Abstract
Despite profound advancements in arthroscopic rotator cuff repair (RCR) techniques, radiologic failure rates may be in excess of 60% with repairs of large and massive tears in the elderly population. One of the strategies to improve these healing rates has been “patch” augmentation of the cuff repair. At the same time, superior capsular reconstruction (SCR) has gained significant popularity as an option for irreparable rotator cuff (RC) tears. Some have also advocated performing SCR in addition to arthroscopic RCR to reinforce the repair and improve healing rates. Techniques involving the use of fascia lata, ECM patches, and long head of the biceps (LHB) for SCR to reinforce the cuff repair have all been elegantly described. In this article, we propose a technique that enables a combination of the aforementioned procedures and involves performing RCR with patch augmentation, as well as SCR using LHB. In doing so, the repaired RC is bordered by the patch over its bursal surface and the LHB on the articular surface (functioning as the superior capsule), thus giving us the name “Hamburger technique” (a 3-layered construct).
Despite profound advancements in arthroscopic rotator cuff repair (RCR) techniques, radiologic failure rates may be in excess of 60% with repairs of large and massive tears in the elderly population.1 One of the strategies to improve these healing rates has been “patch” augmentation of the cuff repair.2 At the same time, superior capsular reconstruction (SCR) has gained significant popularity as an option for irreparable rotator cuff (RC) tears.3 The original technique, as described by Mihata et al.,4 involves using fascia lata. However, in the Western world, the technique has been modified to use extracellular matrix (ECM) patch grafts as an alternative,3 whereas others have explored the use of long head of the biceps (LHB) as a “biological” SCR.”5 There are also a few authors who have advocated performing SCR in addition to arthroscopic RCR to reinforce the repair and improve healing rates.4 Techniques involving using fascia lata, ECM patches, and LHBs for SCR to reinforce the cuff repair have all been elegantly described.4,6,7
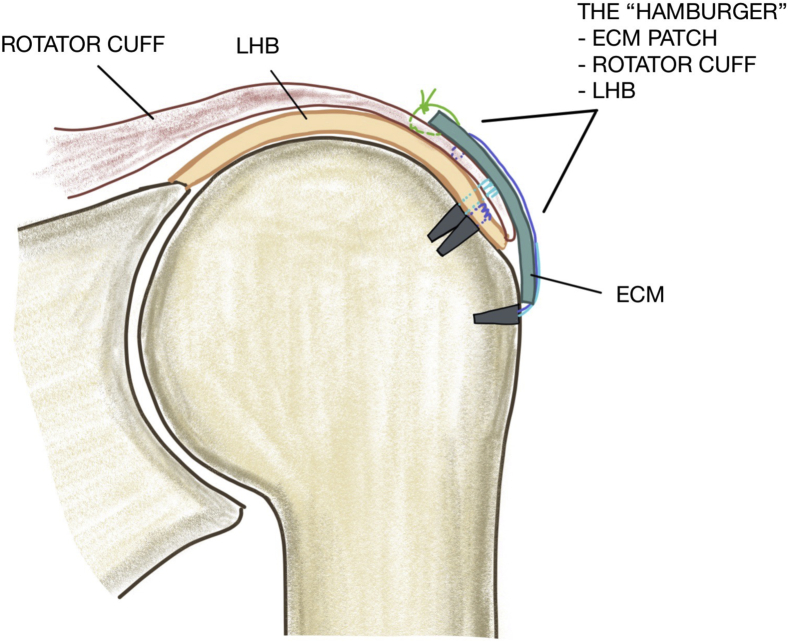
In this article, we propose a technique that enables a combination of the aforementioned procedures and involves performing RCR with patch augmentation, as well as SCR using LHB. In doing so, the repaired RC is bordered by the patch over its bursal surface and the LHB on the articular surface (functioning as the superior capsule), thus giving us the name “Hamburger Technique” (a 3-layered construct) (Tables 1 and 2).
Table 1.
Key Points
|
|
|
LHB, head of the biceps; SCR, superior capsular reconstruction.
Table 2.
Indication and Contraindications
| Indications | Contraindications |
|---|---|
|
|
Surgical Technique (With Video Illustration)
The procedure is performed with the patient under general anaesthesia combined with interscalene block, with the patient positioned in either the beach chair or lateral decubitus position (Table 3). The arthroscope is introduced through a standard posterior viewing portal and a diagnostic arthroscopy is performed initially. Careful attention is paid to whether LHB is present and the state of the tendon (Fig 1). If LHB is absent or significantly damaged, then it cannot be used for SCR. Similarly, the RC tear is carefully assessed for size and degree of retraction to determine whether it is possible to repair it without excessive tension. This technique is only applicable to repairable tears, as we only to use the patch to augment the RC rather than to bridge a gap.
Table 3.
Surgical Steps
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
ACJ, acromioclavicular joint; LHB, head of the biceps; PDS, polydioxanone.
Fig 1.
Cuff tear and prepared footprint. Diagram is of right shoulder.
The arthroscope is then introduced into the subacromial space through the posterior port. Through a standard lateral port, the tear is identified and both bursectomy and acromioplasty performed. If there is acromioclavicular joint tenderness, then the acromioclavicular joint is excised at this point. If a tear of subscapularis is found then this is also repaired.
Superior Capsule Reconstruction With LHB: Layer 1
Via a similar method to SCR with ECM, the distance between the superior glenoid attachment of the LHB and the greater tuberosity (GT) footprint is measured.3 The GT footprint is then prepared. Two free sutures (#2 FiberWire; Arthrex, Naples, FL) are passed through the LHB tendon in a “ratchet loop” manner, at a distance from its insertion equal to the distance measured previously (from the superior glenoid attachment to the GT footprint) (Fig 2). For instance, if the distance between the LHB insertion and GT footprint is 4.5 cm, the 2 free sutures should be passed through LHB at 4.5 cm from its insertion (with a 0.5-cm gap between the 2 sutures). Following this, an LHB tenotomy is performed approximately 1 cm distal to where the free sutures are passed.
Fig 2.
Suture passed through tenotomized LHB stump. The arthroscope is in the standard posterior port of the right shoulder with the patient in the lateral position, but the arthroscope is rotated so the images appear as though the patient is in the beach chair position. (LHB, long head of the biceps.)
The 4 suture limbs of these free sutures are then passed through a standard lateral row anchor (SwiveLock 5.5 SP BCP; Arthrex), which in turn is inserted into the GT footprint. This secures the LHB to the footprint and completes the SCR using the LHB (Fig 3). This forms “layer 1.”
Fig 3.
LHB secured to footprint. The arthroscope is in the standard posterior port of the right shoulder with the patient in the lateral position, but the arthroscope is rotated so the images appear as though the patient is in the beach chair position. (ECM, extracellular matrix; LHB, head of the biceps.)
Supraspinatus Repair With Augmentation: Layers 2 and 3
Following SCR with LHB, the supraspinatus tendon is repaired using patch augmentation via the “pull-over” technique, as previously described.8 This forms “layer 2” and “layer 3.”
Layer 2
This technique consists of a standard medial row repair of the tendon tear using either 1 or 2 medial row anchors. This involves mobilization of the tendon, insertion of the medial row anchors, and passage of the anchor suture limbs through the tendon using a standard suture passer device (Scorpion device; Arthrex) (Fig 4, Video 1). If bone quality is sufficient, we prefer to use all-suture anchors for the medial row (Iconix 2.3; Stryker, Kalamazoo, MI). We prepare the footprint by stimulating the marrow with a 1.4 drill, using multiple drill holes to disrupt the cortex. The “pull-over” technique also involves passing a free suture (#2 FiberWire) through the medial aspect of the tendon and bringing this out through the Neviaser port.8 This free suture is used to help “pull over” the augment into the subacromial bursa and secure it medially.
Fig 4.
Standard medial row repair of the tendon tear using either 1 or 2 medial row anchors. The arthroscope is in the standard posterior port of the right shoulder with the patient in the lateral position, but the arthroscope is rotated so the images appear as though the patient is in the beach chair position.
Following passage of all anchor suture limbs through the torn tendon, knots are tied to secure the medial row repair. However, it is important that no knots are tied in the free FiberWire suture. The distance between the most anterior and the most posterior knots is then measured and the suture limbs belonging to these knots left intact and long, whereas the other suture limbs are cut flush to the knot.
Layer 3
Preparation of Augment Outside the Patient
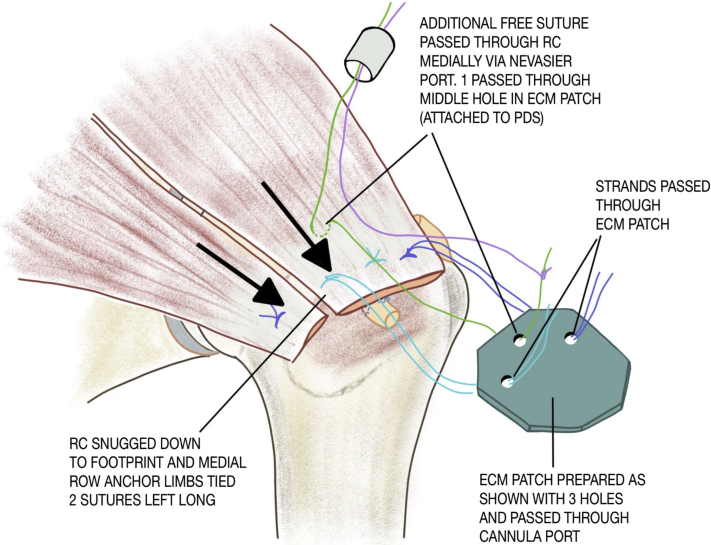
As has previously been described in depth,8 the patch (Arthrex Dx Reinforcement Matrix; Arthrex) is then prepared outside the body by making 2 holes in the augment, through which the anchor suture limbs are passed, and a third hole more medially (approximately 5 mm from the medial edge of the patch and in between the other 2 holes) (Fig 5). In addition, the corners of the rectangular patch are cut to leave an octagon (Fig 5).
Fig 5.
Patch preparation and suture passage into the patch. The patch is prepared outside the body by making2holes in the augment, through which the anchor suture limbs are passed, and a third hole more medially (approximately 5 mm from the medial edge of the patch and in between the other 2 holes). In addition, the corners of the rectangular patch are cut in order to leave an octagon.
Suture Management
One limb of the free FiberWire is passed through the medial hole of the patch using a polydioxanone suture as a shuttle, while the anchor is passed through the 2 anterior and posterior holes (more lateral) of the patch as previously described in the “pull-over” technique (Fig 5).8
Insertion of the Patch
The rolled-over patch is then maneuvered into the subacromial bursa through a size 10 cannula (Passport; Arthrex) in the lateral port. The medial free suture is used to pull the patch over inside the subacromial space (Video 1). Once inside the patch is laid open and flat using a blunt obturator (Video 1).
Medial Stabilization of the Patch
The medial edge of the patch is affixed to the medial aspect of the cuff by tying the 2 limbs of the free FiberWire suture with arthroscopic knots through the Neviaser port.
Lateral Stabilization of the Patch
This is achieved by a transosseous equivalent technique incorporating the augment into the construct. Two lateral row anchors (SwiveLock 5.5 SP; Arthrex) are inserted (laterally), one anterior and one posterior, securing the augments while the medial row anchor sutures are tensioned simultaneously (Video 1). Often, we also pass the internal suture of the lateral row anchors into the patch for additional fixation of the lateral edge (Figs 6 and 7).
Fig 6.
ECM patch secured over rotator cuff repair. The medial edge of the patch is secured to the medial aspect of the cuff by tying the 2 limbs of the free FiberWire suture with arthroscopic knots through the Neviaser port. Lateral stabilization of the patch is achieved by a transosseous equivalent technique incorporating the augment into the construct. Two lateral row anchors (are inserted (laterally), one anterior and one posterior, thus securing the augment. The arthroscope is in the standard posterior port of the right shoulder with the patient in the lateral position, but the arthroscope is rotated so the images appear as though the patient is in the beach chair position. (ECM, extracellular matrix.)
Fig 7.
Hamburger construct with ECM patch on top, RC repair in middle and LBH tendon underneath. Diagram is of right shoulder. (ECM, extracellular matrix; LHB, head of the biceps; RC, rotator cuff.)
Rehabilitation Program
Shoulders were immobilized in a shoulder abduction wedge at the end of the procedure and patients were instructed to wear this for 6 weeks. Physiotherapy as per large-massive rotator cuff repair protocols was organized before discharge. This consists of early pendulum exercises, passive flexion and external rotation to 0° at 4 weeks, and then at 6 weeks progressive exercises starting from passive to active and finally strengthening exercises.
Discussion
Despite significant advances in arthroscopic RC surgery, which have led to good clinical outcomes, retear rates may be in excess of 60% for elderly patients who undergo large or massive cuff repairs.1 There is convincing evidence to suggest that patients with healed RCRs achieve a better clinical outcome than those with retears.9 These compromised healing rates have led to an ongoing drive to develop new techniques that may enhance healing rates.2
One avenue that has been explored is the use of a range of patches to augment the repaired RC tendon.3 Improved processing of biological tissues (ECM) has allowed better removal of antigenic material from the matrix, as well as reduced risk of immune and inflammatory response. This has resulted in a resurgence of biological material as a popular choice for RCR with patch augmentation.2 Moreover, enhanced arthroscopic instrumentation has simplified the arthroscopic technique for RCR with patch augmentation.8
Available patches range from those with cellular components (either allogenic or autogenic) to ECM (xenograft, allograft) and synthetic materials.10 The renewed interest in patches has led to a number of histologic, biomechanical, clinical, and radiologic studies. These in turn have shown promising results, which suggest that the improved patches may result in a stronger construct with superior outcomes.11 However, at present the number of well-constructed randomized controlled trials is limited, and so it remains open to debate whether healing rates are better when compared with standard RCRs.12
In recent years, the role of the superior capsule in providing superior stability of the glenohumeral joint has gained greater appreciation.8 Some authors have even suggested that the defect in the superior capsule may be the “essential lesion” in patients with superior cuff tear, as opposed to the tear in the RC itself and that RCRs that do not involve restoration of normal superior capsular anatomy may result in suboptimal outcomes.12 This comes at a time when reconstruction of the superior capsule has become a fashionable alternative for irreparable RC tears, since the description of this technique by Mihata et al.4 In the Western world, this technique has been adapted to using ECM patches in place of fascia lata.4 Although not all reports on healing rates have matched those of Mihata et al., the short-term clinical outcomes have been promising.3,4
Due to poor healing rates of massive and large RCRs, good short-term clinical outcomes of SCR and greater understanding of the importance of the superior capsule, a number of authors have developed techniques that involve SCR in addition to cuff repair in the presence of large repairable tears.13 In a level 3 cohort study, Mihata et al.4,13 compared clinical and radiologic outcomes of 34 patients who underwent SCR (with fascia lata) and RCR to 91 patients who underwent arthroscopic RCR alone. There were no retears in the group with SCR and RCR, compared with a retear incidence of 4% in the group with RCR only. Functional outcomes were similar between the 2 groups. Other investigators have explored the possibility of using the LHB to reconstruct the superior capsule (for irreparable tears), instead of fascia lata or ECM, or to augment the repaired rotator cuff (in repairable tears).14 The proposed advantages of using LHB for the superior capsule or augment are that it is an autograft (and therefore does not provoke an immune response or donor-site complications), it is cheaper than ECM patches, it remains attached to glenoid so maintains some of its vasculature, and finally it is relatively easy to perform.14 There are also a number of biomechanical studies that have demonstrated the ability of LHB to function as the superior capsule.6,7 Furthermore, the biceps tendon can be used for SCR in addition to RCR to protect the repair.5,15
In this report, we have described a technique that combines the aforementioned methods with the aim of optimizing both clinical/radiologic outcomes and healing rates. We agree with previous authors that the superior capsule may play an important role in providing enhanced superior stability for RCRs.4 As a result, its reconstruction during arthroscopic RCR (in addition to the repair itself) may lead to improved outcomes. Similarly, we feel that patch augmentation with ECM in addition to RCR may improve healing rates by inducing native tissue growth and providing further biomechanical support.2 The patch may provide a degree of load sharing across the repaired tendon, resulting in reduced loading at the repair site. This may help to protect the construct during the vital period required for healing of the repair. Indeed, there are a number of biomechanical studies that provide evidence for improved “load to failure” and initial repair strength, as well as reduced bone-tendon gapping with augmented rotator cuff repairs.2
The technique described here unites these philosophies with the aim of fully optimizing the healing environment for the repaired RC tendon. The tendon is reinforced both on its articular and bursal side in a 3-layered construct (hence the name “Hamburger Technique”). On its articular side, it is reinforced by reconstruction of the superior capsule using the LHB and on its bursal side by the ECM patch. This may represent a “belt and braces” method, with the aim of decreasing retear rates, improving healing, and better restoring clinical function. Whether this technique achieves these aims or not can only be determined by future comparative studies.
There are a number of potential issues with this method. The technique requires the presence of a reasonably healthy LHB. If the LHB is absent or significantly damaged, then it cannot be used to reconstruct the superior capsule. Similarly, in the presence of a pathologic LHB, failure to perform a tenotomy or tenodesis during the cuff repair may leave a potential source of pain. The technique, however, does involve a more distal tenotomy and a “re-routing” of the residual LHB, and therefore may reduce the risk that the LHB will continue to generate discomfort. In addition, as with other procedures that involve ECM, there is a risk of inflammatory response, stiffness, adhesions, and infection (Tables 4 and 5). We feel that these risks are minimized with modern processing techniques, which provide enhanced antigenic material removal (more than 90% DNA removal). In our series of RCR with patch augmentation, we have not yet encountered any cases of infection or excessive inflammatory response. It is important to note, though, that we do not feel that patch augmentation should be performed in patients who have a history of shoulder infection.
Table 4.
Advantages and Risks
| Advantages | Risks |
|---|---|
|
|
ECM, extracellular matrix.
Table 5.
Pearls and Pitfalls
| Ensure biceps tendon harvested at least 1 cm longer than desired length. |
| Use arthroscopic measurement tool. |
| Extensive release of rotator cuff. |
| Secure biceps tendon tightly on humeral head. |
In summary, this report describes a 3-layered “belt and braces” technique for arthroscopic rotator cuff repair with the aim of optimizing and enhancing healing rates and clinical outcomes. The 3 layers of the “Hamburger technique” consist of the repaired RC tendon itself, the LHB functioning as superior capsule on its articular surface, and the ECM patch as the augment on its bursal surface. As with patch augmentation RCR and SCR, well-constructed comparative studies will be needed to evaluate whether this technique is able to deliver its aim.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: A.A.N. is an educational consultant for Stryker, and receives research support from Arthrex. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
“Hamburger technique” technique for rotator cuff repair with augmentation and biological SCR. The arthroscope is looking at the subacromial space via a standard posterior port of the right shoulder with the patient in the lateral position, but the arthroscope is rotated so the images appear as though the patient is in the beach chair position. (SCR, superior capsular reconstruction.)
References
- 1.Narvani A.A., Imam M.A., Godenèche A., Calvo E., Corbett S., Wallace A.L., Itoi E. Degenerative rotator cuff tear, repair or not repair? A review of current evidence. Ann R Coll Surg Engl. 2020;102:248–255. doi: 10.1308/rcsann.2019.0173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Consigliere P., Polyzois I., Sarkhel T., Gupta R., Levy O., Narvani A.A. Preliminary results of a consecutive series of large & massive rotator cuff tears treated with arthroscopic rotator cuff repairs augmented with extracellular matrix. Arch Bone Joint Surg. 2017;5:14–21. [PMC free article] [PubMed] [Google Scholar]
- 3.Dimock R., Malik S., Consigliere P., Imam M., Narvani A.A. superior capsule reconstruction: What do we know? Arch Bone Joint Surg. 2019;7:3–11. [PMC free article] [PubMed] [Google Scholar]
- 4.Mihata T., Lee T.Q., Watanabe C. Clinical results of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthroscopy. 2013;29:459–470. doi: 10.1016/j.arthro.2012.10.022. [DOI] [PubMed] [Google Scholar]
- 5.Kim Y.S., Lee H.J., Park I. Arthroscopic in situ superior capsular reconstruction using the long head of the biceps tendon. Arthrosc Tech. 2018;7:e97–e103. doi: 10.1016/j.eats.2017.08.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen R.E., Soin S.P., El-Shaar R. Reconstruction of the superior glenoid labrum with biceps tendon autograft: A cadaveric biomechanical study. Arthroscopy. 2019;35:353–358. doi: 10.1016/j.arthro.2018.08.049. [DOI] [PubMed] [Google Scholar]
- 7.Han F., Kong C.H., Hasan M.Y. Superior capsular reconstruction for irreparable supraspinatus tendon tears using the long head of biceps: A biomechanical study on cadavers. Orthop Traumatol Surg Res. 2019;105:257–263. doi: 10.1016/j.otsr.2018.10.023. [DOI] [PubMed] [Google Scholar]
- 8.Narvani A.A., Consigliere P., Polyzois I., Sarkhel T., Gupta R., Levy O. The “pull-over” technique for arthroscopic superior capsular reconstruction. Arthrosc Tech. 2017;6:e679–e687. doi: 10.1016/j.eats.2016.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Park J.G., Cho N.S., Song J.H. Rotator cuff repair in patients over 75 years of age: Clinical outcome and repair integrity. Clin Orthop Surg. 2016;8:420–427. doi: 10.4055/cios.2016.8.4.420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen F.M., Liu X. Advancing biomaterials of human origin for tissue engineering. Prog Polym Sci. 2016;53:86–168. doi: 10.1016/j.progpolymsci.2015.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lorbach O., Baums M.H., Kostuj T. Advances in biology and mechanics of rotator cuff repair. Knee Surg Sports Traumatol Arthrosc. 2015;23:530–541. doi: 10.1007/s00167-014-3487-2. [DOI] [PubMed] [Google Scholar]
- 12.Adams C.R., De Martino A.M., Rego G. The rotator cuff and the superior capsule: Why we need both. Arthroscopy. 2016;32:2628–2637. doi: 10.1016/j.arthro.2016.08.011. [DOI] [PubMed] [Google Scholar]
- 13.Mihata T., Lee T.Q., Hasegawa A. Superior capsule reconstruction for reinforcement of arthroscopic rotator cuff repair improves cuff integrity. Am J Sports Med. 2019;47:379–388. doi: 10.1177/0363546518816689. [DOI] [PubMed] [Google Scholar]
- 14.Veen E.J.D., Stevens M., Diercks R.L. Biceps autograft augmentation for rotator cuff repair: A systematic review. Arthroscopy. 2018;34:1297–1305. doi: 10.1016/j.arthro.2017.10.044. [DOI] [PubMed] [Google Scholar]
- 15.Milano G. Editorial Commentary: Is the biceps tendon a valid option for augmentation in rotator cuff repair? Future perspectives on superior capsule reconstruction. Arthroscopy. 2018;34:1306–1307. doi: 10.1016/j.arthro.2018.02.025. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
“Hamburger technique” technique for rotator cuff repair with augmentation and biological SCR. The arthroscope is looking at the subacromial space via a standard posterior port of the right shoulder with the patient in the lateral position, but the arthroscope is rotated so the images appear as though the patient is in the beach chair position. (SCR, superior capsular reconstruction.)