Abstract
Introduction:
Periprosthetic femur fractures (PPFX) are complications of both total hip and knee arthroplasty and may be treated with open reduction and internal fixation (ORIF) or revision arthroplasty. Differences in treatment and fracture location may be related to patient demographics and lead to differences in cost. Our study examined the effects of demographics and treatment of knee and hip PPFXs on length of stay (LOS) and cost.
Methods:
Of all, 932 patients were identified with hip or knee PPFXs in the National Inpatient Sample from January 2013 to September 2015. Age, gender, race, mortality, comorbidity level, LOS, total cost, procedure type, geographic region, and hospital type were recorded. A generalized linear regression model was conducted to analyze the effect of fracture type on LOS and cost.
Results:
Differences in gender (66% vs 83.7% female, P < .01), comorbidities (fewer in hips, P < .01), and costs (US$30 979 vs US$27 944, P < .01) were found between the hip and knee groups. Knees had significantly higher rates of ORIF treatment (80.7% vs 39.1%) and lower rates of revision arthroplasties (19.3% vs 60.9%) than hip PPFXs (P < .01). Within both groups, patients with more comorbidities, revision surgery, and blood transfusions were more likely to have a longer LOS and higher cost.
Conclusion:
Periprosthetic femur fractures patients are not homogenous and treatment varies between hip and knee locations. For knee patients, those treated with ORIF were younger, with fewer comorbidities than those treated with revision. Conversely, hip patients treated with ORIF were older, with more comorbidities than those treated with revision. Hips had higher costs than knees, and cost correlated with revision arthroplasty and more comorbidities. In both hip and knee groups, longer LOS was associated with more comorbidities and being treated in urban teaching hospitals. Total cost had the strongest associations with revision procedures as well as number of comorbidities and blood product use.
Keywords: femur fracture, periprosthetic fracture, revision arthroplasty, hip replacement, knee replacement
Introduction
Periprosthetic femur fracture (PPFX) is a major complication of both total hip arthroplasty (THA) and total knee arthroplasty (TKA). The incidence of PPFX is rising with the increasing prevalence of patients with hip or knee arthroplasties.1 Treatment is costly and associated with poor outcomes, high mortality rate, and failure to recover previous functionality.2,3 Patients with knee, or distal femur, PPFXs are thought to be younger and have less mortality at a year than patients with hip PPFXs.4
Treatment options for PPFXs typically include revision arthroplasty or open reduction and internal fixation (ORIF). Fracture pattern and stability of the joint prosthesis at the time of fracture often dictates choice of treatment. This decisional process, however, is not straight forward across institutions and among providers. In general, fractures with loose implants are treated with revision arthroplasty while fractures with stable implants are treated with fixation.5 However in the hip, Vancouver B fractures with a potentially loose stem have been shown to do just as well with either ORIF or revision arthroplasty.6,7 There may be bias toward fixation or revision surgery depending on the treating surgeon’s subspecialty, joint replacement, or traumatology. The surgical procedure performed may alter weight bearing status, although there is increasing information that all periprosthetic fractures should be allowed to bear weight as tolerated.6
The goal of our study was to examine the demographics, costs, and in-hospital complications of patients with femur PPFXs and to determine risks of hip versus knee fracture pattern and treatment with ORIF versus revision arthroplasty. Our hypothesis was that treatment of PPFX with revision surgery would be more expensive than treatment with ORIF and that treatment of hip PPFXs would have higher costs and increased morbidity than treatment of knee PPFXs.
Methods
The National Inpatient Sample (NIS) was used to analyze frequency and trends of PPFXs in the United States. The NIS, a nationally representative sample, was developed for the Healthcare Cost and Utilization Project (HCUP)—to aid in making national, state, and community decisions. It contains data from more than 7 million inpatient hospital stays a year and is weighted using a 20% stratified discharge sample from US community hospitals to estimate over 30 million hospitalizations nationally.8 This study was deemed exempt by our institutional review board.
Within the NIS database, all hip and knee PPFXs from January 2013 to September of 2015 were identified. This time span includes the most recent data available in the database for which the coding of diagnoses and procedures remained constant (International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM]). To establish the PPFX population, the following combinations of diagnosis codes were used for identification, where “X” is a wildcard: admission of a periprosthetic fracture around prosthetic joint (996.44) with fracture of either femur neck (820.XX) or unspecified part of femur (821.XX). This process produced 1139 patients. With use of this population’s particular diagnosis and procedure codes, admissions were identified as either a hip or knee PPFX. Excluded patients included those whose data supported an interprosthetic fracture (between ipsilateral hip and knee replacements; n = 8) and patients whose data supported neither a hip nor knee PPFX (n = 38). The ICD-9-CM procedure codes were then evaluated to generate a population of patients who underwent either ORIF or revision arthroplasty during their admission (see Figure 1). Patients were excluded who did not have procedure codes suggesting either ORIF or revision arthroplasty (n = 161). Our final data set included 932 patients.
Figure 1.
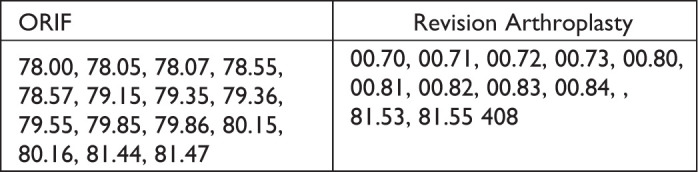
International Classification of Diseases, Ninth Revision, Clinical Modification procedure codes for ORIF and revision arthroplasty. ORIF indicates open reduction and internal fixation.
ICD-9-CM Procedure Codes for ORIF and Revision Arthroplasty
The NIS data were used to produce the final variables examined: age, gender, race, admission year, mortality, comorbidity level, length of hospital stay, total cost, PPFX type (hip or knee), procedure type (ORIF or revision arthroplasty), blood product use, acute transfer admit, geographic region, and hospital classification (rural, urban, or urban teaching). The NIS reclassifies all patients aged 90 years or older as being 89 years old (n = 103). Based on similar NIS orthopedic studies, patients were divided into 3 age categories: 18 to 64, 65 to 74, and 75 and older.9,10 Comorbidities were counted if they were part of the Elixhauser Index.11 Based on the distribution of comorbidities within our population, patients were divided up into 3 comorbidity categories: low (0-2), medium (3-4), and high (5+). These numbers were selected in order to give equal weight to each comorbidity level for use as a categorical variable.12 The Cost-to-Charge Ratio Files provided by the HCUP were used to estimate the cost of resources for patients based on the reported total charge. The HCUP used hospital specific cost-to-charge ratios.13 While charges represent the amount for which a hospital bills, cost reflects the actual expenses incurred in using the hospital’s services, such as wages, supplies, and utility costs. Expenses outside of hospital billing such as provider charges and postacute care are not included. After converting total charges to total costs, inflation was accounted for between the years of our study (2013-2015) and standardized costs to year 2015.
Descriptive statistics were used to summarize the data. Bivariate analysis was used to test for differences between the subgroup means by PPFX location (hip or knee) and, within each location, by procedure (ORIF or revision arthroplasty). The differences between the group means on each measure were analyzed for direction and statistical significance using t tests for continuous variables and χ2 tests for categorical variables. Standard error was reported alongside continuous variable means. Controlling for patient and clinical characteristics, a generalized linear regression model was conducted to analyze the effect of fracture type (knee or hip) on length of stay (LOS) and a linear regression was conducted to analyze the effect on total cost. All analysis accounted for NIS sampling design. Statistical significance was set at α = .05 for all analyses. The analysis was conducted using SAS Software version 9.4 (SAS Institute Inc, SAS 9.4, 2016) and Stata version 15 (StataCorp. Stata Statistical Software: Release 15, 2017).
Results
Overall, 43.5% patients had a knee PPFX and the remaining 56.5% had a hip PPFX ( Table 1). Significantly more knee and hip PPFXs occurred in females (Table 2), comprising 83.7% of knee PPFXs and 66.0% of hip fractures overall (P < .0001). The proportions of patients in the 3 varying comorbidity levels varied significantly from hip to knee PPFX patients with the hip group having more patients with low (0-2) comorbidities (P = .008). Patients with knee PPFXs had a significantly lower mean total cost than patients with hip PPFXs ($27 944 vs $30 979, P < .0001). Knee PPFXs had a significantly different type of treatment selected compared to hip PPFXs, with ORIF procedures comprising 80.7% of surgeries performed (39.1% for hip PPFFX, P < .0001). The proportion of patients with knee PPFXs that received blood did not vary significantly from patients with hip PPFXs (41.7% vs 50.1%, P = .010). Age, race, mortality, LOS, rate of transfer, and hospital classification did not vary significantly between the 2 groups.
Table 1.
Characteristics of the Study Population. a
| Characteristics | Summary measure (n = 4660) |
|---|---|
| Age, years | 74.51 ± 0.40 |
| 18-64, n (%) | 925 (19.9%) |
| 65-74, n (%) | 1095 (23.5%) |
| 75+, n (%) | 2635 (56.6%) |
| Female gender, n (%) | 3430 (73.7%) |
| Race | |
| White, n (%) | 3840 (85.5%) |
| Black, n (%) | 265 (5.9%) |
| Other, n (%) | 385 (8.6%) |
| Dead, n (%) | 85 (1.8%) |
| Comorbidity level | |
| Low (0-2), n (%) | 1695 (36.4%) |
| Medium (3-4), n (%) | 1665 (35.7%) |
| High (5+), n (%) | 1300 (27.9%) |
| LOS (days) | 7.55 ± 0.23 |
| Total cost | 29 656.00 ± 722.35 |
| Knee periprosthetic fracture, n (%) | 2025 (43.5%) |
| Procedure | |
| Internal fixation, n (%) | 2,665 (57.2%) |
| Revision arthroplasty, n (%) | 1995 (42.8%) |
| Blood product, n (%) | 2165 (46.5%) |
| Transfer, n (%) | 570 (12.3%) |
| Year | |
| 2013, n (%) | 1300 (27.9%) |
| 2014, n (%) | 1645 (35.3%) |
| 2015, n (%) | 1715 (36.8%) |
| Hospital region | |
| Midwest, n (%) | 960 (36.4%) |
| Northeast, n (%) | 660 (35.7%) |
| South, n (%) | 1955 (27.9%) |
| West, n (%) | 1085 (23.3%) |
| Hospital classification | |
| Rural, n (%) | 275 (5.9%) |
| Urban NT, n (%) | 1150 (24.7%) |
| Urban T, n (%) | 3235 (69.4%) |
Abbreviations: Blood Product: Blood Products were Ordered; LOS, hospital length of stay; Transfer, Transferred in from Acute Care Hospital; Urban NT, Urban nonteaching; Urban T, Urban teaching.
a Standard error (SE) reported with age, LOS and total cost means.
Table 2.
Comparison of Patient Characteristics by Periprosthetic Fracture Location (Hip vs Knee).a
| Characteristics | Knee (n = 2025) | Hip (n = 2635) | P value |
|---|---|---|---|
| Age, years | 74.8 ± 0.55 | 74.3 ± 0.54 | .452 |
| 18-64, n (%) | 350 (17.3%) | 575 (21.9%) | .014b |
| 65-74, n (%) | 560 (27.7%) | 535 (20.3%) | |
| 75+, n (%) | 1115 (55.1%) | 1520 (57.8%) | |
| Female gender, n (%) | 1695 (83.7%) | 1735 (66.0%) | <.0001c |
| Race | |||
| White, n (%) | 1680 (85.3%) | 2160 (85.7%) | .126 |
| Black, n (%) | 145 (7.4%) | 120 (4.8%) | |
| Other, n (%) | 145 (7.4%) | 240 (9.5%) | |
| Dead, n (%) | 50 (2.5%) | 35 (1.3%) | .206 |
| Comorbidity level | |||
| Low (0-2), n (%) | 635 (31.4%) | 1060 (40.2%) | .008d |
| Medium (3-4), n (%) | 815 (40.2%) | 850 (32.3%) | |
| High (5+), n (%) | 575 (28.4%) | 725 (27.5%) | |
| LOS (days) | 7.30 ± 0.30 | 7.74 ± 0.32 | .320 |
| Total cost | 27 944.00 ± 1146.49 | 30 979.00 ± 843.28 | <.0001c |
| Procedure | |||
| Internal fixation, n (%) | 1635 (80.7%) | 1030 (39.1%) | <.0001c |
| Revision arthroplasty, n (%) | 390 (19.3%) | 1605 (60.9%) | |
| Blood product, n (%) | 845 (41.7%) | 1320 (50.1%) | .010d |
| Transfer, n (%) | 235 (11.8%) | 335 (12.8%) | .613 |
| Hospital classification | |||
| Rural, n (%) | 110 (5.4%) | 165 (6.3%) | .122 |
| Urban NT, n (%) | 445 (22.0%) | 705 (26.8%) | |
| Urban T, n (%) | 1470 (72.6%) | 1765 (67.0%) | |
Abbreviations: LOS, hospital length of stay; Transfer, transferred in from acute care hospital; blood product, blood products were ordered; Urban NT, urban non-teaching; Urban T, Urban Teaching.
a SE reported with age, LOS, and total cost means.
b P ≤ .05.
c P ≤ .001.
d P ≤ .01.
The knee and hip PPFX patient groups were analyzed separately based on their treatment with either ORIF or revision arthroplasty ( Table 3). Compared to knee PPFX patients treated with a revision arthroplasty, knee PPFXs treated with ORIF had a significantly lower mortality rate (1.2% vs 7.7%, P < .0001) and rate of transfer (10.2% vs 17.9%, P < .0001).The breakdown of gender in knee PPFX patients treated with ORIF varied significantly from those treated with revision arthroplasty (82.0% vs 91.0% female; P = .039). The total cost of the hospital stay of PPFX patients treated with ORIF varied significantly compared to the revision arthroplasty for both the knee (US$25 019 vs US$40 591; P < .001) and the hip (US$25 706 vs US$34 352; P < .0001). Age (when categorized), gender, race, comorbidity levels, mortality rates, LOS, rate of use of blood products, and hospital type did not vary significantly in patients with hip PPFX treated with ORIF and revision arthroplasty.
Table 3.
Comparison of Patient Characteristics by Periprosthetic Location (Hip vs Knee) and Procedure (Internal Fixation vs Revision Arthroplasty).a
| Knee | Hip | |||||
|---|---|---|---|---|---|---|
| Characteristics | Internal fixation (n = 1635) | Revision arthroplasty (n = 390) | P value | Internal fixation (n = 1030) | Revision arthroplasty (n = 1605) | P value |
| Age, years | 74.59 ± 0.61 | 75.87 ± 0.99 | .034b | 75.80 ± 0.89 | 73.29 ± 0.67 | .034b |
| 18-64, n (%) | 305 (18.7%) | 45 (11.5%) | .248 | 200 (19.5%) | 375 (23.4%) | .198 |
| 65-74 | 435 (26.6%) | 125 (32.1%) | 185 (18.0%) | 350 (21.8%) | ||
| 75+ | 895 (54.7%) | 220 (56.4%) | 640 (62.4%) | 880 (54.8%) | ||
| Female gender | 1,340 (82.0%) | 355 (91.0%) | .039b | 695 (67.8%) | 1,040 (64.8%) | .441 |
| Race | ||||||
| White | 1385 (87.1%) | 295 (77.6%) | .076 | 835 (84.8%) | 1,325 (86.3%) | .281 |
| Black | 105 (6.6%) | 40 (10.5%) | 35 (3.6%) | 85 (5.5%) | ||
| Other | 100 (6.3%) | 45 (11.8%) | 115 (11.7%) | 125 (8.1%) | ||
| Dead | 20 (1.2%) | 30 (7.7%) | <.0001c | 20 (2.0%) | 15 (0.9%) | .321 |
| Comorbidity level | ||||||
| Low (0-2) | 495 (30.3%) | 140 (35.9%) | .438 | 380 (36.9%) | 680 (42.4%) | .002d |
| Medium (3-4) | 680 (41.6%) | 135 (34.6%) | 285 (27.7%) | 565 (35.2%) | ||
| High (5+) | 460 (28.1%) | 115 (29.5%) | 365 (35.4%) | 360 (22.4%) | ||
| LOS (days) | 7.31 ± 0.34 | 7.27 ± 0.52 | .95 | 7.45 ± 0.38 | 7.92 ± 0.44 | .419 |
| Total Cost | 25 019.00 ± 1209.05 | 40 591.00 ± 2162.28 | <.0001c | 25 706.00 ± 1203.39 | 34 352.00 ± 1042.51 | <.0001c |
| Blood Product | 670 (41.0%) | 175 (44.9%) | .520 | 475 (46.1%) | 845 (52.6%) | .119 |
| Transfer | 165 (10.2%) | 70 (17.9%) | .044 | 125 (12.2%) | 210 (13.2%) | .740 |
| Hospital type | ||||||
| Rural | 90 (5.5%) | 20 (5.1%) | .915 | 60 (5.8%) | 105 (6.5%) | .071 |
| Urban NT | 365 (22.3%) | 80 (20.5%) | 235 (22.8%) | 470 (29.3%) | ||
| Urban T | 1180 (72.2%) | 290 (74.4%) | 735 (71.4%) | 1030 (64.2%) | ||
Abbreviations: LOS, hospital length of stay; transfer, transferred in from acute care hospital; blood product, blood products were ordered; Urban NT, urban non-teaching; Urban T, urban teaching.
a SE reported with age, LOS, and total cost means.
b P ≤ .05.
c P ≤ .001.
d P ≤ .01.
Controlling for transfers, hospital type, age, comorbidities, blood product use, and procedure type, a generalized linear model was used to determine the separate effects of PPFX location on LOS (Table 4). For both hip and knee PPFX locations, age, and procedure type did not significantly impact LOS. The number of comorbidities did effect LOS. Compared to those with 0 to 2 comorbidities, patients with 5 or more comorbidities were more likely to have a longer LOS for both PPFX locations (knee: P = .016; hip: P < .0001). In patients with hip PPFXs, those with 3 to 4 comorbidities were additionally more likely to have a longer LOS than those with 0 to 2 comorbidities (P < .01). For both hip and knee PPFX locations, patients treated at an urban teaching hospital were more likely to have a higher LOS compared to urban nonteaching hospitals (knee: P = .005; hip: P = .054). The use of blood products increased the likelihood of having a higher LOS in patients with knee PPFXs (P = .011) but not for hip PPFX patients.
Table 4.
Length of Stay Regression With Knee and Hip Periprosthetic Fracture.
| Knee | Hip | |||
|---|---|---|---|---|
| Coef. (95% CI) | P value | Coef. (95% CI) | P value | |
| Transfer | −0.029 (−0.225 to 0.166) | .768 | 0.070 (−0.107 to 0.247) | .437 |
| Hospital: urban Ta | 0.220 (0.068 to 0.372) | .005b | 0.127 (−0.002 to 0.257) | .054 |
| Hospital: rurala | 0.002 (−0.314 to 0.318) | .989 | 0.028 (−0.332 to 0.388) | .879 |
| Age: 18-64c | 0.040 (−0.290 to 0.369) | .813 | 0.234 (−0.031 to 0.499) | .084 |
| Age: 75+c | −0.030 (−0.234 to 0.175) | .777 | 0.088 (−0.051 to 0.228) | .213 |
| Comorbidity: medium (3-4)d | 0.023 (−0.228 to 0.273) | .859 | 0.211 (0.077 to 0.345) | .002b |
| Comorbidity: high (5+)d | 0.321 (0.059 to 0.582) | .016e | 0.481 (0.238 to 0.724) | <.0001f |
| Blood product | 0.237 (0.054 to 0.420) | .011e | 0.033 (−0.143 to 0.210) | .711 |
| Procedure: revision arthroplasty | −0.015 (−0.186 to 0.157) | .868 | 0.115 (−0.053 to 0.283) | .179 |
Abbreviations: Blood Product: blood products were ordered; Transfer: transferred in from Acute Care Hospital.
a Referent: Hospital: Urban nonteaching.
b P ≤ 0.01
c Referent: Age: 65-74.
d Referent: comorbidity: low (0-2).
e P ≤ 0.05.
f P ≤ .001.
Controlling for transfers, hospital type, age, comorbidities, blood product use, and procedure type, multivariate linear regression was used to determine the separate effects of PPFX location on log total cost (Table 5). For both hip and knee PPFX, being treated at a rural hospital, age (when categorized), being treated at an urban teaching hospital and having 3 to 4 comorbidities did not significantly impact total costs. Compared to patients with 0 to 2 comorbidities, patients with 5 or more comorbidities on average had higher total costs for both PPFX locations, for knee patients the increase was an average 13.2% higher (P = .049) and for hip patients the increase was an average 18.3% higher (P = .004). Compared to patients treated with ORIF, patients treated with revision arthroplasty had higher total costs for both PPFX locations, for knee patients the average increase was 68.6% (P < .001), and for hip patients, the average increase was an average 39.0% (P < .001). For patients who had a knee PPFX, on average total costs were 11.3% higher if patients received blood products (P = .015) and 16.3% higher if patients were transferred (P = .033).
Table 5.
Total Cost Regression in Knee and Hip Periprosthetic Fracture.
| Knee | Hip | |||||
|---|---|---|---|---|---|---|
| Coef. (95% CI) |
Percent changea | P value | Coef. (95% CI) | Percent changea | P value | |
| Transfer | 0.151 (0.012 to 0.290) | 16.3% | .033b | 0.116 (−0.006 to 0.237) | 12.3% | .061 |
| Hospital: Urban T1 | −0.002 (−0.106 to 0.103) | −0.2% | .974 | 0.087 (−0.002 to 0.176) | 9.1% | .054 |
| Hospital: Ruralc | 0.048 (−0.184 to 0.280) | 5.0% | .681 | 0.068 (−0.117 to 0.254) | 7.1% | .470 |
| Age: 18-64d | 0.022 (−0.141 to 0.184) | 2.2% | .792 | 0.039 (−0.086 to 0.164) | 3.9% | .544 |
| Age: 75+d | 0.046 (−0.061 to 0.153) | 4.7% | .399 | −0.005 (−0.098 to 0.088) | −0.5% | .912 |
| Comorbidity: medium (3-4)e | 0.035 (−0.084 to 0.155) | 3.6% | .562 | 0.071 (−0.019 to 0.162) | 7.4% | .121 |
| Comorbidity: high (5+)e | 0.124 (0.000 to 0.248) | 13.2% | .049b | 0.168 (0.054 to 0.282) | 18.3% | .004f |
| Blood product | 0.154 (0.050 to 0.259) | 16.7% | .004f | 0.107 (0.021 to 0.193) | 11.3% | .015b |
| Procedure: revision arthroplastyg | 0.523 (0.413 to 0.632) | 68.6% | <.0001h | 0.329 (0.240 to 0.418) | 39.0% | <.0001h |
Abbreviations: Blood Product, blood Products were ordered; Transfer, transferred in from Acute Care Hospital.
a (eCoeff−1) × 100.
b P ≤ .05;
c Referent Groups: Hospital: Urban nonteaching.
d Age: 65-74.
e Comorbidity: Low (0-2).
f P ≤ .01.
g Procedure: Internal Fixation.
h P ≤ .001.
Discussion
In this study, we found that hip PPFXs are more common than knee PPFXs with both occurring more predominantly in females. In the United States in 2010, the overall prevalence of total TKAs (4 700 621) in the population was estimated at almost twice that of THAs (2 552 815).14 Our finding of fractures occurring more often after THA than TKA is unique. Overall, the rate of TKA is double that of THA. Our data would suggest that the rate of PPFX is at least 3 times higher after THA than after TKA. The reported rates of PPFXs differ widely in the literature, especially as some elect to include or exclude patients with previously revised arthroplasties.2 The estimated incidence of PPFX after primary THAs is 1%, while primary TKAs have an estimated incidence of PPFX ranging from 0.3% to 2.5%.15 These do not seem to correspond to the high discrepancy of PPFX about the hip that we observed. It is possible that the NIS database did not capture all codes regarding periprosthetic injuries about the knee or that the increased utilization of press-fit designs for primary THA in older individuals could have significant and previously unrecognized ramifications on long-term fracture risks. Potentially, the American Joint Replacement Registry will be able to further answer questions about the incidence and frequency of periprosthetic fractures in the future.
In addition to differences noted in fracture-type frequency, we noted differences in demographic variables between patients with hip or knee PPFXs. Patients having knee PPFX were more frequently female and had higher numbers of comorbidities. The association of femur PPFXs having a higher incidence in women has been well-documented in the literature and is most likely due to a higher predisposition for osteoporosis.2,15 While we did not observe difference inpatient ages between fracture types, Eschbach et al found that in their single institution’s cohort of PPFX, those with knee PPFX were significantly younger and had fewer nonoperative complications than hip PPFXs.4
There are many factors that go into surgical decision-making to treat PPFX with either ORIF or revision arthroplasty. In our study, we found that knee PPFXs treated with ORIF were younger and had fewer comorbidities than those treated with revision arthroplasty. This may indicate that older patients with osteoporosis are more likely to be treated with distal femoral replacement than with ORIF. Distal femoral replacement (DFR) has reported benefits of allowing for immediate weight-bearing without waiting for fracture healing.16,17 Our data set likely reflects these more contemporary considerations of early mobility when decisions were made regarding DFR versus ORIF. What remains unknown is the individual surgeon comfort and training that goes into deciding on attempting ORIF or choosing to do a megaprosthesis, which could skew the data.
On the other hand, we found that hips treated with ORIF were older and had more comorbidities. Unlike knee fracture surgery, revision hip surgery is generally more complicated with greater blood loss and operative times than ORIF. Treatment of hip PPFX is typically guided by fracture pattern and stability. Patients with loose femoral implants are usually treated with revision, although sometimes it is difficult to diagnose component loosening preoperatively.18 In some cases though, simple fixation may be an alternative even if the stem is loose but not subsided. Those patients who are believed to be of low functional demand with an un-revised, loose femoral component, may return to their premorbid level of activity with an ORIF.19 In a recent study evaluating hip PPFX using the National Readmission Database (NRD), we found similar rates of ORIF (206 [39%] of 507 vs Reeves et al: 1269 [28%] of 4523) versus revision surgery (321 [61%] of 507 vs Reeves et al: 3254 [72%] of 4523).20 In the study by Reeves et al, the need for revision increased with age and female gender. Our study did not observe such significant differences in treatment type in the over 75-year-old cohort. As these were using similar years of study, it is unclear if these findings are due to inherent differences between the NIS and the NRD. It is possible that the frailty of the patient drove the underlying decision for revision versus fixation surgery for hip PPFXs in our study.
Cost of treatment was significantly less for both knee and hip PPFXs when treated with ORIF as opposed to revision arthroplasty. In our multivariate analysis, revision surgery was the highest driver of cost, followed by the use of blood products and number of comorbidities. The increased cost of revision arthroplasty versus ORIF is most likely due to the high pricing of revision arthroplasty components. Revision surgery has previously been shown to be more expensive than ORIF in hip PPFX patients.20 This is in contrast to open proximal humerus fractures where no difference in cost was found between arthroplasty versus ORIF in the NIS database from 1998 to 2013.21 Several factors seemed to drive hospital LOS, including admission to an urban teaching hospital and having more comorbidities. Nationally, it is recognized that academic medical centers have an increased consolidation of medically complex patients that tend to have longer lengths of stay than nonacademic or rural hospitals.22 Similar to primary joint arthroplasty, it is logical that patients with a high comorbidities level, regardless of PPFX location, require a longer inpatient stay.23
There are several limitations in using NIS data. Our study is observational and relies on the diagnosis and procedure codes inputted by health care teams. Institutions, departments, and individuals may have differing techniques in recording such data over time, especially when considering the rare incidence of PPFXs. In harnessing the NIS data, we assumed that all PPFXs were properly coded. The use of administrative coding makes it impossible to distinguish between intraoperative and postoperative periprosthetic fractures in addition to fractures after primary or revision implants. We included all types of these fractures in our data set, which may skew our data toward a higher rate of hip PPFX given the higher incidence of intraoperative fractures with the high utilization of press-fit stems in all patient cohort age groups.24 Additionally, many cases of revision arthroplasty may also undergo concurrent ORIF. In general, the surgeon codes for the revision arthroplasty and the ORIF is considered bundled within the arthroplasty procedure. Our study would only pick up these cases as revision arthroplasty, which could underestimate the true incidence of ORIF procedures and may skew cost data. Furthermore, there could be inherent surgeon treatment biases not detected by administrative codes, especially when considering the availability of subspecialty care at rural and nonacademic medical centers. Our use of the Elixhauser methodology for counting individual comorbidities makes it harder to know the effect of an individual comorbidity to outcome. Lastly, cost data may not reflect true costs of care delivery and other factors, namely patient comorbidities, are also intertwined into LOS and cost determinations. The hospital charges do not include physician charges or postoperative acute care which may make up for 40% of the total charges for a diagnosis.13
Conclusion
Our study found difference between patients with hip and knee PPFX. Open reduction and internal fixations were performed for differing populations depending on fracture location: knee PPFXs that received ORIFs were younger with less comorbidities than those who had revisions while hip PPFXs that received ORIFs were older and had more comorbidities than those who had revisions. Total costs were higher in hip versus knee PPFXs and costs were driven by the need for revision arthroplasties as well as comorbidities. For both hip and knee PPFXs, LOS was longer in urban teaching hospitals and for patients with a high number of comorbidities.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Katelyn Ragland  https://orcid.org/0000-0002-4414-1265
https://orcid.org/0000-0002-4414-1265
References
- 1. Kurtz S. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Jt Surg. 2007;89(4):780 doi:10.2106/JBJS.F.00222 [DOI] [PubMed] [Google Scholar]
- 2. Sidler-Maier CC, Waddell JP. Incidence and predisposing factors of periprosthetic proximal femoral fractures: a literature review. Int Orthop. 2015;39(9):1673–1682. doi:10.1007/s00264-015-2721-y [DOI] [PubMed] [Google Scholar]
- 3. Zuurmond RG, van Wijhe W, van Raay JJAM, Bulstra SK. High incidence of complications and poor clinical outcome in the operative treatment of periprosthetic femoral fractures: an analysis of 71 cases. Injury. 2010;41(6):629–633. doi:10.1016/j.injury.2010.01.102 [DOI] [PubMed] [Google Scholar]
- 4. Eschbach D, Buecking B, Kivioja H, et al. One year after proximal or distal periprosthetic fracture of the femur—two conditions with divergent outcomes? Injury. 2018;49(6):1176–1182. doi:10.1016/j.injury.2018.04.025 [DOI] [PubMed] [Google Scholar]
- 5. Ricci WM. Periprosthetic femur fractures. J Orthop Trauma. 2015;29(3):130–137. doi:10.1097/BOT.0000000000000282 [DOI] [PubMed] [Google Scholar]
- 6. Ruder JA, Hart GP, Kneisl JS, Springer BD, Karunakar MA. Predictors of functional recovery following periprosthetic distal femur fractures. J Arthroplasty. 2017;32(5):1571–1575. doi:10.1016/j.arth.2016.12.013 [DOI] [PubMed] [Google Scholar]
- 7. Hoellwarth JS, Fourman MS, Crossett L, et al. Equivalent mortality and complication rates following periprosthetic distal femur fractures managed with either lateral locked plating or a distal femoral replacement. Injury. 2019;49(2):392–397. doi:10.1016/j.injury.2017.11.040 [DOI] [PubMed] [Google Scholar]
- 8. Healthcare Cost and Utilization Project Databases. Healthcare cost and utilization project (HCUP). Published 2018 Accessed March 3, 2019 https://www.hcup-us.ahrq.gov/nisoverview.jsp
- 9. Bhattacharya RK, Dubinsky RM, Lai SM, Dubinsky H. Is there an increased risk of hip fracture in Parkinson’s disease? A nationwide inpatient sample. Mov Disord. 2012;27(11):1440–1442. doi:10.1002/mds.25073 [DOI] [PubMed] [Google Scholar]
- 10. Sharma M, Sonig A, Ambekar S, Nanda A. Discharge dispositions, complications, and costs of hospitalization in spinal cord tumor surgery: analysis of data from the United States Nationwide Inpatient Sample, 2003–2010. J Neurosurg Spine. 2014;20(2):125–141. doi:10.3171/2013.9.SPINE13274 [DOI] [PubMed] [Google Scholar]
- 11. Menendez ME, Neuhaus V, Van Dijk CN, Ring D. The Elixhauser comorbidity method outperforms the Charlson index in predicting inpatient death after orthopaedic surgery. Clin Orthop Relat Res. 2014;472(9):2878–2886. doi:10.1007/s11999-014-3686-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kim CY, Sivasundaram L, LaBelle MW, Trivedi NN, Liu RW, Gillespie RJ. Predicting adverse events, length of stay, and discharge disposition following shoulder arthroplasty: a comparison of the Elixhauser comorbidity measure and Charlson comorbidity index. J Shoulder Elb Surg. 2018;27(10):1748–1755. doi:10.1016/j.jse.2018.03.001 [DOI] [PubMed] [Google Scholar]
- 13. Kurtz SM, Lau E, Ong KL, Katz JN, Bozic KJ. Universal health insurance coverage in Massachusetts did not change the trajectory of arthroplasty use or costs. Clin Orthop Relat Res. 2016;474(5):1090–1098. doi:10.1007/s11999-015-4643-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kremers HM, Larson DR, Crowson CS, et al. Prevalence of total hip and knee replacement in the United States. J Bone Jt Surg - Am Vol. 2014;97(17):1386–1397. doi:10.2106/JBJS.N.01141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Liporace FA, Donegan DJ, Langford JR, Haidukewych GJ. Contemporary internal fixation techniques for periprosthetic fractures of the hip and knee. AAOS Instr Course Lect. 2013;62:317–332. [PubMed] [Google Scholar]
- 16. Rao B, Kamal T, Vafe J, Moss M. Distal femoral replacement for selective periprosthetic fractures above a total knee arthroplasty. Eur J Trauma Emerg Surg. 2014;40(2):191–199. doi:10.1007/s00068-013-0347-6 [DOI] [PubMed] [Google Scholar]
- 17. Hart GP, Kneisl JS, Springer BD, Patt JC, Karunakar MA. Open reduction vs distal femoral replacement arthroplasty for comminuted distal femur fractures in the patients 70 years and older. J Arthroplasty. 2017;32(1):202–206. doi:10.1016/j.arth.2016.06.006 [DOI] [PubMed] [Google Scholar]
- 18. Lindahl H, Malchau H, Herberts P, Garellick G. Periprosthetic femoral fractures: classification and demographics of 1049 periprosthetic femoral fractures from the Swedish national hip arthroplasty register. J Arthroplasty. 2005;20(7):857–865. doi:10.1016/j.arth.2005.02.001 [DOI] [PubMed] [Google Scholar]
- 19. Gitajn IL, Heng M, Weaver MJ, et al. Mortality following surgical management of Vancouver B periprosthetic fractures. J Orthop Trauma. 2017;31(1):9–14. doi:10.1097/BOT.0000000000000711 [DOI] [PubMed] [Google Scholar]
- 20. Reeves RA, Schairer WW, Jevsevar DS. The national burden of periprosthetic hip fractures in the US: costs and risk factors for hospital readmission. HIP Int. 2019;29(5):550–557. doi:10.1177/1120700018803933 [DOI] [PubMed] [Google Scholar]
- 21. Dixit A, Cautela FS, Cooper CS, et al. ORIF versus arthroplasty for open proximal humerus fractures: Nationwide inpatient sample data between 1998 and 2013. J Orthop Traumatol. 2018;19(1):12 doi:10.1186/s10195-018-0503 -1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Doctoroff L, Hsu DJ, Mukamal KJ. Trends in prolonged hospitalizations in the United States from 2001 to 2012: a longitudinal cohort study. Am J Med. 2017;130(4):483. e1–483.e7 doi:10.1016/j.amjmed.2016.11.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Tay KS, Cher EWL, Zhang K, Tan SB, Howe TS, Koh JSB. Comorbidities have a greater impact than age alone in the outcomes of octogenarian total knee arthroplasty. J Arthroplasty. 2017;32(11):3373–3378. doi:10.1016/j.arth.2017.05.041 [DOI] [PubMed] [Google Scholar]
- 24. Springer BD, Etkin CD, Shores PB, Gioe TJ, Lewallen DG, Bozic KJ. Perioperative periprosthetic femur fractures are strongly correlated with fixation method: an analysis from the American joint replacement registry. J Arthroplasty. 2019;34(7):S352–S354. doi:10.1016/j.arth.2019.02.004 [DOI] [PubMed] [Google Scholar]


