Abstract
A greater understanding of the deleterious consequences that a meniscal root tear brings to the knee joint and how its surgical repair can be advantageous over the previously used treatment strategies brings the need for the development of surgical techniques that make the procedure less complex and more reproducible. When meniscal root rupture occurs, a mechanical overload occurs in the affected compartment similar to a total meniscectomy. Several authors have concluded that meniscal root reinsertion significantly improves postoperative outcomes and patient satisfaction, regardless of age or laterality of the meniscal injury. The Meniscus 4 A-II device (Rio de Janeiro, Brazil) allows stitching at the root of the medial and lateral menisci. In this article, we describe the surgical repair technique for posterior-medial and -lateral meniscal root tears using this meniscal suture device. This technique is fast and effective.
The meniscus is a semilunar fibrocartilage present in the medial and lateral compartments of the knees. Its main functions are load absorption and distribution, joint stability, proprioception, and lubrication.1
Meniscal root tears are radial lesions, located up to 0.9 mm from their insertion, or bony avulsions at this level.2 Posterior root tears of the medial meniscus are most commonly degenerative in middle-aged women, occurring during usual, everyday movements such as a slight squat, and correspond to 20% of posterior horn tears of this meniscus. Injuries of the posterior root of the lateral meniscus are closely associated with traumatic injuries of the anterior cruciate ligament.3
One of the pioneering works on the subject was published in 2008 by Allaire et al.4 In this study, the authors showed the biomechanical importance of the meniscal roots, proving that when meniscal root rupture occurs, there is a mechanical overload in the affected compartment similar to a total meniscectomy.
The gold standard for diagnosis is magnetic resonance imaging, and the main suggestive findings are a hyperintense signal perpendicular to the meniscus on the axial view, compatible with a radial lesion; signs of truncation and extrusion greater than 3 mm on the coronal view; and the ghost sign on the sagittal view.5 Meniscal root repair aims to recover joint kinematics, absorption capacity, and load distribution and thus prevent the development of osteoarthritis. LaPrade et al.3 in 2017 published a cohort evaluating 50 knees in 49 patients undergoing meniscal root reinsertion. These patients were divided into 2 groups: those younger than 50 years and those 50 years or older. The study reported that meniscal root reinsertion significantly improved postoperative outcomes and patient satisfaction, regardless of age or laterality of the meniscal injury. Patients younger than 50 years had similar outcomes to those 50 years or older, as did patients who underwent medial versus lateral root repair.3
The Meniscus 4 A-II device (Rio de Janeiro, Brazil) (Fig 1A) makes it possible to perform stitches at the root of the medial and lateral menisci by creating a posteromedial portal for treatment of posterior-medial root tears and a conventional lateral access with identification of the fibular ligament and popliteal tendon for treatment of posterior root tears of the lateral meniscus. In this article, we describe the surgical technique for reinsertion of the posterior meniscal root of the medial and lateral menisci using the Meniscus 4 A-II meniscal suture device. This technique is fast and effective.
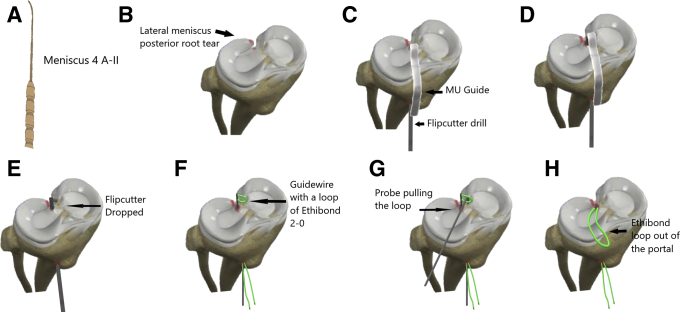
Fig 1.
(A) Meniscus 4 A-II device. (B) Posterior root lesion of lateral meniscus. (C, D) Arthrex MU (multiuse) guide with 6-mm FlipCutter drill positioned on footprint of posterior root of lateral meniscus. (E) Horizontalized FlipCutter drill ready to drill 10-mm-deep tibial tunnel. (F) Inverted needled guidewire crossed by tibial tunnel acting as transport wire. (G) With a probe, a loop of the wire is pulled to the anterolateral portal. (H) Loop formed on anterolateral portal.
Surgical Technique
The patient is anesthetized with spinal cord anesthesia, and a pneumatic cuff is attached to the proximal third of the thigh. Asepsis and antisepsis are performed using detergent chlorhexidine, followed by alcoholic chlorhexidine. Sterile surgical fields are positioned, and the pneumatic cuff is inflated.
Posterior-Lateral Meniscal Root Repair
Standard arthroscopic portals are made beyond a transpatellar accessory portal longitudinally in the center of the patellar tendon. Joint inventory is performed, and the root lesion of posterior-lateral meniscus (Fig 1B) and anterior cruciate ligament rupture are diagnosed.
For the surgical treatment of posterior root injuries of the lateral meniscus, an additional lateral posterolateral access of about 6 cm in length is recommended. The surgical access is performed following the posterior face of the iliotibial tract centered on the articular line toward the Gerdy tubercle. The iliotibial tract is identified via superficial dissection and is incised in its posterior one-third in the same direction as its fibers. Care must be taken during this last step not to injure the lateral collateral ligament. Digital dissection is always performed with care to remain anterior to the tendon of the femoral biceps head to avoid fibular nerve injury and not to dissect posterior to the lateral head of the gastrocnemius.6
We perform reinsertion of the meniscal root through a transtibial bone tunnel. To achieve this, we introduce the MU (multiuse) guide (Arthrex, Naples, FL) through the anterolateral portal, positioning it over the anatomic position of the posterior root of the lateral meniscus (Fig 1C). We introduce a 6-mm FlipCutter drill bit (Arthrex) (Fig 1 D and E). We drop the drill tip within the joint and retract 10 mm, creating a hole measuring 6 mm diameter and 10 mm deep in the anatomic position of the posterior root of the lateral meniscus. We keep the FlipCutter drill cannula fixed to the bone; remove the drill; and and insert an inverted needled guidewire with a No. 2-0 Ethibond wire (Ethicon, Somerville, NJ, U.S.A.) passed over this end, forming a loop, serving as a structure for suture thread transport in the future (Fig 1F). Using 2-finger tweezers, we pull the loop into the anterolateral portal (Fig 1H), remove the metal cannula attached to the bone, and repair the Ethibond wire loop.
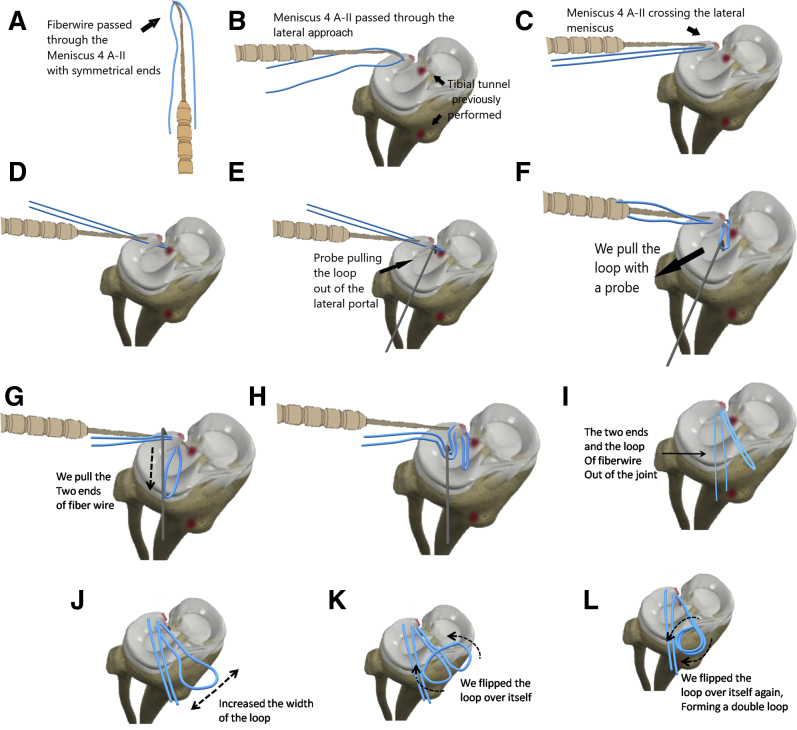
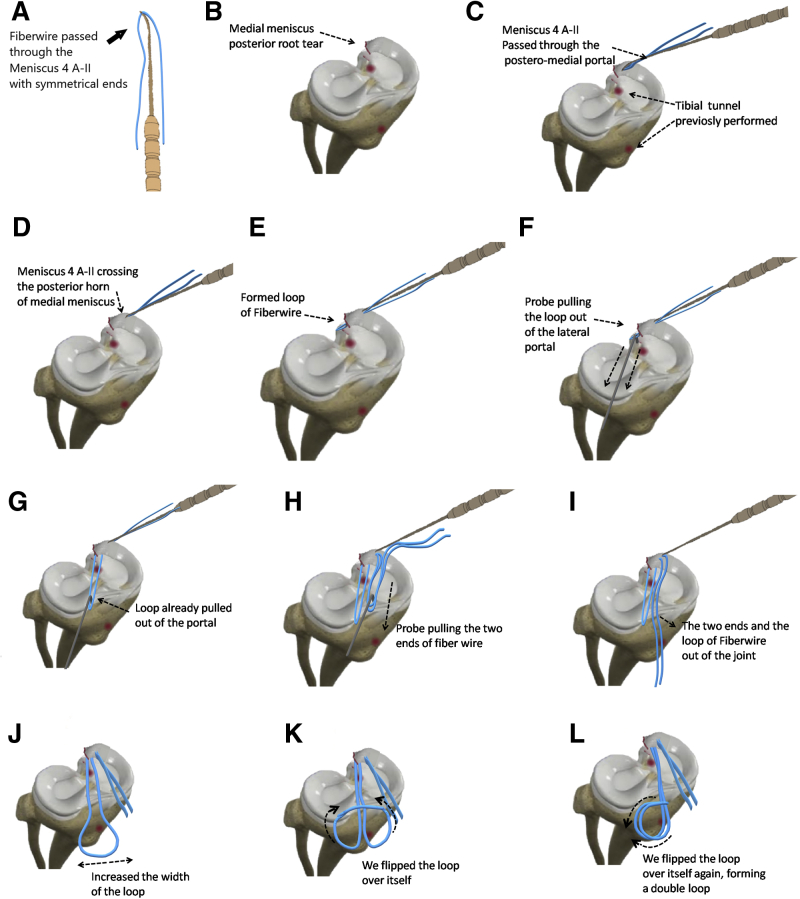
We prepare the Meniscus 4 A-II meniscal suture device with No. 2-0 FiberWire thread (Arthrex) passed through its end folded into 2 symmetrical parts (Fig 2A). We identify the popliteal tendon and introduce the device with the optics positioned on the transpatellar portal, with the knee in the figure-of-4 position forcing varus, consequently opening the lateral compartment. We visualize the Meniscus 4 A-II passing along the popliteal tendon and proximal to the posterior horn of the lateral meniscus (Fig 2B). We place the meniscal repair device over the posterior horn of the lateral meniscus and introduce it from proximal to distal at the posterior root of the lateral meniscus (Fig 2 C and D). With 2-finger tweezers or a probe introduced through the lateral portal, we pull the handle formed on the distal side of the meniscus to the center of the lateral compartment, keeping it fixed to the 2-finger tweezers (Fig 2 E-G); after this step, we remove the meniscal suture device through the lateral access. By use of 2-finger tweezers or a probe again, the 2 ends of the FiberWire that were out of the joint in the lateral access are pulled into the joint (Fig 2 H and I). We pull the ends and loop formed from the FiberWire out of the joint through the lateral portal. Already outside of the portal, we make a stitch called “Mickey's ear” with the handle and the 2 ends of the FiberWire (Fig 2 J-N). This type of stitch enables the handle to run into the joint locking the point at the root of the lateral meniscus. We repeat this step with 2 more No. 2-0 FiberWire strands. We enter the optics through the medial portal and enter the tweezers through the central portal; pull all the wires together, including the Ethibond loop previously formed, to the outside of the joint through the central portal; and pass the wires inside the Ethibond loop handle. This loop of Ethibond is the one that is passed through the tibial tunnel (Fig 2O). We pull the Ethibond wire distally, carrying the 3 wires with their respective 6 legs to the outside of the tibial tunnel (Fig 2P). We apply traction to them, visualizing the reduction of the lateral meniscus to its anatomic position, even observing the opening of the articular space with the reduced meniscus (Video 1). Fixation can be performed with a traditional EndoButton (Smith & Nephew, Andover, MA), with an ABS Button (Arthrex) (Fig 2Q), or even with a large fragment screw and washer as a pole-type device.
Fig 2.
(A) No. 2-0 FiberWire symmetrically passed through Meniscus 4 A-II device. (B) We introduce the Meniscus 4 A-II device posterior and proximal to the popliteal tendon, extending into the proximal side of the lateral meniscus. (C, D) With the meniscal suture device, we pierce the posterior horn of the lateral meniscus from the proximal to distal surface. (E-G) With a probe, we pull a handle of the No. 2-0 FiberWire out of the joint through the anterolateral portal. (H, I) With a probe, we pull both ends of the FiberWire out of the anterolateral portal. (J-N) We pass the 2 ends of the wire through a loop formed at the end of the No. 2-0 FiberWire and pull the 2 ends, causing the tip to run to the posterior horn of the lateral meniscus. (O) We pass the free ends of the wire through the preformed loop to be transported to the tibial tunnel. (P) Reduction of the meniscus to its anatomic position is observed. (Q) Tibial fixation is performed with an ABS Button.
Posterior-Medial Meniscal Root Repair
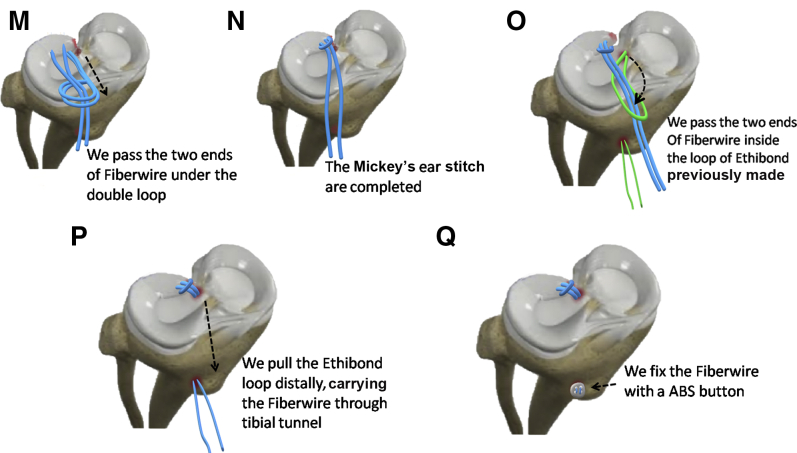
Standard arthroscopic portals are made beyond a transpatellar accessory portal longitudinally in the center of the patellar tendon. Joint inventory is performed, and the root lesion of the posterior-medial meniscus is diagnosed (Fig 3A). We make a posteromedial accessory portal by transillumination, entering a Jelco 14-gauge catheter (Smiths Medical, Minneapolis, MN) under direct view.6 In cases with a tight medial compartment, we use a pie-crusting technique for the medial collateral ligament, also with a Jelco number 14.7
Fig 3.
(A) Posterior root lesion of medial meniscus. (B) The MU (multiuse) guide is positioned under the anatomic position of the posterior root of the medial meniscus with the FlipCutter drill. (C) The FlipCutter is introduced through the tibial bone. (D) The horizontalized FlipCutter drill is ready to drill a 10-mm-deep tibial tunnel. (E) Inverted needled guidewire crossed by tibial tunnel acting as transport wire. (F) With a probe, we pull a loop of the wire to the anterolateral portal. (G) Loop formed on anterolateral portal.
We introduce the MU guide through the medial portal, positioning it under the anatomic position of the posterior root of the medial meniscus (Fig 3B). After confirming the correct positioning of the MU guide, we introduce the 6-mm FlipCutter drill (Fig 3C). We drop the drill tip within the joint and retract 10 mm, creating a hole measuring 6 mm in diameter and 10 mm deep in the anatomic position of the posterior root of the medial meniscus (Fig 3D). We keep the FlipCutter drill cannula fixed to the bone; remove the drill; and insert a guidewire with its needled end proximally, with a No. 2-0 Ethibond wire with thread passed through its end folded into 2 symmetrical parts, serving as a frame for future transport within the joint (Fig 3E). Using 2-finger tweezers or a probe, we pull the loop to the lateral portal, remove the metal cannula attached to the bone, and repair the Ethibond wire loop (Fig 3 F and G).
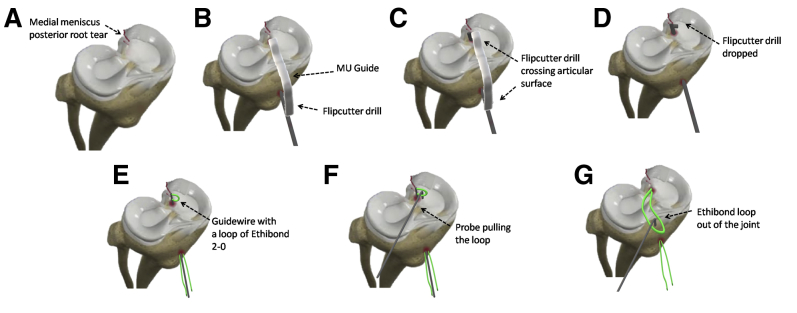
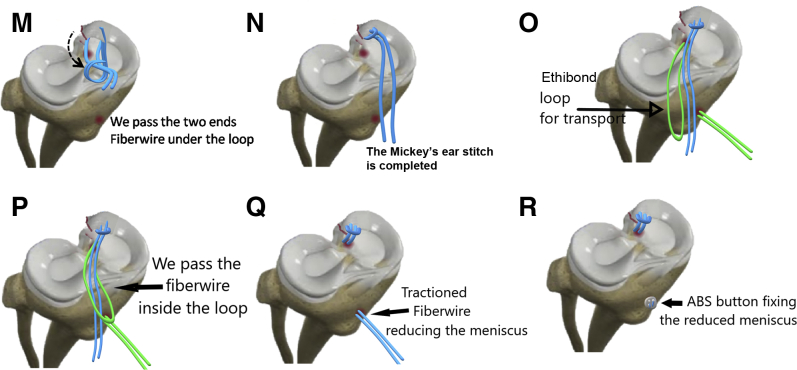
We prepare the Meniscus 4 A-II meniscal suture device with No. 2-0 FiberWire thread passed through its end foldend into 2 symmetrical parts (Fig 4A). We introduce the device in the direction of articulation through the posteromedial portal, with the optics positioned in the transpatellar portal, forcing the knee into a valgus position to open the medial compartment and identifying the posterior meniscal root lesion (Fig 4B). We visualize the Meniscus 4 A-II passing proximal to the posterior horn of the medial meniscus (Fig 4 C-E). We place the meniscal repair device over the posterior horn of the medial meniscus and introduce it from proximal to distal at the posterior root of the medial meniscus. With 2-finger tweezers or a probe introduced through the medial portal, we pull the loop formed on the distal face of the meniscus to the anterolateral portal, keeping it fixed on the tweezers or probe (Fig 4 F and G), after which we remove the meniscal suture device through the posteromedial portal. Using 2-finger tweezers or a probe again, we pull the 2 ends of the FiberWire (which were out of the joint into the posteromedial portal) into the anterolateral portal (Fig 4 H and I). Already outside the portal, we make a Mickey's ear stitch with the handle and the 2 ends of the FiberWire; this type of stitch enables the handle to run into the joint locking the point at the root of the medial meniscus (Fig 4 J-N). We repeat this step with 2 more No. 2-0 FiberWire strands. We enter the optics through the lateral portal and enter the tweezers through the central portal; pull all the wires together, including the Ethibond loop, to the outside of the joint through the central portal; and pass the wires inside the Ethibond loop handle. This loop of Ethibond is the one that is passed through the tibial tunnel (Fig 4 O-Q). We pull the Ethibond wire distally, carrying the 3 wires with their respective 6 legs to the outside of the tibial tunnel. We apply traction to them and visualize the reduction of the medial meniscus to its anatomic position while observing the opening of the articular space with the reduced meniscus. Fixation can be performed with a traditional EnboButton, with an ABS Button (Fig 4R), or even with a large fragment screw and washer as a pole-type device.
Fig 4.
(A) No. 2-0 FiberWire symmetrically passed through Meniscus 4 A-II device. (B) Posterior root lesion of medial meniscus (C) The meniscal suture device is introduced through the posteromedial portal, passing over the posterior horn of the medial meniscus. (D, E) We introduce the device from proximal to distal at the posterior root of the medial meniscus. (F, G) With a probe, we pull the loop formed on the distal face of the meniscus to the anterolateral portal, keeping it fixed on 2-finger tweezers or a probe. (H, I) We pull the 2 ends of the FiberWire (which were out of the joint into the posteromedial portal) into the anterolateral portal. (J-N) We pass the 2 ends of the wire through a loop formed at the end of the No. 2-0 FiberWire and pull the 2 ends, causing the tip to run to the posterior horn of the lateral meniscus. (O, P) We pass the free ends of the wire through the preformed loop to be transported to the tibial tunnel. (Q) Reduction of the meniscus to its anatomic position is observed. (R) Tibial fixation is performed with an ABS Button.
Rehabilitation
The patient remains non–weight bearing on the affected knee for the first 6 weeks. Passive range of motion is allowed from 0° to 90°, initiated on day 1 and maintained until the sixth week. Straight-leg raises are allowed from the first week. Progressive advancement to full weight bearing and gain of passive flexion is started from the sixth week. Deep squats and leg presses are not allowed until the third postoperative month.8,9
Discussion
Choi and Park10 evaluated 197 knees submitted to total knee arthroplasty and, during surgery, observed the integrity (or lack of integrity) of the roots of the medial meniscus. They observed that 78.17% of patients had meniscal root injury and found such injury in 92.8% of patients younger than 60 years. They concluded that the presence of posterior rupture of the medial meniscal root was significantly related to factors associated with the severity of osteoarthritis, such as the Kellgren-Lawrence scale, varus deformity, and mechanical axis deviation.10
In a study published in 2019, Hussain et al.11 reported a systematic review on the role of meniscal injury in the development of spontaneous knee osteonecrosis, concluding that in more than 80% of the cases analyzed in 26 published articles, the development of this pathology was closely related to meniscal injury or meniscectomy, and posterior root injury of the meniscus was the most prevalent. Another study, conducted at Mayo Clinic, Rochester, New York, showed that this type of meniscal injury can lead to early joint degeneration.12 The authors found evidence that 12 months after meniscal rupture, arthrosis may have already developed in the affected compartment in the patient in question. Choi et al.13 similarly showed a rapid progression to arthrosis in 42% of the patients evaluated, whereas Guermazi et al.14 observed that at 30 months of follow-up, high rates of arthrosis developed in patients with medial meniscal posterior root injury when compared with patients with other types of meniscal injury.
Lee et al.15 evaluated the healing of the meniscal root injury using second-look arthroscopy. Seventy percent of patients were stably healed and presented higher scores (Hospital for Special Surgery and International Knee Documentation Committee scores) than those with unstable healing. Therefore, Lee et al. observed improvement in clinical outcomes and the degenerative progress in patients with stable scar tissue.
Kodama et al.16 also performed a study analyzing second-look arthroscopy in patients submitted to tibial reinsertion of the posterior root of the medial meniscus. They evaluated preoperative and postoperative meniscal extrusion, correlating meniscal extrusion with chondral degeneration in the short term. They retrospectively assessed 22 patients who met the inclusion criteria for the study. They observed a clinical improvement with statistical significance in all patients in the short term, as well as a preservation of chondral deterioration with the knee in flexion. Nevertheless, they observed a progression of chondral lesion when the knee was evaluated in extension but without affecting the clinical results at 1 year postoperatively.
Until the advent of meniscal root repair techniques, the treatment options were conservative treatment and medial meniscal posterior horn meniscectomy, but both had poor and unsatisfactory results, with a 54% rate of progression to osteoarthritis in 4.5 years.16 Meniscal repair prevented the evolution to osteoarthritis in 79.7% of cases.17 It is noteworthy that there is no indication for this procedure when there is already osteoarthrosis with chondral involvement superior to Outerbridge grade 3 or mechanical deviation with varus greater than 5° that has not been previously corrected.8,18
Although reinsertion of the meniscal root at its original site is considered the best treatment option, this procedure is technically challenging because of its location quite posterior to the joint and tibial spines. Traditional meniscal repair devices such as all-inside and inside-out needles cannot suture such injuries. The most commonly used tweezers for posterior root repair are shoulder surgery tweezers as adapted for knee surgery. To facilitate posterior root repair, we have developed an inexpensive, easy-to-handle device that will allow surgeons around the world to repair meniscal root injuries quickly and reproducibly (Table 1).
Table 1.
Advantages, Disadvantages, and Risks of Meniscal Suture Device
| Advantages |
| Use of the device presents an angle of attack to the meniscal root from lateral to medial on the posterior horn of the lateral meniscus. |
| Use of the device presents an angle of attack to the meniscal root from medial to lateral on the posterior horn of the medial meniscus. |
| There is a lower risk of injury to the neurovascular popliteal bundle. |
| The device has a low cost and is resistant. |
| Disadvantages |
| A posterolateral approach is required for neurovascular protection. |
| A posteromedial portal is required. |
| It is necessary to create 3 anterior portals: anteromedial, anterolateral, and transpatellar tendon. |
| Risks |
| Fibular nerve injury |
| Chondral injury with tip of device |
| Theoretical possibility of patellar tendinitis |
Footnotes
The authors report the following potential conflicts of interest or sources of funding: J.L.R.d.F. has a patent pending for Dispositivo de Sutura Meniscal. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
We create a lateral access of approximately 6 cm in length, identify the iliotibial tract, and section it at its posterior third; below the iliotibial band, we identified the lateral collateral ligament. We also identify the fibular head and femoral biceps. We perform digital dissection between the posterior surface of the lateral femoral condyle and the head of the lateral gastrocnemius. During arthroscopic visualization, we identify the posterior root lesion of the lateral meniscus. We prepare the Arthrex MU (multiuse) guide with the 6-mm FlipCutter drill. We realize an anterolateral approach to the proximal tibia to make the transtibial tunnel for root reinsertion. We position the MU guide on the footprint of the posterior root of the lateral meniscus. After making sure that the drill is in the correct position, we horizontalize the tip of the FlipCutter drill and make a 10-mm-deep tunnel. We then pass an inverted needled guidewire as a transport wire and pull a loop of this wire to the anterolateral portal. We identify the popliteal tendon and introduce the Meniscus 4 A-II device posterior and proximal to the popliteal tendon, extending into the proximal side of the lateral meniscus. Using tweezers, we grasp the posterior horn of the lateral meniscus and pierce it. Again using tweezers, we pull a handle out of the joint through the anterolateral portal. With the same tweezers, we pull both ends of the FiberWire out of the anterolateral portal. We then make a stitch by passing the 2 ends of the wire through a new loop formed at the end of the loop and pulling the 2 ends, causing the tip to run to the posterior horn of the lateral meniscus. We repeated the same step by passing the meniscal suture device again through the posterior horn of the lateral meniscus. We pull the handle out of the joint through the anterolateral portal. We also pull into the anterolateral portal the 2 ends of the same wire out of the posterolateral approach, making the same point described above. Care must be taken to prevent the previous suture from becoming caught in the new stitch; if this occurs, we remove the wires from the previous stitch from inside the new suture. Then, we pull all the wires simultaneously out of the transpatellar portal to avoid catching any wires in the joint capsule. After this last step, we pass the free ends of the wires through the preformed loop to be transported to the tibial tunnel. Holding them inside the joint makes it easier for them to slide into the tibial tunnel. We pull the 4 wires together, observing the lateral meniscal root reinsertion, and finally fix the wires with a button or post screw.
References
- 1.Scott W.N., editor. Insall & Scott surgery of the knee. Elsevier; Amsterdam: 2012. [Google Scholar]
- 2.LaPrade C.M., James E.W., Cram T.R., Feagin J.A., Engebretsen L., LaPrade R.F. Meniscal root tears: A classification system based on tear morphology. Am J Sports Med. 2015;43:363–369. doi: 10.1177/0363546514559684. [DOI] [PubMed] [Google Scholar]
- 3.LaPrade R.F., Matheny L.M., Moulton S.G., James E.W., Dean C.S. Posterior meniscal root repairs: Outcomes of an anatomic transtibial pull-out technique. Am J Sports Med. 2017;45:884–891. doi: 10.1177/0363546516673996. [DOI] [PubMed] [Google Scholar]
- 4.Allaire R., Muriuki M., Gilbertson L., Harner C.D. Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy. J Bone Joint Surg Am. 2008;90:1922–1931. doi: 10.2106/JBJS.G.00748. [DOI] [PubMed] [Google Scholar]
- 5.LaPrade R.F., Ho C.P., James E., Crespo B., LaPrade C.M., Matheny L.M. Diagnostic accuracy of 3.0 T magnetic resonance imaging for the detection of meniscus posterior root pathology. Knee Surg Sports Traumatol Arthrosc. 2015;23:152–157. doi: 10.1007/s00167-014-3395-5. [DOI] [PubMed] [Google Scholar]
- 6.Chahla J., Serra Cruz R., Cram T.R., Dean C.S., LaPrade R.F. Inside-out meniscal repair: Medial and lateral approach. Arthrosc Tech. 2016;5:e163–e168. doi: 10.1016/j.eats.2015.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Todor A., Caterev S., Nistor D.V. Outside-in deep medial collateral ligament release during arthroscopic medial meniscal surgery. Arthrosc Tech. 2016;5:781–785. doi: 10.1016/j.eats.2016.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pache S., Aman Z.S., Kennedy M. Meniscal root tears: Current concepts review. Arch Bone Jt Surg. 2018;6:250–259. [PMC free article] [PubMed] [Google Scholar]
- 9.Fujii M., Furumatsu T., Kodama Y. A novel suture technique using the FasT-Fix combined with Ultrabraid for pullout repair of the medial meniscus posterior root tear. Eur J Orthop Surg Traumatol. 2017;27:559–562. doi: 10.1007/s00590-017-1930-z. [DOI] [PubMed] [Google Scholar]
- 10.Choi E.S., Park S.J. Clinical evaluation of the root tear of the posterior horn of the medial meniscus in total knee arthroplasty for osteoarthritis. Knee Surg Relat Res. 2015;27:90–94. doi: 10.5792/ksrr.2015.27.2.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hussain Z.B., Chahla J., Mandelbaum B.R., Gomoll A.H., LaPrade R.F. The role of meniscal tears in spontaneous osteonecrosis of the knee: A systematic review of suspected etiology and a call to revisit nomenclature. Am J Sports Med. 2019;47:501–507. doi: 10.1177/0363546517743734. [DOI] [PubMed] [Google Scholar]
- 12.Krych A.J., Johnson N.R., Mohan R. Arthritis progression on serial MRIs following diagnosis of medial meniscal posterior horn root tear. J Knee Surg. 2018;31:698–704. doi: 10.1055/s-0037-1607038. [DOI] [PubMed] [Google Scholar]
- 13.Choi C.J., Choi Y.J., Lee J.J., Choi C.H. Magnetic resonance imaging evidence of meniscal extrusion in medial meniscus posterior root tear. Arthroscopy. 2010;26:1602–1606. doi: 10.1016/j.arthro.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 14.Guermazi A., Hayashi D., Jarraya M. Medial posterior meniscal root tears are associated with development or worsening of medial tibiofemoral cartilage damage: The multicenter osteoarthritis study. Radiology. 2013;268:814–821. doi: 10.1148/radiol.13122544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee S.S., Ahn J.H., Kim J.H., Kyung B.S., Wang J.H. Evaluation of healing after medial meniscal root repair using second-look arthroscopy, clinical, and radiological criteria. Am J Sports Med. 2018;46:2661–2668. doi: 10.1177/0363546518788064. [DOI] [PubMed] [Google Scholar]
- 16.Kodama Y, Furumatsu T, Masuda S, et al. Transtibial fixation for medial meniscus posterior root tear reduces posterior extrusion and physiological translation of the medial meniscus in middle-aged and elderly patients [published online November 28, 2019]. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-019-05810-x. [DOI] [PubMed]
- 17.Krych A.J., Johnson N.R., Mohan R., Dahm D.L., Levy B.A., Stuart M.J. Partial meniscectomy provides no benefit for symptomatic degenerative medial meniscus posterior root tears. Knee Surg Sports Traumatol Arthrosc. 2017;26:1117–1122. doi: 10.1007/s00167-017-4454-5. [DOI] [PubMed] [Google Scholar]
- 18.Jiang E.X., Abouljoud M.M., Everhart J.S. Clinical factors associated with successful meniscal root repairs: A systematic review. Knee. 2019;26:285–291. doi: 10.1016/j.knee.2019.01.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
We create a lateral access of approximately 6 cm in length, identify the iliotibial tract, and section it at its posterior third; below the iliotibial band, we identified the lateral collateral ligament. We also identify the fibular head and femoral biceps. We perform digital dissection between the posterior surface of the lateral femoral condyle and the head of the lateral gastrocnemius. During arthroscopic visualization, we identify the posterior root lesion of the lateral meniscus. We prepare the Arthrex MU (multiuse) guide with the 6-mm FlipCutter drill. We realize an anterolateral approach to the proximal tibia to make the transtibial tunnel for root reinsertion. We position the MU guide on the footprint of the posterior root of the lateral meniscus. After making sure that the drill is in the correct position, we horizontalize the tip of the FlipCutter drill and make a 10-mm-deep tunnel. We then pass an inverted needled guidewire as a transport wire and pull a loop of this wire to the anterolateral portal. We identify the popliteal tendon and introduce the Meniscus 4 A-II device posterior and proximal to the popliteal tendon, extending into the proximal side of the lateral meniscus. Using tweezers, we grasp the posterior horn of the lateral meniscus and pierce it. Again using tweezers, we pull a handle out of the joint through the anterolateral portal. With the same tweezers, we pull both ends of the FiberWire out of the anterolateral portal. We then make a stitch by passing the 2 ends of the wire through a new loop formed at the end of the loop and pulling the 2 ends, causing the tip to run to the posterior horn of the lateral meniscus. We repeated the same step by passing the meniscal suture device again through the posterior horn of the lateral meniscus. We pull the handle out of the joint through the anterolateral portal. We also pull into the anterolateral portal the 2 ends of the same wire out of the posterolateral approach, making the same point described above. Care must be taken to prevent the previous suture from becoming caught in the new stitch; if this occurs, we remove the wires from the previous stitch from inside the new suture. Then, we pull all the wires simultaneously out of the transpatellar portal to avoid catching any wires in the joint capsule. After this last step, we pass the free ends of the wires through the preformed loop to be transported to the tibial tunnel. Holding them inside the joint makes it easier for them to slide into the tibial tunnel. We pull the 4 wires together, observing the lateral meniscal root reinsertion, and finally fix the wires with a button or post screw.