Abstract
Context
Team-based care has been increasingly used to deliver care for patients with chronic conditions, but its effectiveness for managing diabetes has not been systematically assessed.
Evidence acquisition
RCTs were identified from two sources: a high-quality, broader review comparing 11 quality improvement strategies for diabetes management (database inception to July 2010), and an updated search using the same search strategy (July 2010–October 2015).
Evidence synthesis
Thirty-five studies were included in the current review; a majority focused on patients with Type 2 diabetes. Teams included patients, their primary care providers, and one or two additional healthcare professionals (most often nurses or pharmacists). Random effect meta-analysis showed that, compared with controls, team-based care was associated with greater reductions in blood glucose levels (−0.5% in HbA1c, 95% CI= −0.7, −0.3) and greater improvements in blood pressure and lipid levels. Interventions also increased the proportion of patients who reached target blood glucose, blood pressure, and lipid levels, based on American Diabetes Association guidelines available at the time. Data analysis was completed in 2016.
Conclusions
For patients with Type 2 diabetes, team-based care improves blood glucose, blood pressure, and lipid levels.
CONTEXT
Diabetes is a debilitating chronic disease and a costly burden on the American healthcare system. The individual burdens of living with diabetes, especially if diabetes is uncontrolled, can be severe. Individuals face an increased risk of cardiovascular disease, kidney disease, nerve damage, eye damage that may lead to blindness, foot and skin lesions that may lead to amputation, and death; but the risk is reduced when diabetes is properly managed.1,2 In addition, the estimated cost of diabetes has risen from $174 billion in 2007 to $245 billion in 2012 ($176 billion in direct medical costs and $69 billion in reduced productivity).3,4
In the past decade, while the healthcare system in the U.S. has shifted toward greater payer–provider risk sharing,5 the prevalence for chronic diseases such as diabetes has increased.2 Many provider networks have developed coordinated models of care, such as team-based care (TBC), to pursue the “Triple Aim” of reducing cost, improving health outcomes, and improving patient experience.6
TBC to improve diabetes management is a health systems–level, organizational intervention that incorporates a multidisciplinary team to help patients manage their diabetes. Each team includes the patient, the patient’s primary care provider (not necessarily a physician), and one or more other health professionals. TBC to manage diabetes aims to:
ensure patients receive appropriate tests and examinations (e.g., blood glucose level, blood pressure, lipid level, weight, eye and foot examinations);
manage patients’ risk factors (e.g., blood glucose level, blood pressure, lipid level) through diet, exercise, and medications;
educate and assist patients with self-management and adherence to treatment regimens;
promote patients’ adoption of healthy behaviors and lifestyle choices (e.g., improved diet, increased physical activity, cessation of smoking); and
improve patients’ quality of life and prevent diabetes-related complications.
TBC has been touted as a promising way to treat chronic diseases, such as diabetes. TBC aims to improve support for patients with diabetes and often includes systems support, such as decision tools or information systems. Improved patient support is expected to enhance patients’ overall experience with care and favorably affect health outcomes including glycemic and lipid levels, blood pressure, and weight control; diabetes-related complications and hospitalizations; quality of life; and mortality. This is the first systematic review to broadly examine the effectiveness of TBC in improving health outcomes of people living with diabetes. This review aims to determine whether TBC works, and how it should be implemented to be most effective.
The research questions for this review are as follows: How effective is TBC in improving management of Type 1 or 2 diabetes by improving glycemic and lipid levels, blood pressure, and weight control? How effective is TBC in reducing diabetes-related complications/comorbidities? How effective is TBC in improving quality of life and reducing morbidity and mortality among people with diabetes? Does TBC effectiveness vary by demographic characteristics, such as age, gender, race/ethnicity, SES; team member characteristics, such as profession of added team members; and intervention characteristics, such as intervention duration?
EVIDENCE ACQUISITION
A team of specialists in systematic review methods and subject matter experts in research, practice, and policy related to diabetes management conducted the review on behalf of the Community Preventive Services Task Force—an independent, nonpartisan, nonfederal panel of public health and prevention experts appointed by the director of the Centers for Disease Control and Prevention.
Standard systematic review methods used for the Community Guide have been published previously.7,8
Search For Evidence
The detailed search strategy can be found at https://www.thecommunityguide.org/findings/diabetes-management-team-based-care-patients-type-2-diabetes. The search for evidence consisted of two steps. Step 1 involved locating existing systematic reviews on TBC for diabetes management. Although no existing systematic review specific to TBC and diabetes management was found, a broader, RCTs only review by Tricco and colleagues9 was identified. The review (search period: database inception to July 2010) compared 11 quality improvement strategies for diabetes management and was determined to be of high quality. The review was used as a reference list and screened for publications specific to TBC. For Step 2, the review search strategy by Tricco was adopted, an updated search was conducted (search period July 2010 to October 2015), and search results were screened for RCTs related to TBC. Relevant publications identified from the two steps combined to form this review’s body of evidence. Reference lists of these publications were also searched for qualifying studies.
Two review team members independently screened studies to determine which should be included. Uncertainties and disagreements were decided by consensus among review team members.
Inclusion Criteria
Studies were included if the following criteria were met: focused on people diagnosed with Type 1 or 2 diabetes; conducted in a World Bank–designated high-income economy10 and published in English; RCT; team consisted of patient, primary care provider (not necessarily a physician), and one or more healthcare professionals; team members aware of each other’s roles and responsibilities; relied on multidirectional flow of information to manage patient care; care was ongoing, longitudinal (two or more contacts between patients and added team members); and included one or more outcomes of interest listed below.
Outcomes of interest
This review collected three sets of outcomes. The first set was the pre–post change in various diabetes-related health outcomes: blood glucose as measured by HbA1c % or fasting blood glucose (mg/dL); blood pressure (BP), systolic blood pressure (SBP), and diastolic blood pressure (DBP, mmHg); lipids: low-density lipoprotein, high-density lipoprotein, total cholesterol, and triglycerides (mg/dL or mmol/L converted to mg/dL); and weight (kg or BMI).
The second set was the change in proportion of patients meeting target blood glucose, lipids, BP, and weight outcomes. Authors of the included studies set these targets based on standards available at the time and may not reflect current standards.
The third set is downstream outcomes: quality of life; healthcare use (diabetes-related hospitalization, all-cause hospitalization, all-cause emergency department use); and diabetes-related morbidity (e.g., incidence of neuropathy and foot lesions) and mortality.
Assessing and Summarizing the Body of Evidence on Effectiveness
Study abstraction
Data from each study meeting the inclusion criteria were independently abstracted by two reviewers, with uncertainties and disagreements reconciled by consensus among review team members. Abstraction was based on the standard Community Guide process (www.thecommunityguide.org/methods/abstractionform.pdf). The team collected information on intervention characteristics, study participant demographics, and outcomes.
Quality of execution
Using Community Guide methods,7,8 each study was assessed for threats to internal and external validity, including inadequate description of intervention, population, and sampling frame; inadequate measurement of exposure or outcome; inadequate description or inappropriate use of analytic methods; high attrition; or failure to control for confounding or biasing factors. Because only RCTs were included, additional quality of execution criteria were used, including inadequate reporting of the randomization process, not accounting for missing outcome data because of failure to follow-up, and failure to control for cross-contamination bias. Studies are categorized as having good (zero to one limitations); fair (two to four); or limited (more than four) quality of execution. Studies judged to be of limited quality of execution were excluded from analysis.
Analysis
Included studies that compared TBC interventions with usual care were evaluated. Depending on the outcome examined, a variety of synthesis techniques were employed to summarize the data.
For most of the health-related outcomes (HbA1c, BP, lipids), DerSimonian Laird random effects meta-analysis11 was used to calculate a summary effect estimate, 95% CI, 95% prediction interval, and I2 value. For each study, a net difference in pre–post means was calculated for the effect size. If baseline data were unavailable, mean difference was calculated using post-intervention data. For studies that reported median outcome measures, the team used the value as a mean value and used an approximation to convert the reported IQR to a 95% CI (IQR/1.35=1 SD).12
For weight outcomes, relative changes in either BMI or kilograms were calculated. When at least five independent individual effect estimates were available, interquartile intervals were calculated to provide a measure of variation as per Community Guide methods7,8; otherwise, the range of estimates was indicated.
For the change in proportion of patients meeting target health outcomes, studies with the same targets were grouped together and net absolute percentage point change was calculated. Post-intervention data were used when baseline data were unavailable. Median and interquartile interval were calculated as described above. For all other outcomes, effect sizes were calculated when possible; otherwise, results were reported narratively.
TBC varied in team composition, operation, and care delivery. Stratified analyses examined the influence of these factors on patients’ health-related outcomes. Stratified analyses were conducted using mixed effect meta-analysis. A random effects model was used to produce a summary measure for each stratum, and a fixed effect model was employed to compare the summary measures across strata. Inferential testing of between-strata differences was performed to assess statistical significance. Stratified analyses were conducted to examine the influence of intervention characteristics on change in HbA1c, BP, and lipid outcomes; assess generalizability of review findings in different settings and populations; and explore the source of heterogeneity in health-related outcomes.
Funnel plot analysis was used to test for publication bias (Appendix Figure 1, available online). All analyses were conducted using Microsoft Excel, Professional Plus 2016, and completed in 2016.
EVIDENCE SYNTHESIS
Search Yield
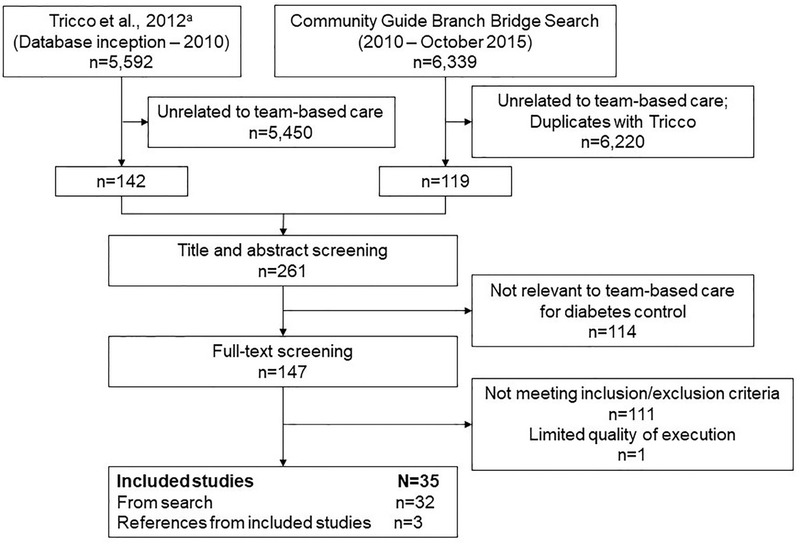
From the review by Tricco et al.,9 the team identified 142 publications that were potentially related to TBC for diabetes management. The updated search yielded a total of 6,339 publications, with 119 identified as potentially relevant. From these two sources, a total of 33 studies met inclusion criteria, with one study13 excluded because of limited quality of execution. Three more studies14–16 were identified from references of already included studies. Overall, 35 qualified studies14–48 were included in the current review (Figure 1).
Figure 1.
Search process and results.
aTricco AC, Ivers NM, Grimshaw JM, et al. Effectiveness of quality improvement strategies on the management of diabetes: a systematic review and meta-analysis. Lancet. 2012;379(9833):2252–2261. https://doi.org/10.1016/S0140–6736(12)60480–2.
Quality of Execution Assessment
Seven16,19,20,25,36,43,47 of the included studies had good quality of execution (one or no limitation), and the others had fair quality of execution (two to four limitations). The most commonly assigned limitations were related to sampling (did not clearly describe their randomization process or sampling frame, 21 studies) 15,17,18,21,23,24,26–30,32–35,37,39,42,45,46,48; data analysis (did not report on treatment of missing data, 21 studies) 17,18,22,24,27–33,35,36,40,41,43–48; or bias (did not report on control for bias, 17 studies).15,16,18,19,21–23,29,30,35,37–39,42,44,45,48
Study and Intervention Characteristics
Detailed description of intervention and team member characteristics can be found in Appendix Tables 1 and 2 (available online). Briefly, most of the included studies were conducted in the U.S., and a majority in clinics or hospitals in an urban setting (Appendix Table 1, available online).
Most interventions added one or two team members to the primary care provider and patient relationship. Most teams added a nurse (including registered nurses and nurse practitioners) or a pharmacist. Patients’ medication regimens could be changed in one of three ways: primary care providers made all medication changes, team members proposed medication changes that required approval from primary care provider, or all qualified team members made changes to medication as appropriate. Most of the teams established active communication channels for team members to exchange information; these channels could be team meetings or other formal interactions. Some teams used passive communication channels when notes were left in patients’ health records or primary care providers’ folders (Appendix Table 1, available online).
Team members provided various services to patients, including education or counseling about diabetes, necessary lifestyle changes related to diet and physical activity, and importance of medication adherence. Team members also helped patients set goals and develop an action plan, medication modification, and testing and monitoring. These services were delivered remotely through telephone or e-mails only, face-to-face only, or a combination of both (Appendix Table 2, available online).
Demographic Characteristics of Participants in Included Studies
Detailed information on demographic characteristics of study participants can be found in Appendix Table 3 (available online). A majority of studies focused on patients with Type 2 diabetes. Study participants had a mean age of 58.4 years and were 52.2% female. Only nine studies reported participants’ income or employment status. Six of the included studies were implemented among low-income or underserved populations. Twelve studies reported that slightly more than half of the participants had high school education or less (median of 51.3%; Appendix Table 3, available online).
Eighteen of the 25 U.S. studies reported on race, and the study population is similar to the U.S. population (Appendix Table 3, available online).
Outcomes
Pre–post differences in blood glucose, blood pressure, lipid level, and weight changes
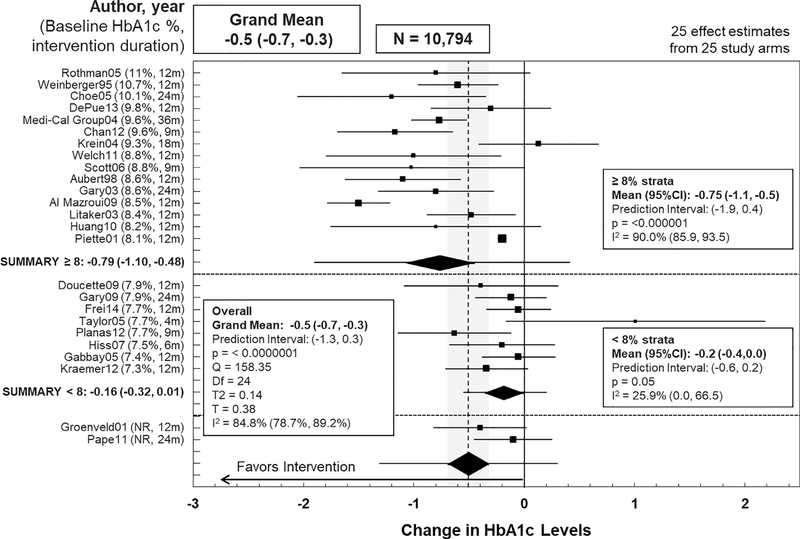
Of the 35 studies in the review, 25 studies14,17,18,20,21,23–30,32,33,35–37,41–44,46–48 reported blood glucose (as measured by HbA1c levels) that could be used in the meta-analysis (Figure 2). Compared with usual care, TBC reduced HbA1c levels by an additional 0.5% (95% CI= −0.7, −0.3, I2=84.8%). The high heterogeneity was partially explained by stratifying results on baseline HbA1c levels. Participants with baseline HbA1c <8% experienced a mean reduction of 0.2% in HbA1c levels (95% CI= −0.3, 0.0, I2=25.9%), whereas participants with baseline HbA1c ≥8% experienced a mean reduction of 0.8% in HbA1c levels (95% CI= −1.1, −0.5, I2=91.0%, difference of 0.58%, 95% CI=0.23, 0.93, p=0.001; Figure 2). TBC was also associated with greater improvements in SBP, DBP, high-density lipoprotein, low-density lipoprotein, total cholesterol, and triglyceride levels (Table 1). There was, however, a slight mean increase in weight (median 1.3%, interquartile interval −0.6%, 2.4%) among participant groups receiving TBC.17,20,25,26,28–30,33,43–45,48
Figure 2.
Impact of team-based care on blood glucose levels in patients with Type 2 diabetes.
Table 1.
Overall Impact of Team-Based Care (Random Effects Meta-Analysis)
| Outcome | Summary effects |
|---|---|
| Blood glucose, measured using HbA1c levels | |
| 25 studies14,17,18,20,21,23–30,32,33,35–37,41–44,46–48 | Grand mean: decrease of 0.5% (95% CI= −0.7, −0.3) Prediction interval, 95%= −1.4, 0.3; **p<0.01 I2 =85.7% (95% CI=80.1%, 89.8%) |
| Stratified by baseline HbA1c | |
| ≥8% (15 studies)17,18,20,21,23,28,30,33,36,37,41,43,44,47,48 | Mean: decrease of 0.8% (95% CI= −1.1, −0.5) I2 =91.0% (95% CI=86.9%, 93.9%) |
| <8% (8 studies)24–27,32,35,42,46 | Mean: decrease of 0.2% (95% CI= −0.3, 0.0) I2 =25.9% (95% CI=0.0%, 66.5%) |
| Blood pressure | |
| Systolic (18 studies)17,18,20,24–26,29,30,32,33,35,36,38,42–44,46,48 | Grand mean: decrease of 5.5 mmHg (95% CI= −8.1, −3.0) Prediction interval, 95%= −15.4, 4.3; **p<0.01 I2 =81.3% (95% CI=71.4%, 87.8%) |
| Diastolic (17 studies)17,18,20,24–26,28–30,32,33,35,36,42,43,46,48 | Grand mean: decrease of 3.2 mmHg (95% CI= −4.8, −1.5) Prediction interval, 95%= −9.3, 3.0; **p<0.01 I2 =81.1% (95% CI=70.7%, 87.8%) |
| Lipids | |
| HDL (9 studies)17,18,20,25,30,33,35,37,46 | Grand mean: increase of 0.7 mg/dL (95% CI= −0.8, 2.2) Prediction interval, 95%= −3.4, 4.8; p=0.35 I2 =50.9% (95% CI=0%, 77%) |
| LDL (14 studies)14,17,18,20,24–26,30,33,35,36,42,44,46 | Grand mean: decrease of 8.0 mg/dL (95% CI= −11.8, −4.3) Prediction interval, 95%= −18.5, 2.4; **p<0.01 I2 =42.2% (95% CI=0%, 69.2%) |
| Total cholesterol (12 studies)17,18,20,25,29,30,32,33,35,37,43,46 | Grand mean: decrease of 7.4 mg/dL (95% CI= −13.9, −0.9) Prediction interval, 95%= −28.0, 13.2; *p=0.02 I2 =63.3% (95% CI=31.6%, 80.3%) |
| Triglycerides (7 studies)17,18,20,30,33,35,46 | Grand mean: decrease of 13.3 mg/dL (95% CI= −38.4, 11.8) Prediction interval, 95%= −82.6, 56.0; p=0.30 I2 =70% (95% CI=10.7%, 82.9%) |
Note: Boldface indicates statistical significance (*p<0.05; **p<0.01).
BP, blood pressure; DBP, diastolic blood pressure; HDL, high-density lipoprotein; LDL, low-density lipoprotein; SBP, systolic blood pressure.
Pre–post changes in proportions of patients reaching diabetes-related health outcome goals
TBC resulted in increased proportions of patients meeting target health outcomes for HbA1c, SBP, BP, low-density lipoprotein, and total cholesterol levels (Table 2). There was minimal change in proportions of patients reaching DBP and high-density lipoprotein goals (Table 2). One study found that compared with usual care, TBC helped patients reach their BMI goal of <30.45
Table 2.
Proportion of Participants Who Reached Diabetes Management Targets
| Outcome | Summary effects |
|---|---|
| Blood glucose, measured using HbA1c levels | |
| Reached below 7.0% (7 studies)14,17,20,39,42,44,48 | Median increase of 15.1 percentage points (IQI: 2.0 to 27.9) |
| Reached below 7.5% (1 study)45 | Increase of 18 percentage points |
| Blood pressure | |
| Blood pressure reached below 130/80 mmHg (10 studies)14,17,20,26,37,38,42,44,45,48 | Median increase of 15.0 percentage points (IQI: 6.0 to 27.2) |
| SBP reached below 130 mmHg (3 studies)20,44,45 | Median increase of 4.4 percentage points (range: −1.2 to 40) |
| DBP reached below 80 mmHg (3 studies)20,44,45 | Median decrease of 1 percentage point (range: −1 to 5.9) |
| Lipids | |
| HDLa | |
| Reached above 35 mg/dL (1 study)45 | 3.2 percentage point decrease |
| Reached above 40 mg/dL (1 study)44 | 0.6 percentage point increase |
| Reached above 43 mg/dL for males or above 50 mg/dL for females (1 study)20 | 2 percentage point increase |
| LDL | |
| Reached below 130 mg/dL (5 studies)14,20,42,44,45 | Median increase of 16.7 percentage points (IQI: 5.7 to 21.8) |
| Total cholesterol reached below 200 mg/dL (1 study)45 | 14 percentage point increase |
An increase in HDL is considered favorable.
DBP, diastolic blood pressure; HDL, high-density lipoprotein; IQI, interquartile interval; LDL, low-density lipoprotein; SBP, systolic blood pressure.
Other outcomes
TBC slightly increased patients’ satisfaction with care when compared with control14,36,37,41,43,48 and produced small15,20,22 or no25,39 improvement in patients’ adherence to medication. Of the few studies that reported on diabetes-related complications, TBC resulted in slightly fewer foot lesions,25 less complaints of nocturia and polyuria,15 but no significant change in the percentage of patients with microalbuminuria/proteinuria19 or new cardiovascular events.19
The systematic review team examined whether TBC could lead to tighter glucose control or medication over-prescription, potentially resulting in more hypoglycemic events. Seven15,18,25,30,34,41,43 of the included studies examined this issue and found that hypoglycemic events were very rare, and there were no differences in rates of these events between intervention and control groups.
Compared with usual care, intervention participants were just as likely to be hospitalized for diabetes-related reasons,25 but less likely to report all-cause hospitalization15,18,36,43,45 or emergency room use.15,18,43,45 TBC interventions were able to improve study participants’ diabetes-related quality of life,37,44,46 and general physical17,18,37,46,47 and mental health.17,37,47,48
Stratified analysis
Detailed results can be found in Appendix Table 4 (available online). Greater reductions in patients’ blood glucose levels were reported when a pharmacist was added to the team when compared with adding a nurse, though the addition of either led to improved blood glucose levels. Similar improvements in patient outcomes were reported when teams added one or two members to the patient–primary care provider relationship.
Programs that allowed team members to make suggestions with primary care provider approval led to greater reductions in DBP than did programs that allowed only primary care providers to make medication changes.
More favorable results were observed when teams had active rather than passive communication channels, all team members had access to patients’ medical records, and services were delivered both in person and remotely rather than just in person or remotely.
Similar improvements in patient outcomes were reported when interventions were implemented from <6 months to >36 months, and additional team members were recruited by hiring new people or expanding the roles of existing staff.
Funnel plot analysis of the health-related outcomes indicates minimal publication bias (Appendix Figure 1, available online).
DISCUSSION
The available evidence demonstrates that for patients with diabetes, TBC improves their blood glucose, BP, and lipid levels. TBC interventions also increase the proportion of patients who reach target blood glucose, BP, and lipid levels.
Teams evaluated in this review included patients, their primary care providers (not necessarily physicians), and one or two additional healthcare professionals (most often nurses or pharmacists). None of the included studies evaluated intervention impacts on participants with Type 1 diabetes alone, and thus the findings are limited to participants with Type 2 diabetes.
Limitations
The random effects meta-analyses of the health outcomes produced I2 values above 75%for HbA1c, SBP, and DBP, a commonly used benchmark to indicate high heterogeneity. Stratified analysis based on baseline HbA1c levels explained a large portion of the heterogeneity observed for blood glucose outcomes. This benchmark, however, is based on a systematic review of pharmaceutical and device RCTs,49 with much less heterogeneity when compared with a multifaceted, health system intervention delivered to a variety of populations. The I2 values also only tell part of the story. For each of these three outcomes, the null was more than 1 SD away from the grand mean. Assuming a normal distribution, the vast majority of the effect sizes are in the favorable direction.
The included studies had highly variable comparison conditions, ranging from no services offered to services that were similar to TBC. TBC has become more commonly used to manage chronic diseases, making it more difficult to assess the impact of implementing de novo TBC, producing more conservative effect estimates.
This review only included RCTs. Although RCTs are referred to as the gold standard of evidence, they have inherent limitations with generalizability of findings,50 though many of the included studies were pragmatic trials conducted in real-world settings.
Applicability
All included studies examined intervention impact on participants with Type 2 diabetes; only one study also included participants with Type 1 diabetes. TBC was effective when implemented inside or outside the U.S., in clinics and in other settings, such as hospitals, pharmacies, or Veterans Affairs facilities. These interventions were effective across population groups with different racial, ethnic, and socioeconomic backgrounds.
TBC implemented among racial or ethnic minorities reduced blood glucose levels.19,23,40,48 Interventions implemented among low-income populations improved blood glucose, BP, and lipids.30,43,44 Studies that exclusively recruited African Americans with low income found reductions in blood glucose and DBP.22,27,28
The evaluated TBC interventions ran for a median of 12 months. Results from stratified analyses showed that TBC produced favorable glycemic and BP outcomes regardless of intervention duration, suggesting these interventions can improve diabetes-related outcomes after 6 months and sustain them through continued care.
No additional postulated benefits or harms were identified in the included studies or in the broader literature.
Evidence Gaps
Additional research and evaluation are needed to answer the following questions and fill existing gaps in the evidence base:
What are the effects of TBC interventions on diabetes-related complications and healthcare use?
How effective are TBC interventions in the following populations: people with Type 1 diabetes, younger people with diabetes, pregnant women with gestational diabetes, uninsured people with diabetes, and people with diabetes living in rural settings?
How effective are TBC interventions with different team composition and operation characteristics, such as services provided; methods of communication between team members; and whether protocols exist to specify team roles and responsibilities (e.g., should the team member who serves as team lead provide the majority of services, or who should serve as primary contact for patients)?
CONCLUSIONS
The current systematic review and meta-analysis found favorable changes in intermediary diabetes-related health outcomes that could produce downstream health benefits for the study participants. The United Kingdom Prospective Diabetes Study was the largest and longest cohort study ever performed on patients with Type 2 diabetes.51 The study found that for every percentage point decrease in HbA1c (e.g., 9% to 8%), there was a 35% reduction in microvascular complications, a 25% reduction in diabetes-related deaths, a 7% reduction in all-cause mortality, and an 18% reduction in combined fatal and nonfatal myocardial infarction, irrespective of baseline HbA1c.51 From this estimation, the 0.5% mean reduction in HbA1c found in this review could have important clinical implications.
Patients whose baseline HbA1c was 8% or more experienced greater reductions in their HbA1c when compared with patients whose baseline was less than 8%, though all reductions were significant. This may be because patients with higher baseline measurements had more room to improve.
There was a small and statistically insignificant increase in mean weight. A recent study52 showed that intensive weight management within routine primary care can lead to sustained weight loss, resulting in remission of Type 2 diabetes. Providers implementing TBC may want to enhance weight management efforts to further improve diabetes-related health outcomes.
TBC is patient-centered care delivered by a team of healthcare professionals from different disciplines. In most included studies, care was tailored to reflect each patient’s knowledge of diabetes, ability to adopt behavior modifications to manage diabetes, severity of diabetes indicators, and diabetes-related complications. TBC improved patients’ quality of life and overall physical and mental health and slightly increased their satisfaction with care. There was also a reduction in all-cause hospitalization and emergency department use for study participants. TBC interventions allow for more frequent and regular interactions between patients and healthcare professionals, which gives patients more opportunities to address health concerns.
TBC has been implemented for various populations in different settings, and with different team composition and operation procedures. Although each team is unique with its own purpose, setting, patient needs, and resource availability, there are some overarching principles for building effective teams. Five principles of TBC identified in the broader literature include shared goals between the team and the patient, clear roles and expectations for all team members, mutual trust among team members, effective communication, and measurable processes and outcomes.53
Stratified analysis suggests that TBC with active communication between team members is more effective than TBC with less formal and less active communication channels. A combination of face-to-face and remote interactions between patients and added team members produced better outcomes than either face-to-face or remote interactions alone. Studies included in the stratified analysis only used telephones for remote communication, but other mobile technologies can also be used, such as text messaging, web portals, and apps.
Composition of effective teams can be flexible, with one or two added team members, either nurses or pharmacists, recruited either as new hires or existing staff with expanded roles. Teams that added a pharmacist showed more improvement in blood glucose when compared with teams that added a nurse, consistent with results from a previous Community Guide review on TBC to control BP.54 Nurses, however, may be more widely available than pharmacists. TBC with an added pharmacist tends to focus more on medication adherence and modification.
Outside of research settings, TBC interventions can face challenges such as limited resources, or lack of knowledge on how to be patient-centered or form a functional and effective multidisciplinary team. A list of resources to guide interested health teams through implementing TBC is at www.thecommunityguide.org.
Supplementary Material
ACKNOWLEDGMENTS
The authors acknowledge Onnalee A. Gomez (formerly Library Science Branch, Division of Public Health Information Dissemination, Centers for Disease Control and Prevention [CDC]) for conducting the searches. Stacy A. Benton, from the Community Guide Branch, CDC, provided input to the development of the manuscript.
The work of Timothy Levengood and Ka Xiong was supported with funds from the Oak Ridge Institute for Science and Education. Marshall Chin was supported in part by the Chicago Center for Diabetes Translation Research (National Institute of Diabetes and Digestive and Kidney Diseases P30 DK092949). Mohammed Ali was partially supported by Georgia Center for Diabetes Translation Research (P30DK111024).
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the CDC or NIH.
Footnotes
No financial disclosures were reported by the authors of this paper.
SUPPLEMENTAL MATERIAL
Supplemental materials associated with this article can be found in the online version at https://doi.org/10.1016/j.amepre.2019.02.005.
REFERENCES
- 1.Centers for Disease Control and Prevention (CDC). Living with diabetes: prevent complications. www.cdc.gov/diabetes/managing. Published 2017. Accessed November 7, 2017.
- 2.Deshpande AD, Harris-Hayes M, Schootman M. Epidemiology of diabetes and diabetes-related complications. Phys Ther. 2008;88 (11):1254–1264. 10.2522/ptj.20080020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.American Diabetes Association. Economic costs of diabetes in the U.S. in 2012. Diabetes Care. 2013;36(4):1033–1046. 10.2337/dc12-2625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention (CDC). National Diabetes Statistics Report, 2017. Atlanta, GA: CDC, HHS, 2017. [Google Scholar]
- 5.Edwards ST, Bitton A, Hong J, Landon BE. Patient-centered medical home initiatives expanded in 2009−13: providers, patients, and payment incentives increased. Health Aff (Millwood). 2014;33(10):1823–1831. 10.1377/hlthaff.2014.0351. [DOI] [PubMed] [Google Scholar]
- 6.Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff (Millwood). 2008;27(3):759–769. 10.1377/hlthaff.27.3.759. [DOI] [PubMed] [Google Scholar]
- 7.Briss P, Zaza S, Pappaioanou M, et al. Developing an evidence-based guide to Community Preventive Services—methods. Am J Prev Med. 2000;18(15):35–43. 10.1016/S0749-3797(99)00119-1. [DOI] [PubMed] [Google Scholar]
- 8.Zaza S, Wright-De Aguero LK, Briss PA, et al. Data collection instrument and procedure for systematic reviews in the Guide to Community Preventive Services. Am J Prev Med. 2000;18(suppl 1):44–74. 10.1016/S0749-3797(99)00122-1. [DOI] [PubMed] [Google Scholar]
- 9.Tricco AC, Ivers NM, Grimshaw JM, et al. Effectiveness of quality improvement strategies on the management of diabetes: a systematic review and meta-analysis. Lancet. 2012;379(9833):2252–2261. 10.1016/S0140-6736(12)60480-2. [DOI] [PubMed] [Google Scholar]
- 10.The World Bank. World Bank Country and Lending Groups. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups. Published 2018. Accessed February 21, 2018.
- 11.DerSimonian R, Laird N. Meta-analysis in clinical trials. Controlled Clin Trials. 1986;7(3):177–188. 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 12.Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0. www.handbook.cochrane.org. Published 2011. Accessed February 12, 2019.
- 13.Jacobs M, Sherry PS, Taylor LM, Amato M, Tataronis GR, Cushing G. Pharmacist Assisted Medication Program Enhancing the Regulation of Diabetes (PAMPERED) study. J Am Pharm Assoc (2003). 2012;52 (5):613–621. 10.1331/JAPhA.2012.10183. [DOI] [PubMed] [Google Scholar]
- 14.Pape GA, Hunt JS, Butler KL, et al. Team-based care approach to cholesterol management in diabetes mellitus: two-year cluster randomized controlled trial. Arch Intern Med. 2011;171(16):1480–1486. 10.1001/archinternmed.2011.417. [DOI] [PubMed] [Google Scholar]
- 15.Sczupak CA, Conrad WF. Relationship between patient-oriented pharmaceutical services and therapeutic outcomes of ambulatory patients with diabetes mellitus. Am J Hosp Pharm. 1977;34(11):1238–1242. [PubMed] [Google Scholar]
- 16.Simpson SH, Majumdar SR, Tsuyuki RT, Lewanczuk RZ, Spooner R, Johnson JA. Effect of adding pharmacists to primary care teams on blood pressure control in patients with Type 2 diabetes: a randomized controlled trial. Diabetes Care. 2011;34(1):20–26. 10.2337/dc10-1294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Al Mazroui NR, Kamal MM, Ghabash NM, Yacout TA, Kole PL, McElnay JC. Influence of pharmaceutical care on health outcomes in patients with Type 2 diabetes mellitus. Br J Clin Pharmacol. 2009;67 (5):547–557. 10.1111/j.1365-2125.2009.03391.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Aubert RE, Herman WH, Waters J, et al. Nurse case management to improve glycemic control in diabetic patients in a health maintenance organization: a randomized, controlled trial. Ann Intern Med. 1998;129 (8):605–612. 10.7326/0003-4819-129-8-199810150-00004. [DOI] [PubMed] [Google Scholar]
- 19.Bellary S, O’Hare JP, Raymond NT, et al. Enhanced diabetes care to patients of south Asian ethnic origin (the United Kingdom Asian Diabetes Study): a cluster randomised controlled trial. Lancet. 2008;371 (9626):1769–1776. 10.1016/S0140-6736(08)60764-3. [DOI] [PubMed] [Google Scholar]
- 20.Chan CW, Siu SC, Wong CK, Lee VW. A pharmacist care program: positive impact on cardiac risk in patients with Type 2 diabetes. J Cardiovasc Pharmacol Ther. 2012;17(1):57–64. 10.1177/1074248410396216. [DOI] [PubMed] [Google Scholar]
- 21.Choe HM, Mitrovich S, Dubay D, Hayward RA, Krein SL, Vijan S. Proactive case management of high-risk patients with Type 2 diabetes mellitus by a clinical pharmacist: a randomized controlled trial. Am J Manag Care. 2005;11(4):253–260. [PubMed] [Google Scholar]
- 22.Crowley MJ, Powers BJ, Olsen MK, et al. The Cholesterol, Hypertension, And Glucose Education (CHANGE) study: results from a randomized controlled trial in African Americans with diabetes. Am Heart J. 2013;166 (1):179–186. 10.1016/j.ahj.2013.04.004. [DOI] [PubMed] [Google Scholar]
- 23.DePue JD, Dunsiger S, Seiden AD, et al. Nurse-community health worker team improves diabetes care in American Samoa: results of a randomized controlled trial. Diabetes Care. 2013;36(7):1947–1953. 10.2337/dc12-1969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Doucette WR, Witry MJ, Farris KB, McDonough RP. Community pharmacist-provided extended diabetes care. Ann Pharmacother. 2009;43(5):882–889. 10.1345/aph.1L605. [DOI] [PubMed] [Google Scholar]
- 25.Frei A, Senn O, Chmiel C, Reissner J, Held U, Rosemann T. Implementation of the chronic care model in small medical practices improves cardiovascular risk but not glycemic control. Diabetes Care. 2014;37(4):1039–1047. 10.2337/dc13-1429. [DOI] [PubMed] [Google Scholar]
- 26.Gabbay RA, Lendel I, Saleem TM, et al. Nurse case management improves blood pressure, emotional distress and diabetes complication screening. Diabetes Res Clin Pract. 2006;71(1):28–35. 10.1016/j.diabres.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 27.Gary TL, Batts-Turner M, Yeh HC, et al. The effects of a nurse case manager and a community health worker team on diabetic control, emergency department visits, and hospitalizations among urban African Americans with Type 2 diabetes mellitus: a randomized controlled trial. Arch Intern Med. 2009;169(19):1788–1794. 10.1001/archinternmed.2009.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gary TL, Bone LR, Hill MN, et al. Randomized controlled trial of the effects of nurse case manager and community health worker interventions on risk factors for diabetes-related complications in urban African Americans. Prev Med. 2003;37(1):23–32. 10.1016/S0091-7435(03)00040-9. [DOI] [PubMed] [Google Scholar]
- 29.Groeneveld Y, Petri H, Hermans J, Springer M. An assessment of structured care assistance in the management of patients with Type 2 diabetes in general practice. Scand J Prim Health Care. 2001;19(1):25–30. 10.1080/02813430117968. [DOI] [PubMed] [Google Scholar]
- 30.The California Medi-Cal Type 2 Diabetes Study Group. Closing the gap: effect of diabetes case management on glycemic control among low-income ethnic minority populations: the California Medi-Cal Type 2 diabetes study. Diabetes Care. 2004;27(1):95–103. 10.2337/diacare.27.1.95. [DOI] [PubMed] [Google Scholar]
- 31.Hargraves JL, Ferguson WJ, Lemay CA, Pernice J. Community health workers assisting patients with diabetes in self-management. J Ambul Care Manage. 2012;35(1):15–26. 10.1097/JAC.0b013e31822cbe35. [DOI] [PubMed] [Google Scholar]
- 32.Hiss RG, Armbruster BA, Gillard ML, McClure LA. Nurse care manager collaboration with community-based physicians providing diabetes care: a randomized controlled trial. Diabetes Educ. 2007;33(3):493–502. 10.1177/0145721707301349. [DOI] [PubMed] [Google Scholar]
- 33.Huang MC, Hsu CC, Wang HS, Shin SJ. Prospective randomized controlled trial to evaluate effectiveness of registered dietitian-led diabetes management on glycemic and diet control in a primary care setting in Taiwan. Diabetes Care. 2010;33(2):233–239. 10.2337/dc09-1092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jameson JP, Baty PJ. Pharmacist collaborative management of poorly controlled diabetes mellitus: a randomized controlled trial. Am J Manag Care. 2010;16(4):250–255. [PubMed] [Google Scholar]
- 35.Kraemer DF, Kradjan WA, Bianco TM, Low JA. A randomized study to assess the impact of pharmacist counseling of employer-based health plan beneficiaries with diabetes: the EMPOWER study. J Pharm Pract. 2012;25(2):169–179. 10.1177/0897190011418513. [DOI] [PubMed] [Google Scholar]
- 36.Krein SL, Klamerus ML, Vijan S, et al. Case management for patients with poorly controlled diabetes: a randomized trial. Am J Med. 2004;116(11):732–739. 10.1016/j.amjmed.2003.11.028. [DOI] [PubMed] [Google Scholar]
- 37.Litaker D, Mion L, Planavsky L, Kippes C, Mehta N, Frolkis J. Physician−nurse practitioner teams in chronic disease management: the impact on costs, clinical effectiveness, and patients’ perception of care. J Interprof Care. 2003;17(3):223–237. 10.1080/1356182031000122852. [DOI] [PubMed] [Google Scholar]
- 38.McLean DL, McAlister FA, Johnson JA, et al. A randomized trial of the effect of community pharmacist and nurse care on improving blood pressure management in patients with diabetes mellitus: Study of Cardiovascular Risk Intervention by Pharmacists−Hypertension (SCRIP-HTN). Arch Intern Med. 2008;168(21):2355–2361. 10.1001/archinte.168.21.2355. [DOI] [PubMed] [Google Scholar]
- 39.Odegard PS, Goo A, Hummel J, Williams KL, Gray SL. Caring for poorly controlled diabetes mellitus: a randomized pharmacist intervention. Ann Pharmacother. 2005;39(3):433–440. 10.1345/aph.1E438. [DOI] [PubMed] [Google Scholar]
- 40.O’Hare JP, Raymond NT, Mughal S, et al. Evaluation of delivery of enhanced diabetes care to patients of South Asian ethnicity: the United Kingdom Asian Diabetes Study (UKADS). Diabet Med. 2004;21 (12):1357–1365. 10.1111/j.1464-5491.2004.01373.x. [DOI] [PubMed] [Google Scholar]
- 41.Piette JD, Weinberger M, Kraemer FB, McPhee SJ. Impact of automated calls with nurse follow-up on diabetes treatment outcomes in a Department of Veterans Affairs Health Care System: a randomized controlled trial. Diabetes Care. 2001;24(2):202–208. 10.2337/diacare.24.2.202. [DOI] [PubMed] [Google Scholar]
- 42.Planas LG, Crosby KM, Farmer KC, Harrison DL. Evaluation of a diabetes management program using selected HEDIS measures. J Am Pharm Assoc (2003). 2012;52(6):e130–e138. 10.1331/JAPhA.2012.11148. [DOI] [PubMed] [Google Scholar]
- 43.Rothman RL, Malone R, Bryant B, et al. A randomized trial of a primary care-based disease management program to improve cardiovascular risk factors and glycated hemoglobin levels in patients with diabetes. Am J Med. 2005;118(3):276–284. 10.1016/j.amjmed.2004.09.017. [DOI] [PubMed] [Google Scholar]
- 44.Scott DM, Boyd ST, Stephan M, Augustine SC, Reardon TP. Outcomes of pharmacist-managed diabetes care services in a community health center. Am J Health Syst Pharm. 2006;63(21):2116–2122. 10.2146/ajhp060040. [DOI] [PubMed] [Google Scholar]
- 45.Taylor CB, Miller NH, Reilly KR, et al. Evaluation of a nurse-care management system to improve outcomes in patients with complicated diabetes. Diabetes Care. 2003;26(4):1058–1063. 10.2337/diacare.26.4.1058. [DOI] [PubMed] [Google Scholar]
- 46.Taylor KI, Oberle KM, Crutcher RA, Norton PG. Promoting health in Type 2 diabetes: nurse-physician collaboration in primary care. Biol Res Nurs. 2005;6(3):207–215. 10.1177/1099800404272223. [DOI] [PubMed] [Google Scholar]
- 47.Weinberger M, Kirkman MS, Samsa GP, et al. A nurse-coordinated intervention for primary care patients with non-insulin-dependent diabetes mellitus: impact on glycemic control and health-related quality of life. J Gen Intern Med. 1995;10(2):59–66. 10.1007/BF02600227. [DOI] [PubMed] [Google Scholar]
- 48.Welch G, Allen NA, Zagarins SE, Stamp KD, Bursell SE, Kedziora RJ. Comprehensive diabetes management program for poorly controlled Hispanic Type 2 patients at a community health center. Diabetes Educ. 2011;37(5):680–688. 10.1177/0145721711416257. [DOI] [PubMed] [Google Scholar]
- 49.Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Br Med J. 2003;327(7414):557–560. 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Frieden TR. Evidence for health decision making: beyond randomized, controlled trials. N Engl J Med. 2017;377(5):465–475. 10.1056/NEJMra1614394. [DOI] [PubMed] [Google Scholar]
- 51.UK Prospective Diabetes Study (UKPDS) Group. Intensive blood glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with Type 2 diabetes (UKPDS 33). Lancet. 1998;352(9131):837–853. 10.1016/S0140-6736(98)07019-6. [DOI] [PubMed] [Google Scholar]
- 52.Lean MEJ, Leslie WS, Barnes AC, et al. Primary care-led weight management for remission of Type 2 diabetes (DiRECT): an open-label, cluster-randomised trial. Lancet. 2018;391(10120):541–551. 10.1016/S0140-6736(17)33102-1. [DOI] [PubMed] [Google Scholar]
- 53.Wynia MK, Von Kohorn I, Mitchell PH. Challenges at the intersection of team-based and patient-centered health care: insights from an IOM working group. JAMA. 2012;308(13):1327–1328. 10.1001/jama.2012.12601. [DOI] [PubMed] [Google Scholar]
- 54.Proia KK, Thota AB, Njie GJ, et al. Team-based care and improved blood pressure control: a Community Guide systematic review. Am J Prev Med. 2014;47(1):86–99. 10.1016/j.amepre.2014.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.