Abstract
A common and potent consideration has recently entered the landscape of the novel coronavirus disease of 2019 (COVID-19): venous thromboembolism (VTE). COVID-19 has been associated to a distinctive related coagulopathy that shows unique characteristics. The research community has risen to the challenges posed by this « evolving COVID-19 coagulopathy » and has made unprecedented efforts to promptly address its distinct characteristics. In such difficult time, both national and international societies of thrombosis and hemostasis released prompt and timely responses to guide recognition and management of COVID-19-related coagulopathy. However, latest guidelines released by the international Society on Thrombosis and Haemostasis (ISTH) on May 27, 2020, followed the American College of Chest Physicians (CHEST) on June 2, 2020 showed some discrepancies regarding thromboprophylaxis use. In this forum article, we would like to offer an updated focus on thromboprophylaxis with current incidence of VTE in ICU and non-ICU patients according to recent published studies; highlight the main differences regarding ISTH and CHEST guidelines; summarize and describe which are the key ongoing RCTs testing different anticoagulation strategies in patients with COVID-19; and finally set a proposal for COVID-19 coagulopathy specific risk factors and dedicated trials.
Keywords: COVID-19, Coronavirus, Thromboprophylaxis, Venous thromboembolism, Guidelines
Highlights
Reported incidence of venous thrombotic events in COVID-19 patients
Major differences between ISTH and CHEST guidelines in thromboprophylaxis for patients with COVID-19
Ongoing RCTs of different anticoagulation strategies in patients with COVID-19
A proposal for COVID-19 coagulopathy specific risk factors and dedicated trials
A common and potent consideration has recently entered the landscape of the novel coronavirus disease of 2019 (COVID-19): venous thromboembolism (VTE). COVID-19 has been associated to a distinctive related coagulopathy that shows unique characteristics [1]. The research community has risen to the challenges posed by this « evolving COVID-19 coagulopathy » and has made unprecedented efforts to promptly address its distinct characteristics. However, a key central question that could guide prevention, diagnosis, and treatment strategies of COVID-19 coagulopathy remains under debate: are these haemostatic changes a consequence of severe inflammation or are they a specific effect mediated by the virus? [2]. The immune response to acute SARS-CoV-2 infection and the accompanying surge of cytokines and inflammatory mediators have been accepted as a key pathway triggering thrombogenesis. In this setting, early strategies aimed at reducing inflammation might help prevent thrombosis. The alternative postulate is that the virus directly or indirectly interferes with coagulation pathways. The determinants of both hypotheses seem to stem mostly from host factors such as age, comorbidities, and the prominent role played by the extent of lung injury. Owing to these determinants, the combined use of risk scores to identify high-risk patients for adverse thrombotic events may guide individualized antithrombotic treatment of Covid-19 patients [3]. Another important insight is the recognition of the importance of extravascular fibrinolytic activity in the airway lumen and the alveolar compartment. Extravascular fibrin was demonstrated as a possible mechanism by which inflammatory cells can invade the lung [4]. Breakdown of fibrin as a consequence of high fibrinolytic activity would lead to a marked generation of D-dimers levels independently of thrombotic events. According to this paradigm, high D-dimers levels would not be solely considered as a marker of thrombotic propensity but should be viewed as an integrate marker of disease severity including the extent of lung damage [5].
In the inpatient setting, the prevalence of VTE ranges from 3 to 85%, as detailed in Fig. 1 [6–25].
Fig. 1.
Reported incidence of venous thrombotic events in COVID-19 patients hospitalized in ICU (a) and non-ICU (b). Covid-19 coronavirus disease 201, ICU intensive care unit
However, most of studies on coronavirus patients used different design (systematic screening vs D-Dimer threshold vs symptom-driven approach), different intervention (contrasting intensities of thromboprophylaxis regimens), severity (ICU vs wards) and outcome (asymptomatic vs symptomatic VTE) resulting in reduced data comparability across studies (Table 1).
Table 1.
Prevalence of venous thrombotic events (acute pulmonary embolism and/or deep vein thrombosis) in COVID-19 patients
| Design | VTE | Thromboprophylaxis | Age | Male sex | |
|---|---|---|---|---|---|
| ICU COVID-19 patients | |||||
| Klok et al. (n = 184) | Cohort study | 28 (15.2%) | Thromboprophylaxis: 184 (100%). All patients received at least standard doses thromboprophylaxis, although regimens differed between hospitals and doses increased over time | 64 ± 12 | 76% |
| Helms et al. (n = 150) | Cohort study | 27 (18.0%) |
None: 0 (0%) Standard-dose (SD): 105 (70%) Intermediate-dose (ID): 0 (0%) Therapeutic dose (TD) or chronic therapeutic anticoagulation (CA): 45 (30%) |
63 (53–71) | 81.3% |
| Maatman et al. (n = 109) | Cohort study | 31 (28%) |
None: 0 (0%) SD: 109 (100%) ID: 0 (0%) TD or CA: 0 (0%) |
61 ± 16 | 57% |
| Poisy et al. (n = 107) | Cohort study | 22(20.6%) |
Among the 22 patients with pulmonary embolism None: 0 (0) SD: 20 (91%) ID: 0 (0%) TA or CA: 2 (9%) |
N/A | N/A |
| Cui et al. (n = 81) | Systematic screening for VTE | 20 (24.7%) |
None: 81 (100%) SD: 0 (0%) ID: 0 (0%) TD or CA: 0 (0%) |
59.9 ± 14.1 | 46% |
| Middeldorp et al. (n = 75) | Cohort study | 35 (47%) |
"Most ICU patients receiving routine thrombosis prophylaxis. Thrombosis prophylaxis was initiated in 167 (ICU + non-ICU) patients (84%) while 19 (9.6%) continued therapeutic anticoagulation" None: N/A SD: N/A IT: N/A TD or CA: 7 (9.3%) |
62 ± 10 | 77% |
| Lodigiani et al. (n = 61) | CT cohort study | 8 (16.7%) |
SD: 42 (68.8%) ID: 17 (27.9%) CT or CA: 2 (3.3%) |
61 (55–69) | 80.3% |
| Voicu et al. (n = 56) | Systematic screening for DVT | 26 (46%) |
None: 0 (0%) SD: 49 (87%) ID: 0 (0%) TD or CA: 7 (13%) |
N/A | 75% |
| Ren et al. (n = 48) | Systematic screening for DVT | 41 (85.4%) |
None: 1 (2%) SD: 41 (98%) ID: 0 (0%) TD or CA: 0 (0%) |
70 (62.5–80) | 54.2% |
| Grillet et al. (n = 39) | Chest CT cohort study | 17 (74%) | N/A | N/A | |
| Nahum et al. (n = 34) | Systematic screening for DVT | 27 (79%) | « All patients received anticoagulant prophylaxis at hospital admission» | 62.9 ± 7.9 | 74% |
| Llitjos et al. (n = 26) | Systematic screening for DVT | 18 (69%) |
None: 0 (0%) SD: 8 (31%) ID: 0 (0%) TD or CA: 18 (69%) |
68 (51.5–74.5) | 77% |
| Longchamp et al. (n = 25) | Systematic screening for DVT | 8 (32%) |
SD: 23 (92%) CA: 2 (8%) |
68 ± 11 | 64% |
| Non-ICU COVID-19 patients | |||||
| Fauvel et al. (n = 1240) | Cohort study | 103 (8.3%) |
None: 267 (21.5%) SD: 738 (63%) ID: 99 (8.4%) TA or CA: 136 (11%) |
64 ± 17.0 | 58.1% |
| Galeano-Valle et al. (n = 785) | Cohort study | 24 (3%) | N/A | N/A | N/A |
| Lodigiani et al. (n = 327) | Cohort study | 20 (6.4%) |
None: 53 (16.2%) SD: 133 (40.7%) ID: 67 (20.5%) TA or CA: 74 (22.6%) |
68 (55–77) | 65.7% |
| Trimaille et al. (n = 289) | Cohort study | 49 (17.0%) |
None: 31 (10.7%) SD: 170 (58.8%) ID: 31 (10.7%) TD or CA: 57 (19.7%) |
62.2 ± 17.0 | 59.2% |
| Demelo-Rodríguez et al. (n = 156) | Systematic screening for DVT with D-dimer > 1000 ng/ml | 23 (14.7%) |
None: 0 (0%) Pneumatic compression 3 (1.9%) DS: 133 (98.1%) ID: 0 (0%) TA or CA: 0(0%) |
68.1 ± 14.5 | 65.4% |
| Zhang et al. (n = 143) | Systematic screening for DVT | 66 (46.1%) |
None: 90 (62.9%) SD: 53 (37.1%) ID: 0 (0%) TA or CA: 0 (0%) |
63 ± 14 | 51.7% |
| Middeldorp et al. (n = 123) | Cohort study | 4 (3.3%) |
"Thromboprophylaxis was initiated in 167 (ICU + non-ICU) patients (84%) while 19 (9.6%) continued therapeutic anticoagulation" None: N/A SD and ID: N/A TA or CA: 12 (9.8%) |
60 ± 10 | 59% |
| Santoliquido et al. (n = 84) | Systematic screening for DVT | 10 (11.9%) |
None: 0 (0%) SD: 84 (100%) ID: 0 (0%) TD or CA: 0 (0%) |
67.6 ± 13.5 | 72.6% |
| Artifoni et al. (n = 71) | Systematic screening for DVT | 16 (22.5%) |
None: 0 (0%) SD: 71 (100%) ID: 0 (0%) TA or CA: 0 (0%) |
64 (46.0–75) | 60.6% |
| Grillet et al. (n = 61) | Chest CT cohort study | 6 (26%) | N/A | N/A | N/A |
CA chronic therapeutic anticoagulation, COVID-19 coronavirus disease 2019, CT computed tomography, DOAC direct oral anticoagulant, DVT deep vein thrombosis, ICU intensive care unit, IT thromboprophylaxis with intermediate-dose of LMWH/UFH, LMWH low-molecular-weight heparin, N/A not available, SD routine thromboprophylaxis with standard-dose of UFH or LMWH, TD thromboprophylaxis with therapeutic dose, UFH unfractionated heparin, VTE venous thrombotic events
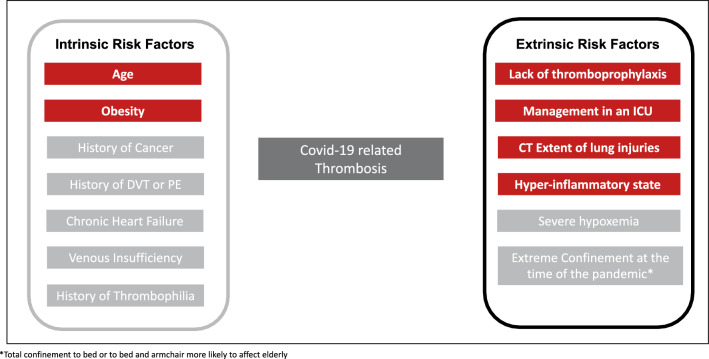
Furthermore, investigations from the outpatients are warranted with high priority, as they represent the vast majority of Covid-19 cases and VTE rate in this specific subset has not been reported yet [26]. Early reports suggested a high incidence of VTE and frequent haemostasis disorders in COVID-19 patients [27, 28]. Though, it remains to be demonstrated that theses frequent «new thrombotic» features at first glance are any different from previous experience from severe viral pneumonia [29–33]. Both intrinsic and extrinsic risk factors for VTE (Fig. 2) together with large number of patients considered at high risk on the basis of current VTE risk scores [34] lead to first interim [35] followed by updated guidance on thromboprophylaxis in hospitalized patients with COVID-19 [36, 37].The first reminder of a beneficial effect of thromboprophylaxis came as early as March 27, 2020 with reduced mortality in critically ills affected by severe COVID-19 and treated with heparin [38]. Of note, only 22.0% of the population analyzed by Tang et al. received anticoagulant therapy for the prevention of VTE and this reinforced the role for routine VTE risk assessment and the initiation of adequate thromboprophylaxis [39]. A substantial 5 to 10% risk of VTE in critically ills is currently reported despite the use of prophylactic anticoagulants [40–43]. COVID-19 patients presented in later reports with unusual higher rates of VTE despite the use of prophylactic anticoagulants [6–9, 12, 21].
Fig. 2.
Intrinsic and extrinsic risk factors for venous thromboembolism in COVID-19. Covid-19 coronavirus disease 2019, CT computed tomography, DVT deep vein thrombosis, ICU intensive care unit, PE pulmonary embolism
Latest ISTH consensus statement published on May 27, 2020 recommended routine thromboprophylaxis in non-ICU and ICU hospitalized COVID-19 patients with preferably standard-dose LMWH or UFH [37]. Due to time-sensitivity with the pandemic and in the absence of robust evidence, a “stepped therapy” approach in non-ICU patients or treatment-dose heparin in critically ills did not reach full consensus yet. With regards to the rapid deterioration reported in many COVID-19 patients requiring ICU transfer, long half-life and/or reversibility concerns, both fondaparinux and prophylactic dose DOAC were not recommended in critically ill hospitalized COVID-19 patients. Apart from body weight-adjusted dose on extremes cases (< 50 kg or > 120 kg or BMI), the ISTH expert panel recommended against the general use of intermediate dose of LMWH/UFH in non-ICU. Wisely awaiting for some strong evidences, intermediate-dose LMWH was only advocated by 30% of ISTH respondent in non-ICU and up to 50% in ICU patients (Table 2).
Table 2.
Major differences between ISTH and CHEST guidelines in thromboprophylaxis for patients with COVID-19
| Major differences between ISTH and CHEST guidelines in thromboprophylaxis for patients with COVID-19 | |
|---|---|
| International Society on Thrombosis and Haemostasis (ISTH) | CHEST Guideline and Expert Panel Report |
| VTE prophylaxis in acutely ill hospitalized patients | |
| Thromboprophylaxis with LMWH over UFH. Half-life and reversibility concerns regarding fondaparinux | Thromboprophylaxis with LMWH or fondaparinux over UFH. Thromboprophylaxis with LMWH, fondaparinux or UFH over a DOAC |
| Standard-dose anticoagulant thromboprophylaxis recommended, but intermediate-dose LMWH may also be considered (30% of responders) | Standard dose anticoagulant thromboprophylaxis over intermediate (LMWH BID or increased weight-based dosing) |
| VTE prophylaxis in critically ill patients | |
| Thromboprophylaxis with LMWH or UFH | Thromboprophylaxis with LMWH over UFH; and LMWH or UFH over fondaparinux or a DOAC |
|
Standard-dose anticoagulant thromboprophylaxis recommended, but intermediate-dose LMWH (50% of respondents) may be considered in high risk patients Patients with obesity as defined by actual body weight or BMI should be considered for a 50% increase in the dose of thromboprophylaxis |
Standard dose anticoagulant thromboprophylaxis over intermediate (LMWH BID or increased weight-based dosing) |
| Multi-modal thromboprophylaxis with mechanical methods (i.e., intermittent pneumonic compression devices) should be considered (60% of respondents) | Against the addition of mechanical prophylaxis to pharmacological thromboprophylaxis |
| After hospital discharge | |
| Extended post-discharge thromboprophylaxis should be considered for all hospitalized patients with COVID-19 that meet high VTE risk criteria. The duration of post-discharge thromboprophylaxis can be approximately 14 days at least (50% of respondents), and up to 30 days (20% of respondents) |
Inpatient thromboprophylaxis only over inpatient plus extended thromboprophylaxis after hospital discharge Extended thromboprophylaxis in patients at low risk of bleeding should be considered if emerging data on the post-discharge risk of VTE and bleeding risk indicate a net benefit |
BID twice-daily, BMI body mass index, Covid-19 coronavirus disease 2019, DOAC direct oral anticoagulant, ICU intensive care unit, LMWH low-molecular-weight heparin, UFH unfractionated heparin, VTE venous thromboembolism
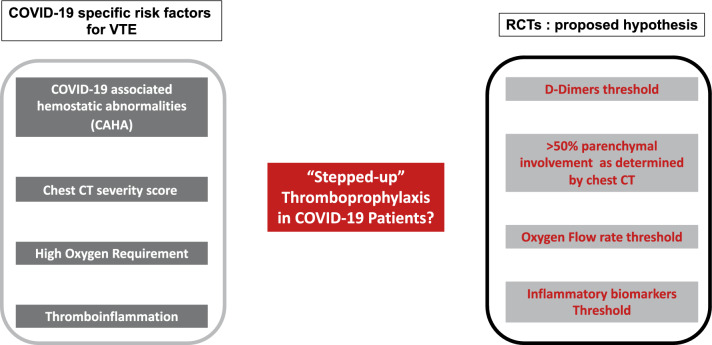
No more that 6 days after the ISTH guidance had been released, an American College of Chest Physicians (CHEST) panel of experts provided a conflicting set of guidelines on June 2, 2020 [44]. CHEST experts recommended (i) standard dose anticoagulant thromboprophylaxis in non-ICU and ICU patients, (ii) LMWH or fondaparinux over UFH in non-ICU patients, (iii) suggested against the addition of mechanical prophylaxis (i.e. intermittent pneumatic compression) to pharmacological thromboprophylaxis while 60% of ISTH experts pledged for it. Armed with this two set of guidelines, one being « conservative » and the other much more « liberal» on both stepped-up pharmacological and mechanical approach, how is the physician supposed to react in day use practice? Both guidelines nonetheless advocated for more evidence coming from ongoing randomized trials (Table 3), more extensive description of the « sicker » or « higher risk » patient profile likely to benefit from increased intensity anticoagulant thromboprophylaxis, and finally a call for updated evidences regarding bleeding risk in this population as they are insufficient so far. Identifying very-high-risk patients for VTE is undoubtedly the main issue of reducing both incidence and mortality risk of VTE [45]. The triad of risk seems to essentially rely on marked prothrombotic state, thromboinflammation and the extent of lung injury (Fig. 3).
Table 3.
Ongoing RCTs of different anticoagulation strategies in patients with COVID-19
| Ongoing RCTs of different anticoagulation strategies in patients with COVID-19 | |||
|---|---|---|---|
| RCT | Estimated sample size | Interventions | Estimated completion date |
| ICU | |||
| NCT04362085 | 462 | Therapeutic (LMWH or UFH) vs. Prophylactic-Dose (LMWH, UFH or fondaparinux) | December 2020 |
| NCT04367831 | 100 | Intermediate vs. Prophylactic-Dose with LMWH or UFH | April 2021 |
| Acute Respiratory Distress Syndrome (ARDS) | |||
| NCT04445935 | 100 | Bivalirudin Injection vs. Standard treatment in COVID-19 ARDS | March 2021 |
| NCT04357730 | 60 | Fibrinolytic Therapy (Alteplase) to Treat ARDS | November 2020 |
| ICU and non-ICU | |||
| NCT04359277 | 1000 | Intermediate vs. Prophylactic-Dose with Enoxaparin with LMWH or UFH | April 2021 |
| NCT04344756 | 808 | Therapeutic (Tinzaparin or UFH) vs. Prophylactic-Dose (Enoxaparin, Tinzaparin, dalteparin or UFH) | September 2020 |
| NCT04373707 | 602 | Low Prophylactic vs. Weight-Adjusted Prophylactic Dose of LWMH | October 2020 |
| NCT04394377 | 600 | Therapeutic (Rivaroxaban 20 mg/ daily or enoxaparin or UFH) vs. Prophylactic-Dose (Enoxaparin) | December 2020 |
| NCT04351724 | 500 | Rivaroxaban 5 mg BID vs. Prophylactic-Dose of LMWH | December 2020 |
| NCT04416048 | 400 | Rivaroxaban vs. LMWH or UFH at prophylactic doses | May 2021 |
| NCT04401293 | 308 | Therapeutic (LMWH) vs. Prophylactic/Intermediate Dose (LMWH or UFH) in high risk COVID-19 patients (SIC score > 4 OR D-dimer > 4.0 X ULN) | April 2021 |
| NCT04377997 | 300 | Therapeutic vs. Prophylactic-Dose with Enoxaparin or UFH and D-dimer > 1.5 g/mL | January 2022 |
| NCT04345848 | 200 | Therapeutic vs. Prophylactic-Dose with Enoxaparin | November 2020 |
| NCT04406389 | 186 | Therapeutic vs. intermediate dose with LMWH or UFH or fondaparinux | June 2021 |
| Non-ICU | |||
| NCT04366960 | 2712 | Intermediate vs. Prophylactic-Dose with Enoxaparin | November 2020 |
| NCT04444700 | 462 | Therapeutic Enoxaparin vs. Prophylactic-Dose with Enoxaparin or UFH | December 2020 |
| NCT04360824 | 170 | Intermediate vs. Prophylactic-Dose with Enoxaparin | April 2021 |
| Ambulatory patients | |||
| NCT04400799 | 1000 | Prophylactic dose of Enoxaparin 4000 IU antiXa activity vs. control | April 2021 |
| Children | |||
| NCT04354155 | 38 | Safety, dose-requirements, and exploratory efficacy of enoxaparin BID | October 2022 |
Covid-19 coronavirus disease 2019, ICU intensive care unit, LMWH low-molecular-weight heparin, RCTs randomized controlled trials; VTE venous thromboembolism
Fig. 3.
A proposal for COVID-19 coagulopathy specific risk factors and dedicated trials. Covid-19 coronavirus disease 2019, CT computed tomography, ICU intensive care unit, RCTs randomized controlled trials, VTE venous thromboembolic events
All studies of haemostasis have identified a prothrombotic state in COVID-19 [46]. Thachil et al. lately proposed a new staging classification characterizing COVID-19 associated hemostatic abnormalities (CAHA) [3]. The authors proposed that the spectrum of CAHA first represents a localized phenomenon of hypercoagulability in the lung, which then becomes extensive and systemic (increased D-Dimer level, reduced platelet count and prolonged PT) if not treated adequately. We promptly confirmed a stepwise increase in VTE rates and excess mortality and/or transfer to ICU for each increment in stage of CAHA among 150 non-ICU patients with COVID-19 [47]. Hence, we proposed a CAHA threshold ≥ 2 to consider early aggressive strategies including early VTE imaging screening, “stepped-up” anticoagulant dose regimens and critical care support. VTE risk stratification scheme and prospective RCTs are needed to determine whether intermediate or treatment-dose anticoagulant confer both survival benefit and decreased VTE incidence according to biomarkers threshold including the use of very elevated D-dimer levels and inflammatory markers in hospitalized patients with COVID-19.
Hyperinflammation has been advocated as a key component triggering thromboinflammation and subsequent increased risk of VTE [48, 49]. The first event after inhalation of SARS coronaviruses is invasion of type II alveolar cells in the lung. Viral cell entry triggers the host’s immune response and an inflammatory cascade. While viral multiplication and localized inflammation in the lung is the norm, severe COVID-19 patients will develop an overproduction of proinflammatory cytokines resulting in a cytokine storm [50]. On top of anti-inflammatory or antiviral effects, current therapeutic strategies (e.g. intravenous immunoglobulin, selective cytokine blockade etc.) [51] may have indirect antithrombotic effects and modulate the risk of VTE.
Lung and pulmonary thrombosis have an intimate relationship in COVID-19. The first hint came from accumulating evidence of published necropsy series with the prominence of clot, widespread micro-thrombi and occlusion of alveolar capillaries [26, 52–54]. More evidence followed with proof of pulmonary endotheliitis in the time course of SARS-CoV-2 infection [55]. A distinctive pattern of pulmonary intravascular coagulopathy has finally been proposed [56, 57]. The current consensus puts the lungs as the epicenter for the hemostatic and inflammatory issues in COVID-19. Desborough et al. nicely addressed this issue providing evidence that many of the acute pulmonary embolism are indeed described on CT pulmonary angiograms as segmental or subsegmental and that these thromboses may be immunothromboses due to local inflammation, rather than thromboembolic disease [58]. First localized to the lung, then extensive and finally systemic if not treated, the phenomenon of pulmonary intravascular coagulopathy in COVID-19 pneumonia translates in clinical practice with higher oxygen requirement and extensive lung injuries assessed by chest CT [18, 47, 59].
Several anticoagulant regimens are been currently investigated in patients with COVID-19. Systematic screening for marked prothrombotic state, hyperinflammation and the extent of lung injury as determined by chest CT could be helpful to guide individualized thromboprophylaxis in COVID-19 patients.
Abbreviations
- CA
Chronic therapeutic anticoagulation
- BID
Twice-daily
- BMI
Body mass index
- COVID-19
Coronavirus disease 2019
- CT
Computed tomography
- DOAC
Direct oral anticoagulant
- DVT
Deep vein thrombosis
- ICU
Intensive care unit
- IT
Thromboprophylaxis with intermediate dose of LMWH/ UFH
- LMWH
Low molecular weight heparin
- N/A
Not available
- PE
Pulmonary embolism
- RCTs
Randomized controlled trials
- SD
Routine thromboprophylaxis with standard dose of UFH or LMWH
- TD
Thromboprophylaxis with therapeutic dose
- UFH
Unfractionated heparin
- VTE
Venous thromboembolism
Author contributions
Drafting of the manuscript, review, and editing, BM; drafting of the manuscript and critical revision for important intellectual content, AT; drafting of the manuscript, review, and critical revision for important intellectual content, AC; drafting of the manuscript, and critical revision for important intellectual content, KM; drafting of the manuscript, and critical revision for important intellectual content, LJ; drafting of the manuscript, and critical revision for important intellectual content, review, and supervision, OM.
Funding
No funding source in the writing of the manuscript and/or the decision to submit it for publication.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Informed Consent
All the authors take responsibility for all aspects of the reliability and freedom from bias of the data presented and their discussed interpretation. All authors have read and approved submission of the manuscript.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Marchandot B, Sattler L, Jesel L, Matsushita K, Schini-Kerth V, Grunebaum L, Morel O. COVID-19 related coagulopathy: a distinct entity? A review. J Clin Med. 2020;9:1651. doi: 10.3390/jcm9061651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.The Lancet Haematology COVID-19 coagulopathy: an evolving story. Lancet Haematol. 2020 doi: 10.1016/S2352-3026(20)30151-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thachil J, Cushman M, Srivastava A. A proposal for staging COVID-19 coagulopathy. Res Pract Thromb Haemost. 2020 doi: 10.1002/rth2.12372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wagers SS, Norton RJ, Rinaldi LM, Bates JH, Sobel BE, Irvin CG. Extravascular fibrin, plasminogen activator, plasminogen activator inhibitors, and airway hyperresponsiveness. J Clin Invest. 2004;114(1):104–111. doi: 10.1172/JCI19569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thachil J. All those D-dimers in COVID-19. J Thromb Haemost. 2020 doi: 10.1111/jth.14939.10.1111/jth.14939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Klok FA, Kruip M, van der Meer N, Arbous MS, Gommers D, Kant KM, Kaptein F, van Paassen J, Stals M, Huisman MV, Endeman H. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145–147. doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Helms J, Tacquard C, Severac F, Leonard-Lorant I, Ohana M, Delabranche X, Merdji H, Clere-Jehl R, Schenck M, Fagot Gandet F, Fafi-Kremer S, Castelain V, Schneider F, Grunebaum L, Anglés-Cano E, Sattler L, Mertes PM, Meziani F, CRICS TRIGGERSEP Group (Clinical Research in Intensive Care and Sepsis Trial Group for Global Evaluation and Research in Sepsis) High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study. Intens Care Med. 2020;46(6):1089–1098. doi: 10.1007/s00134-020-06062-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maatman TK, Jalali F, Feizpour C, Douglas A, 2nd, McGuire SP, Kinnaman G, Hartwell JL, Maatman BT, Kreutz RP, Kapoor R, Rahman O, Zyromski NJ, Meagher AD. Routine venous thromboembolism prophylaxis may be inadequate in the hypercoagulable state of severe coronavirus disease 2019. Crit Care Med. 2020 doi: 10.1097/CCM.0000000000004466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Poissy J, Goutay J, Caplan M, Parmentier E, Duburcq T, Lassalle F, Jeanpierre E, Rauch A, Labreuche J, Susen S, Haemostasis LICU, COVID-19 group Pulmonary embolism in COVID-19 patients: awareness of an increased prevalence. Circulation. 2020 doi: 10.1161/CIRCULATIONAHA.120.047430. [DOI] [PubMed] [Google Scholar]
- 10.Cui S, Chen S, Li X, Liu S, Wang F. Prevalence of venous thromboembolism in patients with severe novel coronavirus pneumonia. J Thromb Haemost. 2020 doi: 10.1111/jth.14830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Middeldorp S, Coppens M, van Haaps TF, Foppen M, Vlaar AP, Müller M, Bouman C, Beenen L, Kootte RS, Heijmans J, Smits LP, Bonta PI, van Es N. Incidence of venous thromboembolism in hospitalized patients with COVID-19. J Thromb Haemost. 2020 doi: 10.1111/jth.14888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lodigiani C, Iapichino G, Carenzo L, Cecconi M, Ferrazzi P, Sebastian T, Kucher N, Studt JD, Sacco C, Alexia B, Sandri MT, Barco S, Humanitas COVID-19 Task Force Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb Res. 2020;191:9–14. doi: 10.1016/j.thromres.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ren B, Yan F, Deng Z, Zhang S, Xiao L, Wu M, Cai L. Extremely high incidence of lower extremity deep venous thrombosis in 48 patients with severe COVID-19 in Wuhan. Circulation. 2020 doi: 10.1161/CIRCULATIONAHA.120.047407. [DOI] [PubMed] [Google Scholar]
- 14.Grillet F, Behr J, Calame P, Aubry S, Delabrousse E. Acute pulmonary embolism associated with COVID-19 pneumonia detected by pulmonary CT angiography. Radiology. 2020 doi: 10.1148/radiol.2020201544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Llitjos JF, Leclerc M, Chochois C, Monsallier JM, Ramakers M, Auvray M, Merouani K. High incidence of venous thromboembolic events in anticoagulated severe COVID-19 patients. J Thromb Haemost. 2020 doi: 10.1111/jth.14869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Longchamp A, Longchamp J, Manzocchi-Besson S, Whiting L, Haller C, Jeanneret S, Godio M, Martinez JJG, Bonjour T, Caillat M, Maitre G, Thaler JM, Pantet R, Donner V, Dumoulin A, Emonet S, Greub G, Friolet R, Robert-Ebadi H, Righini M, Sanchez B, Delayoe J. Venous thromboembolism in critically ill patients with Covid-19: results of a screening study for deep vein thrombosis. JTH. 2020 doi: 10.1002/rth2.12376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Galeano-Valle F, Oblitas CM, Ferreiro-Mazón MM, Alonso-Muñoz J, Del Toro-Cervera J, Demelo-Rodríguez P. Antiphospholipid antibodies are not elevated in patients with severe COVID-19 pneumonia and venous thromboembolism. Thromb Res. 2020 doi: 10.1016/j.thromres.2020.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Trimaille A, Curtiaud A, Marchandot B, Matsushita K, Sato C, Leonard-Lorant I, Sattler L, Grunebaum L, Ohana M, Von Hunolstein JJ, Andre E, Goichot B, Danion F, Kaeuffer C, Poindron C, Ohlmann P, Jesel L, Morel O (2020) Venous thromboembolism in non-critically ill patients with COVID-19 infection. Thrombosis Res. 10.1016/j.thromres.2020.07.033 [DOI] [PMC free article] [PubMed]
- 19.Demelo-Rodríguez P, Cervilla-Muñoz E, Ordieres-Ortega L, Parra-Virto A, Toledano-Macías M, Toledo-Samaniego N, García-García A, García-Fernández-Bravo I, Ji Z, de-Miguel-Diez J, Álvarez-Sala-Walther LA, Del-Toro-Cervera J, Galeano-Valle F. Incidence of asymptomatic deep vein thrombosis in patients with COVID-19 pneumonia and elevated D-dimer levels. Thromb Res. 2020;192:23–26. doi: 10.1016/j.thromres.2020.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang L, Feng X, Zhang D, Jiang C, Mei H, Wang J, Zhang C, Li H, Xia X, Kong S, Liao J, Jia H, Pang X, Song Y, Tian Y, Wang B, Wu C, Yuan H, Zhang Y, Li Y, Sun W, Zhang Y, Zhu S, Wang S, Xie Y, Ge S, Zhang L, Hu Y, Xie M. Deep vein thrombosis in hospitalized patients with coronavirus disease 2019 (COVID-19) in Wuhan, China: prevalence, risk factors, and outcome. Circulation. 2020 doi: 10.1161/CIRCULATIONAHA.120.046702. [DOI] [PubMed] [Google Scholar]
- 21.Artifoni M, Danic G, Gautier G, Gicquel P, Boutoille D, Raffi F, Néel A, Lecomte R. Systematic assessment of venous thromboembolism in COVID-19 patients receiving thromboprophylaxis: incidence and role of D-dimer as predictive factors. J Thromb Thrombolysis. 2020;25:1–6. doi: 10.1007/s11239-020-02146-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Voicu S, Bonnin P, Stépanian A, Chousterman BG, Le Gall A, Malissin I, Deye N, Siguret V, Mebazaa A, Mégarbane B. High prevalence of deep vein thrombosis in mechanically ventilated COVID-19 patients. J Am Coll Cardiol. 2020 doi: 10.1016/j.jacc.2020.05.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nahum J, Morichau-Beauchant T, Daviaud F, Echegut P, Fichet J, Maillet JM, Thierry S. Venous thrombosis among critically ill patients with coronavirus disease 2019 (COVID-19) JAMA Netw Open. 2020;3(5):e2010478. doi: 10.1001/jamanetworkopen.2020.10478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Santoliquido A, Porfidia A, Nesci A, De Matteis G, Marrone G, Porceddu E, Cammà G, Giarretta I, Fantoni M, Landi F, Gasbarrini A, Pola R. Incidence of deep vein thrombosis among non-ICU patients hospitalized for COVID-19 despite pharmacological thromboprophylaxis. JTH 10.1111/JTH.14992 [DOI] [PMC free article] [PubMed]
- 25.Fauvel C, Weizman O, Trimaille A, Mika D, Pommier T, Pace N, et al. Pulmonary embolism in COVID-19 patients: a French multicentre cohort study. Eur Heart J. 2020 doi: 10.1093/eurheartj/ehaa500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Benzakoun J, Hmeydia G, Delabarde T, Hamza L, Meder JF, Ludes B, Mebazaa A. Excess out-of-hospital deaths during COVID-19 outbreak: evidence of pulmonary embolism as a main determinant. Eur Heart Fail. 2020 doi: 10.1002/ejhf.1916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DS, et al. China medical treatment expert group for Covid-19. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18:844–847. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yin S, Huang M, Li D, Tang N. Difference of coagulation features between severe pneumonia induced by SARS-CoV2 and non-SARS-CoV2. J. Thromb. Thrombolysis. 2020 doi: 10.1007/s11239-020-02105-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chong PY, Chui P, Ling AE, Franks TJ, Tai DY, Leo YS, Kaw GJ, Wansaicheong G, Chan KP, Ean Oon LL, Teo ES, Tan KB, Nakajima N, Sata T, Travis WD. Analysis of deaths during the severe acute respiratory syndrome (SARS) epidemic in Singapore: challenges in determining a SARS diagnosis. Arch Pathol Lab Med. 2004;128(2):195–204. doi: 10.1043/1543-2165(2004)128<195:AODDTS>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 31.Giannis D, Ziogas IA, Gianni P. Coagulation disorders in coronavirus infected patients: COVID-19, SARS-CoV-1, MERS-CoV and lessons from the past. J Clin Virol. 2020 doi: 10.1016/j.jcv.2020.104362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Obi AT, Tignanelli CJ, Jacobs BN, Arya S, Park PK, Wakefield TW, Henke PK, Napolitano LM. Empirical systemic anticoagulation is associated with decreased venous thromboembolism in critically ill influenza A H1N1 acute respiratory distress syndrome patients. J Vasc Surg. 2019;7(3):317–324. doi: 10.1016/j.jvsv.2018.08.010. [DOI] [PubMed] [Google Scholar]
- 33.Levi M, Schultz M, van der Poll T. Disseminated intravascular coagulation in infectious disease. Semin Thromb Hemost. 2010;36(4):367–377. doi: 10.1055/s-0030-1254046. [DOI] [PubMed] [Google Scholar]
- 34.Wang T, Chen R, Liu C, Liang W, Guan W, Tang R, Tang C, Zhang N, Zhong N, Li S. Attention should be paid to venous thromboembolism prophylaxis in the management of COVID-19. Lancet Haemat. 2020;7(5):e362–e363. doi: 10.1016/S2352-3026(20)30109-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Thachil J, Tang N, Gando S, Falanga A, Cattaneo M, Levi M, Clark C, Iba T. ISTH interim guidance on recognition and management of coagulopathy in COVID-19. J Thromb Haemost. 2020;18:1023–1026. doi: 10.1111/jth.14810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bikdeli B, Madhavan MV, Jimenez D, Chuich T, Dreyfus I, Driggin E, Nigoghossian CD, Ageno W, Madjid M, Guo Y et al (2020) COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up. J Am Coll Cardiol [DOI] [PMC free article] [PubMed]
- 37.Spyropoulos AC, Levy JH, Ageno W, Connors JM, Hunt BJ, Iba T, Levi M, Samama CM, Thachil J, Giannis D, Douketis JD. Subcommittee on Perioperative, Critical Care Thrombosis, Haemostasis of the Scientific, Standardization Committee of the International Society on Thrombosis, Haemostasis. Scientific and Standardization Committee Communication: Clinical Guidance on the Diagnosis, Prevention and Treatment of Venous Thromboembolism in Hospitalized Patients with COVID-19. J Thromb Haemost. 2020 doi: 10.1111/jth.14929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tang N, Bai H, Chen X, Gong J, Li D, Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020 doi: 10.1111/jth.14817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Porfidia A, Pola R. Venous thromboembolism in COVID-19 patients. J Thromb Haemost. 2020 doi: 10.1111/jth.14842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.PROTECT Investigators for the Canadian Critical Care Trials Group and the Australian and New Zealand Intensive Care Society Clinical Trials Group. Cook D, Meade M, Guyatt G, Walter S, Heels-Ansdell D, Warkentin TE, Zytaruk N, Crowther M, Geerts W, Cooper DJ, Vallance S, Qushmaq I, Rocha M, Berwanger O, Vlahakis NE. Dalteparin versus unfractionated heparin in critically ill patients. N Engl J Med. 2011;364(14):1305–1314. doi: 10.1056/NEJMoa1014475. [DOI] [PubMed] [Google Scholar]
- 41.Cade JF. High risk of the critically ill for venous thromboembolism. Crit Care Med. 1982;10:448–450. doi: 10.1097/00003246-198207000-00006. [DOI] [PubMed] [Google Scholar]
- 42.Kapoor M, Kupfer YY, Tessler S. Subcutaneous heparin prophylaxis significantly reduces the incidence of venous thromboembolic events in the critically ill [abstract] Crit Care Med. 1999;27:A69. doi: 10.1097/00003246-199912001-00165. [DOI] [Google Scholar]
- 43.Fraisse F, Holzapfel L, Couland JM, Simonneau G, Bedock B, Feissel M, Herbecq P, Pordes R, Poussel JF, Roux L. Nadroparin in the prevention of deep vein thrombosis in acute decompensated COPD. The Association of Non-University Affiliated Intensive Care Specialist Physicians of France. Am J Respir Crit Care Med. 2000;161(4):1109–1114. doi: 10.1164/ajrccm.161.4.9807025. [DOI] [PubMed] [Google Scholar]
- 44.Moores LK, Tritschler T, Brosnahan S, Carrier M, Collen JF, Doerschug K, Holley AB, Jimenez D, LeGal G, Rali P, Wells P. Prevention, diagnosis and treatment of venous thromboembolism in patients with COVID-19: CHEST Guideline and Expert Panel Report. Chest. 2020 doi: 10.1016/j.chest.2020.05.559. [DOI] [PubMed] [Google Scholar]
- 45.Thachil J, Juffermans NP, Ranucci M, Connors JM, Warkentin TE, Ortel TL, Levi M, Iba T, Levy JH. ISTH DIC subcommittee communication on anticoagulation in COVID-19. J Thromb Haemost. 2020 doi: 10.1111/JTH.15004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Polimeni A, Leo I, Spaccarotella C, Mongiardo A, Sorrentino S, Sabatino J, Rosa SD, Indolfi C. Prognostic impact of coagulopathy in patients with COVID-19: a meta-analysis of 35 studies and 6427 patients. Res Sq. 2020 doi: 10.21203/rs.3.rs-31142/v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Marchandot B, Trimaille A, Curtiaud A, Carmona A, Matsushita K, Sato C, Leonard-Lorant I, Sattler L, Grunebaum L, Ohana M, Ohlmann P, Jesel L, Morel O. Staging COVID-19 coagulopathy in non-critically ill patient (in review)
- 48.Siddiqi HK, Mehra MR. COVID-19 illness in native and immunosuppressed states: a clinical-therapeutic staging proposal. J Heart Lung Transplant. 2020;39(5):405–407. doi: 10.1016/j.healun.2020.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Connors JM, Levy JH. Thromboinflammation and the hypercoagulability of COVID-19. J Thromb Haemost. 2020 doi: 10.1111/jth.14849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jose RJ, Manuel A. COVID-19 cytokine storm: the interplay between inflammation and coagulation. Lancet Respir Med. 2020 doi: 10.1016/S2213-2600(20)30216-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bikdeli B, Madhavan MV, Gupta A, Jimenez D, Burton JR, Der Nigoghossian C, Chuich T, Nouri SN, Dreyfus I, Driggin E, Sethi S, Sehgal K, Chatterjee S, Ageno W, Madjid M, Guo Y, Tang LV, Hu Y, Bertoletti L, Giri J, Global COVID-19 Thrombosis Collaborative Group et al. Pharmacological Agents Targeting Thromboinflammation in COVID-19: Review and Implications for Future Research. Thromb Haemost. 2020 doi: 10.1055/s-0040-1713152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dolhnikoff M, Duarte-Neto AN, de Almeida Monteiro RA, Ferraz Da Silva LF, Pierre de Oliveira E, Nascimento Saldiva PH, Mauad T, Marcia Negri E. Pathological evidence of pulmonary thrombotic phenomena in severe COVID-19. J Thromb Haemost. 2020 doi: 10.1111/jth.14844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wichmann D, Sperhake JP, Lütgehetmann M, Steurer S, Edler C, Heinemann A, Heinrich F, Mushumba H, Kniep I, Schröder AS, Burdelski C, de Heer G, Nierhaus A, Frings D, Pfefferle S, Becker H, Bredereke-Wiedling H, de Weerth A, Paschen HR, Sheikhzadeh-Eggers S, et al. Autopsy findings and venous thromboembolism in patients with COVID-19. Ann Intern Med. 2020 doi: 10.7326/M20-2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ackermann M, Verleden SE, Kuehnel M, Haverich A, Welte T, Laenger F, Vanstapel A, Werlein C, Stark H, Tzankov A, Li WW, Li VW, Mentzer SJ, Jonigk D. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in Covid-19. N Engl J Med. 2020 doi: 10.1056/NEJMoa2015432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, Mehra MR, Schuepbach RA, Ruschitzka F, Moch H. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395:1417–1418. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.McGonagle D, O’Donnell JS, Sharif K, Emery P, Bridgewood C. Immune mechanisms of pulmonary intravascular coagulopathy in COVID-19 pneumonia. Lancet Rheumatol. 2020 doi: 10.1016/S2665-9913(20)30121-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ciceri F, Beretta L, Scandroglio AM, Colombo S, Landoni G, Ruggeri A, Peccatori J, D'Angelo A, De Cobelli F, Rovere-Querini P, Tresoldi M, Dagna L, Zangrillo A (2020) Microvascular COVID-19 lung vessels obstructive thromboinflammatory syndrome (MicroCLOTS): an atypical acute respiratory distress syndrome working hypothesis. Crit Care Resusc [DOI] [PMC free article] [PubMed]
- 58.Desborough MJR, Doyle AJ, Griffiths A, Retter A, Breen KA, Hunt BJ. Image-proven thromboembolism in patients with severe COVID-19 in a tertiary critical care unit in the United Kingdom. Thromb Res. 2020 doi: 10.1016/j.thromres.2020.05.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Morel O, Marchandot B, Jesel L, Sattler L, Trimaille L, Curtiaud A, Ohana M, Fafi-Kremer S, Schini-Kerth V, Grunebaum L, Freyssinet JM. Microparticles in Covid-19 as a link between lung injury and thrombosis (in review) [DOI] [PMC free article] [PubMed]