Abstract
Spatial contexts and spatial mobility are important factors of the HIV epidemic and sexually transmitted infections. Using global positioning system (GPS) devices, we examined the associations of objectively measured spatial mobility with sexual risk behaviors among gay, bisexual and other men who have sex with men (MSM) in New York City. This observational study included a subgroup of 253 HIV-negative MSM from the Project 18 Cohort Study, who participated in the GPS monitoring sub-study. Spatial mobility was measured as (1) distance traveled and (2) activity space size defined as daily path area during 2-week of GPS tracking. We examined the associations of these measures with numbers of male sexual partners and condomless anal intercourse (CAI) acts during last six months using quasi-Poisson models, adjusting for socio-demographics. Results demonstrated that spatial mobility was positively associated with sexual risk behaviors, for example, with CAI (incidence rate ratio [IRR] = 1.01 for a 10 km increase in distance traveled and IRR=1.04 for a 1 km2 increase in 50m-buffer activity space size). Our findings may enhance the understanding of spatial contexts of HIV risk. Future studies should be conducted to examine the mechanisms for the associations between spatial mobility behaviors with sexual risk behaviors as well as the influence of neighborhood characteristics in various neighborhood contexts, which may guide the place-based HIV prevention services.
Keywords: spatial analysis, mobility, Global Positioning System (GPS), sexual behavior, Men who have Sex with Men (MSM), HIV prevention
Introduction
The incidence rate of human immunodeficiency virus (HIV) is disproportionately high among gay, bisexual and other men who have sex with men (MSM), especially young MSM. In 2018, MSM accounted for 69.6% of new HIV cases among adult and adolescent (age over 13 years) in the United States (U.S.), and young MSM (aged 13 to 29 years old) made up 48.6% of new HIV infections among MSM (Centers for Disease Control and Prevention, 2019). Furthermore, even though HIV incidence in the general population in the U.S. has decreased since 2008, the rate among MSM during 2008–2015 remained high and even increased by 5.7% per year among MSM between age 25 and 34 (Singh et al., 2018).
In addition to standard individual-level sociodemographic factors affecting vulnerability to HIV infection, geographic factors such as the spatial mobility behavior and characteristics of spatial contexts have been studied to explain variations in HIV incidence in heterosexual population as well as among MSM. Theoretical and empirical studies have identified that spatial mobility, including migration, commuting, and local mobility, is one of important factors influencing HIV transmission (Vaughan et al., 2017; Cassels and Camlin, 2016; Cassels et al., 2017; Deane et al., 2010; Coffee et al., 2007; Camlin et al., 2013). The theoretical frameworks suggested multiple pathways that may explain the associations between mobility and HIV risks. Mobile individuals may have potentials to be connected to riskier sexual network with larger number of partners in different places (Cassels et al., 2017). In addition, non-residential places may be separated from conventional HIV prevention supports and have higher risk of environmental exposures (Frye et al., 2014; Vaughan et al., 2017). Lastly, exposure to diverse non-residential contexts may increase HIV risk, since lack of social-monitoring and non-kin ties in the neighborhoods may facilitate more frequent engagement in sexual risk behaviors (Seeley and Allison, 2005; Camlin et al., 2013). To illustrate, previous studies have demonstrated that highly mobile men are more likely to be engaged in risky sexual behaviors, such as more frequent engagement in condomless sex and having increased numbers of sexual partners (Saggurti et al., 2008; Saggurti et al., 2009; Lydie et al., 2004; Kishamawe et al., 2006; Khan et al., 2008; Gupta et al., 2010; Schuyler et al., 2017). However, most of the studies on local daily mobility and HIV infection have investigated heterosexual populations in African or low-income countries, and only a handful of studies have assessed the role of spatial mobility in the context of the HIV epidemic among MSM in the U.S. (Mustanski et al., 2015; Tobin et al., 2013)
The spatial context of risk behaviors may also be salient to MSM population in the U.S., since studies have shown that MSM experience different types of neighborhoods (Koblin et al., 2017; Tobin et al., 2014; Koblin et al., 2013; Duncan et al., 2014), and thus may have differential influences from diverse neighborhood environments. Two recent studies have shown that few MSM reside, socialize, and meet sexual partners in the same neighborhoods (Koblin et al., 2013; Duncan et al., 2014). Young MSM are especially likely to have higher degree of spatial mobility compared to general MSM, due to the developmental characteristics of this age group during their transition to adulthood (Schachter, 2001). In addition, MSM with higher mobility may experience different venues to meet their sexual partners, and such diverse venues play important role in shaping sexual risk behaviors (Al-Ajlouni et al., 2018a; Young et al., 2017).
The scant research on spatial mobility behavior and HIV among MSM has examined a limited measure of mobility, mostly relying on self-reported mobility, raising concerns of recall bias and misclassification. Objective measures of mobility and spatial context are increasingly used in the field of physical activity and obesity research (Jia et al., 2019; James et al., 2016; Chaix et al., 2013), but not widely applied in HIV epidemiology. Use of global positioning system (GPS) technologies is an objective approach to investigate the aspects of spatial mobility by allowing researchers to identify participants’ continuous spatial location over time. Such spatio-temporal data can be used to measure local daily mobility and construct activity spaces, and these data, in conjunction with survey data, can measure time and duration of different types of neighborhood exposures (Duncan et al., 2016). GPS technologies present an opportunity to enhance understandings of the relationship between personal spatial mobility behavior and HIV risk among MSM population.
As such, the purpose of this study was to investigate the association of spatial mobility behavior measured using GPS, with sexual risk behaviors among young MSM. In the present study, we hypothesize that more mobile young MSM may have higher numbers of sexual partners and more frequently engage in condomless anal intercourse.
Method
P18 Neighborhood Study
The present study recruited participants of the Project 18 Cohort Study, a prospective cohort study of 665 HIV-negative MSM in New York City designed to study longitudinal trajectories of sexual behavior, substance use, and mental health among young MSM (Halkitis et al., 2013). Venue-based (e.g., community events, afterschool events, service agencies, public spaces, and nightlife venues) and internet-based (e.g., social networking and dating websites) recruitments were employed for the original cohort. Both active (e.g., approaching individuals to solicit study participation) and passive (e.g., flyers, advertising on internet) methods were used for the participant recruitment. Inclusion criteria for the original cohort were: (a) age 18 to 19 years old; (b) male sex assignment at birth; (c) currently identify as male; (d) residence in the New York City metropolitan area; (e) report sexual contact with another man in the preceding six months; and (f) reported negative or unknown HIV status. The study started from May 2009. We randomly sorted the 665 P18 Cohort participants and invited them to the sub-study, known as the P18 Neighborhood Study. We contacted the randomly sorted participants via email or text messaging until the number of enrollments was reached to 250. A total of 450 participants were contacted, and the 250 participants enrolled in the sub-study between January 2017 and January 2018. The response rate was 56%. Additional eligibility criteria were applied for the subgroup study, including (1) having no mobility restrictions through a screening question, “Do you have serious difficulty walking or climbing stairs?”; (2) being comfortable carrying a GPS device for two weeks; and (3) being able to come in for the first and follow-up visits. The selected subgroup of 250 participants showed similar socio-demographics with the original cohort. For example, the percentages of Black/African-American in the sub-cohort and the original cohort were 30% and 27% respectively (White: 32% vs. 25%; Asian: 10% vs. 8%, school enrollment: 25% vs 33%, less than high school:34% vs. 39%; Associate: 11% vs 13%; College: 55% vs. 48%) (Jaiswal et al., 2018).
At the first visit, participants were consented to the subgroup study, completed the first survey, and received instructions on GPS device. At the follow-up visit, they returned the GPS device, completed an exit survey, and were compensated $110. Three participants did not complete the two visits, therefore, three additional participants were randomly selected and enrolled in the sub-study. The University Committee on Activities Involving Human Subjects at New York University and the institutional review board of the New York University School of Medicine approved the research protocol prior to subject enrollment.
GPS Protocol
Participants were asked to carry a small GPS device (BT-Q1000XT, QStarz International Co., Ltd., Taipei, Taiwan) at all times over a two-week period, except when sleeping, swimming, and showering. The device collected location data in 10-second intervals, and additional GPS-use diary was used to evaluate the GPS data quality. Feasibility and acceptability of proposed GPS protocol was tested from a prior pilot study (Duncan et al., 2016), and a similar protocol was applied for this study. Of total 250 participants with GPS data, 39 participants were excluded as they (1) lived outside of New York City, (2) had invalid addresses, and/or (3) had less than 1 hour of GPS data for one day, which did not meet the data quality protocol. A total of 211 participants were used in the analysis. GPS data cleaning used a set of processing scripts to eliminate erroneous data, such as duplicated time stamps and isolated GPS points. Spatially isolated points were identified using 400-meter distance between two consecutive points (10 second apart), and those points were removed from the dataset.
Geographic Mobility Calculation
To quantify the local daily mobility of participants, we employed two measures; distance traveled and activity space size (Figure 1). The distance traveled was measured using inter-point distance calculation, and for the activity spaces, daily path area calculation was employed (Boruff et al., 2012, Sherman et al., 2005, Hirsch et al., 2014, Duncan et al., 2018b). The daily path area was defined by creating 50, 100, 200, and 400-meter buffering radiuses around the GPS points in New York City. We selected 50-meter buffer activity space as the main metric of exposure, based on the line-of sight theory and existing studies on GPS-based activity space. It is suggested that micro street-level features may impact on how individuals perceive and interact with the urban context (Llobera, 2003, Ewing et al., 2006), thus we assumed that the 50-meter buffer can effectively capture the street-level environments, especially in the settings of New York City. In addition, previous studies on GPS-based mobility described that the 50-buffer can avoid potential dependence of the urban environmental characteristics between consecutive points when assessing neighborhood exposures from walking activity (Rodriguez et al., 2012, Troped et al., 2010). As the estimates may be sensitive to the sizes of buffer due to the modifiable areal unit problem (Wong, 2009), we also ran sensitivity analyses for different buffer sizes, and reported in the supplement table. The activity space sizes (i.e., the sizes of the daily path area) were expressed in square kilometers (km2), based on Universal Transverse Mercator (UTM) zone 18N projection, one of two-dimensional Cartesian coordinate systems corresponding to New York City metropolitan area. All GPS data processing and cleaning were conducted using ESRI ArcGIS 10.4 and Quantum QGIS 2.6.
Figure 1.
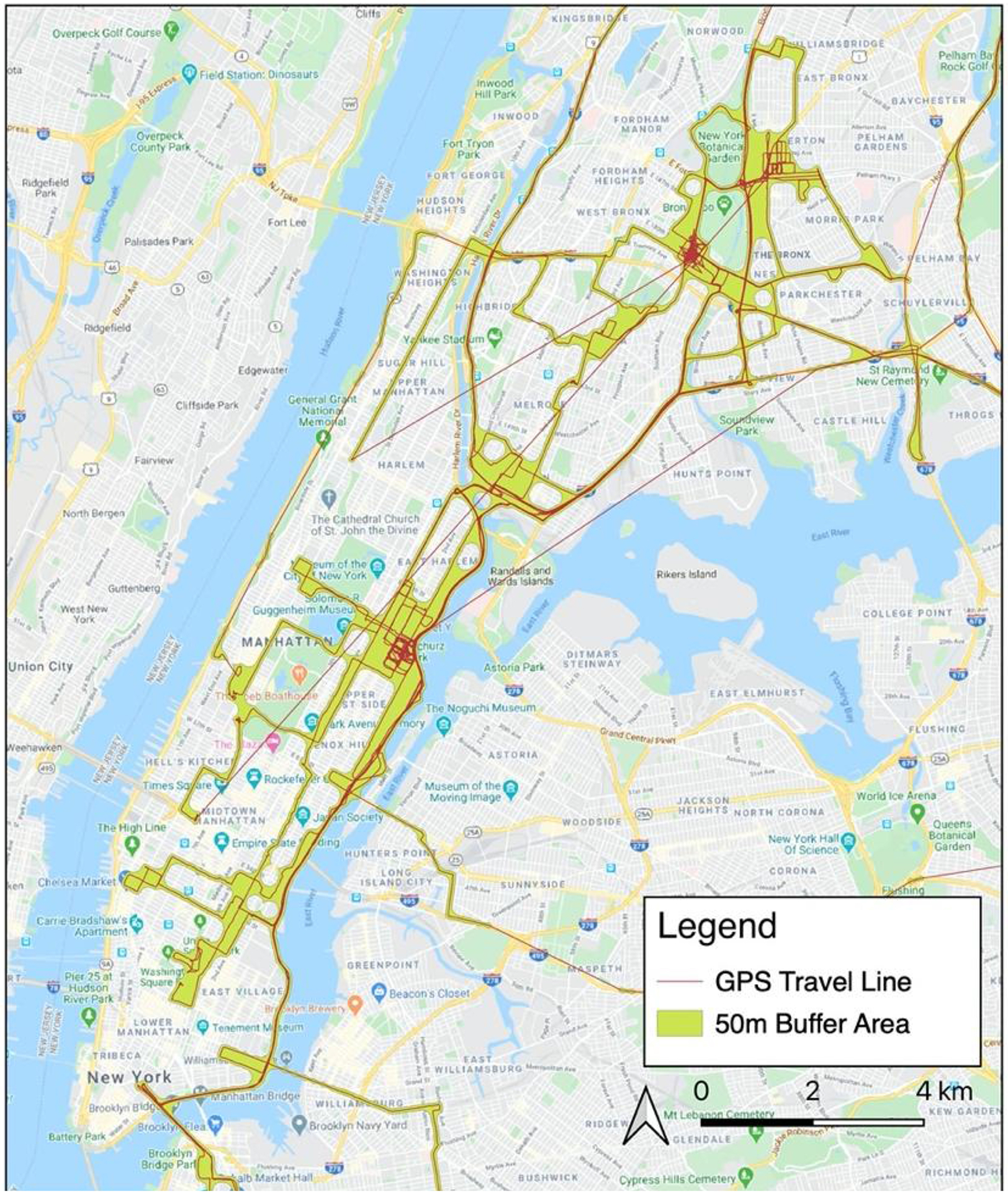
Example map of distance travelled and 50m buffer activity space
Sexual behavior outcomes
In this study, we focused on sexual behaviors associated with risk of HIV infection among MSM. The Project 18 Cohort Study collected data on sexual behaviors including number of male sexual partners and number of condomless sexual encounters in past six months. The number of male sexual partners was assessed from two questions: (1) “In the past 6 months, how many male steady partners have you have anal or oral sex with?,” (2) “In the past 6 months, how many casual male partners have you had anal or oral sex with?”. The total number from those two questions was used as one outcome and was considered a count type variable in the analyses (Koblin et al., 2006; Vittinghoff et al., 1999; Page-Shafer et al., 1997; Kuiken et al., 1990; Darrow et al., 1987). In addition, numbers and types of sexual encounters were assessed to create three variables: total numbers of condomless anal intercourse (CAI) acts, (2) total numbers of condomless insertive anal intercourse (CIAI) acts, and (3) total number of condomless receptive anal intercourse (CRAI) acts in past six months (Patel et al., 2014; Koblin et al., 2006; Vittinghoff et al., 1999; Page-Shafer et al., 1997; Kuiken et al., 1990; Darrow et al., 1987).
Covariates
Participants reported their socio-demographic characteristics, such as age (years), ethnicity (Hispanic or non-Hispanic), race (Black, Asian, White, and others), education attainment (high school or less, some college/ technical school, college degree or more), current school enrollment status (yes/no), and foreign-born status (yes/no). Homelessness was also included in the analyses, as it is an important factor of mobility and risk behaviors (Aidala et al., 2005). Self-reported total individual annual income was categorized as less than $15,000, between $15,000 and $35,000, more than $35,000 per year, which approximates national poverty level (<$15,000) (U.S. Department of Health and Human Services, 2017). The national poverty level is criterion of various social support programs, such as Supplemental Nutrition Assistance Program (SNAP) and Home Energy Assistance Program (HEAP), thus the categorical value may reflect people who were eligible for such programs (Falk and Aussenberg, 2013).
Other potential confounders were included: drug use (any type of substance in any form except marijuana) in the past 6-months (yes/no), numbers of alcoholic drinks in the past 30 days, and number of days of experiencing mental health problems (stress, depression, and emotional problems in the past 30 days). In addition, participants’ sexual identification (gay or bisexual) and relationship status (currently having a main romantic partner) were included in the analyses (Harawa et al., 2008; Everett, 2013; Mustanski et al., 2011; Hoff et al., 2012).
Lastly, residential self-selection of individual, which describes that people choose where to live based on their travel needs and preferences, may influence the mobility patterns and health behaviors (Boone-Heinonen et al., 2011; Mokhtarian and Cao, 2008), thus two ordinal variables were included: (1) “How important was housing price to you when choosing to live in your current neighborhood?” and (2) “How important was living in the city center to you when choosing to live in your current neighborhood?”. Response options for the two questions were (1) not at all important, (2) not too important, (3) somewhat important, (4) mostly important, and (5) very important. All abovementioned variables were included in the multivariate models.
Statistical Analyses
Descriptive statistics were generated to summarize data of the study. In order to identify associations between spatial mobility and sexual risk behaviors, quasi-Poisson regression models were fitted with a logarithmic link function, and for CAI, CIAI, and CRAI models, total number of anal intercourse acts was included as an offset variable. We examined bivariate and multivariable models of different mobility measures with covariates. Adjusted multivariate models were fitted with abovementioned covariates. Lastly, we tested effect modification between the exposure and two potential modifiers (sexual identification and relationship status) using multiplicative interaction terms. All estimates are presented with 95% confidence intervals (CIs). All statistical analyses were conducted using R.3.3.2 with built-in functions including “glm” for quasi-Poisson modeling.
Results
Socio-demographic characteristics of participants are shown on Table 1. The average distance traveled during the two-week monitoring period was 400.9 kilometers and the size of activity spaces for 50, 100, 200, and 400 m buffers were 6.0 km2, 9.4 km2, 16.3 km2, 29.2 km2, respectively. Participants reported an average of 5.6 male sexual partners in the past six months (standard deviation [SD]: 7.1). Over the same period, participants engaged in CAI an average of 15.1 times (SD: 25.9), including 8.3 CIAI acts (SD: 18.1) and 7.0 CRAI acts (SD: 13.8). The sample was relatively young (mean age of 24.9, SD=0.9) and mostly gay (84%). The participants were diverse in terms of race/ethnicity; 32% White, 30% Black, 17% others, 10% Asian; and 30% Hispanic/Latino.
Table 1.
Socio-demographic characteristics, activity space size, and sexual risk behaviors, The P18 Neighborhood Study (n=211)
| Variables | Levels | Mean (SD) or N (%) |
|---|---|---|
| Age | In years, min=23, max=26 | 24.9 (0.9) |
| Race | White | 67 (32%) |
| Black/African American | 64 (30%) | |
| Others | 35 (17%) | |
| Asian | 21 (10%) | |
| Two or more | 21 (10%) | |
| Ethnicity | Non-Hispanic/Latino | 148 (70%) |
| Hispanic/Latino | 63 (30%) | |
| Annual income (total, individual) | <$15,000 | 51 (24%) |
| $15,000 – $35,000 | 70 (33%) | |
| >$35,000 | 76 (36%) | |
| Current student | Yes | 52 (25%) |
| Education | ≤ High School | 71 (34%) |
| Associate | 23 (11%) | |
| College/Graduate | 116 (55%) | |
| Homeless | Yes | 7 (3%) |
| Foreign-born | Yes | 30 (14%) |
| Drug use in the past 6 months | Yes | 101 (48%) |
| Alcohol use in the past 30 days | Number of drinks | 8.3 (7.5) |
| Experience of mental health issues | Number of days | 5.0 (7.5) |
| Sexual identity | Gay | 177 (84%) |
| Bisexual | 30 (14%) | |
| Relationship type | Has a romantic partner | 77 (36%) |
| Distance traveled | (in km2) | 400.9 (224.9) |
| Importance of price in current housing choice | Not at all important | 13 (6%) |
| Nott too important | 4 (2%) | |
| Somewhat important | 39 (18%) | |
| Mostly important | 45 (21%) | |
| Very important | 92 (44%) | |
| Importance of being city center in current | Not at all important | 25 (12%) |
| housing choice | Nott too important | 55 (26%) |
| Somewhat important | 59 (28%) | |
| Mostly important | 33 (16%) | |
| Very important | 27 (13%) | |
| 50m activity space size | (in km2) | 6.0 (5.1) |
| 100m activity space size | (in km2) | 9.4 (8.2) |
| 200m activity space size | (in km2) | 16.3 (14.1) |
| 400m activity space size | (in km2) | 29.2 (24.3) |
| Number of male sexual partners | In the past 6 months | 5.6 (7.1) |
| Number of CAI | In the past 6 months | 15.1 (25.9) |
| Number of CIAI | In the past 6 months | 8.3 (18.1) |
| Number of CRAI | In the past 6 months | 7.0 (13.8) |
SD: standard deviation,
CAI: condomless anal intercourse,
CIAI: condomless insertive anal intercourse,
CRAI: condomless receptive anal intercourse
Table 2 describes the results of quasi-Poisson models for the associations between distance traveled and sexual risk behaviors. From the multivariate models, distance traveled during the two-week period was not associated with the number of male sexual partners. The total distance traveled was associated with CAI acts and CIAI acts. The number of CAI acts increased by 1% per additional 10 kilometers traveled (IRR: 1.01, 95% CI: 1.00–1.02) and the number of CIAI acts increased by 2% from the full models.
Table 2.
Quasi-Poisson model results for associations between distance traveled and sexual risk behaviors, The P18 Neighborhood Study (n=211)
| Incidence rate ratio (IRR) for 10km increase in distance travelled | ||||
|---|---|---|---|---|
| Sexual Partner | CAI | CIAI | CRAI | |
| Bivariate Model | ||||
| Distance Travelled | 1.01 (1.00, 1.01) | 1.01 (1.00, 1.01) | 1.00 (0.99, 1.01) | 1.01 (1.01, 1.02)* |
| Full Model | ||||
| Distance Travelled | 1.00 (0.99, 1.01) | 1.01 (1.00, 1.02)* | 1.02 (1.01, 1.03)* | 1.01 (1.00, 1.02) |
| Age (years) | 0.82 (0.65, 1.04) | 1.24 (1.03, 1.50)* | 1.59 (1.25, 2.04)* | 0.96 (0.74, 1.25) |
| Race | ||||
| White | REF | REF | REF | REF |
| Black | 0.39 (0.21, 0.71)* | 0.62 (0.35, 1.08) | 0.71 (0.35, 1.39) | 0.47 (0.21, 1.02) |
| Others | 0.58 (0.26, 1.24) | 1.35 (0.75, 2.40) | 2.23 (1.08, 4.62)* | 0.59 (0.27, 1.25) |
| Asian | 0.42 (0.16, 0.91) | 0.35 (0.16, 0.70)* | 0.32 (0.11, 0.76)* | 0.59 (0.22, 1.43) |
| Two or more | 0.43 (0.20, 0.86) | 1.38 (0.77, 2.40) | 1.67 (0.89, 3.06) | 0.87 (0.34, 2.06) |
| Ethnicity | ||||
| Non-Hispanic | REF | REF | REF | REF |
| Hispanic | 0.99 (0.58, 1.62) | 0.66 (0.45, 0.95)* | 0.76 (0.47, 1.20) | 0.96 (0.56, 1.62) |
| Annual income | ||||
| < $15,000 | REF | REF | REF | REF |
| $15,000 – $35,000 | 0.75 (0.42, 1.36) | 1.07 (0.69, 1.67) | 0.94 (0.51, 1.74) | 1.23 (0.74, 2.05) |
| >$35,000 | 0.83 (0.48, 1.47) | 0.90 (0.58, 1.43) | 1.02 (0.57, 1.87) | 0.79 (0.44, 1.41) |
| Current student (yes) | 0.61 (0.34, 1.06) | 1.11 (0.73, 1.67) | 0.55 (0.31, 0.95) | 2.36 (1.38, 4.07)* |
| Education | ||||
| Less than high school | REF | REF | REF | REF |
| Associate | 1.31 (0.60, 2.78) | 0.82 (0.42, 1.55) | 0.87 (0.35, 2.04) | 1.41 (0.59, 3.23) |
| College/Graduate | 0.99 (0.59, 1.73) | 0.92 (0.64, 1.36) | 1.25 (0.75, 2.14) | 0.66 (0.40, 1.12) |
| Homeless (yes) | 1.12 (0.20, 3.94) | 0.68 (0.26, 1.66) | 1.42 (0.45, 4.10) | 0.09 (0.01, 0.45)* |
| Foreign-born (yes) | 0.98 (0.52, 1.90) | 0.69 (0.40, 1.22) | 0.62 (0.32, 1.23) | 1.21 (0.59, 2.61) |
| Drug use in 6 months (yes) | 1.54 (1.03, 2.34)* | 1.25 (0.88, 1.78) | 1.45 (0.92, 2.33) | 0.90 (0.56, 1.46) |
| Alcohol use (drinks/month) | 0.99 (0.96, 1.02) | 1.00 (0.98, 1.02) | 0.94 (0.91, 0.97)* | 1.05 (1.02, 1.08)* |
| Days of mental health issues | 1.01 (0.98, 1.04) | 1.00 (0.97, 1.03) | 1.01 (0.97, 1.05) | 1.01 (0.97, 1.05) |
| Sexual identity | ||||
| Gay | REF | REF | REF | REF |
| Bisexual | 0.83 (0.39, 1.58) | 0.56 (0.29, 1.01) | 1.25 (0.65, 2.26) | 0.02 (0.00, 0.18)* |
| Romantic Partner (yes) | 0.71 (0.48, 1.06) | 1.85 (1.28, 2.73)* | 1.60 (0.97, 2,75) | 2.85 (1.74, 4.82)* |
CAI: condomless anal intercourse, CIAI: condomless insertive anal intercourse, CRAI: condomless receptive anal intercourse.
Table 3 shows model results with activity space size, measured as 50m buffer daily path area. Activity space size was associated with the number of male sexual partners from the full model (IRR:1.04, CI: 1.00–1.08). Activity space size was associated with the number of CAI acts (IRR: 1.04, CI: 1.01–1.06). In particular, the number of CIAI acts increased by 5% (IRR: 1.05; 95% CI: 1.01–1.09) for each additional square kilometer increase in activity space size as defined with a 50-meter buffer from the full model. The number of CRAI acts was not associated with the activity space size from the full model. The association of interest between activity space size and sexual risk behaviors tended to decrease, as the radius considered defining the daily path area was larger (Supplemental Table 1), yet the direction of coefficients and confidence intervals remain consistent with main findings.
Table 3.
Quasi-Poisson model results for associations between activity space sizes (50m-buffer) and sexual risk behaviors, The P18 Neighborhood Study (N=211)
| Incidence rate ratio (IRR) for 1km2 increase in activity space size | ||||
|---|---|---|---|---|
| Sexual Partner | CAI | CIAI | CRAI | |
| Bivariate Model | ||||
| Activity Space Size (50m) | 1.03 (1.01, 1.06)* | 1.02 (1.00, 1.03) | 0.99 (0.96, 1.02) | 1.04 (1.02, 1.06)* |
| Full Model | ||||
| Activity Space Size (50m) | 1.04 (1.00, 1.08)* | 1.04 (1.01, 1.06)* | 1.05 (1.01, 1.09)* | 1.03 (0.99, 1.07) |
| Age (years) | 0.82 (0.66, 1.01) | 1.20 (0.99, 1.46) | 1.55 (1.19, 2.04)* | 0.94 (0.72, 1.22) |
| Race | ||||
| White | REF | REF | REF | REF |
| Black | 0.39 (0.22, 0.67)* | 0.59 (0.33, 1.02) | 0.66 (0.31, 1.32) | 0.46 (0.20. 0.99)* |
| Others | 0.57 (0.28,1.15) | 1.14 (0.64, 2.00) | 1.86 (0.89, 3.83) | 0.49 (0.22, 1.05) |
| Asian | 0.43 (0.18, 0.90)* | 0.36 (0.16, 0.75)* | 0.38 (0.12, 1.01) | 0.49 (0.18, 1.26) |
| Two or more | 0.45 (0.22, 0.86)* | 1.34 (0.75, 2.34) | 1.60 (0.82, 3.05) | 0.82 (0.33, 1.93) |
| Ethnicity | ||||
| Non-Hispanic | REF | REF | REF | REF |
| Hispanic | 1.09 (0.67, 1.72) | 0.80 (0.52, 1.20) | 1.06 (0.62, 1.78) | 0.97 (0.52, 1.77) |
| Annual income | ||||
| < $15,000 | REF | REF | REF | REF |
| $15,000 – $35,000 | 0.69 (0.39, 1.21) | 1.10 (0.70, 1.73) | 0.84 (0.43, 1.66) | 1.30 (0.80, 2.14) |
| >$35,000 | 0.78 (0.47, 1.33) | 0.87 (0.54, 1.39) | 0.85 (0.44, 1.68) | 0.77 (0.43, 1.37) |
| Current student (yes) | 0.65 (0.38, 1.08) | 1.26 (0.84, 1.89) | 0.78 (0.45, 1.33) | 2.42 (1.42, 4.16)* |
| Education | ||||
| Less than high school | REF | REF | REF | REF |
| Associate | 1.31 (0.53, 2.66) | 0.90 (0.45, 1.73) | 0.99 (0.38, 2.41) | 1.46 (0.61, 3.27) |
| College/Graduate | 1.02 (0.63, 1.71) | 0.97 (0.67, 1.44) | 1.41 (0.82, 2.50) | 0.67 (0.40, 1.13) |
| Homeless (yes) | 1.11 (0.23, 3.68) | 0.55 (0.21, 1.36) | 1.04 (0.31, 3.23) | 0.08 (0.01, 0.37)* |
| Foreign-born (yes) | 1.04 (0.57, 1.93) | 0.82 (0.46, 1.49) | 0.71 (0.34, 1.49) | 1.45 (0.67, 3.38) |
| Drug use in 6 months (yes) | 1.50 (1.03, 2.22)* | 1.08 (0.77, 1.52) | 1.10 (0.70, 1.77) | 0.82 (0.51, 1.31) |
| Alcohol use (drinks/month) | 0.99 (0.96, 1.02) | 1.00 (0.97, 1.02) | 0.94 (0.91, 0.98)* | 1.05 (1.02, 1.08)* |
| Days of mental health issues | 1.01 (0.98, 1.04) | 1.00 (0.97, 1.03) | 1.01 (0.97, 1.05) | 1.02 (0.98, 1.06) |
| Sexual identity | ||||
| Gay | REF | REF | REF | REF |
| Bisexual | 0.78 (0.39, 1.44) | 0.62 (0.31, 1.14) | 1.37 (0.66, 2.62) | 0.03 (0.00, 0.19)* |
| Romantic Partner (yes) | 0.69 (0.47, 0.99)* | 1.70 (1.15, 1.14)* | 1.32 (0.78, 2.34) | 2.87 (1.67, 5.10)* |
CAI: condomless anal intercourse, CIAI: condomless insertive anal intercourse, CRAI: condomless receptive anal intercourse.
The coefficients of covariates showed similar directions and trends from both the distance travelled and the activity space size models (Table 2 and 3). Drug use was positively associated with the number of sexual partners, and presence of romantic partner was positively associated with CAI. Increased age was associated with higher numbers of CIAI. Alcohol use was negatively associated with CIAI, while it is positively associated with CRAI. School enrollment status and presence of romantic partner were strong and positive predictors of CRAI. Lastly, the multivariate models with multiplicative interaction terms showed no interactions between geographic mobility and the two potential effect modifiers; sexual identification and presence of romantic partner (data not shown).
Discussion
This study examined mobility-related correlates of sexual risk behaviors among a sample of HIV-negative young MSM in New York City. From our models, we found that higher local daily mobility, defined as longer distance traveled and larger activity space sizes, was correlated with increased total numbers of CAI acts. Despite the relatively small effect sizes, these finding suggest that local daily mobility is predictor of sexual behaviors of young MSM in New York City.
Spatial mobility may be related to sexual risk networks, as greater mobility may be associated with expanded sexual networks (Cassels et al., 2017, Vaughan et al., 2017). Formation of sexual networks is linked to spatial mobility, and people with greater spatial mobility are likely to develop more social ties in different places (Gesink et al., 2019, Belot and Ermisch, 2009, Carrasco et al., 2008, Larsen et al., 2006). The total number of CAI may also be related to potential engagement in risky sexual networks in different places. Our findings are consistent with existing findings on mobility and risk of HIV infection. Previous studies found that MSM with high mobility were at higher risk for HIV infection (Ramesh et al., 2014; Mustanski et al., 2015) and MSM who travel for leisure engage in more frequent sexual risk behaviors than those who do not (Benotsch et al., 2006b; Benotsch et al., 2006a; Benotsch et al., 2011; Harry-Hernandez et al., 2019).
In addition, personality may play an important role in determining both mobility and sexual risk behaviors. Under this hypothesis, the mobility measures would reflect aspects of the personality that are also related to sexual risk behaviors (e.g., a preference for new and exciting experiences may lead an individual to meet sexual partners in different neighborhoods and a proclivity for CAI). However, it should be mentioned that visiting several places with sexual purposes during the GPS observation period might have contributed to increased local daily mobility. To illustrate, large proportions of young MSM in the U.S. uses diverse range of social networking smartphone applications to meet male partners, and such internet or app-users may be more likely to have higher mobility compared to non-users (Duncan et al., 2018a; Benotsch et al., 2011; Card et al., 2018). The latter particular case does not correspond to a causal effect of spatial mobility behavior on sexual risk behavior.
This study is not without limitations. First, the study was conducted in New York City, and participants were sampled from HIV-negative and mobile young MSM. Thus, our findings may not be generalizable to other environments, such as small cities and rural areas, and other MSM populations including those who are HIV-positive, older, or disabled. Second, the measured mobility does not capture the content of experiences of participants within neighborhoods. In other words, we did not investigate the characteristics of neighborhood exposures, such as social and physical features of neighborhoods that participants visited, or the types of places that participants visited and related activities. Studies suggest that the venue of partner meeting plays role in shaping sexual risk behaviors (Al-Ajlouni et al., 2018b; Grov et al., 2007; Colfax et al., 2001), however, the increased spatial mobility did not reflect actual exposures to risky environments; rather, it may indicate longer commutes or travel routes. Previous studies suggested that higher mobility may be associated with lack of conventional social supports for HIV prevention (Frye et al., 2014; Vaughan et al., 2017), however, we were not able to ascertain the differential social environments of diverse neighborhood exposures. Also, although the two-week monitoring period is relatively long compared to most health studies using GPS (Duncan et al., 2018b), the measured mobility assessed over the period may not represent participants’ typical travel behaviors. However, a recent study by Zenk et al. (2018) reported that a two-week period is adequate to measure individual travel behavior. Third, the GPS protocol was designed for 2-week data collection, but not all participants engaged in the full-period tracking. We did not standardize the distance traveled and activity space size by number of days of tracking. Fourth, GPS signal errors and data losses may be introduced due to special settings in large metropolitan locations such as subway, underground, and large buildings (Georgiadou and Kleusberg, 1988). Despite the GPS error, we processed the data to maximize reliability by eliminating isolated points and duplicated timestamps. Lastly, there are several limitations inherent in any cross-sectional survey including difficulties to infer causality. We were not able to examine temporal association between the mobility behaviors and sexual risk behaviors, and so it remains possible as discussed above that sexual risk behaviors, especially the willingness to have a large number of partners, may have influenced the size of the activity space captured over the monitoring period due to participants travelling to meet their sexual partners.
Our study also has numerous strengths, including assessing the objective measure of local daily mobility, a large sample size for a sensor-based study, and a relatively long period of GPS tracking period (Zenk et al., 2018; Duncan et al., 2018b). To our knowledge, this study is the largest GPS study to examine the association between objectively measured mobility and sexual risk behaviors in any MSM population. The GPS protocol allowed 10-second epochs, in which high monitoring frequency enhanced the overall quality of the GPS data. Moreover, the two-week monitoring period was longer than most existing GPS studies that typically monitor participants over one week, capturing more variations of travel behavior of participants. This is a significant step forward beyond place-based analysis based on residential administrative boundaries such as census tracts or ZIP codes.
As noted above, further studies should be conducted to examine the effects of different neighborhoods and meeting venues including residential, work, social, and sexual contexts to understand actual influences of neighborhoods. In addition, temporal dimensions (e.g. duration) of exposure can be tested with the GPS data to test dose-response associations. Social and physical characteristics of the various neighborhoods will have to be considered, on the basis of the GPS data that we collected, for instance population density, HIV prevalence, crime rates, neighborhood disorder, racial segregation, and proximity to clinical and social services (Duncan et al., Forthcoming). One could test psychosocial factors and social network characteristics that may shape sexual health behaviors in order to increase our level of understanding of the impact of socio-spatial contexts on the sexual risk behaviors. Additionally, GPS-based ecological momentary assessment (EMA) method will be helpful to better understand the actual exposures to neighborhood characteristics (Duncan et al., 2019). Lastly, longitudinal studies should be conducted to investigate causal influences over time of spatial mobility behavior and socio-spatial contexts on sexual risk behaviors.
Conclusions
Our innovative study found that local daily mobility was associated with sexual risk behaviors, confirming the role of geographic mobility in the context of the HIV epidemic among MSM in the U.S. Future research should seek to understand the impacts of different types of neighborhoods and places visited on HIV risk behaviors using this mobility-based approaches in order to enhance place-based HIV prevention by allowing specific target places for interventions.
Supplementary Material
Highlights.
GPS-based spatial mobility was positively associated with sexual risk behaviors.
Findings confirm the spatial contexts of HIV risks in urban environments.
Future studies may guide the place-based HIV prevention services.
Acknowledgements
This study was funded by the National Institute of Mental Health, Award #R21MH110190 awarded to Dustin T. Duncan. Mr. Byoungjun Kim is supported in part by the NYU Training Program in Healthcare Delivery Science and Population Health funded by Agency for Healthcare Research and Quality (Grant Number T32HS026120; Leora Horwitz, MD and Mark Schwartz, MD, Principal Investigators). In addition, Mr. Goedel is supported by the Brown University Clinical and Community-Based HIV/AIDS Research Training Fellowship (funded by the National Institute of Mental Health, Award #R25MH awarded to Amy S. Nunn). The authors would like to thank the participants of the study that contributed to the project.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Reference
- AIDALA A, CROSS JE, STALL R, HARRE D & SUMARTOJO E 2005. Housing status and HIV risk behaviors: implications for prevention and policy. AIDS Behav, 9, 251–65. [DOI] [PubMed] [Google Scholar]
- AL-AJLOUNI YA, PARK SH, SCHNEIDER JA, GOEDEL WC, HAMBRICK HR, HICKSON DA, CANTOR MN & DUNCAN DT 2018a. Partner meeting venue typology and sexual risk behaviors among French men who have sex with men. International Journal of STD & AIDS, 29, 1282–1288. [DOI] [PubMed] [Google Scholar]
- AL-AJLOUNI YA, PARK SH, SCHNEIDER JA, GOEDEL WC, RHODES HAMBRICK H, HICKSON DA, CANTOR MN & DUNCAN DT 2018b. Partner meeting venue typology and sexual risk behaviors among French men who have sex with men. International Journal of STD & AIDS, 29, 1282–1288. [DOI] [PubMed] [Google Scholar]
- BELOT M & ERMISCH J 2009. Friendship ties and geographical mobility: evidence from Great Britain. Journal of the Royal Statistical Society Series a-Statistics in Society, 172, 427–442. [Google Scholar]
- BENOTSCH EG, MARTIN AM, ESPIL FM, NETTLES CD, SEAL DW & PINKERTON SD 2011. Internet Use, Recreational Travel, and HIV Risk Behaviors in Men Who Have Sex With Men. Journal of Community Health, 36, 398–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BENOTSCH EG, MIKYTUCK JJ, RAGSDALE K & PINKERTON SD 2006a. Sexual risk and HIV acquisition among men who have sex with men travelers to Key West, Florida: A mathematical modeling analysis. AIDS Patient Care and STDs, 20, 549–556. [DOI] [PubMed] [Google Scholar]
- BENOTSCH EG, SEELEY S, MIKYTUCK JJ, PINKERTON SD, NETTLES CD & RAGSDALE K 2006b. Substance use, medications for sexual facilitation, and sexual risk behavior among traveling men who have sex with men. Sexually Transmitted Diseases, 33, 706–711. [DOI] [PubMed] [Google Scholar]
- BOONE-HEINONEN J, GORDON-LARSEN P, GUILKEY DK, JACOBS DR & POPKIN BM 2011. Environment and physical activity dynamics: The role of residential self-selection. Psychology of Sport and Exercise, 12, 54–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BORUFF BJ, NATHAN A & NIJËNSTEIN S 2012. Using GPS technology to (re)-examine operational definitions of ‘neighbourhood’in place-based health research. International Journal of Health Geographics, 11, 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CAMLIN CS, KWENA ZA & DWORKIN SL 2013. Jaboya Vs. Jakambi: Status, Negotiation, and Hiv Risks among Female Migrants in the “Sex for Fish” Economy in Nyanza Province, Kenya. AIDS Education and Prevention, 25, 216–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CARD KG, GIBBS J, LACHOWSKY NJ, HAWKINS BW, COMPTON M, EDWARD J, SALWAY T, GISLASON MK & HOGG RS 2018. Using Geosocial Networking Apps to Understand the Spatial Distribution of Gay and Bisexual Men: Pilot Study. JMIR Public Health Surveill, 4, e61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CARRASCO JA, MILLER EJ & WELLMAN B 2008. How Far and with Whom Do People Socialize? Empirical Evidence About Distance Between Social Network Members. Transportation Research Record, 114–122. [Google Scholar]
- CASSELS S & CAMLIN CS 2016. Geographical mobility and heterogeneity of the HIV epidemic. Lancet HIV, 3, E339–E341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CASSELS S, JENNESS SM, BINEY AAE & DODOO FNA 2017. Geographic mobility and potential bridging for sexually transmitted infections in Agbogbloshie, Ghana. Social Science & Medicine, 184, 27–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CENTERS FOR DISEASE CONTROL AND PREVENTION 2019. HIV Surveillance Reports: Diagnoses of HIV Infection in the United States and Dependent Areas, 2018 (Preliminary).
- CHAIX B, MELINE J, DUNCAN S, MERRIEN C, KARUSISI N, PERCHOUX C, LEWIN A, LABADI K & KESTENS Y 2013. GPS tracking in neighborhood and health studies: A step forward for environmental exposure assessment, a step backward for causal inference? Health & Place, 21, 46–51. [DOI] [PubMed] [Google Scholar]
- COFFEE M, LURIE MN & GARNETT GP 2007. Modelling the impact of migration on the HIV epidemic in South Africa. AIDS, 21, 343–350. [DOI] [PubMed] [Google Scholar]
- COLFAX GN, MANSERGH G, GUZMAN R, VITTINGHOFF E, MARKS G, RADER M & BUCHBINDER S 2001. Drug use and sexual risk behavior among gay and bisexual men who attend circuit parties: A venue-based comparison. Journal of Acquired Immune Deficiency Syndromes, 28, 373–379. [DOI] [PubMed] [Google Scholar]
- DARROW WW, ECHENBERG DF, JAFFE HW, O’MALLEY PM, BYERS RH, GETCHELL JP & CURRAN JW 1987. Risk factors for human immunodeficiency virus (HIV) infections in homosexual men. Am J Public Health, 77, 479–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DEANE KD, PARKHURST JO & JOHNSTON D 2010. Linking migration, mobility and HIV. Tropical Medicine & International Health, 15, 1458–1463. [DOI] [PubMed] [Google Scholar]
- DUNCAN D, KIM B, AL-AJLOUNI Y & CALLANDER D Forthcoming. Neighborhood-Level Structural Factors, HIV and Communities of Color In: OJIKUTU B & STONE V (eds.) HIV/AIDS in US Communities of Color. 2n Edition ed.: Springer. [Google Scholar]
- DUNCAN DT, KAPADIA F & HALKITIS PN 2014. Examination of Spatial Polygamy among Young Gay, Bisexual, and Other Men Who Have Sex with Men in New York City: The P18 Cohort Study. International Journal of Environmental Research and Public Health, 11, 8962–8983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DUNCAN DT, KAPADIA F, REGAN SD, GOEDEL WC, LEVY MD, BARTON SC, FRIEDMAN SR & HALKITIS PN 2016. Feasibility and Acceptability of Global Positioning System (GPS) Methods to Study the Spatial Contexts of Substance Use and Sexual Risk Behaviors among Young Men Who Have Sex with Men in New York City: A P18 Cohort Sub-Study. PLoS One, 11, e0147520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DUNCAN DT, PARK SH, GOEDEL WC, SHEEHAN DM, REGAN SD & CHAIX B 2019. Acceptability of smartphone applications for global positioning system (GPS) and ecological momentary assessment (EMA) research among sexual minority men. PLoS One, 14, e0210240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DUNCAN DT, PARK SH, HAMBRICK HR, DANGERFIELD DT, GOEDEL WC, BREWER R, MGBAKO O, LINDSEY J, REGAN SD & HICKSON DA 2018a. Characterizing Geosocial-Networking App Use Among Young Black Men Who Have Sex With Men: A Multi-City Cross-Sectional Survey in the Southern United States. JMIR Mhealth and Uhealth, 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DUNCAN DT, REGAN SD & CHAIX B 2018b. Operationalizing neighborhood definitions in health research: Spatial misclassification and other issues Neighborhoods and Health. Oxford University Press. [Google Scholar]
- EVERETT BG 2013. Sexual Orientation Disparities in Sexually Transmitted Infections: Examining the Intersection Between Sexual Identity and Sexual Behavior. Archives of Sexual Behavior, 42, 225–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- EWING R, HANDY S, BROWNSON RC, CLEMENTE O & WINSTON E 2006. Identifying and Measuring Urban Design Qualities Related to Walkability. J Phys Act Health, 3, S223–S240. [DOI] [PubMed] [Google Scholar]
- FALK G & AUSSENBERG R 2013. The Supplemental Nutrition Assistance Program: categorical eligibility. Congressional Research Service. [Google Scholar]
- FRYE V, EGAN JE, TIEU HV, CERDA M, OMPAD D & KOBLIN BA 2014. “I didn’t think I could get out of the fucking park.” Gay men’s retrospective accounts of neighborhood space, emerging sexuality and migrations. Social Science & Medicine, 104, 6–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GEORGIADOU Y & KLEUSBERG A 1988. On carrier signal multipath effects in relative GPS positioning. Manuscripta Geodaetica, 13, 172–179. [Google Scholar]
- GESINK D, SALWAY T, KIMURA L, CONNELL J, WIDENER M & FERLATTE O 2019. The Social Geography of Partner Selection in Toronto, Canada: A Qualitative Description of “Convection Mixing”. Archives of Sexual Behavior. [DOI] [PubMed] [Google Scholar]
- GROV C, PARSONS JT & BIMBI DS 2007. Sexual risk behavior and venues for meeting sex partners: An intercept survey of gay and bisexual men in LA and NYC. AIDS and Behavior, 11, 915–926. [DOI] [PubMed] [Google Scholar]
- GUPTA K, VAIDEHI Y & MAJUMDER N 2010. Spatial Mobility, Alcohol Use, Sexual Behavior and Sexual Health Among Males in India. AIDS and Behavior, 14, 18–30. [DOI] [PubMed] [Google Scholar]
- HALKITIS PN, KAPADIA F, SICONOLFI DE, MOELLER RW, FIGUEROA RP, BARTON SC & BLACHMAN-FORSHAY J 2013. Individual, psychosocial, and social correlates of unprotected anal intercourse in a new generation of young men who have sex with men in New York City. Am J Public Health, 103, 889–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HARAWA NT, WILLIAMS JK, RAMAMURTHI HC, MANAGO C, AVINA S & JONES M 2008. Sexual behavior, sexual identity, and substance abuse among low-income bisexual and non-gay-identifying African American men who have sex with men. Archives of Sexual Behavior, 37, 748–762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HARRY-HERNANDEZ S, PARK SH, MAYER KH, KRESKI N, GOEDEL WC, HAMBRICK HR, BROOKS B, GUILAMO-RAMOS V & DUNCAN DT 2019. Sex Tourism, Condomless Anal Intercourse, and HIV Risk Among Men Who Have Sex With Men. Janac-Journal of the Association of Nurses in AIDS Care, 30, 405–414. [DOI] [PubMed] [Google Scholar]
- HIRSCH JA, WINTERS M, CLARKE P & MCKAY H 2014. Generating GPS activity spaces that shed light upon the mobility habits of older adults: a descriptive analysis. International Journal of Health Geographics, 13, 51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HOFF CC, CHAKRAVARTY D, BEOUGHER SC, NEILANDS TB & DARBES LA 2012. Relationship Characteristics Associated with Sexual Risk Behavior Among MSM in Committed Relationships. AIDS Patient Care and STDs, 26, 738–745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- JAISWAL J, GRIFFIN M, SINGER SN, GREENE RE, ACOSTA ILZ, KAUDEYR SK, KAPADIA F & HALKITIS PN 2018. Structural Barriers to Pre-exposure Prophylaxis Use Among Young Sexual Minority Men: The P18 Cohort Study. Current HIV Research, 16, 237–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- JAMES P, JANKOWSKA M, MARX C, HART JE, BERRIGAN D, KERR J, HURVITZ PM, HIPP JA & LADEN F 2016. “Spatial Energetics” Integrating Data From GPS, Accelerometry, and GIS to Address Obesity and Inactivity. American Journal of Preventive Medicine, 51, 792–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- JIA P, XUE H, YIN L, STEIN A, WANG MQ & WANG YF 2019. Spatial Technologies in Obesity Research: Current Applications and Future Promise. Trends in Endocrinology and Metabolism, 30, 211–223. [DOI] [PubMed] [Google Scholar]
- KHAN MR, PATNAIK P, BROWN L, NAGOT N, SALOUKA S & WEIR SS 2008. Mobility and HIV-related sexual behavior in Burkina Faso. AIDS and Behavior, 12, 202–212. [DOI] [PubMed] [Google Scholar]
- KISHAMAWE C, VISSERS DCJ, URASSA M, ISINGO R, MWALUKO G, BORSBOOM GJJM, VOETEN HACM, ZABA B, HABBEMA JDF & DE VLAS SJ 2006. Mobility and HIV in Tanzanian couples: both mobile persons and their partners show increased risk. AIDS, 20, 601–608. [DOI] [PubMed] [Google Scholar]
- KOBLIN BA, EGAN JE, NANDI V, SANG JM, CERDA M, TIEU HV, OMPAD DC, HOOVER DR & FRYE V 2017. Congruence of Home, Social and Sex Neighborhoods among Men Who Have Sex with Men, NYCM2M Study. Journal of Urban Health-Bulletin of the New York Academy of Medicine, 94, 364–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KOBLIN BA, EGAN JE, RUNDLE A, QUINN J, TIEU HV, CERDA M, OMPAD DC, GREENE E, HOOVER DR & FRYE V 2013. Methods to Measure the Impact of Home, Social, and Sexual Neighborhoods of Urban Gay, Bisexual, and Other Men Who Have Sex with Men. PloS One, 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KOBLIN BA, HUSNIK MJ, COLFAX G, HUANG YJ, MADISON M, MAYER K, BARRESI PJ, COATES TJ, CHESNEY MA & BUCHBINDER S 2006. Risk factors for HIV infection among men who have sex with men. AIDS, 20, 731–739. [DOI] [PubMed] [Google Scholar]
- KUIKEN CL, VAN GRIENSVEN GJ, DE VROOME EM & COUTINHO RA 1990. Risk factors and changes in sexual behavior in male homosexuals who seroconverted for human immunodeficiency virus antibodies. Am J Epidemiol, 132, 523–30. [DOI] [PubMed] [Google Scholar]
- LARSEN J, URRY J & AXHAUSEN KW 2006. Mobilities, networks, geographies, Aldershot, England: ; Burlington, VT, Ashgate. [Google Scholar]
- LLOBERA M 2003. Extending GIS-based visual analysis: the concept of visualscapes. International Journal of Geographical Information Science, 17, 25–48. [Google Scholar]
- LYDIE N, ROBINSON NJ, FERRY B, AKAM E, DE LOENZIEN M, ABEGA S & HIV SGOHO 2004. Mobility, sexual behavior, and HIV infection in an urban population in Cameroon. Jaids-Journal of Acquired Immune Deficiency Syndromes, 35, 67–74. [DOI] [PubMed] [Google Scholar]
- MOKHTARIAN PL & CAO XY 2008. Examining the impacts of residential self-selection on travel behavior: A focus on methodologies. Transportation Research Part B-Methodological, 42, 204–228. [Google Scholar]
- MUSTANSKI B, BIRKETT M, KUHNS LM, LATKIN CA & MUTH SQ 2015. The Role of Geographic and Network Factors in Racial Disparities in HIV Among Young Men Who have Sex with Men: An Egocentric Network Study. AIDS and Behavior, 19, 1037–1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MUSTANSKI B, NEWCOMB ME & CLERKIN EM 2011. Relationship characteristics and sexual risk-taking in young men who have sex with men. Health Psychology, 30, 597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PAGE-SHAFER K, VEUGELERS PJ, MOSS AR, STRATHDEE S, KALDOR JM & VAN GRIENSVEN GJ 1997. Sexual risk behavior and risk factors for HIV-1 seroconversion in homosexual men participating in the Tricontinental Seroconverter Study, 1982–1994. Am J Epidemiol, 146, 531–42. [DOI] [PubMed] [Google Scholar]
- PATEL P, BORKOWF CB, BROOKS JT, LASRY A, LANSKY A & MERMIN J 2014. Estimating per-act HIV transmission risk: a systematic review. AIDS, 28, 1509–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- RAMESH S, MEHROTRA P, MAHAPATRA B, GANJU D, NAGARAJAN K & SAGGURTI N 2014. The effect of mobility on sexual risk behaviour and HIV infection: a cross-sectional study of men who have sex with men in southern India. Sexually Transmitted Infections, 90, 491-+. [DOI] [PMC free article] [PubMed] [Google Scholar]
- RODRIGUEZ DA, CHO GH, EVENSON KR, CONWAY TL, COHEN D, GHOSH-DASTIDAR B, PICKREL JL, VEBLEN-MORTENSON S & LYTLE LA 2012. Out and about: Association of the built environment with physical activity behaviors of adolescent females. Health & Place, 18, 55–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAGGURTI N, SCHENSUL SL & VERMA RK 2009. Migration, Mobility and Sexual Risk Behavior in Mumbai, India: Mobile Men with Non-Residential Wife Show Increased Risk. AIDS and Behavior, 13, 921–927. [DOI] [PubMed] [Google Scholar]
- SAGGURTI N, VERMA RK, JAIN A, RAMARAO S, KUMAR KA, SUBBIAH A, MODUGU HR, HALLI S & BHARAT S 2008. HIV risk behaviours among contracted and non-contracted male migrant workers in India: potential role of labour contractors and contractual systems in HIV prevention. AIDS, 22, S127–S136. [DOI] [PubMed] [Google Scholar]
- SCHACHTER J 2001. Geographical Mobility: Population Characteristics. Current Population Reports, US Census Bureau, Washington, DC. [Google Scholar]
- SCHUYLER AC, EDELSTEIN ZR, MATHUR S, SEKASANVU J, NALUGODA F, GRAY R, WAWER MJ, SERWADDA DM & SANTELLI JS 2017. Mobility among youth in Rakai, Uganda: Trends, characteristics, and associations with behavioural risk factors for HIV. Global Public Health, 12, 1033–1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SEELEY JA & ALLISON EH 2005. HIV/AIDS in fishing communities: Challenges to delivering antiretroviral therapy to vulnerable groups. AIDS Care-Psychological and Socio-Medical Aspects of AIDS/HIV, 17, 688–697. [DOI] [PubMed] [Google Scholar]
- SHERMAN JE, SPENCER J, PREISSER JS, GESLER WM & ARCURY TA 2005. A suite of methods for representing activity space in a healthcare accessibility study. Int J Health Geogr, 4, 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SINGH S, SONG R, JOHNSON AS, MCCRAY E & HALL HI 2018. HIV Incidence, Prevalence, and Undiagnosed Infections in U.S. Men Who Have Sex With Men. Ann Intern Med, 168, 685–94. [DOI] [PubMed] [Google Scholar]
- TOBIN KE, CUTCHIN M, LATKIN CA & TAKAHASHI LM 2013. Social geographies of African American men who have sex with men (MSM): A qualitative exploration of the social, spatial and temporal context of HIV risk in Baltimore, Maryland. Health & Place, 22, 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- TOBIN KE, LATKIN CA & CURRIERO FC 2014. An examination of places where African American men who have sex with men (MSM) use drugs/drink alcohol: A focus on social and spatial characteristics. International Journal of Drug Policy, 25, 591–597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- TROPED PJ, WILSON JS, MATTHEWS CE, CROMLEY EK & MELLY SJ 2010. The Built Environment and Location-Based Physical Activity. American Journal of Preventive Medicine, 38, 429–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES 2017. 2017 Poverty Guidelines. VAUGHAN AS, KRAMER MR, COOPER HLP, ROSENBERG ES & SULLIVAN PS 2017. Activity spaces of men who have sex with men: An initial exploration of geographic variation in locations of routine, potential sexual risk, and prevention behaviors. Social Science & Medicine, 175, 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VITTINGHOFF E, DOUGLAS J, JUDSON F, MCKIRNAN D, MACQUEEN K & BUCHBINDER SP 1999. Per-contact risk of human immunodeficiency virus transmission between male sexual partners. American Journal of Epidemiology, 150, 306–311. [DOI] [PubMed] [Google Scholar]
- WONG D 2009. The modifiable areal unit problem (MAUP) In: FOTHERINGHAM AS& ROGERSON PA (eds.) The SAGE handbook of spatial analysis. London: SAGE. [Google Scholar]
- YOUNG LE, MICHAELS S, JONAS A, KHANNA AS, SKAATHUN B, MORGAN E, SCHNEIDER JA & TEAM US 2017. Sex Behaviors as Social Cues Motivating Social Venue Patronage Among Young Black Men Who Have Sex with Men. AIDS and Behavior, 21, 2924–2934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ZENK SN, MATTHEWS SA, KRAFT AN & JONES KK 2018. How many days of global positioning system (GPS) monitoring do you need to measure activity space environments in health research? Health & Place, 51, 52–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


