Abstract
Objective:
To examine how the deprivation level of the community in which one lives influences discharge disposition and the odds of 90-day readmission after elective THA.
Methods:
We performed a retrospective cohort study on 84,931 patients who underwent elective THA in the Pennsylvania Health Care Cost Containment Council database from 2012 to 2016. We used adjusted binary logistic regression models to test the association between community ADI and patient discharge destination as well as 90-day readmission. We included an interaction term for community ADI and patient race in our models to assess the simultaneous effect of both on the outcomes.
Results:
After adjusting for patient and facility level characteristics, patients from high ADI (most disadvantaged) communities, compared to patients from low ADI (least disadvantaged) communities, were more likely to be discharged to an institution as opposed to home for post-op care and rehab (age <65: aOR = 1.47; age ≥65; aOR = 1.31; both p<0.001). The interaction effect of patient race and ADI on discharge destination was statistically significant in those ≥ 65 years of age, but not in patients < 65 years. The association of ADI on 90-day readmission was not statistically significant.
Conclusions:
In this statewide sample of patients who underwent elective THA, the level of deprivation of the community in which patients reside influences their discharge disposition, but not their odds of 90-day readmission to an acute care facility.
Hip osteoarthritis (OA) is a leading cause of chronic pain and disability in the elderly worldwide,1,2 and its incidence is increasing even in younger populations.3 Elective total hip arthroplasty (THA) is an effective treatment option for advanced hip OA and one of the fastest growing procedures in the United States (US). By 2030, THA utilization in the US is projected to grow to 572,000 procedures per year.4
Numerous studies demonstrate marked variations in the use, outcomes, and costs of elective THA. Besides racial and ethnic disparities in utilization and outcomes of THA,5-8 geographic variations in utilization are also documented.9 There is evidence that social determinants of health such as socioeconomic status may influence joint replacement utilization and outcomes.10-12 Social determinants of health are the economic and social conditions that influence individual and group differences in health status.13 There are also substantial variations in THA costs, and post-discharge costs represent a sizeable portion of this.14
The reasons for variations in THA utilization, outcomes, and costs are multiple, complex, and compounded by substantial variation in post-THA discharge disposition. These include clinical and social factors, patient preference, primary insurance status, reimbursement policy, and bundled payments amongst many others. Post-discharge costs after THA have been frequently ignored despite being a considerable portion of the total episode payment and having significant variation.15,16 THA patients are typically discharged to one of four settings for post-operative and rehabilitative care: (1) a skilled nursing facility (SNF), (2) an inpatient rehabilitation facility (IRF), (3) home with home care services, or (4) home without home care services. This discharge decision is a leading source of cost variation in THA.17,18 As a result, the Centers for Medicare and Medicaid Services (CMS) have targeted THA for payment reform models such as bundled payments to reduce this variation.
In a previous analysis, we found significant variation in post-THA discharge disposition by patient race.19 There is increasing evidence that social determinants of health, including community characteristics, might independently impact healthcare utilization and decision-making. 20,21 However, little is known about the relationship between community socioeconomic status, which is an important measure in other health outcomes,22 with post-THA discharge disposition and patient outcomes.
Therefore, the primary objective of this analysis was to determine whether there is an association between the socioeconomic status of the community in which patients reside and their discharge disposition for post-operative care and rehabilitation after elective THA. Our primary hypothesis was that compared to patients from affluent communities, those from impoverished communities are more likely to be institutionalized for post-op care and rehab.
Materials Methods:
Sample
We performed a retrospective cohort study of all eligible THA cases in the Pennsylvania Health Care Cost Containment Council (PHC4) Database from 2012-2016. PHC4 is an independent state agency formed under Pennsylvania statute to address increasing health care costs. Each year, PHC4 collects de-identified patient demographic data, diagnostic and procedural codes, discharge disposition, and outcomes and cost data for over 4.5 million procedures performed in 170 non-governmental inpatient, ambulatory, and freestanding surgery centers located in Pennsylvania. We identified all PCH4 patients who underwent elective primary THA using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) procedure code 81.51 for primary THA from January 1, 2012 through September 30, 2015, and ICD-10 procedure codes 0SR90xx or 0SRB0xx thereafter. These are validated codes from the American Joint Replacement Registry with a sensitivity of 99%, specificity of 91%, and positive predictive value of 91%.23,24 This study cohort and methodology were previously described in detail.25
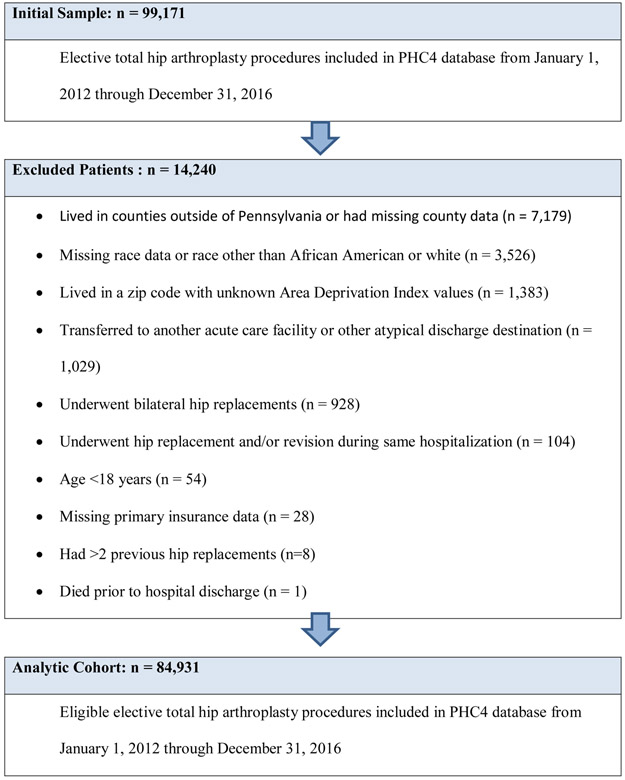
From 99,171 THA records in PHC4, we included 84,931 elective THA procedures performed in the State of Pennsylvania from January 1, 2012 through December 31, 2016. We excluded 14,240 procedures performed on patients who: (1) lived in counties outside the state or had missing county data (n=7,179); (2) had missing race data or race other than African American or white (n=3,526); (3) lived in a zip code with unknown Area Deprivation Index values (n=1,383); (4) were transferred to another acute care facility or other atypical discharge destination (n=1,029); (5) underwent bilateral hip replacements (n=928) or hip replacement and revision during the same hospitalization (n=104); (6) were <18 years of age (n=54); (7) had missing primary insurance data (n=28); (8) had >2 previous hip replacements (n=8); or (9) died prior to hospital discharge (n=1) (Figure 1).
Figure 1.
Sample flow chart and cohort selection
Study Variables:
Exposure variable
Our primary exposure variable was Area Deprivation Index (ADI), a validated measure of neighborhood socioeconomic disadvantage.26, 27 Previous studies assessed neighborhood socioeconomic status based on average household income in a specific community, but could not identify households above the specified income levels that experience poverty-level standards of living, or households below the specified income level that have above-poverty standards of living.28 The ADI encompasses the theoretical domains of income, education, employment, and housing quality, thus providing a more finely tuned assessment of standard of living at the household level. The ADI we used for our analyses was constructed using 2013 American Community Survey (ACS) 5-Year Estimates, representing a 5-year average of ACS data obtained from 2008-2013.
ADIs are ranked in deciles from 1 to 10 for each individual state. An ADI value of 1 is the lowest ADI (least disadvantaged) and 10 is the highest ADI (most disadvantaged). Each 9-digit zip code in Pennsylvania has an ADI ranking. In order to integrate ADI data for our study cohort, we calculated a single ADI value for each 5-digit zip code in Pennsylvania by averaging all 9-digit zip code ADI values within their respective 5-digit zip code areas.22 Once the 5-digit zip code level indices were constructed and linked to the PHC4 dataset, we further categorized each index into 3 ordinal groups for regression analyses: low (within lower quartile- 25th percentile), middle (within quartiles 2 and 3), and high disadvantaged group (within upper quartile- 75th percentile).
Outcome measures
Our primary outcome of interest was discharge disposition following elective THA surgery. We dichotomized discharge to home (home with home health care [HH] or home with self-care [Home]) and institution (inpatient rehabilitation facility [IRF] and skilled nursing facility [SNF]). In all analyses, discharge to home was used as the reference category. We also examined odds of 90-day readmission to an acute care hospital as our secondary outcome of interest. The dataset captures all Pennsylvania-based readmissions within 90 days after the primary procedure.
Study Covariates
We extracted data for important covariates such as race, age, sex, primary health insurance (commercial, Medicaid, Medicare or other government-sponsored program, uninsured), and clinical- and facility-level variables from PCH4. We incorporated two facility-level variables (metro area status and volume of THA procedures) to characterize the facilities where the patients underwent THA. We used the 2013 US Department of Agriculture’s Rural-Urban Continuum Codes to assign the Metro area status to each hospital.29 Hospital THA procedure volume was categorized into three ordinal groups based on the number of procedures performed annually (<100, 100-199, and ≥200). In-hospital post-operative complications including myocardial infarction, prosthetic device complication, surgical wound infection, and venous thromboembolism were identified using ICD-9/10 codes (Appendix Table 1). Lastly, medical comorbidities were identified using the Quan adaptation of the Elixhauser Comorbidity index.30,31 The same covariates from the primary outcome analysis were included in the multivariable logistic models for 90-day readmission. The study methods and results are described in accordance with the Strengthening of Reporting in Observational studies in Epidemiology (STROBE) guideline for cohort studies.32 The study was deemed exempt from Institutional Review Board review by Weill Cornell Medicine.
Statistical Analyses:
We compared patient and facility characteristics, along with complications, by ADI levels (low, middle, high) separately for patients <65 years of age, and those ≥ age 65. We did so since at the age of 65, a lot of patients qualify for Medicare insurance and thus account for assess differences. We used Generalized Estimating Equations (GEE) to test the association between ADI and discharge disposition, accounting for clustering by facility. The adjusted model accounts for the following covariates: patient age, sex, primary insurance, Elixhauser Comorbidity index (a widely used measure of baseline comorbidity), in-hospital surgical complications and facility metro status, and volume of cases. Odds ratios of being discharged to institution given a high ADI value, compared to patients with a low ADI value (reference category) for unadjusted and adjusted models were estimated. The interaction effect of race and ADI was also estimated in separate models.
We also used GEE to test the association between ADI and 90-day readmissions, accounting for clustering by hospital facility. The covariates included in the adjusted model are the same as those included in the primary outcome analysis, along with discharge disposition (institution vs. home). The interaction effect of race and ADI was also estimated in separate models.
Data management and analyses were conducted using R.3.5.1 in RStudio (version 1.1.463, RStudio, Inc., Boston, MA). Geocoded data were mapped and generated using ArcGIS Pro software, version 2.3.0.
Results:
Study sample characteristics
Table 1 summarizes baseline demographic and clinical characteristics of the cohort (84,931 THA cases) stratified by age group and ADI. The two age groups were <65 (n = 40,304) and ≥ 65 (n = 44,627) years. In the younger age group, 6,882 (17.1%) came from high ADI communities, 18,741 (46.5%) from middle ADI communities, and 14,681 (36.4%) from low ADI communities. The distribution for high, middle, and low ADI among patients ≥ 65 years of age were 6,174 (13.8%), 21,001 (47.1%), and 17,452 (39.1%), respectively.
Table 1:
Baseline Characteristics and Complications by Area Deprivation Index (ADI) and age group (N = 84 931)
| Age <65 (N = 40,304) | Age ≥65 (N = 44,627) | |||||||
|---|---|---|---|---|---|---|---|---|
| Variable | Low ADI | Middle | High ADI | p a | Low ADI | Middle | High ADI | pa |
| N = 14 681 | N = 18 741 | N = 6882 | N = 17 452 | N = 21 001 | N = 6174 | |||
| Patient Characteristics: | ||||||||
| Sex: Female | 6808 (46.4) | 8867 (47.3) | 3295 (47.9) | 10 568 (60.6) | 12 928 (61.6) | 3981 (64.5) | *** | |
| Race: | *** | *** | ||||||
| White | 14 126 (96.2) | 17 341 (92.5) | 4917 (71.4) | 17 082 (97.9) | 20 290 (96.6) | 5223 (84.6) | ||
| African American | 555 (3.78) | 1400 (7.47) | 1965 (28.6) | 370 (2.12) | 711 (3.39) | 951 (15.4) | ||
| Discharge Destination: | *** | *** | ||||||
| Home or HH | 13 230 (90.1) | 16 308 (87.0) | 5340 (77.6) | 11 253 (64.5) | 12 886 (61.4) | 3446 (55.8) | ||
| Institution | 1451 (9.88) | 2433 (13.0) | 1542 (22.4) | 6199 (35.5) | 8115 (38.6) | 2728 (44.2) | ||
| Primary Insurance: | *** | *** | ||||||
| Other | 130 (0.89) | 193 (1.03) | 43 (0.62) | 96 (0.55) | 109 (0.52) | 20 (0.32) | ||
| Medicare | 1057 (7.20) | 2332 (12.4) | 1278 (18.6) | 15 026 (86.1) | 18 643 (88.8) | 5550 (89.9) | ||
| Medicaid | 698 (4.75) | 1696 (9.05) | 1463 (21.3) | 18 (0.10) | 38 (0.18) | 37 (0.60) | ||
| Commercial | 12 638 (86.1) | 14 299 (76.3) | 4036 (58.6) | 2292 (13.1) | 2168 (10.3) | 552 (8.94) | ||
| Government | 158 (1.08) | 221 (1.18) | 62 (0.90) | 20 (0.11) | 43 (0.20) | 15 (0.24) | ||
| Elixhauser Index b: | *** | *** | ||||||
| 0 | 2820 (19.2) | 3295 (17.6) | 1109 (16.1) | 3172 (18.2) | 3428 (16.3) | 1029 (16.7) | ||
| 1-4 | 10 914 (74.3) | 14 247 (76.0) | 5346 (77.7) | 13 230 (75.8) | 16 224 (77.3) | 4757 (77.0) | ||
| ≥ 5 | 947 (6.45) | 1199 (6.40) | 427 (6.20) | 1050 (6.02) | 1349 (6.42) | 388 (6.28) | ||
| Facility Characteristics: | *** | *** | ||||||
| Metro area: Metro | 14 662 (99.9) | 17 469 (93.2) | 6004 (87.2) | 17 424 (99.8) | 19 253 (91.7) | 5125 (83.0) | ||
| Volume of cases (by facility): | *** | *** | ||||||
| <100/year | 1735 (11.8) | 3113 (16.6) | 1460 (21.2) | 2122 (12.2) | 3954 (18.8) | 1356 (22.0) | ||
| 100 - 199/year | 3570 (24.3) | 4372 (23.3) | 1832 (26.6) | 4865 (27.9) | 5199 (24.8) | 1888 (30.6) | ||
| ≥200/year | 9376 (63.9) | 11 256 (60.1) | 3590 (52.2) | 10 465 (60.0) | 11 848 (56.4) | 2930 (47.5) | ||
| Complications: | ||||||||
| 90-day readmission | 1038 (7.07) | 1641 (8.76) | 743 (10.8) | 1922 (11.0) | 2443 (11.6) | 821 (13.3) | ||
| Myocardial infarction | 7 (0.05) | 9 (0.05) | 4 (0.06) | 40 (0.23) | 62 (0.30) | 18 (0.29) | ||
| Prosthetic device complication | 22 (0.15) | 28 (0.15) | 18 (0.26) | 36 (0.21) | 42 (0.20) | 16 (0.26) | ||
| Surgical wound infection | 7 (0.05) | 9 (0.05) | 2 (0.03) | 9 (0.05) | 3 (0.01) | 1 (0.02) | ||
| Venous thromboembolism | 6 (0.04) | 3 (0.02) | 3 (0.04) | 22 (0.13) | 29 (0.14) | 11 (0.18) | ||
Data are presented as n (%). HH – Home with home health care
Variables are compared by ADI for each age group (years < 65, ≥ 65) using Pearson χ2 test or fisher’s exact test, as appropriate. Significance levels:
= p<0.05
= p<0.01
= p<0.001
Clinical comorbidities were identified based on coding algorithms developed by Quan and colleagues (enhanced Elixhauser version), using either ICD-9-CM or ICD-10 codes, as appropriate. The Elixhauser co-morbidity index score is calculated based on the cumulative number of comorbidity conditions
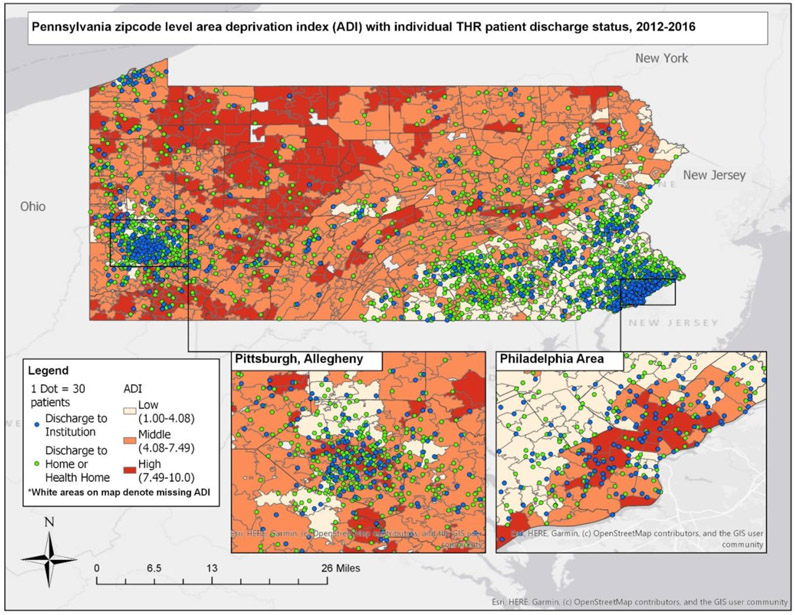
Among younger patients (< 65 years), low ADI communities had only 3.78% African American (AAs), whereas high ADI communities had 28.6% AAs; 7.2% of those living in low ADI communities and 18.6% of those in high ADI communities relied on Medicare, whereas 86.1% of low ADI and 58.6% of high ADI community patients had commercial insurance. Similarly, among older patients (≥ 65 years), the proportion of AA patients was higher in more deprived communities compared to less deprived communities (15.4% vs. 2.12%); 86.1% low ADI and 89.9% high ADI community patients relied on Medicare; whereas 13.1% of low ADI and 8.94% of high ADI community patients relied on commercial insurance. There were no significant differences in post-operative complication rates between patients from all three ADI groups, irrespective of the age group. Figure 2 shows the geospatial localization and relationship of THA patients in Pennsylvania with respect to different community ADI levels. Higher proportion of AAs are seen in high ADI areas.
Figure 2.
Adjusted relative risk ratios of referral to varying discharge locations in African American THA patients (vs. whites) in two age groups
Characteristics by discharge destination: < 65 years versus ≥ 65 years
Demographic and clinical characteristics by discharge destination are described in Table 2. Among those <65 years of age, 5,426 (13.4%) patients were discharged to an institution, whereas 34,878 (86.5%) were discharged to home. Among patients ≥65 years of age, 17,042 (38.2%) were discharged to an institution and 27,585 (61.8%) were discharged to home. Among the younger patients, there was a higher proportion of AAs discharged to an institution (23.1%) compared to home (7.64%), while whites were largely discharged to home (92.4%). Similarly, among the older patients, a higher proportion of AAs (6.34%) were discharged to an institution compared to home, with whites again being largely discharged to home (96.5%). Among the younger group, 19.6% relied on Medicaid who were discharged to an institution compared to 8.01% who were discharged home. Among those in the older age group, 92.1% of patients discharged to an institution relied on Medicare compared to 85.2% who were discharged home. Of the patients who were discharged to an institution, 51.2% of <65 years group and 7.05% of the > 65 years group relied on commercial insurance.
Table 2.
Baseline characteristics and outcomes by discharge destination and age group (N = 84 931).
| Age <65 (N = 40 304) | Age ≥65 (N = 44 627) | |||||
|---|---|---|---|---|---|---|
| Variable | Home or HH | Institution | pa | Home or HH | Institution | pa |
| N = 34 878 | N = 5426 | N = 27 585 | N = 17 042 | |||
| ADI: | *** | *** | ||||
| Low | 13230 (37.9) | 1451 (26.7) | 11253 (40.8) | 6199 (36.4) | ||
| Middle | 16308 (46.8) | 2433 (44.8) | 12886 (46.7) | 8115 (47.6) | ||
| High | 5340 (15.3) | 1542 (28.4) | 3446 (12.5) | 2728 (16.0) | ||
| Sex: Female | 15 875 (45.5) | 3095 (57.0) | *** | 15 532 (56.3) | 11 945 (70.1) | *** |
| Race: | *** | *** | ||||
| White | 32 213 (92.4) | 4171 (76.9) | 26 633 (96.5) | 15 962 (93.7) | ||
| African American | 2665 (7.64) | 1255 (23.1) | 952 (3.45) | 1080 (6.34) | ||
| Primary Insurance: | *** | *** | ||||
| Unknown/Uninsured | 332 (0.95) | 34 (0.63) | 178 (0.65) | 47 (0.28) | ||
| Medicare | 3155 (9.05) | 1512 (27.9) | 23 516 (85.2) | 15 703 (92.1) | ||
| Medicaid | 2792 (8.01) | 1065 (19.6) | 37 (0.13) | 56 (0.33) | ||
| Commercial | 28 197 (80.8) | 2776 (51.2) | 3810 (13.8) | 1202 (7.05) | ||
| Government | 402 (1.15) | 39 (0.72) | 44 (0.16) | 34 (0.20) | ||
| Metro area: Metro | 32 995 (94.6) | 5140 (94.7) | 25 845 (93.7) | 15 957 (93.6) | ||
| Volume of cases (by facility): | *** | *** | ||||
| <100/year | 4885 (14.0) | 1423 (26.2) | 3671 (13.3) | 3761 (22.1) | ||
| 100 - 199/year | 8396 (24.1) | 1378 (25.4) | 7262 (26.3) | 4690 (27.5) | ||
| ≥200/year | 21 597 (61.9) | 2625 (48.4) | 16 652 (60.4) | 8591 (50.4) | ||
| 90-day readmission | 2463 (7.06) | 959 (17.7) | *** | 2160 (7.83) | 3026 (17.8) | *** |
| Elixhauser Index b: | ||||||
| 0 | 6297 (18.1) | 927 (17.1) | 4719 (17.1) | 2910 (17.1) | ||
| 1-4 | 26 363 (75.6) | 4144 (76.4) | 21 114 (76.5) | 13 097 (76.9) | ||
| ≥ 5 | 2218 (6.36) | 355 (6.54) | 1752 (6.35) | 1035 (6.07) | ||
| Postoperative myocardial infarction | 12 (0.03) | 8 (0.15) | *** | 31 (0.11) | 89 (0.52) | *** |
| Prosthetic device complication | 39 (0.11) | 29 (0.53) | *** | 29 (0.11) | 65 (0.38) | *** |
| Surgical wound infection | 12 (0.03) | 6 (0.11) | ** | 6 (0.02) | 7 (0.04) | |
| Venous thromboembolism | 6 (0.02) | 6 (0.11) | *** | 16 (0.06) | 46 (0.27) | *** |
Data are presented as n (%). HH – Home with home health care. ADI – Area Deprivation Index
Variables are compared by discharge destination for each age group (years < 65, ≥ 65) using Pearson χ2 test or fisher’s exact test, as appropriate. Significance levels:
= p<0.05,
= p<0.01
= p<0.001
Clinical comorbidities were identified based on coding algorithms developed by Quan and colleagues (enhanced Elixhauser version), using either the ICD-9-CM or the ICD-10 coding system, as appropriate. The Elixhauser co-morbidity index score is calculated based on the cumulative number of comorbidity conditions.
Community ADI and Discharge destination
Compared to low ADI, patients from high ADI communities were more likely to be discharged to an Institution (age <65: aOR = 1.47, 95% CI = 1.34 – 1.61; age ≥65; aOR = 1.31, 95% CI = 1.22 – 1.41). This relationship was significant even after adjusting for patient- and facility-level confounders (Figure 3). To assess whether patient race modifies this relationship between neighborhood ADI and discharge destination, we estimated the odds of discharge destination and included an interaction term for ADI and race. The effect of race on the relationship of ADI and discharge destination was not significant in patients <65 years of age, but it was significant in the older group (aOR = 1.34, 95%CI = 1.01-1.77; p < 0.05).
Figure 3.
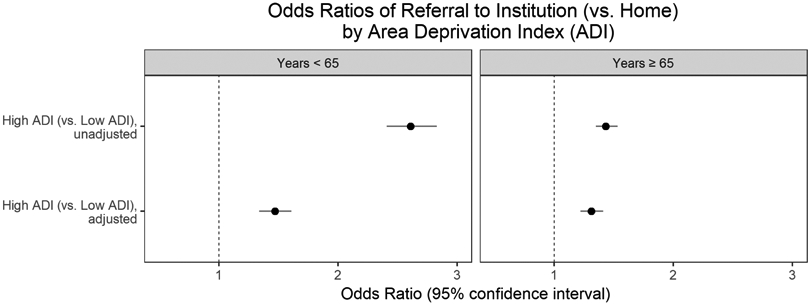
Adjusted odds ratios of 90-day readmission in patients who were discharged to various locations compared to home before and after coarsened exact matching (CEM)
Community ADI and 90-day readmission
In examining the association between community ADI and 90-day readmission rates to an acute care facility, we found no statistically significant differences for those living in high vs. low ADI communities, regardless of the age group (<65 years, p = 0.73; and ≥65, p = 0.97). The interaction of race and ADI on 90-day readmission was also not statistically significant.
Discussion:
In this sample of >84,000 patients who underwent elective THA in the State of Pennsylvania between 2012 and 2016, we found that patients from low-ADI communities were more likely to be discharged to an institution for post-operative care and rehabilitation. This relationship was accentuated by AA race in patients ≥65 years of age. These findings were significant even after controlling for patient demographics, comorbidities, and post-operative complications as well as facility-level characteristics. However, community deprivation did not affect the odds of 90-day readmission to acute care hospital.
Others have examined how socioeconomic factors may influence elective joint arthroplasty access, utilization, and outcomes.33 However, there is relatively less research on social factors that influence post-surgical discharge planning. A few studies suggest a relationship between race/ethnicity and post-operative discharge destination.19,34 For instance, AAs have been reported to have higher likelihood of discharge to an institution rather than home.19 Another study found minority patients to be more likely than whites to be discharged to an institution post-operatively.35 In a larger study using California statewide data (n=14,326), race, primary insurance, and comorbidity were the main factors driving patients’ likelihood of being discharged to an institution.34
However, it is not clear if race is the only social factor that influences discharge destination after elective THA. One study previously examined the relationship of socioeconomic status (SES) and discharge destination using household income on a community level. However, that study measured SES as a community-level measure of median household income for each zip code. Using similar methods to ours and dividing SES indicators into quartiles, they found that patients coming from communities with worse SES had a 26% higher likelihood of discharge to an institution compared to those from more affluent communities.36 Using a more robust measure of community level socioeconomic status (ADI) and a much larger data set spanning multiple years, our analysis confirms the influence of community-level SES on discharge destination in patients who undergo elective THA. Even though there were a higher proportion of AAs in high ADI communities, we found that patient race has an additive effect on discharge to an institution only in patients who are ≥65 years of age, many of whom rely on Medicare insurance.
Our findings add to literature that not only race, but also socioeconomics of the community determines discharge destination. Previous studies have shown that early discharge to home is associated with reduced costs, improved clinical outcomes, and increased patient satisfaction.35, 36 Given the growing demand for THA, and the costs associated with discharge to an institution after elective joint replacement surgery, it is important to understand the non-clinical factors that influence this decision. To our knowledge, this is one of the first large-scale analyses that demonstrates that neighborhood SES may have implications for post-THA discharge decision-making. This information is particularly timely given the emergent payment reform policies such as bundle payments that target post-operative care and rehabilitation.
Possible explanations for our findings that community level factors such as SES may influence the decision for discharge destination are multifactorial. These include patient preferences, family support (impoverished are known to have lesser family support), the health care system/physician preferences, community resources available (for example, accessible streets, sidewalks, walkways, elevators, primary-care physicians (PCPs), urgent care centers), all of which may factor into the decision to discharge to an institution vs home or even 90-day readmissions. Also, there is evidence that SES influences 90-day readmissions in other diseases and procedures.37,38 Community-level factors play a huge role in health care delivery and access, especially in deprived communities. For patients from low SES communities, institutional post-operative and rehabilitative care might present as a “safer” option in clinical decision-making. That patient race has additive effect on the relationship between community level ADI and discharge destination to facility is not surprising; after all, on average many more minority patients reside in deprived communities. What is not clear is why this relationship is not apparent in patients who are less than 65 years in age. Perhaps it is easier to place Medicare-insured minority patients into SNFs or IRFs. On the positive side, it is reassuring that even though community deprivation level influences discharge destination, it is not associated with risk of 90-day readmission to acute hospital.
There are important limitations to consider in interpreting our results. First, we used an administrative dataset that lacks granular information on potentially important confounders such as body mass index. In other words, the comorbidity index we used may not fully capture the universe of comorbidities that could influence discharge decision-making. Second, we do not have data on patient preference for discharge destination. Third, we have no data on level of social support and care continuity that exist in these communities. The ADI provides some insight into community-level factors, but does not indicate what support resources exist within a community. Fourth, we lack individual-level SES measures which may cause residual confounding. Since most clinical information systems and registries are currently unable to capture accurate individual level SES, a proxy measure ADI was created to capture patient level social risk factors. ADI is developed based on census data and is validated in a number of conditions. Community-level ADI is used to inform policy in other studies and helps us assess how one’s neighborhood of residence effects healthcare outcomes such as ours.39 Fifth, we studied only patients with primary elective THA in Pennsylvania; thus our results may not be generalizable to other states or regions. Lastly, the ADI has the same limitations as the US Census Bureau data from which it is derived, including limited accounting for undocumented immigrant populations. However, we used the updated index, which is validated for a range of health outcomes and disease domains for use at the neighborhood level.40,41
Conclusion:
In summary, in this large-scale study of >84,000 patients who underwent primary THA across 170 Pennsylvania hospitals, we found that patients from less affluent neighborhoods were more likely to be discharged to institutions (i.e., IRFs and SNFs) than home. We also found that community ADI is not associated with risk of 90-day readmission to an acute care facility following elective THA. Future studies should examine what aspect of community-level factors shape this relationship and how they could be modified to allow more patients to go home after elective THA.
Significance and Innovation:
Studies have shown that individual-level factors such as race influence discharge destination and risk of 90-day readmissions after elective hip replacement surgery. This analysis broadens the evaluation by examining how community-level social determinants of health such as area deprivation index impact surgical care.
We found that patients from highly deprived communities as measured by Area Deprivation Index(ADI) were more likely to be discharged to an institution rather than home for post-op care and rehab after elective THA. However, we found no statistically significant difference in 90-day readmission based on patient community ADI level.
The study is innovative because it expands our understanding of the relationships between markers of social vulnerability and healthcare use and outcomes. This information is needed to help design socially informed health care policies to improve quality and outcomes.
Acknowledgements:
Dr. Ibrahim is supported by Grant Number K24AR055259 from the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Dr. Mehta is supported by the C. Ronald MacKenzie Young Scientist Endowment Award.
Funding: None
Appendix
Appendix Table 1.
ICD-9/10 codes of inclusion hip procedure and surgical complications. 19
| ICD 9 codes | ICD 10 codes | |
|---|---|---|
| Hip Replacement | 81.51 | 0SR90xx, 0SRB0xx |
| Venous Thromboembolism | 453.40, 453.41, 453.6, 453.42, 453.84, 453.81, 453.86, 453.89, 453.82, 453.9, 453.85 | I82441, I82433, I82B19, I82409, I82621, I82411, I82402, I82401, I824Z9, I82491, I824Z1, I82432, I82412, I824Z2, I82512 |
| Acute Myocardial Infarction | 410.71, 410.21, 410.11, 410.72, 410.81, 410.01, 410.61, 410.91, 410.42, 410.70, 410.90, 410.20, 410.41 | I214, I213, I2129, I2119, I2102 |
| Surgical Wound Infection | 998.59 | K6811, T814XXA |
| Prosthetic Device Complications | 996.77, 996.47, 996.42, 996.78, 996.44, 996.40, 996.49, 996.43, 996.66, 996.67, 996.41, 996.01, 996.46, 996.79 | T8481XA, T84115D, T84020A,T84041A, T84114A, T84218A, T8484XA, T84498A, T84199A, T84011A, T84021A, T8489XA, T8451XA, T84010A, T84091A, T84031A, T84328A, T84030A, T847XXA, T84050S, T84099A, T84040A, T84090A, T84428A, T8451XD, T84038A, T84061A, T84050A, T8486XA, T8452XA, T8483XA |
Footnotes
Ethics Approval: IRB exempt
References
- 1.Murray CJ, Atkinson C, Bhalla K, et al. The state of US health, 1990-2010: burden of diseases, injuries, and risk factors. JAMA. 2013;310(6):591–608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhang Y, Jordan JM. Epidemiology of osteoarthritis. Clinics in geriatric medicine. 2010;26(3):355–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cameron KL, Hsiao MS, Owens BD, Burks R, Svoboda SJ. Incidence of physician-diagnosed osteoarthritis among active duty United States military service members. Arthritis and rheumatism. 2011;63(10):2974–2982. [DOI] [PubMed] [Google Scholar]
- 4.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. JBJS. 2007;89(4):780–785. [DOI] [PubMed] [Google Scholar]
- 5.Lawrence RC, Helmick CG, Arnett FC, et al. Estimates of the prevalence of arthritis and selected musculoskeletal disorders in the United States. Arthritis and rheumatism. 1998;41(5):778–799. [DOI] [PubMed] [Google Scholar]
- 6.Jordan JM, Linder GF, Renner JB, Fryer JG. The impact of arthritis in rural populations. Arthritis care and research : the official journal of the Arthritis Health Professions Association. 1995;8(4):242–250. [DOI] [PubMed] [Google Scholar]
- 7.Jha AK, Fisher ES, Li Z, Orav EJ, Epstein AM. Racial trends in the use of major procedures among the elderly. The New England Journal of Medicine. 2005;353(7):9. [DOI] [PubMed] [Google Scholar]
- 8.Nwachukwu BU, Kenny AD, Losina E, Chibnik LB, Katz JN. Complications for racial and ethnic minority groups after total hip and knee replacement: a review of the literature. The Journal of bone and joint surgery American volume. 2010;92(2):338–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Banerjee D, Illingworth KD, Novicoff WM, Scaife SL, Jones BK, Saleh KJ. Rural vs. urban utilization of total joint arthroplasty. J Arthroplasty. 2013;28(6):888–891. [DOI] [PubMed] [Google Scholar]
- 10.Krupic F, Eisler T, Garellick G, Karrholm J. Influence of ethnicity and socioeconomic factors on outcome after total hip replacement. Scandinavian journal of caring sciences. 2013;27(1):139–146. [DOI] [PubMed] [Google Scholar]
- 11.Clement ND, Muzammil A, Macdonald D, Howie CR, Biant LC. Socioeconomic status affects the early outcome of total hip replacement. The Journal of bone and joint surgery British volume. 2011;93(4):464–469. [DOI] [PubMed] [Google Scholar]
- 12.Agabiti N, Picciotto S, Cesaroni G, et al. The influence of socioeconomic status on utilization and outcomes of elective total hip replacement: a multicity population-based longitudinal study. International journal for quality in health care : journal of the International Society for Quality in Health Care. 2007;19(1):37–44. [DOI] [PubMed] [Google Scholar]
- 13.2019; https://www.cdc.gov/socialdeterminants/index.htm. Accessed 9.26.2019, 2019.
- 14.Sabeh KG, Rosas S, Buller LT, Roche MW, Hernandez VH. The impact of discharge disposition on episode-of-care reimbursement after primary total hip arthroplasty. The Journal of arthroplasty. 2017;32(10):2969–2973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bozic KJ, Ward L, Vail TP, Maze M. Bundled payments in total joint arthroplasty: targeting opportunities for quality improvement and cost reduction. Clinical orthopaedics and related research. 2014;472(1):188–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lavernia CJ, D’Apuzzo MR, Hernandez VH, Lee DJ, Rossi MD. Postdischarge costs in arthroplasty surgery. J Arthroplasty. 2006;21(6 Suppl 2):144–150. [DOI] [PubMed] [Google Scholar]
- 17.Chen LM, Norton EC, Banerjee M, Regenbogen SE, Cain-Nielsen AH, Birkmeyer JD. Spending On Care After Surgery Driven By Choice Of Care Settings Instead Of Intensity Of Services. Health affairs (Project Hope). 2017;36(1):83–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Finkelstein A, Ji Y, Mahoney N, Skinner J. Mandatory Medicare Bundled Payment Program for Lower Extremity Joint Replacement and Discharge to Institutional Postacute Care: Interim Analysis of the First Year of a 5-Year Randomized Trial. Jama. 2018;320(9):892–900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vina ER, Kallan MJ, Collier A, Nelson CL, Ibrahim SA. Race and Rehabilitation Destination After Elective Total Hip Arthroplasty: Analysis of a Large Regional Data Set. Geriatric orthopaedic surgery & rehabilitation. 2017;8(4):192–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ortiz CA, Goodwin JS, Freeman JL. The effect of socioeconomic factors on incidence, stage at diagnosis and survival of cutaneous melanoma. Medical science monitor : international medical journal of experimental and clinical research. 2005;11(5):Ra163–172. [PubMed] [Google Scholar]
- 21.Parikh-Patel A, Bates JH, Campleman S. Colorectal cancer stage at diagnosis by socioeconomic and urban/rural status in California, 1988-2000. Cancer. 2006;107(5 Suppl):1189–1195. [DOI] [PubMed] [Google Scholar]
- 22.Everett E, Mathioudakis N. Association of Area Deprivation and Diabetic Ketoacidosis Readmissions: Comparative Risk Analysis of Adults vs Children With Type 1 Diabetes. The Journal of Clinical Endocrinology & Metabolism. 2019;104(8):3473–3480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Daneshvar P, Forster AJ, Dervin GF. Accuracy of administrative coding in identifying hip and knee primary replacements and revisions. Journal of evaluation in clinical practice. 2012;18(3):555–559. [DOI] [PubMed] [Google Scholar]
- 24.Cahue SR, Etkin CD, Stryker LS, Voss FR. Procedure coding in the American Joint Replacement Registry. Arthroplasty today. 2019;5(2):251–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Singh J, Kwoh C, Boudreau R, Lee G, Ibrahim S. Hospital volume and surgical outcomes after elective hip/knee arthroplasty: a risk-adjusted analysis of a large regional database. Arthritis Rheum. 2011;63(8):2531–2539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yelin E, Trupin L, Bunde J, Yazdany J. Poverty, Neighborhoods, Persistent Stress, and SLE Outcomes:A Qualitative Study of the Patients’ Perspective. Arthritis Care Res (Hoboken). 2018. [DOI] [PMC free article] [PubMed]
- 27.Kind AJH, Buckingham WR. Making Neighborhood-Disadvantage Metrics Accessible - The Neighborhood Atlas. N Engl J Med. 2018;378(26):2456–2458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Matern R, Mendelson M, Oliphant M, Bank DBF. Testing the validity of the Ontario deprivation index. Caledon Institute of Social Policy; 2009. [Google Scholar]
- 29.Rural-Urban Continuum Codes. 2013; http://www.ers.usda.gov/data-products/rural-urban-continuum-codes/documentation.aspx. Accessed Accessed June 13, 2016.
- 30.<w/>(HCUP) AHCaUP. HCUP Elixhauser Comorbidity Software. 2016; http://www.hcup-us.ahrq.gov/toolssoftware/comorbidity/comorbidity.jsp, 3.7.
- 31.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Medical care. 2005;43(11):1130–1139. [DOI] [PubMed] [Google Scholar]
- 32.von Elm E, Altman D, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453–1457. [DOI] [PubMed] [Google Scholar]
- 33.Dowsey MM, Nikpour M, Choong PF. Outcomes following large joint arthroplasty: does socio-economic status matter? BMC Musculoskelet Disord. 2014;15:148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schwarzkopf R, Ho J, Snir N, Mukamel DD. Factors Influencing Discharge Destination After Total Hip Arthroplasty: A California State Database Analysis. Geriatr Orthop Surg Rehabil. 2015;6(3):215–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lan RH, Kamath AF. Post-acute care disparities in total joint arthroplasty. Arthroplasty today. 2017;3(3):187–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Inneh IA, Clair AJ, Slover JD, Iorio R. Disparities in Discharge Destination After Lower Extremity Joint Arthroplasty: Analysis of 7924 Patients in an Urban Setting. The Journal of arthroplasty. 2016;31(12):2700–2704. [DOI] [PubMed] [Google Scholar]
- 37.Ostler K, Thompson C, Kinmonth A-L, Peveler R, Stevens L, Stevens AJTBJoP. Influence of socio-economic deprivation on the prevalence and outcome of depression in primary care: the Hampshire Depression Project. 2001;178(1):12–17. [DOI] [PubMed] [Google Scholar]
- 38.Arroyo NS, White RS, Gaber-Baylis LK, La M, Fisher AD, Samaru MJPhm. Racial/ethnic and socioeconomic disparities in total knee arthroplasty 30-and 90-ay eadmissions: a multi-payer and multistate analysis, 2007-2014. 2019;22(2):175–185. [DOI] [PubMed] [Google Scholar]
- 39.Kind AJ, Jencks S, Brock J, et al. Neighborhood socioeconomic disadvantage and 30-day rehospitalization: a retrospective cohort study. Ann Intern Med. 2014;161(11):765–774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lantos PM, Hoffman K, Permar SR, et al. Neighborhood disadvantage is associated with high cytomegalovirus seroprevalence in pregnancy. Journal of racial and ethnic health disparities. 2017:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hu J, Kind AJ, Nerenz D. Area Deprivation Index predicts readmission risk at an urban teaching hospital. American Journal of Medical Quality. 2018;33(5):493–501. [DOI] [PMC free article] [PubMed] [Google Scholar]