Introduction
Social distancing (SD) is a powerful means of blocking the transmission of infectious diseases. However, maintaining social distance for a long period of time reduces its effectiveness and the socio-economic impact is enormous. In order to prepare for the second epidemic of the coronavirus disease 2019 (COVID-19), it is now necessary to clarify the standards for implementing and mitigating SD.
Purpose and Limitations of SD
The purpose of SD is to alleviate an infectious disease pandemic so that the number of patients does not exceed the capacity of medical institutions.1,2,3 As a result, the incidence and death of critically ill patients can be reduced. The most important goal of SD is to slow the spread of the virus and flatten the epidemic curve.2,4
There have been international outbreaks of a directly transmitted pathogen with high case fatality rates in which social distancing measures (SDMs) were not implemented. Although non-pharmaceutical public health strategies were effective at reducing morbidity and mortality, there was no systematic relationship between the duration and the impact of interventions.1 SD is difficult to maintain for a long period of time and its' effectiveness decreases as time goes on. Long-term SD breaches the limits of people's physical and mental endurance and the negative effects on socio-economics are enormous. On June 3, 2020, the government proposed a 3rd additional budget to overcome the economic crisis and prepare for a post-COVID-19 economy in Korea.5
Effects of SD in Korea
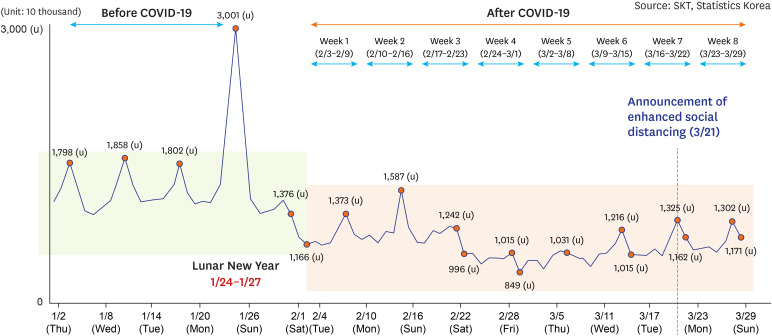
After the first COVID-19 patient in Korea,6 SD was initiated voluntarily even before the government implemented it. People chose to wear masks and refrained from going out. As can be seen from the movement analysis based on mobile big data, public movement decreased by 38.1%, the lowest level, in the 4th week of the COVID-19 outbreak (February 24–March 1), compared to the days before a confirmed COVID-19 case was identified (January 9–22) (Fig. 1). The number of daily passengers at major stations in Seoul, specifically subway line 2, also significantly reduced (Fig. 2).
Fig. 1. Daily level of personal movements based on mobile big data (No. of movements), January 2, 2020 to March 29, 2020 (from regular briefing of Central Disaster and Safety Countermeasure Headquarters on COVID-19, April 4, 2020).
COVID-19, coronavirus disease 2019.
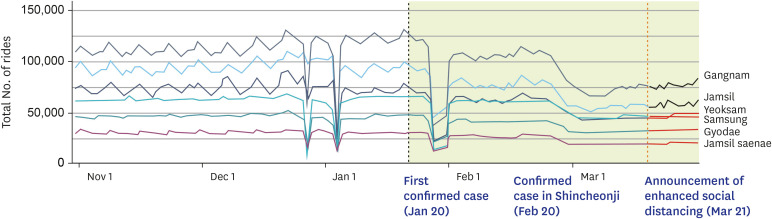
Fig. 2. Daily number of rides in major stations of Seoul Subway Line 2, November 2019 to March 2020, weekdays (from regular briefing of Central Disaster and Safety Countermeasure Headquarters on coronavirus disease 2019, April 4, 2020).
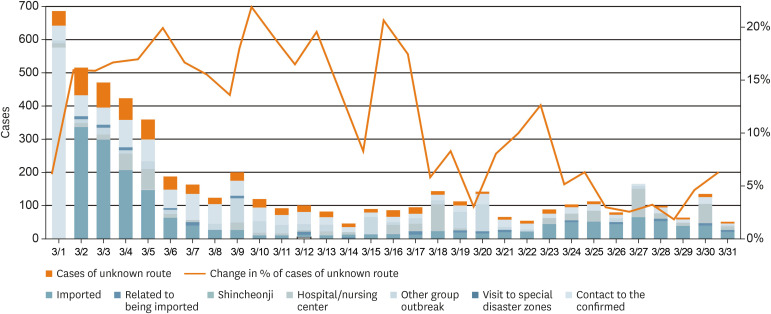
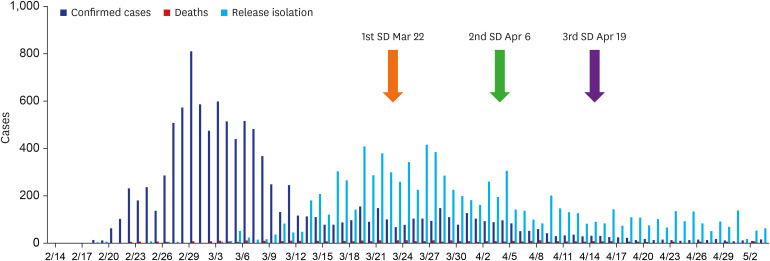
When the mass outbreak in Daegu-Gyeongbuk occurred, SD was strengthened by the people themselves and the floating population halved (Fig. 2). The Korean government first conducted SD for two weeks starting March 22, 2020, when about 100-150 COVID-19 patients occurred every day. After confirming the initial impact of SD, the government decided to prolong and strengthen SD for two more weeks. From April 6, 2020, due to the strengthened SD, the incidence of COVID-19 patients decreased to less than 100 people per day. As a result of SD, the number and percentage of confirmed persons from unknown transmission route dropped from 37 cases (19.8%) on March 6 to 3 cases (6.1%) on March 31 (Fig. 3). To increase the effectiveness of SD, the government extended SD a third time for another two weeks. Since then, the incidence rate decreased to less than 10 patients per day, and there were days without any new endemic patients (Fig. 4).
Fig. 3. Daily cases based on transmission routes, changes in the route of infection after social distancing (from regular briefing of Central Disaster and Safety Countermeasure Headquarters on coronavirus disease 2019, April 4, 2020).
Fig. 4. The effect of strengthening SD (from Korea Centers for Disease Control and Prevention, as of May 6, 2020).
SD = social distancing.
Strategies for Preventing the Failure of SD
As can be seen from its' effects, SD is a proven means of preventing and containing infectious diseases in Korea (Fig. 4 and Table 1).7 However, there are no clear standards for when and how to implement SD. Conversely, the establishment of reasonable principles and standards should also apply when alleviating SD. This is because intensive SD has high social and economic costs. Until now, SD was enforced by the government. Decisions on when and how to implement or mitigate SD should always be made from evidence, but little is based on pure evidence due to the current scientific uncertainties associated with COVID-19. Also, clear standards for SD should be based on regional community, occupation, type of business, institution and personal life, not on a uniform basis. When individuals are able to understand and accept the individual and collective standards of SD, voluntary participation may continue and SD may not fail.
Table 1. The changes of SD index comparison over two weeks - before and after extending SD.
| Index | April 5–April 18 | April 19–May 2 |
|---|---|---|
| Newly confirmed patients | 35.5 people | 9.1 people |
| Cluster outbreaks (based on newly confirmed cases) | 4 cases | 4 cases |
| Rate of infections with unidentified route | 3.6% (18/497) | 5.5% (7/127) |
| Management rate within the quarantine network | 80% or over | 80% or over |
From Regular Briefing of Central Disaster and Safety Countermeasure Headquarters on coronavirus disease 2019, May 3, 2020.
SD = social distancing.
Mitigation of SD
As of May 6, 2020, “distancing in daily life” implemented by the government, is a means of mitigating SD. The main goals of mitigation are to minimize morbidity and mortality, maintain social-economic impact at a manageable level and keep the epidemic curve flat while waiting for vaccines and treatments to be developed.4 It is difficult to achieve these mitigation objectives in a short amount of time. The government did not take steps to gradually and selectively alleviate SD while maintaining individual and collective rules. As a result, on May 5, 2020, just before the transition from “SD” to “distancing in daily life”, multiple outbreaks occurred at clubs in Itaewon, Seoul, leading to the spread in the region.
It is clear that SD should be mitigated because long-term enhanced SD is neither sustainable nor effective. The first considerations in alleviating SD are the preconditions, procedures and methods of mitigation. Prerequisites to mitigate SD should be the preparation of SD guidelines that take into account the characteristics of each individual and community. Then, it is necessary to consider the rate of community infection, the proportion of high-risk populations, the degree of close contact in social activities, preemptive blocking of external sources of infection, and preparing medical institutions and essential facilities related to livelihoods. Most importantly, the process of SD should be done step by step and selectively; the method must be a mixture of individual and collective mitigation principles.
Exit Strategy from the COVID-19 Epidemic
It is inevitable that multiple outbreaks and regional infections, where the route of infection is unknown, is a concern when alleviating the strengthened SD. Nevertheless, we need to think about an exit strategy from the epidemic. It has been five months since the epidemic has spread. We are gaining more information and experience from the virus but the initial quarantine criteria have not adapted. Numerous industrial sites have been closed by administrative orders. Except for the high-risk groups, we too need to prepare to go back to our daily lives with non-pharmaceutical interventions such as physical distancing of 1m or more, personal protective measures (hand and respiratory hygiene, cough etiquette, use of face masks) and environmental measures (routine cleaning of frequently used surfaces, clothes and objects, minimizing the sharing of objects, ensuring appropriate ventilation).3,8,9
Based on trial and error and accumulated experience over the past several months, on June 28th, the government unified ‘SD’, divided it into 3 stages according to the degree of COVID-19 spread, and announced ‘Standards and Actions for Stepping in SD', containing each standard and step-by-step measures in 3 stages.10,11 The risk assessment items for each stage include newly confirmed patients, cluster outbreaks based on newly confirmed cases, rate of infections with unidentified route, and management rate within the quarantine network. In addition to these items, the stage is shifted in consideration of regional characteristics such as intensive care unit capacity, medical system capabilities, and distribution of high-risk facilities and population, as well as social costs. These policies can be applied differently in different regions. In fact, on July 2nd, with the rapid increase of infected people in the community, the stage II policy was applied in some areas due to high concern about group infection. It can be seen as an advanced strategy compared to the strengthened SD that was applied uniformly, regardless of the region, during the earlier stages of quarantine (Table 2).
Table 2. Stepwise enhancement or loosening of SD measures according to level of risk assessment index.
| Index (last 2 weeks) | SD | ||
|---|---|---|---|
| Stage I | Stage II | Stage III | |
| No. of newly confirmed patients (mainly focus on community) | Less than 50 | 50 to less than 100 | 100–200 or more or doublinga occurs twice a week |
| Rate of infections with unidentified route | Less than 5% | - | Sharp increase |
| No. of cluster outbreaks (based on newly confirmed cases) | Reduction or suppression | Continuous increase | Sharp increase |
| Management rate within the quarantine network | 80% or over | - | - |
SD = social distancing.
aMore than twice the number of confirmed patients per day occurs twice or more within a week.
Many countries currently prohibit foreigners from entry into their countries. For the countries that do not prohibit foreigners' entry, quarantine measures are carried out along with 14 days of mandatory self-isolation quarantine. Thus, a strong containment policy is in effect. As with SD however, step-by-step standards are needed and the 14 days self-isolation/quarantine standards should be relaxed and applied with adjustments because we now have more information about the COVID-19 infection and spread than when COVID-19 first appeared. Using COVID-19 information and test results, it is necessary to examine closely whether 5 to 7 days of self-isolation/quarantine is sufficient, instead of 14 days. Self-quarantine data of travelers who have entered Korea should also be analyzed. Considering the asymptomatic incubation period and early infectivity of COVID-19 patients, foreigners' self-isolation can be reduced to less than 7 days if re-testing is done after 4 days from the time of entry. It is necessary to refer to the infection rate and current symptoms of the traveler's country of departure. Using all the information we have of the COVID-19 virus so far, we must begin the ‘new normal’ era.
In order for the SD policy to succeed without failing, it is necessary to disclose information that leads to voluntary participation of the people, to inform about policy changes in real time, and to educate about the adverse outcomes that will occur if not followed. Also, in the current situation of the ever-increasing infection rate around the world, international travel cannot be blocked unconditionally, but stricter immigration control will help people believe and follow government policies.
It is easy to say that SD should be strengthened and continuing with this policy is a way to avoid responsibility. On the other hand, mitigating SD is difficult to initiate, complicated to apply, and requires responsibility. People do not want to live on emergency disaster relief funds. We need an exit strategy from the COVID-19 epidemic.
Footnotes
Disclosure: The authors have no potential conflicts of interest to disclose.
- Conceptualization: Yum HK.
- Writing - original draft: Park IN.
- Writing - review & editing: Yum HK.
References
- 1.Hollingsworth TD, Klinkenberg D, Heesterbeek H, Anderson RM. Mitigation strategies for pandemic influenza A: balancing conflicting policy objectives. PLoS Comput Biol. 2011;7(2):e1001076. doi: 10.1371/journal.pcbi.1001076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Qualls N, Levitt A, Kanade N, Wright-Jegede N, Dopson S, Biggerstaff M, et al. Community mitigation guidelines to prevent pandemic influenza - United States, 2017. MMWR Recomm Rep. 2017;66(1):1–34. doi: 10.15585/mmwr.rr6601a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fong MW, Gao H, Wong JY, Xiao J, Shiu EY, Ryu S, et al. Nonpharmaceutical measures for pandemic influenza in nonhealthcare settings-social distancing measures. Emerg Infect Dis. 2020;26(5):976–984. doi: 10.3201/eid2605.190995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anderson RM, Heesterbeek H, Klinkenberg D, Hollingsworth DT. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet. 2020;395(10228):931–934. doi: 10.1016/S0140-6736(20)30567-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ministry of Economy and Finance. 3rd supplementary budget proposal of 2020. [Updated 2020]. [Accessed July 7, 2020]. http://english.moef.go.kr/pc/selectTbPressCenterDtl.do?boardCd=N0001&seq=4914.
- 6.Yoo JH, Hong ST. The outbreak cases with the novel coronavirus suggest upgraded quarantine and isolation in Korea. J Korean Med Sci. 2020;35(5):e62. doi: 10.3346/jkms.2020.35.e62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yum HK. Suggestions to prepare for the second epidemic of COVID-19 in Korea. J Korean Med Sci. 2020;35(19):e191. doi: 10.3346/jkms.2020.35.e191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.European Centre for Disease Prevention and Control. Guidelines for the Use of Non-pharmaceutical Measures to Delay and Mitigate the Impact of 2019-nCoV. Stockholm: European Centre for Disease Prevention and Control; 2020. [Google Scholar]
- 9.Chu DK, Akl EA, Duda S, Solo K, Yaacoub S, Schünemann HK, et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020;395(10242):1973–1987. doi: 10.1016/S0140-6736(20)31142-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ministry of Health and Welfare. Coronavirus infectious diseases-19 central disaster safety response headquarters regular briefing. [Updated 2020]. [Accessed July 7, 2020]. http://www.mohw.go.kr/react/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&page=6&CONT_SEQ=355170.
- 11.Yoo JH. Social distancing and lessons from Sweden's lenient strategy against corona virus disease 2019. J Korean Med Sci. 2020;35(27):e250. doi: 10.3346/jkms.2020.35.e250. [DOI] [PMC free article] [PubMed] [Google Scholar]