Abstract
Trigger finger is a common condition usually curable by a safe, simple corticosteroid injection. Trigger finger results from a stenotic A1 pulley that has lost its gliding surface producing friction and nodular change in the tendon. This results in pain and tenderness to palpation of the A1 pulley, progressing to catching and then locking. Splinting for 6 to 9 weeks produces gradual improvement in most patients as does a quick steroid injection with the latter resulting in resolution of pain in days and resolution of catching or locking in a few weeks. Percutaneous or open release should be reserved for injection failures particularly those at high risk for continued injection failure including diabetics and those with multiple trigger fingers. We present a step-by-step method for injection with illustrations to encourage primary care providers to offer this easily performed procedure to their patients.
Keywords: trigger finger, trigger thumb, stenosing tenosynovitis, stenosing flexor tenosynovitis, steroid injection, corticosteroid injection
Introduction
Trigger finger and trigger thumb (TF to denote all digits), or stenosing flexor tenosynovitis, is a common cause of pain and disability characterized by painful clicking or locking of a finger or thumb. We searched PubMed for relevant English language articles using the terms “trigger finger” and “stenosing tenosynovitis,” and further focused our search using the terms “steroid injection” and “corticosteroid injection.” We then identified additional articles to read from the references cited by these articles.
TF has an annual incidence of 28 cases per 100 000 and a lifetime prevalence of 2.6% in the general population, peaking among adults in their 50s and 60s.1-3 Diabetics have an increased lifetime prevalence of 5% to 10%.4-6 TF may also be seen in association with carpal tunnel syndrome, Duputryen’s disease, and inflammatory arthritis.7-9 Multiple digits can simultaneously be involved.6 The thumb, third and fourth finger, and the dominant hand are most often involved.10,11 TF can be seen in children usually as a trigger thumb,2,12-14 which may be a distinct clinical entity from pediatric trigger finger15 and may be acquired rather than congenital as a prospective cohort study of 2-week-old infants without trigger thumb developed it 3.3/1000 by 1 year of age.16
The pathophysiology of TF in adults is a combination of a thickened, stenotic A1 pulley (Figure 1) with progressive deterioration of its inner fibrocartilaginous gliding surface17,18 producing tendon friction. This friction results in nodular change in the tendon and inflammation seen as hypervascularity in the flexor tendon on ultrasound (US).19,20 The 5- to 7-mm length A1 pulley of each digit can be located on surface anatomy on the palmar side opposite the bony prominence of the dorsum of the metacarpophalangeal (MCP) joint.7,21 Alternatively, on palmar surface anatomy, the A1 pulley is located at the ulnar side of the thumb at its proximal crease, the proximal palmar crease of digit 2, and the distal palmar crease of digits 3 to 5.22
Figure 1.
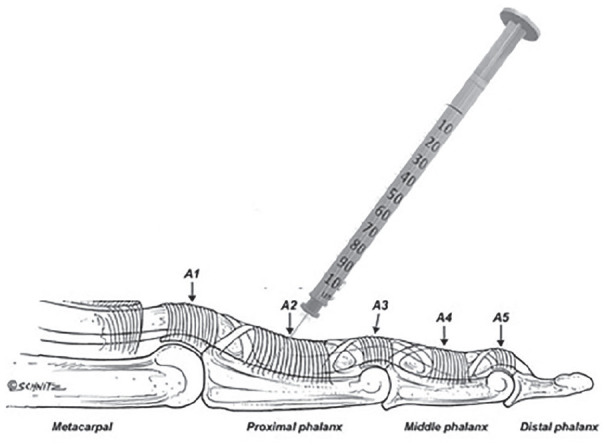
The digital pulley system and flexor tendon sheath injection at the proximal phalanx.
After Ryzewicz and Wolf (2006).22
An etiologic relation in adults performing manual labor, particularly those whose work or hobbies require prolonged tight repetitive gripping with palmar pressure or use of power tools with direct vibratory forces on the flexor tendons, has long been suspected though unproven.11,23-25 Occupational causes were not associated with TF in 2 series of patients presenting to hand surgeons for treatment.26,27 Querying patients regarding hobbies involving flexor tendon overuse such as pulling weeds, biking or power tool use might elicit causative or contributory activities.
Diagnosis is based on the presence of pain and tenderness of the A1 pulley in grade I Green’s classification,28 catching during flexion and extension of a finger or thumb in grade II and locking requiring use of the contralateral hand to open the finger after flexion in grade III. Rarely, patients will present with a locked finger that cannot be even passively extended (grade IV).
Even though the pathology is in the A1 pulley on the volar metacarpal head, patients may insist that the location of the “catching” is in their interphalangeal (IP) thumb or proximal interphalangeal (PIP) finger joint. Gentle digital pressure on the A1 pulley with active and passive digit movement to demonstrate triggering and palpation for pain and potentially a tendon nodule at that location confirms the diagnosis and may help patients understand that the pathology is indeed in the A1 pulley. US imaging of the A1 pulley is 85% sensitive and specific for TF using a pulley thickness cutoff of 0.62 mm with an average pulley thickness in TF of 0.77 to 0.79 mm (normal 0.43 to 0.47 mm) regardless of age, sex, body mass index, or adult height.29 The pain of TF should be differentiated from Duputryen’s contracture, carpal tunnel syndrome, infectious tenosynovitis, and MCP arthritis.
Splinting is an efficacious treatment for TF, resulting in an approximately 60% cure rate, but must be maintained for 6 to 9 weeks.22,30 It is unknown whether an MCP or a PIP joint blocking orthosis is superior as various studies have shown differing results.31-33 A recent novel approach to increase acceptability is night splinting, which showed resolution of symptoms in 55% of patients presenting with grade I or II TF for less than 3 months duration who were splinted at night for 6 weeks.34 Observation is another option as one retrospective case series by a hand surgeon found that 52% of patients had complete resolution of trigger finger within an average time of 8 months without splinting or corticosteroid injection.35 Avoidance of suspected causative activities is often recommended, but whether it hastens resolution beyond simple observation is unknown.
Most patients in the United States who learn that a 5-minute injection will be at least as effective and result in more rapid symptom relief as 6 to 9 weeks of finger splinting or 8 months of observation will choose injection.22 First reported in 1953 by Howard, single corticosteroid injections in TF have been associated with long-term cure rates of 60% in many case series, cohort studies, and a few randomized trials with cure rates approaching 90% particularly when a second or third injection is given.36-43 All of the long-acting corticosteroids appear nearly equally effective.44
In one series of 77 patients followed for an average 4.5 years after TF steroid injection, patients experienced resolution of pain in the first few days, resolution of locking in the first few weeks, and complete or near complete improvement in 80% and partial improvement in 17% at 6 weeks with persisting cures in 61% at 4.5 years.36 Cure rates of 70% to 80% were reported by 4 other investigators reporting over 2- to 3-year follow-up data after up to 3 injections.42,45-47 A 2007 meta-analysis on TF injection included four prospective randomized controlled trials and concluded steroid injections resolve TF in 57% of patients.31 A Cochrane review from a 2007 literature search published in 2009, including 2 of those randomized controlled trials concluded that corticosteroid versus placebo lidocaine injection for TF had a number needed to treat (NNT) of 3 to benefit at 1 month and NNT of 2 to benefit at 4 months post-injection.37,41,48,49 Lower rates of resolution have been demonstrated in fingers (vs thumbs), in diabetics, those with multiple TF, diffuse swelling (vs a palpable nodule) and patients with more severe grades of disease.8,38,50,51 For patients with partial improvement, optimal timing of the next injection appears to be after 69 days,52 not sooner.53
Ultrasound guidance offers no advantage over landmark guidance, other than greater accuracy of intrasheath placement of steroid,54 which did not correlate with higher efficacy in a 1998 radiographic dye study55 or in 2 randomized trials of US-guided intrasheath versus landmark-guided intrasheath injections.56,57 Two other randomized trials of US-guided intrasheath injection versus extrasheath injection similarly showed no difference in efficacy.58,59 This is likely because any steroid placed in the area has the same salutary effects on the regional structures.
Side effects of steroid injection include pain, bleeding, steroid flare reaction, infection, and transient elevation of blood glucose levels in diabetic patients. Rare cases of tendon rupture and deep space infection have been reported though neither was seen in the multiple case series and randomized trials including hundreds of patients referenced above. Patients with rheumatoid arthritis are at higher risk for tendon rupture and should be referred for release.22
Percutaneous or open A1 pulley release is used for TF cases that fail splinting and/or steroid injection. A recent Cochrane analysis of 14 trials including over 1200 patients undergoing surgical release was unable to ascertain a benefit of release procedures over steroid injection, and demonstrated increased short-term pain.60 Landmark-guided methods of longitudinal laceration of the A1 pulley are still used, though are being replaced by US-guided techniques, which have demonstrated low risk of tendon laceration or neurovascular bundle injury.61,62 US-guided TF release and open release appear to have equal efficacy in a nonblinded randomized controlled trial.62 Medicare reimbursement for TF release in the United States is low, albeit with some regional variation,63 leading some to suggest that early referral is better because percutaneous release may be more cost-effective for those at higher risk of nonresponse to injection.64
Procedure
The 4 approaches to steroid injection for TF appear to be equally effective.55-58,65 The classic method is to inject into the superficial tendon sheath through the A1 pulley, moving the finger to ensure one is not in the tendon. A cadaver dissection of fingers using this technique found that only 15% actually were into the sheath.54 A modification of that technique is to inject extra-synovial superficial to the tendon sheath. The least painful approach may be to inject the proximal phalangeal portion of the tendon sheath through a lateral approach while carefully avoiding the neurovascular bundle66,67; but this technique is technically more difficult for those infrequently performing such injections. A fourth method and the one we use and teach to our learners in our procedure clinic is a simple, safe entry over the volar proximal phalanx through the tendon to inject into the posterior (deep) space between tendon and sheath without US guidance as shown in Figure 1.
This has been demonstrated to also be less painful than the classic technique and is safe and simple to learn.68,69 A subcutaneous single-injection digital block with 2 mL of 1% lidocaine administered prior to injection further reduced pain in a recent randomized clinical trial.70
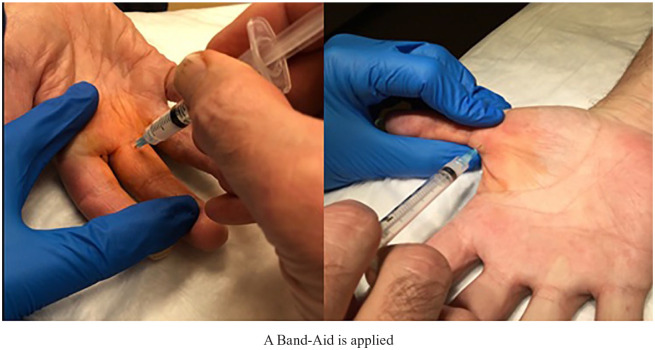
Step 1: Obtain written informed consent for risks of pain, bleeding, steroid flare reaction, and rare risk of infection, tendon rupture, and possible failure to improve. Position the patient with their hand supine on the examining table. Conduct a procedural pause to assure correct finger. Mark the target with the tip of an ear speculum for no-touch technique over the central proximal phalangeal flexor crease as shown in Figure 2.
Step 2: Prep the area with chlorhexidine-alcohol for 30 seconds. Betadine paint and dry may be substituted in patients with a chlorhexidine or alcohol allergy/sensitivity.
Step 3: Draw up a syringe with 0.5 mL bupivacaine 0.25% and 0.5 mL of methylprednisolone 40 mg/mL with a large (eg, 18g) needle then replace with a 25-27g needle. Lidocaine 1% or 2% may be substituted for bupivacaine but results in a shorter duration of pain relief.
Step 4: Insert the 25-27g needle into the target down through the combined superficial and deep flexor tendon to the central volar proximal phalanx bone (Figure 3). Depress the plunger on the syringe and if no flow occurs, withdraw the needle almost imperceptibly about 1 mm to achieve flow into the space between the posterior flexor tendon sheath and the tendon. There is no need to confirm placement outside the tendon through movement of the digit as in the classic method of injection into the sheath at the A1 pulley. Since the flexor tendon of the thumb is less flat, it may help to grasp either side of the tendon with a clean gloved nondominant hand in the no-touch technique (Figure 3) to insert the needle on the ulnar/palmar side of the thumb over the proximal phalanx.
Figure 2.

Marking the target.
Figure 3.
Trigger finger and thumb proximal phalangeal intra-sheath injection technique.
What Postinjection Advice Do You Give?
Patients are provided the following “rule of 3s” advice:
Don’t use your finger much for 3 days. (Buddy taping or splinting their finger will remind them to not use it.)
Avoid tight grasping for the next 3 weeks—“no power gripping” to avoid tendon rupture.
If not completely better, return for repeat injection in 3 months (and again for a third and final injection after that as needed).
Expect improvement of pain in days, locking and stiffness in weeks.
For future prevention, use padded gloves, tools, handlebars.
Decrease use of vibratory power tools requiring tight gripping as possible.
Discussion
Stenosing flexor tenosynovitis (TF) is a common disabling condition. Primary care providers should be able to quickly diagnose and provide rapid cure with a simple, low-risk landmark-guided corticosteroid injection. Injection into the flexor tendon sheath overlying the proximal phalanx is safe, effective, and less painful than an injection at the A1 pulley.
Night splinting the affected finger in for 6 to 9 weeks is an acceptable alternative and may augment compliance over continuous splinting. Release procedures are a reasonable alternative for patients who have failed to improve with multiple steroid injections, particularly those at high risk of continued failure.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Stephen P. Merry  https://orcid.org/0000-0002-3816-8154
https://orcid.org/0000-0002-3816-8154
Jason S. O’Grady  https://orcid.org/0000-0002-0541-7265
https://orcid.org/0000-0002-0541-7265
Christopher L. Boswell  https://orcid.org/0000-0002-9034-3415
https://orcid.org/0000-0002-9034-3415
References
- 1. Fahey JJ, Bollinger JA. Trigger-finger in adults and children. J Bone Joint Surg Am. 1954;36-A:1200-1218. [PubMed] [Google Scholar]
- 2. Weilby A. Trigger finger. Incidence in children and adults and the possibility of a predisposition in certain age groups. Acta Orthop Scand. 1970;41:419-427. [DOI] [PubMed] [Google Scholar]
- 3. Strom L. Trigger finger in diabetes. J Med Soc N J. 1977;74:951-954. [PubMed] [Google Scholar]
- 4. Vance MC, Tucker JJ, Harness NG. The association of hemoglobin A1c with the prevalence of stenosing flexor tenosynovitis. J Hand Surg Am. 2012;37:1765-1769. [DOI] [PubMed] [Google Scholar]
- 5. Kuczmarski AS, Harris AP, Gil JA, Weiss AC. Management of diabetic trigger finger. J Hand Surg Am. 2019;44:150-153. [DOI] [PubMed] [Google Scholar]
- 6. Koh S, Nakamura S, Hattori T, Hirata H. Trigger digits in diabetes: their incidence and characteristics. J Hand Surg Eur Vol. 2010;35:302-305. [DOI] [PubMed] [Google Scholar]
- 7. David M, Rangaraju M, Raine A. Acquired triggering of the fingers and thumb in adults. BMJ. 2017;359:j5285. [DOI] [PubMed] [Google Scholar]
- 8. Shultz KJ, Kittinger JL, Czerwinski WL, Weber RA. Outcomes of corticosteroid treatment for trigger finger by stage. Plast Reconstr Surg. 2018;142:983-990. [DOI] [PubMed] [Google Scholar]
- 9. Berlanga-de-Mingo D, Lobo-Escolar L, Lopez-Moreno I, Bosch-Aguila M. Association between multiple trigger fingers, systemic diseases and carpal tunnel syndrome: a multivariate analysis. Rev Esp Cir Ortop Traumatol. 2019;63:307-312. [DOI] [PubMed] [Google Scholar]
- 10. Schubert C, Hui-Chou HG, See AP, Deune EG. Corticosteroid injection therapy for trigger finger or thumb: a retrospective review of 577 digits. Hand (N Y). 2013;8:439-444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Moore JS. Flexor tendon entrapment of the digits (trigger finger and trigger thumb). J Occup Environ Med. 2000;42:526-545. [DOI] [PubMed] [Google Scholar]
- 12. Rodgers WB, Waters PM. Incidence of trigger digits in newborns. J Hand Surg Am. 1994;19:364-368. [DOI] [PubMed] [Google Scholar]
- 13. Moon WN, Suh SW, Kim IC. Trigger digits in children. J Hand Surg Br. 2001;26:11-12. [DOI] [PubMed] [Google Scholar]
- 14. Womack ME, Ryan JC, Shillingford-Cole V, Speicher S, Hogue GD. Treatment of paediatric trigger finger: a systematic review and treatment algorithm. J Child Orthop. 2018;12:209-217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Shah AS, Bae DS. Management of pediatric trigger thumb and trigger finger. J Am Acad Orthop Surg. 2012;20:206-213. [DOI] [PubMed] [Google Scholar]
- 16. Kikuchi N, Ogino T. Incidence and development of trigger thumb in children. J Hand Surg Am. 2006;31:541-543. [DOI] [PubMed] [Google Scholar]
- 17. Sbernardori MC, Bandiera P. Histopathology of the A1 pulley in adult trigger fingers. J Hand Surg Eur Vol. 2007;32:556-559. [DOI] [PubMed] [Google Scholar]
- 18. Drossos K, Remmelink M, Nagy N, De Maertelaer V, Pasteels JL, Schuind F. Correlations between clinical presentations of adult trigger digits and histologic aspects of the A1 pulley. J Hand Surg. 2009;34:1429-1435. [DOI] [PubMed] [Google Scholar]
- 19. Guerini H, Pessis E, Theumann N, et al. Sonographic appearance of trigger fingers. J Ultrasound Med. 2008;27:1407-1413. [DOI] [PubMed] [Google Scholar]
- 20. Hueston JT, Wilson WF. The aetiology of trigger finger explained on the basis of intratendinous architecture. Hand. 1972;4:257-260. [DOI] [PubMed] [Google Scholar]
- 21. Jongjirasiri Y. Length and landmark of A1 pulley in hand: an anatomical study. J Med Assoc Thai. 2009;92:41-46. [PubMed] [Google Scholar]
- 22. Ryzewicz M, Wolf JM. Trigger digits: principles, management, and complications. J Hand Surg Am. 2006;31:135-146. [DOI] [PubMed] [Google Scholar]
- 23. Moore JS, Garg A. Upper extremity disorders in a pork processing plant: relationships between job risk factors and morbidity. Am Ind Hyg Assoc J. 1994;55:703-715. [DOI] [PubMed] [Google Scholar]
- 24. Sampson SP, Badalamente MA, Hurst LC, Seidman J. Pathobiology of the human A1 pulley in trigger finger. J Hand Surg Am. 1991;16:714-721. [DOI] [PubMed] [Google Scholar]
- 25. Gorsche R, Wiley JP, Renger R, Brant R, Gemer TY, Sasyniuk TM. Prevalence and incidence of stenosing flexor tenosynovitis (trigger finger) in a meat-packing plant. J Occup Environ Med. 1998;40:556-560. [DOI] [PubMed] [Google Scholar]
- 26. Trezies AJ, Lyons AR, Fielding K, Davis TR. Is occupation an aetiological factor in the development of trigger finger? J Hand Surg. 1998;23:539-540. [DOI] [PubMed] [Google Scholar]
- 27. Kasdan ML, Leis VM, Lewis K, Kasdan AS. Trigger finger: not always work related. J Ky Med Assoc. 1996;94:498-499. [PubMed] [Google Scholar]
- 28. Green D, Hotchkiss R, Pederson W, Wolfe S. Green’s Operative Hand Surgery. 5th ed. Churchill Livingstone; 2005. [Google Scholar]
- 29. Spirig A, Juon B, Banz Y, Rieben R, Vögelin E. Correlation between sonographic and in vivo measurement of A1 pulleys in trigger fingers. Ultrasound Med Biol. 2016;42:1482-1490. [DOI] [PubMed] [Google Scholar]
- 30. Patel MR, Bassini L. Trigger fingers and thumb: when to splint, inject, or operate. J Hand Surg Am. 1992;17:110-113. [DOI] [PubMed] [Google Scholar]
- 31. Fleisch SB, Spindler KP, Lee DH. Corticosteroid injections in the treatment of trigger finger: a level I and II systematic review. J Am Acad Orthop Surg. 2007;15:166-171. [DOI] [PubMed] [Google Scholar]
- 32. Tarbhai K, Hannah S, von Schroeder HP. Trigger finger treatment: a comparison of 2 splint designs. J Hand Surg Am. 2012;37:243-249,249.e1. [DOI] [PubMed] [Google Scholar]
- 33. Teo SH, Ng DCL, Wong YKY. Effectiveness of proximal interphalangeal joint-blocking orthosis vs metacarpophalangeal joint-blocking orthosis in trigger digit management: a randomized clinical trial. J Hand Ther. 2019;32:444-451. [DOI] [PubMed] [Google Scholar]
- 34. Drijkoningen T, van Berckel M, Becker SJE, Ring DC, Mudgal CS. Night splinting for idiopathic trigger digits. Hand (N Y). 2018;13:558-562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. McKee D, Lalonde J, Lalonde D. How many trigger fingers resolve spontaneously without any treatment? Plast Surg (Oakv). 2018;26:52-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Anderson B, Kaye S. Treatment of flexor tenosynovitis of the hand (“trigger finger”) with corticosteroids: a prospective study of the response to local injection. Arch Intern Med. 1991;151:153-156. [PubMed] [Google Scholar]
- 37. Chambers RG., Jr. Corticosteroid injections for trigger finger. Am Fam Physician. 2009;80:454. [PubMed] [Google Scholar]
- 38. Freiberg A, Mulholland R, Levine R. Nonoperative treatment of trigger fingers and thumbs. J Hand Surg. 1989;14:553-558. [DOI] [PubMed] [Google Scholar]
- 39. Howard LD, Jr, Pratt DR, Bunnell S. The use of compound F (hydrocortone) in operative and non-operative conditions of the hand. J Bone Joint Surg. 1953;35-A:994-1002. [PubMed] [Google Scholar]
- 40. Kerrigan CL, Stanwix MG. Using evidence to minimize the cost of trigger finger care. J Hand Surg Am. 2009;34:997-1005. [DOI] [PubMed] [Google Scholar]
- 41. Peters-Veluthamaningal C, van der Windt DA, Winters JC, Meyboom-de Jong B. Corticosteroid injection for trigger finger in adults. Cochrane Database Syst Rev. 2009;(1):CD005617. [DOI] [PubMed] [Google Scholar]
- 42. Rhoades CE, Gelberman RH, Manjarris JF. Stenosing tenosynovitis of the fingers and thumb. Results of a prospective trial of steroid injection and splinting. Clin Orthop Relat Res. 1984;(190):236-238. [PubMed] [Google Scholar]
- 43. Rozental TD, Zurakowski D, Blazar PE. Trigger finger: prognostic indicators of recurrence following corticosteroid injection. J Bone Joint Surg Am. 2008;90:1665-1672. [DOI] [PubMed] [Google Scholar]
- 44. Roberts JM, Behar BJ, Siddique LM, Brgoch MS, Taylor KF. Choice of corticosteroid solution and Outcome After Injection for Trigger Finger. Hand (N Y). [published online June 18, 2019]. doi: 10.1177/1558944719855686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Faunø P, Andersen H, Simonsen O. A long-term follow-up of the effect of repeated corticosteroid injections for stenosing tenovaginitis. J Hand Surg Br. 1989;14:242-243. [DOI] [PubMed] [Google Scholar]
- 46. Marks MR, Gunther SF. Efficacy of cortisone injection in treatment of trigger fingers and thumbs. J Hand Surg Am. 1989;14:722-727. [DOI] [PubMed] [Google Scholar]
- 47. Newport ML, Lane LB, Stuchin SA. Treatment of trigger finger by steroid injection. J Hand Surg Am. 1990;15:748-750. [DOI] [PubMed] [Google Scholar]
- 48. Lambert M, Morton R, Sloan J. Controlled study of the use of local steroid injection in the treatment of trigger finger and thumb. J Hand Surg Br. 1992;17:69-70. [DOI] [PubMed] [Google Scholar]
- 49. Murphy D, Failla JM, Koniuch MP. Steroid versus placebo injection for trigger finger. J Hand Surg Am. 1995;20:628-631. [DOI] [PubMed] [Google Scholar]
- 50. Chang CJ, Chang SP, Kao LT, Tai TW, Jou IM. A meta-analysis of corticosteroid injection for trigger digits among patients with diabetes. Orthopedics. 2018;41:e8-e14. [DOI] [PubMed] [Google Scholar]
- 51. Luther GA, Murthy P, Blazar PE. Cost of immediate surgery versus non-operative treatment for trigger finger in diabetic patients. J Hand Surg. 2016;41:1056-1063. [DOI] [PubMed] [Google Scholar]
- 52. Usmani RH, Abrams SS, Merrell GA. Establishing an efficient care paradigm for trigger finger. J Hand Surg Asian Pac Vol. 2018;23:356-359. [DOI] [PubMed] [Google Scholar]
- 53. Sheikh E, Peters JD, Sayde W, Maltenfort M, Leinberry C. A prospective randomized trial comparing the effectiveness of one versus two (staged) corticosteroid injections for the treatment of stenosing tenosynovitis. Hand (N Y). 2014;9:340-345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Lee DH, Han SB, Park JW, Lee SH, Kim KW, Jeong WK. Sonographically guided tendon sheath injections are more accurate than blind injections: implications for trigger finger treatment. J Ultrasound Med. 2011;30:197-203. [DOI] [PubMed] [Google Scholar]
- 55. Taras JS, Raphael JS, Pan WT, Movagharnia F, Sotereanos DG. Corticosteroid injections for trigger digits: is intrasheath injection necessary? J Hand Surg. 1998;23:717-722. [DOI] [PubMed] [Google Scholar]
- 56. Cecen GS, Gulabi D, Saglam F, Tanju NU, Bekler HI. Corticosteroid injection for trigger finger: blinded or ultrasound-guided injection? Arch Orthop Trauma Surg. 2015; 135:125-131. [DOI] [PubMed] [Google Scholar]
- 57. Roh YH, Kim S, Gong HS, Baek GH. A randomized comparison of ultrasound-guided versus landmark-based corticosteroid injection for trigger finger. J Hand Surg Eur Vol. [published online April 4, 2019]. doi: 10.1177/1753193419839892 [DOI] [PubMed] [Google Scholar]
- 58. Shinomiya R, Sunagawa T, Nakashima Y, Yoshizuka M, Adachi N. Impact of corticosteroid injection site on the treatment success rate of trigger finger: a prospective study comparing ultrasound-guided true intra-sheath and true extra-sheath injections. Ultrasound Med Biol. 2016;42:2203-2208. [DOI] [PubMed] [Google Scholar]
- 59. Mardani-Kivi M, Karimi-Mobarakeh M, Jandaghi AB, Keyhani S, Saheb-Ekhtiari K, Hashemi-Motlagh K. Intra-sheath versus extra-sheath ultrasound guided corticosteroid injection for trigger finger: a triple blinded randomized clinical trial. Phys Sportsmed. 2018;46:93-97. [DOI] [PubMed] [Google Scholar]
- 60. Fiorini HJ, Tamaoki MJ, Lenza M, Dos Santos JBG, Faloppa F, Belloti JC. Surgery for trigger finger. Cochrane Database Syst Rev. 2018;2(2):CD009860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Smith J, Rizzo M, Lai JK. Sonographically guided percutaneous first annular pulley release: cadaveric safety study of needle and knife techniques. J Ultrasound Med. 2010;29: 1531-1542. [DOI] [PubMed] [Google Scholar]
- 62. Xie P, Zhang QH, Zheng GZ, et al. Stenosing tenosynovitis: evaluation of percutaneous release with a specially designed needle vs open surgery. Orthopade. 2019;48:202-206. [DOI] [PubMed] [Google Scholar]
- 63. Veltre DR, Yakavonis M, Curry EJ, et al. Regional variations of Medicare physician payments for hand surgery procedures in the United States. Hand (N Y). 2019;14:209-216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Brozovich N, Agrawal D, Reddy G. A critical appraisal of adult trigger finger: pathophysiology, treatment, and future outlook. Plast Reconstr Surg Glob Open. 2019;7:e2360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Kazuki K, Egi T, Okada M, Takaoka K. Clinical outcome of extrasynovial steroid injection for trigger finger. Hand Surg. 2006;11:1-4. [DOI] [PubMed] [Google Scholar]
- 66. Carlson CS, Jr, Curtis RM. Steroid injection for flexor tenosynovitis. J Hand Surg Am. 1984;9:286-287. [DOI] [PubMed] [Google Scholar]
- 67. Jianmongkol S, Kosuwon W, Thammaroj T. Intra-tendon sheath injection for trigger finger: the randomized controlled trial. Hand Surg. 2007;12:79-82. [DOI] [PubMed] [Google Scholar]
- 68. Pataradool K, Buranapuntaruk T. Proximal phalanx injection for trigger finger: randomized controlled trial. Hand Surg. 2011;16:313-317. [DOI] [PubMed] [Google Scholar]
- 69. Rosenbaum YA, Benvenuti N, Yang J, Ruff ME, Awan HM, Samora JB. The effect of trigger finger injection site on injection-related pain. Hand (N Y). 2018;13:164-169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Kosiyatrakul A, Songchou K, Luenam S. Reduction in pain from corticosteroid injection for the treatment of trigger finger with subcutaneous single‑injection digital block: a randomized controlled trial. Musculoskelet Surg. [published online April 29, 2020]. doi: 10.1007/s12306-020-00661-z [DOI] [PubMed] [Google Scholar]