Abstract
The perinatal period involves major developmental transitions which can be conceptualized through a biopsychosocial (BPS; Engel in Science 196:129–136, 1977, 10.1126/science.847460, in The American Journal of Psychiatry 137:535–544, 1980, 10.1176/ajp.137.5.535), systemic (von Bertalanffy, General system theory: Foundations, development, applications, George Braziller, New York, 1968) framework. Thus, no one domain of health in the perinatal period can be understood without exploring how the other domains are both impacted by and impacting the others. As a result of COVID-19, popular media is paying special attention to the biomedical domain of women in the perinatal period as it relates to health outcomes and changes in perinatal healthcare policies; however, considerably less attention is being paid to the other BPS health domains and systemic impacts. This paper will outline U.S. changes in healthcare as a result of the COVID-19 pandemic for individuals, couples, and families within the perinatal period (i.e., family planning and conception, prenatal, labor and delivery, and postpartum) and explore the unique psychosocial, systemic impacts. Recommendations for care, including telehealth and virtual support options, and future directions for research will be provided.
Keywords: Biopsychosocial, COVID-19, Perinatal, Pregnancy, Systems
The perinatal period is one of major transition as a family is formed or expanded. Perinatal patients are deemed a vulnerable population and are therefore uniquely impacted by COVID-19 (Inter-Agency Standing Committee [IASC] 2020). For the purposes of the present paper we conceptualize the perinatal period, the developmental period before and after birth, as broadly as possible to include family planning and conception, prenatal, labor and delivery, and postpartum. Furthermore, we understand this period through the biopsychosocial (BPS; Engel 1977, 1980), systemic lens (von Bertalanffy 1968). That is, we understand the relevance of conceptualizing all individuals who are within or impacted by the perinatal period through a comprehensive and contextual framework that considers physiological aspects of health (biomedical); thoughts, feelings, and overall mental health (psychological); and social determinants of health, sources of support, and relationships (social); (Engel 1977; Hodgson et al. 2007). Although the BPS framework has been updated to include a spiritual domain to further explore individual’s belief systems (i.e., BPSS; Wright et al. 1996), for the purposes of this paper we will focus on the BPS domains. The physiological domain of health in the perinatal period is inextricably linked to the psychosocial domains; therefore, no one domain of health can be understood without exploring how the other domains are impacting it (Aamar and Kolobova 2016).
As of July 6, 2020 there are over 2.9 million confirmed cases of COVID-19 in the U.S., making it the country with the highest rates (See Johns Hopkins University & Medicine 2020). Tracking data on pregnant women with COVID-19 between January 22 and June 30, 2020 shows 10,537 total cases; 3077 hospitalized cases, and 30 deaths (Centers for Disease Control & Prevention [CDC] 2020a). Overall, true prevalence rates are fluid, difficult to assess, and may be underreported (Ai et al. 2020); this is extended to the pregnant population. In a small study at two New York hospitals, nearly 90% of women with COVID-19 were asymptomatic when first admitted to hospital to give birth (Sutton et al. 2020). Thus, it is understandable why perinatal healthcare policies (e.g., restrictions in visitors, reduced in-person appointments, etc.) have been intentionally cautious. While popular media is paying special attention to the biomedical domain of health as it relates to changes in perinatal healthcare and hospital policies, less attention is being paid to the other BPS health domains. Regardless of the necessity of changes in healthcare policies, the psychosocial impacts across the family and healthcare system exist. And in a health pandemic like COVID-19, stressors are heightened, as are fears and worry from realistic dangers of being part of a vulnerable population (IASC 2020). This paper will outline unique considerations across the perinatal period during the COVID-19 pandemic paying special attention to the psychosocial, systemic impact1 followed by recommendations for care and future research.
Biopsychosocial, Systemic Framework in the Perinatal Period
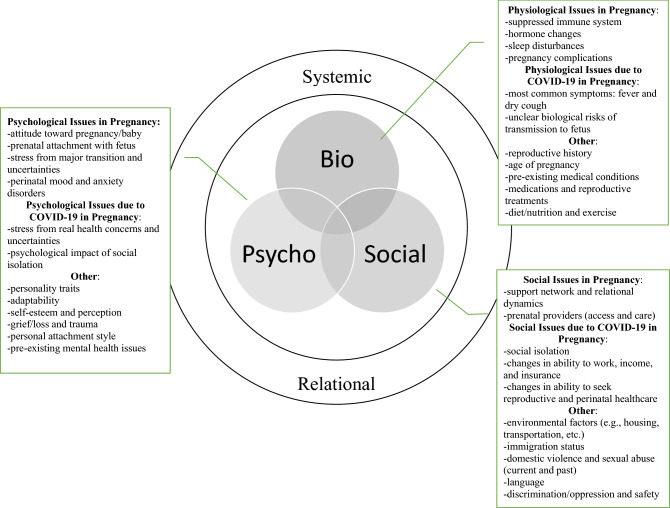
The BPS framework is well suited to describe the perinatal period due to its ability to conceptualize health through biological, psychological, and social processes. Figure 1 provides a visual portrayal of this framework for the perinatal period.
Fig. 1.
BPS framework in the perinatal period
Biology
The biological domain of health focuses on physiological and biomedical issues that include considerations related to acute and chronic conditions and symptoms, health diagnoses, medications, medical treatments, etc. In pregnancy, for example, there are a number of physiological changes that occur to develop the fetus and prepare the woman for labor and delivery (Soma-Pillay et al. 2016). As it relates to COVID-19, it is important to recognize that some physiological changes in pregnancy may mimic symptoms of medical disease (e.g., shortness of breath), and physiological changes may also make women more vulnerable to illnesses (e.g., changes to immune system).
COVID-19 is a novel virus; thus, evidence available on health outcomes that would guide clinical decision making is based on low quality case studies/reports and expert opinion (Evidence Based Birth 2020). At present, what is known about pregnancy is that it causes physiological changes that may increase risk of infections and severe symptoms when infected with viruses similar to COVID-19 (CDC 2020b). When taking into consideration maternal age, underlying conditions, and race/ethnicity, pregnant women infected with COVID-19 were 1.5 times more likely to be admitted to the ICU and 1.7 times more likely to receive mechanical ventilation compared to their non-pregnant counterparts (Ellington et al. 2020). The physiological changes that occur during pregnancy are thought to increase mother’s risk for severe illness. In general, the most common symptoms found in pregnant women contracting COVID-19 have been fever and dry cough (see Zaigham and Andersson 2020 for additional maternal characteristics and rates). Fetal risk of exposure has little evidence though there are some recent reports of such incidences (Chen et al. 2020; Weigel 2020). The unknown biological risks during pregnancy contributes to already present and typical stressors around the perinatal period.
Psychology
The psychological domain of health includes the thoughts, feelings, and behaviors that are typically considered when assessing mental health. Much has been written about the psychological impact of the perinatal period. As Slade et al. (2009) described, “pregnancy is no ordinary time in the life of a woman. At no other point in her life will so much about her change in such a brief period, or will the nature and quality of her adaptations have such far-reaching implications for her own and her child’s physical and psychological health” (p. 22). This transition is further described as one of hope and possibility, as well as crisis and potential disorganization. With the unprecedented COVID-19 pandemic, there may be an understandable psychological crisis as this is a time of exacerbated uncertainty and anxiety with health-related concerns and changes to traditional perinatal care. Complicated by the decrease in access to mental health services and limitations surrounding teletherapy, attention to psychological impacts is overwhelmed by the biological implications of pregnancy during COVID-19, yet should not be overlooked.
Social
The social domain of health considers the relationships and conditions of one’s environment, which is severely limited for all due to the risks around COVID-19 and especially for vulnerable populations. This domain includes considerations such as the quality of romantic and family relationships, use and efficacy of social support, patient-provider relationships, and social determinants of health (e.g., access and quality of necessary resources, education, and employment). As it relates to pregnancy during COVID-19, a primary guideline includes social distancing and isolation, particularly after 28 weeks’ gestation (Royal College of Obstetricians & Gynaecologists [RCOG] 2020). Social distancing guidelines, overall, are of psychosocial concern.
Research demonstrates a significant association between social isolation (i.e., lack of interactions with others or the wider community) and loneliness (i.e., feelings of the absence of a social network or companion) with poorer mental health outcomes, such as depression (Leigh-Hunt et al. 2017). Not only have there been disruptions in people’s ability to engage socially with important support systems, there have been changes to patient-provider relationships (Gildner and Thayer 2020). Namely, in the perinatal period there have been disruptions or discontinuation of reproductive treatments, reductions to face-to-face appointments, and increased use of telehealth.
Systems
Understanding the BPS framework through the complimentary systems paradigm is well explained by McDaniel et al. (2014):
… human life is a seamless cloth spun from biological, psychological, social, and cultural threads; that patients and families come with bodies as well as minds, feelings, interaction patterns, and belief system; that there are no biological problems without psychosocial implications, and no psychosocial problems without biological implications. (p. 1-2)
The health domains described above are inextricably interconnected so that one’s health can best be understood and treated at the intersection of the BPS domains (Aamar and Kolobova 2016). As one example, issues related to the social domain of health such as social isolation (recommended due to biological risks), insecurity, financial difficulty, and inability to access one’s support systems are all widely recognized as risk factors for psychological health (RCOG 2020).
In addition to the interconnectedness of BPS health domains is the interconnectedness of individuals across systems. We can best understand issues within the perinatal period not within any one person (e.g., the mother), but “in the relationships, interactions and language that develop between individuals” (Pote et al. 2000, p. 9). For example, a mother’s mental health within the perinatal period is intimately tied to the mental health of the supports around her (Freitas and Fox 2015). Supports may include a partner/spouse, children, family, friends, and healthcare team. Each person plays an important role in shaping the perinatal period. With current best health practice guidelines, the perinatal period is occurring in isolation without these support systems in place; thus, negatively impacting the psychosocial domains of health.
Family Planning & Conception
According to the CDC (2020b), we are unsure if pregnant women have a greater chance of infection; however, the immunologic and physiologic changes in pregnant women appear to increase severity risk (Ellington et al. 2020). Additionally, COVID-19 does not appear to pass from mother to fetus during pregnancy, but some cases of newborn infection have been reported (Chen et al. 2020; Weigel 2020). It is important to note that, at present, research related to the impact on mother and baby are based on small studies, generally in late pregnancy, and the evidence is inconclusive (Baud et al. 2020). With what is known, and still unknown, people may be left uncertain about how to move forward with family planning. People might question whether or not they should wait or discontinue trying to conceive while others have experienced barriers to decision-making (e.g., fertility treatments and obtaining contraception) due to changes across the medical system.
Fertility Treatment
Infertility is a common problem within the perinatal period; about 9% of men, 11% of women, and 12–15% of couples in the United Sates have experienced fertility problems (National Institute of Health [NIH] 2018). Further, approximately 1.9% of infants born each year in the U.S. are conceived using fertility treatments (CDC 2020c). It is likely, however, that usage rates of these treatments will demonstrate a noticeable decrease immediately following the COVID-19 health pandemic. Recommendations from the American Society for Reproductive Medicine (ASRM 2020) as of March 17, 2020 include the suspension of new fertility treatment cycles and cancelling embryo transfers. An update provided on April 24, 2020 (ASRM 2020) issued recommendations for gradual and judicious resumption of reproductive care which has since been elaborated.
For the many individuals and couples who already waited a significant amount of time trying to start or grow their family, delaying or modifying fertility treatments may further add to the psychosocial impact (Jaffe and Diamond 2011). Infertility, and its related medical treatments, involve a range of emotional processes which include, but are not limited to, feelings of distress, loss of control, stigmatization, and disruption in the hoped for developmental trajectory of adulthood (Jaffe and Diamond 2011; Cousineau and Domar 2007). Disruptions in care delivery, uncertainties about timelines, and health threats present new psychological, social, and emotional concerns and will likely exacerbate those that already existed (ASRM 2020). While infertility is one area of reproductive healthcare with significant BPS disruption, we must also consider another aspect of family planning: the choice to not have a baby through use of contraception.
Birth Control
Time Magazine recently highlighted the loss of access to family planning methods as a result of quarantine (Schuettge 2020), with the full impacts not yet understood. At the start of quarantine, health authorities recommended people stockpile necessary health-related supplies. However, for reproductive care there is a lack of access due to shutdowns and supply shortages, as well as insurance barriers (Ahmed and Sonfield 2020). Manufacturing, shipping, and regulatory approvals of condoms and other contraceptives was reduced or ceased in response to COVID-19 (Purdy 2020); meanwhile, insurance barriers around prescription limits prevents “stockpiling”. Research has found that in times of trauma and fear, like the COVID-19 pandemic, and when facing high mortality risks, individuals might discount future and indulge in reproductive activities (Raschky and Wang 2012). In this time of quarantine and uncertainty, couples may turn to each other as sources of both psychological and social support. With increased demand, restrictions on supply, and lack of access, birth control methods have become limited. Intersecting this with quarantine and an already high rate of unplanned pregnancy, even higher risk for (unplanned) pregnancy could be a result. As the restrictions for quarantine and shutdown are unprecedented in the last 100 years, the impact is unknown and absent from the research (Stone 2020).
Prenatal
As described above, there remains much to be known about the effects of COVID-19 on pregnant women and their babies and, because of this, perinatal healthcare policies have demonstrated intentional caution. While aspects of physiological health remain unknown, it is expected that significant psychosocial impacts are occurring during pregnancy due to changes based on unknown potentials in the biological domain of health.
Pregnancy
Whether conscious or not, everyone has a reproductive story—a personal narrative that details thoughts, feelings, and hopes about one’s parenting journey (Jaffe and Diamond 2011). While the development of this story begins long before conception, pregnancy can be a developmental point in which it becomes salient as people imagine their experiences related to pregnancy, birth, and parenting. Because pregnant women are considered a vulnerable population, practicing social distancing during the COVID-19 health pandemic is of particular importance (IASC 2020). Social distancing guidelines has resulted in changes to traditional pregnancy rituals and prenatal care. Families must forgo certain rituals such as baby showers and gender reveals. Additionally, based on new guidelines for prenatal care, pregnant women may see an increase in telehealth appointments and may be required to leave support people at home during necessary in-person visits (Boelig et al. 2020; RCOG 2020). A study by Saccone et al. (2020) surveyed pregnant woman in Italy from March 15, 2020 to April 1, 2020 and found that more than half of woman rated the psychological impact of COVID-19 as severe, and about two-thirds reported anxiety higher than normal. Interestingly, women in their first trimester identified higher levels of anxiety and more severe psychological impact compared to those later in pregnancy. As the pandemic continues to unfold it will be important to understand this result and post-partum outcomes.
The changes as a result of COVID-19 impacts the BPS experience of pregnancy and will significantly alter the reproductive stories of all involved. That is, these changes are systemic and effect the whole family. For example, research demonstrates fathers desire to connect with their baby throughout pregnancy and that aspects of prenatal care, such as being present for an ultrasound scan is of great importance (Poh et al. 2014). However, new restrictions leave fathers, and other important members of the system, unable to participate in important moments, such as these, during pregnancy. Rituals during this period create a designated time and space to create meaning around the significant transition within the family system (Imber-Black 2002). Thus, grief around the loss of a vision for a pregnancy, for expected parents and those that are also attached to the pregnancy, may surface.
Pregnancy Loss
With the limited data available with COVID-19 there have been mixed findings regarding pregnancy loss. An analysis by Yan et al. (2020) demonstrated no increased risk of miscarriage or spontaneous preterm birth. However, two other studies have suggested the possibility of perinatal death with COVID-19 infection (Zaigham and Andersson 2020; Baud et al. 2020). Of note is the most recent study (Baud et al. 2020) that demonstrated placental infection with COVID-19. This mimics the prenatal infection found in similar viruses (e.g., SARS) which resulted in miscarriage or fetal growth restriction in 40% of observed infected cases (Baud et al. 2020). Whether or not a pregnant person is infected by COVID-19, there are also healthcare policy changes that may have a significant psychological impact on families experiencing pregnancy loss.
Perinatal death is a profoundly traumatic event typically associated with feelings of loss, grief, emotional numbness, and sorrow (Diamond and Roose 2016; Diamond and Diamond 2016; Koopmans et al. 2013). As a result of the restrictions put in place due to COVID-19, support persons are unlikely able to attend in-office prenatal appointments leaving women to receive difficult news regarding the viability of pregnancy alone. Additionally, with hospitals allowing fewer non-emergency medical procedures, more women are being offered only home-based management of miscarriage rather than hospital-based treatments (Miscarriage Association 2020). For those seeking hospital-based treatments, women are again typically alone due to visitor restrictions. What will be the psychosocial effect of all of this?
While each culture has unique rituals and processes for managing pregnancy loss, it is considered a universal response to turn towards others during times of grief and loss (Markin and Zilcha-Mano 2018). Thus, not being allowed to have support persons physically present at the time of loss and during the grieving process may significantly complicate one’s mourning. As Rose Carlson of Share Pregnancy and Infant Loss Support noted, “support from loved ones is so crucial during the time of the loss, and a mom giving birth alone with no support to a baby who has died or will die after birth is going to be at great risk for complicated grief and [post-traumatic stress disorder]” (Holohan 2020).
Labor and Delivery
Similar to the lack of conclusive information about the impact of COVID-19 on pregnancy, little is known about the health outcomes for mother’s delivering with confirmed or suspected COVID-19 as studies, to date, have relied on small samples and case studies (Breslin et al. 2020; Chen et al. 2020). Based on limited findings, infection prevention and control considerations impacting labor and delivery (L&D) policies are largely based on information gained from similar virus experiences and these implemented policies have been intentionally cautious until more definitive information is known (The American College of Obstetricians and Gynecology [ACOG] 2020).
At the onset of the pandemic, L&D practices restricted hospital visitors (Society for Maternal–Fetal Medicine 2020; RCOG 2020). Birthing mothers have generally being limited to one healthy support person throughout the duration of the L&D stay (e.g., UCLA Health, Johns Hopkins Medicine).2 However, in instances of a cesarean section (C-section) a support person might not be allowed to be present during delivery (e.g., University of Chicago). Furthermore, in some high COVID-19 prevalence areas, all visitors were eliminated regardless of method of delivery (e.g., New York-Presbyterian and Mount Sinai). This visitor ban was reversed by an executive order on March 28, 2020 to permit one healthy support person following a petition that quickly garnered more than 600,000 signatures (Van Syckle and Caron 2020). It is understandable why restrictions in visitor policies led to psychological stress, as birth is not just a physiological experience. For fathers, being present for childbirth is of particular importance. Many fathers may struggle to fully connect with their baby during pregnancy, as they lack the physiological changes that mothers undergo; as such, many fathers attribute their experience at their child’s birth to be the start of their fatherhood (Poh et al. 2014). Mothers have BPS benefits from this as well. Having a compassionate and trustworthy labor companion to provide continuous support during labor is known to make a significant difference in improving birth experiences and the health and well-being of birthing mothers and babies (Bohren et al. 2019); thus, women should be allowed to have such a person present throughout their L&D stay (RCOG 2020). In a recent study of 1400 pregnant women (Gildner and Thayer 2020), 45.2% reported changing some aspect of their birth plan due to COVID-19 based on concerns of their own (53.9%), their partner (21.9%), family and friends (13.8), and comments from medical providers (60.8%). These statistics not only demonstrate concrete effects of the impact of COVID-19 on L&D, but also the relational factors that influence decision-making.
Early recommendations from the CDC (February 18, 2020) included the separation of mothers with confirmed COVID-19 from her newborn; thus, eliminating opportunity for early contact and direct breastfeeding. Revision has since been made (CDC, April 4, 2020) toward a more neutral stance that now states the decision regarding separation between a mother with known or suspected COVID-19 and her infant be on a “case-by-case basis, using shared decision-making between the mother and clinical team.” This is better aligned with recommendations from WHO (March 13, 2020), RCOG (April 17, 2020), and the National Perinatal Association (NPA; 2020) that suggest mothers be able to engage in decision-making to allow for remaining together while also respecting the unique challenges of doing so.
Participation in childbirth and the parenting tasks of the early sensitive period following birth has demonstrated significant immediate and long-term effects for both mothers and fathers (Brandao and Figueirdeo 2012; Bystrova et al. 2009) Research has demonstrated positive associations for mothers with early and longer contact with their infant with maternal satisfaction and breastfeeding (Redwhaw et al. 2014). Even if a woman is symptomatic, recommendations do not preclude breastfeeding. Instead, both mother and baby may obtain many of the benefits of breastfeeding by engaging in proper hygiene and having the mother either wear a mask during feeding at the breast or expressing milk for another caregiver to provide (CDC 2020b). Additionally, important research has demonstrated long-term positive effects of mother-infant contact versus separation (Bystrova et al. 2009). Importantly, the negative effect of separation after birth was not compensated for by later rooming-in. Furthermore, there are known benefits to fathers and their newborns from the participation of fathers in L&D, such as umbilical cord cutting and skin-to-skin contact (Brandao and Figueirdeo 2012; Shorley et al. 2016). Thus, it would be particularly prudent to have a support person present, particularly in instances in which the mother and baby would need to be separated. A final important consideration of the outcomes from L&D policy changes described above is the potential for trauma.
Prior to the COVID-19, research demonstrated that an upwards of 34% of women report having experienced a traumatic birth (Beck and Watson 2008). While there are often physiological aspects of a traumatic birth (e.g., emergency C-section, medical interventions during birth, lacerations), what is of most importance are the psychosocial experiences during childbirth such as perceiving a lack of personal care, poor communication, feeling powerless, and/or not believing the ends (e.g., a healthy baby) justify the means (e.g., mother-infant separation due to COVID-19 diagnosis in mother) (Beck 2004). Due to the multiple changes to hospital births because of COVID-19, it is probable that rates of traumatic birth will increase, particularly if treatment accommodations are not considered.
Neonatal Intensive Care Unit
A newborn may be admitted to the Neonatal Intensive Care Unit (NICU) following delivery due to factors such as premature birth and/or immediate medical needs. Understandably, admission of a newborn to the NICU is a stressful event that may impact the psychosocial domains of health across the family. Not only are there physiological health concerns for the newborn, but the family experiences loss of expected dreams, increased separation, and financial burdens; thus, parents’ experience of having an infant in a NICU has demonstrated increased stress and vulnerability to emotional difficulties as compared to parents of full-term babies (Clottey and Dillard 2013). Gonulal et al. (2014) found that 38% of NICU mothers and 11% of NICU fathers experienced depression when measured 2-weeks post-delivery; however, with new NICU guidelines in place to combat COVID-19 psychosocial impacts may increase.
Copious hospitals have decreased their number of visitors at the infant’s bedside from two to one at a time, with a maximum of two overall (e.g. University of Chicago, New York Presbyterian, Northwestern Medicine’s Prentice Women’s Hospital). Such restrictions mean that parents must be alone supporting their newborn without the support of their partner or other loved ones. Additionally, some have policies that ban parents altogether (e.g., ProHealth Care, Einstein Health, Methodist Hospitals). For NICUs still allowing visitors, some require the caregiver at bedside to be at the hospital for a minimum of 12 h before switching with another caregiver (e.g. Benioff Children’s Hospital of San Francisco) to minimize the frequency of people coming and going. NICU parents tend to already experience isolation during the time their infant is hospitalized due to a withdrawal of friends and denial responses of well-meaning family members (Lindsay et al. 1993). These new guidelines may present additional challenges for NICU parents as it may intensify their sense of isolation and distress.
Postpartum
Even under the best of conditions, the postpartum transition can be difficult for families, as there is a wide range of BPS, systemic changes and stressors (Shaw et al. 2006). And, with recommendations due to COVID-19 encouraging early discharge post-delivery coupled with social distancing orders, parents are faced with these adjustments almost immediately and oftentimes on their own. Thus, there must be changes to traditional “fourth trimester” treatment plans that generally include in-person support of others to assist with childcare activities and respite care. Research has already demonstrated parents’ altering their fourth trimester plan due to COVID-related concerns such as care disruptions due to shelter-in-place responses (e.g., relocating to be closer to family) and loved ones not being able to visit following birth (Gildner and Thayer 2020). Loneliness created by social distancing may build on other psychosocial stressors experienced by mothers and their families after birth. For example, strained relationships across the family system can impact the adjustment and mental health of families in the postpartum period (Freitas and Fox 2015). Not only is the postpartum period during COVID-19 creating losses and stressors for new parents, but also family members who will now have to put off meeting the newborn for an uncertain length of time. Indeed, there is a true potential for trauma and exacerbation of postpartum mental health issues that may negatively impact the postpartum period for families (NPA 2020).
Recommendations for Care
The COVID-19 pandemic presents an unprecedented threat that will increase the need for emotional and psychological support for individuals within the perinatal period. Typically, 15–20% of women and 10% of men experience perinatal mood and anxiety disorders (PMADs) (Freitas and Fox 2015; Postpartum Support International [PSI] 2020). Social factors that increase the risk for PMADs includes inadequate lack of support, financial stress, and recent losses—all of which are more likely and exacerbated due to COVID-19. Guidelines put out by RCOG (2020) specifically identify the importance of providers recognizing and addressing (BPS) stressors impacting the perinatal period: COVID-19 itself and major changes in the manner in which perinatal care is delivered (biological domain), bereavement and feelings of insecurity and uncertainty (psychological domain), and the impact of social isolation resulting in reduced access to outside support systems (social domain). Despite these recommendations, the ongoing COVID-19 and Reproductive Effects (CARE) study found that 40% of surveyed pregnant mothers, including 25% in their third trimester, reported their provider had not spoken with them about COVID-19 perinatal impacts. We recommend all providers coming into contact with pregnant patients and their support system communicate effectively about the pandemic and what to expect about their care, as well as asking about mental health at every contact across the perinatal period due to the exacerbated BPS stressors. A study by Davenport et al. (2020) found a substantial increase in the likelihood of maternal depression and anxiety during the COVID-19 pandemic for pregnant and post-partum women; thus, recommendations for heightened assessment and treatment is imperative. This is important because serious mental health concerns, such as anxiety and depression, that have significant adverse outcomes for parents and their children develop both during pregnancy and in the postpartum period (Wisner et al. 2013). These effects range the BPS framework: increased risk for preterm birth, cognitive and emotional development delays in infants, and reduced parent–child bonding (Davenport et al. 2020). Individuals who are experiencing psychosocial stressors can then be offered timely mental health services and resources. These resources should be accessible (e.g., telehealth and virtual social support services) and suitable to the stay-at-home orders.
Early predictions on outcomes of COVID-19 are that it will have the largest impact on girls and women both in terms of caregiver burden and health (Husain and Jain 2020; Shane 2020). Thus, caution is advised not to overburden coordination of care on the already stressed pregnant or postpartum mother. The below recommendations are aimed at health professionals to offer avenues to incorporate BPS, systemic considerations.
Telehealth
With visitor restrictions across healthcare settings and social distancing recommendations throughout the perinatal period, a larger responsibility is placed on medical staff to attend to patients both for physical and psychosocial needs. On a basic level, simply acknowledging the psychosocial difficulties families are experiencing due to COVID-19 can help to contain some of the anticipated anxieties (RCOG 2020). Providers taking the lead on such conversations is crucial, as the CARE study found 1 in 5 pregnant women were not comfortable speaking with their provider about COVID-19 related worries (Thayer and Gildner 2020). Reproductive health practices should also be prepared to facilitate appropriate referrals to mental health professionals who are using telehealth in order to increase accessibility to care and maintain social distancing guidelines (IASC 2020).
Overall, attention to perinatal mental health through (telehealth) screening is of particular importance given the additional stressors and changes to birth plans. And, every effort should be made to screen both parents since both parent’s mental health is intimately tied to that of their partner (Freitas and Fox 2015). Furthermore, accessible tele(mental)health options are imperative since treatment seeking for parents in the perinatal period is already lower than the general population (Freitas and Fox 2015; Wisner et al. 2013); rates in the current pandemic in which there may be additional barriers to accessing services is unknown.
Providers offering tele(mental) health treatment must recognize the grief of lost plans around the perinatal period—expectations for what pregnancy, birth, and the postpartum period would look like. As such, providers should work with families to revise their expectations and plans in ways that still honor the aspects that are most important. For example, if a pregnant mother must attend an ultrasound alone and it was important for the partner to participate, the couple could find ways for the partner to be present virtually or for the mother to record important parts of the appointment (e.g., record short audio clip of heartbeat). Additionally, expecting parents should be encouraged to involve partners and other significant supports in the pregnancy in other meaningful ways, such as feeling fetal movements and talking to the baby as additional means of connection (Poh et al. 2014). It is recommended that providers seek guidance from their patient on a variety of the offered care opportunities to include support persons rather than implement a “one size fits all” modification to treatment due to COVID-19.
Virtual Support
Overall, psychosocial support programs have demonstrated improved maternal knowledge, attitudes, and skills related to parenting, mental health, quality of life, and physical health (Shaw et al. 2006). In this time of social distancing it may not be feasible to receive in-person support so it is recommended that perinatal parents utilize virtual support options. Fortunately, research has demonstrated benefits to support received through this medium. During pregnancy, there are apps that can serve as a means of support and psychosocial assessment. The app Veedamom, for example, can provide virtual interventions including mindfulness, psychoeducation, and journaling (Dyurich and Oliver in press). In the postpartum period, findings suggest virtual support forums for new mothers have the ability to facilitate information sharing, act as entertainment, and provide community which is more important than ever in this time of social distancing (Teaford et al. 2019). And, because the transition for fathers is different than that of mothers due to the social construction of masculinity and fatherhood (Freitas and Fox 2015), it is important to help fathers find their own virtual community.
Virtual support can also be extended throughout one’s natural support system. For example, virtual attendance of support persons to important out-patient appointments (e.g., dating scan or anomaly ultrasound) or during the L&D stay can allow everyone to feel more involved in important parts of the perinatal journey. Additionally, for families with a newborn in the NICU some hospitals have created opportunities to virtually visit the baby. For example, at Northwestern Medicine where there in-person visitor restrictions are in place, they offer a virtual platform that allows parents to check in on their babies when they are unable to be there in-person, as well as receive emotional support and psychoeducation (Samuelson 2020). Finally, families can receive access to virtual doula services, which can include education; comforting affirmations; and support throughout pregnancy, birth, and postpartum (Evidence Based Birth 2020). This may be particularly beneficial given that hospitals are restricting birthing mothers to choose one healthy support person (Society for Maternal–Fetal Medicine 2020; RCOG 2020). Consequently, this one person must serve all the various roles of BPS support that may have otherwise been extended across individuals. That is, companions during labor have been shown to provide the birth mother with a range of supports: providing information and communicating with providers, advocating for birth mother’s wishes, practical support and guidance through comfort measures, and emotional support (Bohren et al. 2019). Therefore, it would be important to make clear what roles are expected of the in-person support person and how virtual supports, who are unable to be physically present during L&D, can complement care.
Limitations
The absence of the spiritual domain of the BPSS model in consideration of the perinatal period is an acknowledged limitation from the outset of this review. The authors recognize the importance of inclusion of the spiritual domain especially in consideration of the support religion, faith, and/or spirituality can provide in times of stress and loss, as well as a support in managing physiological experiences, such as pain (e.g. Sisson 2011; Wachholtz and Pargament 2004; Weich et al. 2008). Though we value the incorporation of spirituality, access to a deeper understanding of beliefs, meaning-making, and values specific to the perinatal period during COVID-19 was limited and serves as a recommendation for future research.
Due to the novelty of COVID-19 and limited access to current and conclusive data on specifics of its impact, an additional limitation is in terms of equity. Data around diagnosis, fatality, and recovery from COVID-19 has already shown skewed outcomes amongst people of color and across lower socioeconomic status populations (Bowen 2020; CDC 2020a; Hedgpeth et al. 2020; Johnson and Buford 2020; Olumhense and Choi 2020), as these women experience increased burdens from systemic racism in healthcare and society, at large, as well as socioeconomic factors impacting their ability to seek care. These early reports on impact parallels confirmed findings in perinatal healthcare for women of color and lower socioeconomic status around equity and access (Lu and Halfon 2003). COVID-19 has impacted the reproductive journeys across social locations in disproportionate ways and we recognize many of our recommendations for care include assumptions of privilege in terms of access and resources. As a clearer picture emerges of the true toll of COVID-19 on the perinatal period, future research must view data utilizing a social justice lens so that we may better understand how to modify the broad application of guidelines to better meet the nuances of different affected populations.
Future Research
With time, our hope is that the included recommendations for care will become obsolete as the health threat of COVID-19 decreases and strict guidelines around social distancing is lifted. This article serves as a response to the urgency of the current pandemic to facilitate better outcomes for perinatal families and urged consideration of the psychosocial, systemic impact of changes to perinatal health policies. In hindsight of this pandemic, the authors recommend longitudinal studies on conception and birth during this health pandemic to broaden the understanding of any pandemic on the perinatal period. Question for future research include:
How did changes to traditional perinatal healthcare and social distancing practices impact the psychosocial experience of pregnancy, L&D, and the “fourth trimester” for women and families?
How did the suspension and modifications to fertility treatments impact individuals and couples at their different stages of intervention?
How did a lack of access and decreased availability of contraception impact conception during the pandemic in regards to decision-making and rates of (un)planned pregnancies?
What was the perinatal experience of Women of Color (both those infected and not) during the COVID-19 pandemic?
How have restrictions around prenatal visits, L&D, and NICU stays impacted parent–child attachment in the prenatal and postpartum periods?
Conclusion
Perinatal research on the impact of viruses similar to COVID-19 provides an understanding of the need for specific recommendations in response to the current health pandemic, as provided in this article. Data is in flux and evidence based/outcome research is not yet possible due to the limited timeframe, with the U.S. entering shutdown only in March 2020. Though this article utilized historical and confirmed understandings of the importance of BPS consideration and support systems on health outcomes, actual outcomes of this unprecedented time have yet to unfold.
Footnotes
Due to the rapidly changing landscape of the COVID-19 pandemic, information is constantly evolving. This paper was submitted on May 17, 2020 and revised on July 6, 2020. Importantly, even if changes occur in the information presented here, significant numbers of individuals were impacted by the policies and data that existed at the time of writing this paper.
Readers can search visitor hospital policies related to COVID-19 at Birth Monopoly’s Hospital Policy Tracker: Doulas and Visitors (United States): https://birthmonopoly.com/covid-19/
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Aamar RO, Kolobova I. Biopsychosocial model in couple and family therapy. In: Lebow J, Chambers A, Breunlin D, editors. Encyclopedia of couple and family therapy. Cham: Springer; 2016. [Google Scholar]
- Ahmed, Z., & Sonfeld, A. (2020). The COVID-19 outbreak: Potential fallout for sexual and reproductive health and rights. Guttmacher Institute. Retrieved May 15, 2020 from https://www.guttmacher.org/article/2020/03/covid-19-outbreak-potential-fallout-sexual-and-reproductive-health-and-rights.
- Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, Tao Q, Sun Z, Xia L. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: A report of 1014 cases. Radiology. 2020 doi: 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Society for Reproductive Medicine. (2020). Patient management and clinical recommendations during the Coronavirus (COVID-19) pandemic. Retrieved from https://www.asrm.org/news-and-publications/covid-19/statements/patient-management-and-clinical-recommendations-during-the-coronavirus-covid-19-pandemic/.
- Baud D, Greub G, Favre G, Gengler C, Jaton K, Dubruc E, Pomar L. Second-trimester miscarriage in a pregnant woman with SARS-CoV-2 infection. JAMA. 2020 doi: 10.1001/jama.2020.7233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck CT. Birth trauma: In the eye of the beholder. Nursing Research. 2004;53(1):28–35. doi: 10.1097/00006199-200401000-00005. [DOI] [PubMed] [Google Scholar]
- Beck CT, Watson S. Impact of birth trauma on breast-feeding: A tale of two pathways. Nursing Research. 2008;57(4):228–236. doi: 10.1097/01.NNR.0000313494.87282.90. [DOI] [PubMed] [Google Scholar]
- Boelig R, Saccone G, Bellussi F, Berghella V. MFM guidance for COVID-19. American Journal of Obstetrics & Gynecology MFM. 2020 doi: 10.1016/j.ajogmf.2020.100106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohren MA, Berger BO, Munthe-Kaas H, Tuncalp O. Perceptions and experiences of labour companionship: a qualitative evidence synthesis. Cochrane Database of Systematic Reviews. 2019 doi: 10.1002/14651858.CD012449.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen, A. (2020). Of the COVID-19 pregnancy cases reported in Illinois, Black and Latina women make up over 70%. Chicago Tribune. Retrieved July 6, 2020 from https://www.chicagotribune.com/coronavirus/ct-life-coronavirus-hispanic-black-moms-pregnant-women-covid-20200702-opoekt3avvbqvfkf3caxtvrnkm-story.html.
- Brandao, S., & Figueirdeo, B. (2012). Fathers' emotional involvement with the neonate: Impact of the umbilical cord cutting experience. Journal of Advanced Nursing. 10.1111/j.1365-2648.2012.05978.x. [DOI] [PubMed]
- Breslin N, Baptiste C, Gyamfi-Bannerman C, Miller R, Martinez R, Bernstein K, Ring L, Landau R, Purisch S, Friedman AM, Fuchs K, Sutton D, Andrikopoulou M, Rupley D, Sheen J, Aubey J, Zork N, Moroz L, Mourad M, Wapner R, Simpson LL, D’Alton ME, Goffman D. COVID-19 infection among asymptomatic and symptomatic pregnant women: Two weeks of confirmed presentations to an affiliated pair of New York City hospitals. American Journal of Obstetrics & Gynecology MFM. 2020 doi: 10.1016/j.ajogmf.2020.100118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bystrova K, Ivanova V, Edhborg M, Matthisen A, Ransjo-Arvidson A, Mukhamedrakhimov R, Uvnas-Moberg K, Widstrom A. Early contact versus separation: Effects on mother-infant interaction one year later. Birth Issues in Perinatal Care. 2009 doi: 10.1111/j.1523-536X.2009.00307.x. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2020a). Data on COVID-19 during pregnancy. Retrieved July 6, 2020 from https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/special-populations/pregnancy-data-on-covid-19.html.
- Centers for Disease Control and Prevention. (2020b). Coronavirus Disease 2019: Pregnancy & breastfeeding. Retrieved July 6, 2020 from https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/pregnancy-breastfeeding.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fprepare%2Fpregnancy-breastfeeding.html.
- Centers for Disease Control and Prevention (2020c). Assisted reproductive technology (ART). Retrieved July 6, 2020 from https://www.cdc.gov/art/artdata/index.html.
- Chen H, Guo J, Wang C, Luo F, Yu X, Zhang W, Li J, Zhao D, Xu D, Gong Q, Liao J, Yang H, Hou W, Zhang Y. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: A retrospective review of medical records. Lancet. 2020;395(10226):809–815. doi: 10.1016/S0140-6736(20)30360-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clottey M, Dillard DM. Post-traumatic stress disorder and neonatal intensive care. International Journal of Childbirth Education. 2013;28(3):23–29. [Google Scholar]
- Cousineau TM, Domar AD. Psychological impact of infertility. Best Practice & Research Clinical Obstetrics & Gynaecology. 2007;21(2):293–308. doi: 10.1016/j.bpobgyn.2006.12.003. [DOI] [PubMed] [Google Scholar]
- Davenport MH, Meyer S, Meah VL, Strynadka MC, Khurana R. Moms are not ok: COVID-19 and maternal mental health. Frontiers in Global Women’s Health. 2020 doi: 10.3389/fgwh.2020.00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diamond DJ, Diamond MO. Understanding and treating the psychosocial consequences of pregnancy loss. In: Wenzel A, editor. The Oxford handbook of perinatal psychology. Oxford: Oxford University Press; 2016. pp. 487–523. [Google Scholar]
- Diamond RM, Roose RE. Development and evaluation of a peer support program for parents facing perinatal loss. Nursing for Women’s Health. 2016;20(2):146–156. doi: 10.1016/j.nwh.2016.02.001. [DOI] [PubMed] [Google Scholar]
- Dyurich, A., & Oliver, M. (in press). Use of the Veedamom electronic app as a pregnancy treatment companion. Journal of Feminist Family Therapy.
- Ellington S, Strid P, Tong VT, Woodworth K, Galang RR, Zambrano LD, Nahabedian J, Anderson K, Gilboa S. Characteristics of women of reproductive age with laboratory-confirmed SARS-CoV-2 infection by pregnancy status—United States, January 22–June 7, 2020. Morbidity and Mortality Weekly Report. 2020;69(25):769–775. doi: 10.15585/mmwr.mm6925a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engel GL. The need for a new medical model: A challenge for biomedicine. Science. 1977;196:129–136. doi: 10.1126/science.847460. [DOI] [PubMed] [Google Scholar]
- Engel GL. The clinical application of the biopsychosocial model. The American Journal of Psychiatry. 1980;137(5):535–544. doi: 10.1176/ajp.137.5.535. [DOI] [PubMed] [Google Scholar]
- Evidence Based Birth. (2020). Coronavirus COVID-19: Evidence Based Birth resource page. Retrieved May 10, 2020 from https://evidencebasedbirth.com/covid19/.
- Freitas CJ, Fox CA. Fathers matter: Family therapy’s role in the treatment of paternal peripartum depression. Contemporary Family Therapy. 2015;37:417–425. doi: 10.1007/s10591-015-9347-5. [DOI] [Google Scholar]
- Gildner TE, Thayer ZM. Birth plan alterations among American women in response to COVID-19. Health Expectations. 2020;00:1–3. doi: 10.1111/hex.13077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonulal D, Yalaz M, Altun-Köroğlu Ö, Kültürsay N. Both parents of neonatal intensive care unit patients are at risk of depression. Turkish Journal of Pediatrics. 2014;56(2):171–176. [PubMed] [Google Scholar]
- Hedgpeth, D., Fears, D., & Scruggs, G. (2020). Indian country, where residents suffer disproportionately from disease, is bracing for coronavirus. The Washington Post. Retrieved May 10, 2020 from https://www.washingtonpost.com/climate-environment/2020/04/04/native-american-coronavirus/
- Hodgson, J., Lamons, A.L., Reese, L. (2007). The biopsychosocial-spiritual interview method. In D. Linville & K. M. Hertlein (Eds.), The therapist's notebook for family health care. (pp. 3–12). Philadelphia: The Haworth Press.
- Holohan, M. (2020). Women endure pregnancy loss alone as hospitals bar visitors during COVID-19. Today. Retrieved May 10, 2020 from https://www.today.com/parents/covid-19-hospital-changes-mean-many-deal-loss-alone-t177724
- Husain, I., & Jain, S. (2020). The mother of all burdens: COVID-19 and physician parents. Ms. Retrieved May 15, 2020 from https://msmagazine.com/2020/04/01/the-mother-of-all-burdens-covid-19-and-physician-parents/?utm_campaign=SocialWarfare&utm_medium=social&utm_source=twitter
- Imber-Black, E. (2002). Family rituals—From research to the consulting room and back again: Comment on the special section. Journal of Family Psychology, 16(4), 445–446. 10.1037/0893-3200.16.4.445. [DOI] [PubMed]
- Inter-Agency Standing Committee. (2020). Interim briefing note: Addressing mental health and psychosocial aspects of COVID-19 outbreak. Retrieved from https://interagencystandingcommittee.org/system/files/2020-03/MHPSS%2520COVID19%2520Briefing%2520Note%25202%2520March%25202020-English.pdf.
- Jaffe J, Diamond MO. Reproductive trauma: Psychotherapy with infertility and pregnancy loss clients. Washington: American Psychological Association; 2011. [Google Scholar]
- Johnson, A., & Buford, T. (2020). Early data shows African Americans have contracted and died of coronavirus at an alarming rate. ProPublica. Retrieved May 15, 2020 from https://www.propublica.org/article/early-data-shows-african-americans-have-contracted-and-died-of-coronavirus-at-an-alarming-rate
- Johns Hopkins University & Medicine. (2020). Coronavirus resource center. Retrieved July 6, 2020 from https://coronavirus.jhu.edu/data.
- Koopmans L, Wilson T, Cacciatore J, Flenady V. Support for mothers, fathers and families after perinatal death. The Cochrane Database of Systematic Reviews. 2013 doi: 10.1002/14651858.CD000452.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leigh-Hunt N, Bagguley D, Bash K, Turner V, Turnbull S, Valtorta N, Caan W. An overview of systematic reviews on the public health consequence of social isolation and loneliness. Public Health. 2017;152:157–171. doi: 10.1016/j.puhe.2017.07.035. [DOI] [PubMed] [Google Scholar]
- Lindsay JK, Roman L, DeWys M, Eager M, Levick J, Quinn M. Creative caring in the NICU: Parent-to-parent support. Neonatal Network: NN. 1993;12(4):37–44. [PubMed] [Google Scholar]
- Lu MC, Halfon N. Racial and ethnic disparities in birth outcomes: A life course perspective. Maternal and Child Health Journal. 2003;7(1):13–30. doi: 10.1023/A:1022537516969. [DOI] [PubMed] [Google Scholar]
- Markin RD, Zilcha-Mano S. Cultural processes in psychotherapy for perinatal loss: Breaking the cultural taboo against perinatal grief. Psychotherapy. 2018;55(1):20–26. doi: 10.1037/pst0000122. [DOI] [PubMed] [Google Scholar]
- McDaniel, S. H., Doherty, W. J., & Hepworth, J. (2014). Medical family therapy and integrated care (2nd ed.). Washington: American Psychological Association.
- Miscarriage Association. (2020). Coronavirus and miscarriage: Your care. Retrieved May 10, 2020 from https://www.miscarriageassociation.org.uk/information/information-on-coronavirus-covid-19/.
- National Institutes of Health. (2018). How common is infertility? Retrieved May 10, 2020 from https://www.nichd.nih.gov/health/topics/infertility/conditioninfo/common.
- National Perinatal Association. (2020). Mothers with COVID-19 and their newborn infants: Joint position paper. The National Association of Neonatal Nurses and the National Perinatal Association. Retrieved May 5, 2020 from http://www.nationalperinatal.org/resources/Documents/COVID-19/COVID-19_NPA%20and%20NANN.pdf.
- Olumhense, E., & Choi, A. (2020). Bronx residents twice as likely to die from COVID-19 in NYC. The City. Retrieved May 15, 2020 from https://thecity.nyc/2020/04/bronx-residents-twice-as-likely-to-die-from-covid-19-in-nyc.html.
- Poh HL, Koh SSL, He HG. An integrative review of fathers’ experiences during pregnancy and childbirth. International Nursing Review. 2014;61:543–554. doi: 10.1111/inr.12137. [DOI] [PubMed] [Google Scholar]
- Postpartum Support International. (2020). Pregnancy & postpartum mental health overview. Retrieved May 10, 2020 from https://www.postpartum.net/learn-more/pregnancy-postpartum-mental-health/.
- Pote H, Stratton P, Cottrell D, Boston P, Shapiro D, Hanks H. The Leeds Systemic Family Therapy Manual. LFTRC: Leeds; 2000. [Google Scholar]
- Purdy, C. (2020). Opinion: How will COVID-19 affect global access to contraceptives – and what can we do about it? Devex. Retrieved May 10, 2020 from https://www.devex.com/news/opinion-how-will-covid-19-affect-global-access-to-contraceptives-and-what-can-we-do-about-it-96745.
- Raschky, P. and Wang, L.C. (2012). Reproductive behavior at the end of the world: The effect of the Cuban missile crisis on U.S. fertility. 10.2139/ssrn.2175387.
- Redshaw M, Hennegan J, Kruske S. Holding the baby: Early mother–infant contact after childbirth and outcomes. Midwifery. 2014;30(5):e177–e187. doi: 10.1016/j.midw.2014.02.003. [DOI] [PubMed] [Google Scholar]
- Royal College of Obstetricians & Gynaecologists. (2020). Coronavirus (COVID-19) infection in pregnancy: Information for healthcare professionals (Version 8). Retrieved May 10, 2020 from https://www.rcog.org.uk/globalassets/documents/guidelines/2020-04-17-coronavirus-covid-19-infection-in-pregnancy.pdf.
- Saccone G, Florio A, Aiello F, Venturella R, De Angelis MC, Locci M, Bifulco G, Zullo F, Di Spiezio SA. Psychological impact of COVID-19 in pregnant women. American Journal of Obstetrics and Gynecology. 2020 doi: 10.1016/j.ajog.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samuelson, K. (2020). New app allows NICU families to ‘visit’ baby during COVID-19 pandemic. Northwestern Now. Retrieved May 10, 2020 from https://news.northwestern.edu/stories/2020/03/nicu-app-limited-visitation-covid-19/.
- Schuettge, A., (2020). My husband and I want to have another baby. The pandemic has disrupted our plans. Time. Retrieved May 10, 2020, from https://time.com/5825663/coronavirus-getting-pregnant/.
- Shane, C. (2020). Economics of a pandemic: In times of distress, girls and women are the biggest losers. Fortune. Retrieved May 10, 2020 from https://fortune.com/2020/04/02/coronavirus-women-girls-gender-equality-economy.
- Shaw E, Levitt C, Wong S, Kaczorowski J, The McMaster University Postpartum Research Group Systematic review of the literature on postpartum care: Effectiveness of postpartum support to improve maternal parenting, mental health, quality of life, and physical health. Birth. 2006;33(3):210–220. doi: 10.1111/j.1523-536X.2006.00106.x. [DOI] [PubMed] [Google Scholar]
- Shorley S, Hong-Gu H, Morelius E. Skin-to-skin contact by fathers and the impact on infant and paternal outcomes: An integrative review. Midwifery. 2016;20:207–217. doi: 10.1016/j.midw.2016.07.007. [DOI] [PubMed] [Google Scholar]
- Sisson, L. (2011). The relationship between spirituality and postpartum pain. Dissertation.
- Slade A, Cohen LJ, Sadler LS, Miller M. The psychology and psychopathology of pregnancy: Reorganization and transformation. In: Zeanah CH, editor. Handbook of infant mental health. 3. New York: Guilford Press; 2009. [Google Scholar]
- Society for Maternal-Fetal Medicine. (2020). Society for Maternal-Fetal Medicine and Society for Obstetric and Anesthesia and Perinatology Labor and Delivery COVID-19 Considerations. Retrieved May 10, 2020 from https://s3.amazonaws.com/cdn.smfm.org/media/2319/SMFM-SOAP_COVID_LD_Considerations_-_revision_4-14-20_PDF_(003).pdf.
- Soma-Pillay P, Catherine NP, Tolppanen H, Mebazaa A. Physiological changes in pregnancy. Cardiovascular Journal of Africa. 2016;27(2):89–94. doi: 10.5830/CVJA-2016-021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone, L. (2020) Will the coronavirus spike births? Institute for Family Studies. Retrieved from https://ifstudies.org/blog/will-the-coronavirus-spike-births.
- Sutton D, Fuchs K, D’Alton M, Goffman D. Universal screening for SARS-CoV-2 in women admitted for delivery. New England Journal of Medicine. 2020 doi: 10.1056/NEJMc2009316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thayer, Z.M., & Gildner, T.E. (2020). COVID-19 and reproductive effects (CARE) study. Dartmouth. Retrieved July 6, 2020 from https://sites.dartmouth.edu/care2020/research-results/.
- Teaford D, McNiesh S, Goyal D. New mothers’ experience with online postpartum forums. MCN: The American Journal of Maternal/Child Nursing. 2019;44(1):40–45. doi: 10.1097/NMC.0000000000000489. [DOI] [PubMed] [Google Scholar]
- The American College of Obstetricians and Gynecologists. (2020). Novel Coronavirus 2019 (COVID-19): Practice Advisory. Retrieved May 10, 2020 from https://www.acog.org/en/Clinical/Clinical%20Guidance/Practice%20Advisory/Articles/2020/03/Novel%20Coronavirus%202019.
- Van Syckle, K., & Caron, C. (2020). Women will not be forced to be alone when they are giving birth. New York Times. Retrieved May 10, 2020 from https://www.nytimes.com/2020/03/28/parenting/nyc-coronavirus-hospitals-visitors-labor.html.
- von Bertalanffy L. General system theory: Foundations, development, applications. New York: George Braziller; 1968. [Google Scholar]
- Wachholz A, Pargament K. Is spirituality a critical ingredient of meditation? Comparing the effects of spiritual meditation, secular meditation, and relaxation on spiritual, psychological, cardiac, and pain outcomes. Journal of Behavioral Medicine. 2004;28(4):369–383. doi: 10.1007/s10865-005-9008-5. [DOI] [PubMed] [Google Scholar]
- Weich K, Farias M, Kahane G, Shackel N, Tiede W, Tracey I. An fMRI student measuring analgesia enhanced by religion as a belief system. Pain. 2008;139(2):467–476. doi: 10.1016/j.pain.2008.07.03. [DOI] [PubMed] [Google Scholar]
- Weigel, G. (2020). Novel Coronavirus “COVID-19”: Special Considerations for Pregnant Women. Retrieved May 10, 2020 from https://www.kff.org/womens-health-policy/issue-brief/novel-coronavirus-covid-19-special-considerations-for-pregnant-women/.
- Wisner KL, Sit DKY, McShea MC, Rizzo DR, Zoretich RA, Hughes CL, Eng HF, Luther JF, Wisniewski SR, Costantino ML, Confer AL, Moses-Kolko EL, Famy CS, Hanusa BH. Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. JAMA Psychiatry. 2013;70(5):490–498. doi: 10.1001/jamapsychiatry.2013.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2020). Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected. Retrieved May 10, 2020 from https://www.WHO/2019-nCoV/clinical/2020.4.
- Wright LM, Watson WL, Bell JM. Beliefs: The heart of healing in families and illness. New York: Basic Books; 1996. [Google Scholar]
- Yan, J., Guo, J., Fan, C., Juan, J., Yu, X., Li, J., Feng, L., Li, C., Chen, H., Qiao, Y., Lei, D., Wang, C., Xiong, G., Xiao, F., He, W., Pang, Q., Hu, X., Wang, S., Chen, D., …,Yang, H. (2020). Coronavirus disease 2019 (COVID-19) in pregnant women: A report based on 116 cases. American Journal of Obstetrics and Gynecology10.1016/j.ajog.2020.04.014. [DOI] [PMC free article] [PubMed]
- Zaigham M, Andersson O. Maternal and Perinatal Outcomes with COVID-19: A systematic review of 108 pregnancies. Acta Obstetricia et Gynecologica Scandinavica. 2020 doi: 10.1111/aogs.13867. [DOI] [PMC free article] [PubMed] [Google Scholar]