Abstract
Background
Treatment of diaphyseal open tibia fractures often results in reoperation and impaired quality of life. Few studies, particularly in resource-limited settings, have described factors associated with outcomes after these fractures.
Questions/purposes
(1) Which patient demographic, perioperative, and treatment characteristics are associated with an increased risk of reoperation after treatment of open tibia fractures with intramedullary nailing or an external fixation device in Tanzania? (2) Which patient demographic, perioperative, and treatment characteristics are associated with worse 1-year quality of life after treatment of open tibia fractures with intramedullary nailing or an external fixation device in Tanzania?
Methods
A prospective study was completed in parallel to a similarly conducted RCT at a tertiary referral center in Tanzania that enrolled adult patients with diaphyseal open tibia fractures from December 2015 to March 2017. Patients were treated with either a statically locked intramedullary nail or external fixator and examined at 2 weeks, 6 weeks, 3 months, 6 months, and 1 year postoperatively. The primary outcome, reoperation, was any deep infection or nonunion treated with a secondary intervention. The secondary outcome was the 1-year EuroQol-5D (EQ-5D) index score. There were 394 patients screened and ultimately, 267 patients enrolled in the study (240 from the primary RCT and 27 followed for the purposes of this study). Of these, 90% (240 of 267) completed 1-year follow-up and were included in the final analysis. This group comprised 110 patients who underwent IMN and 130 who had external fixation; follow-up was similar between study groups. Patients were an average of 33 years old and were primarily males who sustained road traffic injuries resulting in AO/Orthopaedic Trauma Association (OTA) classification type A or B fractures. There were 51 reoperations. For the purposes of analysis, all patients were pooled to identify all other factors, in addition to treatment type, associated with increased risk of reoperation and 1-year quality of life. An exploratory bivariable analysis identifying various factors associated with reoperation risk and EQ-5D was subsequently included in a multivariate modeling procedure to control for confounding of effect on our primary outcome. Multivariable modeling was performed using standard hierarchical modeling simplification procedures with log-likelihood ratios. Alpha levels were set to 0.05.
Results
After controlling for potentially confounding variables such as gender, smoking status, mechanism of injury, and treatment type, the following factors were independently associated with reoperation: Time from hospital presentation to surgery more than 24 hours (odds ratio 7.7 [95% confidence interval 2.1 to 27.8; p = 0.002), AO/OTA fracture classification Type 42C fracture (OR 4.2 [95% CI 1.2 to 14.0]; p = 0.02), OTA-Open Fracture Classification muscle loss (OR 7.5 [95% CI 1.3 to 42.2]; p = 0.02), and varus coronal angle on an immediate postoperative AP radiograph (OR 4.8 [95% CI 1.2 to 14.0]; p = 0.002). After again controlling for confounding variables such as gender, smoking status, mechanism of injury, and treatment type factors independently associated with worse 1-year EQ-5D scores included: Wound length ≥ 10 cm (ß = [change in EQ-5D score] -0.081 [95% CI -0.139 to -0.023]; p = 0.006), OTA-Open Fracture Classification muscle loss (ß = -0.133 [95% CI -0.215 to -0.051]; p = 0.002), and OTA-Open Fracture Classification bone loss (ß = -0.111 [95% CI -0.208 to -0.013]; p = 0.03). We observed a modest, but independent association between reoperation and worse 1-year EQ-5D scores (ß = -0.113 [95% CI -0.150 to -0.077]; p < 0.001).
Conclusions
We found two potentially modifiable factors associated with the risk of reoperation: reducing time to surgical treatment and avoiding varus coronal angulation during definitive stabilization. Hospitals may be able to minimize time to surgery, and thus, reoperation, by increasing the number of available operative personnel and space and emphasizing the importance of open tibia fractures as an injury requiring emergent orthopaedic management. Given the lack of fluoroscopy in the study setting and similar settings, surgeons should emphasize appropriate fracture alignment, even into slight valgus, to avoid varus angulation and subsequent reoperation risk.
Level of Evidence
Level II, therapeutic study.
Introduction
Musculoskeletal trauma represents an increasingly large amount of the morbidity in low- and middle-income countries (LMICs) [16, 31]. Appropriate, timely, and affordable care is difficult and, at times, impossible for patients to obtain in low-resource settings due to multiple factors including too few surgeons, under-developed trauma systems, economic hardship, and overall limitations in hospital resources [8, 29, 49]. Moreover, LMICs have recently experienced an increase in gross domestic product (GDP) and individual wealth with a corresponding increase in automobile use. For example, from 2003 to 2018, Tanzania has seen a rise in GDP per capita from USD 583 to USD 957 (as measured by constant USD) [50], and we assume that road traffic injuries resulting in musculoskeletal trauma, particularly open tibia fractures, will occur with increasing frequency [23, 24, 51, 53]. The frequency of these injuries is driving a surgical burden of disease that many LMICs are not currently equipped to address given their relative lack of medical infrastructure when compared with high-income countries (HICs) [3, 24, 29, 49]. Although the treatment of traumatic orthopaedic injuries is relatively standard in HICs, less is known about their treatment in LMICs.
Open tibia fractures are orthopaedic emergencies needing rapid antibiotic administration, thorough irrigation and débridement, and frequently, definitive fixation with intramedullary nailing [4, 5, 14, 20]. However, there is little evidence in the existing literature as to whether or not the standard of care in HICs regarding fixation strategy applies to patients in LMICs given their local resources and constraints. To address the question of fixation strategy, a randomized clinical trial (RCT) was recently completed in Tanzania examining the treatment of primarily closeable open tibia shaft fractures with either SIGN intramedullary nailing (IMN) or uniplanar external fixators to determine the effect on the primary outcome, reoperation [17]. This study demonstrated that IMN did not increase complication rates in the treatment of primarily closable open tibia shaft fractures and reduced malalignment risk while having sustained improvement in radiographic healing. However, the study did not definitively determine that nailing is superior to external fixation in the study setting, and furthermore, it did not detail all other important and potentially modifiable patient and treatment factors associated with reoperation and poor 1-year quality of life (QoL). The current study, as a follow-up to the RCT, thus fills a known gap in the literature in LMICs concerning open tibia fractures [2, 18, 26] and builds upon the results of that study by evaluating the association of treatment delays with reoperations in LMICs. We explore the association of all other patient, injury, and treatment characteristics with reoperation risk and poor 1-year QoL in a prospective study of patients with open, diaphyseal tibia fractures treated with either IMN or external fixation at a tertiary orthopaedic hospital in Tanzania.
We sought to answer: (1) Which patient demographic, perioperative, and treatment characteristics are associated with an increased risk of reoperation after treatment of open tibia shaft fractures with intramedullary nailing or an external fixation device in Tanzania? (2) Which patient demographic, perioperative, and treatment characteristics are associated with worse 1-year quality of life after treatment of open tibia shaft fractures with intramedullary nailing or an external fixation device in Tanzania?
Patients and Methods
Study Setting and Study Groups
We completed a prospective study of skeletally mature patients with diaphyseal open tibia fractures (AO/Orthopaedic Trauma Association [OTA] Type 42) [28] who had been screened for enrollment in a separate parent-study, RCT comparing IMN with external fixation at a Tanzanian hospital. Tanzania has a population of approximately 58 million people with half of the population being aged 15-54 years, a life expectancy of 64 years, and about 1/3 living in urban centers [9]. The specific objectives and methodology of that RCT have been reported separately [17]. Patients were screened for inclusion during the enrollment period from December 17, 2015 to March 25, 2017. Patients were included in the current study if they were skeletally mature and had an AO/OTA Type 42 open tibia shaft fracture without extension into the proximal or distal bony metaphysis or had articular involvement. Patients were excluded if they had an ipsilateral femur fracture, contralateral femur or tibia fracture, pathologic fracture, prior lower-limb deformity, severe traumatic brain injury (Glasgow-Coma score < 12), spinal cord injury, severe burns (> 10% of the total body surface area or > 5% of the total body surface area with a full-thickness or circumferential injury), or inability to complete follow-up. All patients eligible for the parent RCT were included in the current prospective study. A subset of patients who were excluded from the parent RCT were followed prospectively, which included patients presenting more than 24 hours after injury and patients with wounds that could not be closed primarily (Gustilo-Anderson Classification Type IIIB) (Fig. 1). The study was approved by the institutional review boards (IRBs) of the University of California, San Francisco and the Tanzanian National Institute for Medical Research. All data were collected prospectively and the current study question regarding the association of demographic and perioperative variables with reoperation and health-related quality of life (EQ-5D) was developed in the initial study IRB application and protocol.
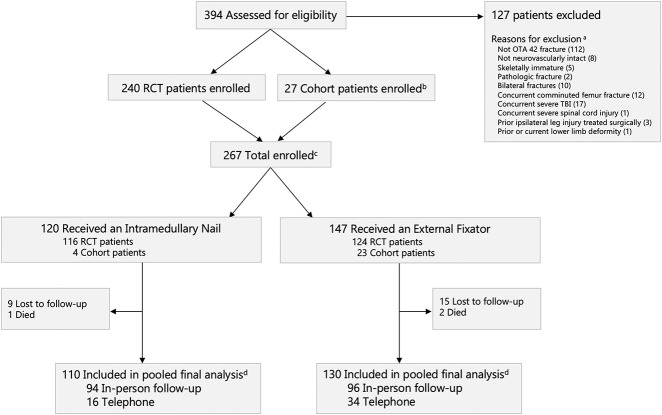
Fig. 1.
This CONSORT diagram demonstrates patient screening and enrollment, treatment cohort, and patients included in the final analysis. aSeveral patients had more than one reason for exclusion from the study. bPatients followed prospectively for the purposes of the cohort study were not included as part of the randomization module. Their treatment was left up to the discretion of the treating surgeon. cFollowing exclusion of 127 patients, those enrolled in the study consisted of 267 total patients with 240 from the RCT group and 27 from the cohort group dThis was an as-treated analysis of those patients completing 1-year follow-up in-person or by telephone. Follow-up was not different between RCT and cohort patients. All patients were part of a pooled analysis for the purposes of this study; OTA = Orthopaedic Trauma Association; TBI = traumatic brain injury; RCT = randomized controlled trials.
Surgical Treatment and Aftercare
All patients received prophylactic intravenous ceftriaxone as soon as possible after presentation and were taken to the operating room for irrigation and débridement with bony stabilization. Patients included in the RCT were allocated to receive either IMN or uniplanar external fixator according to a web-based electronic randomization tool, REDCap (Research Electronic Data Capture, Nashville, TN, USA) [19], with blocks randomly permuted in sizes of 4, 6, or 8. Patients excluded from the RCT but included in the current study were treated at the discretion of the treating surgeon using the same implants. Patients receiving IMN were treated using a statically locked Surgical Implant Generation Network (SIGN) standard nail (SIGN Fracture Care International, Richland, WA, USA) with light hand-reaming. The number of interlocking screws was determined at the discretion of the treating surgeon. Patients receiving external fixation were treated using the uniplanar AO Dispofix, (Dispofix Indústria e Comério, São Paulo, Brazil) consisting of a single aluminum bar with two Schanz pins (5 mm or 6 mm, DePuy Synthes, West Chester, PA, USA) placed in the proximal and distal segments. Intraoperative fluoroscopy was not used in any procedures.
Demographic, injury, treatment, and perioperative characteristics were recorded at the initial enrollment. Fracture characteristics were recorded according to the AO/OTA fracture classification (Type A: simple; Type B: wedge; Type C: multifragmentary) [28]. We also characterized injuries according to the OTA open fracture classification, in which wounds are evaluated according to skin approximation, muscle damage, arterial disruption, wound contamination, and bone loss [33]. Study coordinators recorded perioperative data including the timeliness of hospital arrival, antibiotic administration, and surgery. Time from hospital arrival to surgery was the time from presentation at the hospital to the first débridement in the operating room. The time from hospital arrival to antibiotics was the time from presentation to antibiotic administration at the hospital where the patient received definitive treatment. Additional intraoperative antibiotic use was evaluated according to whether or not a surgeon believed additional antibiotic coverage was required in the operating theater based on assessment of wound contamination. Regarding treatment characteristics, reduction quality was determined by two fellowship-trained orthopaedic trauma surgeons (DS, SM) who evaluated all radiographs in duplicate for coronal and sagittal alignment using goniometry.
Primary and Secondary Study Outcomes
The primary outcome was reoperation for infection or nonunion as determined by an adjudication committee composed of two fellowship-trained orthopaedic trauma surgeons (DS, SM). Because many patients for whom reoperation was recommended did not actually undergo reoperation, most frequently because of financial barriers, the following criteria for a primary event due to infection were applied: reoperation due to infection, exposed bone at any timepoint, and any wound drainage occurring after the 3-month appointment. A primary event due to nonunion was defined as reoperation to promote bone healing or a modified Radiographic Union Scale for Tibia fracturs (mRUST) of less than or equal to 10 at or after the 6-month follow-up visit, when surgery was recommended to treat infection or nonunion [27]. The secondary outcome was the EuroQoL-5 Dimensions (EQ-5D) (Swahili version) index score at 1-year postoperatively. Data were collected by locally trained research coordinators using REDCap. In-clinic follow-up visits were scheduled at 2 weeks, 6 weeks, 3 months, 6 months, and 12 months postoperatively. For patients unable to attend follow-up visits, study coordinators used a telephone follow-up protocol by which they could obtain the primary study outcome, reoperation, and secondary outcome, EQ-5D. Data quality responsibilities were performed by the methods center, with review by the adjudication committee every 6 months. Data quality responsibilities including regular database audits for missingness of data were carried out and communicated with the local site investigators and research coordinators.
Study Population
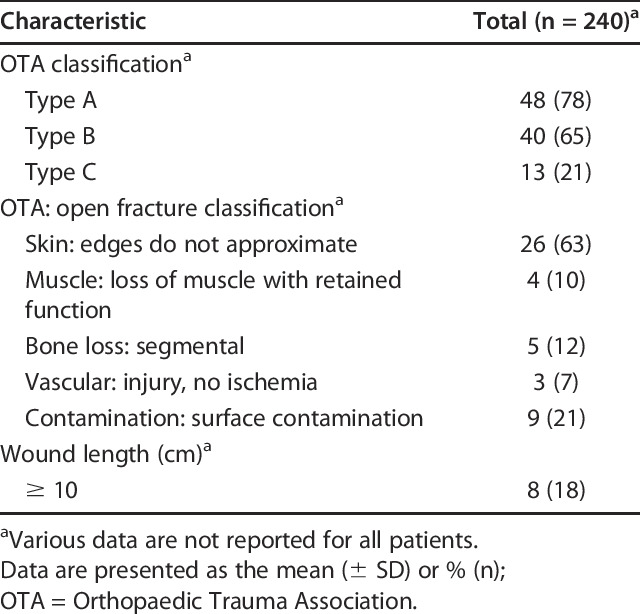
There were 394 open tibia fractures treated during the study period; 32% (127 of 394) were excluded based on the clinical criteria. In all, 90% (240 of 267) of patients completed 1-year follow-up and were included in the final pooled analysis. Of the final study population, 91% (218 of 240) included patients from the RCT; three patients died before completing 1-year follow-up. Nine percent (22 of 240) of the final study population was comprised of patients who were initially excluded from the RCT, primarily due to treatment delay, and who were followed for the purposes of the current study because one of the primary goals of this follow-up study was to identify the effect of treatment delay on reoperation. There was no differential follow-up between the RCT and the prospectively followed cohort patients as identified by a Fisher’s exact test with an alpha set to 0.05 (1-year follow-up rates: RCT 91% [218 of 240]; cohort 81% [22 of 27]). The study primarily consisted of young, healthy men who sustained open tibia fractures because of road traffic injuries (Table 1). Patients were definitively treated with external fixation more often than with IMN (54% [130 of 240] and 46% [110 of 240], respectively). Most fractures were AO/OTA Type A or B fractures (48% and 40%, respectively) (Table 2). A reoperation occurred in 21% (51 of 240) of all patients; there was a lower proportion of reoperations in the IMN group (17% [19 of 110]) than in the external fixation group (25% [32 of 130]; relative risk [RR], 0.7 [95% CI 0.4 to 1.2]; p = 0.17). Deep surgical-site infection (53% [27 of 51]), aseptic nonunion (29% [15 of 51]), and infected nonunion (14% [7 of 51]) were the most frequent causes of reoperation.
Table 1.
Patient and treatment characteristics
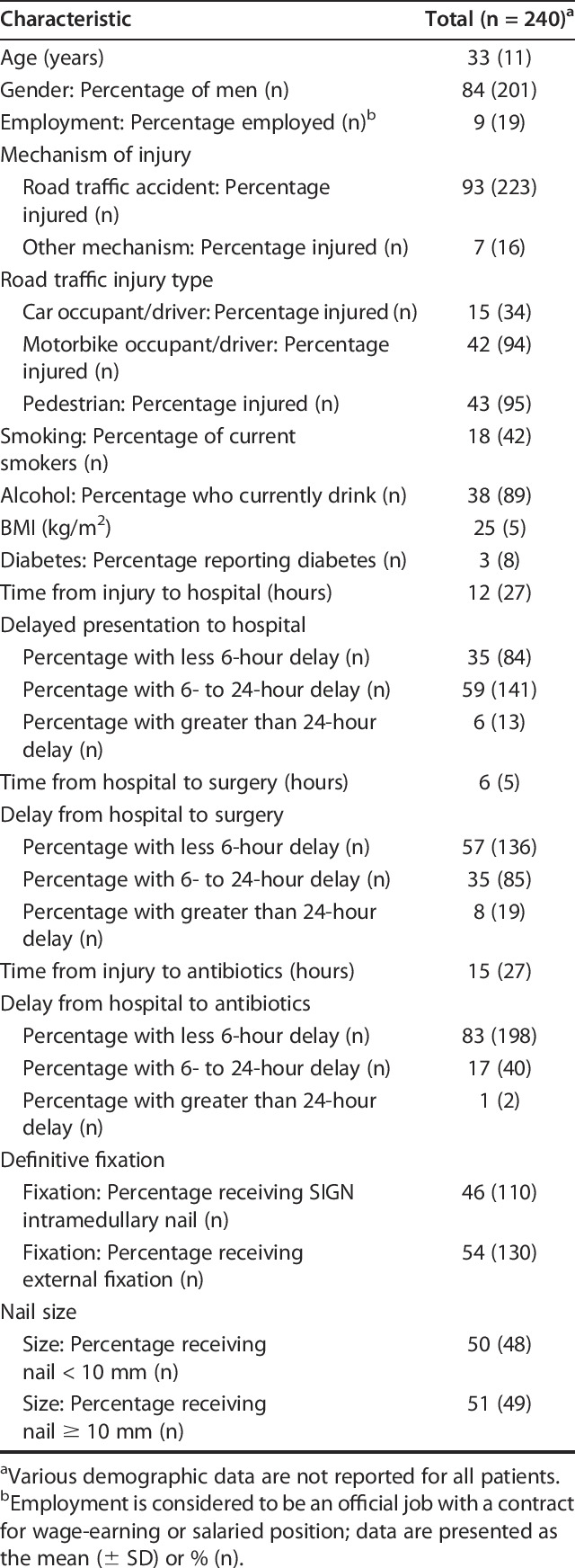
Table 2.
Fracture characteristics
Statistical Analysis
All patients completing 1-year follow-up were included in the final, pooled, analysis. Although patients were allocated into two treatment groups, the primary goal of the current study was to explore the association of all other patient, injury, and treatment characteristics with risk of reoperation and poor 1-year QoL in a group of patients with open, diaphyseal tibia fractures. To complete this analysis, the two patient treatment groups were pooled to evaluate all other variables among the entire study cohort. The association of treatment type on the risk of reoperation and EQ-5D is explored in the now-published RCT [17]. An exploratory bivariate analysis was performed using the Fisher’s exact test for categorical variables and the Wilcoxon rank-sum test for continuous variables. Since the primary aim of the study was to determine all other variables, in addition to treatment type, associated with reoperation and poorer 1-year EQ-5D, multivariate models assessing variable association with the outcomes, reoperation, and EQ-5D were built based on those variables associated with the outcomes on bivariate analysis. We used a conservative approach to hierarchical modeling in which those variables associated with the outcomes on bivariate analysis (p values < 0.2) were included in the initial model. All variables were included as part of the exploratory analysis. Subsequent model simplification methodology using likelihood ratio testing between nested models and Hosmer-Lemeshow chi-square goodness of fit test was used to specify the model. Treatment type was included as part of the initial model for reoperation but was found to be colinear with other variables included in the model. Multivariate modeling found that all significant variables associated with reoperation remained significant when treatment type was included in the model. However, per multivariate model simplification procedures, treatment type was ultimately excluded as the model was better specified without inclusion of treatment type. A multivariate linear regression model for the secondary outcome, EQ-5D score, was similarly constructed and assessed for model fit. Those variables advancing to the multivariate modeling procedure for association with reoperation included mechanism of injury, motorbike injury, smoking status, time from injury to hospital, time from hospital to surgical treatment, time from injury to antibiotics, treatment type, nail size, varus coronal angulation, OTA fracture classification, and wound length. Those variables advancing to the multivariate modeling procedure for association with EQ-5D included treatment type, wound length, presence/absence of OTA open-fracture classification variables, reoperation, gender, diabetes status, alcohol status, insurance status, employment, mechanism of injury, and delay to surgery. Reoperation was ultimately excluded from the multivariate model for EQ-5D as it is also a primary outcome of this study. Post-hoc sensitivity analyses were performed to evaluate outcome sensitivity to the lack of data using multiple imputation with chained equations [37]. Sensitivity analyses of both primary reoperation and EQ-5D yielded similar results for multiply imputed data. Data were analyzed in STATA (SE version 15.0; StataCorp LP, College Station, TX, USA) with significance set at a two-tailed alpha of 0.05.
Results
Association of Patient Demographic, Perioperative, and Treatment Characteristics with Reoperation after Treatment of an Open Tibia Shaft Fracture
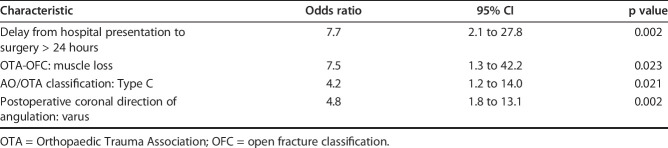
After controlling for potentially confounding variables such as gender, smoking status, mechanism of injury, and treatment type, we found several factors that were independently associated with reoperation. Patients experiencing delays from hospital to surgical treatment greater than 24 hours (odds ratio 7.7 [95% CI 2.1 to 27.8]; p = 0.002), suffering muscle loss (OR 7.5 [95% CI 1.3 to 42.2]; p = 0.02), presenting with AO/OTA fracture classification type C fractures (OR 4.2 [95% CI 1.2 to 14.0]; p = 0.02), and having postoperative coronal varus angulation (OR 4.8 [95% CI 1.8 to 13.1]; p = 0.002) were more likely to experience a reoperation after treatment of an open tibia shaft fracture (Table 3).
Table 3.
Logistic regression model for predictors of reoperation after tibial shaft fractures
Association of Patient Demographic, Perioperative, and Treatment Characteristics with One-year EQ-5D after Treatment of an Open Tibia Shaft Fracture
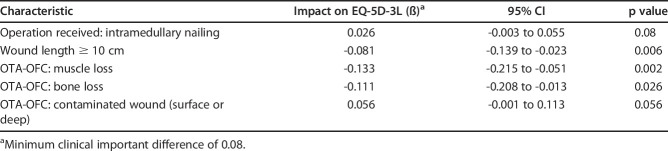
After controlling for potentially confounding variables such as treatment type, wound length, gender, alcohol status, insurance status, mechanism of injury, and delay to surgery, we found several factors that were independently associated with 1-year EQ-5D where a minimum clinically meaningful difference in EQ-5D was determined to be 0.08 [11]. Patients having a wound length greater than 10 cm (ß [change in EQ-5D score] -0.081 [95% CI -0.139 to -0.023]; p = 0.006), experiencing extensive muscle loss (ß -0.133 [95% CI -0.215 to -0.051]; p = 0.002), or bone loss (ß -0.111 [95% CI -0.208 to -0.013]; p = 0.03) had reduced 1-year EQ-5D scores (Table 4). Reoperation, while not included in the multivariate model for EQ-5D, was independently associated with poor 1-year EQ-5D scores (ß = -0.113; 95% CI, -0.150 to -0.077; p < 0.001).
Table 4.
Linear regression model for predictors of 1-year EQ-5D-3L after tibial shaft fractures
Discussion
Musculoskeletal trauma, particularly open tibia fractures, causes a disproportionately high surgical burden of disease in LMICs [24, 31,53]. Although there is a consensus in HICs regarding the management of open tibia shaft fractures [4, 5, 14, 20], the treatment of these injuries and factors predisposing patients to their complications are less well understood in austere environments. A recently published RCT examined the question as to how the definitive fixation method of these injuries affects reoperation and QoL [17]. However, that study did not address other modifiable patient and treatment factors associated with reoperation after the treatment of these injuries in a low-resource study setting. In particular, the RCT did not address the association of treatment delays with the proportion of reoperations. This study differs from the previously published RCT both in methodologic considerations as well as in the reporting of its outcomes. It builds on the results of the RCT and reports critical findings pertinent to surgeons in the study setting. We prospectively evaluated all patient demographic, perioperative, and treatment characteristics associated with reoperation and 1-year EQ-5D (QoL) in a group of patients with open tibia shaft fractures in Tanzania. We found that delays from hospital arrival to surgery greater than 24 hours and postoperative coronal varus angulation were associated with increased reoperation rates. Furthermore, wounds greater than 10 cm in length, muscle loss, and bone loss were associated with lower 1-year EQ-5D scores. Finally, reoperation was independently associated with a worse 1-year EQ-5D.
This investigation has several limitations. The first dealing primarily with the patient population of the study. As a follow-up study to the recently completed RCT, patient data (those patients included in the RCT) was used twice for the purposes of this study. Although potentially problematic for the purposes of a systematic review or meta-analysis, there is much precedent in the orthopaedic evidence for completing this type of follow-up study (such as the, SPRINT, FAITH, and FLOW trials) [5, 12, 38, 42, 44]. We pooled the two patient populations; those individuals receiving IMN and those receiving external fixation, which might introduce a selection bias in treatment. However, as mentioned, the goal of this study was to evaluate all variables among the study cohort that would be associated with reoperation and 1-year QoL. To complete this type of analysis, the patient population must be viewed as a whole with treatment type being one of many variables examined in bivariate and multivariate analyses. The reader should keep the two treatment types in mind as they evaluate those factors associated with reoperation and 1-year QoL but refer to the primary RCT to evaluate the specific effect of treatment on the primary outcome, reoperation. Furthermore, it was critical to pool the RCT patients with the non-RCT patients to evaluate the effect of treatment delays on our primary outcomes. As mentioned previously, the RCT excluded those patients who presented more than 24 hours after injury.
The analysis has limitations inherent to a multivariate, regression modeling analysis. One of the purposes of such a methodology is to control for important and confounding differences among the patient population. The iterative, hierarchical, modeling procedure we outline in our methodology is one of many standard protocols that is considered sufficient for controlling for these differences among the study population, but nonetheless, the introduction of new data or variables would likely mean that the model may not provide adequate fit. For this reason, the model is limited by the potential for unknown and unmeasured covariates that could not be controlled for in the analysis. Data that were not collected for this study or were of poor quality would include, but are not limited to, amount of alcohol consumed, NSAID use, comorbidities, robust socioeconomic data, irrigation pressure or solutions, and HIV status. The results of this study should thus be interpreted in light of the absence of these covariates, and the results of this analysis would be limited to solely those variables and data collected as part of the original RCT. The HIV status of our patients was also different from that of the Tanzanian general population (5.1% national prevalence among those aged 15 to 64 years) [46]. We relied on self-reporting rather than mandatory HIV screening, and HIV rates may have been underreported, preventing us from evaluating its association with reoperation and QoL. It is well reported in the literature that HIV is associated with increased infection risk in open fractures, overall mortality, and loss to follow-up proportions [1, 15, 48, 53]. Due to the likely underreported HIV status, some patients experiencing reoperation due to infection may have had concomitant HIV infections that increased their baseline reoperation risk and thus acted as a potentially confounding variable. A more rigorous methodology for identifying HIV status may be useful in future studies, but this must be balanced with concerns for patient privacy, social stigma, and potential barriers to study recruitment. Furthermore, the primary event, reoperation, was indicated by the adjudication committee regardless of whether the patient received a reoperation. Some patients who had an infection did not receive reoperation or deep-tissue culture. Tissue culture was not routinely available at our study location because of local resource constraints, and we relied on alternative criteria for diagnosing infection. Ultimately, several patients did not receive a reoperation because of financial hardship or failure to return for surgery. This study had patients who were lost to follow-up along with missing data. The use of telephone follow-up in this study does have limitations in obtaining completely adequate and reliable 1-year follow-up data. However, we consider the additional sample size and higher follow-up rate one of the study’s methodological strengths rather than a weakness in a setting where it is difficult to obtain adequate in-clinic follow-up rates. Also, sensitivity analyses demonstrated consistent findings, and given the local environment, our follow-up proportion (90%) is likely above average. Furthermore, we used multiple imputation with chained equations analysis to assess the sensitivity of our results to the missingness of the data. After this sensitivity analysis, our primary study findings were unchanged. Lastly, given that the study took place in only one Sub-Saharan African country, there is a lack of generalizability to other LMICs and HICs. The results of the study should be interpreted in this context. Recognizing that although some LMICs share common resource limitations, there is not a one-size-fits-all solution to ameliorating these resource disparities, and our findings, particularly delay to surgical care, may require different solutions in different settings.
Patient Demographic, Perioperative, and Treatment Characteristics Influencing Rates of Reoperations
We found several common, worse injuries, and unique characteristics, delays to surgery and coronal varus angulation, associated with a higher risk of reoperation in this selected population. Regarding delays to surgical intervention after hospital arrival, we found that a delay longer than 24 hours was associated with an increased reoperation risk. This finding compares favorably with the only other study, to our knowledge, to have evaluated risk factors for complications after open tibia fracture treatment with IMN in LMICs [47]. That study used the SIGN nail database and found that increased infection rates after IMN of open tibia shaft fractures in LMICs was associated with delayed mean time from injury to surgery, from injury to wound closure, and severe soft tissue injury. Our finding builds on the evidence of that study and is particularly important in LMICs where treatment delays are common and in HICs where there has been less emphasis on the timeliness of surgery [35, 45]. In HICs, there has been a shift away from performing the initial wound débridement within 6 hours [36, 39, 40]. However, these studies were completed in ideal resource-rich environments. Other studies in LMICs have similarly noted, as we identified in our study, that surgeons should quickly consider the wound’s severity and fracture grade when determining the urgency of wound débridement [22, 32]. Our findings indicate that although urgent débridement may not be necessary in the treatment of open tibia fractures, at some point, and in our case, after 24 hours, delaying débridement may result in increased adverse patient outcomes. This has potential implications for surgical capacity-building initiatives and decision-making in LMICs where patients may have delayed fracture management. These delays are an opportunity to relieve the surgical burden and improve patient outcomes by minimizing treatment delay. Regarding postoperative varus coronal angulation, to our knowledge, this has not been specifically studied as a distinct risk factor for reoperation in open tibia fractures. However, cortical discontinuity is a well-established risk factor for nonunion and reoperation in tibial fractures, and varus angulation may lead to decreased cortical continuity [6, 13]. Additionally, varus alignment may place greater stress on the bone-implant interface. Varus coronal malalignment has been identified as a risk factor for complications and reoperations in other long-bone fractures and has been linked to osteoarthritis in patients with tibial-shaft fractures [10, 30]. Our findings add to the existing evidence, and more importantly, provide evidence for emphasizing appropriate fracture reduction and alignment particularly in settings where fluoroscopy access is limited and the use of the SIGN IMN is prevalent. By overcorrecting deformities, even into slight valgus, surgeons in the study setting and similar settings with limited fluoroscopy may be able to reduce the increased reoperation risk associated with varus deformity in open tibia fractures.
Patient Demographic, Perioperative, and Treatment Characteristics Resulting in Worse 1-year Quality of Life as Measured by EQ-5D
We also found that patients who presented with severe injuries involving bone loss, muscle loss, or having a wound length greater than 10 cm, or who experienced reoperation in the course of care, were more likely to experience poorer QoL after injury and treatment. With respect to QoL, several studies have been conducted to assess risk factors for negative outcomes after long-bone fractures [7, 21, 25, 41, 43, 52]. Most relevant to the current study, a large analysis of open fractures found that lower-extremity fractures, smoking, and open surgical wounds were associated with lower 1-year QoL [43]. The primary finding in our study, that higher severity injuries result in worse 1-year QoL, is consistent with their findings but remain useful in the current study setting. Our finding emphasizes the importance of recognizing the severity of these injuries as orthopaedic emergencies requiring skilled and diligent management to ensure successful long-term patient outcomes regardless of study setting. Additionally, avoiding reoperations, particularly those made necessary by nonunion, may improve QoL. Nonunion, a frequent cause of reoperation, results in worse QoL than congestive heart failure or end-stage hip arthroses [7], and the EQ-5D scores for patients undergoing a reoperation was similar to that of patients living with various cancers [34].
Conclusions
We identified two potentially modifiable factors, delays to surgical treatment and postoperative coronal varus angulation, that are associated with increased reoperation risk after treatment of open tibia shaft fractures with intramedullary nailing or external fixation at a tertiary care center in Tanzania. Furthermore, we identified that higher severity injuries including extended wound length, bone loss, and muscle loss result in poorer 1-year quality of life in patients with these injuries. These findings are particularly relevant in the study setting where treatment delays are common. Furthermore, there is seldom availability of intraoperative fluoroscopy in Tanzania, and it can be difficult to avoid malalignment during definitive fracture fixation. By emphasizing the importance of scaling up fluoroscopy access and even over-correction into slight valgus, it may be possible to ameliorate some of the risk associated with reoperation after open tibia fracture fixation. Future studies should seek to elaborate on how to address setting-specific barriers to timely surgical care such as advancing the number of trained, available operative personnel, the operative space at a given institution, and the scaling of access to and maintenance of fluoroscopic operative technology. These studies should emphasize economic analyses, particularly cost-benefit analyses, to allow policy makers to appreciate the economic and social value of reducing these barriers to orthopaedic care as a means of decreasing open tibia fracture burden.
Acknowledgments
We thank the study research coordinators, Ibrahim Sasillo, Justin Kessy, Joshua Ngayoma, for their tireless work and contributions to this study.
Footnotes
The institution of one or more of the authors (DS, SM) has received, during the study period, funding from the Wyss Foundation and Doris Duke Charitable Foundation. One author (DS) is a member of the board of directors of SIGN Fracture Care International, Richland, WA, USA, a non-profit company based in the United States that manufactures and donates the intramedullary nail used in this study; the author (DS) certifies that he receives no salary, royalties, or other payment of any kind from SIGN. Each other author certifies that he has no commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at the University of California, San Francisco, San Francisco, CA, USA and the Muhimbili Orthopaedic Institute, Dar es Salaam, Tanzania.
References
- 1.Aird J, Noor S, Lavy C, Rollinson P. The effect of HIV on early wound healing in open fractures treated with internal and external fixation. J Bone Joint Surg Br. 2011;93:678-683. [DOI] [PubMed] [Google Scholar]
- 2.Aluede EE, Phillips J, Bleyer J, Jergesen HE, Coughlin R. Representation of developing countries in orthopaedic journals: a survey of four influential orthopaedic journals. Clin Orthop Relat Res. 2012;470:2313-2318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bach O. Musculoskeletal trauma in an East African public hospital. Injury. 2004;35:401-406. [DOI] [PubMed] [Google Scholar]
- 4.Bhandari M, Guyatt GH, Swiontkowski MF, Schemitsch EH. Treatment of open fractures of the shaft of the tibia. J Bone Joint Surg Br . 2001;83:62-68. [DOI] [PubMed] [Google Scholar]
- 5.Bhandari M, Guyatt G, Tornetta P, III, Schemitsch E, Swiontkowski M, Sanders D, Walter S. Randomized Trial of Reamed and Unreamed Intramedullary Nailing of Tibial Shaft Fractures: By the Study to Prospectively Evaluate Reamed Intramedullary Nails in Patients with Tibial Fractures (SPRINT) Investigators*. J Bone Joint Surg Am. 2008;90:2567-2578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bhandari M, Tornetta P, Sprague S, Najibi S, Petrisor B, Griffith L, Guyatt GH. Predictors of reoperation following operative management of fractures of the tibial shaft. J Orthop Trauma . 2003;17:353-361. [DOI] [PubMed] [Google Scholar]
- 7.Brinker MR, Hanus BD, Sen M, O’Connor DP. The devastating effects of tibial nonunion on health-related quality of life. J Bone Joint Surg Am. 2013;95:2170-2176. [DOI] [PubMed] [Google Scholar]
- 8.Callese TE, Richards CT, Shaw P, Schuetz SJ, Paladino L, Issa N, Swaroop M. Trauma system development in low- and middle-income countries: a review. J Surg Res. 2015;193:300-307. [DOI] [PubMed] [Google Scholar]
- 9.Central Intelligence Agency. Africa: Tanzania — The World Factbook - https://www.cia.gov/library/publications/the-world-factbook/geos/print_tz.html. Accessed March 5, 2020.
- 10.Chandrappa MH, Hajibandeh S, Hajibandeh S. Postoperative outcomes of initial varus versus initial valgus proximal humerus fracture: A systematic review and meta-analysis. J Clin Orthop Trauma. 2017;8:14-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dolan P. Modeling valuations for EuroQol health states. Med Care. 1997;35:1095-1108. [DOI] [PubMed] [Google Scholar]
- 12.Fixation using Alternative Implants for the Treatment of Hip fractures (FAITH) Investigators. Fracture fixation in the operative management of hip fractures (FAITH): an international, multicentre, randomised controlled trial. Lancet. 2017;389:1519-1527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fong K, Truong V, Foote CJ, Petrisor B, Williams D, Ristevski B, Sprague S, Bhandari M. Predictors of nonunion and reoperation in patients with fractures of the tibia: an observational study. BMC Musculoskelet Disord. 2013;14:103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fu Q, Zhu L, Lu J, Ma J, Chen A. External Fixation versus Unreamed Tibial Intramedullary Nailing for Open Tibial Fractures: A Meta-analysis of Randomized Controlled Trials. Sci Rep . 2018;8:12753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Geng EH, Bangsberg DR, Musinguzi N, Emenyonu N, Bwana MB, Yiannoutsos CT, Glidden DV, Deeks SG, Martin JN. Understanding reasons for and outcomes of patients lost to follow-up in antiretroviral therapy programs in Africa through a sampling-based approach. J Acquir Immune Defic Syndr. 2010;53:405-411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gosselin RA, Spiegel DA, Coughlin R, Zirkle LG. Injuries: the neglected burden in developing countries. Bull World Health Organ. 2009;87:246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Haonga BT, Liu M, Albright P, Challa ST, Ali SH, Lazar AA, Eliezer EN, Shearer DW, Morshed S. Intramedullary Nailing Versus External Fixation in the Treatment of Open Tibial Fractures in Tanzania: Results of a Randomized Clinical Trial. J Bone Joint Surg Am. [Published online ahead of print February 5, 2020]. DOI: 10.2106/JBJS.19.00563 [DOI] [PMC free article] [PubMed]
- 18.Haonga BT, Liu M, Wu HH, Zehraban Z, Eliezer EN. Reopearation rates following intramedullary naling versus external fixation of Gustilo type 3A open tibia shaft fractures. East African Orthop. J 2016;10. [Google Scholar]
- 19.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N CJ. Research electronic data capture (REDCap) – A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377-381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Henley MB, Chapman JR, Agel J, Harvey EJ, Whorton AM, Swiontkowski MF. Treatment of type II, IIIA, and IIIB open fractures of the tibial shaft: a prospective comparison of unreamed interlocking intramedullary nails and half-pin external fixators. J Orthop Trauma . 1998;12:1-7. [DOI] [PubMed] [Google Scholar]
- 21.Ibrahim JM, Conway D, Haonga BT, Eliezer EN, Morshed S, Shearer DW. Predictors of lower health-related quality of life after operative repair of diaphyseal femur fractures in a low-resource setting. Injury. 2018;49:1330-1335. [DOI] [PubMed] [Google Scholar]
- 22.Ikem IC, Oginni LM, Bamgboye EA. Open fractures of the lower limb in Nigeria. Int Orthop . 2001;25:386-388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Johal H, Schemitsch EH, Bhandari M. Why a decade of road traffic safety? J Orthop Trauma. 2014;28:S8-S10. [DOI] [PubMed] [Google Scholar]
- 24.Joshipura M, Gosselin RA. Surgical Burden of Musculoskeletal Conditions in Low- and Middle-Income Countries. World J Surg. 2020;44:1026-1032. [DOI] [PubMed] [Google Scholar]
- 25.Kanakaris NK, Giannoudis PV. The health economics of the treatment of long-bone non-unions. Injury. 2007;38:S77-S84. [DOI] [PubMed] [Google Scholar]
- 26.Kilama WL. The 10/90 gap in sub-Saharan Africa: resolving inequities in health research. Acta Trop. 2009;112:S8-S15. [DOI] [PubMed] [Google Scholar]
- 27.Litrenta J, Tornetta P, 3rd, Mehta S, Jones C, O'Toole RV, Bhandari M, Kottmeier S, Ostrum R, Egol K, Ricci W, Schemitsch E, Horwitz D. Determination of Radiographic Healing: An Assessment of Consistency Using RUST and Modified RUST in Metadiaphyseal Fractures. J Orthop Trauma . 2015;29:516-520. [DOI] [PubMed] [Google Scholar]
- 28.Meinberg EG, Agel J, Roberts CS, Karam MD, Kellam JF. Fracture and Dislocation Classification Compendium-2018. J Orthop Trauma . 2018; 2:S1-S170. [DOI] [PubMed] [Google Scholar]
- 29.Meara JG, Leather AJM, Hagander L, Alkire BC, Alonso N, Ameh EA, Bickler SW, Conteh L, Dare AJ, Davies J, Mérisier ED, El-Halabi S, Farmer PE, Gawande A, Gillies R, Greenberg SL, Grimes CE, Gruen RL, Ismail EA, Kamara TB, Lavy C, Lundeg G, Mkandawire NC, Raykar NP, Riesel JN, Rodas E, Rose J, Roy N, Shrime MG, Sullivan R, Verguet S, Watters D, Weiser TG, Wilson IH, Yamey G, Yip W. Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet. 2015;386:569-624. [DOI] [PubMed] [Google Scholar]
- 30.Milner SA, Davis TRC, Muir KR, Greenwood DC, Doherty M. Long-term outcome after tibial shaft fracture: is malunion important? J Bone Joint Surg Am. 2002;84A:971-980. [DOI] [PubMed] [Google Scholar]
- 31.Mock C, Cherian MN. The Global Burden of Musculoskeletal Injuries: Challenges and Solutions. Clin Orthop Relat Res. 2008;466:2306-2316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nobert N, Moremi N, Seni J, Dass RM, Ngayomela IH, Mshana SE, Gilyoma JM. The effect of early versus delayed surgical debridement on the outcome of open long bone fractures at Bugando Medical Centre, Mwanza, Tanzania. J Trauma Manag Outcomes. 2016;10:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Orthopaedic Trauma Association: Open Fracture Study Group. A new classification scheme for open fractures. J Orthop Trauma . 2010;24: 457-464. [DOI] [PubMed] [Google Scholar]
- 34.Pickard AS, Jiang R, Lin HW, Rosenbloom S, Cella D. Using Patient-reported Outcomes to Compare Relative Burden of Cancer: EQ-5D and Functional Assessment of Cancer Therapy-General in Eleven Types of Cancer. Clin Ther . 2016;38:769-777. [DOI] [PubMed] [Google Scholar]
- 35.Pollak AN, Jones AL, Castillo RC, Bosse MJ, MacKenzie EJ. The relationship between time to surgical débridement and incidence of infection after open high-energy lower extremity trauma. J Bone Joint Surg Am . 2010;92:7-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Prodromidis AD, Charalambous CP. The 6-Hour Rule for Surgical Debridement of Open Tibial Fractures: A Systematic Review and Meta-Analysis of Infection and Nonunion Rates. J Orthop Trauma . 2016;30:397-402. [DOI] [PubMed] [Google Scholar]
- 37.Raghunathan T, Lepkowski J, Van Hoewyk J, Solenberger P. A Multivariate Technique for Multiply Imputing Missing Values Using a Sequence of Regression Models. Surv Methodol . 2001;27: 85-95. [Google Scholar]
- 38.Schemitsch EH, Bhandari M, Guyatt G, Sanders DW, Swiontkowski M, Tornetta P, Walter SD, Zdero R, Goslings JC, Teague D, Jeray K, Mckee MD, SPRINT Investigators Prognostic factors for predicting outcomes after intramedullary nailing of the tibia. J Bone Joint Surg Am . 2012;94:1786-1793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schenker ML, Ahn J, Donegan D, Mehta S, Baldwin KD. The cost of after-hours operative debridement of open tibia fractures. J Orthop Trauma . 2014;28:626-31. [DOI] [PubMed] [Google Scholar]
- 40.Schenker ML, Yannascoli S, Baldwin KD, Ahn J, Mehta S. Does timing to operative debridement affect infectious complications in open long-bone fractures? A systematic review. J Bone Joint Surg Am. 2012;94:1057-1064. [DOI] [PubMed] [Google Scholar]
- 41.Sprague S, Bhandari M, Heetveld MJ, Liew S, Scott T, Bzovsky S, Heels-Ansdell D, Zhou Q, Swiontkowski M, Schemitsch EH. Factors associated with health-related quality of life, hip function, and health utility after operative management of femoral neck fractures. Bone Joint J. 2018;100-B:361-369. [DOI] [PubMed] [Google Scholar]
- 42.Sprague S, Petrisor B, Jeray K, McKay P, Heels-Ansdell D, Schemitsch E, Liew S, Guyatt G, Walter SD, Bhandari M; FLOW Investigators. Wound irrigation does not affect health-related quality of life after open fractures: results of a randomized controlled trial. Bone Joint J. 2018;100-B:88-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sprague S, Petrisor BA, Jeray KJ, Mckay P, Scott T, Heels-Ansdell D, Schemitsch EH, Liew S, Guyatt GH, Walter SD, Bhandari M. Factors Associated With Health-Related Quality of Life in Patients With Open Fractures. J Orthop Trauma . 2018;32:e5-e11. [DOI] [PubMed] [Google Scholar]
- 44.Sprague S, Schemitsch EH, Swiontkowski M, Della Rocca GJ, Jeray KJ, Liew S, Slobogean GP, Bzovsky S, Heels-Ansdell D, Zhou Q, Bhandari M; FAITH Investigators. Factors Associated with Revision Surgery After Internal Fixation of Hip Fractures. J Orthop Trauma. 2018;32:223-230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Srour M, Inaba K, Okoye O, Chan C, Skiada D, Schnüriger B, Trump M, Lam L, Demetriades D. Prospective evaluation of treatment of open fractures: effect of time to irrigation and debridement. JAMA Surg . 2015;150:332-336. [DOI] [PubMed] [Google Scholar]
- 46.Tanzania Commission for AIDS (TACAIDS), Zanzibar AIDS Commission (ZAC). Tanzania HIV Impact Survey (THIS) 2016-2017: Final Report. Dar es Salaam, Tanzania; December 2018. [Google Scholar]
- 47.Whiting PS, Galat DD, Zirkle LG, Shaw MK, Galat JD. Risk Factors for Infection After Intramedullary Nailing of Open Tibial Shaft Fractures in Low- and Middle-Income Countries. J Orthop Trauma . 2019;33: e234-239. [DOI] [PubMed] [Google Scholar]
- 48.Wijesekera MPC, Graham SM, Lalloo DG, Simpson H, Harrison WJ. Fracture management in HIV positive individuals: a systematic review. Int Orthop. 2016;40:2429-2445. [DOI] [PubMed] [Google Scholar]
- 49.Wong EG, Gupta S, Deckelbaum DL, Razek T, Kushner AL. Prioritizing injury care: a review of trauma capacity in low and middle-income countries. J Surg Res. 2015;193:217-222. [DOI] [PubMed] [Google Scholar]
- 50.World Bank Group. GDP (constant 2010 US$) Tanzania | Data. Available at: https://data.worldbank.org/indicator/NY.GDP.MKTP.KD?locations=TZ. Accessed March 11, 2020.
- 51.World Health Organization; Geneva. Global status report on road safety 2018. Licence: CC BY- NC-SA 3.0 IGO. Available at: https://www.who.int/publications-detail/global-status-report-on-road-safety-2018. Accessed March 11, 2020.
- 52.Yildiz C, Uzun O, Sinici E, Ateşalp AS, Ozşahin A, Başbozkurt M. [Psychiatric symptoms in patients treated with an Ilizarov external fixator]. Acta Orthop Traumatol Turc. 2005;39:59-63. [PubMed] [Google Scholar]
- 53.Young S. Orthopaedic trauma surgery in low-income countries. Acta Orthop Suppl. 2014;85:1-35. [DOI] [PubMed] [Google Scholar]