Abstract
COVID-19 affected our mental health as well as our physical health. In this study, the anxiety and hopelessness levels of healthcare workers and non-healthcare workers and the factors affecting them were evaluated in Turkey. Beck Hopelessness Scale and State-Trait Anxiety Inventory (STAI) was applied online to participants. Totally 2156 individuals were included in the study and 52.0% (n:1121) of them are healthcare workers. The hopelessness and state anxiety levels of healthcare workers were higher than non-healthcare workers. Nurses' hopelessness levels are higher than doctors, and state anxiety levels are higher than both doctors and other healthcare workers. Anxiety and hopelessness levels were higher in women, those living with a high-risk individual at home during the pandemic, those who had difficulty in caring for their children, and those whose income decreased. Anxiety levels are an important predictor of hopelessness. The increase in anxiety levels explained 28.9% of the increase in hopelessness levels. Increased working hours is one of the important factors affecting anxiety. As a conclusion, healthcare workers were more affected psychologically in the COVID-19 pandemic compared to the society. Nurses were affected more than other healthcare workers. It is important to identify the factors affecting anxiety, hopelessness, and individuals who may be more psychologically affected during the pandemic. An important contribution can be made to the protection of public health by ensuring that psychosocial interventions for high-risk groups are planned in advance.
Keywords: COVID-19, Mental health, Anxiety, Hopelessness, Healthcare workers
1. Introduction
An pandemic described as occurring worldwide or over a very wide area, crossing international boundaries, and usually affecting a large number of people (Porta, 2014). Pandemic expresses an extraordinary situation and during this period, problems may arise in terms of feeding, sheltering and basic needs besides being affected by the disease. In the periods of pandemic, in addition to physical health, the mental health of the society can be significantly affected (Fiorillo and Gorwood, 2020). Anxiety of being ill, social and economic problems, and being under quarantine can cause more anxiety and depressive symptoms in individuals during pandemic (Brooks et al., 2020; Fiorillo and Gorwood, 2020; Shah et al., 2020; Shigemura et al., 2020). It is known that there is an increase in anxiety disorders, mood disorders, and psychiatric disorders such as post-traumatic stress disorder after outbreaks (Taylor, 2019). COVID-19, which was first announced to the world by the World Health Organization (WHO) on December 31, 2019 as a new viral pneumonia, and then became a pandemic, is one of the most serious pandemics experienced in the last decades. The COVID-19 outbreak has spread rapidly around the world. In the fifth month of the outbreak (12 May 2020), 4.088.848 people were infected and 283.153 people died (WHO). In Turkey, the first case was reported on March 11, 2020 and until the date of May 12, 2020, 141.475 people became ill and 3.894 people died (Republic of Turkey Ministry of Health Corona Table, 2020). Many healthcare workers in our country and in the world became ill during the pandemic and died among them. This rapid spread has caused serious measures to be taken in many countries. International flights are terminated, border gates are closed, curfews have begun. Due to the prevalence of COVID-19, unlike other traumas, safe place perception for people has disappeared. The exact course of the disease is not known, its severity and duration cannot be predicted, the lack of a definitive treatment method and vaccine, and the risk of high mortality can create anxiety and hopelessness about the future. Hopelessness is defined as follows: the feeling that any effort aimed at constructive change in a patient's illness is doomed before it is even attempted (Shea and Hurley, 1964).
It is known that there are psychological effects in healthcare workers and society after epidemics. Previously, studies on the psychological effects of pandemics have been carried out. It was mentioned that there is a need for hospital administrators to be aware of the extent and sources of stress and psychological distress among frontline healthcare workers during severe acute respiratory syndrome (SARS) outbreak (Tam et al., 2004). In a large survey study investigating the psychosocial effects of SARS on hospital staff, four factors were identified as being significantly associated with the presence of emotional distress: being a nurse, part-time employment status, lifestyle affected by SARS outbreak and ability to do one's job affected by the precautionary measures (Nickell et al., 2004). However, there are currently a limited number of studies on the effect of COVID-19 pandemic, on which the whole world fights, on the mental state and anxiety levels of individuals. In a study, it was stated that isolation of health workers from their families, changing their routines and narrowing social support networks during COVID-19 pandemic may cause mental problems. In the same study, it was reported that there may be different psychological effects such as feelings of loneliness, helplessness, stress, irritability, physical and mental fatigue, and hopelessness (Huang et al., 2020). In a study conducted in China, a considerable proportion of health care workers reported experiencing symptoms of depression, anxiety, insomnia, and distress, especially women, nurses and front-line health care workers directly engaged in diagnosing, treating, or providing nursing care to patients with suspected or confirmed COVID-19 (Lai et al., 2020). This is the first comparative study that evaluates the psychological effects of COVID-19 pandemic in both healthcare workers and other community samples. The main purpose of the study is to evaluate the factors affecting the anxiety and hopelessness levels of healthcare professionals and to compare this with those of non-healthcare professionals. The results of this study will guide the determination of the effect of the pandemic on the level of anxiety and hopelessness, and the planning of psychiatric treatments as well as treatments for physical symptoms for pandemics. It is also thought that study data will contribute to the implementation of preventive mental health services for individuals who are psychologically healthy.
2. Material and method
2.1. Procedure
This research is a cross-sectional study in which the scales are applied online in order to evaluate the state and trait anxiety levels and hopelessness levels of healthcare workers and the society during the pandemic period and to determine the factors affecting them. The sociodemographic data form created by the researchers, State Trait Anxiety Scale (STAI) and Beck Hopelessness Scale (BHS) were created in Google Documents and delivered to both healthcare workers and non-healthcare workers via social media.
2.2. Sample
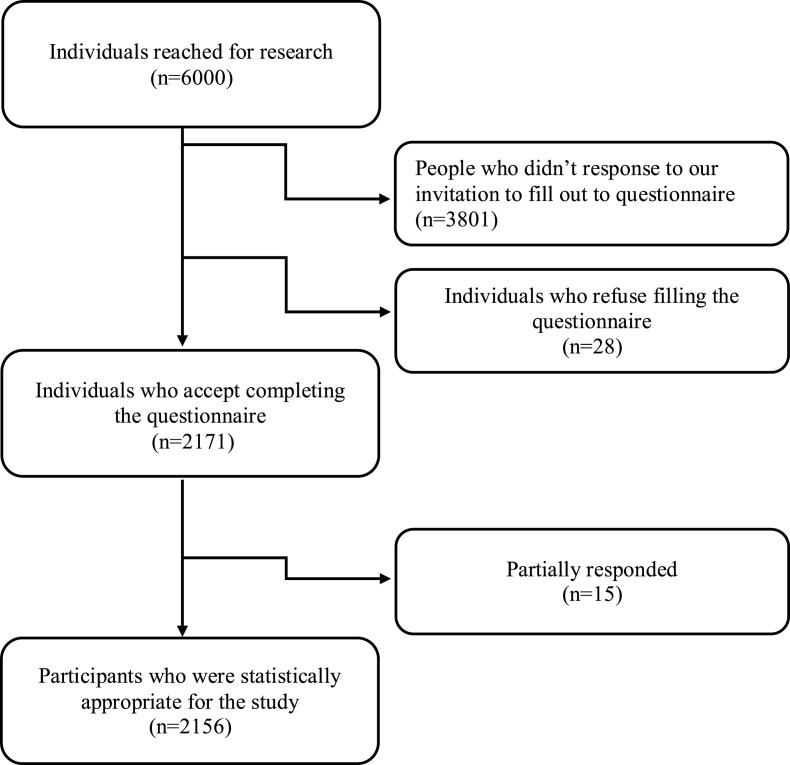
Forms for the study were delivered to a total of 6000 people, including 20,000 people who are not healthcare workers (society) and 15,000 people who are healthcare workers in social media groups. A form was delivered to 3000 people from both groups. A total of 2156 volunteer individuals, 1121 healthcare workers and 1035 non-healthcare workers, participated in the study (Fig. 1 ). When Confidence Level was determined as 99% and Confidence Interval as 5% in power analysis, it was found sufficient to include at least 656 people to the study.
Fig. 1.
Flow chart of participants included in the study.
2.3. Data collection tools
All data collection tools were delivered to individuals between April 1–15, 2020 and filled in online with the Google Documents application. If socio-demographic data and those whose scales were filled completely in application were evaluated. Missing or abandoned forms were not evaluated. Also, individuals with a known psychiatric illness and treatment were not included in the study.
The individuals who agreed to participate in the study were informed about the study and were asked to provide their electronic informed consent. After informed consent, those who agreed to participate in the study were able to continue to filling the scales. The data collection process was performed in accordance with the rules of the Declaration of Helsinki. The study was approved by the Yozgat Bozok University Ethics Committee (2017-KAEK-189_2020.04.09_07). All participants were informed that their information was coded and was kept confidential.
2.3.1. Sociodemographic and descriptive data form
It was created by researchers and includes the following information about the participants: age, gender, whether there are healthcare workers, occupation of healthcare workers, frequency of handwashing, level of anxiety, change in income status, whether there are individuals from the high-risk group at home, having difficulty in childcare.
2.3.2. State-Trait Anxiety Inventory
It was developed by Spielberger et al., in 1970, and has two subscales: state (STAI-S) and trait (STAI-T) (Spielberger et al., 1970). There are 40 items in total, 20 items in each scale. STAI-S determines how the individual feels at a certain moment and under certain conditions. STAI-T generally determines how the individual feels, regardless of the situation and circumstances. The answers are scored between 1 and 4 on the 4-point Likert scale, and high scores indicate that the level of anxiety is high. The scale was adapted to Turkish by Öner and Le Compte in 1983 (Öner and Le Compte, 1998).
2.3.3. Beck Hopelessness Scale
It was developed by Beck et al., in 1974 (Beck et al., 1974). It is used to determine the negative expectations of the individual for the future. Turkish validity and reliability study was done by Seber et al. (Seber et al., 1993). Durak has been reworked on the scale's validity, reliability and factor structure (Durak and Palabıyıkoğlu, 1994). BHS consists of 20 items and each question is scored between 0 and 1. In high scores, the level of hopelessness in the individual is assumed to be high.
2.4. Statistical analysis
The data were analyzed with SPSS 22 program (Statistical Package for Social Sciences, IBM Inc., Chicago, IL, USA). Histogram, Skewness and Kurtosis values were used in addition to Kolmogorov-Smirnov test for normality distribution. Chi-square was used to compare categorical groups. In correlation evaluation, Pearson correlation for normal distribution values and Spearman correlation for those without normal distribution values were performed.
Independent Samples T-Test was used to compare the averages of two independent groups with normal distribution and Mann Whitney U test was used to compare the median of two independent groups with no normal distribution. There is a difference between the average age and gender ratio of those who are healthcare workers and non-healthcare workers. Additionally, because of the age and gender were related to hopelessness, STAI-S and STAI-T levels, Multiple Analysis of Covariance (MANCOVA) was applied in all comparisons as age and gender were covariate. A post-hoc Bonferroni test was applied to determine which groups the difference is from. In gender comparison, only age was taken as a covariate and in age comparison, only gender was taken as a covariate. Kruskal Wallis H Test was used for independent 3-group comparisons of scales that did not show normal distribution. In cases where there is a significant difference between the groups, two groups were compared and Bonferroni correction was applied to determine the difference between which groups. Logistic regression was performed to determine the factors affecting hand washing and anxiety increase, and multiple regression analysis was conducted to evaluate the level of predicting STAI's increase in the level of BHS. Significance level was accepted if p < 0.05.
3. Results
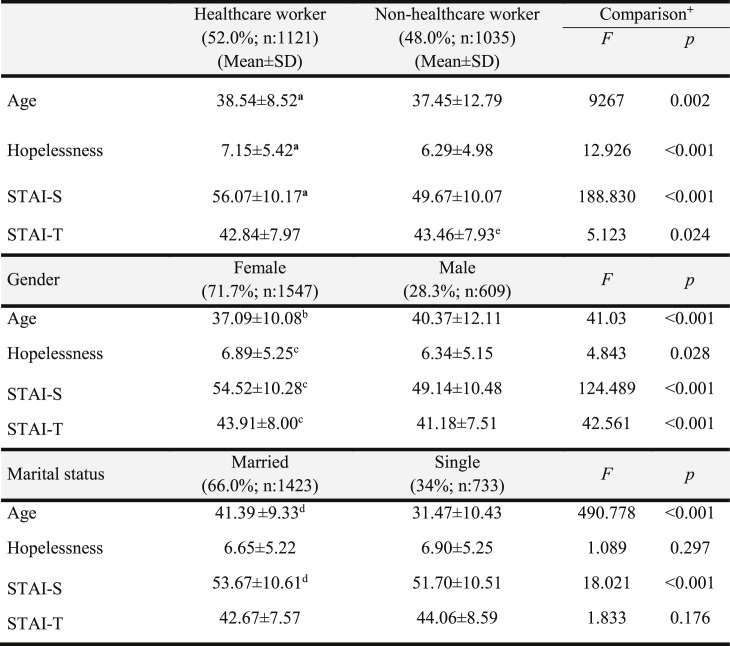
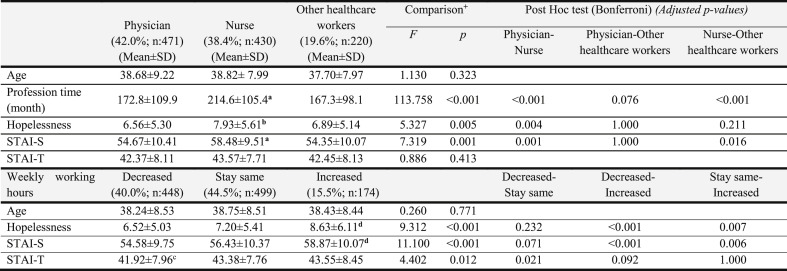
The sample of this study consists of 2156 participants (mean age: 38.03 ± 10.80). Of the participants, 52.0% (n:1121) were healthcare workers, 48.0% (n:1035) were non-healthcare workers. The age range of health workers was 21–68 years, and non-health workers was 18–70 years. The hopelessness and STAI-S levels of the healthcare workers were found to be significantly higher than the non-healthcare workers (p < 0.001) (Table 1 ). The STAI-T levels of the non-healthcare workers were found to be significantly higher than the healthcare workers (p = 0.024) (Table 1). Among healthcare workers, 42.0% of them are doctors, 38.4% of them are nurses, 19.6% of them are other healthcare workers. Age, working time, hopelessness and anxiety levels of healthcare workers are shown in Table 2 . When the MANCOVA method is applied by taking the gender and age covariant in the comparison of hopelessness, STAI-S and STAI-T levels according to the duties of the healthcare workers, hopelessness (p = 0.005) and STAI-S (p = 0.001) levels were statistically different among the healthcare workers. Post-hoc Bonferroni Test was applied to determine from which groups the difference is from. Nurses' hopelessness levels were found to be significantly higher than doctors (p = 0.004). STAI-S levels in nurses were found significantly higher than doctors (p = 0.001) and other healthcare professionals (p = 0.016). No statistically significant difference was found among the healthcare professionals in terms of STAI-T levels (Table 2).
Table 1.
Comparison of age, anxiety and hopelessness levels of healthcare workers and non-healthcare workers.
+Multiple Analysis of Covariance (MANCOVA), SD: Standard deviation; n: Number of participants; STAI-S: State–Trait Anxiety Inventory-State, STAI-T: State–Trait Anxiety Inventory-Trait.
aSignificantly higher than non-healthcare workers.
bSignificantly lower than males.
cSignificantly higher than males.
dSignificantly higher than singles.
eSignificantly higher than healthcare workers.
Table 2.
Comparison of age, working hours and hopelessness and anxiety levels of healthcare workers according to their occupations and weekly working hours.
+Multiple Analysis of Covariance (MANCOVA), SD: Standard deviation; n: Number of participants.
aSignificantly higher than physicians and other healthcare workers.
bSignificantly higher than physicians.
cSignificantly lower than those with weekly working hours stay same.
dSignificantly higher than those with weekly working hours decreased and stay same.
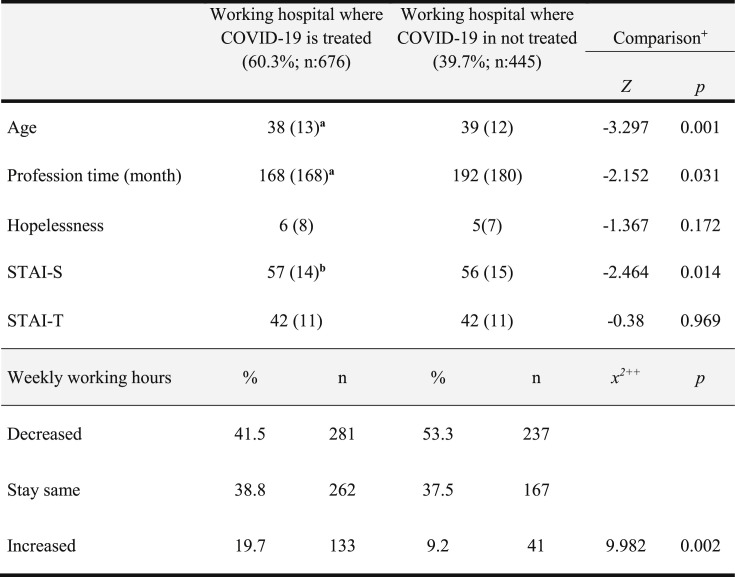
Considering the rates of those who increased the working hours, the rate of those working hospital where COVID-19 is treated (19.7%) was significantly higher than those in the hospital where COVID-19 is not treated (9.2%) (Table 3 ). The proportion of participants reported that they were working in the hospital where COVID-19 patients were being followed up was 60.3% (n:676). Healthcare workers working hospitals where COVID-19 is treated had lower ages and lower working years, and higher STAI-S levels (Table 3). There was no significant correlation between age, profession time, number of children, hopelessness and STAI-S in healthcare workers (p > 0.05). There is a very weak negative correlation between age and profession time with STAI-T in healthcare professionals (respectively: r = −0.104; p < 0.001, r = −0.096; p < 0.001).
Table 3.
The effect of working hospital where COVID-19 is treated on anxiety and hopelessness levels.
+ Mann-Whitney U Test.
++ Chi-square. IR: Interquartile range
aSignificantly lower.
bSignificantly higher.
The level of hopelessness, STAI-S and STAI-T in women was significantly higher than men (Table 1). STAI-S levels were significantly higher in married people than in singles (Table 1).
Thirty percent of the participants (n:646) reported that their income decreased after the pandemic started. Thirty-point nine percentage of participants (n:666) stated that they had difficulty in caring for their children and 91.0% (n: 1963) increased their hand washing behavior. In 89.5% (n: 929), general anxiety level was found to increase. A total of 66.6% (n:896) of the 1345 participants who have children reported anxiety about their child's education.
Comparison of hopelessness, STAI-S and STAI-T levels according to the place of residence, having difficulty in child care, having a high-risk individual at home, change in income level, hand washing behavior and change in anxiety level are shown in Table 3. Hopelessness, STAI-S and STAI-T levels were found to be significantly higher in those living outside metropolitan (city or county) than in metropolitan ones. Hopelessness, STAI-S and STAI-T levels are significantly higher in those who have difficulties in childcare than those who do not have difficulties. They are also higher in those who lives with high-risk individual for COVID-19 such as elderly than those who do not. Hopelessness and STAI-S levels were found to be significantly higher in those whose income level decreased, compared to those whose income level did not change. STAI-S levels are significantly higher in those with increased hand washing behavior compared to those whose hand washing behavior did not change. Hopelessness, STAI-S and STAI-T levels were found to be significantly higher in those who stated that their anxiety increased (Table 4 ).
Table 4.
Comparison of hopelessness, STAI-S and STAI-T levels according to the place of residence, having difficulty in childcare, having a high-risk individual at home, change in income, hand washing behavior and change in anxiety level.
| Hopelessness |
STAI-S |
STAI-T |
|
|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | |
| Place of residence | |||
| Metropolitan (n:1431) | 6.54 ± 5.15 | 52.57 ± 10.61 | 42.61 ± 7.32 |
| City or county (n:725) | 7.12 ± 5.36a | 53.84 ± 10.57a | 44.18 ± 8.11a |
| Comparison+ | t = −2.407; p = 0.018 | t = −2.620; p = 0.009 | t = −4.319; p < 0.001 |
| Difficulty in Child care | |||
| Yes (n:666) | 7.44 ± 5.41b | 57.27 ± 9.88b | 43.19 ± 7.79b |
| No (n:701) | 5.99 ± 4.97 | 50.69 ± 9.81 | 42.16 ± 7.07 |
| Comparison+ | t = −5.135; p < 0.001 | t = −12.363; p < 0.001 | t = −2.546; p = 0.011 |
| High-risk individual at home | |||
| Yes (n:803) | 7.27 ± 5.35c | 54.59 ± 10.12c | 43.72 ± 8.31c |
| No (n:1353) | 6.42 ± 5.13 | 52.05 ± 10.79 | 42.79 ± 7.72 |
| Comparison+ |
t = −3.684; p < 0.001 |
t = −5.495; p < 0.001 |
t = −4.319; p = 0.01 |
| Median (IR) | Median (IR) | Median (IR) | |
|
Income |
|||
| Decrease (n:646) | 6 (8)d | 54 (14)d | 43 (11) |
| Stay same (n:1473 | 5 (8) | 53 (14) | 43 (10) |
| Comparison++ | z = −2.056; p = 0.040 | z = −2.361; p = 0.018 | z = −0.901; p = 0.368 |
| Hand washing | |||
| Increase (n:1963) | 5 (8) | 54 (14)e | 43 (10) |
| Stay same (n:188) | 4 (8) | 48 (14) | 42 (12) |
| Comparison++ | z = −1.140; p = 0.254 | z = −6.915; p < 0.001 | z = −0.546; p = 0.585 |
| Anxiety | |||
| Increase (n:1929) | 6 (8)f | 55 (13)f | 43 (10)f |
| Stay same (n:222) | 3 (6) | 41 (12) | 40 (12) |
| Comparison++ | z = −6.159; p < 0.001 | z = −16.624; p < 0.001 | z = −5.516; p < 0.001 |
+Independent -Samples T Test, ++Mann-Whitney U Test, STAI-S: State–Trait Anxiety Inventory-State, STAI-T: State–Trait Anxiety Inventory-Trait, SD: Standart Deviation, IR: Interquartile Range.
Significantly higher than in people who lives in metropolitan.
Significantly higher than those who have no difficulties in childcare.
Significantly higher than those have no high-risk individual at home.
Significantly higher than in people whom income stay same.
Significantly higher than those with stay same hand washing behavior.
Significantly higher than people with stay same anxiety levels.
In the logistic regression analysis, anxiety increased the hand washing behavior 5.18 times, and being married increased 1.58 times (Table 5 , Model 1). Having a female gender increased the anxiety 1.81 times, being a high-risk individual at home increased the anxiety 1.58 times, and being a healthcare worker increased the anxiety 2.09 times (Table 5, Model 2).
Table 5.
Logistic regression analysis for hand washing behavior and anxiety.
| B |
Wald |
Exp (B) |
95% CI for Exp(B) |
p |
||
|---|---|---|---|---|---|---|
| Model 1a | Lower | Upper | ||||
| Being anxious | 1.645 | 88.672 | 5.179 | 3.678 | 7.294 | <0.001 |
| Being married | 0.457 | 8.506 | 1.58 | 1.162 | 2.148 | 0.004 |
| Model 2b | ||||||
| Female gender | 0.595 | 16.644 | 1.813 | 1.362 | 2.414 | <0.001 |
| High-risk individual at home | 0.462 | 8.652 | 1.587 | 1.167 | 2.160 | 0.003 |
| Being healthcare worker | 0.738 | 24.863 | 2.092 | 1.565 | 2.795 | <0.001 |
Model 1: The effect of increased anxiety and marital status on hand washing behavior.
Model 2: Impact of gender, having a high-risk individual at home, and being a healthcare worker on anxiety.
There is a positive and moderate relationship between hopelessness levels and STAI-S and STAI-T levels. (r = 0.423; n:2156; p < 0.001, r = 0.457; n:2156; p < 0.001, respectively). In multiple linear regression analysis, the increase in STAI levels explained 28.9% of the increase in hopelessness levels (beta: 0.354; df: 2,2153; Adjusted R2:28.9; F:439.642. p < 0.001) (Table 6 ).
Table 6.
The effect of STAI-S and STAI-T levels on BHS levels: Multiple regression analysis.
| Ba | Std. Error | βb | t | p | |
|---|---|---|---|---|---|
| STAI-S | 0.149 | 0.010 | 0.303 | 15.682 | <0.001 |
| STAI-T | 0.233 | 0.013 | 0.354 | 18.357 | <0.001 |
| F(2,2153) = 339.642; p=<0.001; Adjusted R2: 0.289 | |||||
Ba: non-standardized regression coefficient, βb: standardized regression coefficient.
The proportion of those with increased hand washing behavior in participants with increased anxiety (91.6%) was statistically significantly higher than in those reported that their anxiety levels stay same (67.4%). [x 2 (df = 1, n = 2156) = 107.476; p < 0.001; Phi(φ) = 0.226]. The proportion of those with increased handwashing behavior (93.4%) and anxiety (93%) in healthcare workers was significantly higher than those non-healthcare workers (88.5%; 85.7%, respectively). [x 2 (df = 1, n = 2156) = 15.234; p < 0.001; φ = 0.086; x 2(df = 1, n = 2156) = 29.231; p < 0.001; φ = 0.118, respectively]. The rate of increased anxiety (92.2%) in those live with high-risk individuals at home was significantly higher than those who do not (87.9%). [x 2(df = 1, n = 2156) = 9.331; p = 0.002; φ = 0.067]. However, the presence of a high-risk individual at home did not cause a significant increase in hand washing behavior (92.0%, 90.5%, respectively). [x 2(df = 1, n = 2156) = 1.327; p = 0.249; φ = 0.026].
The proportion of those who had increased hand washing behavior among healthcare workers did not differ significantly according to their positions. [x 2(df = 2, n = 1121) = 0.566; p = 0.754; Cramer's V (V) = 0.022]. The proportion of nurses with increased anxiety (95.1%) was significantly higher than doctors (90.9%) in healthcare workers [x 2(df = 1, n = 901) = 5.514; p = 0.019; φ = 0.083].
The proportion of women with increased anxiety (91.5%) was significantly higher than that of men (84.4%) [x 2(df = 1, n = 2516) = 22.421; p < 0.001; φ = −0.104]. The proportion of those who reported increased anxiety was significantly higher in married people (90.6%) than single ones (87.3%) [x 2(df = 1, n = 2516) = 5.153; p < 0.001; φ = 0.05].
The proportion of those with increased anxiety in participants with increased income (73%) was significantly lower than in those whose income did not change (89.3%) or in those with decreased income (90.7%) [x 2(df = 2, n = 2156) = 11.773; p = 0.003; V = 0.074].
When post hoc power analysis is performed for comparation of hopelessness level in healthcare workers and non-healthcare workers with alpha 0.05, effect size was 0.632, and the power of the study was found to be 0.999. For STAI-S level effect size was 0.164, and the power of the study was found to be 0.973.
4. Discussion
The main findings of this cross-sectional study are:
-
a)
The hopelessness and state anxiety levels of healthcare workers are high compared to the community sample.
-
b)
When health workers are evaluated among themselves, nurses' hopelessness and state anxiety levels are higher than doctors. Working in the hospital where COVID-19 is treated causes and increases the state anxiety levels. The increase in the weekly working hours of healthcare workers increases their anxiety and hopelessness levels.
-
c)
Hopelessness and state anxiety levels were increased in those whose income decreased in the whole sample.
-
d)
Those who had difficulty in caring for their children had higher levels of hopelessness, state and trait anxiety. The levels of hopelessness, state and trait anxiety of those living with a high-risk individuals for COVID-19 at home were significantly higher than those who did not live with a high-risk individuals.
-
e)
There was a positive and moderate relationship between hopelessness and STAI-S and STAI-T levels. In multiple linear regression analysis, the increase in STAI explained 28.9% of the increase in hopelessness.
Although trait anxiety levels in healthcare workers were significantly lower than other individuals of the society, higher state anxiety levels may be related to the active role they have taken during their pandemic period. In addition, news associated with healthcare workers going through a very difficult period under heavy working conditions in different countries may have further increased state anxiety. In the pandemic, healthcare workers have a higher risk of developing disease and contaminating to their family members than those non-healthcare workers. It is known that in quarantine situations, healthcare workers feel more emotions such as anger, fear, frustration, guilt, helplessness, anxiety, experience more trauma symptoms in the long term and are frequently exposed to stigmatization by the community (Reynolds et al., 2008).
This may explain the trait anxiety levels being higher in healthcare workers. In a study conducted in Italy, it was reported that the risk perception and anxiety levels of healthcare workers were higher in the COVID-19 pandemic compared to the society (Simione and Gnagnarella, 2020). Stressful life events, traumas, depressive symptoms and anxiety can affect hopelessness in individuals (Mathew et al., 2011; Minkoff et al., 1973; Rholes et al., 1985). State anxiety levels are closely related to stressful events. Such events that continue and include uncertainty, such as a pandemic, may also increase state anxiety and hopelessness. In this study, there is a positive correlation between hopelessness levels and anxiety. Anxiety levels were found to be a significant predictor of determining the level of hopelessness. 29% of the increase in hopelessness levels could be explained by the increase in anxiety levels. In a pilot study, it was reported that there was an important relationship between state anxiety and hopelessness. In this study hope was suggested as an important and integral construct as related to anxiety (Carretta et al., 2014). Similarly, it is known that there is a linear relationship between anxiety and hopelessness (Marai, 2004; Solmaz et al., 2000).
When the healthcare workers are examined, the hopelessness levels of the nurses were found higher than the doctors. In addition, the state anxiety levels of nurses were higher than both doctors and other healthcare workers. This may be due to the negative change in the working conditions of nurses during the pandemic period compared to other healthcare workers. In inpatient services, the fact that nurses have more physical contact with patients than doctors may be an important factor. In a study with nurses and doctors conducted by Li et al. it has been reported that negative life events correlate with symptoms of depression and anxiety, doctors experience more work-related negative events than nurses, but nurses show higher levels of anxiety and depression than doctors (Li et al., 2016). This difference was explained by the gender distribution of nurses and doctors, and it was stated that female gender was higher in the nurse group and women showed higher anxiety symptoms compared to previous studies (Altemus et al., 2014). In our study, 92% of the nurses and 68.4% of the doctors were women. In a study in which health records were examined, it was reported that mental health disorders were higher in women healthcare workers than men (Kim et al., 2018).
In a review published recently, evaluating the studies conducted during the COVID pandemic period, nurses reported that they experienced more mental symptoms than doctors (Spoorthy, 2020). In our study, the profession time of nurses was higher than doctors and other healthcare workers. This may have affected anxiety and hopelessness levels.
In our study, hopelessness and state anxiety levels were higher in healthcare workers with an increase in weekly working hours. For those working in medicine; wrong clinical decision making and fear of having a forensic problem (Gerrity et al., 1990), exposure to violence (Shabazz et al., 2016), sleep disturbance or sleep deprivation, long working hours, response to work-related calls outside working hours, lack of staff, difficulties in dealing with severe cases have been reported (Keller et al., 2013; Shirom et al., 2010; Wen et al., 2016). All these worker challenges pose a risk for burnout, anxiety, depression, stress, sleep problems and other mental illnesses (Gerrity et al., 1990; Medisauskaite and Kamau, 2019). While an increase in working hours causes anxiety, unhappiness and burnout in individuals, it is anticipated that the change and uncertainty in working hours in a risky situation such as pandemic will be associated with anxiety and state anxiety. In addition, the date of the present study is the first month of the pandemic in Turkey. The fact that the working order has not yet been determined may have increased anxiety in relation to the uncertainty in individuals. Indeed, uncertainty is known to increase anxiety (Hirsh et al., 2012). In addition, the fact that working in the hospital where COVID-19 is treated also increases the state anxiety levels, can be explained by the perception that people are at high risk of disease, thinking that they will be confronted with difficult cases and increase in working hours. In our study, the proportion of those working in the hospital where COVID-19 is treated with an increase in working hours was significantly higher than those in the hospital who did not take care of the COVID-19 patient.
Previously, pandemics have been reported to have serious social (Nickell et al., 2004) and economic negative consequences (Putri et al., 2018; Rothman, 2017) as well as physical illness. It has been reported that previous pandemics have serious social and economic adverse consequences besides physical illness. Similar to the SARS epidemic period experienced in the COVID-19 outbreak, many healthcare providers have not been trained in the spiritual field. In these settings, assessment and intervention should be applied for psychosocial concerns. It has been reported that it would be ideal practice to integrate psychological support into COVID-19 care, to address organizational level through state and local planning (Pfefferbaum and North, 2020). Curfews and quarantine measures have been implemented almost worldwide. It is inevitable that the economy will be significantly affected by this situation. In our study, loss of income seems to increase the state anxiety and hopelessness of people. The uncertainty in the pandemic process and the inability to anticipate the expiration date further affect this situation.
During the pandemic, schools were vacated, and children had to stay at home. This situation has caused many problems for working parents, such as caring for their children, and their education. Parents who could not get permission because they had to work had difficulty finding someone to care for their children, some of the caregivers left their jobs, and the difficulties of working parents increased. In such stressful life events, an increase in anxiety levels of individuals is an expected result (McLaughlin and Hatzenbuehler, 2009). Negative life events have been reported to cause anxiety and decrease in self-esteem (Joiner et al., 1999).
Deaths in the COVID-19 pandemic occurred mostly in elderly individuals and those with chronic disease (Feng et al., 2020). Therefore, an increase in anxiety and hopelessness levels is expected in individuals who live with high-risk groups at home and who are forced to work. Our study results are compatible with this.
In the study, there is a positive relationship between hopelessness levels and anxiety. There can be many reasons for despair. Uncertainty is one of the most important factors that trigger anxiety. Anxiety and uncertainty can cause an increase in people's hopelessness.
The most important limitation of this study is that it makes a cross-sectional assessment and self-report scales are used. Another limitation would be that surveys were conducted online instead of face-to-face interviews. However, as long-term close contact with participants will increase the risk of disease spread during the pandemic period, online questionnaire was inevitable in this period. Since the increase of the number of questions in online surveys will decrease the number of participations, the number of questions is limited. For this reason, data could not be collected such as whether the participants were diagnosed with COVID-19 or whether there was a relative who was under treatment. The strengths of the study are the high number of participants that could not be reached in one hundred percent of the interviews, the careful choice of the sample selection, and the exclusion of the participants with any missing data.
As a result, state anxiety and hopelessness levels of healthcare workers are higher than the society. It is seen that anxiety and hopelessness levels of nurses have increased more among healthcare workers. The increase in working hours is one of the important factors affecting anxiety. Anxiety is an important predictor of hopelessness.
In line with these results, determining the factors affecting anxiety and hopelessness during the pandemic period can contribute to the protection of public health by ensuring that the psychosocial interventions for risky groups are planned in advance. In further studies, it is recommended to conduct longitudinal studies on how these psychological effects progress and the effects of the individuals on work and family life are monitored.
Credit author statements
Yunus Hacimusalar: Conceptualization, Data curation, Methodology, Software, Formal analysis, Investigation, Writing - Original Draft, Writing - Review & Editing.
Aybeniz Civan Kahve: Conceptualization, Methodology, Data curation, Investigation, Writing - Original Draft, Writing - Review & Editing.
Alisan Burak Yasar: Data curation, Methodology, Investigation, Writing - Original Draft, Writing - Review & Editing.
Mehmet Sinan Aydin: Data curation, Methodology, Investigation, Writing - Original Draft, Writing - Review & Editing.
Declaration of competing interest
No conflict of interest was declared by the authors.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jpsychires.2020.07.024.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Altemus Margaret, Sarvaiya Nilofar, Epperson C Neill. Sex differences in anxiety and depression clinical perspectives. Front. Endocrinol. 2014;35(3):320–330. doi: 10.1016/j.yfrne.2014.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck A.T., Weissman A., Lester D., Trexler L. The measurement of pessimism: the Hopelessness Scale. J. Consult. Clin. Psychol. 1974;42:861–865. doi: 10.1037/h0037562. [DOI] [PubMed] [Google Scholar]
- Brooks Samantha K., Webster Rebecca K., Smith Louise E., Woodland Lisa, Wessely Simon, Greenberg Neil, Rubin Gideon James. Rapid review. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carretta Carrie M., Ridner Sheila H., Dietrich Mary S. Hope, hopelessness, and anxiety: a pilot instrument comparison study. Arch. Psychiatr. Nurs. 2014;28(4):230–234. doi: 10.1016/j.apnu.2014.05.005. [DOI] [PubMed] [Google Scholar]
- Durak Ayşegül, Palabıyıkoğlu Refia. Beck umutsuzluk ölçeği geçerlilik çalışması. Kriz Dergisi. 1994;2(2):311–319. [Google Scholar]
- Feng Zijian, Li Qun, Zhang Yanping, Wu Zunyou, Dong Xiaoping, Ma Huilai, Yin Dapeng, Chinese Center for Disease Control and Prevention . 2020. The Epidemiological Characteristics of an Outbreak of 2019 Novel Coronavirus Diseases (COVID-19)—China. [Google Scholar]
- Fiorillo Andrea, Gorwood Philip. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur. Psychiatr. 2020;63(1) doi: 10.1192/j.eurpsy.2020.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerrity Martha S., DeVellis Robert F., Earp Jo Anne. Physicians' reactions to uncertainty in patient care: a new measure and new insights. Med. Care. 1990:724–736. doi: 10.1097/00005650-199008000-00005. [DOI] [PubMed] [Google Scholar]
- Hirsh Jacob B., Mar Raymond A., Peterson Jordan B. Psychological entropy: a framework for understanding uncertainty-related anxiety. Psychol. Rev. 2012;119(2):304. doi: 10.1037/a0026767. [DOI] [PubMed] [Google Scholar]
- Huang J.Z., Han M.F., Luo T.D., Ren A.K., Zhou X.P. Mental health survey of 230 medical staff in a tertiary infectious disease hospital for COVID-19. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi. 2020;38 doi: 10.3760/cma.j.cn121094-20200219-00063. E001-E001. [DOI] [PubMed] [Google Scholar]
- Joiner Thomas E., Jr., Katz Jennifer, Lew Angela. Harbingers of depressotypic reassurance seeking: negative life events, increased anxiety, and decreased self-esteem. Pers. Soc. Psychol. Bull. 1999;25(5):632–639. [Google Scholar]
- Keller Monika, Bamberg Eva, Kersten Maren, Nienhaus Albert. Instrument for stress-related job analysis for hospital physicians: validation of a short version. J. Occup. Med. Toxicol. 2013;8(1):10. doi: 10.1186/1745-6673-8-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim Min-Seok, Taeshik Kim, Lee Dongwook, Yook Ji-hoo, Hong Yun-Chul, Lee Seung-Yup. Mental disorders among workers in the healthcare industry: 2014 national health insurance data. Ann. Occup. Environ. Med. 2018;30(1):31. doi: 10.1186/s40557-018-0244-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Yamin, Zhang Hongliang, Feng Zhijuan, Chen Shubao, Liu Tieqiao, Chen Xiaogang. Life events, anxiety and depression among doctors and nurses in the emergency department: a study from eleven general hospital in Hunan Province, China. J. Psychiatr. Brain Sci. 2016;1(1) [Google Scholar]
- Lai Jianbo, Ma Simeng, Wang Ying, Cai Zhongxiang, Hu Jianbo, Wei Ning. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw. Open. 2020;3(3) doi: 10.1001/jamanetworkopen.2020.3976. e203976-e203976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marai Leo. Anxiety and hopelessness in two South Pacific countries: exploratory studies. Soc. Behav. Pers. 2004;32(8):723–730. [Google Scholar]
- Mathew A.R., Pettit J.W., Lewinsohn P.M., Seeley J.R., Roberts R.E. Co-morbidity between major depressive disorder and anxiety disorders: shared etiology or direct causation? Psychol. Med. 2011;41(10):2023. doi: 10.1017/S0033291711000407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin Katie A., Hatzenbuehler Mark L. Stressful life events, anxiety sensitivity, and internalizing symptoms in adolescents. J. Abnorm. Psychol. 2009;118(3):659. doi: 10.1037/a0016499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medisauskaite Asta, Kamau Caroline. Reducing burnout and anxiety among doctors: randomized controlled trial. Psychiatr. Res. 2019;274:383–390. doi: 10.1016/j.psychres.2019.02.075. [DOI] [PubMed] [Google Scholar]
- Minkoff Kenneth, Bergman Eric, Beck Aaron T., Beck Roy. Hopelessness, depression, and attempted suicide. Am. J. Psychiatr. 1973;130(4):455–459. doi: 10.1176/ajp.130.4.455. [DOI] [PubMed] [Google Scholar]
- Nickell Leslie A., Crighton Eric J., Tracy C Shawn, Hadi Al-Enazy, Yemisi Bolaji, Sagina Hanjrah. Psychosocial effects of SARS on hospital staff: survey of a large tertiary care institution. CMAJ (Can. Med. Assoc. J.) 2004;170(5):793–798. doi: 10.1503/cmaj.1031077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Öner Necla, Le Compte Ayhan. Basım, Boğaziçi Üniversitesi Yayınevi; İstanbul: 1998. Süreksiz Durumluk/sürekli Kaygı Envanteri El Kitabı, 2. [Google Scholar]
- Pfefferbaum Betty, North Carol S. Mental health and the Covid-19 pandemic. N. Engl. J. Med. 2020:1–3. doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- Porta Miquel. Oxford university press; 2014. A Dictionary of Epidemiology. [Google Scholar]
- Putri Wayan CWS., Muscatello David J., Stockwell Melissa S., Newall Anthony T. Economic burden of seasonal influenza in the United States. Vaccine. 2018;36(27):3960–3966. doi: 10.1016/j.vaccine.2018.05.057. [DOI] [PubMed] [Google Scholar]
- Republic of Turkey Ministry of Health Corona Table 2020. https://covid19.saglik.gov.tr/ Retrieved from. Accessed May 13, 2020.
- Reynolds Diane L., Garay J.R., Deamond S.L., Moran Maura K., Gold W., Styra R. Understanding, compliance and psychological impact of the SARS quarantine experience. Epidemiol. Infect. 2008;136(7):997–1007. doi: 10.1017/S0950268807009156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rholes William S., Riskind John H., Neville Brian. The relationship of cognitions and hopelessness to depression and anxiety. Soc. Cognit. 1985;3(1):36–50. [Google Scholar]
- Rothman T. The cost of influenza disease burden in US Population. Int. J. Econ. Manag. Sci. 2017;6:443. [Google Scholar]
- Seber Güiten, Dilbaz Nesrin, Kaptanoğlu Cem, Tekin Durmuş. Umutsuzluk ölçeği geçerlilik ve güvenirliği. Kriz Dergisi. 1993;1(3):139–142. [Google Scholar]
- Shabazz Tariq, Parry-Smith William, Oates Sharon, Henderson Steven, Mountfield Joanna. Consultants as victims of bullying and undermining: a survey of Royal College of Obstetricians and Gynaecologists consultant experiences. BMJ. 2016;6(6) doi: 10.1136/bmjopen-2016-011462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah Kaushal, Kamrai Dhwani, Mekala Hema, Mann Birinder, Desai Krishna, Patel Rikinkumar S. Focus on mental health during the coronavirus (COVID-19) pandemic: applying learnings from the past outbreaks. Cureus. 2020;12(3) doi: 10.7759/cureus.7405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shea Frank, Hurley Elizabeth. Hopelessness and helplessness. Psychiatr. Care. 1964;2(1):32–38. [Google Scholar]
- Shigemura Jun, Ursano Robert J., Morganstein Joshua C., Kurosawa Mie, Benedek David M. Public responses to the novel 2019 coronavirus (2019‐nCoV) in Japan: mental health consequences and target populations. Psychiatr. Clin. Neurosci. 2020;74(4):281. doi: 10.1111/pcn.12988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shirom Arie, Nirel Nurit, Vinokur Amiram D. Work hours and caseload as predictors of physician burnout: the mediating effects by perceived workload and by autonomy. Appl. Psychol. 2010;59(4):539–565. [Google Scholar]
- Simione Luca, Gnagnarella Camilla. Psyarxiv Preprints. 2020. Differences between health workers and general population in risk perception, behaviors, and psychological distress related to COVID-19 spread in Italy. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solmaz M., Sayar K., Ozer O.A., Ozturk M., Acar B. Alexithymia, hopelessness and depression in social phobic patients: a study with a control group. Klin Psikiyatr Derg. 2000;3:235–241. [Google Scholar]
- Spielberger C.D., Gorsuch R.L., Lushene R., Vagg P.R., Jacobs L. vol. 22. Calif Consulting Psychologists Press; 1970. pp. 1–24. (Manual for the State-Trait. Anxiety Inventory Palo Alto). [Google Scholar]
- Spoorthy M.S. Mental health problems faced by healthcare workers due to the COVID-19 pandemic-A review. Asian J. Psychiatr. 2020;51:102119. doi: 10.1016/j.ajp.2020.102119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tam Cindy WC., Pang Edwin PF., Lam Linda CW., Chiu Helen FK. Severe acute respiratory syndrome (SARS) in Hong Kong in 2003: stress and psychological impact among frontline healthcare workers. Psychol. Med. 2004;34(7):1197. doi: 10.1017/s0033291704002247. [DOI] [PubMed] [Google Scholar]
- Taylor S. Newcastle upon Tyne, NE6 2PA, UK. Cambridge Scholars Publishing; 2019. The psychology of pandemics. [Google Scholar]
- Wen J., Cheng Y., Hu X., Yuan P., Hao T., Shi Y. Workload, burnout, and medical mistakes among physicians in China: a cross-sectional study. Biosci. Trends. 2016;10:27–33. doi: 10.5582/bst.2015.01175. [DOI] [PubMed] [Google Scholar]
- WHO Coronavirus disease (COVID-19) situation report-113. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200512-covid-19-sitrep-113.pdf?sfvrsn=feac3b6d_2 Retrieved from. Accessed May 13, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.