Abstract
Valgus malalignment can be corrected with a medial closing-wedge proximal tibia osteotomy in patients with symptomatic lateral compartment disease. Advantages of this technique include the inherent stability of the closing wedge with direct bone contact and reliable healing that enables early weight bearing and shorter recovery time. In addition, a tibial-based osteotomy alters joint contact forces in both flexion and extension versus femoral-based osteotomies. The purpose of this article is to present a reproducible technique for medial closing-wedge proximal tibia osteotomy and review the indications, preoperative planning, rationale, and clinical outcomes.
Osteotomies about the knee have long been an established treatment for various pathologies in patients with coronal plane malalignment.1 More recently, advances in cartilage restoration and meniscal transplant procedures have led to increasing interest in biologic joint reconstruction. Neutral mechanical alignment is an important factor in the success of these operations, and there has been increased interest in osteotomies to achieve this goal.1, 2, 3
Several techniques have been described for correction of valgus malalignment, including distal femoral osteotomy (lateral opening wedge or medial closing wedge) and proximal tibial osteotomy (lateral opening wedge or medial closing wedge). Although distal femoral osteotomies have long been considered the standard for treatment of valgus with lateral compartment disease, these techniques preferentially affect joint contact forces in full extension with less effect at greater knee flexion angles and no effect at 90° or beyond.4, 5, 6 In patients with mild-to-moderate valgus alignment and lateral compartment arthritis, meniscal deficiency, or focal osteochondral defects, our preference is to perform a medial closing-wedge proximal tibia osteotomy (MCWPTO) to alter joint contact forces both in flexion and extension. Other advantages of this technique compared with femoral osteotomies are summarized in Table 1. The purpose of this article is to present a reproducible technique for MCWPTO and review the indications, preoperative planning, rationale, and clinical outcomes.
Table 1.
Advantages and Disadvantages of Osteotomies in the Treatment of Valgus Malalignment
| MCWPTO |
LOWPTO |
MCWDFO |
LOWDFO |
|---|---|---|---|
| Advantages | Advantages | Advantages | Advantages |
|
|
|
|
| Disadvantages | Disadvantages | Disadvantages | Disadvantages |
|---|---|---|---|
|
|
|
|
LOWDFO, lateral opening-wedge distal femur osteotomy; LOWPTO, lateral opening-wedge proximal tibia osteotomy; MCWDFO, medial closing-wedge distal femur osteotomy; MCWPTO, medial closing-wedge proximal tibia osteotomy.
Surgical Technique (With Video Illustration)
Detailed information regarding the MCWPTO surgical technique is shown in Video 1. The pearls and pitfalls of this technique are also summarized in Table 2.
Table 2.
Pearls and Pitfalls
| Pearls |
|
| Pitfalls |
|
|
Surgical Indications and Contraindications
Proper patient selection is paramount for the success of this operation. The primary indications for this procedure are mild-to-moderate valgus malalignment (up to 10°) with a previous injury to the lateral compartment cartilage or meniscus, or lateral compartment arthritis. Most often, patients have undergone previous surgical procedures for partial lateral meniscectomy, lateral meniscus repair, chondroplasty, or other cartilage procedures in the lateral compartment. The MCWPTO also may be used as an adjunct procedure in patients undergoing concomitant lateral meniscus allograft transplantation or lateral compartment cartilage repair procedures. Absolute contraindications for MCWPTO include symptomatic medial compartment disease, inflammatory arthritis, severe ligamentous laxity or joint subluxation greater than 1 cm, and nicotine use. Relative contraindications include obesity (body mass index greater than 35), age greater than 60 years, moderate-to-severe patellofemoral disease, excessive joint line obliquity, and an aberrant anterior tibial artery identified on magnetic resonance imaging.6, 7, 8, 9
Preoperative Planning
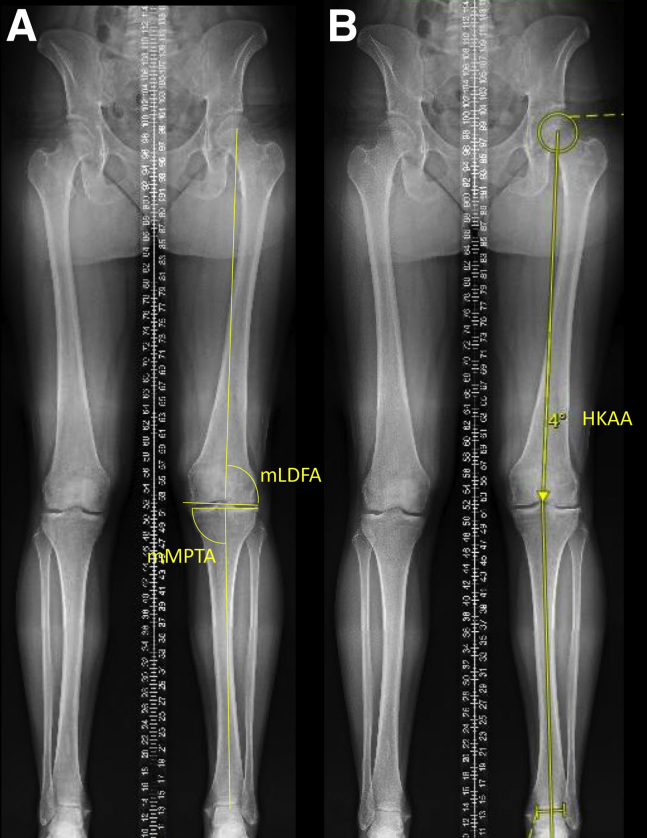
Limb alignment is assessed using full-length bilateral weight-bearing radiographs. The mechanical axis or hip–knee–ankle angle of the lower limb is used to measure the coronal plane deformity (Fig 1). In addition, the mechanical medial proximal tibia articular angle and mechanical lateral distal femur articular angle are calculated as the angle formed between the mechanical axis of the tibia and tibial plateau, and the mechanical axis of the femur and distal articular angle of the femur, respectively (Fig 1). Magnetic resonance imaging is obtained in all patients to assess for intra-articular pathology as well to assess for an aberrant anterior tibial artery.9
Fig 1.
Full length standing anteroposterior radiographs with measurements of the left lower extremity demonstrating (A) mLDFA and mMPTA, and (B) HKAA with planned 4° correction to the medial tibial spine. (HKAA, hip–knee–ankle angle; mLDFA, mechanical lateral distal femoral angle; mMPTA, mechanical medial proximal tibial angle.)
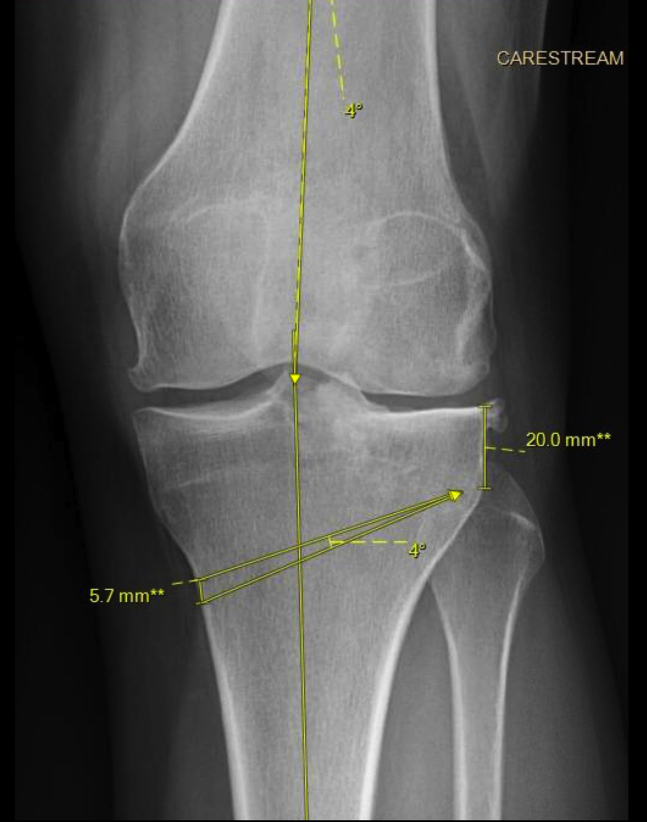
Surgical correction is calculated using the hip–knee–ankle angle (Fig 1). In general, the correction is planned to the center of the knee joint, although in cases of more severe lateral compartment disease, correction to the medial tibial spine may be preferred. The calculated angle of correction is then transposed to the tibia at the desired level of the osteotomy cut with the trajectory toward a point about 2 cm distal to the articular surface of the lateral tibial plateau and about 0.5 to 1 cm from the lateral cortex to preserve a lateral “hinge.” The length of the wedge of bone to be removed is measured along the medial tibial cortex (Fig 2).
Fig 2.
Anteroposterior knee radiograph with preoperative templating for medial closing-wedge proximal tibia osteotomy. The 4° correction is calculated using the hip–knee–ankle angle and transposed to the desired cut at the proximal tibia to a point 2 cm below the lateral joint surface. The wedge of bone to be removed is measured at the medial cortex; in this case 5.7 mm.
Patient Positioning
The patient is positioned supine on a radiolucent table that will allow fluoroscopy from the hip joint to the ankle. After induction of general anesthesia, a bilateral knee examination is performed to assess for any ligamentous instability and knee range of motion. A well-padded thigh tourniquet is placed. A lateral thigh post is used and placed high enough to allow a figure of four position. A foot post is placed at the mid-calf level or distal to ensure the osteotomy will not be flexed during fixation, and to allow for knee flexion if a concomitant intra-articular procedure will be performed (Fig 3).
Fig 3.
Patient is positioned supine with the left lower extremity exposed at the end of a regular operating room table with a lateral thigh post (arrowhead) and foot post (arrow).
Detailed Procedure
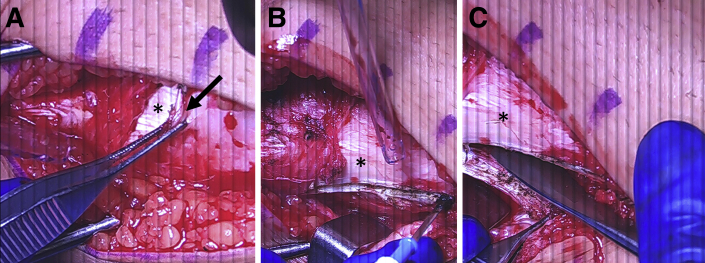
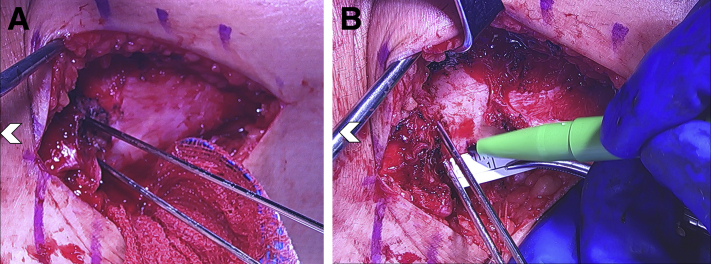
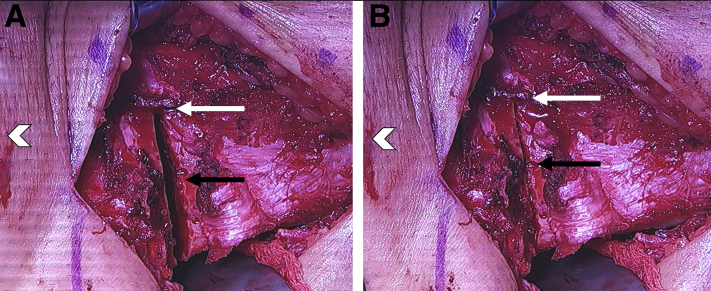
Diagnostic arthroscopy is performed before the osteotomy. Concomitant pathology may be addressed at this time, and the medial compartment is further assessed for any damage that would contraindicate this procedure. In general, we do not use a tourniquet during the procedure. A standard medial approach to the proximal tibia is used with the incision centered over the medial border of the tibia from 1 cm distal to the level of the joint line to about 4 finger-breadths distal to the top of the tibial tubercle. The sartorius fascia is split and the upper border of the pes tendons are identified and elevated from its tibial insertion to allow access to the posterior border of the tibia (Fig 4). The superficial medial collateral ligament is then split in line with its fibers at the posterior one-third and elevated from the posteromedial border of the tibia proximally and distally (Fig 4). This subperiosteal dissection is continued around the posterior border of the tibia and to the posterior aspect of the proximal tibiofibular joint, which is palpated to ensure adequate dissection. A lap sponge is packed into this space, and a 1-inch malleable retractor is placed across to the proximal tibiofibular joint.
Fig 4.
Intraoperative photographs of a left leg with a medial approach to the proximal tibia. Patient is positioned supine with head of the patient on the left side of the figures. (A) The pes tendons (black arrow) are identified and the upper portion is released to expose the superficial MCL (asterisk). (B) A split is made at the posterior border of the superficial MCL (asterisk) down to bone using electrocautery. (C) The posterior aspect of the superficial MCL and musculature is elevated subperiosteally from the posteromedial border of the proximal tibia. (MCL, medial collateral ligament.)
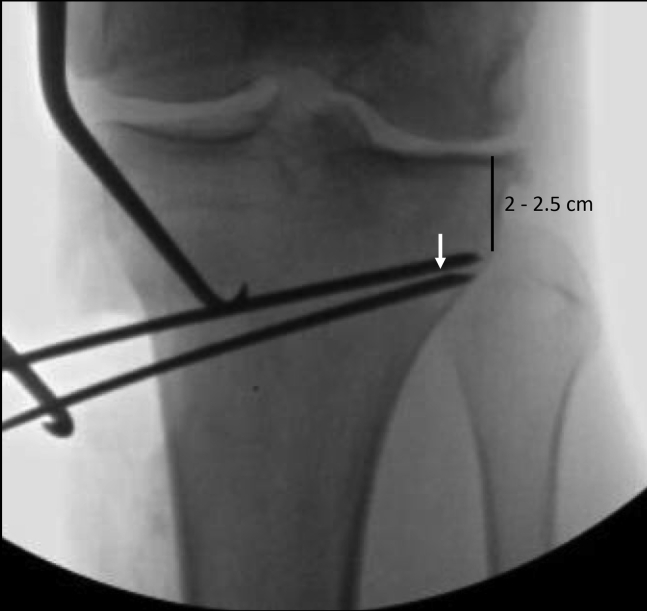
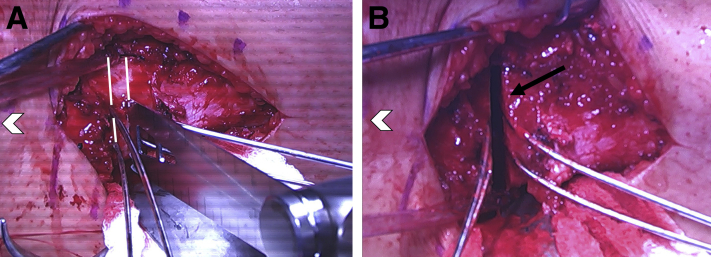
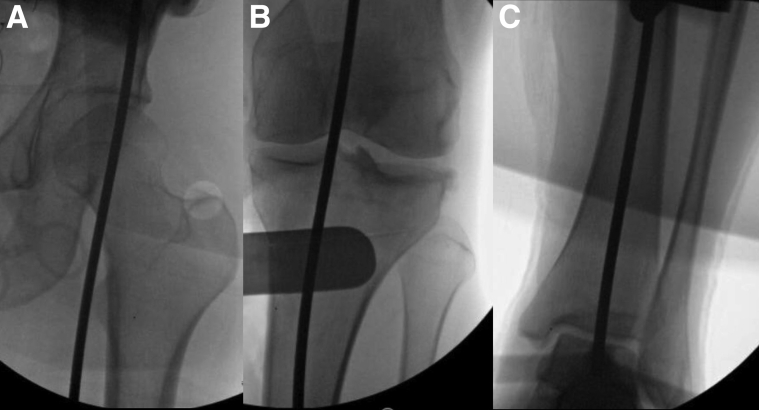
Fluoroscopy is then used to confirm the starting point for the initial K-wire. The starting point is at the upper border of the tibial tubercle or no more than 1 cm distal to this point. The first K-wire is then driven across the tibia to a point about 2 to 2.5 cm distal to the lateral tibial joint surface toward the proximal tibiofibular joint to establish the trajectory of the osteotomy (Fig 5). It is important to leave at least 5 to 10 mm of lateral tibial cortex intact as a “hinge” to preserve stability of the osteotomy. A second K-wire is then placed in line with this K-wire and parallel to the joint surface to match the posterior tibial slope, which can be assessed by slightly flexing the knee on a bump to obtain an anteroposterior view along the joint line. The medial collateral ligament is then split perpendicular to its fibers in line with these K-wires, and elevated about 1 cm distally to expose the medial tibia cortex (Fig 6A). A ruler is then used to measure the desired size of our wedge at the medial cortex that was determined with our preoperative plan (Fig 6B). A third K-wire is then drilled from this point toward the tip of our first K-wire. It is important for this K-wire to be placed to allow the saw blade or osteotomes to get to within 1 cm of the far lateral cortex for the osteotomy (Fig 5). A fourth K-wire is placed in line with the third K-wire and again parallel with the tibial slope (Fig 7).
Fig 5.
Intraoperative fluoroscopy showing placement of the K-wires. The upper K-wires are placed about 2 to 2.5 cm below the lateral tibia joint line. The third and fourth K-wires are placed to allow the saw blade or osteotomes to cut to the desired depth for the osteotomy between the tips of the K-wires (white arrow).
Fig 6.
Intraoperative photographs of a left leg with a medial approach to the proximal tibia. Patient is positioned supine with white arrowhead pointing toward the head of the patient. (A) The superficial MCL is split along the inferior edge of these K-wires to expose the medial cortex. (B) A ruler is then used to measure the desired correction and marked for placement of the third K-wire. (MCL, medial collateral ligament.)
Fig 7.
Intraoperative photographs of a left leg with a medial approach to the proximal tibia. Patient is positioned supine with white arrowhead pointing toward the head of the patient. Four K-wires are in place to create the wedge of bone to be removed
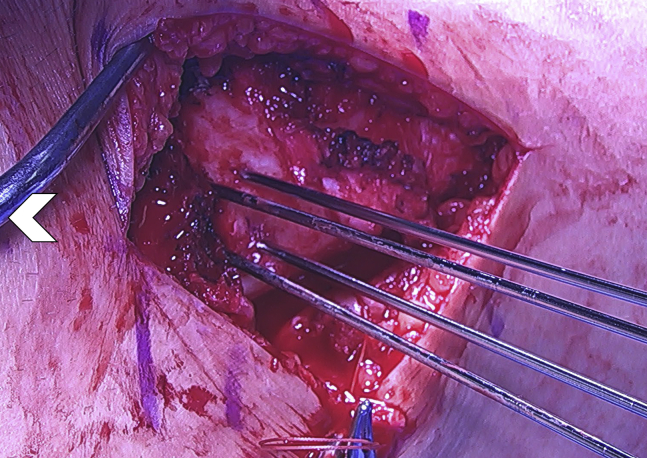
The proximal K-wires can be bent proximally and the distal K-wires can be bent distally to allow working space for the saw. An initial retrotubercle cut is made in line with the tibial shaft to preserve at least 1 cm of bone behind the tibial tubercle (Fig 8). An oscillating saw (CONMED, Utica, NY) is then used to start the medial tibia cuts between the K-wires. The saw cut is made about three-fourths of the way across the tibia and the cut is completed using thin osteotomes (Fig 9).
Fig 8.
Intraoperative photographs of a left leg with a medial approach to the proximal tibia. Patient is positioned supine with white arrowhead pointing toward the head of the patient. (A) The initial retrotubercle cut (black arrow) is made with a quarter-inch saw blade (CONMED, Utica, NY). (B) The retrotubercle cut is shown (black arrow) with the planned medial wedge saw cuts (white lines).
Fig 9.
Intraoperative photographs of a left leg with a medial approach to the proximal tibia. Patient is positioned supine with white arrowhead pointing toward the head of the patient. (A) The medial tibial cuts (white lines) are made using an oscillating saw (CONMED). (B) The medial tibia cut is shown after removal of the cortical bone wedge (black arrow).
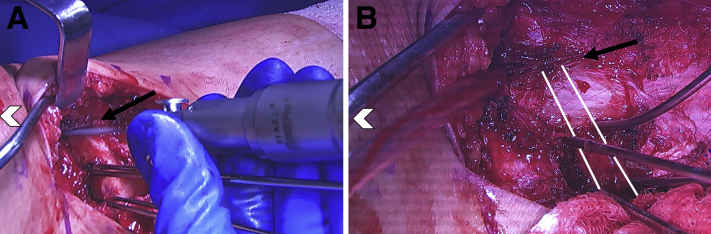
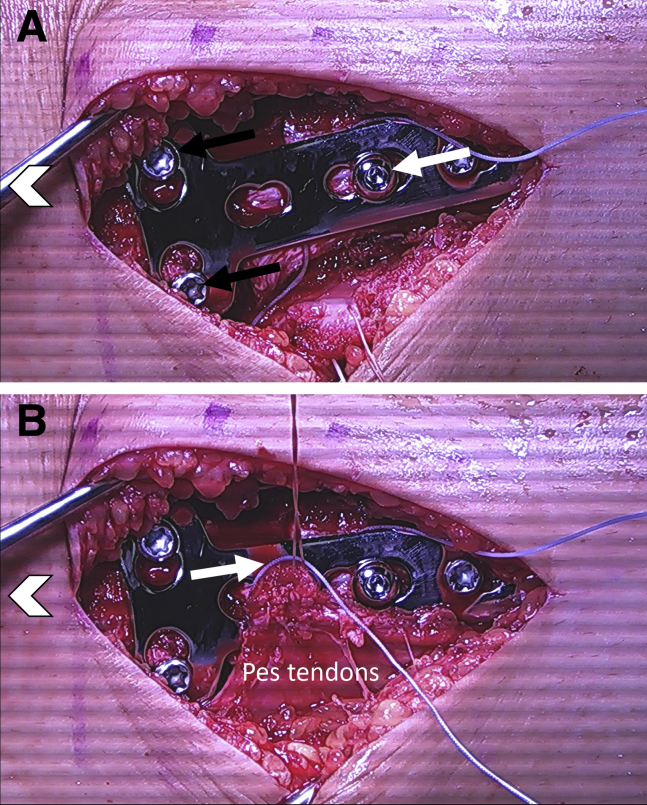
The osteotomy site is then manually closed by placing a gentle varus force across the lower leg (Fig 10). A limb-alignment rod is used to confirm the amount of correction with fluoroscopic views centered at the hip, knee, and ankle (Fig 11). The osteotomy may be provisionally held with a staple at this point, or held by hand. Fixation of the osteotomy is achieved using a 4-hole 4.5-mm locking compression plate T-plate from the large fragment set (Depuy Synthes; West Chester, PA) (Fig 12). A nonabsorbable #2 FiberWire suture (Arthrex, Naples, FL) will be placed under the plate before fixation to allow for repair of the pes tendons if needed. Proximal locking screws are placed through the plate first, and then a nonlocking screw is placed in compression mode distal to the osteotomy site.
Fig 10.
Intraoperative photographs of a left leg with a medial approach to the proximal tibia. Patient is positioned supine with white arrowhead pointing toward the head of the patient. (A) The medial tibia osteotomy is show (black arrow) with the retro-tubercle biplanar cut (white arrow). (B) Varus force is applied to close the osteotomy site (black arrow) and this will slide along the retrotubercle cut (white arrow).
Fig 11.
Anteroposterior fluoroscopic views of the hip, knee, and ankle using a straight metal alignment rod to assess the intraoperative alignment from (A) the center of the hip, (B) through the knee, and (C) to the center of the ankle.
Fig 12.
Intraoperative photographs of a left leg with a medial approach to the proximal tibia. Patient is positioned supine with white arrowhead pointing toward the head of the patient. (A) Fixation of the osteotomy is achieved using a 4.5-mm locking compression plate (Synthes) and the 2 proximal locking screws are placed first (black arrows), followed by a cortical screw to compress the osteotomy (white arrow). (B) The pes tendons are then repaired over the plate using the FiberWire (Arthrex) suture that was placed under the plate (white arrow).
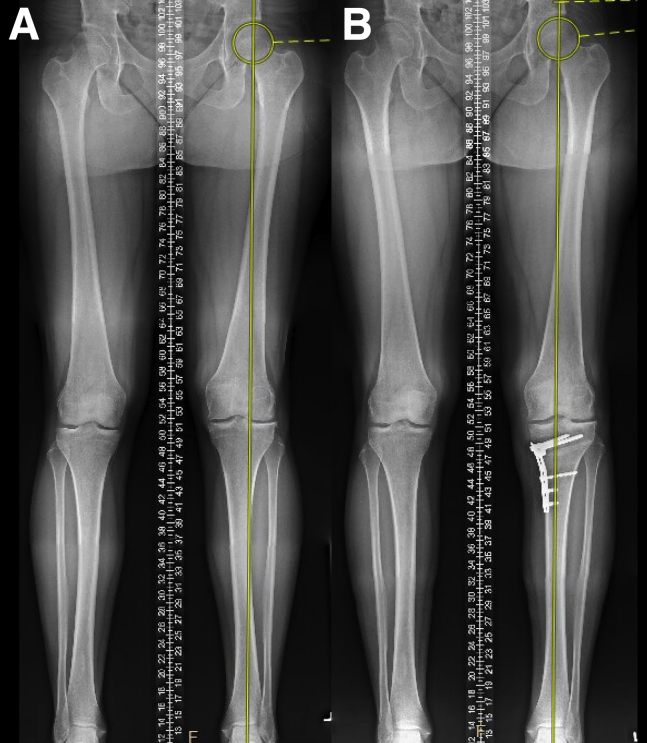
The postoperative protocol is summarized in Table 3. Full-length radiographs are obtained at 6 weeks if patient is weight bearing without pain to assess correction and repeated at 1 year postoperatively (Figs 13 and 14).
Table 3.
Postoperative Protocol
| Intraoperative |
Day 0 - 1
Weeks 0-2
Weeks 3-4
|
DVT, deep vein thrombosis; HKB, hinged knee brace; ROM, range of motion.
Fig 13.
(A) Preoperative full-length standing anteroposterior radiograph demonstrating the mechanical axis of the lower limb through the lateral compartment. (B) Postoperative full-length standing anteroposterior radiograph demonstrating the mechanical axis of the lower corrected to the medial tibial spine.
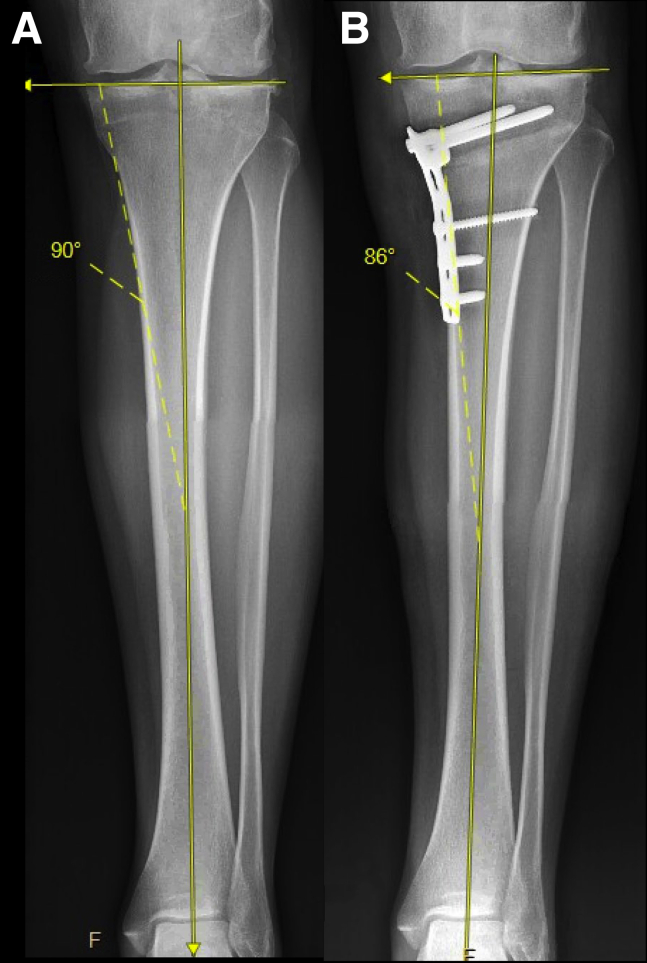
Fig 14.
(A) Preoperative full-length tibia anteroposterior radiograph demonstrating the mMPTA. (B) Postoperative full-length tibia anteroposterior radiograph demonstrating the mMPTA increased to 4° of varus. (mMPTA, mechanical medial proximal tibial angle.)
Discussion
Patients indicated for MCWPTO are younger, active, and often have sustained previous injury to the lateral compartment cartilage or meniscus with mild-to-moderate valgus alignment. Studies have also demonstrated that lateral compartment disease preferentially affects the joint posteriorly in deeper knee flexion angles—both in lateral compartment arthritis and after partial lateral meniscectomy.10,11 One of the primary advantages of performing a tibial osteotomy over a femoral-based is the ability to alter joint contact forces both in flexion and extension.6
One important consideration when performing this technique is the obliquity of the joint line at the knee. It has been reported that 12° of valgus is the upper limit of acceptable correction using a proximal tibia osteotomy to avoid creating an excessive mechanical medial proximal tibia articular angle.4,12,13 One of the earliest osteotomy studies by Shoji and Insall14 demonstrated that gradual subluxation of the tibia will occur if more than 10° of medial tibia tilting is created.14 More recent clinical studies have supported a joint surface tilt of 10° or less is well tolerated.4,7,15 This concern for excessive joint line obliquity has been cited as a reason for the MCWPTO technique falling out of favor.8,16,17 In the authors’ experience, this technique is best suited for patients with mild-to-moderate valgus (up to 8°). In the case presented here, 4° of varus joint line obliquity was created (Fig 14).
Other risks of this procedure include intra-articular fracture—often due to placement of the guide pin within 2 cm of the lateral joint line. Fracture of the lateral hinge may also occur, requiring more robust fixation with a larger plate and screws, or an additional lateral incision to place a staple at the lateral hinge. Tibial slope can also be altered and especially in cases of anterior or posterior ligamentous instability should be carefully assessed pre- and intraoperatively. Overcorrection into varus should also be avoided, as this is generally not well tolerated.4,15 Other complications inherent to osteotomy procedures include non-union, malunion, wound complications, infection, thromboembolism, stiffness, and painful hardware requiring reoperation.1,6,7
There are very few published studies on long-term clinical outcomes after MCWPTO. In the largest series of 47 patients, Chambat et al.4 reported that 72% had “good” or “very good” results with an improvement in pain in 91% at a mean 7 years of follow-up. They concluded that the ideal correction is to about neutral, joint line obliquity must be less than 10° of varus, and younger patients with mild arthritis had better outcomes. Coventry13 reported on 31 knees treated with MCWPTO for painful lateral compartment arthritis associated with valgus malalignment. At an average follow-up of 9.4 years (range: 2-17 years), the author reported 77% had no pain or mild pain, 19% with moderate pain, and 1 patient with severe pain. Six knees required conversion to total knee arthroplasty at an average of 9.8 years after osteotomy.13 Puddu et al.7 reported on 6 cases with excellent improvement of pain and functional capabilities.
In conclusion, this technical note describes our preferred technique to correct mild-to-moderate valgus malalignment in patients with symptomatic lateral compartment disease via a MCWPTO. Although modern studies are needed to evaluate the clinical outcomes using this technique, the authors believe this procedure is a reproducible and effective treatment option to reduce pain and improve function in a younger patient population in whom arthroplasty is less desirable.
Acknowledgments
R.A.D. would like to acknowledge and thank Dr. Andreas Gomoll for all of his teaching and advice when first learning this technique.
Footnotes
The authors report the following potential conflict of interest or source of funding: R.A.D. reports other from Arthrex, from null, outside the submitted work. D.F. reports grants and other from Smith & Nephew, other from DePuy Mitek, grants and other from Zimmer Biomet, grants and other from Vericel, other from MTF, other from KCRN, other from Hyalex, grants and other from CartiHeal, grants and other from Anika Therapeutics, grants and other from Aesculap, and grants and other from Moximed, outside the submitted work. C.K. reports other from Smith & Nephew, grants from Active Implants, grants from Zimmer Biomet, and grants from Vericel, outside the submitted work. R.M. reports other from Arthrex and grants from Zimmer Biomet, outside the submitted work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
A technique for medial closing-wedge proximal tibia osteotomy is presented. Arthroscopy is performed before the osteotomy to address intra-articular pathology and assess the medial compartment. The osteotomy is performed through a direct medial approach to the proximal tibia. K-wires are placed to create a rectangular wedge of bone that is removed with an oscillating saw and osteotomes. The osteotomy is then closed and fixation is achieved with a locking plate.
References
- 1.Zampogna B., Vasta S., Papalia R. Patient evaluation and indications for osteotomy around the knee. Clin Sports Med. 2019;38:305–315. doi: 10.1016/j.csm.2019.02.011. [DOI] [PubMed] [Google Scholar]
- 2.Hsu A.C., Tirico L.E.P., Lin A.G., Pulido P.A., Bugbee W.D. Osteochondral allograft transplantation and opening wedge tibial osteotomy: Clinical results of a combined single procedure. Cartilage. 2018;9:248–254. doi: 10.1177/1947603517710307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Harris J.D., McNeilan R., Siston R.A., Flanigan D.C. Survival and clinical outcome of isolated high tibial osteotomy and combined biological knee reconstruction. Knee. 2013;20:154–161. doi: 10.1016/j.knee.2012.12.012. [DOI] [PubMed] [Google Scholar]
- 4.Chambat P., Ait Si Selmi T., Dejour D., Denoyers J. Varus tibial osteotomy. Oper Tech Sports Med. 2000;8:44–47. [Google Scholar]
- 5.Wylie J.D., Schiederer B., Obopilwe E. The effect of lateral opening wedge distal femoral varus osteotomy on tibiofemoral contact mechanics through knee flexion. Am J Sports Med. 2018 doi: 10.1177/0363546518799353. 036354651879935. [DOI] [PubMed] [Google Scholar]
- 6.Collins B., Getgood A., Alomar A.Z. A case series of lateral opening wedge high tibial osteotomy for valgus malalignment. Knee Surg Sport Traumatol Arthrosc. 2013;21:152–160. doi: 10.1007/s00167-012-2070-y. [DOI] [PubMed] [Google Scholar]
- 7.Puddu G., Cipolla M., Cerullo G., Franco V., Giannì E. Which osteotomy for a valgus knee? Int Orthop. 2010;34(2 SPECIAL ISSUE):239–247. doi: 10.1007/s00264-009-0820-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sherman C., Cabanela M.E. Closing wedge osteotomy of the tibia and the femur in the treatment of gonarthrosis. Int Orthop. 2010;34(2 SPECIAL ISSUE):173–184. doi: 10.1007/s00264-009-0883-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Klecker R.J., Winalski C.S., Aliabadl P., Minas T. The aberrant anterior tibial artery surgical implications. Am J Sports Med. 2008;36:720–727. doi: 10.1177/0363546507311595. [DOI] [PubMed] [Google Scholar]
- 10.Gulati A., Chau R., Beard D.J., Price A.J., Gill H.S., Murray D.W. Localization of the full-thickness cartilage lesions in medial and lateral unicompartmental knee osteoarthritis. J Orthop Res. 2009;27:1339–1346. doi: 10.1002/jor.20880. [DOI] [PubMed] [Google Scholar]
- 11.Scott C.E.H., Nutton R.W., Biant L.C. Lateral compartment osteoarthritis of the knee: Biomechanics and surgical management of end-stage disease. Bone Jt J. 2013;95 B:436–444. doi: 10.1302/0301-620X.95B4.30536. [DOI] [PubMed] [Google Scholar]
- 12.Nakayama H., Schröter S., Yamamoto C. Large correction in opening wedge high tibial osteotomy with resultant joint-line obliquity induces excessive shear stress on the articular cartilage. Knee Surg Sport Traumatol Arthrosc. 2018;26:1873–1878. doi: 10.1007/s00167-017-4680-x. [DOI] [PubMed] [Google Scholar]
- 13.Coventry M.B. Proximal tibial varus osteotomy for osteoarthritis of the lateral compartment of the knee. J Bone Joint Surg Am. 1987;69:32–38. [PubMed] [Google Scholar]
- 14.Shoji H., Insall J. High tibial osteotomy for osteoarthritis of the knee with valgus deformity. J Bone Joint Surg Am. 1973;55:963–973. [PubMed] [Google Scholar]
- 15.Marti R.K., Verhagen R.A., Kerkhoffs G.M., Moojen T.M. Proximal tibial varus osteotomy. Indications, technique, and five to twenty-one-year results. J Bone Joint Surg Am. 2001;83:164–170. [PubMed] [Google Scholar]
- 16.Puddu G., Cipolla M., Cerullo G., Franco V., Giannì E. Osteotomies: The surgical treatment of the valgus knee. Sports Med Arthrosc. 2007;15:15–22. doi: 10.1097/JSA.0b013e3180305c76. [DOI] [PubMed] [Google Scholar]
- 17.Mattei L., Lea S., Nicolaci G., Ferrero G., Marmotti A., Castoldi F. Closing wedge tibial osteotomy: is it an actual procedure nowadays? Ann Joint. 2017;2 30-30. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A technique for medial closing-wedge proximal tibia osteotomy is presented. Arthroscopy is performed before the osteotomy to address intra-articular pathology and assess the medial compartment. The osteotomy is performed through a direct medial approach to the proximal tibia. K-wires are placed to create a rectangular wedge of bone that is removed with an oscillating saw and osteotomes. The osteotomy is then closed and fixation is achieved with a locking plate.