Abstract
Aim
To asses if telemedicine with telemonitoring is a clinically useful and safe tool for monitoring patients with COVID-19.
Methods
A prospective observational study of patients with COVID-19 diagnosed via a positive PCR test who were considered high-risk and who were monitored with telemedicine and telemonitoring in the Lugo Healthcare Area between March 17th and April 17th, 2020, was conducted. Two groups of patients were included: those in outpatient monitoring from the beginning and those in outpatient monitoring following hospital discharge. Every patient completed a clinical questionnaire with his or her temperature once per day and oxygen saturation levels three times per day. Proactive monitoring was done by getting in touch with every patient at least once a day.
Results
A total of 313 patients (52.4% female) with a mean age of 60.9 (SD 15.9) years were included. Two patients refused to participate in the program. Finally, 224 were monitored from the beginning and 89 patients were monitored after discharged. In the first group, 38 (16.90%) were referred to the Emergency department on 43 occasions; 18 (8.03%) were hospitalized, and two died. There were no deaths or lifethreatening at home. Including the patients monitored after hospitalization, monitoring was performed in 304 cases. One patient was readmited (0.32%) and another left the program (0.32%). The mean time of monitoring was 11.64 (SD 3.58) days and 224 (73.68%) patients were discharged during the 30 days the study lasted.
Conclusions
Our data suggest that telemedicine with at-home telemonitoring, when used proactively, allows for clinically useful and safe monitoring of high-risk patients with COVID-19.
Keywords: Telemedicine, COVID-19, Case management, COVID-19 management
Abstract
Objetivo
Evaluar si la telemedicina con telemonitorización es una herramienta clínicamente útil y segura para el seguimiento de pacientes con COVID-19.
Métodos
Estudio observacional prospectivo de los pacientes con diagnóstico de COVID-19 por PCR positiva y considerados de alto riesgo que se siguieron con telemedicina y telemonitorización en el Área Sanitaria de Lugo entre el 17 de marzo y el 17 de abril del 2020. Se incluyeron 2 grupos de pacientes: seguimiento ambulatorio desde el inicio y tras el alta hospitalaria. Cada paciente remitió un cuestionario clínico al día con su temperatura y saturación de oxígeno 3 veces al día. El seguimiento fue proactivo, contactando con todos los pacientes al menos una vez al día.
Resultados
Se incluyó a 313 pacientes (52,4% mujeres) con edad media 60,9 (DE 15,9) años. Otros 2 pacientes rehusaron entrar en el programa. Desde el inicio, se siguió ambulatoriamente a 224 pacientes y a 89 pacientes tras su alta hospitalaria. Entre los primeros, 38 (16,90%) se remitieron a Urgencias en 43 ocasiones con 18 (8,03%) ingresos y 2 fallecidos. En los domicilios no hubo fallecimientos ni urgencias vitales. Incluyendo a los pacientes tras hospitalización, el seguimiento se realizó en 304 casos. Un paciente reingresó (0,32%) y otro abandonó (0,32%). El tiempo medio de seguimiento fue 11,64 (DE 3,58) días y en los 30 días del estudio 224 (73,68%) pacientes fueron dados de alta.
Conclusiones
Nuestros datos sugieren que la telemedicina con telemonitorización domiciliaria, utilizada de forma proactiva, permite un seguimiento clínicamente útil y seguro en pacientes con COVID-19 de alto riesgo.
Palabras clave: Telemedicina, COVID-19, Gestión caso, Gestión COVID-19
The COVID-19 pandemic caused by SARS-CoV-2, which has progressed rapidly and has had tragic consequences, has caused a worldwide public health emergency.1, 2 The fight against this disease, whose epidemiological, clinical, and prognostic characteristics are still being studied,3 is making it necessary to modify manners of providing care, which includes substituting some face-to-face consultations with distance consultations.4
Telemedicine, in its different forms, has been used to diagnose, treat, or monitor patients with acute infectious diseases, such as community-acquired pneumonia; upper respiratory tract, soft tissue, or urinary tract infections; or bacterial endocarditis.5, 6 It is believed that it can also be of use in a crisis like the current one.4, 7 However, the information currently available on the possible benefits or its safety is very limited.
In recent years, the Galician Health Service has developed a tool (TELEA) that is integrated into the electronic medical record and is able to perform at-home telemedicine and telemonitoring. It allows for telematic monitoring and for anticipating possible episodes of exacerbation of a disease. Since 2015, it has been used in patients with heart failure. It has not only demonstrated its clinical utility, but has also been very well received by patients and their family members.8
Approximately 80% of patients with COVID-19 present with a mild or moderate clinical course and habitually require treatment of symptoms. 20% of patients, especially those who are elderly or who have comorbidities, will require hospitalization due to severity criteria.2, 3 The use of telemedicine and telemonitoring would allow for the clinical evaluation of patients who present with a mild course and are isolated at home, thus avoiding exposing healthcare personnel to risks.
In this study, we will evaluate the efficacy of telemedicine and telemonitoring in detecting potentially severe cases of COVID-19 among patients cared for while isolating at home.
Patients and methods
Design. This work is a prospective observational study of patients with COVID-19 diagnosed by a positive PCR test and in at-home monitoring with telemedicine and telemonitoring.
Study scope and period. The study was conducted in the Lugo healthcare area between March 17 and April 17, 2020. This healthcare area provides coverage to the 345,000 residents of Lugo and has three hospitals (Da Mariña Hospital in the north, Lucus Augusti University Hospital in the central area, and Monforte Hospital in the south).
In recent years, the Galician Health Service has developed the TELEA tool, which is integrated into the electronic medical record and is able to perform at-home telemedicine and telemonitoring. With this tool, any patient who has provided the pertinent permission can send information in a pre-established format to their own electronic medical record. It is accessible to healthcare personnel from any point in the Galician healthcare network. Information can be evaluated in real-time and action can be taken in consequence.
By adapting an existing model used for heart failure8 to acute diseases, TELEA has been used for the follow-up and monitoring of patients with COVID-19 in all the Galician healthcare areas since March 3, 2020. In the Lugo healthcare area, teams of professionals were created (medical and nursing department personnel) from different departments (internal medicine, home hospitalization, allergology, rehabilitation, etc.). As nobody had previous experience in handling this tool, basic instructions were given and a detailed protocol was established, with criteria and rules for monitoring.
Participants. All patients with confirmed COVID-19 in outpatient monitoring or who were possible candidates for it were classified into groups according to their risk, with different monitoring programs established. Two groups considered to be at greater risk were selected to be included in this program:
-
1.
Adult patients who are not institutionalized; who have a positive PCR test; who are symptomatic; and who, in a previous medical evaluation, have been deemed able to continue at-home treatment despite being considered high-risk. Patients were included in this group if they presented with at least one of the following characteristics: age over 60 years, pregnancy, hypertension, diabetes mellitus, known cardiopathy of any nature, chronic obstructive pulmonary disease, chronic kidney disease, or immunosuppresion of any origin. In addition, people with symptoms who live in close quarters with patients were included after an evaluation of the criteria, at least while they did not have a microbiological study available.
Patients in this group communicated with the monitoring team every day of the week at 8:00 a.m.
-
2.
Patients with known disease after hospital discharge due to COVID-19. These patients were included in the program at the time of hospital discharge.
The exclusion criteria were: (1) refusal on the part of the patient to monitoring via this method; (2) not having a smartphone, and (3) presence of clinical alarm signs in the initial interview that made it necessary to refer the patient to the Emergency Department.
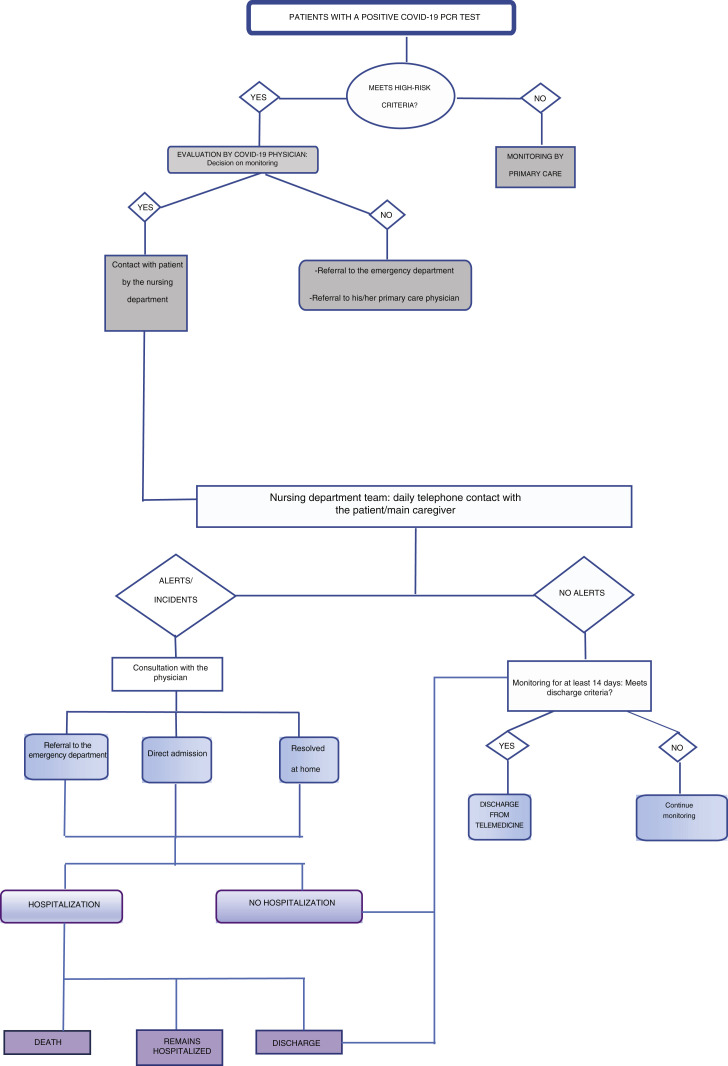
In Fig. 1 , the manner in which the process was carried out is shown graphically. When faced with a possible COVID-19 case, a physician contacts the patient via telephone, explaining the objectives, characteristics, and conditions of the monitoring. The most relevant clinical aspects are collected and, if the patient does not present with alarm signs, oral informed consent is requested. After confirmation, the physician notifies the nursing department personnel of the new enrollment. A member of this team contacts the patient to provide them with a user name and password to access the platform webpage, explaining how to enter the biomeasurements and how to answer the questionnaire. In addition, they are notified that a courier will deliver written instructions, a pulse oximeter, and a thermometer to their home that same day. The materials are collected at the end of monitoring.
Figure 1.
Patient monitoring work flow.
The nursing department team periodically reviews the information received (daily questionnaire, body temperature, and oxygen saturation three times per day) and proactively contacts all the patients via telephone, prioritizing according to the information received. As a general rule, they contact the patient at least once per day or more, if the clinical situation required it.
In addition, the patient has a telephone contact number that is operational from 8:00 a.m. to 9:30 p.m. In the event of incidents (changes in biomeasurements or clinical situation as assessed by the questionnaire [Table 1 ]), the nursing department contacts the patient and evaluates whether it is possible to solve the problem via telephone. If it is not possible, a physician will evaluate the situation and decide if it is necessary to refer him or her to the hospital emergency department. In this case, this physician is the person who contacts the department and explains the reasons why he or she advises referral.
Table 1.
Clinical questionnaire and biomeasurement alerts used in patient evaluation.
| Survey for patients with respiratory pathology | ||
| Have you noted more fatigue? | Yes | No |
| Have you noted more cough? | Yes | No |
| Have you noted changes in the color or amount of expectoration? | Yes | No |
| Referral due to alarm criteria | ||
| Body temperature over 38 °C which does not remit with antipyretics | ||
| Oxygen saturation less than 92% maintained with and without dyspnea | ||
| Crisis or increase in dyspnea on minimal exertion or at rest | ||
| Pleuritic-type costal pain or chest pain | ||
Outcomes. During the monitoring, it is considered that a patient can be discharged if they meet the following conditions: (1) at least 14 days have passed since the onset of symptoms; (2) the patient does not have symptoms or they are residual; (3) the patient has been afebrile in at least the last 72 h, and (4) no other medical problem or complication is observed.
To evaluate the results, two types of outcome measurements were used:
-
1.
Process outcomes: number of patients who completed monitoring with vital signs monitoring and daily telephone calls, dropouts during the program, and number of days in which the connection was erroneous or if there were serious technological difficulties.
-
2.
Results outcomes: at-home death, cases referred to the Emergency Department, in-hospital mortality among those referred for admission, and number of discharges after telemedicine with telemonitoring.
Ethical and legal aspects. The data are included in a registry approved by the Center's Research Ethics Committee. For this study, the following variables were collected: origin of the patient; date of entry into the program; date of referral to the Emergency Department and admission, if applicable; and the final result of each of the evaluations. The sources of information included both the data from the monitoring of each patient and the records from the various hospital centers in the area.
Statistical methods. In creating the patient flow figure, the habitual descriptive statistics techniques were used. In order to compare two means, Student's T test was used after evaluating homoscedasticity. To establish the time of follow-up, the Kaplan–Meier method was used, considering April 17, 2020 as the censor date. The SPSS v18 (SPSS Inc., Chicago, IL, USA) statistical program was used for the analysis.
Results
Participants. In the period indicated, a total of 765 cases confirmed by PCR were detected. Of them, 432 were monitored in primary care and the remaining 313 (40.91%) were included in this study (224 from outpatient tests and 89 after hospital discharge).
In terms of sex, 149 (47.6%) were males and 164 (52.4%) were women. The mean age was 60.9 (SD 15.9) years, with a range of 18–92 years. There were no differences in age according to sex (61.60 [SD 14.8] vs. 60.18 [SD 16.9], respectively; p = NS). The general characteristics of the patients are shown in Table 2 .
Table 2.
Characteristics of patients monitored with telemedicine and telemonitoring.
| Patients monitored | |
|---|---|
| (N = 313) | |
| Sex (male) | 149 (47.6%) |
| Age, years | |
| Mean age (SD) | 60.9 (15.9) years |
| Range | 18–92 |
| Age groups, years | |
| 18–40 | 34 (11.4%) |
| 41–60 | 97 (30.7%) |
| 61–70 | 89 (28.3%) |
| 71–80 | 65 (20.8%) |
| 81–90 | 25 (8.1%) |
| ≥91 | 3 (0.7%) |
| Time from onset of symptoms to start of telemedicine (calculated in 167 cases), mean (SD) | 4.6 (3.8) days |
| Hypertension | 119 (38%) |
| Diabetes | 78 (24.9%) |
| Cardiovascular disease | 74 (23.6%) |
| Neoplasia | 63 (20.1%) |
| Heart failure | 29 (9.3%) |
| Obesity | 28 (8.9%) |
| Chronic renal disease | 23 (7.3%) |
| Asthma | 22 (7%) |
| Chronic liver disease | 20 (6.4%) |
| Chronic obstructive pulmonary disease | 18 (5.7%) |
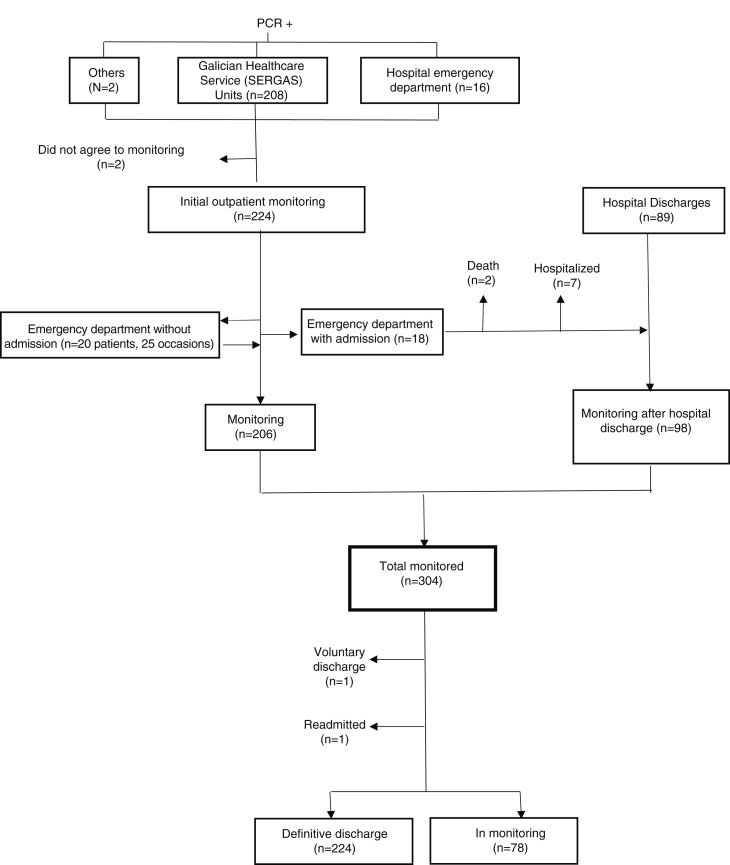
Flow of patients. In Fig. 2 , the origin of patients, their flow through the different care areas, and the results of the monitoring are indicated. The origin was mainly from the different care units where PCR tests are performed. Only 7.14% of those included came from tests performed on non-hospitalized patients after coming to the hospital emergency department.
Figure 2.
Flow chart of COVID-19 positive adult patients who are considered high-risk and in at-home monitoring (March 17 to April 17, 2020).
Of the 224 patients who were monitored as outpatients from the beginning, 38 (16.90%) were referred from the emergency department; 20 (8.87%) (referred on a total of 25 occasions) were discharged after their evaluation; and 18 (8.03%) were hospitalized. It should be noted that only one patient from this group came to the Emergency Department of their own volition.
The second route of access to the program was hospital discharges (Fig. 2). Two groups of patients were included therein: those who entered the program referred by the monitoring team and those discharged without previous contact. Of the 18 patients referred, two died and seven others continued hospitalized at the time the study ended. Therefore, of a total of 107 possible cases, monitoring was performed in 98 of them.
Outcomes. If we consider the totality of patients in the monitoring program, only two patients did not agree to be included in the study. All the others were able to connect every day and no serious problems were detected in the operation of the system.
The mean time of monitoring of the 304 patients in the study was 11.64 (SD 3.58) days and the median time of monitoring was 11 days. In the 30 days of the study, 224 (73.68%) patients were discharged from the program; one patient (0.32%) requested voluntary discharge; and one patient (0.32%) required readmission to the hospital after reactivation of COVID-19 (both in the monitoring after discharge group). At the time the study ended, 78 (25.65%) patients continued in the program (32 in monitoring since the beginning and 46 in monitoring after hospital discharge).
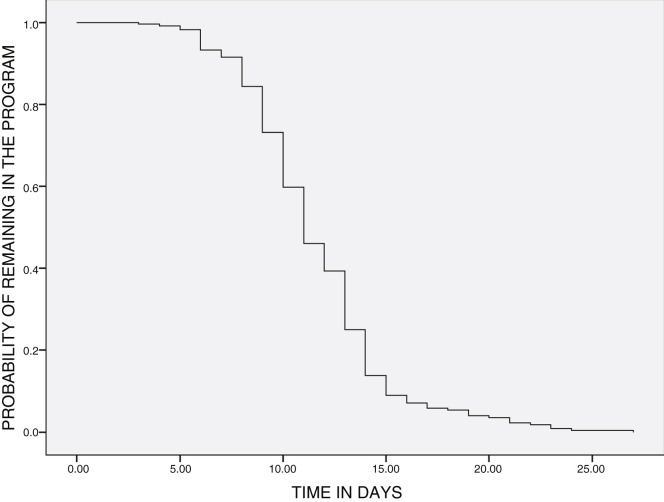
In Fig. 3 , the times of discharge are shown. 89.1% of discharges took place between days 6 and 15 of monitoring and only 4.6% of patients who started the program continued in it after 20 days. Though very few patients exited the program during the first five days, it should be noted that the two patients who later died were referred to the Emergency Department on days 1 and 3 of monitoring.
Figure 3.
Monitoring of COVID-19 patients with telemedicine: probability of continuing in the program over time.
Discussion
The data from this study suggest that at-home monitoring with telemedicine and telemonitoring in patients with COVID-19 is a well-accepted, useful, and safe system. Its use in higher-risk but not seriously ill patients allows for appropriate clinical monitoring, detects worsening of the disease early, helps order care at times of high demand, contributes to maintaining “social distancing” by preventing visits to emergency departments or clinics, and offers support to patients and their families.
Though telemedicine has been used in monitoring acute infectious diseases,5, 6 the majority of available evidence comes from managing patients with chronic diseases.8, 9, 10, 11 The information available on the role that telemedicine with telemonitoring can play in the control of an epidemic is scarce.12
In the case of COVID-19, there are various studies that provide guidelines on the work method and manner of implementing it.13, 14, 15 Nevertheless, we believe that this is the first study that provides in-depth detail both on the technology system, the procedures for its use, and the clinical criteria for management in daily practice. One of its contributions is the definition of work strategies that have been associated with promising results. It is undoubtedly a solid foundation so that future research, which could be broader and with control groups, can define the role telemedicine should play in this or future pandemics.
The strategy that combines telemedicine and proactive monitoring has been well accepted by patients (only two did not give their consent and there was only one voluntary discharge). Contrary to what occurs in other diseases, monitoring was completed without major problems in the majority of patients.16, 17, 18, 19 We understand that such a high degree of adherence is influenced by different factors: the ease of installation and use of the tools, the brief monitoring time (median of 11 days), and the exceptional situation of the state of alarm at the time of the study. Though many of the patients were elderly, the lockdown situation facilitated technological support from other family members who live with them.
Most likely, another reason behind adherence is that this monitoring strategy gives the user a sense of safety in uncertain times. The proactive attitude, the response to alerts, and the calls to patients within reasonable periods of time provide a feeling of surveillance and control. We understand that, at least in part, this justifies the fact that seeking out care in the hospital was uncommon.
From a clinical point of view, our data suggest that in this population, monitoring with telemedicine is clinically useful and safe. It is evident that appropriate clinical control was achieved; more severe patients were referred to the emergency department (nearly 50% were hospitalized); and, among those discharged, just one patient had symptoms of reactivation,20 which was detected in the initial phases. All this was achieved without any situations of poor control or extreme emergency.
We understand that this system has contributed to ensuring orderly patient flows and that spontaneous visits to the emergency department have been the exception. Therefore, it is probable that it helps reduce the overloading of the system and perhaps may contribute to a lower rate of infection among healthcare personnel as well.21 We understand that this must be linked to proactive monitoring and greater care at the times in which it is more likely that the disease would worsen.22
Lastly, three out of every four patients were discharged in the 30 days of the study—the majority in 15 days or less—which indicates the system's agility. These data may help control patient flows and avoid overloading units. Although these results are promising, it is evident that new, multicentric, broad, controlled studies that allow for confirming these findings must be evaluated.
Nevertheless, a strategy that uses telemedicine is not free of barriers. Among them, it requires having a nationwide unified electronic medical record or procedures for action that have already been tested in other situations. Likewise, it requires a certain degree of logistical capacity, such as distributing pulse oximeters to a large number of people in a brief period of time. Furthermore, it is necessary to involve a large number of professionals to cover departments every day of the week. In this case, the marked decline in healthcare activity in the hospital made it possible to incorporate professionals from other departments, who were quickly able to adapt thanks to the simplicity of the program.
When evaluating this study, certain limitations must be taken into account. First, the data come from a single hospital center. Given that it is possible that the results are not the same in areas with different COVID-19 incidence rates, it is necessary to replicate this study in other healthcare areas. Second, doubts may arise given the absence of clinical data. However, we must consider that the aim was to evaluate the impact of the use of telemedicine with telemonitoring on the flow of patients in the system and their safety and, for these purposes, the information available is complete and rigorous. Third, the objection can be raised that a very brief period of time has been analyzed and it is not related to the clinical course of the disease. This decision was made considering that given the study's aim, it was more suitable to use, as a reference, periods of time that are related to the monitoring; easily reproducible; and restricted to the most acute phase of the disease, when the amount of care provided is greater.
In conclusion, our data suggest that at-home telemedicine with telemonitoring, used in a proactive manner, allows for clinically useful and safe monitoring of patients with COVID-19 who are high-risk yet stable at the time of diagnosis. New studies are needed to confirm these findings and evaluate its possible application in future pandemics.
Conflicts of interest
None.
Footnotes
Please cite this article as: Martínez-García M, Bal-Alvarado M, Santos Guerra F, Ares-Rico R, Suárez-Gil R, Rodríguez-Álvarez A, et al. Telemedicina con telemonitorización en el seguimiento de pacientes con COVID-19. Rev Clin Esp. 2020;220:472–479.
Annex 1 The TELEA-COVID-19 Joint Monitoring Team (Lugo)
Álvaro Fernández Rial, Ramón Rabuñal Rey, Ana Rodríguez Álvarez, Antía Pérez López (physicians, Internal Medicine Department). Rafael Golpe Gómez (Pulmonology Department). Cristina Gil Mouce (physician, Endocrinology Department). Nicolás Suárez Ramírez (physician, Psychiatry Department). Carmen Almuiña Simón (physician, Pediatrics-Primary Care Department). María José Cereijo Quinteiro, Luis Daporta Rodríguez, Elvira Fernández Valdivieso, Andrés Vázquez Fernández, Andrea Barcia Losada, Arantza García Martínez (physicians, Home Hospitalization Department). Amparo Portero Vázquez, Natalia Trillo Dono, Concepción Revilla Villegas, Raquel Fernández Rodríguez, Isabel García Armesto, Rocío Giadas Piñeiro, Ana Rosa Rodríguez Macía (physicians, Rehabilitation Department). Francisco Carballada González, Ramón Núñez Orjales, Joaquín Martin Lázaro, Luis Alfredo González Guzmán (physicians, Allergology Department). María Mar Abad García, María Gloria Álvarez Silveiro, María Carmen Coria Abel, Javier Díaz Sánchez, María Jesús Freire Regueiro (Nursing Department, Cardiology Department). Ana María Casanova Quiñoá, María José Dobao Feijoo, María Luisa Fernández Rodríguez, Ángela Rey Ponce (Nursing Department, Anesthesia Department). Rafael Monte Secades, María Jesús Pérez Taboada, Rafael Sánchez Fernández, Juan Pérez Peña (Coordination). Manuel Pereira (Logistics Area). Jesús Conde Freire (Clinical Documentation Department).
References
- 1.Guan W.J., Ni Z.Y., Hu Y., Liang W.H., Ou C.Q., He J.X. China Medical Treatment Expert Group for COVID-19. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020 doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 3.and the Northwell COVID-19 Research Consortium. Richardson S., Hirsch J.S., Narasimhan M., Crawford J.M., McGinn T., Davidson K.W. Presenting characteristics comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area. JAMA. 2020;323:2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bashshur R., Doarn C.R., Frenk J.M., Kvedar J.C., Woolliscroft J.O. Telemedicine and the COVID-19 pandemic. Lessons for the future. Telemed J E Health. 2020;26:571–573. doi: 10.1089/tmj.2020.29040.rb. [DOI] [PubMed] [Google Scholar]
- 5.Young J.D., Abdel-Massih R., Herchline T., McCurdy L., Moyer K.J., Scott J.D. Infectious Diseases Society of America Position Statement on telehealth and telemedicine as applied to the practice of infectious diseases. Clin Infect Dis. 2019;68:1437–1443. doi: 10.1093/cid/ciy907. [DOI] [PubMed] [Google Scholar]
- 6.Parmar P., Mackie D., Varghese S., Cooper C. Use of telemedicine technologies in the management of infectious diseases: a review. Clin Infect Dis. 2015;60:1084–1094. doi: 10.1093/cid/ciu1143. [DOI] [PubMed] [Google Scholar]
- 7.Ohannessian R., Duong T.A., Odone A. Global telemedicine implementation and integration within health systems to fight the COVID-19 pandemic: a call to action. JMIR Public Health Surveill. 2020;6:e18810. doi: 10.2196/18810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Casariego E. Guerra F. Cerqueiro J.M. Rosón B. Chaos P. Guerrero H. Telemedicina en ICC: eficacia clínica y valor para el paciente. XXI Congreso Nacional de Hospitales y Gestión Sanitaria. Premio Patient Journey. Santiago de C, 8 de mayo de 2019 [consultado 16 Abr 2020]. Disponible en: https://www.21congresohospitales.org/media/attachments/2019/05/09/programacompleto09_05_2019.pdf
- 9.Lee J.Y., Lee S.W.H. Telemedicine cost-effectiveness for diabetes management: a systematic review. Diabetes Technol Ter. 2018;20:492–500. doi: 10.1089/dia.2018.0098. [DOI] [PubMed] [Google Scholar]
- 10.Batsis J.A., DiMilia P.R., Seo L.M., Fortuna K.L., Kennedy M.A., Blunt H.B. Effectiveness of ambulatory telemedicine care in older adults: a systematic review. J Am Geriatr Soc. 2019;67:1737–1749. doi: 10.1111/jgs.15959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhu Y., Gu X., Xu C. Effectiveness of telemedicine systems for adults with heart failure: a meta-analysis of randomized controlled trials. Heart Fail Rev. 2020;25:231–243. doi: 10.1007/s10741-019-09801-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mahmoodpoor A., Akbarzadeh M.A., Sanaie S., Hosseini M.S. Role of telehealth in outbreaks—where the classical healthcare systems fail. Infect Control Hosp Epidemiol. 2020;13:1–2. doi: 10.1017/ice.2020120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Greenhalgh T., Koh G.C.H., Car J. COVID-19: a remote assessment in primary care. BMJ. 2020;368:m1182. doi: 10.1136/bmj.m1182. [DOI] [PubMed] [Google Scholar]
- 14.Greenhalgh T., Wherton J., Shaw S., Morrison C. Video consultations for COVID-19. BMJ. 2020;368:m998. doi: 10.1136/bmj.m998. [DOI] [PubMed] [Google Scholar]
- 15.Keshvardoost S., Bahaadinbeigy K., Fatehi F. Role of telehealth in the management of COVID-19: lessons learned from previous SARS, MERS, and Ebola outbreaks. Telemed J E Health. 2020 doi: 10.1089/tmj.2020.0105. [DOI] [PubMed] [Google Scholar]
- 16.Tsou C., Robinson S., Boyd J., Jamieson A., Blakeman R., Bosich K. Improving engagement among patients with chronic cardiometabolic conditions using mHealth: critical review of reviews. Syst Rev. 2020;9:82. doi: 10.2196/15446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lang C., Voigt K., Neumann R., Bergmann A., Holthoff-Detto V. Adherence and acceptance of a home-based telemonitoring application used by multi-morbid patients aged 65 years and older. J Telemed Telecare. 2020;2 doi: 10.1177/1357633X20901400. 1357633X20901400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Linardon J., Fuller-Tyszkiewicz M. Attrition and adherence in smartphone-delivered interventions for mental health problems: a systematic and meta-analytic review. J Consult Clin Psychol. 2020;88:1–13. doi: 10.1037/ccp0000459. [DOI] [PubMed] [Google Scholar]
- 19.de Moreira T.C., Signor L., Figueiró L.R., Fernandes S., Bortolon C.B., Benchaya M.C. Non-adherence to telemedicine interventions for drug users: systematic review. Rev Saúde Publica. 2014;48:521–531. doi: 10.1590/S0034-8910.2014048005130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ye G., Pan Z., Pan Y., Deng Q., Chen L., Li J. Clinical characteristics of severe acute respiratory syndrome coronavirus 2 reactivation. J Infect. 2020;80:e14–e17. doi: 10.1016/j.jinf.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ji Y., Ma Z., Peppelenbosch M.P., Pan Q. Potential association between COVID-19 mortality and health-care resource availability. Lancet Glob Health. 2020;8:e480. doi: 10.1016/S2214-109X(20)30068-1. Epub 2020 Feb. 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]