Abstract
Partial-thickness articular-sided rotator cuff tears are a common cause of shoulder pain in adults. Although partial rotator cuff tears have a high prevalence, there is still controversy over their proper surgical treatment. Different surgical procedures have been suggested when partial tears involve the articular side of the rotator cuff, such as arthroscopic debridement of the tear with or without acromioplasty, tear completion and repair, and transtendinous in situ repair. Although multiple repair techniques have been described, significant clinical data to definitively support one technique over the others are currently lacking. We describe an arthroscopic technique for repair of a partial articular supraspinatus tendon avulsion that avoids the transtendinous insertion of suture anchors to preserve the tendon integrity.
Partial-thickness rotator cuff tears are common, with an incidence from 17% to 37%.1 In patients younger than 40 years, the prevalence is 4%; however, in patients older than 60 years, the prevalence increases to 26%.2 Ultrasound studies of asymptomatic volunteers have further shown this age-related difference, with a 5% to 11% incidence of full- or partial-thickness tears in subjects aged 40 to 60 years, increasing to 80% in patients 70 years or older.3 Full or partial rotator cuff tears are also common in overhead athletes, with a prevalence of up to 40% in the dominant throwing shoulder.4
Partial-thickness rotator cuff tears can involve the articular surface, bursal surface, or both surfaces. However, articular surface lesions occur approximately 2 to 3 times more often than bursal tears.5 PASTA (partial articular supraspinatus tendon avulsion) lesions can be caused by multiple different mechanisms including acute trauma, repetitive microtrauma, age-related degeneration, and instability of the shoulder with internal impingement.6,7
Conservative treatment with physical therapy, rest, and nonsteroidal anti-inflammatories should be considered a first option. If conservative treatment fails, different surgical treatment methods are available, such as arthroscopic debridement of the tear with or without acromioplasty, tear completion and repair, and transtendinous repair.
Tear completion and transtendinous repair both have potential drawbacks. Tear completion with repair has the benefit of stimulating healing, but the remaining intact tendon may be damaged by detaching it from the greater tuberosity. A negative aspect of the transtendon approach is that suture anchors usually have to be inserted directly through the tendon. In addition, the remaining tendon may be degenerative. Currently, there is no clinical evidence suggesting one method is superior to the other methods,8, 9, 10 which has led to a debate over the proper treatment of PASTA lesions. We describe a modified arthroscopic technique that minimizes violation of the tendon by using a curved drill guide to insert 2 suture anchors without passing them through the intact tendon.
Surgical Technique
Preoperative Setup
The patient can be positioned in the operating room for shoulder arthroscopy per the surgeon's preference. The photographs and diagrams that follow were obtained with the patient in the beach-chair position.
Portal Placement and Arthroscopic Assessment
A standard posterior portal is created to enter the shoulder and examine the glenohumeral joint. An anterior portal is then established and used to place a cannula in the rotator interval. The tear is visualized (Fig 1) and debrided. Once the tendon is debrided to a healthy edge, the tear is measured. The footprint can be decorticated in preparation for repair.
Fig 1.

View of the left shoulder from the posterior portal with the patient in the beach-chair position. The biceps has been tenotomized. Once the status of the supraspinatus has been assessed and the tendon has been debrided, we proceed with the repair. (L, lateral; M, medial.)
Technical Procedure
We have found that leaving a switching stick in the joint can help with re-entry and subacromial bursoscopy can be performed from a separate posterolateral portal. The rotator cuff tendon is inspected from the bursal side. In cases with coracoacromial ligament fraying or impingement of the bursal surface, the surgeon can proceed with subacromial decompression and acromioplasty. We then direct a Arthrex curved drill guide (Naples, FL) through the rotator interval (Fig 2) and place FiberTak soft suture anchors (Arthrex) at the posterior and anterior margins of the tear. The posterior anchor necessitates positioning the arm in extension for a more favorable angle. With the anchors in place, a spinal needle is passed percutaneously through the supraspinatus at the desired repair sites, and the sutures are shuttled through the tendon using a monofilament suture (Fig 3). The central 2 sutures are retrieved through the lateral portal and tied outside the cannula. The most anterior and most posterior free suture limbs are tensioned to deliver the knot against the tendon, completing our partial articular supraspinatus repair (Fig 4).
Fig 2.
(A) View of the left shoulder from the posterior portal with the patient in the beach-chair position. The curved drill guide is placed through the rotator interval and used to place the anterior and posterior anchors. (B) View from outside the portal with the curved drill in place. (L, lateral; M, medial.)
Fig 3.
(A) View of the left shoulder from the posterior portal with the patient in the beach-chair position. A spinal needle is used to place shuttling sutures through the desired repair site. (B) View of sutures after shuttling has occurred. (A, anterior; L, lateral; M, medial.)
Fig 4.

View of the left shoulder from the posterior lateral portal with the patient in the beach-chair position. The tied sutures have been delivered down to the bursal side of the supraspinatus. (Ca, caudal; Ce, cephalic; L, lateral; M, medial.)
The 4 suture limbs can then be loaded into a lateral-row SwiveLock anchor (Arthrex), and the suture anchors are tensioned appropriately (Fig 5); all 4 limbs or just the anterior and posterior limbs can be loaded. Once compression of the tendon has been verified, the remainder of the procedure is completed per the surgeon's preference (Fig 6). Sling immobilization is used for approximately 4 weeks. Table 1 summarizes the pearls and pitfalls of the procedure.
Fig 5.
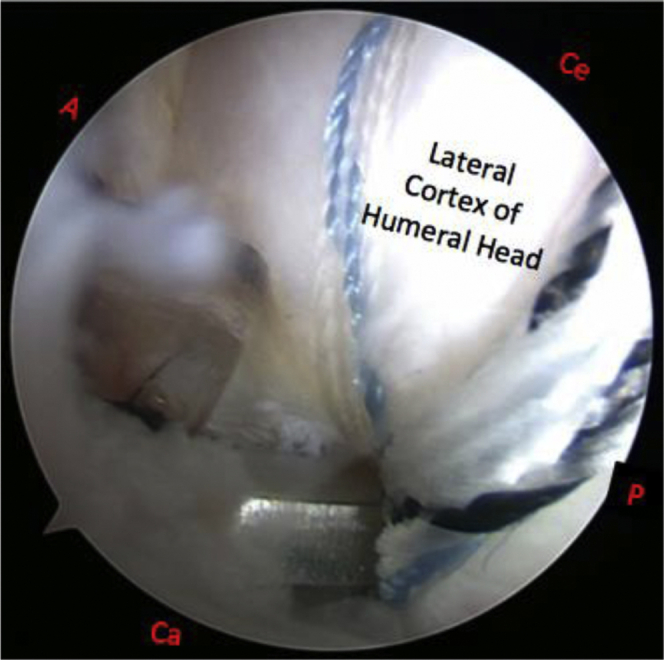
View of the left shoulder from the posterior lateral portal with the patient in the beach-chair position. The sutures are loaded into a lateral-row anchor and impacted into the lateral cortex of the humeral head. The sutures are then tensioned appropriately. (Ca, caudal; Ce, cephalic; L, lateral; M, medial.)
Fig 6.

View of the left shoulder from the posterior portal with the patient in the beach-chair position. The repair has been completed, and the glenohumeral joint is re-entered to verify the reduction of the supraspinatus down to bone. (L, lateral; M, medial.)
Table 1.
Pearls and Pitfalls
| Pearls |
| During positioning of the anchors, the arms should be in extension to achieve the proper angle for placement. |
| When placing the anchors, the surgeon should ensure they are seated and slide appropriately prior to tying. |
| If the appropriate angle cannot be achieved, the procedure should be converted into a transtendinous insertion. |
| Pitfalls |
| The surgeon should avoid overly oblique angles with posterior portal drilling. |
| To minimize the risk of suture laceration, care should be taken to clear out the subacromial bursa prior to suture passage. |
| In a patient with a prominent acromion, care should be taken to avoid overly oblique suture passage angles. |
Discussion
PASTA lesions can be a common cause of shoulder pain in adults, with a particularly high prevalence in athletes. Repetitive contact between the articular side of the rotator cuff and the posterior-superior glenoid, commonly seen in overhead athletes, produces posterosuperior glenoid internal impingement, causing repetitive microtrauma on the articular cuff side.6,7 The recommended initial management for the symptomatic shoulder is an extended conservative treatment period. If conservative care is unsuccessful, numerous surgical treatments have shown favorable results. Among these treatments are arthroscopic debridement of the tear with or without acromioplasty, tear completion and repair, and transtendinous in situ repair.
The traditional consensus has been to perform debridement in tears of less than 50% of the tendon thickness and to repair those of greater than 50% thickness.11 However, it is still debated whether partial tears should be converted into full tears followed by repair or should be treated using transtendinous repair. Sun et al.8 showed no significant differences using tear completion with repair versus traditional transtendinous repair regarding clinical outcomes with American Shoulder and Elbow Surgeons scores. However, they found a superior outcome for the retear rate using transtendon repair.
In a study by Deutsch,9 41 patients underwent arthroscopic completion of the lesion with repair and showed significant improvements in American Shoulder and Elbow Surgeons scores; 98% of patients were satisfied with their outcome. Although completion of the tear stimulates healing and shows favorable outcomes, it also sacrifices the intact bursal surface and may lead to length-tension mismatches.
The transtendon technique preserves the intact bursal layer, restores the anatomy of the footprint, and returns the avulsed tendon to its original insertion while avoiding excision of normal tendon tissue to enhance healing. In a study of 80 patients by Ranalletta et al.,12 92.5% reported good or excellent results and 7.5% reported fair results. One drawback of transtendon repair is the necessity to pass the anchor directly through the tendon, which can compromise a portion of the intact bursal layer and potentially lead to tear progression. Hirahara et al.13 published results showing that PASTA repair yielded biomechanically equivalent outcomes to the traditional transtendinous technique. However, they also noted that the PASTA repair technique is technically easier to perform, is more reproducible, and poses fewer risks.
Although transtendinous repair and tear completion with repair have shown excellent results in the nonthrowing population, arthroscopic debridement has been shown to have improved outcomes in throwing athletes.14 Arthroscopic debridement in throwing shoulders has the advantages of an accelerated rehabilitation period, shorter postoperative immobilization period, and reduced operation time. These factors reduce the risk of postoperative stiffness and allow throwing athletes to return to play earlier. The main disadvantage is that debridement may be only a temporary solution because it may not completely resolve progression in overhead athletes.6
The technique described in this report aims to circumvent transtendinous insertion of suture anchors by passing a curved drill guide through the rotator interval for anchor placement. This allows the anchors to be placed at the anterior and posterior portions of the tear without passing them directly through the intact bursal layer of the tendon. An 18-gauge spinal needle is used to shuttle sutures, which maintains the minimally invasive approach to lesion repair. Using small soft anchors and drilling with an oblique angle both increase the risk of anchor pullout, which may necessitate switching anchors during a case. Table 2 reviews the advantages and disadvantages of this technique. The goal is to improve on the traditional transtendinous method by maintaining all the advantages while minimizing trauma to intact structures.
Table 2.
Advantages and Disadvantages
| Advantages |
| Less violation of natural tendon insertion |
| Minimal bone loss for anchor placement |
| Disadvantages |
| Higher potential of anchor pullout with oblique-angle drilling or soft bone |
| More technically challenging than traditional PASTA repair methods |
PASTA, partial articular supraspinatus tendon avulsion.
In this Technical Note and Video 1, we describe our approach for transtendinous repair of PASTA lesions. Past studies have failed to show superiority of any one technique. However, by avoiding the insertion of anchors through the intact bursal layer, our technique may provide a less invasive approach for the treatment of PASTA lesions.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: N.G. receives personal fees from Wright Medical and DJO Surgical, outside the submitted work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Technique for repair of PASTA (partial articular supraspinatus tendon avulsion) lesions making use of rotator interval. This approach allows for placement of suture anchors without violating the rotator cuff.
References
- 1.Fukuda H., Mikasa M., Yamanaka K. Incomplete thickness rotator cuff tears diagnosed by subacromial bursography. Clin Orthop Relat Res. 1987;(223):51–58. [PubMed] [Google Scholar]
- 2.Sher J.S., Uribe J.W., Posada A., Murphy B.J., Zlatkin M.B. Abnormal findings on magnetic resonance images of asymptomatic shoulders. J Bone Joint Surg Am. 1995;77:10–15. doi: 10.2106/00004623-199501000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Milgrom C., Schaffler M., Gilbert S., Holsbeeck M.V. Rotator-cuff changes in asymptomatic adults. The effect of age, hand dominance and gender. J Bone Joint Surg Br. 1995;77-B:296–298. [PubMed] [Google Scholar]
- 4.Connor P.M., Banks D.M., Tyson A.B., Coumas J.S., Dalessandro D.F. Magnetic resonance imaging of the asymptomatic shoulder of overhead athletes. Am J Sports Med. 2003;31:724–727. doi: 10.1177/03635465030310051501. [DOI] [PubMed] [Google Scholar]
- 5.Wolff A.B., Sethi P., Sutton K.M., Covey A.S., Magit D.P., Medvecky M. Partial-thickness rotator cuff tears. J Am Acad Orthop Surg. 2006;14:715–725. doi: 10.5435/00124635-200612000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Caldwell P.E., Dyer D.C., Pearson S.E. Arthroscopic debridement of the throwers shoulder: Less is more. Arthrosc Tech. 2016;5:e1381–e1386. doi: 10.1016/j.eats.2016.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Osti L., Buda M., Andreotti M., Osti R., Massari L., Maffulli N. Transtendon repair in partial articular supraspinatus tendon tear. Br Med Bull. 2017;123:19–34. doi: 10.1093/bmb/ldx023. [DOI] [PubMed] [Google Scholar]
- 8.Sun L., Zhang Q., Ge H.A., Sun Y., Cheng B. Which is the best repair of articular-sided rotator cuff tears: A meta-analysis. J Orthop Surg Res. 2015;10:84. doi: 10.1186/s13018-015-0224-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Deutsch A. Arthroscopic repair of partial-thickness tears of the rotator cuff. J Shoulder Elbow Surg. 2007;16:193–201. doi: 10.1016/j.jse.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 10.Castricini R., Camera F.L., Gori M.D. Functional outcomes and repair integrity after arthroscopic repair of partial articular supraspinatus tendon avulsion. Arch Orthop Trauma Surg. 2018;139:369–375. doi: 10.1007/s00402-018-3044-4. [DOI] [PubMed] [Google Scholar]
- 11.Woods T.C., Carroll M.J., Nelson A.A. Transtendon rotator-cuff repair of partial-thickness articular surface tears can lead to medial rotator-cuff failure. Open Access J Sports Med. 2014;5:151–157. doi: 10.2147/OAJSM.S62885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ranalletta M., Rossi L.A., Bertona A.B. Arthroscopic transtendon repair of partial-thickness articular-side rotator cuff tears. Arthroscopy. 2016;32:1523–1528. doi: 10.1016/j.arthro.2016.01.027. [DOI] [PubMed] [Google Scholar]
- 13.Hirahara A.M., Andersen W.J. The PASTA bridge—a repair technique for partial articular-sided rotator cuff tears: A biomechanical evaluation of construct strength. Am J Orthop (Belle Mead NJ) 2018;47 doi: 10.12788/ajo.2018.0095. [DOI] [PubMed] [Google Scholar]
- 14.Reynolds S.B., Dugas J.R., Cain E.L., McMichael C.S., Andrews J.R. Débridement of small partial-thickness rotator cuff tears in elite overhead throwers. Clin Orthop Relat Res. 2008;466:614–621. doi: 10.1007/s11999-007-0107-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Technique for repair of PASTA (partial articular supraspinatus tendon avulsion) lesions making use of rotator interval. This approach allows for placement of suture anchors without violating the rotator cuff.




