Abstract
Schools have closed worldwide as part of measures to prevent SARS-CoV-2 transmission but are beginning to reopen in some countries. Various measures are being pursued to minimise transmission but existing guidance has not developed a comprehensive framework or theory of change. We present a framework informed by the occupational health hierarchy of control and a theory of change informed by realist approaches. We present measures focused on elimination, substitution, engineering, administration, education and personal protective equipment. We theorise that such measures offer a means of disrupting SARS-CoV-2 transmission via routes involving fomites, faeco-oral routes, droplets and aerosols.
Keywords: COVID-19, SARSCoV2, Schools, Environment, Disease control, Prevention
1. Introduction
Schools have closed worldwide as part of wider efforts to minimise SARS-Cov-2 transmission and resultant COVID-19-related morbidity and mortality (WHO Regional Office for Europe et al., 2020; Viner et al., 2020b). Approximately 1.6 billion students in 191 countries have ceased attending school (Centre For Global Development, 2020; United Nations Education, 2020). There are huge concerns, and some emerging evidence, about the harmful impacts of school closures on young people's education, social development and relationships (Pearcey et al., 2020), mental and physical wellbeing (Levita, 2020; Parnham et al., 2020), and exposure to violence (Sidpra et al., 2020), as well as decreasing access to support services (Bhopal et al., 2020). It is therefore clear that any risks of transmission in schools need to be weighed against the harms of schools remaining closed.
Several countries, including Denmark, France, Germany and Singapore, have reopened schools. There is some emerging evidence that children might be less susceptible to SARS-CoV-2 infection than adults (Viner et al., 2020a) and, because of this and their lower rate of symptom expression when infected (Davies et al., 2020), may play a smaller role in transmission than adults. Current evidence suggests that partially re-opening schools has not led to significant school outbreaks in the UK (Public Health England, 2020; Rapid Investigation Team, 2020) or elsewhere (Fontanet et al., 2020; Gudbjartsson et al., 2020). Nonetheless, modelling suggests that reopening schools could lead to second infection waves unless community test-trace-isolate (TTI) measures achieve good coverage (Panovska-Griffiths et al., 2020) and evidence from across Europe suggests that the impact of reopening schools is likely to vary with broader community rates of transmission (Stage et al., 2020).
Given the importance of schools reopening to children and young people's education, social development and wellbeing but the need to minimise the risks associated with this, it is important that reopened schools implement effective measures to minimise risks of transmission particular in contexts where rates of community transmission are significant (Stage et al., 2020).
Countries are pursuing a range of measures to prevent SARS-CoV-2 transmission in reopened schools. For example: class sizes are being reduced in Australia, France and Germany; students are attending schools in rotas in Austria and the Netherlands; school cleaning is being made more frequent in Denmark, Germany and Japan; temperature checks are being conducted in Singapore and Japan; face masks are to be used in Australia, Belgium and Japan; and physical distancing rules are to be applied in France, Germany and Singapore.
Schools can only open when staff and parents are convinced that it is safe enough for them to do so. This job cannot be left to school leaders; governments must provide citizens with clear information about transmission risks and the means of reducing these so that people can make informed decisions about the return to school. This includes providing: updates in the face of emerging evidence about the role of children and schools in transmission; information about the extent to which preventive measures within and beyond schools are in place; and rates of coverage and adherence with community TTI, given the importance of this in minimising the risk of resurgent infections (Panovska-Griffiths et al., 2020).
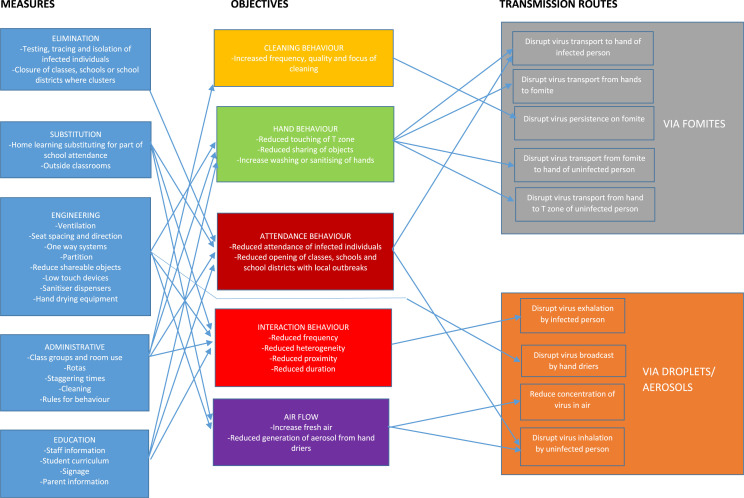
To reopen, schools need support, guidance and sufficient time and resources to plan and implement changes. Existing guidance does not take a systematic approach to defining measures and mechanisms via which these will reduce transmission (UNICEF, 2020; Resolve to Save Lives, 2020). This paper was developed by a group providing scientific advice to the UK national government and international bodies, and draws on existing reviews and other literature to propose an evidence-based theory of change and diagrammatic ‘logic model’ (Fig. 1 ).
Fig. 1.
Presents a diagrammatic logic model summarising our theory of change.
We take a realist approach to thinking about intervention implementation and mechanisms (Bonell et al., 2012). Realists suggest that interventions ‘work’ by providing resources which actors in settings take up and use, triggering mechanisms which may, depending on context, generate the intended outcomes. Realists focus not only on what works but what works for whom, under what conditions. Outcomes may fail to materialise in a certain context, for example where intervention resources are not fully used (e.g. because of limited school management capacity), where local factors prevent mechanisms from occurring (e.g. younger children may be unable to adopt some preventive behaviours) or where mechanisms do occur but are swamped by other factors (such as intense local outbreaks) (Pawson and Tilley, 1997). Although we do not include such ‘moderating’ factors in our diagrammatic logic model in the interests of clarity, we make suggestions about the contexts in which measures may prove most feasible or effective in the main text. Because some mechanisms will fail to be delivered or to generate benefits in some schools, often in unpredictable ways, we suggest that multiple measures be enacted so that there is a degree of redundancy and therefore overall resilience.
Because of the novelty of the COVID-19 pandemic, there is no direct evidence for every measure we recommend (Lunn et al., 2020). Our recommendations are informed by behavioural science developed through the study of other infections (including other coronaviruses), and other areas of health and behaviour. This evidence is cited but not described in detail.
2. Theory of change
2.1. Transmission prevention goals
To prevent SARS-CoV-2 infections in schools requires the disruption of the following transmission routes (WHO, 2020):
I. Transmission via fomites (objects or surfaces which can harbour and aid transmission of an infection) or faeco-oral routes if these are significant in transmissions among children (Hindson, 2020) by reducing: a) transport of the virus to the hands of those infected, b) transport of the virus from hands of the infected to fomites, c) persistence of the virus on fomites, d) transport of the virus from fomites to the hands of the uninfected, and e) transport of the virus from the hands to the face of the uninfected.
II. Transmission via aerosols/droplets by reducing: a) exhalation of the virus from infected individuals in droplets and aerosols; b) viral broadcast by hand-driers used by those with virus on their hands, c) viral concentration in the air, and d) inhalation of the virus in aerosols or droplets by uninfected individuals.
2.2. Objectives of measures to prevent transmission
To disrupt the above transmission routes, measures need to achieve behavioural and other objectives:
-
1.
Cleaning behaviours - increased frequency, quality and focus of cleaning of objects and surfaces.
-
2.
Hand behaviour – reduced touching of the T zone (eyes, nose, mouth) with hands, reduced sharing of objects (Dietz et al., 2020) and increased washing or sanitising of hands.
-
3.
Interaction behaviour – reduce social contacts in terms of reduced frequency, heterogeneity, proximity and duration (Uscher-Pines et al., 2018; Steffen et al., 2012).
-
4.
Attendance behaviour – reduced attendance at school of infected individuals; and reduced opening of classes, schools and districts affected by local outbreaks.
-
5.
Increase fresh air and reduced generation of aerosol from hand driers.
2.3. Measures to be implemented
Occupational health hierarchies of control aim to limit disease transmission in workplaces via: elimination; substitution; engineering, administrative; and personal protective equipment (ILO, 2003). Education can be considered a subset of administrative solutions but we have distinguished this as a separate category for school-based measures.
2.4. Elimination
Transmissions can be reduced by ensuring that infected individuals do not attend schools, achieved by testing individuals and, for those infected, isolating and contact tracing (and in turn isolation of household members and other contacts). Given that infections among children are often asymptomatic, there should be regular testing of all staff and students (Peto, 2020). However, in contexts where there is limited testing capacity, schools must at least ensure that they have a policy for identifying staff and students exhibiting COVID-19-type symptoms and ensuring that these individuals engage with community TTI systems where available, and do not attend school. Although temperature-testing is an imprecise indicator for infection, schools could test student temperatures each day to identify febrile students (who should be referred for testing and sent home) and maintain awareness. For students with symptoms who need collection from school, safe spaces must be provided for their isolation while ensuring such students are supported and not stigmatised (UNICEF, 2020).
A further means of preventing school-based transmission is to close a school to specific classes or the whole school when there is a cluster of infection defined by a clear threshold, for example as done in Taiwan. For this to occur, agencies leading TTI must communicate with schools so that the latter are aware of cases of infection among their staff or students.
2.5. Substitution
Another way to reduce the risk of infection is to substitute less risky for more risky conditions. Schools can limit the time that staff and students spend in schools to reduce their potential exposure (if uninfected) or transmission (if infected). For example, students could attend school only on alternate weeks as part of ‘temporal management’ strategies (see below), and this should be a particularly important approach in contexts where there are high local rates of transmission. Students or staff with underlying health conditions or those with such individuals in their households, should remain at home and not attend school (UNICEF, 2020) with the rates of these varying considerably across different countries. Other substitutions include administrative and other staff who can work from home being encouraged to do so. Outdoor education should substitute for indoors classes in settings where weather and space permits.
To minimise the extent to which partly substituting home-based for school-based education hampers students’ education or increases educational inequalities, such reductions in face-to-face learning should be accompanied by corresponding increases in home-based distance learning and support for parents helping with learning (Uscher-Pines et al., 2018, UNICEF, 2020), facilitated by digital platforms. Some countries, such as Canada, New Zealand, Spain and Singapore, have provided poorer students with internet access and devices but this may be more challenging in countries and with individuals lacking resources or technology, and may be less feasible and effective with younger compared with older students.
2.6. Engineering
Engineering solutions modify school buildings, equipment, furniture and other objects. Schools have poor ventilation compared to offices so modifications should be made to increase this such as opening windows and doors during school hours in countries and months when this is feasible (Dietz et al., 2020). Within classrooms and offices, desks should be re-arranged with one individual per desk, all facing in the same direction with 2 m spacing (Uscher-Pines et al., 2018; Honey-Rosés et al., 2020). However, ensuring distancing within classrooms will be very challenging with very young students. Perspex partitions or, in more resource-poor settings rope cordons, could also be introduced in offices and classrooms to support physical distancing (Dietz et al., 2020; Jourdan et al., 2020). In corridors and other shared spaces where physical distancing is difficult, one-way systems can be used to promote distancing and reduce face-to-face interactions (Uscher-Pines et al., 2018). Other school spaces, such as playgrounds, can be zoned for use by different subgroups of students (Uscher-Pines et al., 2018) if the size of school yards allows. However, because transmission risks are much lower with outdoor or brief contacts such measures are likely to be less important than good ventilation, hygiene and distancing within classrooms.
In terms of objects, no/low touch devices can reduce shared touching of objects where resources allow. Doors and soap dispensers should be upgraded so that these are operated without touch or using elbows (Dietz et al., 2020). Hand sanitiser dispensers should be fitted at the school entrance and in classrooms and other spaces (Staniford and Schmidtke, 2020). When used by those with the virus on their hands, airflow-based hand-driers can create virus-containing aerosols; these must be disconnected and replaced by paper-towels dispensed using no/low-touch dispensers.
Schools should further limit fomite-based transmission by limiting the sharing of objects by ensuring students have their own individual stationery, equipment, and learning materials, though this will be easier to achieve among older students and in resource-rich settings (Dietz et al., 2020; Steffen et al., 2012). Unnecessary objects and surfaces, such as some furniture, displays and equipment, should be removed.
2.7. Administration
Administrative processes can support physical distancing and hygiene. ‘Temporal management’ concerns the way an organisation manages the densities and movements of individuals (Uscher-Pines et al., 2018; Zhang et al., 2012). Schools should where possible reduce the number and heterogeneity of contacts between individuals by retaining students within a single class grouping throughout the day, including break and lunch times. Contacts with students in other classes should where possible be reduced by teachers, rather than students, moving between rooms (Uscher-Pines et al., 2018). However, this will generally not be feasible for older students who study different subjects with different peers because of academic setting or academic choices. While the former might be discontinued with minimal impacts on educational attainment (Education Endowment Foundation, 2018), the latter will be much less open to change.
Contacts among class members can be reduced, and physical distancing facilitated, where classes are divided into subgroups (usually halves) with each attending on a rota at different times, with cleaning occurring between these times. Modelling suggest that rotas involving each half class attending school on alternating weeks will reduce transmission in contexts of significant levels of transmission (Panovska-Griffiths et al., 2020) though this approach may be resisted by governments wishing to keep schools fully open and parents struggling with balancing work and family demands.
Schools should reduce contacts between different classes by using staggering, whereby different classes start and end the school day, take breaks or use other common spaces at slightly different times (Steffen et al., 2012, UNICEF, 2020). This may, however, raise problems for parents taking several young children to school at slightly different times, particularly where schools are situated some distance from homes. Schools must also avoid larger gatherings of staff or students for breaks, lunch, assemblies, sporting events or staff meetings (Steffen et al., 2012). Where practical, such gatherings should be replaced by virtual interactions using digital meetings packages but this may only be feasible in resource-rich settings and for older students. Schools should also exclude parents from entering the school site and support distancing among parents waiting to pick up students by use of signage and space markings.
Schools should reduce SARS-CoV-2 transmission via fomites by increasing cleaning. Cleaning must occur more frequently, more intensively (using products such as bleach or alcohol which kill the virus) and more extensively (for example cleaning door handles or walls which function as effective fomites but are not traditional targets for hygiene). Schools should provide lunches for students in classrooms rather than communal canteens; schools must ensure rigorous hygiene in the preparation of lunches to minimise the risk of fomite-based transmission.
Schools should promote adherence to physical distancing and hand hygiene by incorporating these into policies, rules and reward systems. Rules should precisely define what behaviours are required (e.g. hands below shoulders; cough or sneeze into tissue or elbow); these are more likely to be understood and followed than lists of outlawed behaviours (Michie et al., 2011) and by older more than younger children. However, proscriptions should cover behaviours such as touching others, spitting and shouting. Staff should monitor behaviour and intervene where this is not optimal (Steffen et al., 2012). In some cases, persistent non-adherence will require students to be temporarily excluded. However, behaviour change is most effectively achieved by enabling and rewarding rather than punishing (Alnabulsi et al., 2018; Drury et al., 2009). Reward systems can be used to incentivise preventive behaviours, for example by awarding prizes to classes with high adherence. Rules and behavioural norms are most likely to be adhered to when these are developed in collaboration with target audiences (Bonell et al., 2018). While schools will need to develop and implement new preventive measures quickly, implementation science suggests that spending time at the outset discussing these with staff and students can increase adherence and identify problems or solutions not apparent to school leaders (May, 2013).
Policies and rules must also address some behaviours outside of school such as staying home when experiencing COVID-19-like symptoms, and maintaining physical distancing on the journey to and from school. The latter can be supported by policies encouraging walking or cycling to school and discouraging use of public transport where possible. Policies should reduce fomite transmission by limiting what students bring to and from school (clean clothes and shoes but not books, equipment or packed lunches) (Dietz et al., 2020; Steffen et al., 2012).
2.8. Education
Students, parents and staff should be educated on how to minimise SARS-CoV-2 transmission at school. This should build on not be instead of continuing clear information and health promotion campaigns from government as we argue above. Staff must receive written guidance on the behaviours that they should adopt and the behaviours that they should not engage in, as well as how they should educate students, monitor their behaviour and respond to any non-adherence (UNICEF, 2020). Students should be provided with clear and specific information (Michie et al., 2011) and motivation (Michie et al., 2020). Particularly in the context of children and young people likely perceiving themselves to be at low risk of severe consequences from COVID-19, messages should emphasise collective identity, solidarity and care for family and community members (Drury et al., 2019; Chaudhuri, 2011).
Students will be more likely to engage with preventive behaviours when they feel a sense of school engagement and belonging (Bonell et al., 2019) so impacts may be moderated by this. It is therefore essential that, despite schools being deeply challenged to educate students in difficult circumstances, they reach out to those students most at risk of disengagement, discussing their circumstances and needs, and where possible involving them in decision-making (Bonell et al., 2018).
Evidence suggests that students, in particular older students in adolescence, will be most influenced by messages from peers (Blakemore, 2018). Peer education is therefore a promising approach which could be delivered within class grouping and online (Campbell et al., 2008). Peer educators could be provided with key messages and advice on effective communication strategies. Educational messages should be supported by messages communicated within schools via signage and digital displays (Dietz et al., 2020).
Different subjects may be used to teach students about different aspects of the pandemic, for example in terms of its biology, politics and media representation. Learning in these areas might be enlivened by considering examples relating to the pandemic. Schools should promote physical distancing and limit sharing of objects by adapting how different subjects are taught. For example, schools should promote physical distancing and limit sharing of objects by replacing team-based physical activity with individual exercise (with adequate spacing) or by avoiding science practical work that requires working in groups or sharing equipment (Honey-Rosés et al., 2020).
Parents should also be educated on the behaviours required of their children, particularly where these relate to the interface between school and home such as: not bringing packed lunches or books to and from school; wearing fresh clothing every day (although this may be unfeasible for poorer families); physical distancing and avoidance of public transport when travelling to and from school (although this will be much more challenging for those who have no means of travel other than public transport); and limiting contacts with peers, particularly those in other classes.
2.9. Personal protective equipment
N95 surgical grade respirators offer protection to the wearer against SARS-CoV-2 infection, while non-clinical masks can reduce onward transmission from infected individuals (Howard et al., 2020; Chu et al., 2020). Controversy has raged about whether face masks should be recommended for the general population because of concerns about risk compensation and masks, if used incorrectly, facilitating fomite transmission via increasing touching of the T zone. Because of the likely challenges in ensuring effective use with younger children, and the likely unacceptability of recommending masks to older but not younger students within the same school, cloth masks are unlikely to be an effective strategy in primary schools but may be feasible in secondary schools, if accompanied by education (Royal Society, 2020). However, face masks should be a feasible and acceptable means of reducing transmission risk in secondary schools. N95 surgical masks could protect staff against infection but where supplies are short should be prioritised for clinical and social care staff.
3. Discussion
Although the above measures have not been empirically evaluated in the context of the current pandemic, they are informed where possible by broader evidence and designed to be a comprehensive strategy to prevent SARS-CoV-2 transmission in schools. As we have described, different measures will be more or less feasible or acceptable, and may be more or less effective in different countries, schools or individuals. This underlines the importance of a multi-faceted approach which is more likely to be resilient to some elements not being feasible or effective.
Planning must start early so that governments give schools, parents and trade unions sufficient notice of the timing and extent of reopenings (UNICEF, 2020). The measures outlined above have implications for procurement and these must be considered well in advance to ensure that there are no critical shortages, for example of paper-towels, single desks or sanitiser dispeners.
Particularly where there is currently some uncertainty about the effectiveness of measures such as face masks, our recommendations should be updated as new evidence emerges. The effectiveness of specific measures in changing behaviour, and of programmes of multiple measures in minimising transmissions should be evaluated, both formally at a regional or national level but also informally within schools. Schools should use checklists completed by staff to monitor whether measures are being implemented with fidelity and convene (virtual) discussions among staff and students to reflect on the feasibility, acceptability and consequences of measures. Where measures bring about unintended consequences, they may need to be dropped, modified, mitigated or used more selectively.
There is a risk that some of the suggested measures will impact negatively on the social development or mental wellbeing of some students. Restricting students to smaller groups will cut across important friendships and schools should consider this when allocating students to groups. Implementing rotas will reduce students’ contact time at school, likely hindering their education even if good home learning technology is available and hampering the ability of parents of young children to go to work. If such rotas are implemented, for example to disrupt transmission chains in the face of high rates of infections, schools will need to decide what patterns of rotas are the least worst. Wearing of masks will, as we have suggested, be more feasible in secondary than primary schools. But even in the former, masks may hinder social interactions and be particularly problematic for students with conditions such as autism and hearing difficulties. Requiring clean clothes each day may stigmatise poorer families.
School staff will need to use their judgement and learn from their experiences in deciding questions of feasibility, acceptability and the balance of risks and harms relating to specific measures. We reiterate the point that while schools will need to implement preventive measures quickly, evidence suggests that planning these in collaboration with staff and students will increase feasibility and acceptability, and may limit harmful consequences (May, 2013).
School-based preventive measures need to build in plans for gradually easing or exiting measures, once epidemiological data suggest that this is unlikely to increase transmission. Government and school leaders should indicate that this will be kept under review, informed by epidemiological data including on infections among children. Adequate notice should be given when nearing the point at which an exit strategy is being considered. As with measures to curtail societal lock-downs, it is likely that any exit strategy will be phased and contingent on regular assessment of its epidemiological effects. Some measures, such as enhanced hygiene and cleaning, which reduce transmission of SARS-CoV-2 and other infections, may be retained longer than other measures, which though valuable in preventing infections also harm students’ wellbeing in other ways as discussed above.
Acknowledgements
Rogers and Rubin are affiliated to the National Institute for Health Research Health Protection Research Unit (NIHR HPRU) in Emergency Preparedness and Response at King's College London in partnership with Public Health England (PHE), in collaboration with the University of East Anglia. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, the Department of Health and Social Care or Public Health England.
Handling editor: Jamie Pearce
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.healthplace.2020.102398.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- Alnabulsi H., Drury J., Templeton A. Predicting collective behaviour at the Hajj: place, space and the process of cooperation. Philos. Trans. R. Soc. B. 2018;373 doi: 10.1098/rstb.2017.0240. 20170240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhopal S., Buckland A., Mccone R., Villis A., Owens S. Who has been missed? Dramatic decrease in numbers of children seen for child protection assessments during the pandemic. Arch. Dis. Child. 2020 doi: 10.1136/archdischild-2020-319783. https://search.crossref.org/?q=Who+has+been+missed%3F+Dramatic+decrease+in+numbers+of+children+seen+for+child+protection+assessments+during+the+pandemic 2020, published Online First. [DOI] [PubMed] [Google Scholar]
- Blakemore S.J. Avoiding social risk in adolescence. Curr. Dir. Psychol. Sci. 2018;27:116–122. [Google Scholar]
- Bonell C., Allen E., Warren E., Mcgowan J., Bevilacqua L., Jamal F., Legood R., Wiggins M., Opondo C., Mathiot A., Sturgess J., Fletcher A., Sadique Z., Elbourne D., Christie D., Bond L., Scott S., Viner R.M. Initiating change in the school environment to reduce bullying and aggression: a cluster randomised controlled trial of the Learning Together (LT) intervention in English secondary schools. Lancet. 2018;392:2452–2464. doi: 10.1016/S0140-6736(18)31782-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonell C., Beaumont E., Dodd M., Elbourne D., Bevilacqua L., Mathiot A., Mcgowan J., Sturgess J., Warren E., Viner R., Allen E. Effects of school environments on student risk-behaviours: evidence from a longitudinal study of secondary schools in England. J. Epidemiol. Community Health. 2019 doi: 10.1136/jech-2018-211866. Published Online First. 23 February. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonell C., Fletcher A., Morton M., Lorenc T. 'realist Randomised Controlled Trials': a new approach to evaluating complex public health interventions. Soc. Sci. Med. 2012;75:2299–2306. doi: 10.1016/j.socscimed.2012.08.032. [DOI] [PubMed] [Google Scholar]
- Campbell R., Starkey F., Holliday J., Audrey S., Bloor M., Parry- Langdon N., Hughes R., Moore L. An informal school-based peer-led intervention for smoking prevention in adolescence (ASSIST): a cluster randomised trial. Lancet. 2008;371:1595–1602. doi: 10.1016/S0140-6736(08)60692-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centre For Global Development . Centre for Global Development; Washington Dc: 2020. Cgd Covid Education Policy Tracking.https://docs.google.com/spreadsheets/d/1ndhgp53atj5j-Etxgwcpsfyg8ldzhpusnb6mwyberyg/edit?ts=5e6f893e#gid=0 [Google Scholar]
- Chaudhuri A. Sustaining cooperation in laboratory public goods experiments: a selective survey of the literature. Exp. Econ. 2011;14:47–83. doi: 10.1007/s10683-010-9257-1. [DOI] [Google Scholar]
- Chu D., Akl E., Duda S., Solo K., Yaacoub S., Schünemann H.J. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of Sars-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020;395 doi: 10.1016/S0140-6736(20)31142-9. 19733-198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies N.G., Klepac P., Liu Y., Prem K., Jit M., Cmmid Covid-19 Working Group, Eggo R.M. Age-dependent effects in the transmission and control of COVID-19 epidemics. Nat Med. 2020 doi: 10.1038/s41591-020-0962-9. 2020. published Online First. [DOI] [PubMed] [Google Scholar]
- Dietz L., Horve P.F., Coil D.A., Fretz M., Eisen J.A., K V.D.W. 2019 Novel Coronavirus (Covid-19) pandemic: built environment considerations to reduce transmission. mSystems. 2020;5 doi: 10.1128/msystems.00245-20. e00245-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drury J., Carter H., Cocking C., Ntontis E., Tekin Guven S., Amlôt R. Facilitating collective resilience in the public in emergencies: twelve recommendations based on the social identity approach. Front. Publ. Health. 2019;7:141. doi: 10.3389/fpubh.2019.00141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drury J., Cocking C., Reicher S. Everyone for themselves? A comparative study of crowd solidarity among emergency survivors. Br. J. Soc. Psychol. 2009;48:487–506. doi: 10.1348/014466608X357893. [DOI] [PubMed] [Google Scholar]
- Education Endowment Foundation . Education Endowment Foundation; London: 2018. Setting or Streaming Teaching & Learning Toolkit. [Google Scholar]
- Fontanet A., Tondeu R.L., Madec Y., Grant R., Besombes C., Jolly N., Fernandes Pellerin S., Ungeheuer M., Cailleau I., Kuhmel L., Temmam S., Huon C., Chen K., Crescenzo B., Munier S., Demeret C., Grzelak L., Staropoli I., Bruel T., Gallian P., Cauchemez S., Van Der Werf S., Schwartz O., Eloit M., Hoen B. 2020. Cluster of COVID-19 in northern France: a retrospective closed cohort study. medrxiv preprint server 2020. [published Online First: 23 April 2020] [DOI] [Google Scholar]
- Gudbjartsson D.F., Helgason A., Jonsson H., Magnusson O., Melsted P., Norddahl G., Saemundsdottir J., Sigurdsson A., Sulem P., Agustsdottir A., Eiriksdottir B., Fridriksdottir R., Gardarsdottir E., Georgsson G., Gretarsdottir O., Gudmundsson K., Gunnarsdottir T., Gylfason A., Holm H., Jensson B., Jonasdottir A., Jonsson F., Josefsdottir K., Kristjansson T., Magnusdottir D., Le Roux L., Sigmundsdottir G., Sveinbjornsson G., Sveinsdottir K., Sveinsdottir M., Thorarensen E., Thorbjornsson B., Löve A., Masson G., Jonsdottir I., Möller A., Gudnason T., Kristinsson K., Thorsteinsdottir U., Stefansson K., Original Spread of Sars-Cov-2 in the Icelandic population. N. Engl. J. Med. 2020 doi: 10.1056/Nejmoa2006100. [published Online First: 2020/04/15] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hindson J. Covid-19: faecal–oral transmission? Nat. Rev. Gastroenterol. Hepatol. 2020;17 doi: 10.1038/s41575-020-0295-7. 259-259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Honey-Rosés J., Anguelovski I., Bohigas J., Chireh V., Daher C., Konijnendijk C., Litt J., Mawani V., Mccall M., Orellana A., Oscilowicz E., Sánchez U., Senbel M., Tan X., Villagomez E., Zapata O., Nieuwenhuijsen M. The impact of Covid-19 on public space: a review of the emerging questions. 2020. https://osf.io/rf7xa/ Pre-print.
- Howard J., Huang A., Li Z., Tufekci Z., Zdimal V., Van Der Westhuizen H., Von Delft A., Price A., Fridman L., Tang L., Tang V., Watson G.L., Bax C.E., Shaikh R., Questier F., Hernandez D., Chu L.F., Ramirez C.M., Rimoin A.W. Face masks against covid-19: an evidence review. Preprints. 2020;2020:2020040203. doi: 10.20944/preprints202004.0203.v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ILO . Interational Labour Organisation; 2003. Encyclopaedia of Occupational Health and Safety. Geneva. [Google Scholar]
- Jourdan D., Marmot M., Gray N. There is an urgent need to reopen schools - this is how to make it happen. The Conversation. 2020. https://theconversation.com/coronavirus-there-is-an-urgent-need-to-re-open-schools-this-is-how-to-make-it-happen-137818
- Levita L. /University of Sheffield; 2020. Initial Research Findings on the Impact of Covid-19 on the Well-Being of Young People Aged 13 to 24 in the UK, Sheffield, Covid-19 Psychological Research Consortium (C19prc) [Google Scholar]
- Lunn P., Belton C., Lavin C., Mcgowan F., Timmons S., Robertson D. Economic and Social Research Institute; 2020. Using behavioural science to help fight the Corona virus.https://www.esri.ie/publications/using-behavioural-science-to-help-fight-the-coronavirus [Google Scholar]
- May C. Towards a general theory of implementation. Implement. Sci. 2013;8 doi: 10.1186/1748-5908-8-18. 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michie S., Van Stralen M.M., West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement. Sci. 2011;6:42. doi: 10.1186/1748-5908-6-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michie S., West R., Amlôt R. Behavioural strategies for reducing covid-19 transmission in the general population. BMJ Opin. 2020 March 3 2020. [Google Scholar]
- Panovska-Griffiths J., Kerr C.C., Stuart R.M., Mistry D., Klein D.J., Bonell C., Viner R.M. Determining the optimal strategy for reopening schools in the UK: balancing earlier opening with the occurrence of a secondary Covid-19 pandemic wave. Lancet Child Adolescent Health. 2020 doi: 10.1016/S2352-4642(20)30250-9. (under review) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parnham J.C., Laverty A.A., Majeed A., Vamos E. 2020. Half of children entitled to free school meals do not have access to the scheme during the Covid-19 lockdown in the UK. medrxiv 2020:2020.06.19.20135392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pawson R., Tilley N. Sage; 1997. Realistic Evaluation. [Google Scholar]
- Pearcey S., Shum A., Waite P., Patalay P., Creswell C. Cospace study; Oxford: 2020. Report 04: Changes in Children and Young People's Emotional and Behavioural Difficulties through Lockdown. [Google Scholar]
- Peto J. Covid-19 mass testing facilities could end the epidemic rapidly. Br. Med. J. 2020;368 doi: 10.1136/bmj.m1163. m1163. [DOI] [PubMed] [Google Scholar]
- Public Health England . vol. 25. Public Health England; London: 2020. (Weekly Coronavirus Disease 2019 (COVID-19) Surveillance Report). Week. [Google Scholar]
- Rapid Investigation Team . Public Health England; 2020. Preliminary Investigation into COVID-19 Exceedances in Leicester (June 2020) London. [Google Scholar]
- Resolve To Save Lives . Resolve to Save Lives; New York City Ny: 2020. Reopening America's Schools: A Public Health Approach. [Google Scholar]
- Royal Society . Royal Society Delve initiative; 2020. Face Masks for the General Public.https://rs-delve.github.io/reports/2020/05/04/face-masks-for-the-general-public.html May 2020, Available from: Url. [Google Scholar]
- Sidpra J., Abomeli D., Hameed B., Baker J., Mankad K. Rise in the incidence of abusive head trauma during the Covid-19 pandemic. Arch. Dis. Child. 2020;2020 doi: 10.1136/archdischild-2020-319872. [published Online First: 2020/07/04] [DOI] [PubMed] [Google Scholar]
- Stage H.B., Shingleton J., Ghosh S., Scarabel F., Pellis L., Finnie T. 2020. (Shut and Re-open: the Role of Schools in the Spread of Covid-19 in Europe). medrxiv 2020.vol. 6.24.20139634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Staniford L.J., Schmidtke K.A. A systematic review of hand-hygiene and environmental-disinfection interventions in settings with children. BMC Publ. Health. 2020;20:195. doi: 10.1186/s12889-020-8301-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steffen R., Bouchama A., Johansson A., Dvorak J., Isla N., Smallwood C., Memish Z.A. Non-communicable health risks during mass gatherings. Lancet Infectious Disease. 2012;12:142–149. doi: 10.1016/S1473-3099(11)70293-6. [DOI] [PubMed] [Google Scholar]
- UNICEF . Unicef; New York City: 2020. Framework for Reopening Schools. [Google Scholar]
- United Nations Education S.A.C.O. Unesco; 2020. Covid Education Disruption and Response.https://en.unesco.org/covid19/educationresponse Geneva. [Google Scholar]
- Uscher-Pines L., Schwartz H.L., Ahmed F., Zheteyeva Y., Meza E., Baker G., Uzicanin A. School practices to promote social distancing in K-12 schools: review of influenza pandemic policies and practices. BMC Publ. Health. 2018;18 doi: 10.1186/s12889-018-5302-3. 406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viner R.M., Mytton O., Bonell C., Melendez-Torres G.J., Ward J., Hudson L., Waddington C., Thomas J., Russell S., Van Der Klis F., Panovska-Griffiths J., Davies N.G., Booy R., Eggo R.M. 2020. Susceptibility to Covid-19 amongst children and adolescents compared with adults: a systematic review and meta-analysis. medrxiv preprint server 2020, [published Online First: 24 May 2020] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viner R.M., Russell S.J., Croker H., Packer J., Ward J., Stansfield C., Mytton O., Bonell C., Booy R. School closure and management practices during coronavirus outbreaks including Covid-19: a rapid systematic review. Lancet Child Adolescent Health. 2020 doi: 10.1016/S2352-4642(20)30095-X. 2020; online first. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . World Health Organization; Geneva: 2020. Modes of Transmission of Virus Causing Covid-19: Implications for Ipc Precaution Recommendations: Scientific Brief, 27 March 2020. [Google Scholar]
- WHO Regional Office For Europe, European Commission & European Observatory On Health Systems And Policies . World Health Organisation; 2020. Covid-19 Health Systems Response Monitor.https://www.covid19healthsystem.org/mainpage.aspx Geneva. [Google Scholar]
- Zhang T., Fu X., Ma S., Xiao G., Wong L., Keong Kwoh C., Lees M., Khoon Lee G.K., Hung T. Evaluating temporal factors in combined interventions of workforce shift and school closure for mitigating the spread of influenza. PloS One. 2012;7 doi: 10.1371/journal.pone.0032203. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.