Abstract
The opioid receptors are a family of G-protein coupled receptors (GPCRs) with close structural homology. The opioid receptors are activated by a variety of endogenous opioid neuropeptides, principally β-endorphin, dynorphins, leu- and met-enkephalins. The clinical potential of targeting opioid receptors has largely focused on the development of analgesics. However, more recent attention has turned to the role of central opioid receptors in the regulation of stress responses, anhedonia and mood. Activation of the κ opioid receptor (KOP) subtype has been shown in both human and rodent studies to produce dysphoric and pro-depressive like effects. This has led to the idea that selective KOP antagonists might have therapeutic potential as antidepressants. Here we review data showing that mixed μ opioid (MOP) and KOP antagonists have antidepressant-like effects in rodent behavioural paradigms and highlight comparable studies in treatment-resistant depressed patients. We propose that developing multifunctional ligands which target multiple opioid receptors open up the potential for fine-tuning hedonic responses mediated by opioids. This alternative approach towards targeting multiple opioid receptors may lead to more effective treatments for depression.
Keywords: antidepressants, depression, opioid receptors
Introduction
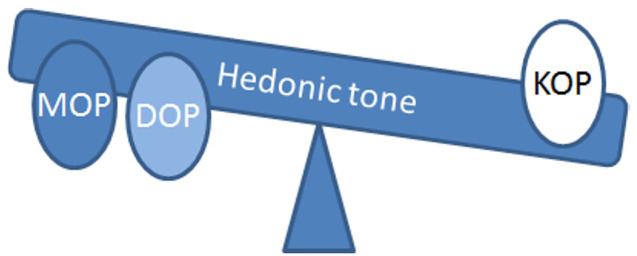
The opioid neuropeptides are β-endorphin, enkephalins and dynorphins, which preferentially act at μ (MOP), δ (DOP) and κ (KOP) opioid receptors respectively [1]. Together with the homologous but non-opioid nociceptin/orphanin FQ (NOP) receptor, these opioid receptors form a subfamily of G-protein coupled receptors (GPCRs) that are expressed throughout the brain and increasingly recognized to play a role in mood and stress responsivity [2,3]. We and others, have focused on developing KOP receptor antagonists with potential as antidepressant and anxiolytic agents [4]. KOP receptors are Gαi/o coupled receptors with a unique pharmacology [5]. In this article, we highlight findings that suggest compounds which have activity at a range of opioid receptors may represent a more effective antidepressant strategy by rebalancing hedonic tone.
Opioid receptors regulate mood
Anhedonia or the reduced capacity to experience pleasure, is a core feature of major depressive disorder [6,7]. The mesolimbic dopaminergic system is involved in the reward system and in mediating the degree of anhedonia and risk of developing depression [6–8]. Hedonic tone can be defined as the trait or genetic predisposition underlying an individual’s baseline range and lifelong characteristic ability to feel pleasure [7]. The activity of the limbic-cortical-striatal-pallidal-thalamic pathway (which consists of connections between the prefrontal cortex, ventro-medial striatum, ventral pallidum, hippocampal subiculum, mediodorsal and midline thalamic nuclei and amygdala) is correlated with hedonic tone in healthy individuals and altered in major depressive disorder [7]. These circuits integrate higher cognitive function with mood and emotional states via reciprocal connections between cortical regions and areas involved in the regulation of autonomic functions such as the periaqueductal grey and the hypothalamus. Neuronal activity in the limbic-cortical-striatal-pallidal-thalamic pathway is predominantly glutamatergic in nature modulated by GABA. Release of both glutamate and GABA can be modulated by opioids in the ventral tegmental area (VTA), amygdala and hippocampus [9]. Dysfunctional reward processing in depression is well characterized and anhedonia has been shown to be a predictor of treatment-resistant depression, particularly in adolescent depression [10,11]. The relative ineffectiveness of SSRIs used to treat anxiety and depression in patients with low hedonic tone is associated with dysfunction of these circuits [12,13]. This would suggest a specific beneficial effect of an antidepressant strategy targeting opioid receptors that could regulate hedonic tone in treatment-resistant depression, and perhaps particularly in adolescent depression where effective treatment options are limited [14,15].
The ‘opium cure’ was recommended for depressed patients before the discovery of current antidepressant treatments or electroconvulsive therapy [16]. Of the endogenous neuropeptide opioids that have been identified as contributing to the aetiology of major depressive disorder, β-endorphin has been the most extensively investigated. However, studies of basal β-endorphin levels in depressed patients have been equivocal with several reports suggesting increased β-endorphin levels compared with controls while others suggest no change or decreased β-endorphin levels [17,18]. This variability may reflect differences between the studies including subgroups of depressed patients, comorbidities and medication status [17]. Despite concerns about the risks of abuse and dependency, opiates acting at MOP receptors, including oxycodone, oxymorphone and the partial MOP agonist buprenorphine, have all been shown to be beneficial in patients with treatment-resistant depression [19–22] and buprenorphine may have antisuicidal effects [23]. In ten patients with treatment-resistant unipolar non-psychotic depression, clinical improvements were evident after 1 week of treatment with buprenorphine (0.15–1.8 mg/day), a significant improvement on existing therapies [19]. More recently, in a small cohort of older treatment-resistant depressed adults, clinically significant improvements were evident within 3 weeks of starting buprenorphine (0.4–0.7 mg/day) treatment [20]. In severely suicidal patients receiving ultra-low-dose buprenorphine (0.1 mg once or twice daily) a greater reduction in Beck Suicide Ideation Score was observed after 2 and 4 weeks of treatment, compared with placebo [21]. Buprenorphine has a complex pharmacology (see below) and its therapeutic mechanisms of action are not well understood. In these studies, different patient populations and different dosing regimes were used but in all cases clinically significant improvements were observed. However, high and moderate efficacy MOP receptor agonists, because of their rewarding properties, are all associated with abuse liability and the potential for developing opiate dependency.
Stress is a risk factor for developing a range of psychiatric disorders including depression [24]. Multiple mediators are implicated in how the body responds to stress including corticotrophin releasing factor (CRF), vasopressin, adrenocorticotrophic hormone and glucocorticoids, which mediate the actions of the hypothalamic-pituitary-adrenal (HPA) axis. Opioids have been suggested to have a counter-regulatory role in modulating HPA stress responsivity under stress conditions [25]. β-endorphin and dynorphin exert tonic inhibition and stimulation of HPA activity by acting on MOP and KOP respectively. β-endorphin acting at MOP exerts tonic inhibition of CRF and thus of the HPA axis in rodents, whereas KOP agonists stimulate plasma corticosterone and these stimulatory effects were blocked by KOP antagonists [26]. Alongside this, accumulating evidence specifically implicates KOP receptors as part of the body’s response to stress [27]. Dynorphin and KOP receptors are expressed in limbic brain regions associated with the regulation of mood. Stress releases CRF which then functions to increase dynorphin release and subsequent activation of KOP receptors in specific brain circuits [28]. In this regard, acute or subchronic stress in rodents produced stress-induced immobility that was reduced by treatment with the KOP receptor antagonist norbinaltorphamine (norBNI) and absent from dynorphin and KOP receptor knockout mice [29–32], confirming that endogenous dynorphins are released and activate KOP receptors during exposure to acute or repeated stress [33]. The mesolimbic dopamine system has been implicated in the blockade of the dysphoric actions of dynorphin and in the antidepressant effects of KOP receptor antagonists [34]. KOP receptors are expressed on VTA cell bodies and on the presynaptic terminals of VTA afferents in the nucleus accumbens and their activation decreases dopamine release, thereby producing a dysphoric effect. Interestingly, direct microinfusion of norBNI into the nucleus accumbens produced an antidpressant effect (Newton et al. (2002) [35]). Together with observations showing that KOP receptor agonists produce dysphoric and psychotomimetic responses in humans [36–39] and aversive responses in rodents [28,35,40], these findings have led to the view that KOP antagonists could be potential antidepressant drugs.
Clinical trials of selective KOP antagonists
A number of high affinity, selective KOP receptor antagonists have been described in the literature including norBNI, 5′-guanidinonaltrindole (GNTI) and the (3R,4R)-dimethyl-4-(3-hydroxyphenyl) piperidine based JDTic [41–43]. These compounds share an unusual pharmacodynamic property in that there is slow onset of antagonist activity (typically peaking at approximately 24 h) and exceedingly long duration of action in vivo (up to 3–4 weeks following a single systemic administration) [44–46]. The first study in humans for JDTic to establish its safety, tolerability and pharmacokinetics was terminated because of adverse effects and specifically non-sustained ventricular tachycardia (https://www.clinicaltrials.gov/ct2/show/NCT01431586). Concerns about the feasibility of developing KOP antagonists for the clinic have centred around the long duration of action of high affinity selective compounds, leading to the development of a number of short-acting KOP antagonists [47–52]. Ligand-directed signalling may account for the duration of activity of KOP antagonists which has been demonstrated to correlate with activation of c-Jun N-terminal kinase-1 (JNK1). The long acting KOP antagonists such as norBNI and JDTic activate JNK1 whereas shorter acting KOP antagonists such as CERC-501 (previously LY-2456302) do not [53,54]. Additionally, there are differences in blood–brain barrier permeability and bioavailability with JDTic showing poor brain penetration, and compounds such as CERC-501 showing relatively rapid absorption. Irrespective of the duration of activity, it is clear that the long-lasting blockade of KOP receptors is not necessary to block stress-induced or pro-depressant responses and indeed the short-acting KOP antagonist CERC-501 has been evaluated in phase II clinical trials in a proof of concept study for the treatment of mood and anxiety (https://www.clinicaltrials.gov/ct2/show/NCT02218736).
Mixed KOP/MOP antagonists are antidepressant in animal models
We investigated the in vivo KOP activity of two naltrindole derivatives which had been identified in vitro to have high selectivity for the KOP receptor; 5′-(aminomethyl) naltrindole (5′-AMN) (compound 5, [55]) and the closely related amidine N-((Naltrindol-5-yl) methyl) pentanimidamide (5′-MABN) (compound 10b, [56]). Primary amines are known to be readily metabolizable by amine oxidases and we predicted that these naltrindole derivatives would maintain their selectivity for KOP receptors while having a shorter duration of action than standard KOP antagonists such as norBNI. In vitro studies showed that both 5′-AMN and 5′-MABN had high affinity for KOP receptors (Ki: 1.36 ± 0.98 and 0.27 ± 0.08 respectively) and were revealed as potent antagonists at both KOP (pA2: 7.43 and 8.18 respectively) and MOP receptors (pA2: 7.62 and 7.85 respectively) in the isolated guinea pig ileum [57]. Systemic administration of both 5′-AMN and 5′-MABN in mice blocked KOP agonist-induced (U50,488) antinociception establishing that they were KOP antagonists. However, they were not short acting and had a duration of action similar to or longer than that of norBNI [57]. Despite this significant MOP antagonist activity, both 5′-AMN and 5′-MABN decreased mouse anxiety- and depression-related behaviours in the elevated plus maze and forced swim test respectively [57]. It was perhaps surprising that concurrent MOP receptor antagonism did not negate the antidepressant effects of KOP receptor antagonism, with both compounds being as effective as the standard selective KOP antagonist norBNI.
An alternative approach to developing short-acting ligands KOP antagonists with antidepressant-like potential was to investigate the effects of combination buprenorphine and naltrexone [58]. Buprenorphine/naltrexone (4 mg sublingual: 50 mg oral) has proved safe and effective in treating opioid dependence in an observational study, in part because it improves the dysphoria associated with drug withdrawal [59]. This would suggest that combination buprenorphine/naltrexone may improve mood. Buprenorphine is a partial MOP receptor agonist, a KOP receptor antagonist and at higher concentrations, a DOP antagonist and also possesses NOP receptor partial agonist activity [60,61]. Naltrexone is a relatively non-selective opioid antagonist with a higher affinity for MOP than KOP receptors. Combining buprenorphine with naltrexone (1:1) produced a functional short acting blockade of both KOP and MOP receptors in CD1 mice as evaluated in the warm water tail withdrawal assay (Almatroudi et al. 2015) [58]. The combination dose of buprenorphine/naltrexone (both 1 mg/kg) produced no locomotor effects, was not rewarding nor aversive but did produce antidepressant and anxiolytic like responses in the forced swim and novelty-induced hypophagia tasks [58]. More recently, we have shown that a novel compound, BU10119, derived from buprenorphine, with a pharmacology resembling combination buprenorphine/naltrexone, also shows antidepressant-like responses [62]. BU10119 was also able to block stress-induced analgesia but not stress-induced increases in corticosterone [62]. Others have shown that stress-induced behaviours can be blocked by KOP antagonists, such as norBNI, even though corticosterone levels may or may not have been affected (see discussion in [62]).
In our experiments, we were also able to demonstrate that naltrexone alone also produced antidepressant-like responses in CD1 mice [58]. The mixed KOP/MOP receptor antagonist profile of naltrexone has recently been proposed to account for its ability to reduce the latency to feed in the novelty-induced hypophagia task in C57BL/6J mice [63]. This was somewhat surprising, since the aversive effects of naltrexone have been known for a long time [64]. While some have shown no effect of naltrexone on mood (daily, 200 mg dose) in overweight healthy volunteers [65], others have shown, in opioid-dependent patients, with a high baseline affective burden, depot naltrexone treatment produced a significant improvement in depression scores [66]. Recently Mischoulon et al. [67] demonstrated that low dose naltrexone (1 mg, twice a day), in a small cohort of patients with recurrent major depressive disorder on dopaminergic antidepressant regimens, showed some benefit as an adjunct therapy, compared with placebo. The present study restricted the patients to those on dopaminergic therapies, predominantly bupropion, because their hypothesis was based on observations in Restless Leg Syndrome which suggested that naltrexone might facilitate sensitization of dopamine D2 and D3 receptors.
As discussed earlier, buprenorphine on its own has demonstrated clinical efficacy in treatment-resistant depression and has also been shown to reduce depressive and anxiety-like behaviours in rats and mice [58,68,69]. There remains concerns about the non-therapeutic misuse of buprenorphine, because of its partial MOP receptor agonist activity, which appears to be rising among drug users [70]. Initially it was believed that buprenorphine’s efficacy in treating depressed patients was derived from its partial MOP agonist actions but this has been challenged in recent years with evidence suggesting these behavioural effects of buprenorphine can be attributed to its KOP receptor antagonism [58,69]. Intriguingly, the most recent data indicate that MOP receptors do play a role in buprenorphine’s behavioural response where there is a motivational component [63,71] but perhaps not in the way initially envisaged. In the novelty-induced hypophagia task in C57BL/6J mice buprenorphine, when used at a time point when it was acting as an MOP receptor antagonist, reduced the latency to approach the food in the novel cage but not in MOP receptor knockout mice. That this activity was mediated through blockade of MOP receptors was confirmed by use of a selective MOP receptor antagonist, cyprodime. These authors suggest that antagonism of MOP receptors by buprenorphine could block stress-induced activation of MOP receptors in the VTA which has been shown to reduce dopaminergic transmission in the nucleus accumbens [63]. It would therefore appear that both KOP receptor antagonism and MOP receptor antagonism may be important for buprenorphine’s ability to regulate emotional state. Clinical evidence is supportive of this hypothesis; Alkermes have combined buprenorphine with the MOP antagonist samidorphan in a single sublingual tablet (ALKS5461) and in a 1:1 combination that provides KOP receptor antagonism and antagonism or extremely low stimulation at MOP receptors. ALKS5461 has been shown to have potential in the treatment of major depressive disorder [72,73] confirming the pre-clinical findings with buprenorphine-naltrexone and BU10119 [58,62].
Overall, these data provide good evidence of the therapeutic potential for exploiting mixed KOP/MOP receptor antagonists as antidepressant treatments, particularly in treatment- resistant depressed patients, to rebalance hedonic tone (Figure 1).
Figure 1. Opioid receptors regulate hedonic tone.
The opioid receptors MOP, DOP and KOP have all been implicated in the control of hedonic tone. The above diagram illustrates how the balance of activation of these receptors could contribute to overall hedonic tone. Agonist activation of MOP and DOP receptors is proposed to increase hedonic tone whereas activation of KOP receptors produces anhedonia. Blockade of both KOP and MOP receptors by BU10119, buprenorphine, naltrexone, 5′-AMN and 5′-MABN produced antidepressant-like responses in rodents, perhaps by rebalancing hedonic tone.
Future prospects for opioid ligands in the treatment of mood?
In addition to MOP and KOP receptors, DOP and NOP receptors also play a role in the regulation of hedonic tone and the response to stress. Activation of DOP receptors has been shown to be an antidepressant in a number of preclinical behavioural studies [3]. However, DOP agonists may be limited by their pro-seizure-like properties [74,75], although DOP agonists that generate antidepressant-like effects without convulsions have recently been developed [76]. Buprenorphine has no DOP agonist activity, but is a DOP antagonist [61]. The effects of the NOP receptor on stress-related behaviour are less well characterized [77]. NOP receptor agonists have been shown to have anxiolytic-like effects comparable with those of benzodiazepines in a range of behavioural assays [78]. NOP agonists have also been shown to decrease extracellular dopamine in the nucleus accumbens and to block the rewarding and reinforcing properties of morphine and alcohol (Toll et al. (2016) [77]). While buprenorphine and BU10119 show some efficacy at NOP receptors in vitro, these effects are evident only at drug concentrations approximately 1000-fold higher than required for MOP and KOP antagonism [61,62,79]. The close structural homologies between the three classic opioid receptors, MOP, DOP and KOP, and the NOP receptor has presented challenges in obtaining conventional selective ligands to study these receptors but will be aided by knowledge of the crystal structure of these GPCRs complexed with ligands [80]. Perhaps bivalent or multifunctional opioid ligands like buprenorphine and BU10119, each with a unique profile of pharmacological activity across the opioid receptors, offer wider therapeutic potential in the treatment of mood disorders [81].
In addition to close structural homology, opioid receptors can function either as a monomer or as part of a homo- or heterodimer or higher multimer [82]. For example, MOP and DOP receptors heterodimerize in vivo causing a change in receptor properties and signalling [83]. Both in vivo and in vitro evidence suggest that these heteromers can switch G-protein coupling preference, thus displaying a significantly different signalling pathway compared with their corresponding homomers [84]. It has also been demonstrated that KOP and DOP receptors heterodimerize in vivo in the spinal cord where they produce a unique receptor pharmacology making the design of analgesics with functional selectivity a possibility [85]. Adding further complexity, MOP, KOP and DOP receptors are increasingly recognized to show functional selectivity or biased agonism [86]. This means that ligands which bind to the same receptor can elicit distinct conformations that preferentially signal through distinct G-protein or arrestin subtypes. There is interest in exploiting bias signalling at opioid receptors to improve analgesics as a way of separating the desired therapeutc effect from the unwanted side effects, which limit their clinical utility [87]. The effects of agonist bias signalling through opioid receptors implicated in regulation of mood and anhedonia are largely unknown.
Rebalancing of opioid receptor dysregulation in stress-induced mood disorders is not as simple as targeting a single opioid receptor. There is much potential for designing multifunctional opioid ligands with a unique pharmacology targeting multiple opioid receptors and activating biased intracellular signalling. Better understanding of the downstream signalling pathways of opioid receptors, the role of heterodimers and ligand bias signalling and their role in hedonic tone and motivated behaviours should lead to promising new treatments for depression.
Abbreviations
- CRF
corticotrophin releasing factor
- DOP
δ opioid receptor
- GABA
gamma-aminobutyric acid
- GPCR
G-protein coupled receptor
- HPA
hypothalamus-pituitary-adrenal
- JDTic
(3R)-7-Hydroxy-N-[(1S)-1-[[(3R,4R)-4-(3-hydroxyphenyl)-3,4-dimethyl-1-piperidinyl]methyl]-2-methylpropyl]-1,2,3,4-tetrahydro-3-isoquinoline-carboxamide
- JNK1
c-jun n-terminal kinase-1
- KOP
κ opioid receptor
- MOP
μ opioid receptor
- NOP
nociceptin/orphanin FQ receptor
- norBNI
norbinaltorphamine
- SSRI
selective serotonin reuptake inhibitor
- VTA
ventral tegmental area
- 5′-AMN
5′-(aminomethyl) naltrindole
- 5′-MABN
N-((Naltrindol-5-yl) methyl) pentanimidamide
Competing interests
The authors declare that there are no competing interests associated with the manuscript.
References
- 1.Corbett A.D., Henderson G., McKnight A.T. and Paterson S.J. (2006) 75 years of opioid research: the exciting but vain quest for the Holy Grail. Br. J. Pharmacol. 147 (Suppl. 1), S153–S162 10.1038/sj.bjp.0706435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Van’t Veer A. and Carlezon W. Jr (2013) Role of kappa-opioid receptors in stress and anxiety-related behavior. Psychopharmacology (Berl.) 229, 435–452 10.1007/s00213-013-3195-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lutz P.-E. and Kieffer B.L. (2013) Opioid receptors: distinct roles in mood disorders. Trends Neurosci. 36, 195–206 10.1016/j.tins.2012.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carroll F.I. and Carlezon W.A. (2013) Development of κ opioid receptor antagonists. J. Med. Chem. 56, 2178–2195 10.1021/jm301783x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Toll L., Caló G., Cox B.M., Chavkin C., Christie M.J., Civelli O. et al. (2017) Opioid receptors. In IUPHAR/BPS Guide to Pharmacology, http://www.guidetopharmacologyorg/GRAC/FamilyDisplayForward?familyId=50
- 6.Belujon P. and Grace A.A. (2017) Dopamine system dysregulation in major depressive disorders. Int. J. Neuropsychopharmacol. 20, 1036–1046 10.1093/ijnp/pyx056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sternat T. and Katzman M.A. (2016) Neurobiology of hedonic tone: the relationship between treatment-resistant depression, attention-deficit hyperactivity disorder, and substance abuse. Neuropsychiatr. Dis. Treat. 12, 2149–2164 10.2147/NDT.S111818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nestler E.J. and Carlezon W.A. Jr (2006) The mesolimbic dopamine reward circuit in depression. Biol. Psychiatry 59, 1151–1159 10.1016/j.biopsych.2005.09.018 [DOI] [PubMed] [Google Scholar]
- 9.Terman G.W., Drake C.T., Simmons M.L., Milner T.A. and Chavkin C. (2000) Opioid modulation of recurrent excitation in the hippocampal dentate gyrus. J. Neurosci. 20, 4379–4388 10.1523/JNEUROSCI.20-12-04379.2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rubin D.H. (2012) Joy returns last: anhedonia and treatment resistance in depressed adolescents. J. Am. Acad. Child Adolesc. Psychiatry 51, 353–355 10.1016/j.jaac.2012.01.012 [DOI] [PubMed] [Google Scholar]
- 11.McMakin D.L., Olino T.M., Porta G., Dietz L.J., Emslie G., Clarke G. et al. (2012) Anhedonia predicts poorer recovery among youth with selective serotonin reuptake inhibitor treatment–resistant depression. J. Am. Acad. Child Adolesc. Psychiatry 51, 404–411 10.1016/j.jaac.2012.01.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McCabe C., Mishor Z., Cowen P.J. and Harmer C.J. (2010) Diminished neural processing of aversive and rewarding stimuli during selective serotonin reuptake inhibitor treatment. Biol. Psychiatry 67, 439–445 10.1016/j.biopsych.2009.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Price J., Cole V. and Goodwin G.M. (2009) Emotional side-effects of selective serotonin reuptake inhibitors: qualitative study. Br. J. Psychiatry 195, 211–217 10.1192/bjp.bp.108.051110 [DOI] [PubMed] [Google Scholar]
- 14.Cousins L. and Goodyer I.M. (2015) Antidepressants and the adolescent brain. J. Psychopharmacol. 29, 545–555 10.1177/0269881115573542 [DOI] [PubMed] [Google Scholar]
- 15.Walkup J.T. (2017) Antidepressant efficacy for depression in children and adolescents: industry- and NIMH-funded studies. Am. J. Psychiatry 174, 430–437 10.1176/appi.ajp.2017.16091059 [DOI] [PubMed] [Google Scholar]
- 16.Berrocoso E., Sanchez-Blazquez P., Garzon J. and Mico J.A. (2009) Opiates as antidepressants. Curr. Pharm. Des. 15, 1612–1622 10.2174/138161209788168100 [DOI] [PubMed] [Google Scholar]
- 17.Hegadoren K.M., O’Donnell T., Lanius R., Coupland N.J. and Lacaze-Masmonteil N. (2009) The role of β-endorphin in the pathophysiology of major depression. Neuropeptides 43, 341–353 10.1016/j.npep.2009.06.004 [DOI] [PubMed] [Google Scholar]
- 18.Goodwin G.M., Austin M.-P., Curran S.M., Ross M., Murray C., Prentice N. et al. (1993) The elevation of plasma β-endorphin levels in major depression. J. Affect. Disord. 29, 281–289 10.1016/0165-0327(93)90018-F [DOI] [PubMed] [Google Scholar]
- 19.Bodkin J.A., Zornberg G.L., Lukas S.E. and Cole J.O. (1995) Buprenorphine treatment of refractory depression. J. Clin. Psychopharmacol. 15, 49–57 10.1097/00004714-199502000-00008 [DOI] [PubMed] [Google Scholar]
- 20.Karp J.F., Butters M.A., Begley A.E., Miller M.D., Lenze E.J., Blumberger D.M. et al. (2014) Safety, tolerability, and clinical effect of low-dose buprenorphine for treatment-resistant depression in midlife and older adults. J. Clin. Psychiatry 75, e785–e793 10.4088/JCP.13m08725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yovell Y., Bar G., Mashiah M., Baruch Y., Briskman I., Asherov J. et al. (2016) Ultra-low-dose buprenorphine as a time-limited treatment for severe suicidal ideation: a randomized controlled trial. Am. J. Psychiatry 173, 491–498 10.1176/appi.ajp.2015.15040535 [DOI] [PubMed] [Google Scholar]
- 22.Stoll A.L. and Rueter S. (1999) Treatment augmentation with opiates in severe and refractory major depression. Am. J. Psychiatry 156, 2017. [DOI] [PubMed] [Google Scholar]
- 23.Striebel J.M. and Kalapatapu R.K. (2014) The anti-suicidal potential of buprenorphine: a case report. Int. J. Psychiatry Med. 47, 169–174 10.2190/PM.47.2.g [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Charney D.S. and Manji H.K. (2004) Life stress, genes, and depression: multiple pathways lead to increased risk and new opportunities for intervention. Sci. STKE 2004, re5, [DOI] [PubMed] [Google Scholar]
- 25.Zhou Y., Leri F., Ho A. and Kreek M.J. (2013) Suppression of hypothalamic–pituitary–adrenal axis by acute heroin challenge in rats during acute and chronic withdrawal from chronic heroin administration. Neurochem. Res. 38, 1850–1860 10.1007/s11064-013-1091-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhou Y. and Leri F. (2016) Neuroscience of opiates for addiction medicine: From stress-responsive systems to behavior. In Progress in Brain Research vol. 223, (Ekhtiari H. and Paulus M., eds), pp. 237–251, Elsevier; [DOI] [PubMed] [Google Scholar]
- 27.Knoll A. and Carlezon W. (2010) Dynorphin, stress, and depression. Brain Res. 1314, 56–73 10.1016/j.brainres.2009.09.074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Land B.B., Bruchas M.R., Lemos J.C., Xu M., Melief E.J. and Chavkin C. (2008) The dysphoric component of stress is encoded by activation of the dynorphin kappa-opioid system. J. Neurosci. 28, 407–414 10.1523/JNEUROSCI.4458-07.2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McLaughlin J.P., Land B.B., Li S., Pintar J.E. and Chavkin C. (2006) Prior activation of kappa opioid receptors by U50,488 mimics repeated forced swim stress to potentiate cocaine place preference conditioning. Neuropsychopharmacology 31, 787–794 10.1038/sj.npp.1300860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McLaughlin J.P., Li S., Valdez J., Chavkin T.A. and Chavkin C. (2006) Social defeat stress-induced behavioral responses are mediated by the endogenous kappa opioid system. Neuropsychopharmacology 31, 1241–1248 10.1038/sj.npp.1300872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McLaughlin J.P., Marton-Popovici M. and Chavkin C. (2003) Kappa opioid receptor antagonism and prodynorphin gene disruption block stress-induced behavioral responses. J. Neurosci. 23, 5674–5683 10.1523/JNEUROSCI.23-13-05674.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bruchas M.R., Land B.B., Aita M., Xu M., Barot S.K., Li S. et al. (2007) Stress-induced p38 mitogen-activated protein kinase activation mediates kappa-opioid-dependent dysphoria. J. Neurosci. 27, 11614–11623 10.1523/JNEUROSCI.3769-07.2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shirayama Y., Ishida H., Iwata M., Hazama G.I., Kawahara R. and Duman R.S. (2004) Stress increases dynorphin immunoreactivity in limbic brain regions and dynorphin antagonism produces antidepressant-like effects. J. Neurochem. 90, 1258–1268 10.1111/j.1471-4159.2004.02589.x [DOI] [PubMed] [Google Scholar]
- 34.Newton S.S., Thome J., Wallace T.L., Shirayama Y., Schlesinger L., Sakai N. et al. (2002) Inhibition of cAMP response element-binding protein or dynorphin in the nucleus accumbens produces an antidepressant-like effect. J. Neurosci. 22, 10883–10890 10.1523/JNEUROSCI.22-24-10883.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Todtenkopf M.S., Marcus J.F., Portoghese P.S. and Carlezon W.A. Jr (2004) Effects of kappa-opioid receptor ligands on intracranial self-stimulation in rats. Psychopharmacology (Berl.) 172, 463–470 10.1007/s00213-003-1680-y [DOI] [PubMed] [Google Scholar]
- 36.Pfeiffer A., Brantl V., Herz A. and Emrich H.M. (1986) Psychotomimesis mediated by kappa opiate receptors. Science 233, 774–776 10.1126/science.3016896 [DOI] [PubMed] [Google Scholar]
- 37.Ranganathan M., Schnakenberg A., Skosnik P.D., Cohen B.M., Pittman B., Sewell R.A. et al. (2012) Dose-related behavioral, subjective, endocrine, and psychophysiological effects of the κ opioid agonist Salvinorin A in humans. Biol. Psychiatry 72, 871–879 10.1016/j.biopsych.2012.06.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.White K.L. and Roth B.L. (2012) Psychotomimetic effects of kappa opioid receptor agonists. Biol. Psychiatry 72, 797–798 10.1016/j.biopsych.2012.08.014 [DOI] [PubMed] [Google Scholar]
- 39.Taylor G.T. and Manzella F. (2016) Kappa opioids, salvinorin A and major depressive disorder. Curr. Neuropharmacol. 14, 165–176 10.2174/1570159X13666150727220944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Carlezon W.A. Jr, Beguin C., DiNieri J.A., Baumann M.H., Richards M.R., Todtenkopf M.S. et al. (2006) Depressive-like effects of the kappa-opioid receptor agonist salvinorin A on behavior and neurochemistry in rats. J. Pharmacol. Exp. Ther. 316, 440–447 10.1124/jpet.105.092304 [DOI] [PubMed] [Google Scholar]
- 41.Portoghese P., Nagase H., Lipkowski A., Larson D. and Takemori A. (1988) Binaltorphimine-related bivalent ligands and their kappa opioid receptor antagonist selectivity. J. Med. Chem. 31, 836–841 10.1021/jm00399a026 [DOI] [PubMed] [Google Scholar]
- 42.Stevens W., Jones R., Subramanian G., Metzger T., Ferguson D. and Portoghese P. (2000) Potent and selective indolomorphinan antagonists of the kappa-opioid receptor. J. Med. Chem. 43, 2759–2769 10.1021/jm0000665 [DOI] [PubMed] [Google Scholar]
- 43.Thomas J.B., Atkinson R.N., Rothman R.B., Fix S.E., Mascarella S.W., Vinson N.A. et al. (2001) Identification of the first trans-(3R,4R)-dimethyl-4-(3-hydroxyphenyl)piperidine derivative to possess highly potent and selective opioid κ receptor antagonist activity. J. Med. Chem. 44, 2687–2690 10.1021/jm015521r [DOI] [PubMed] [Google Scholar]
- 44.Endoh T., Matsuura H., Tanaka C. and Nagase H. (1992) Nor-binaltorphimine: a potent and selective kappa-opioid receptor antagonist with long-lasting activity in vivo. Arch. Int. Pharmacodyn. Ther. 316, 30–42 [PubMed] [Google Scholar]
- 45.Negus S., Mello N., Linsenmayer D., Jones R. and Portoghese P. (2002) Kappa opioid antagonist effects of the novel kappa antagonist 5′-guanidinonaltrindole (GNTI) in an assay of schedule-controlled behavior in rhesus monkeys. Psychopharmacology (Berl.) 163, 412–419 10.1007/s00213-002-1038-x [DOI] [PubMed] [Google Scholar]
- 46.Carroll I., Thomas J., Dykstra L., Granger A., Allen R., Howard J. et al. (2004) Pharmacological properties of JDTic: a novel kappa-opioid receptor antagonist. Eur. J. Pharmacol. 501, 111–119 10.1016/j.ejphar.2004.08.028 [DOI] [PubMed] [Google Scholar]
- 47.Aldrich J., Patkar K. and McLaughlin J. (2009) Zyklophin, a systemically active selective kappa opioid receptor peptide antagonist with short duration of action. Proc. Natl. Acad. Sci. U.S.A. 106, 18396–18401 10.1073/pnas.0910180106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Peters M.F., Zacco A., Gordon J., Maciag C.M., Litwin L.C., Thompson C. et al. (2011) Identification of short-acting κ-opioid receptor antagonists with anxiolytic-like activity. Eur. J. Pharmacol. 661, 27–34 10.1016/j.ejphar.2011.04.017 [DOI] [PubMed] [Google Scholar]
- 49.Verhoest P.R., Sawant Basak A., Parikh V., Hayward M., Kauffman G.W., Paradis V. et al. (2011) Design and discovery of a selective small molecule kappa opioid antagonist (2-Methyl-N-((2′-(pyrrolidin-1-ylsulfonyl)biphenyl-4-yl)methyl)propan-1-am ine, PF-4455242). J. Med. Chem. 54, 5868–5877 10.1021/jm2006035 [DOI] [PubMed] [Google Scholar]
- 50.Ross N., Reilley K., Murray T., Aldrich J. and McLaughlin J. (2012) Novel opioid cyclic tetrapeptides: Trp isomers of CJ-15,208 exhibit distinct opioid receptor agonism and short-acting kappa opioid receptor antagonism. Br. J. Pharmacol. 165, 1097–1108 10.1111/j.1476-5381.2011.01544.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Casal-Dominguez J.J., Furkert D., Ostovar M., Teintang L., Clark M.J., Traynor J.R. et al. (2014) Characterization of BU09059: a novel potent selective κ-receptor antagonist. ACS Chem. Neurosci. 5, 177–184 10.1021/cn4001507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rorick-Kehn L.M., Witkin J.M., Statnick M.A., Eberle E.L., McKinzie J.H., Kahl S.D. et al. (2014) LY2456302 is a novel, potent, orally-bioavailable small molecule kappa-selective antagonist with activity in animal models predictive of efficacy in mood and addictive disorders. Neuropharmacology 77, 131–144 10.1016/j.neuropharm.2013.09.021 [DOI] [PubMed] [Google Scholar]
- 53.Melief E.J., Miyatake M., Carroll F.I., Beguin C., Carlezon W.A. Jr, Cohen B.M. et al. (2011) Duration of action of a broad range of selective kappa-opioid receptor antagonists is positively correlated with c-Jun N-terminal kinase-1 activation. Mol. Pharmacol. 80, 920–929 10.1124/mol.111.074195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bruchas M.R. and Chavkin C. (2010) Kinase cascades and ligand-directed signaling at the kappa opioid receptor. Psychopharmacology (Berl.) 210, 137–147 10.1007/s00213-010-1806-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Olmsted S.L., Takemori A.E. and Portoghese P.S. (1993) A remarkable change of opioid receptor selectivity on the attachment of a peptidomimetic kappa address element to the delta antagonist, naltrindole: 5′-[N2-alkylamidino) methyl]naltrindole derivatives as a novel class of kappa opioid receptor antagonists. J. Med. Chem. 36, 179–180 10.1021/jm00053a025 [DOI] [PubMed] [Google Scholar]
- 56.Stevens W.C. Jr, Jones R.M., Subramanian G., Metzger T.G., Ferguson D.M. and Portoghese P.S. (2000) Potent and selective indolomorphinan antagonists of the kappa-opioid receptor. J. Med. Chem. 43, 2759–2769 10.1021/jm0000665 [DOI] [PubMed] [Google Scholar]
- 57.Casal-Dominguez J.J., Clark M., Traynor J.R., Husbands S.M. and Bailey S.J. (2013) In vivo and in vitro characterization of naltrindole-derived ligands at the κ-opioid receptor. J. Psychopharmacol. 27, 192–202 10.1177/0269881112464828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Almatroudi A., Husbands S.M., Bailey C.P. and Bailey S.J. (2015) Combined administration of buprenorphine and naltrexone produces antidepressant-like effects in mice. J. Psychopharmacol. 29, 812–821 10.1177/0269881115586937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Gerra G., Fantoma A. and Zaimovic A. (2006) Naltrexone and buprenorphine combination in the treatment of opioid dependence. J. Psychopharmacol. 20, 806–814 10.1177/0269881106060835 [DOI] [PubMed] [Google Scholar]
- 60.Huang P., Kehner G.B., Cowan A. and Liu-Chen L.-Y. (2001) Comparison of pharmacological activities of buprenorphine and norbuprenorphine: norbuprenorphine is a potent opioid agonist. J. Pharmacol. Exp. Ther. 297, 688–695 [PubMed] [Google Scholar]
- 61.Lutfy K. and Cowan A. (2004) Buprenorphine: a unique drug with complex pharmacology. Curr. Neuropharmacol. 2, 395–402 10.2174/1570159043359477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Almatroudi A., Ostovar M., Bailey C.P., Husbands S.M. and Bailey S.J. (2017) Antidepressant-like effects of BU10119, a novel buprenorphine analogue with mixed κ/μ receptor antagonist properties, in mice. Br. J. Pharmacol., 10.1111/bph.14060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Robinson S.A., Erickson R.L., Browne C.A. and Lucki I. (2017) A role for the mu opioid receptor in the antidepressant effects of buprenorphine. Behav. Brain Res. 319, 96–103 10.1016/j.bbr.2016.10.050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hollister L.E., Johnson K., Boukhabza D. and Gillespie H.K. (1981) Aversive effects of naltrexone in subjects not dependent on opiates. Drug Alcohol Depend. 8, 37–41 10.1016/0376-8716(81)90084-3 [DOI] [PubMed] [Google Scholar]
- 65.Malcolm R., O’Neil P.M., Von J.M. and Dickerson P.C. (1987) Naltrexone and dysphoria: a double-blind placebo controlled trial. Biol. Psychiatry 22, 710–716 10.1016/0006-3223(87)90202-2 [DOI] [PubMed] [Google Scholar]
- 66.Mysels D.J., Cheng W.Y., Nunes E.V. and Sullivan M.A. (2011) The association between naltrexone treatment and symptoms of depression in opioid-dependent patients. Am. J. Drug Alcohol Abuse 37, 22–26 10.3109/00952990.2010.540281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Mischoulon D., Hylek L., Yeung A.S., Clain A.J., Baer L., Cusin C. et al. (2017) Randomized, proof-of-concept trial of low dose naltrexone for patients with breakthrough symptoms of major depressive disorder on antidepressants. J. Affect. Disord. 208, 6–14 10.1016/j.jad.2016.08.029 [DOI] [PubMed] [Google Scholar]
- 68.Browne C.A., van Nest D.S. and Lucki I. (2015) Antidepressant-like effects of buprenorphine in rats are strain dependent. Behav. Brain Res. 278, 385–392 10.1016/j.bbr.2014.10.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Falcon E., Maier K., Robinson S.A., Hill-Smith T.E. and Lucki I. (2015) Effects of buprenorphine on behavioral tests for antidepressant and anxiolytic drugs in mice. Psychopharmacology (Berl.) 232, 907–915 10.1007/s00213-014-3723-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Cicero T.J., Ellis M.S., Surratt H.L. and Kurtz S.P. (2014) Factors contributing to the rise of buprenorphine misuse: 2008-2013. Drug Alcohol Depend. 142, 98–104 10.1016/j.drugalcdep.2014.06.005 [DOI] [PubMed] [Google Scholar]
- 71.Browne C.A., Falcon E., Robinson S.A., Berton O. and Lucki I. (2017) Reversal of stress-induced social interaction deficits by buprenorphine. Int. J. Neuropsychopharmacol., 10.1093/ijnp/pyx079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ehrich E., Turncliff R., Du Y., Leigh-Pemberton R., Fernandez E., Jones R. et al. (2015) Evaluation of opioid modulation in major depressive disorder. Neuropsychopharmacology 40, 1448–1455 10.1038/npp.2014.330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Fava M., Memisoglu A., Thase M.E., Bodkin J.A., Trivedi M.H., de Somer M. et al. (2016) Opioid modulation with buprenorphine/samidorphan as adjunctive treatment for inadequate response to antidepressants: a randomized double-blind placebo-controlled trial. Am. J. Psychiatry 173, 499–508 10.1176/appi.ajp.2015.15070921 [DOI] [PubMed] [Google Scholar]
- 74.Broom D.C., Jutkiewicz E.M., Folk J.E., Traynor J.R., Rice K.C. and Woods J.H. (2002) Nonpeptidic δ-opioid receptor agonists reduce immobility in the forced swim assay in rats. Neuropsychopharmacology 26, 744 10.1016/S0893-133X(01)00413-4 [DOI] [PubMed] [Google Scholar]
- 75.Broom D.C., Jutkiewicz E.M., Folk J.E., Traynor J.R., Rice K.C. and Woods J.H. (2002) Convulsant activity of a non-peptidic δ-opioid receptor agonist is not required for its antidepressant-like effects in Sprague-Dawley rats. Psychopharmacology (Berl.) 164, 42–48 10.1007/s00213-002-1179-y [DOI] [PubMed] [Google Scholar]
- 76.Dripps I.J. and Jutkiewicz E.M. (2017) Delta Opioid Receptors and Modulation of Mood and Emotion, pp. 1–19, Springer Berlin Heidelberg, Berlin, Heidelberg: [DOI] [PubMed] [Google Scholar]
- 77.Toll L., Bruchas M.R., Calo’ G., Cox B.M. and Zaveri N.T. (2016) Nociceptin/orphanin FQ receptor structure, signaling, ligands, functions, and interactions with opioid systems. Pharmacol. Rev. 68, 419–457 10.1124/pr.114.009209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Goeldner C., Spooren W., Wichmann J. and Prinssen E.P. (2012) Further characterization of the prototypical nociceptin/orphanin FQ peptide receptor agonist Ro 64-6198 in rodent models of conflict anxiety and despair. Psychopharmacology (Berl.) 222, 203–214 10.1007/s00213-012-2636-x [DOI] [PubMed] [Google Scholar]
- 79.Cueva J.P., Roche C., Ostovar M., Kumar V., Clark M.J., Hillhouse T.M. et al. (2015) C7β-methyl analogues of the orvinols: the discovery of kappa opioid antagonists with nociceptin/orphanin FQ peptide (NOP) receptor partial agonism and low, or zero, efficacy at mu opioid receptors. J. Med. Chem. 58, 4242–4249 10.1021/acs.jmedchem.5b00130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Filizola M. and Devi L.A., Grand opening of structure-guided design for novel opioids. Trends Pharmacol. Sci. 34, 6–12 10.1016/j.tips.2012.10.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Schiller P.W. (2010) Bi- or multifunctional opioid peptide drugs. Life Sci. 86, 598–603 10.1016/j.lfs.2009.02.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Cox B.M., Christie M.J., Devi L., Toll L. and Traynor J.R. (2015) Challenges for opioid receptor nomenclature: IUPHAR Review 9. Br. J. Pharmacol. 172, 317–323 10.1111/bph.12612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Fujita W., Gomes I. and Devi L.A. (2015) Heteromers of μ-δ opioid receptors: new pharmacology and novel therapeutic possibilities. Br. J. Pharmacol. 172, 375–387 10.1111/bph.12663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Milan-Lobo L. and Whistler J.L. (2011) Heteromerization of the μ- and δ-opioid receptors produces ligand-biased antagonism and alters μ-receptor trafficking. J. Pharmacol. Exp. Ther. 337, 868–875 10.1124/jpet.111.179093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Berg K.A., Rowan M.P., Gupta A., Sanchez T.A., Silva M., Gomes I. et al. (2012) Allosteric interactions between δ and κ opioid receptors in peripheral sensory neurons. Mol. Pharmacol. 81, 264–272 10.1124/mol.111.072702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Pradhan A.A., Smith M.L., Kieffer B.L. and Evans C.J. (2012) Ligand-directed signalling within the opioid receptor family. Br. J. Pharmacol. 167, 960–969 10.1111/j.1476-5381.2012.02075.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Charfi I., Audet N., Bagheri Tudashki H. and Pineyro G. (2015) Identifying ligand-specific signalling within biased responses: focus on δ opioid receptor ligands. Br. J. Pharmacol. 172, 435–448 10.1111/bph.12705 [DOI] [PMC free article] [PubMed] [Google Scholar]