Abstract
Objectives
We conducted a subanalysis of data from the multicentre, retrospective observational Nivolumab Japan Real World (CA209-9CR) study to evaluate nivolumab effectiveness and safety in elderly patients (aged ≥75 years) with advanced/metastatic non-small cell lung cancer.
Materials and methods
Medical record data of patients initiating nivolumab treatment between April 2016 and December 2016 were collected using electronic data capture from 23 cancer hospitals in Japan between March 2017 and August 2018. Nivolumab treatment data were collected to investigate the treatment patterns by age group (<75 and ≥75 years), and the effectiveness and safety of nivolumab treatment.
Results
Of the 901 patients evaluated, 178 (19.8%) were aged ≥75 years. Overall, patients received a median of five nivolumab treatments regardless of age group. Comparable progression-free survival was observed, with a median of 2.1 months in patients aged <75 years and 2.1 months in patients aged ≥75 years (p=0.5441). No significant differences were found in duration of response, overall response rate or disease control rate between the two age groups. Median overall survival in patients aged <75 and ≥75 years was 14.7 months and 12.3 months, respectively. Grade ≥3 adverse events (AEs) occurred in 29.2% and 28.1% of patients aged <75 and ≥75 years, respectively. Immune-related AEs decreased slightly with increasing age; time to onset and rates of improvement were similar for patients aged <75 and ≥75 years. The most common grade 3–4 AEs were interstitial lung disease in both age groups (4.0% in patients aged <75 years and 2.8% in those aged ≥75 years). Poor performance status was associated with worse outcomes in both age groups.
Conclusion
Based on Japanese real-world data, the effectiveness and safety of nivolumab were confirmed regardless of age.
Keywords: nivolumab, elderly, Japan, non-small cell lung cancer
Key question.
What is already known about this subject?
As longevity of the Japanese population rises, elderly patients account for the majority of patients with non-small cell lung cancer (NSCLC) in Japan.
Age has been found to be a major prognostic factor of survival in patients with NSCLC treated with conventional chemotherapies; however, a similar association between age and survival has not been fully determined in immune checkpoint inhibitors.
What does this study add?
This study assessed effectiveness and safety of nivolumab, the first approved immune checkpoint inhibitor in Japan, in elderly patients with NSCLC and found that safety and effectiveness were consistent among elderly (75 years old or more) and non-elderly (less than 75 years) patients. Instead of age, better performance status was associated with better outcomes regardless of age.
How might this impact on clinical practice?
This study suggests that age is not associated with the effectiveness or safety of nivolumab in a large Japanese population.
Moreover, nivolumab treatment for elderly patients with good performance status may be a reasonable option.
Introduction
Globally, lung cancer is the most commonly diagnosed cancer (11.6% of all cancers) and the leading cause of cancer deaths (18.4% of total cancer deaths).1 It is a significant problem in Japan, affecting 15.0% (n=86 700) of men and 10.0% (n=42 000) of women, and resulting in 25.0% and 14.0% of cancer deaths, respectively.2 The age at diagnosis of Japanese patients with lung cancer is increasing, with a notable increase in incidence rate among patients aged ≥70 years in the past three decades.2 According to epidemiological data, >80% of all lung cancer cases are classified as non-small cell lung cancer (NSCLC).3 4
Programmed death-1 (PD-1) inhibitors, such as the immune checkpoint inhibitor nivolumab, have shown superiority over conventional therapy when used as monotherapy in patients with NSCLC, malignant melanoma, renal cell cancer, head and neck carcinoma and gastric cancer, and are now routinely used for the treatment of NSCLC.5 In two phase III NSCLC studies conducted outside of Japan, nivolumab was shown to be superior to docetaxel in terms of overall survival (OS). In CheckMate 017,6 in patients with squamous cell NSCLC who received nivolumab or docetaxel as second-line therapy after platinum treatment, the median OS was 9.2 months with nivolumab versus 6.0 months with docetaxel. In CheckMate 057,7 in patients with non-squamous cell NSCLC, the median OS was 12.2 months with nivolumab versus 9.4 months with docetaxel. The efficacy and safety of nivolumab have also been confirmed in two phase II Japanese studies in patients with NSCLC. In ONO-4538-05 (squamous cell)8 and ONO-4538-06 (non-squamous cell),9 the median OS with nivolumab was 16.3 months and 17.1 months, respectively. Based on these results, in December 2015, nivolumab was approved for the treatment of previously treated, unresectable, locally advanced or metastatic NSCLC regardless of histological type or programmed death ligand 1 (PD-L1) mutation presence. Nivolumab is the first approved PD-1 inhibitor in Japan.
Although age has been identified as a major prognostic factor of survival in patients with lung cancer receiving conventional therapy,10 a similar association has not yet been determined for PD-1 or immunotherapy. Nevertheless, because elderly patients comprise the largest proportion of patients with lung cancer, both in Japan2 and in Western countries,11–13 treatment and management of patients with lung cancer may need to be optimised according to age.14 Furthermore, it is clear that the prevalence of multimorbidity increases substantially with age15 and concurrently, physiological function gradually decreases with age.16 However, historically, patients aged 75 years and over have been excluded from clinical trials in Japan.17 Eastern Cooperative Oncology Group Performance Status (ECOG PS) has also been reported as a prognostic factor of survival in pharmacotherapy,18 19; however, for this reason, reports of effectiveness by ECOG PS in Japanese elderly patients were insufficient.
According to the Japanese Lung Cancer Society Guideline for NSCLC, stage IV17 elderly patients are defined as those aged ≥75 years, and the recommended treatment method can differ according to age. In CheckMate 0176 and CheckMate 057,7 the proportions of patients aged ≥75 years were limited to 11% (29 patients) and 7% (43 patients), respectively. For this reason, the efficacy and safety data of immune checkpoint inhibitors, including nivolumab, in this population are limited. Therefore, real-world large-cohort data are needed.
The multicentre, retrospective, observational Nivolumab Japan Real World (CA209-9CR) study was designed to evaluate the effectiveness, safety and treatment patterns of nivolumab in Japanese patients with NSCLC.18 Herein, we describe a subanalysis of elderly patients (aged ≥75 years) with advanced/metastatic NSCLC treated with nivolumab to evaluate nivolumab effectiveness and safety in this age group.
Materials and methods
Study design, data collection, treatment and ethical considerations
The full details of the study design were recently reported.19 This was a multicentre, non-interventional, retrospective medical chart review study (trial registration NCT03273790) in which medical record data (collected by participating investigators using electronic data capture; Mebix, Inc, Tokyo, Japan) from 23 cancer hospitals in Japan were analysed.
The study was conducted from 1 April 2017 to 31 December 2018. Data recorded prior, during and after nivolumab treatment were collected to investigate the treatment trends before and after nivolumab treatment, and the safety and effectiveness of nivolumab treatment.
The study protocol was approved by the Ethics Committees or Independent Review Committees of each participating site. The study was conducted in accordance with Ethical Guidelines for Medical and Health Research Involving Human Subjects,20 and all other applicable national and international guidelines. Informed consent was not required owing to the retrospective nature of this study, although patients were allowed to opt out from study participation.
Study population
The study population has been described.19 Previously treated advanced/metastatic patients with NSCLC who initiated nivolumab treatment between April 2016 and December 2016 were included, with the exception of patients who participated in the postmarketing surveillance of nivolumab and patients who participated in any clinical studies prior to or after nivolumab treatment.
Endpoints and assessments
For this subanalysis, the population was stratified into two groups: <75 years and ≥75 years. OS, progression-free survival (PFS), duration of response (DOR) and best overall response (objective response rate (ORR) and disease control rate (DCR)) were calculated. For a supplementary effectiveness analysis, the population was stratified into three groups: <75 years, 75 to <80 years and ≥80 years. The outcomes included clinical usage and treatment patterns by age group (ie, dosage, median number of treatments, median treatment duration, treatment line and reasons for discontinuation from nivolumab treatment).
Overall effectiveness of nivolumab was investigator assessed. Tumour evaluation was performed according to the methodology described in the Response Evaluation Criteria in Solid Tumors (V.1.1). OS was defined as the date of first nivolumab administration to the date of death from any cause. PFS was defined as the date of first nivolumab administration to the date of disease progression or death. DOR was defined as the time from first response to death or progression. ORR was defined as the number of patients achieving complete response (CR) or partial response (PR), and DCR was the proportion of patients achieving CR, PR or stable disease.
The OS, PFS and best overall response in elderly patients (aged ≥75 years) by ECOG PS were also calculated. In addition, response was evaluated according to serum albumin and body mass index (BMI), with responders defined as patients whose best overall response was CR or PR.
The safety of nivolumab, including incidence and severity of adverse events (AEs) and treatment-related AEs (immune-related AEs (irAEs)), was also investigator assessed. The severity of AEs was assessed according to the National Cancer Institute Common Terminology Criteria for Adverse Events Grading System, V.4.0.21
Statistical methods
Study calculations have been reported.19 All eligible patients enrolled in the study were included in the analyses. For this subanalysis, the effectiveness and safety of nivolumab were assessed in patients aged ≥75 years and compared with patients aged <75 years; for the supplementary analysis, effectiveness outcomes were assessed in patients aged <75 years, 75 to <80 years and ≥80 years. Summary statistics (median (range)) were used for continuous variables, and frequency and percentage were used for categorical or ordinal variables. For OS and PFS, median and 95% CIs were estimated using the Kaplan-Meier method. Differences were considered statistically significant at p values <0.05. Statistical analysis was performed using SAS V.9.4 (SAS Institute Inc, Cary, North Carolina, USA).
Results
Patients
Overall, medical record data of 901 patients were collected from 23 cancer hospitals in Japan.19 The major baseline characteristics and clinical background according to age group (<75 years and ≥75 years) are shown in table 1. Of the 901 patients evaluated, 178 (19.8%) were aged ≥75 years. Most patients aged <75 years had an ECOG PS of 1 (54.4%), adenocarcinoma (67.7%), and presence of metastases (77.5%).
Table 1.
Patient demographics and clinical background by age group
| Variable | All patients | <75 years | ≥75 years | Difference <75 years vs ≥75 years |
| Patients, n (%) | 901 (100.0) | 723 (100.0) | 178 (100.0) | – |
| Gender, n (%) | ||||
| Male | 651 (72.3) | 519 (71.8) | 132 (74.2) | 0.5754* |
| Female | 250 (27.7) | 204 (28.2) | 46 (25.8) | |
| Age (years), median (range) | 67.0 (30.0–90.0) | 65.0 (30.0–74.0) | 78.0 (75.0–90.0) | – |
| BMI (kg/m2), median (range) | 21.4 (12.9–36.9) | 21.4 (12.9–36.9) | 21.3 (13.6–30.7) | 0.4087† |
| Disease stage at diagnosis of NSCLC, n (%) | ||||
| IA−IIIA | 302 (33.5) | 232 (32.1) | 70 (39.3) | 0.1625* |
| IIIB | 102 (11.3) | 86 (11.9) | 16 (9.0) | |
| IV | 497 (55.2) | 405 (56.0) | 92 (51.7) | |
| ECOG PS, n (%) | ||||
| 0 | 193 (21.4) | 162 (22.4) | 31 (17.4) | 0.0253*‡ |
| 1 | 490 (54.4) | 379 (52.4) | 111 (62.4) | |
| 2 | 109 (12.1) | 93 (12.9) | 16 (9.0) | |
| 3 and 4 | 48 (5.3) | 33 (4.6) | 15 (8.4) | |
| Missing | 61 (6.8) | 56 (7.7) | 5 (2.8) | |
| Histological type, n (%) | ||||
| Squamous cell carcinoma | 221 (24.5) | 159 (22.0) | 62 (34.8) | 0.0017* |
| Adenocarcinoma | 610 (67.7) | 505 (69.8) | 105 (59.0) | |
| Other | 28 (3.1) | 21 (2.9) | 7 (3.9) | |
| Unclassified | 42 (4.7) | 38 (5.3) | 4 (2.2) | |
| Other primary malignant tumours, n (%) | 100 (11.1) | 77 (10.7) | 23 (12.9) | 0.4238*§ |
| Smoking history, n (%) | ||||
| Current smoker | 308 (34.2) | 253 (35.0) | 55 (30.9) | 0.5549* |
| Former smoker | 412 (45.7) | 328 (45.4) | 84 (47.2) | |
| Never smoker | 181 (20.1) | 142 (19.6) | 39 (21.9) | |
| EGFR mutation, n (%) | ||||
| Yes | 116 (12.9) | 94 (13.0) | 22 (12.4) | 0.8963*§ |
| No | 641 (71.1) | 524 (72.5) | 117 (65.7) | |
| Unknown | 144 (16.0) | 105 (14.5) | 39 (21.9) | |
| EGFR mutation subtype n (%) | ||||
| TKI sensitive (L858R or Del19) | 94 (10.4) | 76 (10.5) | 18 (10.1) | 0.5183* |
| TKI non-sensitive | 16 (1.8) | 14 (1.9) | 2 (1.1) | |
| ALK mutation, n (%) | ||||
| Yes | 11 (1.2) | 7 (1.0) | 4 (2.2) | 0.1194*§ |
| No | 603 (66.9) | 496 (68.6) | 107 (60.1) | |
| Unknown | 287 (31.9) | 220 (30.4) | 67 (37.6) | – |
| Metastasis, n (%) | 698 (77.5) | 569 (78.7) | 129 (72.5) | 0.0883*§ |
| Metastasis location, n (%) | ||||
| Liver | 104 (11.5) | 82 (11.3) | 22 (12.4) | 0.6954* |
| Lung | 244 (27.1) | 195 (27.0) | 49 (27.5) | 0.9250* |
| Bone | 256 (28.4) | 213 (29.5) | 43 (24.2) | 0.1654* |
| Brain | 201 (22.3) | 178 (24.6) | 23 (12.9) | 0.0006* |
| Adrenal glands | 83 (9.2) | 74 (10.2) | 9 (5.1) | 0.0303* |
| Other | 309 (34.3) | 262 (36.2) | 47 (26.4) | 0.0136* |
| Concomitant disease, n (%) | ||||
| Any | 647 (71.8) | 505 (69.8) | 142 (79.8) | 0.0091* |
| COPD | 109 (12.1) | 81 (11.2) | 28 (15.7) | 0.1227* |
| Pulmonary infection | 22 (2.4) | 18 (2.5) | 4 (2.2) | 1.0000* |
| Interstitial lung disease | 47 (5.2) | 34 (4.7) | 13 (7.3) | 0.1861* |
| Autoimmune disease | 16 (1.8) | 14 (1.9) | 2 (1.1) | 0.7509* |
| Hypertension | 316 (35.1) | 231 (32.0) | 85 (47.8) | 0.0001* |
| Diabetes | 155 (17.2) | 116 (16.0) | 39 (21.9) | 0.0756* |
| Dyslipidaemia | 122 (13.5) | 100 (13.8) | 22 (12.4) | 0.7138* |
| Albumin (g/dL), median (range) | 3.7 (1.5–4.8) | 3.7 (1.5–4.8) | 3.6 (1.9–4.6) | 0.0300† |
*Fisher’s exact test.
†Wilcoxon rank-sum test.
‡0 vs 1 vs 2 vs (3 and 4).
§Yes/positive vs no/negative.
BMI, body mass index; COPD, chronic obstructive pulmonary disease; ECOG PS, Eastern Cooperative Oncology Group Performance Status; EGFR, epidermal growth factor receptor; NSCLC, non-small cell lung cancer.
Most baseline characteristics were comparable between the two age groups. However, the incidences of ECOG PS 3 and 4, squamous cell carcinoma and concomitant hypertension were numerically higher in patients aged ≥75 years. The incidences of brain metastasis and adrenal metastasis were significantly lower in patients aged ≥75 years compared with patients aged <75 years (brain, p=0.0006; adrenal glands, p=0.0303, table 1). Serum albumin levels were significantly lower in patients aged ≥75 years compared with those aged <75 years (p=0.0300).
Nivolumab use and treatment patterns
Most patients aged ≥75 years received nivolumab as second-line treatment (55.6%), followed by third-line treatment (21.3%). The use of nivolumab was similar for patients aged <75 years (table 2). The median number of nivolumab doses per patient was five (both for the whole population and for both age groups). The proportions of patients receiving post-nivolumab treatment were 44.4% and 34.3% in the <75 and ≥75 age groups, respectively (p=0.0180).
Table 2.
Treatment patterns of nivolumab by age group
| All patients (n=901) |
<75 years (n=723) |
≥75 years (n=178) |
Difference <75 years vs ≥75 years |
|
| Treatment line, n (%) | ||||
| Median (range) | 2.0 (1.0–12.0) | 3.0 (1.0–12.0) | 2.0 (1.0–9.0) | |
| 1 | 38 (4.2) | 33 (4.6) | 5 (2.8) | 0.0666*† |
| 2 | 422 (46.8) | 323 (44.7) | 99 (55.6) | |
| 3 | 239 (26.5) | 201 (27.8) | 38 (21.3) | |
| ≥4 | 202 (22.4) | 166 (23.0) | 36 (20.2) | |
| Number of doses, median (range) | 5.0 (1.0–44.0) | 5.0 (1.0–44.0) | 5.0 (1.0–43.0) | 0.5074† |
| Treatment duration, median (range) | 59.0 (1.0–693.0) | 59.0 (1.0–693.0) | 70.5 (1.0–602.0) | 0.4974† |
| Patients who continued nivolumab after the study, n (%) | 129 (14.3) | 101 (14.0) | 28 (15.7) | 0.5511* |
*Fisher’s exact test.
†1 vs 2 vs 3 vs ≥4.
Effectiveness of nivolumab according to age
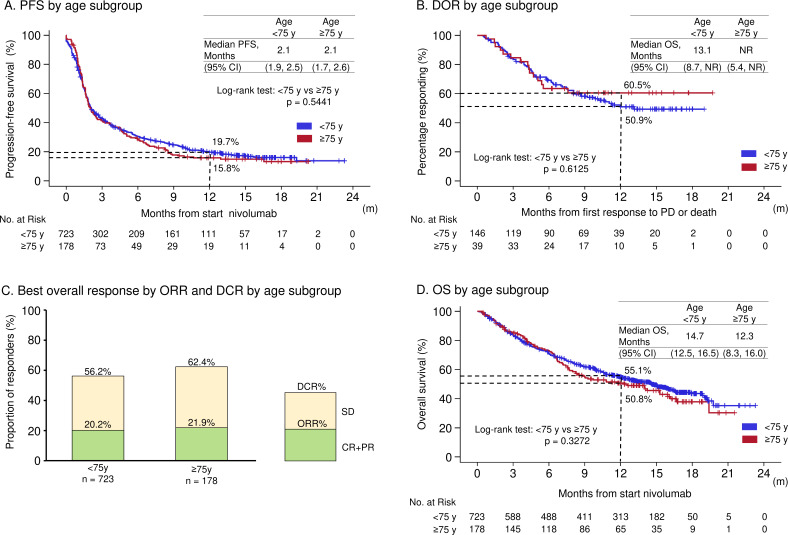
Comparable PFS was observed in patients aged <75 years and ≥75 years (median PFS, 2.1 months vs 2.1 months; p=0.5441). At 1 year, the PFS rate was 19.7% in patients aged <75 years and 15.8% in patients aged ≥75 years (figure 1A). There was no significant difference in DOR between patients aged <75 and those aged ≥75 years (figure 1B). The ORR and DCR were similar in the two age groups (figure 1C). Median OS in patients aged <75 years and those aged ≥75 years was 14.7 months and 12.3 months, respectively (p=0.3272, figure 1D).
Figure 1.
PFS (A), DOR (B), best overall response by ORR and DCR (C) and OS (D) by age subgroup. CR, complete response; DCR, disease control rate; DOR, duration of response; NR, not reached; ORR, objective response rate; OS, overall survival; PD, progressive disease; PFS, progression-free survival; PR, partial response; SD, stable disease; M, months.
In the supplementary effectiveness analysis, median PFS was 2.1 months in all three age groups evaluated (<75 years, 75 to <80 years and ≥80 years, online supplementary figure S1A). The median DOR was not reached in patients aged 75 to <80 years, and was 4.7 months in those aged ≥80 years, compared with 13.1 months in the <75 years group (online supplementary figure S1B). ORR and DCR were comparable between the three age groups (online supplementary figure S1C), as was median OS (online supplementary figure S1D). Significance testing was not performed for these analyses.
esmoopen-2019-000656supp001.pdf (183KB, pdf)
Effectiveness in patients aged ≥75 years according to ECOG PS
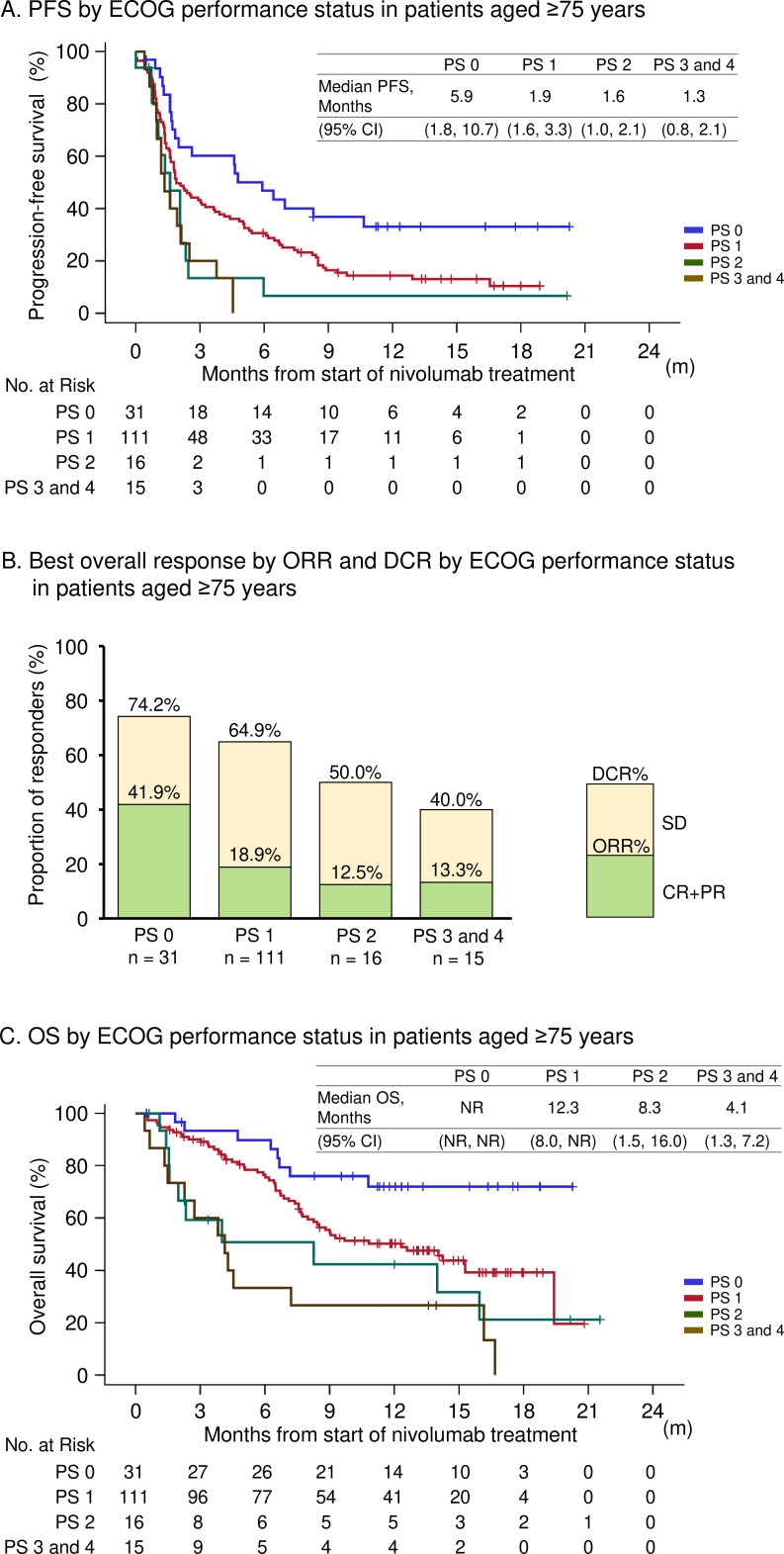
There was a clear trend towards improved PFS according to ECOG PS (figure 2A). Significant differences were observed between ECOG PS 0 and PS 1 (p=0.0170), PS 0 vs PS 2 (p=0.034), PS 0 vs PS 3 and 4 (p<0.0001) and PS 1 vs PS 3 or 4 (p=0.0092). ORR and DCR by ECOG PS are shown in figure 2B. More patients with ECOG PS 0 achieved CR or PR compared with other ECOG PS groups (41.9%). The ORR and DCR were highest in patients with ECOG PS 0 (41.9% and 74.2%, respectively), and lowest in patients with ECOG PS 3 and 4 (13.3% and 40.0%, respectively). There was also a trend towards improved OS according to ECOG PS (figure 2C).
Figure 2.
PFS (A), best overall response by ORR and DCR (B) and OS (C) by ECOG performance status in patients aged ≥75 years. DCR, disease control rate; ECOG, Eastern Cooperative Oncology Group; ORR objective response rate; OS, overall survival; PFS, progression-free survival; PS, performance status; M, months.
Effectiveness in patients aged ≥75 years according to serum albumin, C-reactive protein and BMI
When evaluated according to BMI, patients aged ≥75 years with a median BMI of 22.3 (21.5–23.6) kg/m2 were more likely to be responders (patients whose best overall response was CR or PR) compared with patients <75 years (p=0.040). The serum albumin levels of responders were significantly higher than non-responders in patients ≥75 years, while there were no significant difference in patients <75 years (online supplementary table S1). The median levels of CRP of responders were 0.65 and 1.20 (mg/dL) for patients aged ≥75 and <75 years, respectively. There were no significant difference between patients with responder and with non-responder in both age groups (online supplementary table S1).
esmoopen-2019-000656supp002.pdf (52.3KB, pdf)
Safety of nivolumab according to age
In general, the overall incidence of AEs in each age group was comparable (67.4% in patients aged <75 years and 64.0% in patients aged ≥75 years). Similarly, the incidences of grade ≥3 AEs were comparable between both age groups (29.2% in patients aged <75 years and 28.1% in those aged ≥75 years, table 3). The rates of nivolumab discontinuation due to AEs were 15.4% and 13.5% in patients aged <75 and ≥75 years, respectively. Regarding irAEs, the incidence rates were generally similar between age groups, with a trend towards a lower incidence as age increased (table 3). The time to onset of irAEs and the rate of recovery and improvement were similar in the groups aged <75 years and ≥75 years (online supplementary table S2). Most irAEs resolved or improved, with the exception of endocrine, nervous and renal reactions.
Table 3.
Summary of AEs and irAEs by age group
| All patients (n=901) |
<75 years (n=723) |
≥75 years (n=178) |
|
| AE reported, n (%) | 601 (66.7) | 487 (67.4) | 114 (64.0) |
| AE of grade 3 or 4, n (%) | 261 (29.0) | 211 (29.2) | 50 (28.1) |
| Discontinuation due to AE, n (%) | 135 (15.0) | 111 (15.4) | 24 (13.5) |
| irAE reported, n (%) | 413 (45.8) | 335 (46.3) | 78 (43.8) |
| irAE category, n (%) | |||
| Endocrine disorders | 76 (8.4) | 66 (9.1) | 10 (5.6) |
| Skin toxicity | 151 (16.8) | 114 (15.8) | 37 (20.8) |
| Pulmonary toxicity | 94 (10.4) | 82 (11.3) | 12 (6.7) |
| Liver toxicity | 46 (5.1) | 36 (5.0) | 10 (5.6) |
| Gastrointestinal toxicity | 98 (10.9) | 81 (11.2) | 17 (9.6) |
| Nervous system disorders | 22 (2.4) | 21 (2.9) | 1 (0.6) |
| Renal toxicity | 20 (2.2) | 17 (2.4) | 3 (1.7) |
AEs, adverse events; irAEs, immune-related adverse events.
The most frequently reported AEs of any grade in patients aged <75 years were interstitial lung disease (10.0%), diarrhoea (9.7%), thyroid dysfunction (6.6%) and hepatic dysfunction (5.8%). In patients aged ≥75 years, the most frequently reported AEs were diarrhoea (6.7%), hepatic and thyroid dysfunction (5.1% each) and interstitial lung disease (4.5%). In both age groups, the most common grade 3–4 AEs were interstitial lung disease (4.0% in patients aged <75 years and 2.8% in those aged ≥75 years, online supplementary table S3).
AEs including irAEs were evaluated from the start of nivolumab administration initiation up to the last administration. If there was no subsequent treatment, AEs were included up to 100 days from the last administration of nivolumab.
Discussion
Although Japanese treatment guidelines indicate that treatment for NSCLC may need to be varied according to age,17 there are limited efficacy and safety data available for newly approved treatments, such as nivolumab, in Japanese patients aged ≥75 years. In the absence of prospective clinical trial data, retrospective real-world cohort studies can fill this evidence gap and may inform clinical treatment decisions. This subanalysis of the Nivolumab Japan Real World (CA209-9CR) study,19 evaluated data collected from 901 Japanese patients with NSCLC who received nivolumab, with the aim of investigating the safety and effectiveness outcomes according to age.
When study patients were categorised according to age (<75 and ≥75 years), there were few significant baseline differences between groups, with the exception of higher incidences of ECOG PS 3 and 4, squamous cell carcinoma and concomitant hypertension in patients aged ≥75 years vs <75 years. The overall incidence of concomitant disease in our study was significantly higher in patients aged ≥75 years (79.8%) compared with patients aged <75 years (69.8%; p<0.05). Treatment patterns of nivolumab and administration of subsequent treatment after nivolumab were similar in the two age groups.
It has long been recognised that patients with NSCLC aged ≥80 years, when carefully selected according to clinical factors and medical history, can not only tolerate chemotherapy but also benefit from it.22 However, it is important to obtain real-world efficacy and safety data from patients with NSCLC aged ≥80 years receiving immunotherapies, since data from elderly patients treated with immunotherapies have been relatively scarce in the clinical trial publications to date. The results of our study are in line with those reported from the Italian cohort of an expanded access programme in patients with squamous NSCLC receiving nivolumab,13 in which the median OS was lower in patients aged ≥75 years (5.8 months) compared with patients aged <65 years (8.6 months), but PFS, ORR and DCR rates were similar for all age groups. The Italian EAP (expanded access programme) real-life experiences with nivolumab also focuses on elderly patients,12 23 the ORR was similar among patients aged <65, 65–<75 and ≥75 years (18%, 18% and 19%, respectively) with a similar safety profile for each age group. However, the median OS was shorter in patients aged ≥75 years (8.6 months, 8.0 months and 5.8 months, respectively).12 In non-squamous cells, the ORR and OS were comparable between patients aged ≥75 years and the overall population (ORR: 25% and 18%; Median OS: 12.0 and 11.3 months), with similar safety profiles.23 Considering that non-squamous cells were accounted for in the main population in patients aged ≥75 years in this study, the results of the Italian EAP real-life experiences were similar to the results of this study. Other real-world studies in patients of different ethnicities have also shown the value of nivolumab in treating elderly patients with NSCLC. In an Israeli study of nivolumab in advanced NSCLC,24 the median OS and PFS for the whole population were 5.9 and 2.8 months, and there was no significant difference in OS between patients older than 75 years and those younger than 75 years. In a French study of patients aged ≥70 years with NSCLC treated with nivolumab (median age 75.2 years), the median OS and PFS were 7.1 and 3.3 months, respectively.25 Taken together, our data, and those of other real-world studies indicate that there are no significant differences in the effectiveness of nivolumab between patients aged <75 and ≥75 years, and that nivolumab treatment should be considered in all appropriate patients with NSCLC, regardless of age.
In general, the safety profile of nivolumab was favourable and no new safety concerns were observed in either age group. This is consistent with the data in the literature and the safety data of the 2-year outcomes of CheckMate 017 and CheckMate 057.26 Most of the irAEs observed were similar to those previously reported; the majority recovered or improved, regardless of patient age, and were manageable. Of note, the most frequent grade ≥3 AE was interstitial lung disease in both age groups, which indicates that interstitial lung disease must be cautiously monitored in NSCLC treatment with nivolumab. This result is similar to that reported in a real-world data study of elderly patients with NSCLC treated with nivolumab in which the frequency of irAEs was similar in both older and younger patients.25
As might be expected, in the subgroup analysis of effectiveness, response to nivolumab treatment among patients aged ≥75 years was associated with ECOG PS; these results are in line with those previously reported for the overall population.18 This finding suggests that nivolumab treatment should be based on patient ECOG PS and not age. A previous publication has suggested that PS 2 and symptomatic brain metastases are factors associated with poor response to nivolumab.27 In addition, real-life data from patients with NSCLC treated with nivolumab in Israel,24 and clinical trial data from the Checkmate 153 study,28 have both reported that PS≥2 was associated with poor prognosis.
Serum albumin is a well-known indicator of nutritional status among patients with cancer.29–31 Poor nutrition in patients with cancer can lead to poor quality of life and activities of daily living. Moreover, a low serum albumin level was found to be an independent poor prognostic factor in patients with advanced NSCLC, and it was associated with reduced response rates and reduced survival time.32 In our study, although serum albumin levels were significantly lower in patients aged ≥75 years (p=0.0300), there was no correlation between serum albumin and nivolumab effectiveness in elderly patients, suggesting that nivolumab activity may not be affected by serum albumin levels in elderly patients.
In this study, BMI was correlated with response to nivolumab treatment in patients aged ≥75 years, but BMI and response were not correlated in patients aged <75 years. Patients aged ≥75 years with a median BMI of 22.3 kg/m2 and a range from normal (21.5 kg/m2) to overweight (23.6 kg/m2) according to the Japanese guidelines,33 were more likely to respond (ie, achieve a best overall response of CR or PR) to nivolumab treatment compared with younger patients in the present study. This finding is consistent with the results of recent studies showing that patients with cancer and with low BMI have poor treatment outcomes compared with patients with high BMI.34 Specifically, in patients with metastatic NSCLC treated with nivolumab and pembrolizumab, low BMI was associated with shorter OS and high BMI, with longer OS.35 Another retrospective study on patients with NSCLC, melanoma, renal cell carcinoma and other cancers who were being treated with pembrolizumab, nivolumab or atezolizumab reported that in univariate and multivariate analyses, the median OS and PFS were significantly longer in overweight/obese patients.36
We acknowledge that the present study has several limitations which must be considered when evaluating the data. These include the retrospective design and the fact that a review of medical records is subject to data variability from site to site or incompleteness of the clinical data recorded. Similarly, the retrospective design limits the collection of safety data, and it may be more difficult to determine which AEs may have been linked to study treatment. Finally, differences in PD-L1 expression or presence/type of epidermal growth factor receptor mutations may influence treatment efficacy.
Conclusions
Based on Japanese real-world data, the safety and effectiveness of nivolumab were confirmed regardless of age (<75 or ≥75 years). PS was a factor influencing outcomes in patients aged ≥75 years, with worse PS associated with worsening outcomes. Effectiveness in patients aged ≥80 years was similar to that in patients aged <75 years. No new safety concerns were observed in either age group.
Role of the funding source
This study (CA209-9CR) was company-initiated and funded by ONO Pharmaceutical Co, Ltd and Bristol-Myers Squibb K.K. The companies were involved in the study design and interpretation of the data; however, they did not participate in data collection and data analysis. The two authors of this article who were affiliated with the companies participated in writing the manuscript and decision for its publication.
Acknowledgments
The authors wish to thank Keyra Martinez Dunn, MD (Edanz Medical Writing), for providing medical writing support, which was funded by ONO Pharmaceutical Co, Ltd and Bristol-Myers Squibb K.K. and Hidehito Horinouchi (National Cancer Center, Tokyo, Japan) for advice on the conduct of the study. The authors also thank Mebix for conducting the research operation, construction of the electronic data capture, data management and statistical analysis in their role as the contract research organisation.
Footnotes
Contributors: HH and NY contributed to the conception, design and writing the protocol. KO, RM, JS, HS, HS, YK, OH, MY, MN, KA, OK, TK, KK, HT, SO, DF, HT, KM, TM, TK, TH, HS, IO and YO have contributed to the data collection. HH, NY and KO contributed to data interpretation and preparation of the manuscript. All authors critically reviewed and approved the final manuscript.
Funding: This study (CA209-9CR) was company initiated and funded by ONO Pharmaceutical Co, Ltd and Bristol-Myers Squibb K.K. The companies were involved in the study design and interpretation of the data; however, they did not participate in data collection and data analysis. The two authors of this article who were affiliated with the companies participated in writing the manuscript and decision for its publication.
Competing interests: KO reports personal fees from Ono Pharmaceutical Co, Ltd and MSD K.K. outside the submitted work; JS reports personal fees from Bristol-Myers Squibb K.K. and Ono Pharmaceutical CO, Ltd outside the submitted work; HS reports grants from Chugai Pharmaceutical Co, Ltd, AstraZeneca K.K. and MSD K.K. and personal fees from Ono Pharmaceutical Co, Ltd, Nippon Boehringer Ingelheim Co, Ltd and Novartis Pharma K.K. outside the submitted work; HS reports personal fees from Ono Pharmaceutical Co, Ltd and Bristol-Myers Squibb K.K. during the conduct of the study, personal fees from Chugai Pharmaceutical Co, Ltd and MSD K.K. outside the submitted work; OS reports other from Ono Pharmaceutical Co, Ltd during the conduct of the study, personal fees and other from Novartis Pharma K.K., Nippon Boehringer Ingelheim Co, Ltd and AstraZeneca K.K. and other from Kyorin Pharmaceutical Co, Ltd, Bayer Health, Daiichi Sankyo Co, Ltd, GlaxoSmithKline K.K. and Ono Pharmaceutical Co, Ltd outside the submitted work; MY reports personal fees from Chugai Pharmaceutical Co, Ltd, Ono Pharmaceutical Co, Ltd and AstraZeneca K.K. outside the submitted work; MN reports grants and non-financial support from Ono Pharmaceutical Co, Ltd during the conduct of the study, grants and personal fees from Ono Pharmaceutical Co, Ltd, Bristol-Myers Squibb K.K., Pfizer Japan Inc, Chugai Pharmaceutical Co, Ltd, Eli Lilly Japan K.K., Taiho Pharmaceutical Co, Ltd, AstraZeneca K.K., MSD K.K., Novartis Pharma K.K., Takeda Pharmaceutical Co, Ltd and Daiichi Sankyo Healthcare Co, Ltd and grants from Merck Serono Co, Ltd (currently Merck Biopharma Co, Ltd) and personal fees from Nippon Boehringer Ingelheim Co, Ltd outside the submitted work; KA reports grants and personal fees from Ono Pharmaceutical Co, Ltd, Bristol-Myers Squibb K.K., AstraZeneca K.K. and Eli Lilly Japan K.K. and grants from MSD K.K. and Novartis Pharma K.K. outside the submitted work; TK reports grants and personal fees from Ono Pharmaceutical Co, Ltd, AstraZeneca K.K., Taiho Pharmaceutical Co, Ltd, MSD K.K., Novartis Pharma K.K., Nippon Boehringer Ingelheim Co, Ltd, Eli Lilly Japan K.K., Pfizer Japan Inc and Chugai Pharmaceutical Co, Ltd, and grants from Takeda Pharmaceutical Co, Ltd, Regeneron Pharmaceuticals, Inc and Merck Serono Co, Ltd (currently Merck Biopharma Co, Ltd) and personal fees from Teijin Pharma Ltd and Bristol-Myers Squibb K.K. outside the submitted work; SO reports grants and personal fees from Bristol-Myers Squibb K.K. and Ono Pharmaceutical Co, Ltd during the conduct of the study, grants and personal fees from AstraZeneca K.K., Chugai Pharmaceutical Co, Ltd and Taiho Pharmaceutical Co, Ltd and grants from Kyowa Hakko Kirin Co, Ltd (currently Kyowa Kirin Co, Ltd) and Merck Serono Co, Ltd (currently Merck Biopharma Co, Ltd) and personal fees from MSD K.K. and Eli Lilly Japan K.K. outside the submitted work; DF reports personal fees from Ono Pharmaceutical Co, Ltd and Bristol-Myers Squibb K.K. during the conduct of the study, personal fees from AstraZeneca K.K., Taiho Pharmaceutical Co, Ltd, Chugai Pharmaceutical Co, Ltd, MSD K.K., Nippon Boehringer Ingelheim Co, Ltd and Eli Lilly Japan K.K. outside the submitted work; HT reports grants and personal fees from Bristol-Myers Squibb K.K., Eli Lilly Japan K.K., MSD K.K., Taiho Pharmaceutical Co, Ltd, Pfizer Japan Inc, Chugai Pharmaceutical Co, Ltd, Ono Pharmaceutical Co, Ltd, AstraZeneca K.K. and Nippon Boehringer Ingelheim Co, Ltd and grants from Merck Serono Co, Ltd (currently Merck Biopharma Co, Ltd) and personal fees from Novartis Pharma K.K. outside the submitted work; TK reports grants and personal fees from Chugai Pharmaceutical Co, Ltd, AstraZeneca K.K., Eli Lilly Japan K.K. and Bristol-Myers Squibb K.K., and personal fees from Taiho Pharmaceutical Co, Ltd, Ono Pharmaceutical Co, Ltd, MSD K.K., Pfizer Japan Inc, Kyowa Hakko Kirin Co, Ltd (currently Kyowa Kirin Co, Ltd), Nippon Boehringer Ingelheim Co, Ltd, and Nippon Kayaku Co, Ltd and grants from Merck Serono Co, Ltd (currently Merck Biopharma Co, Ltd) outside the submitted work; HS reports other from Mebix, Inc during the conduct of the study, personal fees from AstraZeneca K.K. outside the submitted work; IS reports grants from Nippon Boehringer Ingelheim Co, Ltd during the conduct of the study, grants and personal fees from AstraZeneca K.K., Taiho Pharmaceutical Co, Ltd, Nippon Boehringer Ingelheim Co, Ltd, Ono Pharmaceutical Co, Ltd, MSD K.K, Eli Lilly Japan K.K., Bristol-Myers Squibb K.K. and Chugai Pharmaceutical Co, Ltd and grants from Astellas Pharma Inc, Novartis Pharma K.K. and AbbVie GK, and personal fees from Pfizer Japan Inc outside the submitted work; YO reports grants and personal fees from Ono Pharmaceutical Co, Ltd and Bristol-Myers Squibb K.K. during the conduct of the study, grants and personal fees from AstraZeneca K.K., Chugai Pharmaceutical Co, Ltd, Eli Lilly Japan K.K., Pfizer Japan Inc, MSD K.K., Kyorin Pharmaceutical Co, Ltd, Takeda Pharmaceutical Co, Ltd, Novartis Pharma K.K., Taiho Pharmaceutical Co, Ltd, and AbbVie GK, and personal fees from Celltrion Healthcare Co, Ltd, Amgen Inc, and Nippon Boehringer Ingelheim Co, Ltd, and grants from Kissei Pharmaceutical Co, Ltd, Loxo Oncology, Inc, and Janssen Pharmaceutical K.K. outside the submitted work; HH is an employee of Bristol-Myers Squibb K.K.; NY is an employee of Ono Pharmaceutical Co, Ltd; RM, YHK, OS, KK, HT, KM, TM and TH have nothing to declare.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: No data are available.
References
- 1.Bray F, Ferlay J, Soerjomataram I, et al. . Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018;68:394–424. 10.3322/caac.21492 [DOI] [PubMed] [Google Scholar]
- 2.Cancer statistics in Japan, 2017. Available: https://ganjohojp/data/reg_stat/statistics/brochure/2017/cancer_statistics_2017_fig_Epdf [Accessed 25 Sep 2019].
- 3.Sher T, Dy GK, Adjei AA. Small cell lung cancer. Mayo Clin Proc 2008;83:355–67. 10.4065/83.3.355 [DOI] [PubMed] [Google Scholar]
- 4.Zappa C, Mousa SA. Non-Small cell lung cancer: current treatment and future advances. Transl Lung Cancer Res 2016;5:288–300. 10.21037/tlcr.2016.06.07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Planchard D, Popat S, Kerr K, et al. . Metastatic non-small cell lung cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 2018;29:iv192–237. 10.1093/annonc/mdy275 [DOI] [PubMed] [Google Scholar]
- 6.Brahmer J, Reckamp KL, Baas P, et al. . Nivolumab versus docetaxel in advanced squamous-cell non-small-cell lung cancer. N Engl J Med 2015;373:123–35. 10.1056/NEJMoa1504627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Borghaei H, Paz-Ares L, Horn L, et al. . Nivolumab versus docetaxel in advanced Nonsquamous non-small-cell lung cancer. N Engl J Med 2015;373:1627–39. 10.1056/NEJMoa1507643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hida T, Nishio M, Nogami N, et al. . Efficacy and safety of nivolumab in Japanese patients with advanced or recurrent squamous non-small cell lung cancer. Cancer Sci 2017;108:1000–6. 10.1111/cas.13225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nishio M, Hida T, Atagi S, et al. . Multicentre phase II study of nivolumab in Japanese patients with advanced or recurrent non-squamous non-small cell lung cancer. ESMO Open 2016;1:e000108. 10.1136/esmoopen-2016-000108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ferguson MK, Skosey C, Hoffman PC, et al. . Sex-associated differences in presentation and survival in patients with lung cancer. J Clin Oncol 1990;8:1402–7. 10.1200/JCO.1990.8.8.1402 [DOI] [PubMed] [Google Scholar]
- 11.Key statistics for lung cancer. Available: https://wwwcancerorg/cancer/non-small-cell-lung-cancer/about/key-statisticshtml [Accessed 25 Sep 2019].
- 12.Grossi F, Crinò L, Logroscino A, et al. . Use of nivolumab in elderly patients with advanced squamous non-small-cell lung cancer: results from the Italian cohort of an expanded access programme. Eur J Cancer 2018;100:126–34. 10.1016/j.ejca.2018.05.015 [DOI] [PubMed] [Google Scholar]
- 13.Makrantonakis PD, Galani E, Harper PG. Non-Small cell lung cancer in the elderly. Oncologist 2004;9:556–60. 10.1634/theoncologist.9-5-556 [DOI] [PubMed] [Google Scholar]
- 14.Tas F, Ciftci R, Kilic L, et al. . Age is a prognostic factor affecting survival in lung cancer patients. Oncol Lett 2013;6:1507–13. 10.3892/ol.2013.1566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barnett K, Mercer SW, Norbury M, et al. . Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet 2012;380:37–43. 10.1016/S0140-6736(12)60240-2 [DOI] [PubMed] [Google Scholar]
- 16.Sawhney R, Sehl M, Naeim A. Physiologic aspects of aging: impact on cancer management and decision making, part I. Cancer J 2005;11:449–60. 10.1097/00130404-200511000-00004 [DOI] [PubMed] [Google Scholar]
- 17.Akamatsu H, Ninomiya K, Kenmotsu H, et al. . The Japanese lung cancer Society guideline for non-small cell lung cancer, stage IV. Int J Clin Oncol 2019;24:731–70. 10.1007/s10147-019-01431-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Salloum RG, Smith TJ, Jensen GA, et al. . Survival among non-small cell lung cancer patients with poor performance status after first line chemotherapy. Lung Cancer 2012;77:545–9. 10.1016/j.lungcan.2012.04.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Morita R, Okishio K, Shimizu J, et al. . Real-World effectiveness and safety of nivolumab in patients with non-small cell lung cancer: a multicenter retrospective observational study in Japan. Lung Cancer 2020;140:8–18. 10.1016/j.lungcan.2019.11.014 [DOI] [PubMed] [Google Scholar]
- 20.Japan Ministry of Labor, Health and Welfare Ethical guidelines for medical and health research involving human subjects. Available: https://www.mhlw.go.jp/file/06-Seisakujouhou-10600000-Daijinkanboukouseikagakuka/0000153339.pdf [Accessed 25 Sep 2019].
- 21.National Institutes of Health National Cancer Institute Common terminology criteria for adverse events (CTCAE) version 4.0. Available: http://wwwhrcgovtnz/sites/default/files/CTCAE%20manual%20-%20DMCCpdf [Accessed 25 Sep 2019].
- 22.Altundag O, Stewart DJ, Fossella FV, et al. . Many patients 80 years and older with advanced non-small cell lung cancer (NSCLC) can tolerate chemotherapy. J Thorac Oncol 2007;2:141–6. 10.1097/JTO.0b013e3180311792 [DOI] [PubMed] [Google Scholar]
- 23.Grossi F, Genova C, Crinò L, et al. . Real-Life results from the overall population and key subgroups within the Italian cohort of nivolumab expanded access program in non-squamous non-small cell lung cancer. Eur J Cancer 2019;123:72–80. 10.1016/j.ejca.2019.09.011 [DOI] [PubMed] [Google Scholar]
- 24.Dudnik E, Moskovitz M, Daher S, et al. . Effectiveness and safety of nivolumab in advanced non-small cell lung cancer: the real-life data. Lung Cancer 2018;126:217–23. 10.1016/j.lungcan.2017.11.015 [DOI] [PubMed] [Google Scholar]
- 25.Sabatier R, Nicolas E, Paciencia M, et al. . Nivolumab in routine practice for older patients with advanced or metastatic non-small cell lung cancer. J Geriatr Oncol 2018;9:494–500. 10.1016/j.jgo.2018.02.011 [DOI] [PubMed] [Google Scholar]
- 26.Horn L, Spigel DR, Vokes EE, et al. . Nivolumab versus docetaxel in previously treated patients with advanced non-small-cell lung cancer: two-year outcomes from two randomized, open-label, phase III trials (CheckMate 017 and CheckMate 057). J Clin Oncol 2017;35:3924–33. 10.1200/JCO.2017.74.3062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dumenil C, Massiani M-A, Dumoulin J, et al. . Clinical factors associated with early progression and grade 3-4 toxicity in patients with advanced non-small-cell lung cancers treated with nivolumab. PLoS One 2018;13:e0195945. 10.1371/journal.pone.0195945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Spigel DR, McCleod M, Jotte RM, et al. . Safety, Efficacy, and Patient-Reported Health-Related Quality of Life and Symptom Burden with Nivolumab in Patients with Advanced Non-Small Cell Lung Cancer, Including Patients Aged 70 Years or Older or with Poor Performance Status (CheckMate 153). J Thorac Oncol 2019;14:1628–39. 10.1016/j.jtho.2019.05.010 [DOI] [PubMed] [Google Scholar]
- 29.Gupta D, Lis CG. Pretreatment serum albumin as a predictor of cancer survival: a systematic review of the epidemiological literature. Nutr J 2010;9:69. 10.1186/1475-2891-9-69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kanda M, Fujii T, Kodera Y, et al. . Nutritional predictors of postoperative outcome in pancreatic cancer. Br J Surg 2011;98:268–74. 10.1002/bjs.7305 [DOI] [PubMed] [Google Scholar]
- 31.Mori S, Usami N, Fukumoto K, et al. . The significance of the prognostic nutritional index in patients with completely resected non-small cell lung cancer. PLoS One 2015;10:e0136897. 10.1371/journal.pone.0136897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tanriverdi O, Avci N, Oktay E, et al. . Pretreatment serum albumin level is an independent prognostic factor in patients with stage IIIB non-small cell lung cancer: a study of the Turkish descriptive oncological researches group. Asian Pac J Cancer Prev 2015;16:5971–6. 10.7314/APJCP.2015.16.14.5971 [DOI] [PubMed] [Google Scholar]
- 33.Japan Society for the study of obesity (JASSO), guidelines for diagnosis and treatment in obesity and its comorbidities. Available: http://wwwjassoorjp/contents/english/indexhtml [Accessed 25 Sep 2019].
- 34.Strulov Shachar S, Williams GR. The obesity paradox in Cancer-Moving beyond BMI. Cancer Epidemiol Biomarkers Prev 2017;26:13–16. 10.1158/1055-9965.EPI-16-0439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhi J, Khozin S, Kuk D, et al. . Association of baseline body mass index (BMI) with overall survival (OS) in patients (PTS) with metastatic non-small cell lung cancer (mNSCLC) treated with nivolumab (N) and pembrolizumab (P). JCO 2018;36:6553–53. 10.1200/JCO.2018.36.15_suppl.6553 [DOI] [Google Scholar]
- 36.Cortellini A, Bersanelli M, Buti S, et al. . A multicenter study of body mass index in cancer patients treated with anti-PD-1/PD-L1 immune checkpoint inhibitors: when overweight becomes favorable. J Immunother Cancer 2019;7:57. 10.1186/s40425-019-0527-y [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
esmoopen-2019-000656supp001.pdf (183KB, pdf)
esmoopen-2019-000656supp002.pdf (52.3KB, pdf)