Abstract
Purpose:
To increase awareness of the need for coordinated medical care at 10-km races and to help direct future medical planning for these events.
Methods:
We related medical encounter data from nineteen 10-km road races to runner, race and environmental characteristics. We quantified the most commonly used resources and described the disposition of runners in these encounters.
Results:
Across the 19 races and 90,265 finishers, there were 562 medical events for a cumulative incidence of 6.2 events per 1000 finishers (95% CI 5.7, 6.8). Race size was associated with an increased incidence of medical events. Overall, the most common diagnosis was heat-related illness (1.6 per 1000 finishers), followed by musculoskeletal complaints (1.3 per 1000 finishers) and fluid/electrolyte imbalances (1.2 per 1000 finishers). For all diagnoses, runners with finishing times in the first performance quintile and in the fifth performance quintile had greater representation in the medical tent than mid-pack runners. Most runners were treated with supportive care, basic first aid, and oral rehydration. Ninety-four runners (1.0 per 1000 finishers) required ice water immersion for exertional heat stroke. There were low rates of hospital transport (0.2 per 1000 finishers), and no fatalities.
Conclusions:
In 10-km road races, injury rates are low compared to longer races in similar weather conditions. Common medical issues can be managed with basic resources in the on-site medical tent. Green flag start race conditions may not predict race safety with regard to exertional heat stroke risk. There were no deaths in nearly 100,000 finishers.
Keywords: race medicine, running injury, event medical management, exertional heat stroke
Introduction
More than 18 million runners in the United States participated in road races during 2016 and 2017 (1). Coordinated care - involving on-site medical staff as well as local, regional and federal agencies, and the adoption of standardized emergency protocols for these events - is increasingly recognized as a key component of the health and safety of participants (2). Most publications outlining road race medical encounters, tent set-up, supplies and care protocols are related to the marathon distance (3) (4) (5). However, marathon participation represented only 3% of the more than 17 million road race participants in 2015 (6). Indeed, 7 of the 10 largest road races in 2016 were shorter events, with 56, 993 registrants in the 10-km AJC Peachtree Road Race (7).
The large number of participants in such races presents public health and safety challenges. Yet, there is significant variability in medical care planning and implementation across races, and limited published data or guidelines for non-marathon distance events. The Falmouth Road Race, an 11.3-km event held in mid-August in Falmouth, Massachusetts, is the most studied of these shorter distance races, and is notorious for its hot, humid conditions, late morning start, and high incidence of heat-related illness (8). Studies organized around this race have provided critical information about the management of exertional heat stroke at road races, and about the role of race day environment in contributing to race-related morbidity (9). However, the influence of weather on medical tent encounters at other shorter distance races held under less extreme conditions has not been widely studied. Furthermore, the Falmouth Road Race studies focus primarily on heat-related illness and do not include a detailed examination of other injury and illness.
The purpose of this study was to shed light on the common medical issues in the on-site medical tent at 10-km road races, and to identify the resources required to minimize the impact of these races on the community at large. Our review of the literature identified only one previous publication describing medical encounters at a 10-km road race in detail (the 1979 Peachtree Road Race), which focused primarily on heat-related illness (10). We aimed to increase awareness of the need for coordinated medical care at this race distance and to help direct future medical planning for these events.
Methods
Overview:
We analyzed race characteristics, environmental data, participant characteristics, and finish area medical encounters for nineteen 10-km road races (3 different courses: the Boston Athletic Association (BAA) 10-km, the Finish at the 50 10-km, and the Beach to Beacon 10-km) from 2011 to 2017.
Institutional Approval.
This study was reviewed by the Partners Human Research Committee and was deemed exempt from continuing review (Protocol #: 2018P000468/PHS).
Weather data.
We obtained meteorological data for the day of each race from Local Climatological Data Daily summaries published by US Department of Commerce, National Oceanic & Atmosphere Administration, National Environmental Satellite, Data and Information Service. These daily summaries detail weather conditions at local airports, and we chose the closest airport location to each race (see Table, Supplemental Digital Content 1, which describes the sources of the weather characteristics for each race).
We abstracted the sky conditions, ambient temperature, relative humidity, precipitation and wet bulb globe temperatures for the start time of each race and for the finishing time of each runner who presented to the medical tent. Wet bulb globe temperature is a commonly used calculation for assessing weather conditions in the setting of athletic competition, and uses measurements of air water content, radiant heat and ambient temperature to calculate risk of heat-related illness (11). We categorized each race according to the International Institute for Race Medicine alert level, a guideline developed to direct race modification (12) (13) (see Table, Supplemental Digital Content 2, which describes the International Institute for Race Medicine Alert Levels). We then determined the incidence of exertional heat stroke for each race (Table 1).
Table 1:
Weather and Race Characteristics
| Race | Year | Tamb °C | Sky | Precip (In) | RH (%) | WBGT (°C) | Finishers | Female N (%) | Enc/1000 | EHS/1000 | IIRM |
|---|---|---|---|---|---|---|---|---|---|---|---|
| BAA 10K | Overall | 31898 | 4.2 | 0.6 | |||||||
| BAA 10K | 2012 | 22.2 | CLR | 0 | 52 | 16.1 | 4561 | 2536 (55.6) | 3.9 | 0.7 | Green |
| BAA 10K | 2013 | 24.4 | FEW, SCT | 0 | 62 | 19.6 | 5434 | 3650 (67.1) | 5.7 | 1.3 | Yellow |
| BAA 10K | 2015 | 17.8 | BKN, OVC | 0.27 | 100 | 17.8 | 5960 | 3235 (54.3) | 2.5 | 0 | Green |
| BAA 10K | 2016 | 21.1 | FEW | 0 | 61 | 16.6 | 7816 | 4433 (56.7) | 4.1 | 1.0 | Green |
| BAA 10K | 2017 | 23.9 | FEW | 0 | 46 | 16.8 | 8127 | 4637 (57.3) | 4.7 | 0.2 | Green |
| F50 | Overall | 13823 | 2.9 | 0.3 | |||||||
| F50 | 2011 | 25.6 | FEW | 0 | 69 | 21.5 | 3037 | 1635 (53.8) | 4.3 | 0.3 | Yellow |
| F50 | 2012 | 27.8 | FEW | 0 | 38 | 18.4 | 2991 | 1608 (53.8) | 0.3 | 0 | Green |
| F50 | 2013 | 27.8 | CLR | 0 | 77 | 24.7 | 2283 | 1271 (55.7) | 4.4 | 0.4 | Red |
| F50 | 2014 | 26.7 | CLR | 0 | 67 | 22.2 | 1624 | 877 (54.0) | 2.5 | 1.2 | Red |
| F50 | 2015 | 22.2 | CLR | 0 | 55 | 16.7 | 1357 | 709 (52.2) | 3.7 | 0 | Green |
| F50 | 2016 | 24.4 | CLR | 0 | 42 | 16.4 | 1246 | 626 (50.2) | 4 | 0 | Green |
| F50 | 2017 | 26.1 | CLR | 0 | 41 | 17.6 | 1285 | 656 (51.1) | 1.6 | 0 | Green |
| B2B | Overall | 44544 | 8.7 | 1.6 | |||||||
| B2B | 2011 | 22.2 | FEW | 0 | 82 | 20.1 | 5876 | 2924 (49.8) | 12.6 | 1.4 | Yellow |
| B2B | 2012 | 25.6 | CLR | 0 | 67 | 21.2 | 6105 | 3156 (51.7) | 12.4 | 3.6 | Yellow |
| B2B | 2013 | 16.7 | OVC | T | 90 | 15.7 | 6247 | 3269 (52.3) | 5.8 | 0.3 | Green |
| B2B | 2014 | 20.6 | SCT, OVC | 0 | 87 | 19.2 | 6490 | 3513 (54.1) | 7.4 | 1.1 | Yellow |
| B2B | 2015 | 22.8 | FEW | 0 | 62 | 18 | 6594 | 3635 (55.1) | 11.1 | 1.8 | Yellow |
| B2B | 2016 | 23.3 | OVC | 0 | 74 | 20.1 | 6345 | 3401 (53.6) | 6.5 | 1.4 | Yellow |
| B2B | 2017 | 21.1 | BKN, OVC | 0 | 87 | 19.7 | 6887 | 3742 (54.3) | 5.8 | 1.5 | Yellow |
| Average | 23.3 | 66 | 18.9 | 4751 | 2606 (54.0%) |
Incidence rates are expressed as medical encounters per 1000 finishers.
BAA Boston Athletic Association; F50 Finish at the 50; B2B Beach to Beacon; Tamb (°C) Ambient temperature in °Celsius; Sky Sky Conditions; Precip (In) Precipitation in inches; RH Relative Humidity; WBGT (°C) Wet Bulb Globe Temperature in °Celsius; Enc Medical Encounters; EHS Exertional Heat Stroke; IIRM International Institute for Race Medicine alert level. CLR Clear; FEW Few clouds; SCT Scattered clouds; BKN Broken clouds; OVC Overcast;
Runner data.
We used race results published on www.CoolRunning.com to determine the number of race finishers for each race. We used medical encounter forms from each race to identify runners who presented to the medical tent, and we used first name, last name, and/or bib number to search race results to determine age, sex, finishing time, and runner place. If we were unable to find a runner in the published list of finishers, we assumed that runner was not able to finish the race prior to presenting to the medical tent. We grouped finishers into 5 categories based on quintile of finishing place; non-finishers were not included in performance quintiles. We then entered de-identified demographic and performance data (if available) into a REDCap electronic data capture tool (14) hosted at Brigham and Women’s Hospital.
Injury and Illness data.
Two authors (R.G.B. and A.G.F.) obtained injury and illness data from each race, as well as resources used during treatment, by retrospective review of finish line medical tent encounter forms (see Figure, Supplemental Digital Content 3 for a sample medical encounter form). There were no additional course medical tents; runners requiring medical attention along the course were transported via sweep vehicle or mobile unit to the finish line medical tent. Volunteers in the tent transcribed the medical encounter forms at the time of presentation and during the runner’s clinical course in the tent. The lead physician(s) at the time of discharge from the tent reviewed and signed all encounter forms.
When classifying injury and illness encounters, we differentiated heat-related illness from other types of collapse to be consistent with what was documented on the race medical encounter forms. At the time of presentation, runners with suspected heat-related illness were classified and triaged according to assessment of mental status and physical exam findings. If there was concern for exertional heat stroke, rectal thermistors were used to obtain core body temperatures to confirm the diagnosis. On our records review, we sub-categorized heat-related illness as exertional heat stroke if a runner’s documented core body temperature exceeded 40 °C and they had documented evidence of mental status changes or were treated with ice water immersion. The medical encounter forms of some runners contained written notes reporting “overheated” and/or “cramping”, but had temperature measurements of less than 40°C and did not have documented mental status changes; we considered these runners to have heat-related illness but not exertional heat stroke.
For other complaints, we categorized runners based on the diagnoses and notes written on their medical encounter forms. We categorized runners under “exercise-associated collapse,” if this was written on their encounter form. We considered runners with a written diagnosis of dehydration or hypoglycemia to have “fluid/electrolyte imbalances”, and if they were documented to have nausea, vomiting, stomach cramps, or diarrhea, to have a “gastrointestinal” diagnosis. We grouped runners with documented respiratory distress, or who were administered a bronchodilator, under “respiratory”, and runners with documented chest pain, tachycardia or electrocardiogram evaluation under “cardiac”. We categorized runners with musculoskeletal injuries under “musculoskeletal”, and runners requiring blister care under “dermatologic”. The practice in these 19 races was to use encounter forms made of two layers of carbonless copy paper; when a runner was transported, the top form traveled with him/her to the hospital and the underlying “yellow sheet” remained with the other medical encounter forms for a given race. In the records we reviewed, all transported runners had only a “yellow sheet” as their medical encounter form, which indicated their disposition.
Data analysis.
We summarized race characteristics descriptively using frequency and proportion for categorical variables and mean and ranges for continuous variables. We reported the number of medical tent utilizers per the number of race finishers, as has been done in previous reports (3). We calculated the cumulative incidence of medical events overall, the incidence of all heat-related illness, and the incidence of exertional heat stroke for each race/year and for each race as the number of events divided by the number of finishers and computed exact (Clopper-Pearson) confidence intervals (15).
We summarized overall medical encounter rate, heat-related illness encounters (overall and for exertional heat stroke encounters), and diagnoses overall and by race. To describe the association between race-level characteristics, such as size and environmental conditions, and incidence rate, we used linear regression with log transformed incidence rate as the dependent variable, as incidence rate is not normally distributed. We investigated potential non-linear associations by including a quadratic term for each predictor. Race-level predictors included ambient temperature in degrees Celsius (°C), relative humidity (%), wet bulb globe temperature in °C, and race size. The quadratic terms for each predictor were not significant and did not suggest non-linear associations between predictors and log of injury rate, and thus were not included in the final models. The analyses of temperature and relative humidity were weighted by the race size, and were conducted using the start time environmental conditions. We did this separately for overall events, for exertional heat stroke, and for heat-related illness that did not qualify as exertional heat stroke. Finally, we generated descriptive statistics on participant characteristics (age, sex, finishing quintile) and encounters (diagnosis and disposition).
Results
Weather conditions:
Weather conditions at the start of each race are displayed in Table 1.
Race Characteristics:
There was a total of 90,265 finishers across 19 races. Individual race sizes are presented in Table 1. See Table, Supplemental Digital Content 4 for additional details of location, season, start time, course layout and participants.
Medical Encounters.
There were 562 medical encounters in 90,265 finishers for an incidence of 6.2 encounters per 1000 finishers (95% CI 5.7, 6.8). The medical encounter incidence for each race is presented in Table 1. Race size was associated with an increased incidence of medical encounters. The log of the race injury rate increased by approximately 0.087 for every additional 500 race finishers, which translates to an increased event rate of approximately 0.36 per 1000 runners for each additional 500 finishers (r-squared for race size was 0.25, p=0.03; Figure 1). Increases in wet bulb globe temperature and relative humidity were associated with small positive increases in medical encounters (p=NS), and the r-squared for wet bulb globe temperature was 0.05 (p = 0.35), and relative humidity was 0.10 (p = 0.20), respectively.
Figure 1: Relationship between race size and medical encounters.
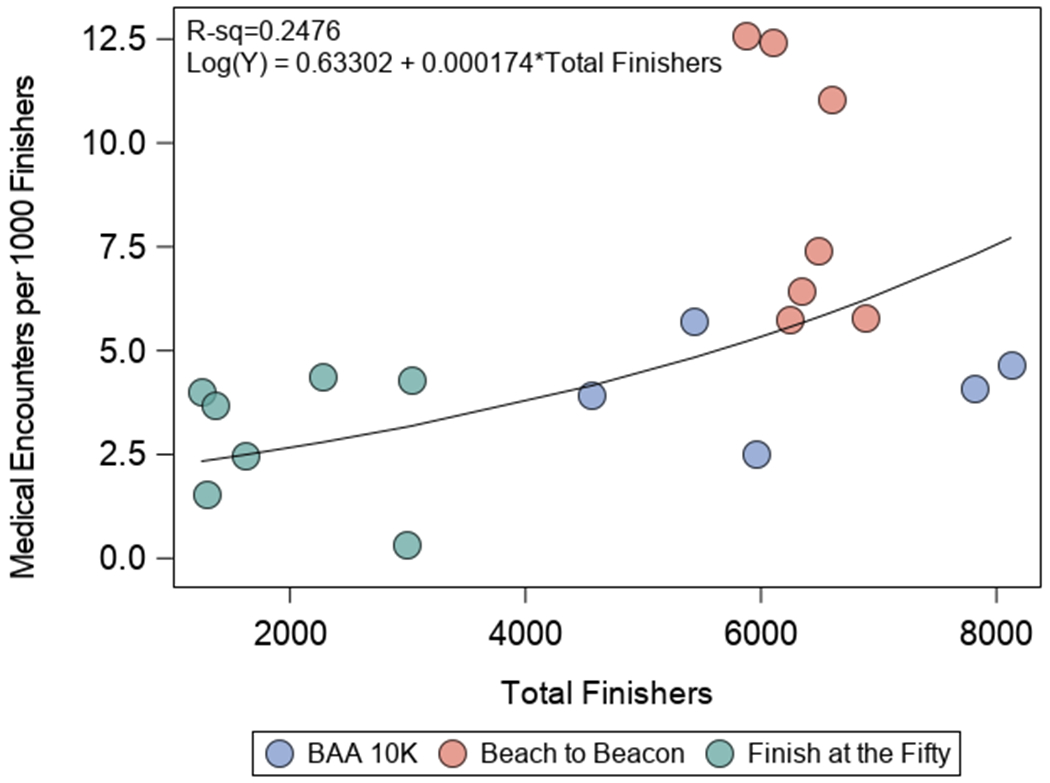
Total finishers is along the x-axis and medical encounters per 1000 finishers is along the y-axis. Each circle represents one race, with different color circles representing different events: blue is BAA 10-km; red is Beach to Beacon; green is Finish at the 50. Race size was associated with an increased incidence of medical events. There was an increased event rate per 1000 runners of approximately 0.36 per additional 500 finishers (p=0.03).
Of the 562 medical encounters in the tent, 494 runners (87.9%) finished their race prior to receiving care in the tent. The mean age of runners in the tent was 38 years, with a range of 14 to 90 years old. 55.9% were female (314 runners). For all common diagnoses, runners with finishing times in the first quintile and in the fifth quintile had greater representation in the medical tent than mid-pack runners (Figure 2).
Figure 2: Distribution of runners (%) into performance quintiles for common diagnoses in the 10-km medical tent.
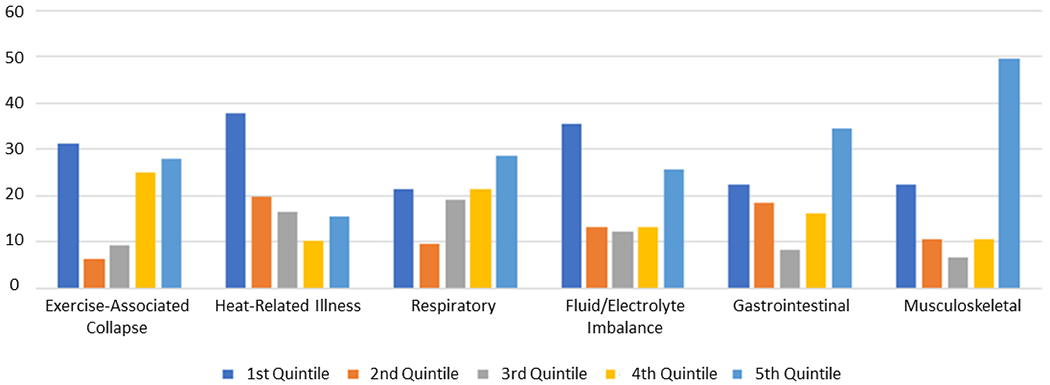
High percentages of first quintile finishers presented with heat-related illness, fluid-electrolyte imbalances or exercise-associated collapse. Fifth quintile finishers more commonly presented with musculoskeletal or gastrointestinal complaints.
Temperature-related illness was documented in 144 runners (1.6 per 1000 finishers). Two runners (0.02 per 1000 finishers) had hypothermia, 142 runners (1.6 per 1000 finishers) had hyperthermia, and 94 runners (1.0 per 1000 finishers) were diagnosed with exertional heat stroke. There was a modest, positive relationship between wet bulb globe temperature and exertional heat stroke encounters (r-squared for wet bulb globe temperature was 0.13, p=0.13; Figure 3) and heat-related illness (r-squared for wet bulb globe temperature was 0.07, p=0.27; see Figure, Supplemental Digital Content 5). The incidence of exertional heat stroke for each race is presented in Table 1. There were 57 cases of exertional heat stroke in males compared to 37 cases in females; incidence rates are shown in Table 2. The mean initial body temperature was approximately 41.2 °C for both sexes (range 39.4°C-42.8°C, SD 0.7°C). All runners diagnosed with exertional heat stroke were treated with ice water immersion, and the average time immersed was 16 minutes (range 5-60 minutes, SD 8.3 minutes). Though the presence of mental status changes was not recorded for all patients with exertional heat stroke, among those with this information recorded, more than half were noted to exhibit mental status changes on their medical encounter forms.
Figure 3: Relationship between Wet Bulb Globe Temperature and Exertional Heat Stroke.
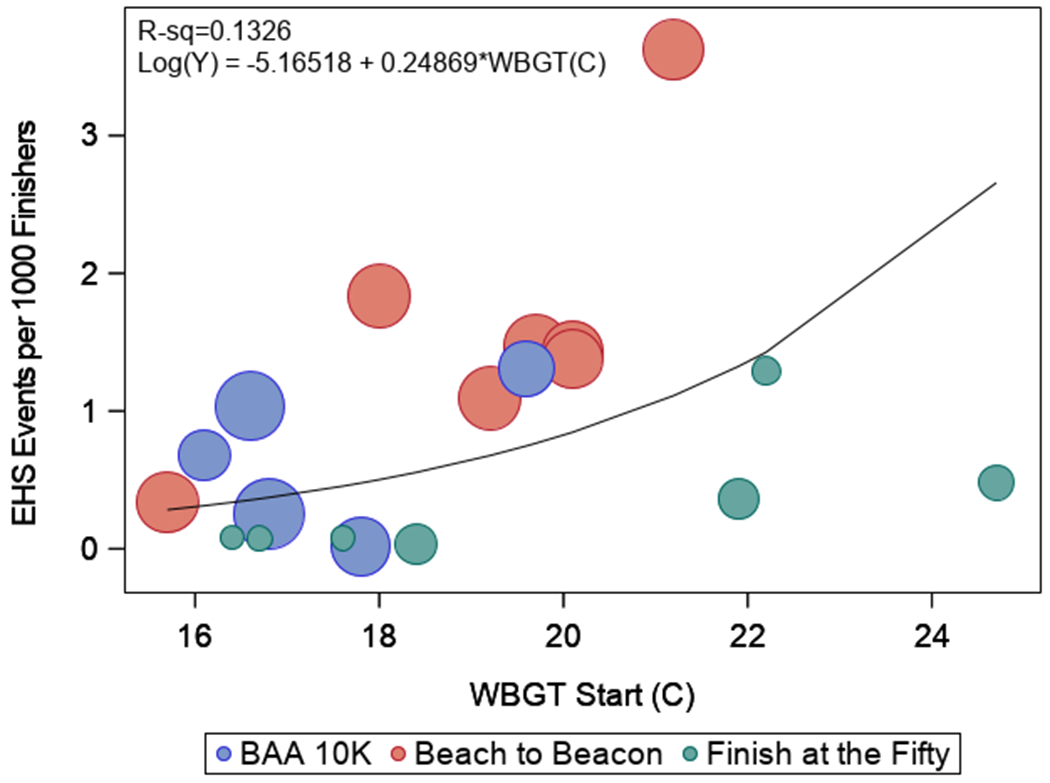
Wet Bulb Globe Temperature (°C) is along the x-axis and exertional heat stroke encounters per 1000 finishers is along the y-axis. Each circle represents one race, with different color circles representing different events: blue is BAA 10-km; red is Beach to Beacon; green is Finish at the 50. Circle diameters are proportional to race size. There was a small positive, but not significant, association between wet bulb globe temperature and exertional heat stroke events. WBGT Wet Bulb Globe Temperature; EHS Exertional Heat Stroke.
Table 2:
Common Finish Area Diagnoses
| Diagnosis | BAA 10K | F50 | B2B | Male | Female | Overall |
|---|---|---|---|---|---|---|
| Heat (EHS) | 1.1 (0.6) | 0.4 (0.3) | 2.3 (1.6) | 1.8 (1.4) | 1.5 (0.7) | 1.6 (1.0) |
| Musculoskeletal | 0.9 | 0.9 | 1.6 | 1.2 | 1.3 | 1.3 |
| Fluid/Electrolyte | 0.5 | 0.6 | 1.8 | 1.3 | 1.1 | 1.2 |
| Gastrointestinal | 0.3 | 0.2 | 1.1 | 0.6 | 0.7 | 0.7 |
| Respiratory | 0.4 | 0.3 | 0.6 | 0.3 | 0.6 | 0.5 |
| EAC | 0.1 | 0 | 0.9 | 0.4 | 0.5 | 0.5 |
| Dermatologic | 0.1 | 0.3 | 0.3 | 0.2 | 0.2 | 0.2 |
| Cardiac | 0.1 | 0 | 0.1 | 0.1 | 0.1 | 0.1 |
Incidence rates are expressed as medical encounters per 1000 finishers.
BAA Boston Athletic Association; F50 Finish at the 50; B2B Beach to Beacon; Heat Heat-Related Illness; EHS Exertional Heat Stroke; EAC Exercise-Associated Collapse
Diagnoses:
The common finish area diagnoses are presented in Table 2.
Treatment and Disposition.
Table 3 details the most common resources and treatments used in the finish line medical tent.
Table 3:
Resources and treatments used in the 10-km medical tent
| Diagnosis | Treatment/Resource | N | N/1000 |
|---|---|---|---|
| Heat | Ice Water Immersion | 94 | 1.0 |
| Observation | 36 | 0.4 | |
| Ice Packs | 12 | 0.1 | |
| Musculoskeletal | Observation | 29 | 0.3 |
| Massage | 18 | 0.2 | |
| Ace/Coban Wrap | 8 | 0.1 | |
| Splint | 1 | 0 | |
| Dehydration | Water | 78 | 0.9 |
| Observation | 14 | 0.2 | |
| Normal Saline | 11 | 0.1 | |
| Sports Drink | 9 | 0.1 | |
| Gastrointestinal | Observation | 39 | 0.4 |
| Water | 23 | 0.3 | |
| Normal Saline | 3 | 0 | |
| Sports Drink | 2 | 0 | |
| Antiemetic | 1 | 0 | |
| Respiratory | Observation | 33 | 0.4 |
| Bronchodilator | 13 | 0.1 | |
| EAC | Observation | 40 | 0.4 |
| Advanced Medical Care | 1 | 0 | |
| Dermatologic | Blister Care | 19 | 0.2 |
| Observation | 1 | 0 | |
| Cardiac | Observation | 6 | 0.1 |
| Electrocardiogram | 5 | 0.1 |
N Number; N/1000 Number per 1000 finishers; Heat Heat-related illness; EAC Exercise-associated collapse
Overall, 22 runners (0.2 per 1000 finishers) required transport from the medical tent to area hospitals; 9 runners (0.2 per 1000 finishers) at Beach to Beacon races, 8 runners (0.3 per 1000 finishers) at BAA 10-km races and 5 runners (0.4 per 1000 finishers) at Finish at the 50 races. Twelve runners were transported for exertional heat stroke. One runner was transported for electrocardiogram changes and chest pain, 1 for supraventricular tachycardia and respiratory distress, and 1 for tongue and throat swelling. The remaining transport reasons were: dehydration (3 runners), syncope (2 runners), musculoskeletal injury (1 runner) and altered mental status (1 runner). There were no fatalities.
Discussion
In the nineteen 10-km races we examined, the most common diagnosis was heat-related illness, followed by musculoskeletal complaints and fluid/electrolyte imbalances. We found that larger races were characterized by increased medical event rates overall, and that higher wet bulb globe temperatures may be associated with small positive increases in medical encounter rates. Supportive care, basic first aid, and oral rehydration were the most common treatments. Though 1.0 per 1000 finishers were diagnosed with exertional heatstroke and required ice water immersion, there were low rates of hospital transport and no fatalities.
We report a cumulative incidence of 6.2 medical encounters per 1000 finishers, which is similar to the incidence of medical encounters at the Army 10-miler road race (3.8 per 1000 entrants) (16). Roberts’ study of 12 years of medical injury and illness at the Twin Cities Marathon reports higher rates of medical encounters (25.3 per 1000 finishers), though medical diagnoses other than skin and musculoskeletal injuries occurred at a rate of 13.7 per 1000 entrants (3). Non-marathon distance road races might be expected to generate lower numbers of medical tent encounters than longer endurance races on the basis of the shorter duration of risk exposure. However, our study shows that other factors, such as larger race size, can also influence medical tent encounter rates. The smaller Finish at the 50 races had the lowest incidence of medical encounters, whereas the larger Beach to Beacon races had higher medical encounter rates than would be expected on the basis of the other included races. It is possible that larger races with more substantial budgets, regardless of race distance, may have more readily accessible medical facilities that are more clearly marked and better publicized to runners. They may have more volunteers to direct them there, thus increasing the number of runners presenting to the tent regardless of the risks of the race itself. Other potential influencing factors include race location, topography, season and start time. Experience level and participants’ acclimatization to heat may also play a role in these differences.
Female sex has previously been associated with a higher risk of some medical complications during road races: for example, Schwabe et al. found that older female runners in a 21-km race were more likely to develop postural hypotension and dermatologic complications (17). In our study, female runners had higher incidence rates for most diagnoses, likely reflecting the slightly greater number of overall female participants. However, a disproportionately high number of runners presenting with respiratory complaints were female: 0.6 per 1000 female finishers compared to 0.3 per 1000 male finishers. In contrast, exertional heat stroke was less common in females: it occurred at a rate of 0.7 per 1000 female finishers, versus 1.4 per 1000 male finishers. Identifying groups at greater risk for specific conditions can help inform future planning and preventative practices.
We found that front-runners and back-of-the-pack runners presented to the medical tent in greater percentages than mid-packers. High percentages of first quintile finishers presented with heat-related illness, fluid-electrolyte imbalances or exercise-associated collapse, illustrated in Figure 2. As discussed by St Clair Gibson et al., failure of physiologic and psychologic regulatory mechanisms during exercise, or a strong psychological drive to override them, can lead to collapse (18). Higher performing first quintile runners with ambitious finishing time goals may have been more motivated to ignore warning signs of conditions leading to collapse, resulting in higher incidence rates among this group. Common diagnoses among fifth quintile finishers included musculoskeletal, dermatologic or gastrointestinal complaints, which may reflect the longer duration race effort by these slower finishers. The race with the lowest medical encounter rate, the Finish at the 50, was also the only race without elite runners. While these data do not allow us to disentangle race effects (e.g. size, topography) from the potential effects of runner experience and performance, this is an important question for future research.
Our findings also show that on-site medical care at a 10-km road race must include adequate staffing and resources to manage exertional heat stroke. Though our overall rate of exertional heat stroke cases was lower than that of the Falmouth Road Race experience – 1.0 per 1000 finishers in our study versus 2.13 per 1000 runners reported at Falmouth (8) – exertional heat stroke posed a significant burden on medical tent personnel at our races. At Falmouth, the coastal location, late start time, and slightly longer distance may have contributed to the higher incidence. However, the three 10-km events in our study share a potential risk with Falmouth: metabolic rates are the key variable in determining the degree of post-race core body temperature elevation (19), and shorter distance races allow participants to run at a high intensity for the duration of the race (8). This suggests that the 10-km race distance may be inherently risky for exertional heat stroke, which should be considered by race directors and medical coordinators planning medical care at these events.
We found small, though not statistically significant, associations between start time wet bulb globe temperature and exertional heat stroke or heat-related illness. As this would predict, many cases of heat-related illness occurred during races run in either less than ideal (Yellow) conditions or potentially dangerous (Red) conditions. However, 26 of the 142 cases, including 15 exertional heat stroke cases, occurred during races in which conditions were considered good (Green). Roberts has shown that standard race cancellation guidelines may not always be appropriate for individual races (20). At the Twin Cities Marathon, start wet bulb globe temperatures of greater than 13°C resulted in increased numbers of medical tent encounters and on-course marathon dropouts, even though by International Institute for Race Medicine alert standards, races held at start wet bulb globe temperatures of 14°C to 18°C would have been considered safe. In another recent case series detailing 3 years’ experience at the Flying Pig Marathon and Half-Marathon, where weather conditions were temperate (an average of 18.1 °C, 64.6 °F), 26 runners presented with exertional heat stroke for an incidence of 5.64 per 10,000 runners (21). In our study, Finish at the 50 races held in Green conditions did not have runners with exertional heat stroke, though some BAA 10-km and Beach to Beacon races held in Green conditions had multiple runners with exertional heat stroke (Table 1). For example, at the BAA 10-km 2016, where the wet bulb globe temperature was a “low-risk” 16.6°C, 8 runners presented with exertional heat stroke. This supports the suggestion by Roberts that races should calculate their own wet bulb globe temperature “do not start” thresholds on the basis of previous data and experience of a given race (20).
Most runners in our study were treated with basic resources. Those with musculoskeletal complaints were most often treated supportively, and few required splints or wraps. Only 14 of 90,265 finishers required intravenous normal saline; the remainder of those with dehydration or gastrointestinal complaints were treated with water and/or sports drink. For those runners who presented with respiratory complaints, about one-third required treatment with a bronchodilator (13/43, 30.2%). Based on these data, we recommend in addition to water, sports drink and basic first aid supplies, a 10-km finish line medical tent should be prepared with the following key resources per 1000 runners: 1-2 ice water immersion tubs, 1 liter intravenous normal saline and intravenous kit, 1 dose antiemetic, 1 bronchodilator inhaler, and 1 portable electrocardiogram machine.
A major limitation of our study was the high level of incomplete documentation. We encountered inadequate documentation regarding diagnosis in 10% of medical encounter forms, and more than 36% of medical encounter forms lacked information on final disposition of runners who sought care in the tent. Individual medical teams at each race varied in background, training and experience, and the recorded clinical information on which we based our diagnostic categories was subject to this variability. Though this has implications for interpreting our results, it also highlights the need for medical encounter forms that can be filled out accurately and completely. A recently published consensus statement establishing standards for medical encounter forms at mass participation events describes optimal medical encounter data collection methods and presents a standardized race medical encounter data form (R-MED) for use in the road race medical tent (22). Implementation of standardized forms such as the R-MED will address documentation problems such as those encountered in our study.
Efforts aimed at optimizing on-site medical care at road races are integral to the success and feasibility of these events. This is highlighted by Jena et al.’s study of emergency care and mortality during major US marathons from 2002 through 2012 (23). This study found longer ambulance transport times and higher 30-day mortality rates in Medicare beneficiaries admitted to marathon-affected hospitals with acute myocardial infarction or cardiac arrest on marathon dates when compared with admissions for the same complaints on non-marathon dates. The findings of our study suggest the volume of serious injury and illness are lower for 10-km races and may not have the same impact on community medical resources as a marathon. However, it is clear that medical preparedness on-site at a road race of any distance not only protects race participants with serious medical issues, but also benefits the community at large by reducing the need for hospital transport from the event and emergency room service utilization by race participants. Future education and training should be standardized according to best practices with goals of bolstering the self-sufficiency of the on-site medical tent and minimizing the impact of a large road race on the surrounding community.
Conclusions:
In 10-km road races, injury rates are low compared to longer races in similar weather conditions. Common medical issues can be managed with basic resources in the on-site medical tent. Green flag start race conditions may not predict race safety with regard to exertional heat stroke risk. There were no deaths in nearly 100,000 finishers.
Supplementary Material
Acknowledgements:
Supported in part by NIH-P30AR072577 (J.N.K.) and the Rheumatology Research Foundation (J.E.C.). The authors gratefully acknowledge the editorial assistance of Angela T. Chen. We would also like to thank the many medical volunteers at the BAA 10-km, Finish at the 50 and Beach to Beacon races, and especially Pierre d’Hemecourt, Sophia Dyer, Aaron Baggish, Eric Berkson, Mylan Cohen, and Michael Baumann.
Footnotes
Conflict of interest:
The authors report no conflicts of interest. The results of the present study do not constitute endorsement by the American College of Sports Medicine. These results are presented clearly, honestly, and without fabrication, falsification, or inappropriate data manipulation.
References
- 1.USA, Running. U.S. Road Race Participation Numbers Hold Steady for 2017. [Internet]. 2018. [cited 2019 Jan 29]. Available from: www.runningusa.org/RUSA/Research/Recent_Reports/Road_Race_Trends
- 2.Yao KV, Troyanos C, D’Hemecourt P, Roberts WO. Optimizing Marathon Race Safety Using an Incident Command Post Strategy: Curr Sports Med Rep. 2017;16(3):144–9. [DOI] [PubMed] [Google Scholar]
- 3.Roberts WO. A 12-yr profile of medical injury and illness for the Twin Cities Marathon: Med Sci Sports Exerc. 2000. September;1549–55. [DOI] [PubMed] [Google Scholar]
- 4.Ewert GD. Marathon Race Medical Administration: Sports Med. 2007;37(4):428–30. [DOI] [PubMed] [Google Scholar]
- 5.Glick J, Rixe J, Spurkeland N, Brady J, Silvis M, Olympia RP. Medical and Disaster Preparedness of US Marathons. Prehospital Disaster Med. 2015. August;30(04):344–50. [DOI] [PubMed] [Google Scholar]
- 6.USA, Running. 2016 State of the Sport - US Road Race Trends [Internet]. 2016. [cited 2018 Feb 4]. Available from: www.runningusa.org/state-of-sport-us-trends-2015
- 7.USA, Running. Running USA Largest Races Report [Internet]. 2016. [cited 2019 Jan 29]. Available from: runningusa.org/RUSA/Research/Recent_Reports/Largest_Road_Races
- 8.DeMartini JK, Casa DJ, Belval LN, Crago A, Davis RJ, Jardine JJ, et al. Environmental Conditions and the Occurrence of Exertional Heat Illnesses and Exertional Heat Stroke at the Falmouth Road Race. J Athl Train. 2014;49(4):478–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Demartini JK, Casa DJ, Stearns R, Belval L, Crago A, Davis R, et al. Effectiveness of Cold Water Immersion in the Treatment of Exertional Heat Stroke at the Falmouth Road Race: Med Sci Sports Exerc. 2015. February;47(2):240–5. [DOI] [PubMed] [Google Scholar]
- 10.England AC. Preventing Severe Heat Injury in Runners: Suggestions from the 1979 Peachtree Road Race Experience. Ann Intern Med. 1982. August 1;97(2):196. [DOI] [PubMed] [Google Scholar]
- 11.Armstrong LE, Casa DJ, Millard-Stafford M, Moran DS, Pyne SW, Roberts WO. Exertional Heat Illness during Training and Competition: Med Sci Sports Exerc. 2007. March;39(3):556–72. [DOI] [PubMed] [Google Scholar]
- 12.Jenks G Prevention of heat injuries during distance running: A position statement from The American College of Sports Medicine. J Sports Med. 1975;3(4):194–6. [PubMed] [Google Scholar]
- 13.Hosokawa Y, Adams WM, Belval LN, Davis RJ, Huggins RA, Jardine JF, et al. Exertional heat illness incidence and on-site medical team preparedness in warm weather. Int J Biometeorol. 2018. July;62(7):1147–53. [DOI] [PubMed] [Google Scholar]
- 14.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009. April;42(2):377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vollset Stein. Confidence Intervals for a Binomial Proportion. Stat Med. 1993;12:809–24. [DOI] [PubMed] [Google Scholar]
- 16.Pasquina PF, Griffin SC, Anderson-Barnes VC, Tsao JW, O’Connor FG. Analysis of Injuries From the Army Ten Miler: A 6-Year Retrospective Review. Mil Med. 2013. January;178(1):55–60. [DOI] [PubMed] [Google Scholar]
- 17.Schwabe K, Schwellnus MP, Derman W, Swanevelder S, Jordaan E. Older females are at higher risk for medical complications during 21 km road race running: a prospective study in 39 511 race starters—SAFER study III. Br J Sports Med. 2014. June;48(11):891–7. [DOI] [PubMed] [Google Scholar]
- 18.St Clair Gibson A, De Koning JJ, Thompson KG, Roberts WO, Micklewright D, Raglin J, et al. Crawling to the Finish Line: Why do Endurance Runners Collapse?: Implications for Understanding of Mechanisms Underlying Pacing and Fatigue. Sports Med. 2013. June;43(6):413–24. [DOI] [PubMed] [Google Scholar]
- 19.Noakes T, Myburgh K, Du Plessis J, Lang L, Lambert M, Van Der Riet C, et al. Metabolic rate, not percent dehydration, predicts rectal temperature in marathon runners. Med Sci Sports Exerc. 1991;23(4). [PubMed] [Google Scholar]
- 20.Roberts WO. Determining a “Do Not Start” Temperature for a Marathon on the Basis of Adverse Outcomes: Med Sci Sports Exerc. 2010. February;42(2):226–32. [DOI] [PubMed] [Google Scholar]
- 21.Divine JG, Daggy MW, Dixon EE, LeBlanc DP, Okragly RA, Hasselfeld KA. Case Series of Exertional Heat Stroke in Runners During Early Spring: 2014 to 2016 Cincinnati Flying Pig Marathon. Curr Sports Med Rep. 2018;17(5):8. [DOI] [PubMed] [Google Scholar]
- 22.Schwellnus M, Kipps C, Roberts WO, Drezner JA, D’Hemecourt P, Troyanos C, et al. Medical encounters (including injury and illness) at mass community-based endurance sports events: an international consensus statement on definitions and methods of data recording and reporting. Br J Sports Med. 2019. February 22;bjsports-2018-100092. [DOI] [PubMed] [Google Scholar]
- 23.Jena AB, Mann NC, Wedlund LN, Olenski A. Delays in Emergency Care and Mortality during Major U.S. Marathons. N Engl J Med. 2017. April 13;376(15):1441–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


