Abstract
Background
Hypertension disproportionately affects ethnic minority groups. Although health literacy may play role in these ethnic inequalities, little is known about the extent to which health literacy affects hypertension prevalence, awareness, treatment and control in different ethnic groups. Therefore, we assessed these associations in a multi-ethnic population.
Methods
Baseline data from the HELIUS study were used including participants of Dutch (n = 1948), South-Asian Surinamese (n = 2054) and African Surinamese (n = 1932) origin aged 18–70 years, who lived in Amsterdam, the Netherlands, were fluent in Dutch and underwent health literacy assessment through the Rapid Estimate of Adult Literacy in Medicine–Dutch (REALM-D). The REALM-D was categorized either as low (<60 sumscore) or adequate (≥60 sumscore) health literacy. Participants completed questionnaires and underwent physical examination.
Results
After adjusting for confounding variables, Dutch [odds ratio (OR) 2.02; 95% confidence interval (CI), 1.11–3.64] and African Surinamese (OR 1.36; 1.03–1.79) with low health literacy were more likely than those with adequate health literacy to have hypertension, whereas in South-Asian Surinamese this association was not significant. No significant associations were found between health literacy and hypertension awareness, treatment and control in any of the ethnic groups.
Conclusion
Findings indicate that health literacy is associated with hypertension prevalence in selected ethnic groups, but not with hypertension awareness, treatment and control. Targeting health literacy might be an entry point for tackling ethnic inequalities in hypertension prevalence. To substantially reduce these inequalities, further research is needed to explore other factors and pathways through which health literacy may impact hypertension outcomes in different ethnic groups.
Introduction
Hypertension is an important global health challenge due to its high prevalence and concomitant risks for cardiovascular complications, including stroke, myocardial infarction and heart failure.1 Current estimates suggest that in 2010, the global prevalence of hypertension exceeded 1.3 billion, a number projected to rise to 1.56 billion by 2025.1,2 Hypertension was estimated to have contributed to 9.4 million of the total 17.5 million cardiovascular deaths, which accounted for a third of all global deaths in 2010.1,3
Globally, large and increasing disparities in hypertension prevalence, awareness, treatment and control are found, in which low and low-middle income countries are at a disadvantage.2 Although improvement in hypertension prevalence and management is underway in high-income countries,2 recent studies suggest that ethnic minority groups are lagging behind. For instance in Europe, ethnic minority groups were found to have a disproportionately higher prevalence of hypertension, compared with the European host populations.4,5 Despite higher levels of hypertension awareness and treatment, hypertension control remains low among ethnic minority groups.6
Several explanatory factors for the ethnic inequalities in hypertension have been proposed, such as culture, socio-economic status, psychosocial factors and gene–environment interactions.7,8 Another potential factor that may explain these ethnic inequalities is health literacy, since many ethnic minority groups have low levels of health literacy.9,10 Health literacy pertains to the ability to access, understand, appraise and apply information in order to make informed health decisions.11
A growing body of evidence indicates that health literacy may be associated with blood pressure among hospitalized patients or patients with hypertension.12,13 In low-income African-American diabetes patients, health literacy has been suggested as a stronger predictor of chronic disease outcomes than socio-economic status and age.14 Although ethnic minority groups with low health literacy have higher risks for cardiovascular disease outcomes,15 we still know little about the extent to which health literacy may affect hypertension outcomes in different ethnic groups in Europe. Therefore, we studied the associations between health literacy and hypertension prevalence, awareness, treatment and control among a multi-ethnic population in Amsterdam, the Netherlands.
Methods
Baseline data of the Healthy Life In an Urban Setting (HELIUS) study were used. The HELIUS study is a large-scale prospective cohort study on health and healthcare utilization among a multi-ethnic population in Amsterdam, the Netherlands. The aims and design of HELIUS study have been published.7,16 In brief, at baseline (January 2011 until November 2015), HELIUS included participants of Dutch, Surinamese, Turkish, Moroccan and Ghanaian origin between 18 and 70 years of age, who live in Amsterdam, the Netherlands. They were randomly sampled via the municipality register, stratified for ethnicity. Of the 90 019 subjects contacted, approximately 55% responded either by card or after a home visit by an ethnically matched interviewer. Of those, 24 789 agreed to participate and for 22 165 participants, both questionnaires and physical examination were available for data analysis.16
Study population
Among all ethnic groups included in the HELIUS study, we only included participants of Dutch (n = 4564), South-Asian Surinamese (n = 3043) and African Surinamese (n = 4151) origin. These ethnic groups are proficient in the Dutch language, as Dutch is the sole official language of Suriname, being the language of education, government, business and media. This Dutch proficiency is essential to prevent bias, as the REALM-D test is highly dependent on a participant’s ability to read Dutch. Due to logistical reasons, the REALM-D test was only measured during the baseline period from January 2011 until March 2014. Until that time, 1948 Dutch, 2054 South-Asian Surinamese and 1932 African Surinamese origin participants were included and performed the REALM-D test, and were therefore included in the present study.
Measurements
Ethnicity was defined based on the participant’s country of origin as well as that of his/her parents.7,16 A participant is of Surinamese origin if either he/she was born in Suriname and at least one of the parents was born in Suriname (first generation), or if he/she was born in the Netherlands, but both parents were born in Suriname (second generation). For the Dutch sample, we invited people who were born in the Netherlands, and whose parents were born in the Netherlands. After data collection, participants of Surinamese ethnic origin were further classified according to self-reported ethnic origin: South-Asian Surinamese, African-Surinamese, Javanese Surinamese or other/unknown Surinamese. Of the Surinamese ethnic groups in the Netherlands, about 80% are either African or South-Asian origin, who are considered two main distinct ethnic groups in Surinam.16 Educational level was determined according to the highest qualification obtained in the Netherlands or in the country of origin. Educational level was stratified into four groups: (i) no schooling or elementary schooling, (ii) lower vocational/lower secondary schooling, (iii) intermediate vocational/higher secondary schooling and (iv) higher vocational schooling/university.
Hypertension prevalence, awareness, treatment and control
Blood pressure (BP) was measured by using a validated automated digital sphygmomanometer (Microlife WatchBP Home). BP was measured on the left arm in a seated position after the respondent had been seated for at least 5 min. All physical and BP measurements were conducted twice and the means of the two readings were used for analyses. The participants were asked to bring all their prescribed medications to the research location, which were categorized using the Anatomical Therapeutic Chemical (ATC) classification system. BP-lowering medication included centrally acting anti-hypertensives (ATC code C02), diuretics (ATC code C03), beta-blockers (ATC code C07), calcium channel blockers (ATC code C08) and agents acting on renin-angiotensin-aldosterone system (ATC code C09). Hypertension prevalence was defined as the proportion of individuals with hypertension [i.e. values ≥140 mmHg systolic blood pressure (SBP) and/or ≥90 mmHg diastolic blood pressure (DBP)], or being on BP lowering medication.
Hypertension awareness was defined as the proportion of hypertensive individuals who were aware and self-reported any prior formal diagnosis of hypertension. Hypertension treatment pertained to the proportion of hypertensive individuals who were receiving prescribed BP lowering medication. Hypertension control referred to the proportion of hypertensive individuals on BP lowering medication with systolic BP < 140 mmHg and diastolic BP < 90 mmHg.
Health literacy
To assess and provide an indication of health literacy, we used the Rapid Estimate of Adult Literacy which was previously translated to Dutch (REALM-D).17 Research assistants were trained using standard operating procedures for pronunciation of the instrument’s medical terms and instructed in detail how to assess accents and pronunciation. These trained research assistants asked participants to read aloud 66 medical terms in Dutch that were arranged in order of increasing difficulty. For each term, the participants received a score of 1 if they pronounced it correctly. This resulted in a total sumscore ranging from 0 to 66. We dichotomized this variable to be able to estimate the number of people with health literacy and to study the association between low health literacy and hypertension outcomes. Following the REALM criteria, sumscores were divided following standard cut-offs that are based on grade-level estimates in the United States: below 60 were considered low health literacy, while sumscores ≥60 indicated adequate health literacy.18
Data analysis
Statistical analyses were conducted with IBM SPSS Statistics 25 (IBM Corporation). Descriptive statistical analyses were carried out on characteristics of the participants, expressed as percentages or means with corresponding 95% confidence intervals (CI) calculated through bootstrapping. Logistic regression analyses were performed to assess the associations between health literacy and hypertension prevalence, awareness, treatment and control in the three ethnic groups. Estimates were adjusted for confounders (age, sex and educational level).19 Based on an interaction analysis, a significant interaction was found between health literacy and ethnicity for hypertension prevalence, after adjusting for age, sex and educational level. Therefore, all analyses were stratified by ethnicity.
Ethical issues
The study protocols were approved by the AMC Ethical Review Board, and all the participants provided written informed consent.
Results
Characteristics of study participants
Table 1 summarizes the characteristics of the participants who underwent REALM-D test stratified by ethnic group. The three ethnic groups were of similar age and had a similar percentage of women. Both Surinamese origin groups had lower educational levels and had higher mean systolic and diastolic BP levels than Dutch. This pattern is consistent with results in the total HELIUS population.16 The prevalence of low health literacy was higher among the Surinamese groups than their Dutch counterparts.
Table 1.
Characteristics of participants by ethnicity
| Dutch | South-Asian Surinamese | African Surinamese | |
|---|---|---|---|
| (n = 1948) | (n = 2054) | (n = 1932) | |
| Age (years) | 46.5 (45.9–47.1) | 45.7 (45.2–46.3) | 47.2 (46.7–47.8) |
| Sex, woman (%) | 54.8 (52.5–56.7) | 55.7 (53.4–57.9) | 64.2 (62.2–66.5) |
| Educational level (%) | |||
| No or elementary schooling | 2.9 (2.2–3.7) | 13.8 (12.3–15.3) | 5.4 (4.4–6.4) |
| Lower vocational/lower secondary schooling | 15.2 (13.6–16.8) | 34.9 (32.7–36.9) | 34.7 (32.6–36.9) |
| Intermediate vocational/higher secondary | 22.6 (20.9–24.6) | 29.6 (27.6–31.6) | 36.0 (33.9–38.2) |
| Higher vocational schooling/university | 58.9 (56.8–61.3) | 21.8 (20.0–23.6) | 23.9 (22.0–25.9) |
| Systolic BP (mmHg) | 126.1 (125.4–125.2) | 129.1 (128.3–129.9) | 132.5 (131.7–133.3) |
| Diastolic BP (mmHg) | 77.0 (76.6–77.4) | 80.1 (79.6–80.5) | 81.8 (81.3–82.3) |
| Low health literacy (%) | 4 (2.9–4.6) | 24 (22.5–26.2) | 17 (15.3–18.7) |
Values are means or % with corresponding 95% CI.
BP, blood pressure.
Health literacy and hypertension prevalence, awareness, treatment and control
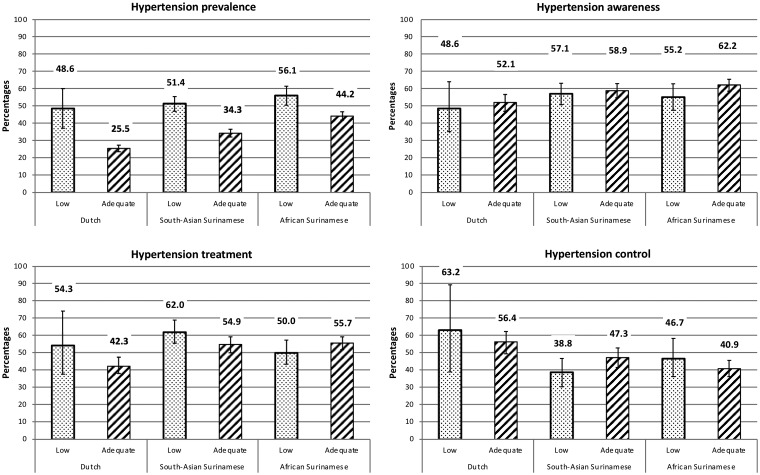
In all ethnic groups, the prevalence of hypertension was higher among those with low health literacy than those with adequate health literacy (figure 1, crude models). However, after adjusting for age and sex, this difference persisted only among Dutch and African Surinamese, but not among South-Asian Surinamese (table 2, hypertension model 1). These results remained significant for Dutch and African Surinamese after further adjustment for educational level (table 2, hypertension model 2).
Figure 1.
The crude proportions of hypertension prevalence, awareness, treatment and control in participants with low and adequate health literacy by ethnic group. The error bars indicate the 95% CI
Table 2.
Associations between low health literacy and hypertension prevalence, awareness, treatment and control
| Dutch | South-Asian Surinamese | African Surinamese | |
|---|---|---|---|
| Hypertensiona | n/N = 512/1948 | n/N = 790/2051 | n/N = 891/1932 |
| Model 1 | 2.90 (1.65, 5.09) | 1.22 (0.97, 1.55) | 1.46 (1.12, 1.91) |
| Model 2 | 2.02 (1.11, 3.64) | 1.16 (0.90, 1.51) | 1.36 (1.03, 1.79) |
| Awareness in hypertensivesb | n/N = 265/512 | n/N = 456/790 | n/N = 537/891 |
| Model 1 | 0.80 (0.39, 1.62) | 0.73 (0.53, 1.08) | 0.71 (0.50, 1.00) |
| Model 2 | 0.85 (0.40, 1.84) | 0.75 (0.53, 1.05) | 0.73 (0.51, 1.05) |
| Treatment in hypertensivesc | n/N = 265/512 | n/N = 452/790 | n/N = 486/891 |
| Model 1 | 1.46 (0.69, 3.06) | 1.03 (0.75, 1.43) | 0.76 (0.54, 1.08) |
| Model 2 | 1.19 (0.53, 2.65) | 0.96 (0.68, 1.37) | 0.72 (0.50, 1.04) |
| Control in treated hypertensivesd | n/N = 126/221 | n/N = 200/452 | n/N = 204/486 |
| Model 1 | 1.49 (0.71, 3.02) | 0.80 (0.57, 1.13) | 1.03 (0.76, 1.61) |
| Model 2 | 1.09 (0.49, 2.45) | 0.78 (0.54, 1.12) | 1.07 (0.72, 1.58) |
Values are odds ratios (ORs) with the corresponding 95% CI.
The reference category is adequate health literacy.
Model 1 is adjusted for age and sex. Model 2 is adjusted for age, sex and educational level.
Missing cases: hypertension: Dutch = 4; South-Asian Surinamese = 3; African Surinamese = 3; hypertension awareness: Dutch = 1; South-Asian Surinamese = 8; African Surinamese = 7.
aHypertension prevalence was the proportion of individuals with hypertension (i.e. values ≥140 mmHg SBP and/or ≥90 mmHg DBP), or being on BP lowering medication.
bHypertension awareness was the proportion of hypertensive individuals who were aware and self-reported any prior formal diagnosis of hypertension.
cHypertension treatment was the proportion of hypertensive individuals who were receiving prescribed BP lowering medication.
dHypertension control was the proportion of hypertensive individuals on BP lowering medication with systolic BP<140 mmHg and diastolic BP<90 mmHg.
Although not statistically significant, there was a pattern for lower hypertension awareness amongst those with low health literacy compared with those with adequate health literacy in all ethnic groups after adjustment for age and sex (table 2, awareness model 1). However, after further adjustment for educational level, people with low and adequate health literacy did not differ in their awareness of hypertension in all ethnic groups (table 2, awareness model 2). No clear pattern was found in the association of health literacy with hypertension treatment and with hypertension control (table 2, treatment and control).
Discussion
Our current findings indicate an association between health literacy and hypertension prevalence in Dutch and African Surinamese resident in the Netherlands, independent of age, sex and educational level. In South-Asian Surinamese, we did not find this association to be significant. Health literacy was not associated with hypertension awareness, treatment and control in any of the ethnic groups.
Associations between health literacy and hypertension
Our findings suggest that the association between health literacy and hypertension differs between ethnic groups. These findings are in line with findings on health literacy and diabetes, which reported associations between health literacy and diabetes in some ethnic groups but not in others. Sentell et al.’s population-based survey in a multi-ethnic sample in Hawaii found significant associations between health literacy and diabetes among native Hawaiians and Japanese, but not among European, Filipino and other Pacific Islanders/Asian Americans.20 The reasons for the ethnic variations in the association between health literacy and hypertension prevalence are complex and not well understood.
Potentially, differences in cultural factors and differences in access to health information may contribute to the observed differences. While the association between health literacy and hypertension prevalence was strongest in the Dutch, followed by African Surinamese and lacking in South-Asian Surinamese, the prevalence of low health literacy rate was highest in South-Asian Surinamese followed by African Surinamese and lowest in Dutch. It is possible that the low health literacy groups within the Dutch and African Surinamese differ uniquely from those of the South-Asian Surinamese, which may contribute to the observed differential associations between the ethnic groups. Among the Dutch, those with low health literacy may experience weak social cohesion and segregation from those with high health literacy due to the individualistic culture in the Netherlands.21 It may also be because the Dutch visit their general practitioners less often than their ethnic minority counterparts.22 Among the Dutch with low health literacy, reduced access to primary healthcare providers may result in poor knowledge about preventive services and a higher predisposition to hypertension.23,24 Higher frequency of doctor visits among other ethnic groups, irrespective of health literacy status, may have a protective effect.
Alternatively, the lack of association between health literacy and hypertension in South-Asian Surinamese might be due to strong social cohesion based on ethnic identity or religion.25 This strong social cohesion may act as a buffer for those with low health literacy to reduce their chance of developing hypertension as they can obtain assistance from peers in accessing and understanding health information.26 Another potential reason may be that South-Asian Surinamese with adequate health literacy might still encounter barriers (e.g. cultural or linguistic barriers) in improving their cardiovascular health,27,28 which may prevent them from accessing preventive services.29
Health literacy is a relatively new concept and there is an ongoing debate about whether health literacy parallels formal educational level.19,30 In our current findings, the identified association between health literacy and hypertension prevalence remained significant in some ethnic groups, even after adjusting for educational level. These findings suggest that health literacy is not merely equivalent to formal education and is associated with hypertension independent of educational level.
In all ethnic groups, we did not find any associations between health literacy and hypertension awareness, treatment and control. These findings are consistent with other studies, which found no significant associations between health literacy and disease management outcomes such as diabetes.31,32 Al Sayah et al.’s systematic literature review on the relationships between health literacy and health outcomes in people with diabetes, for example, found no convincing evidence for associations between health literacy and processes or outcomes of diabetes-related care. Factors that might have contributed to awareness, treatment and control being similar in all ethnic groups include the universal healthcare coverage in the Netherlands as well as the continuous priority toward addressing health inequality over the years in the Netherlands. This message seems to be getting through the clinicians as observed on the equal access to hypertension medication regardless of the level of health literacy.30
A limitation of this study is the use of the cross-sectional data, which makes causation difficult to determine. Patients diagnosed with hypertension, and thus aware of their condition, could have increased their health literacy due to more frequent contact with the healthcare system, which may have attenuated our results. Another limitation is that BP levels were measured twice at a single visit, which might have overestimated BP levels due to the ‘white coat effect’. However, this limitation applies to all ethnic groups and previous study found no significant differences in ‘white coat effect’ across groups with different ethnic backgrounds.33,34 The response rates in our study were relatively low and varied between the ethnic groups, which may bias our study findings. Nonetheless, the distribution of the male and female study population appeared to be largely representative of the original sample; and the non-response analyses showed that socio-economic differences between participants and non-participants were small.16
Finally, the REALM-D, which was the health literacy measure used in this study, did not measure health literacy to its fullest extent. The REALM-D merely measures reading and pronunciation skills, whereas accessing, understanding, appraising and applying health information need more than just reading skills.11 In addition, the REALM-D has not yet been validated for use in a population with different ethnic backgrounds. Nonetheless, the REALM-D provides a good indication of the level of health literacy, as reading skills is essential for all the components of health literacy. Even considering these possible measurement concerns, a number of studies show that the REALM is a valid instrument to measure minimal domains of health literacy particularly in a large-scale population study as HELIUS.18,35,36
Future research in this area should focus on the underlying mechanisms behind the ethnic inequalities in the association between health literacy and hypertension prevalence. Further research should also make use of a health literacy assessment tool, which covers and measures the full extent of health literacy in a population with different ethnic backgrounds.27 In recent years, new health literacy instruments have been developed for the multi-dimensional measurement of health literacy among general population. These tools include for example the Mandarin Health Literacy Scale (MaHLS) or the European Health Literacy Survey Questionnaire (HLS-EU-Q), both of which were validated to have high overall internal consistency. The MaHLS could be used for other language speakers, while the HLS-EU-Q could capture a wide public health perspective, which could be used for large-scale population studies.37
Conclusion
In conclusion, the current study indicates that independent of education, low health literacy is associated with higher hypertension prevalence in Dutch and African Surinamese groups but not in South-Asian Surinamese. In all ethnic groups, health literacy was not associated with hypertension awareness, treatment and control. Targeting health literacy might be an entry point for tackling ethnic inequalities in hypertension prevalence. To substantially reduce these inequalities, further research is needed to explore other factors and pathways through which health literacy may impact hypertension outcomes in different ethnic groups.
Acknowledgements
We gratefully acknowledge the participants of the HELIUS study and the management team, research nurses, interviewers, research assistants and other staff who have taken part in gathering the data of this study. All authors meet the criteria for authorship as stated by the International Committee of Medical Journal Editors authorship guidelines. All authors have given the final approval of the manuscript to be submitted for publication.
Funding
The HELIUS study was conducted by the Academic Medical Center Amsterdam and the Public Health Service of Amsterdam. Both organizations provided core support for HELIUS. The HELIUS study was also funded by the Dutch Heart Foundation (2010T084), the Netherlands Organization for Health Research and Development (ZonMw) (200500003), the European Union (FP-7) (278901) and the European Fund for the Integration of non-EU immigrants (EIF) (2013EIF013). K.A.C.M. was supported by the Intramural Research Program of the National Institutes of Health in the Center for Research on Genomics and Global Health (CRGGH). The CRGGH was supported by the National Human Genome Research Institute, the National Institute of Diabetes and Digestive and Kidney Diseases, the Center for Information Technology and the Office of the Director at the National Institutes of Health (1ZIAHG200362).
Conflicts of interest: None declared.
Key points
Hypertension disproportionately affects ethnic minority groups and health literacy may play a role in these ethnic inequalities.
We assessed the extent to which health literacy affects hypertension prevalence, awareness, treatment and control in different ethnic groups.
We found that health literacy is associated with hypertension prevalence in selected ethnic groups, but not with hypertension awareness, treatment and control.
Targeting health literacy might be an entry point for tackling ethnic inequalities in hypertension prevalence.
To substantially reduce these inequalities, further research is needed to explore other factors and pathways through which health literacy may impact hypertension outcomes in different ethnic groups.
References
- 1. World Health Organisation (WHO; ). Global Status Report on Noncommunicable Diseases. Switzerland, 2014. [Google Scholar]
- 2. Mills KT, Bundy JD, Kelly TN, et al. Global disparities of hypertension prevalence and control. Circulation 2016;134:441–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2224–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Agyemang C, Bindraban N, Mairuhu G, et al. Prevalence, awareness, treatment, and control of hypertension among Black Surinamese, South Asian Surinamese and White Dutch in Amsterdam, The Netherlands: the SUNSET study. J Hypertens 2005;23:1971–7. [DOI] [PubMed] [Google Scholar]
- 5. Agyemang C, Bhopal R. Is the blood pressure of people from African origin adults in the UK higher or lower than that in European origin white people? A review of cross-sectional data. J Hum Hypertens 2003;17:523–34. [DOI] [PubMed] [Google Scholar]
- 6. Agyemang C, Kieft S, Snijder MB, et al. Hypertension control in a large multi-ethnic cohort in Amsterdam, The Netherlands: the HELIUS study. Int J Cardiol 2015;183:180–9. [DOI] [PubMed] [Google Scholar]
- 7. Stronks K, Snijder MB, Peters RJ, et al. Unravelling the impact of ethnicity on health in Europe: the HELIUS study. BMC Public Health 2013;13:402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Agyei B, Nicolaou M, Boateng L, et al. Relationship between psychosocial stress and hypertension among Ghanaians in Amsterdam, the Netherlands - The GHAIA study. BMC Public Health 2014;14:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cunningham CT, Sykes LL, Metcalfe A, et al. Ethnicity and health literacy: a survey on hypertension knowledge among Canadian ethnic populations. Ethn Dis 2014;24:276–82. [PubMed] [Google Scholar]
- 10. Fransen M, Harris V, Essink-Bot M-L. Beperkte gezondheidsvaardigheden bij patiënten van allochtone herkomst [Low health literacy in ethnic minority patients: understandable language is the beginning of good healthcare]. Ned Tijdschr Geneeskd 2013;157:A5581. [PubMed] [Google Scholar]
- 11. Sørensen K, Van den Broucke S, Fullam J, et al. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health 2012;12:80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mcnaughton CD, Kripalani S, Cawthon C, et al. Association of health literacy with elevated blood pressure: a cohort study of hospitalized patients. Med Care 2014;52:346–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Halladay JR, Donahue KE, Cené CW, et al. The association of health literacy and blood pressure reduction in a cohort of patients with hypertension: the heart healthy lenoir trial. Patient Educ Couns 2017;100:542–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Al Sayah F, Majumdar SR, Egede LE, Johnson JA. Associations between health literacy and health outcomes in a predominantly low-income African American population with type 2 diabetes. J Health Commun 2015;20:581–8. [DOI] [PubMed] [Google Scholar]
- 15. Ghisi GLDM, Chaves GSDS, Britto RR, Oh P. Health literacy and coronary artery disease: a systematic review. Patient Educ Couns 2018;101:177–84. [DOI] [PubMed] [Google Scholar]
- 16. Snijder MB, Galenkamp H, Prins M, et al. Cohort profile: the Healthy Life in an Urban Setting (HELIUS) study in Amsterdam, the Netherlands. BMJ Open 2017;7:e017873–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Fransen MP, Van Schaik TM, Twickler TB, Essink-Bot ML. Applicability of internationally available health literacy measures in the Netherlands. J Health Commun 2011;16:134–49. [DOI] [PubMed] [Google Scholar]
- 18. Davis TC, Long SW, Jackson RH, et al. Rapid estimate of adult literacy in medicine: a shortened screening instrument. Fam Med 1993;25:391–5. [PubMed] [Google Scholar]
- 19. Rowlands G, Shaw A, Jaswal S, et al. Health literacy and the social determinants of health: a qualitative model from adult learners. Health Promot Int 2017;32:130–8. [DOI] [PubMed] [Google Scholar]
- 20. Sentell T, Baker KK, Onaka A, Braun K. Low health literacy and poor health status in Asian Americans and Pacific Islanders in Hawai’i. J Health Commun 2011;16: 279–94. [DOI] [PubMed] [Google Scholar]
- 21. Veenhoven R Individualisme zo slecht nog niet [Individualism is not that bad]. Psychol Mag 2000:19:12–15. [Google Scholar]
- 22. Van Der Gaag M, Van Der Heide I, Spreeuwenberg PMM, et al. Health literacy and primary health care use of ethnic minorities in the Netherlands. BMC Health Serv Res 2017;17:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Holland C, Clark A, Katz J, Peace S. Social interactions in urban public places. Open Univ 2007;12:1–84. [Google Scholar]
- 24. Turagabeci AR, Nakamura K, Kizuki M, Takano T. Family structure and health, how companionship acts as a buffer against ill health. Health Qual Life Outcomes 2007;5:61–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. van der Heide I, Wang J, Droomers M, et al. The relationship between health, education, and health literacy : results from the Dutch adult. J Health Commun 2013;18:172–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Bodewes AJ, Kunst AE. Involving hard-to-reach ethnic minorities in low-budget health research: lessons from a health survey among Moluccans in the Netherlands. BMC Res Notes 2016;9:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Friel S, Marmot MG. Action on the social determinants of health and health inequities goes global. Annu Rev Public Health 2011;32:225–36. [DOI] [PubMed] [Google Scholar]
- 28. De Gaudemaris R, Lang T, Chatellier G, et al. Socioeconomic inequalities in hypertension prevalence and care: the IHPAF study. Hypertension 2002;39:1119–25. [DOI] [PubMed] [Google Scholar]
- 29.National Institute for Public Health and Environment (RIVM). Health and determinants [Gezondheid en determinanten]. Houten, 2010. http://edepot.wur.nl/137913 (1 April 2018, date last accessed).
- 30. Nutbeam D Defining, measuring and improving health literacy. JAMHTS 2015;42:450–5. [Google Scholar]
- 31. Al Sayah F, Majumdar SR, Williams B, et al. Health literacy and health outcomes in diabetes: a systematic review. J Gen Intern Med 2013;28:444–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Fransen MP, von Wagner C, Essink-Bot ML. Diabetes self-management in patients with low health literacy: ordering findings from literature in a health literacy framework. Patient Educ Couns 2012;88:44–53. [DOI] [PubMed] [Google Scholar]
- 33. Agyemang C, Bhopal R, Bruijnzeels M, Redekop WK. Does the white-coat effect in people of African and South Asian descent differ from that in White people of European origin? A systematic review and meta-analysis. Blood Pressure Monit 2005;10:243–8. [DOI] [PubMed] [Google Scholar]
- 34. Martin U, Haque MS, Wood S, et al. Ethnicity and differences between clinic and ambulatory blood pressure measurement. Am J Hypertens 2015;28:729–38. [DOI] [PubMed] [Google Scholar]
- 35. Arozullah AM, Yarnold PR, Bennett CL, et al. Development and validation of a short-form, rapid estimate of adult literacy in medicine. Med Care 2007;45:1026–33. [DOI] [PubMed] [Google Scholar]
- 36. Dumenci L, Matsuyama RK, Kuhn L, et al. On the validity of the Rapid Estimate of Adult Literacy in Medicine (REALM) Scale as a measure of health literacy. Commun Methods Meas 2013;7:134–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Liu H, Zeng H, Shen Y, et al. Assessment tools for health literacy among the general population: a systematic review. Int J Environ Res Public Health 2018;15:1711. [DOI] [PMC free article] [PubMed] [Google Scholar]