance. The Scottish Government; May, 2010. [accessed on February 4, 2020]. Available from: https://www.gov.scot/publications/attempt-cardiopulmonary-resu scitation-dnacpr-integrated-adult-policy-decision-making-communication/pages/15/
- 14.Nakagawa Y, Inokuchi S, Kobayashi N, Ohkubo Y. Do not attempt resuscitation order in Japan. Acute Med Surg. 2017;4:286–92. doi: 10.1002/ams2.271. [DOI] [PMC free article] [PubMed] [Google Scholar]