Abstract
The experiences of these recent months have left us with as many new questions as they have given us new solutions. The main question that infection prevention and control department is having these days is “Why have hospital-associated infections (HAIs) reduced during COVID-19 pandemic?” What is the one unique strategy that has brought decline in increasing HAIs? Would it be appropriate to say that rigorous hand hygiene practices among health care workers (HCWs) have reduced HAIs in a tertiary care hospital of Pakistan? This commentary is written to understand the effect of rigorous hand hygiene among HCWs on number of HAIs during COVID-19 pandemic. Given the seriousness of this outbreak, it was observed that the hand hygiene has occupied a new place of importance in the minds of HCWs. We observed 4 times increase in the consumption of hand sanitizers after COVID-19 outbreak. The increased consumption of hand sanitizers was reflected in improved hand hygiene practices. A reduction was observed in the number of HAIs after the COVID-19 outbreak, and we assume that the dip in HAIs is associated with the improvement in hand hygiene practices in the recent months. In the wake of COVID-19 pandemic, these trends reassure us that hand hygiene compliance by HCWs alone can be effective in reducing HAIs in a hospital setting.
Keywords: hand hygiene compliance, hospital-associated infections (HAIs), COVID-19
Hand hygiene, that is, hand washing with soap and water and/or the use of alcohol-based hand sanitizers, is widely accepted as the cornerstone of infection control in a hospital setting.1 The concept of hand hygiene is prevalent since the mid-1800s when it was first introduced by Ignaz P. Semmelweis.2 The World Health Organization (WHO), the Centers for Disease Control and Prevention (CDC), and The Joint Commission have issued hand hygiene guidelines for health care workers (HCWs) to prevent hospital-associated infections (HAIs).3,4 Several multicenter trials have reported that all new strategies developed by top world scientists to reduce HAI can be easily nullified if HCWs fail to maintain hand hygiene in a hospital setting.2,4 Unfortunately, several studies have shown that adherence to hand hygiene guidelines remains low and that improvement efforts often lack sustainability.1 One potential reason for low compliance to hand hygiene is that HCWs fail to realize that they are carrying organisms in their hands because pathogens are not visible. Another possible reason for noncompliance to hand hygiene is that the HCWs are unable to associate their contact with patient when pathogen is perhaps transmitted from HCWs’ contaminated hands. Another possible reason that leads to noncompliant behavior toward hand hygiene is that HCWs are less likely to get HAIs. Also, the lack of compliance for hand hygiene is related to the cost of time for HCWs, and unavailability of hand rub dispensers.2,5
The high rates of HAIs, including multidrug-resistant organism (MDROs), central line-associated bloodstream infection (CLABSI), catheter-associated urinary tract infection (CAUTI), and ventilator-associated pneumonia (VAP), are frequently viewed as signifying poor compliance to hand hygiene guidelines.3 HAIs are a major challenge to the health care system and are associated with significant mortality, morbidity, and an economic burden. The CDC reports HAIs as the most common adverse hospital-related event affecting one in 25 patients during their hospital stays and resulting in more than 99 000 deaths per year.3 In the recent few months, when the new strain of coronavirus (COVID-19) outbreak was observed around the world; several structural and behavioral changes were made to the hospitals around the globe to ensure infection prevention. These changes include stricter visitation policies, new sanitation guidelines, development of negative pressure isolation rooms, PPE (personal protection equipment) usage for caregivers and HCWs, and so on.6 The COVID-19 pandemic has presented significant uncertainty into the hospital environment and thus workflow, including timing of essential medical procedures, foreseeing and managing patient inflows, and swiftly evolving guidelines on patient management.1
HCWs are at the front line of COVID-19 outbreak, and their constant exposure to infected patients and contaminated surfaces can put them at risk for acquiring and transmitting the infection. One of the most frequently reported strategies that has been implemented in hospitals is frequent washing of hands and hand rub by HCWs. WHO recommends that
HCWs should perform hand hygiene using the proper technique and known as “My 5 moments for hand hygiene,” that is, before touching a patient, before clean/aseptic procedure, after procedure/body fluid exposure, after touching a patient, and after touching a patient’s surroundings. In particular, before putting on PPE and after removing it, when changing gloves, after any contact with a patient with suspected or confirmed COVID-19 virus, their waste, or the environment in the patients’ immediate surroundings, after contact with any respiratory secretions, before food preparation and eating, and after using the toilet.7
During this crisis, hand hygiene, along with other infection control activities, has received much attention, not only because it is a priority but also because HCWs are more concerned about their own exposure to COVID-19. Prior to the COVID-19 pandemic, hand hygiene was something hospitals struggled with. The research shows a 50% compliance rate for hand hygiene, on average, among hospital care staff. But now that everyone is hyper-aware, the rates of hand hygiene have generally gone up. In addition, HCWs are scared about carrying virus back to their homes where they have their newborn, young children, and elderly family members who are at more risk.5
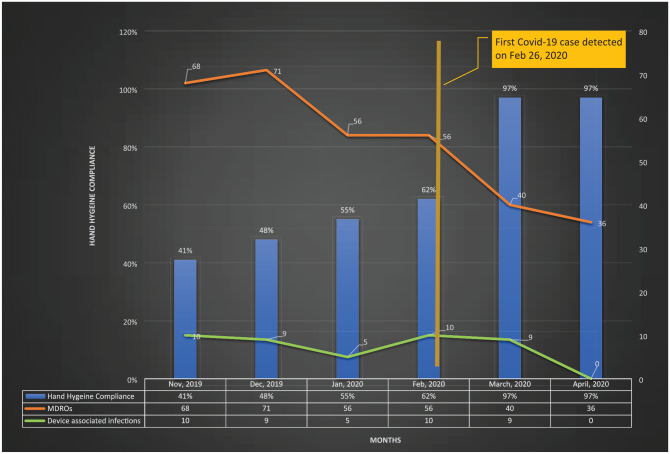
Here we share one example of a private tertiary care hospital in Karachi, Pakistan where we have recently observed that an increase in hand hygiene was associated with the reduction in HAIs. The past experience suggests that the HCWs adherence to hand hygiene practices remains between 80% and 95%, when they are being directly monitored by infection preventionists during audit rounds. In instances when hand hygiene practices are observed covertly through secret shoppers, the average hand hygiene practices remained between 30% and 50%. This suggests that the observation bias, also known as the Hawthorne effect, plays a critical role in evaluating hand hygiene compliance. The Hawthorne effect alters HCWs’ usual behavior and often leads to overestimation of hand hygiene compliance. The low hand hygiene compliance levels have always been a disquieting challenge despite the numerous interventions and campaigns performed in promoting this action. We believe that due to low hand hygiene compliance, the number of HAIs in the tertiary care hospital are on rise for past several years (see Figure 1). This is in spite of the implementation of several interventions, including point of care availability of hand sanitizers at patient bedside, introduction of chlorhexidine wipes, simulated trainings on central line insertion and maintenance including scrub the hub, simulated environmental cleaning for housekeeping staff, and introduction of bundles to decrease HAIs (VAP, CAUTI, CLABSI, MDROs).
Figure 1.
Trends of hospital-associated infections and hand hygiene compliance before and after COVID-19 outbreak.
During the COVID-19 crisis, we observed a sudden increase in the demand of hand sanitizers by HCWs. The data show that there has been 4 times increase in the consumption of hand sanitizers in March and April 2020 (Figure 2). At the same time, the hand hygiene routine audits by infection preventionists and covert observations through secret shoppers, both showed more than 90% compliance to hand hygiene practices. The hand hygiene compliance rates have been validated through direct observations, spot checks, and camera records on weekdays and weekend rounds. Given the seriousness of this outbreak, it was observed that the hand hygiene has occupied a new place of importance in the minds of HCWs. Not only the direct HCWs but the indirect HCWs also improved their compliance without any external reinforcement.
Figure 2.
Sanitizer consumption bottles from October 2019 till April 2020.
With the same intervention, that is, “My 5 Moments for Hand Hygiene” (before touching a patient, before clean/aseptic procedures, after body fluid exposure/risk, after touching a patient, and after touching patient surroundings), we observed a reduction in the number of HAIs in March and April 2020 and we assume that the dip in HAIs is associated with the improvement in hand hygiene practices in the recent months (see Figure 1). The improvement in hand hygiene practices was first observed in the last week of February 2020, when the first case of COVID-19 was detected in Pakistan. As the hand hygiene compliance improved, so the decrease was observed in the number of HAIs, including MDROs and device-associated infections. In the initial 3 weeks of outbreak, the hand hygiene compliance remained around 97% and the number of HAIs reported in these 3 weeks were 19, 12, and 9 respectively. A similar trend was observed in the later weeks, where a smaller number of HAIs were reported with hand hygiene compliance of 97%. In the last week of April 2020, only 4 HAIs were reported with the hand hygiene compliance of 97%; this shows that increasing hand hygiene compliance has an effect on reducing the number of HAIs. We hope to observe a similar association between hand hygiene compliance and number of HAIs in the coming months. Both device-associated infections and MDROs were decreased with the improvement in hand hygiene practices (Figure 1).
Before the COVID-19 outbreak, hospital data show that there was a high prevalence of device associated infections (CAUTI, CLABSI, and VAP) and MDROs in critical care areas including cardiac care unit (CCU), neonatal intensive care unit (NICU), pediatric intensive care unit (PICU), surgical intensive care unit (SICU), and medical intensive care unit (MICU). After the COVID-19 outbreak, the ward-wise data of HAIs show that the number of HAIs reduced in these critical care areas. For example, in NICU, the number of device days remained same throughout the period; however, there were significant decline in number of HAIs. We assume that the reduction in HAIs is mainly due to improved hand hygiene compliance by HCWs.
As stated above, the number of HAIs have not declined in past several years despite implementation of costly interventions. It is assumed that the observed dip in the HAIs may be due to the increasing compliance to hand hygiene practices amid the COVID-19 pandemic. Several decades ago, hand hygiene was declared as one of the most effective, simple, and low-cost procedures against HAIs, if practiced appropriately. In the wake of the COVID-19 pandemic, these trends reassure that hand hygiene compliance by HCWs alone can be effective in reducing HAIs in a hospital setting.
One of the limitations of these findings is that there was a decrease in both the planned and unplanned hospital admissions during COVID-19 outbreak and this may have affected the incidence and prevalence of HAIs. Mainly, the patient admission rates dropped in surgical department because most patients were delaying nonurgent procedure to prevent their exposure to COVID-19. The patient admissions remained more or less similar in other hospital departments, including women and child health, medicine, obstetrics and gynecology, oncology, family medicine, internal medicine, and others.
Future research should be directed to assess the potential impact of several unexamined factors that could influence hand hygiene compliance among HCWs. Also, it would be interesting to study that how previous pandemic and epidemics have influenced practices of HCWs. More important, randomized controlled trials, before and after study design and other rigorous evaluation techniques could be used to see the long-term effect of hand hygiene practices on HAIs.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Anam Shahil Feroz  https://orcid.org/0000-0003-0180-0213
https://orcid.org/0000-0003-0180-0213
References
- 1. Lotfinejad N, Peters A, Pittet D. Hand hygiene and the novel coronavirus pandemic: the role of healthcare workers. J Hosp Infect. [published online March 19, 2020]. doi: 10.1016/j.jhin.2020.03.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Shafer E. Infection prevention in hospitals: the importance of hand hygiene. Infect Dis News. 2014;27(6):1 Accessed July 4, 2020 https://www.healio.com/news/infectious-disease/20140422/10_3928_1081_597x_20140101_00_1340650 [Google Scholar]
- 3. Center for Disease Control and Prevention. Types of healthcare-associated infections. Accessed May 18, 2020 https://www.cdc.gov/hai/infectiontypes.html
- 4. World Health Organization. Evidence for hand hygiene guidelines. Accessed on May 18, 2020 https://www.who.int/gpsc/tools/faqs/evidence_hand_hygiene/en/
- 5. Binder L, Millenson ML. In a pandemic, hospital staffers need to get better at hand-washing. Published March 25, 2020. Accessed on May 18, 2020 https://www.statnews.com/2020/03/25/pandemic-hospitals-more-handwashing/
- 6. Bowdle A, Munoz-Price LS. Preventing infection of patients and healthcare workers should be the new normal in the era of novel coronavirus epidemics. Anesthesiology. 2020;132:1292-1295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. World Health Organization. Recommendation to Member States to improve hand hygiene practices widely to help prevent the transmission of the COVID-19. Accessed May 18, 2020 https://www.who.int/docs/default-source/inaugural-who-partners-forum/who-interim-recommendation-on-obligatory-hand-hygiene-against-transmission-of-covid-19.pdf