Abstract
Overdoses of prescription or illicit opioids claimed the lives of 91 Americans each day in 2015, and the crisis continues to escalate. As healthcare systems evolve to address the crisis, the potential of pharmacists to make a positive difference is significant. In addition to utilizing available prescription drug monitoring programs to help prevent diversion of opioids, practicing pharmacists can be alert for signs of opioid misuse by patients (e.g., multiple prescriptions from different physicians) as well as inappropriate prescribing or hazardous drug combinations that physicians may not be aware of (e.g., opioid analgesics combined with benzodiazepines). They can also supply patients with information on risks of opioids, proper storage and disposal of medications, and the harms (and illegality) of sharing medications with other people. Increasingly, pharmacies are sites of distribution of the opioid antagonist naloxone, which has been shown to save lives when made available to opioid users and their families or other potential bystanders to an overdose; and pharmacists can provide guidance about its use and even legal protections for bystanders to an overdose that customers may not be aware of. Pharmacists can also recommend addiction treatment to patients and be a resource for information on addiction treatment options in the community. As addiction treatment becomes more integrated with general healthcare, pharmacies are also increasingly dispensing medications like buprenorphine and, in the future, possibly methadone. Pharmacists in private research labs and at universities are helping to develop the next generation of addiction treatments and safer, non-addictive pain medications; they can also play a role in implementation research to enhance the delivery of addiction interventions and medications in pharmacy settings. Meanwhile, pharmacists in educational settings can promote improved education about the neurobiology and management of pain and its links to opioid misuse and addiction.
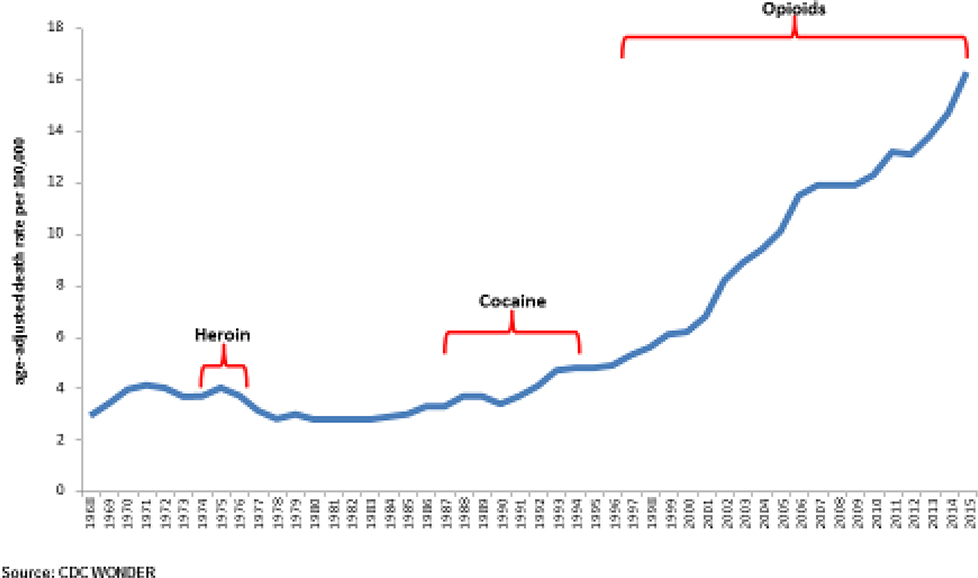
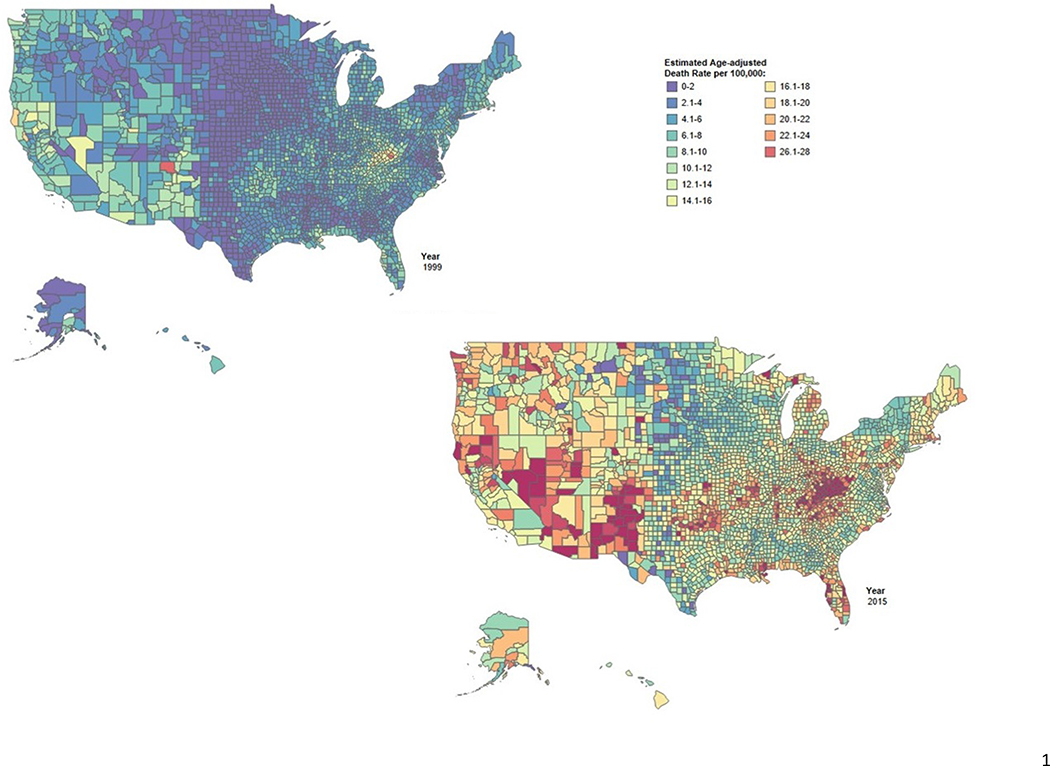
The United States is in the midst of the most devastating drug overdose epidemic it has ever experienced with much higher overdose deaths in the current opioid crisis than in prior epidemics (Figure 1). Increasing overdose deaths have impacted nearly all parts of the U.S., with some regions, such as Appalachia, the rural southwest and the northeast particularly hard hit (Figure 2). Overdoses of prescription or illicit opioids claimed the lives of 91 Americans each day in 2015, and preliminary estimates indicate these numbers have substantially increased in 2016.1–2 As we consider ways that healthcare, researchers, and communities can contribute to preventing opioid misuse, treating opioid addiction, and preventing and reversing overdose deaths, the potential of pharmacists to make a positive difference is significant, yet thus far it has been little discussed and insufficiently studied.3
Figure 1:
Age-adjusted death rates for drug poisonings (“overdoses”) in the U.S. 2000 TO 2015 (Source: CDC WONDER System)
Figure 2:
Estimated Age-adjusted Death Rats for Drug Poisoning (“overdose”) by U.S. County in 1999 and 2015 (Source: http://www.cdc.gov/nchs/data-visualization/drug-poisoning-mortality/)
Practicing pharmacists serve as a major bulwark against diversion and can protect the health and safety of their patients and community in several ways that go beyond obvious measures like using prescription drug monitoring programs (PDMPs) before filling prescriptions or dispensing the opioid-overdose-reversal drug naloxone. They can be alert for inappropriate prescribing and hazardous drug combinations such as opioid analgesics combined with benzodiazepines and may also be alert for signs of opioid misuse, supplying patients with information on risks and addiction treatment options. Pharmacists in private research labs and at universities increasingly have a role in helping to develop the next generation of addiction treatments and safer, non-addictive pain medications. And pharmacists in educational settings can promote improved education about the neurobiology and management of pain and its complex links to opioid misuse and addiction, advancing interprofessional training and collaboration to strengthen prevention, treatment, and recovery support services across the health system.
This article provides an overview of the current opioid crisis in the U.S. and highlights several ways pharmacists can contribute to mitigate its impact.
A Moving Target
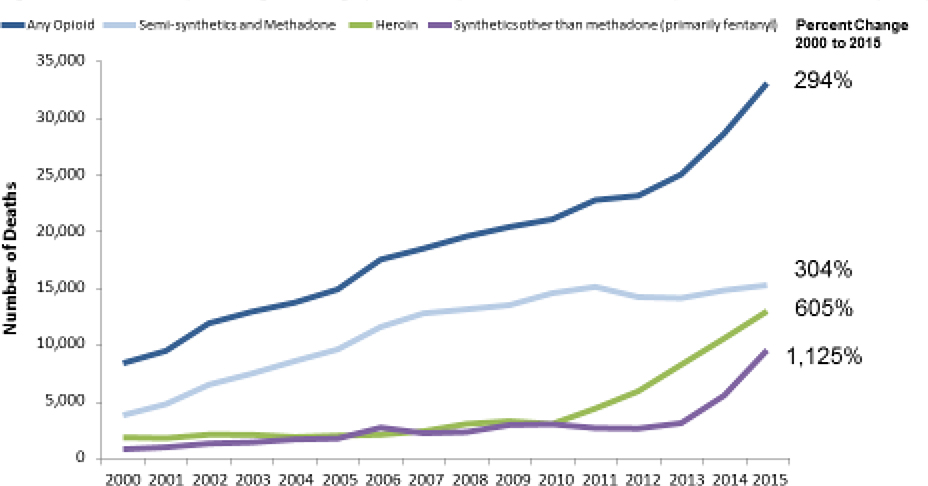
The opioid crisis is evolving year to year, even month to month (Figures 1–3). Overprescribing of opioid analgesics started it: In the mid-1990s, growing concerns that pain was being undertreated, coupled with promises from manufacturers that a new generation of opioids, in particular extended-release products, posed fewer addiction risks, led to increased prescribing of opioids for acute and chronic pain. Those promises proved false, and the flood of pain pills into communities across the U.S. led to widespread diversion and misuse of these medications.4 By 2010, over 250 million opioid prescriptions per year were being dispensed in the U. S.5
Figure 3:
Number of Opioid Drug Poisonings (“overdose”) in the U.S. 2000 to 2015 (Source: CDC WONDER System)
These fundamental changes in prescribing fueled increases in opioid addiction and overdose deaths, seen in the rising number of deaths attributed to prescription-type opioids (Figure 2). And as individuals progressed in their opioid addiction, the growing availability of low cost, high purity heroin contributed to rising numbers of people who were misusing prescription opioids that initiated heroin use.6–7 Overdose deaths from heroin escalated sharply after 2010 and deaths from illicit fentanyl have recently skyrocketed (Figure 3). In 2015 there were 33,091 overdose deaths from prescription or illicit opioids. That same year the National Survey on Drug Use and Health (NSDUH) reported that 2 million people in the United States suffered from a prescription opioid use disorder, and 591,000 people had a heroin use disorder (those are not mutually exclusive).8 There is also reason to believe that the official numbers significantly underestimate the full number of overdoses and opioid use disorders both because of incomplete drug class coding on death certificates and sampling gaps in the NSDUH and other household surveys.9–11
Apart from the risk of overdose, opioid use disorder leads to other health risks and complications. Misuse of illicit as well as prescription opioids via injection contributes to the spread of hepatitis C and HIV12–13, such as the outbreak in southern Indiana in 2015—181 new HIV cases in 12 months.14 Prenatal exposure to opioids is leading to continued increases in admissions for opioid withdrawal syndromes in newborns; Neonatal Intensive Care Unit (NICU) admissions for neonatal abstinence syndrome increased nearly four-fold from 2004 to 2013.15
As awareness of the problem has grown, federal agencies have taken measures to curb prescribing of opioid-based medications. In March 2016, for example, the Centers for Disease Control and Prevention (CDC) published a Guideline for Prescribing Opioids for Chronic Pain to provide recommendations for the prescribing of opioid pain medication (outside the context of cancer or end-of-life care) for patients 18 and older in primary care settings.16 The guideline recommends that non-steroidal anti-inflammatory drugs (NSAIDS) as well as non-drug approaches like exercise and cognitive behavioral therapy should be considered first, and that when opioids are prescribed, the lowest effective dose should be used and their use closely monitored. In addition, acute prescribing, such as that following surgery or injury, was recommended to be of brief duration, to minimize unused medications.
Thanks to increased awareness and caution by providers, we are now seeing modest declines in opioid prescribing5, and overdose deaths from prescription analgesics have plateaued since 2010.1 But an estimated 4 percent of people who misuse prescription opioids shift to heroin within 5 years of initiating prescription opioid misuse.16–17 Consequently, since 2010, we have seen steep increases in heroin use, use disorders and deaths (Figure 3). Of particular concern since 2013, we have witnessed a sharp increase in deaths related to the emergence of illicitly made fentanyl and other highly potent synthetic opioids.1 Although some users are seeking out fentanyl, it is often used to lace heroin or counterfeit prescription drugs sold on the street and thus many users of heroin and other drugs are sometimes exposed unintentionally.18
The dangers of opioids are compounded by other substances that may be co-ingested or that may be in a user’s system. This includes not only alcohol but also other respiratory depressants such as prescription sedatives—particularly benzodiazepines. The rate of nonmedical-use–related emergency department visits involving prescription opioids and benzodiazepines tripled between 2004 and 2011, and the benzodiazepine involvement in fatal overdoses involving opioid analgesics during this time period nearly doubled from 18 percent to 31 percent.19 People who misuse opioids may engage in other forms of poly-drug use, sometimes combining opioids with cocaine, for example. It is also possible that the substances used to dilute heroin or fentanyl may not be inert and thus may have their own side-effects and complications or interactions with opioids.20
At the National Rx Drug Abuse and Heroin Summit in Atlanta, GA, in April 2017, the U.S. Department of Health and Human Services (HHS) released its Opioid Strategy encompassing five priority areas: 1) Improving access to prevention, treatment and recovery services; 2) Targeting the availability and distribution of overdose-reversing drugs; 3) Strengthening timely public health data and reporting; 4) Support cutting edge research on pain and addiction; and 5) Advancing the practice of pain management. 21 Pharmacists can play a role in all these areas through practice, research, education, and collaboration.
Potential for Practice
When dispensing prescriptions for the vast majority of medications, practicing pharmacists need mainly consider the person across the counter. But opioids are different; they are so commonly diverted from the person for whom they’re prescribed that the pharmacist (as well as the prescriber) must also be thinking about the risks to the broader community.22
Nearly all states have passed laws requiring adopting PDMPs, and most have implemented these laws in some fashion. States differ in whether clinicians are required to check the PDMP before prescribing, whether PDMPs proactively report suspicious prescribing patterns to law enforcement, licensing boards, prescribers or pharmacists, whether prescribers and pharmacists are required to register, and whether the PDMP is integrated with electronic health records.23 But in whatever form they exist, they can be an important tool at the pharmacist’s disposal. Practicing pharmacists should check their PDMP before dispensing opioids, and in cases where a patient is receiving multiple opioid prescriptions from different providers—a clear red flag of “doctor shopping”—the pharmacist has a responsibility to not fill those prescriptions and notify the respective prescribers. Preliminary data suggest that PDMPs may be beneficial in reducing opioid misuse and poisoning when fully implemented in practice settings.24–25 These situations also present the pharmacist with an opportunity to engage in a dialogue with the patient about opioid safety, addiction, and the availability of naloxone.
Pharmacists can also prevent diversion of prescription drugs to the community by educating their customers about proper storage and disposal of their medications. One third of people who misuse opioids get them from their own prescriptions; over 50 percent get them from family and friends who have prescriptions, obtaining them via purchase, theft, or being given the pills.22,26 Data suggest that 25–66 percent of people who experience a fatal overdose use opioids from another person’s prescription.27
A recent systematic review found that 42% to 71% of the opioid tablets obtained via prescription by surgical patients went unused; most of those unused pills were not properly disposed of or securely stored, leaving them readily available to be misused, stolen, or otherwise diverted.28 Pharmacists can advise patients on the danger (and illegality) of “loaning” pills to others such as family members and on the need to keep opioids inaccessible to children or visitors in their home. They can also inform patients of the need to dispose of unused medications and provide information about prescription drug take-back or disposal opportunities in their community.29
Pharmacists must strike a difficult balance between protecting the community from diversion of opioids and making sure people who need these medications to treat acute or chronic pain can get them unimpeded and are not stigmatized or suspected of being “addicts.” It may be difficult to distinguish physical dependence on opioids (i.e., the tolerance and withdrawal that is seen in nearly any chronic use of opioids) from the compulsive drug seeking that characterizes the behavioral dysregulation of addiction. Estimates vary, but only a minority of patients with chronic pain are addicted to their medication.30 By and large, the dangers of diversion also do not come from patients with chronic pain; these patients may not be as liable to readily share or sell their medications, since they are mindful of not running out. A bigger diversion risk comes from patients who only use a limited number of pills prescribed after an injury or surgery, for example.28 Importantly, pharmacists can be a critical part of the patient care team, helping to educate their patients as well as other providers about non-opioid pain care options, including self-care, over-the-counter products, non-opioid medications, and nonpharmacological treatments.
Overlapping with protecting the community is protecting the patient, of course. Here is where the pharmacist can be an important second line of defense of the patient’s health and safety, since even prescribers with the best intentions may not have experience with pain management and addiction and also may not be fully aware of complicating factors like other medications the patient is taking. A retrospective cohort study among 2,848 patients who overdosed nonfatally on opioids prescribed for their noncancer pain found that 91 percent were still prescribed opioids after the overdose event; 63 percent had ongoing prescribed high-dose opioid analgesics in the 2 years following their overdose—most by the same doctors as before—and 17 percent of those receiving high-dose opioids overdosed again within that time.31 Since the initial overdoses in that study occurred between 2000 and 2012, most were before the various initiatives and recommendations to more strictly limit prescribing and the increased awareness among physicians about overprescribing, but this study still highlights how easy it is for prescribers to overlook clear warning signs and fail to modify their treatment accordingly.
Prescribers may be unaware of what prescriptions their patients may be getting from other doctors, or even may be unaware of harmful interactions between opioids and other drugs they themselves are prescribing. For instance, many individuals who overdose on opioids are also receiving benzodiazepines, which raises overdose risk as these sedatives also cause respiratory depression.19 In the Larochelle et al., cohort study of patients who had nonfatally overdosed, 33–39 percent of patients still receiving opioids after their overdose were also prescribed benzodiazepines.31 Other research documents that the same clinician frequently prescribes both the opioid and the benzodiazepine.32 Additionally, patients taking opioids with selective serotonin reuptake inhibitors for depression may be at higher risk of serotonin syndrome, prompting the FDA to issue a warning in 2016 about use of these medications together.33 Pharmacists can educate physicians and other prescribers about complex drug interactions and alert them about their patients’ prescriptions from other prescribers.
Targeting the availability and distribution of overdose reversing drugs such as naloxone is a key part of the HHS Opioid Strategy21,34, and it is an area where pharmacists are already, very appropriately, playing a significant role. Initially, naloxone was principally available from community-based naloxone programs, but in 2014, the FDA approved the auto-injector formulation Evzio; the FDA also approved an easy-to-use intranasal formulation, Narcan Nasal Spray, in 2015. Coupled with the rapid proliferation of state laws enabling naloxone dispensing under a “standing order”, collaborative practice agreement, or pharmacist prescriptive authority35, between late 2013 and early 2015, there was a 1,170 percent increase in prescriptions of naloxone being dispensed at retail pharmacies36.
Since persons other than the patient—often a family member or friend—will actually be administering naloxone in an emergency, it is important for pharmacists to educate not only the patient but the third party in its use. Educational materials may accompany the medication and also are available online or through various pharmacies. The pharmacist may also assess the competency of the patient and third party to call 911, perform rescue breaths, check for pulse, prepare and administer naloxone, assess the response, and repeat if necessary.37
Naloxone has minimal side effects, so has few risks on its own. The biggest risks are that a person who has been resuscitated by a bystander may not seek emergency care afterward and that one administration of naloxone might not be enough and the person could experience persistent or recurrent respiratory depression. This is increasingly the case with overdoses involving fentanyl and other powerful synthetic opioids.38 Thus, when dispensing naloxone, pharmacists should reinforce the importance of seeking medical care immediately after use of naloxone.
When dispensing naloxone, pharmacists can also remind the patient of the local Good Samaritan laws in their state. Many states have criminal and civil liability immunity for first responders or bystanders who call for help or use naloxone to revive someone who has overdosed.35 Making patients aware of these protections, where they exist, may prevent a bystander’s undue hesitation or reluctance to intervene in an emergency.
Given their access to information that can reveal problematic prescribing, pharmacists are in a unique position not only to identify patients at risk but also to educate their patients about opioid misuse and the potential of addiction treatment to help with their problem. Obtaining a pain prescription or naloxone at the pharmacy may be one of the few points, other than when visiting their primary care physician or an emergency department, at which a person with an opioid use disorder intersects with a medical authority. Practicing pharmacists may be able to use their authority and trusting relationship patients to encourage those who may be misusing opioids to seek treatment from a qualified provider or clinic.
A study of community pharmacists in Tennessee found that over a quarter (26%) had provided information on addiction treatment facilities to one or more patients. The authors also identified modifiable factors that could enhance the likelihood of pharmacists providing such information, such as availability of treatment facility information, confidence in discussing treatment facility options, and having engaged in continuing education about prescription opioid abuse.39
Although pharmacies have not historically been seen as sites for intervention, there is no reason they should not provide information on treatment opportunities and encouragement to use them. The U.S. Department of Health and Human Services is similarly encouraging a broader range of health providers and public safety personnel to link people to treatment or at least recommend treatment when given the opportunity, such as after administering naloxone to reverse overdose.
Potential for Research
Pharmacists conducting research in private laboratories and at universities also have a role in the initiatives designed to address the opioid problem. Developing new or improved overdose prevention and reversal medications, new addiction treatment medications, and new non-addictive or even non-pharmacological treatments for pain are key priorities in the federal-led initiatives to end the opioid crisis. To this end, the National Institutes of Health has pledged to halve the time necessary to develop new therapeutics through government partnerships with industry and academia.40 This is clearly an area where research pharmacists will have an important role to play in drug development, basic science research on opioid pharmacology, as well as clinical and implementation research.
Avenues for research into novel pharmacotherapies for pain include compounds that interact with the opioid system to impede pain signaling but without producing reward or respiratory depression. Biased agonists at the mu-opioid receptor represent one interesting avenue of research.41 Research on cannabinoids, antagonists at the sodium channel NAv 1.7, and compounds that target inflammatory responses are also showing promise.40 Biologics like vaccines that neutralize the drug before it reaches the brain have also been successful in early studies.42 In the short term, we are likely to see new formulations of existing medications (buprenorphine, methadone, and naltrexone), including depot injections that will enhance the reach and effectiveness of these drugs, especially in rural communities where access to healthcare may be limited. New formulations of naloxone, and other overdose-reversal tools, are also in need of development, given reports of high-potency synthetics not being effectively reversed with existing naloxone dosages.38,40
Implementation research is also needed. The Comprehensive Addiction and Recovery Act signed into law in 2016 now allows pharmacists to partially fill prescriptions for Schedule II drugs. So far, there are no data on whether this provision is being implemented or if it is having an effect on reducing excess environmental availability of opioids. Thus, an opportunity for research pharmacists is determining how many pharmacies are taking advantage of this legislation and whether it is making a difference in reducing diversion or misuse. Even a single small study could be an important contribution in this area.
While it is easy to ask practicing pharmacists to make routine, regular use of their state PDMPs to detect inappropriate or dangerous prescribing, integrating PDMP use into standard business practices in a fast-paced customer-service setting poses real challenges. This is another area where implementation research is needed and where pharmacists can play an essential role.3,43 Also needed is research testing and developing strategies to enhance pharmacists’ ability and confidence in communicating about opioid misuse, overdose, and treatment options with patients and in collaborating with physicians around opioid use disorder screening, prevention, and treatment referral.39
Research into the feasibility of daily dispensing of methadone through pharmacies instead of only through certified opioid treatment programs is also needed. Access to medication-assisted treatment is currently very limited, and stigma is one of several impediments to wider adoption. Pharmacies are sites of methadone distribution in many parts of the world44, and physician office-based methadone maintenance via community pharmacy dispensing was implemented successfully in New Mexico.45 Expanding such an approach appears to be a promising way to increase access to a very effective opioid use disorder treatment, help destigmatize it, and further the integration of addiction treatment into the rest of the healthcare system.
Potential for education
Pharmacists at universities and pharmacy schools play a role in educating students and each other about pain pharmacotherapy and addiction. One of the many contributing factors to the opioid crisis was the minimal education these about two crucial, complexly interconnected areas by U.S. medical, dental, and pharmacy schools. For example, a large proportion of U.S. medical schools offer less than 5 hours of instruction on pain.46 Schools of pharmacy may be able to address this gap in their own curricula and in any affiliated schools for other health professionals. Because of a leading role of pharmacists in interprofessional collaboration, educational efforts may extend well beyond pharmacy students themselves.
Conclusions
Mitigating the impact of opioid addiction and preventing opioid overdose deaths should be a focus for pharmacists.3,37,47 This is true most obviously in a community pharmacy setting, where the practicing pharmacist can be vigilant for signs of misuse by patients, inappropriate prescribing by physicians, or hazards from different prescriptions (e.g., opioids and benzodiazepines) that may come from different prescribers, and they can also be an important resource for information for patients about safe use of medications. Community pharmacies’ role in dispensing naloxone is increasing, as is their potential for dispensing addiction treatment medications—not only naltrexone and buprenorphine but potentially methadone in the near future. And for patients who show signs of opioid misuse or addiction, pharmacists can provide information on effective treatment options in their community. Pharmacists in research labs and pharmacy schools can also be actively involved in developing new pain and addiction treatments and in promoting up-to-date science on pain management, opioid addiction, and their complex interrelationships. The severity and complexity of the opioid crisis demand such participation by all components of the health care system.21
Acknowledgments
Disclaimers: The findings and conclusions of this study are those of the authors and do not necessarily reflect the views of the National Institute on Drug Abuse of the National Institutes of Health, or the Office of the Assistant Secretary for Planning and Evaluation of the U.S. Department of Health and Human Services.
Footnotes
Conflict of Interest Disclosures: Compton reports ownership of stock in General Electric Co., 3M Co., and Pfizer Inc., unrelated to the submitted work.
References
- 1.Rudd RA, Seth P, David F, Scholl L. Increases in Drug and Opioid-Involved Overdose Deaths — United States, 2010–2015. MMWR Morb Mortal Wkly Rep 2016;65. doi: 10.15585/mmwr.mm655051e1. [DOI] [PubMed] [Google Scholar]
- 2.National Center for Health Statistics. (2017) Provisional counts of drug overdose deaths as of 8/6/2017. Available at: https://www.cdc.gov/nchs/data/health_policy/monthly-drug-overdose-death-estimates.pdf. Accessed September 26, 2017. [Google Scholar]
- 3.Wu L-T, Ghitza UE, Burns AL, Mannelli P. The opioid overdose epidemic: opportunities for pharmacists. Substance Abuse and Rehabilitation. 2017;8:53–55. doi: 10.2147/SAR.S144268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.King NB, Fraser V, Boikos C, Richardson R, Harper S. Determinants of increased opioid-related mortality in the United States and Canada, 1990–2013: a systematic review. Am J Public Health 2014;104(8):e32–e42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jones CM. The Latest Prescription Trends for Controlled Prescription Drugs. September 15, 2015. Available from: https://www.drugabuse.gov/news-events/meetings-events/2015/09/latest-prescription-trends-controlled-prescription-drugs. Accessed September 25, 2017. [Google Scholar]
- 6.Jones CM. Heroin use and heroin use risk behaviors among nonmedical users of prescription opioid pain relievers – United States, 2002–2004 and 2008–2010. Drug and Alcohol Dependence 2013;132(1–2):95–100. [DOI] [PubMed] [Google Scholar]
- 7.Compton WM, Jones CM, Baldwin GT. Understanding the relationship between prescription opioid and heroin abuse. New England Journal of Medicine. 2016;374:154–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Center for Behavioral Health Statistics and Quality (CBHSQ). 2015 National Survey on Drug Use and Health: Detailed Tables. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2016. [Google Scholar]
- 10.Humphreys K The federal government is systematically undercounting heroin users. Washington Post; August 22, 2017 Available from: https://www.washingtonpost.com/news/wonk/wp/2017/08/22/the-federal-government-is-systematically-under-counting-heroin-users/?utm_term=.de0f1ec7af7d. [Google Scholar]
- 11.Compton WM, Dawson D, Duffy SQ, Grant BF. The Effect of Inmate Populations on Estimates of DSM-IV Alcohol and Drug Use Disorders in the United States. American Journal of Psychiatry 2010;167:473–475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jones CM, Christensen A, Gladden RM. Increases in prescription opioid injection abuse among treatment admissions in the United States, 2004–2013. Drug Alcohol Dependence. 2017;176:89–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zibbell JE, Iqbal K, Patel RC, Suryaprasad A, Sanders KJ, Moore-Moravian L, Serrecchia J, Blankenship S, Ward JW, Holtzman D. Increases in Hepatitis C Virus Infection Related to Injection Drug Use Among Persons Aged ≤30 Years — Kentucky, Tennessee, Virginia, and West Virginia, 2006–2012. Morb Mort Weekly. 2015;64(17):453–458. [PMC free article] [PubMed] [Google Scholar]
- 14.Peters PJ, Pontones P, Hoover KW, et al. HIV infection linked to injection use of oxymorphone in Indiana, 2014–2015. New England Journal of Medicine, 375 (3) (2016), pp. 229–239, 10.1056/NEJMoa1515195 [DOI] [PubMed] [Google Scholar]
- 15.Tolia VN, Patrick SW, Bennett MM, Murthy K, Sousa J, Smith PB, Clark RH, Spitzer AR. Increasing incidence of the neonatal abstinence syndrome in U.S. neonatal ICUs. N Engl J Med. 2015;372:2118–26. [DOI] [PubMed] [Google Scholar]
- 16.Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain—United States, 2016. JAMA. 2016;315(15):1624–1645. doi: 10.1001/jama.2016.1464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Muhuri PK, Gfroerer JC, Davies MC. Associations of nonmedical pain reliever use and initiation of heroin use in the United States. CBHSQ [Center for Behavioral Health Statistics and Quality] Data Review (2013, August). Available at: http://www.samhsa.gov/data/2k13/DataReview/DR006/nonmedical-pain-reliever-use-2013.htm. Accessed September 25, 2017. [Google Scholar]
- 18.Meier A, Moore SK, Saunders EC, Metcalf SA, McLeman B, Auty S, Marsch LA. NDEWS HotSpot report: understanding opioid overdoses in New Hampshire. 2017. Available at: https://ndews.umd.edu/publications/hotspot-report-understanding-opioid-overdoses-new-hampshire. Accessed September 26, 2017.
- 19.Jones CM, McAninch JK.. Emergency department visits and overdose deaths from combined use of opioids and benzodiazepines. American Journal of Preventive Medicine, 49 (4) (2015), pp. 493–501. [DOI] [PubMed] [Google Scholar]
- 20.Solimini R, Rotolo MC, Pellegrini M, Minutillo A, Pacifici R, Busardò FP, Zaami S. Adulteration practices of psychoactive illicit drugs: an updated review. Curr Pharm Biotechnol 2017. Jul 10. doi: 10.2174/1389201018666170710184531. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 21.Price TE. Secretary Price Announces HHS Strategy for Fighting Opioid Crisis. Available at: Pain Med, 13 (3) (2012), pp. 434–442.22299725 [Google Scholar]
- 22.Han B, Compton WM, Blanco C, Crane E, Lee J, Jones CM. Prescription opioid use, misuse, and use disorders in the U.S. adults: 2015 National Survey on Drug Use and Health. Annals of Internal Medicine 2017;167(5):293–301. [DOI] [PubMed] [Google Scholar]
- 23.Haegerich TM, Paulozzi LJ, Manns BJ, Jones CM. What we know, and don’t know, about the impact of state policy and systems-level interventions on prescription drug overdose. Drug Alcohol Depend, 145 (2014), pp. 34–47, 10.1016/j.drugalcdep.2014.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Reifler LM, Droz D, Bailey JE, et al. Do prescription monitoring programs impact state trends in opioid abuse/misuse? Pain Med, 13 (3) (2012), pp. 434–442, 10.1111/j.1526-4637.2012.01327.x [DOI] [PubMed] [Google Scholar]
- 25.Patrick SW, Fry CE, et al. (2016) Implementation of Prescription Drug Monitoring Programs Associated With Reductions in Opioid Related Death Rates. HEALTH AFFAIRS 35, NO. 7 (2016): 1324–1332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jones CM, Paulozzi LJ, Mack KA. Sources of Prescription Opioid Pain Relievers by Frequency of Past-Year Nonmedical UseUnited States, 2008–2011. JAMA Intern Med. 2014;174(5):802–803. doi: 10.1001/jamainternmed.2013.12809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Centers for Disease Control and Prevention (CDC) CDC grand rounds: prescription drug overdoses – a U.S. epidemic. MMWR Morb Mortal Wkly Rep 2012;61:10–13. [PubMed] [Google Scholar]
- 28.Bicket MC, Long JJ, Pronovost PJ, Alexander GC, Wu CL. Prescription Opioid Analgesics Commonly Unused After Surgery: A Systematic Review. JAMA Surg Published online August 02, 2017. doi: 10.1001/jamasurg.2017.0831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gray JA, Hagemeier NE. Prescription Drug Abuse and DEA-Sanctioned Drug Take-Back Events: Characteristics and Outcomes in Rural Appalachia. Arch Intern Med 2012;172(15):1186–1187. doi: 10.1001/archinternmed.2012.2374 [DOI] [PubMed] [Google Scholar]
- 30.Minozzi S, Amato L and Davoli M (2013), Development of dependence following treatment with opioid analgesics for pain relief: a systematic review. Addiction, 108: 688–698. doi: 10.1111/j.1360-0443.2012.04005.x [DOI] [PubMed] [Google Scholar]
- 31.Larochelle MR, Liebschutz JM, Zhang F, Ross-Degnan D, Wharam JF. Opioid Prescribing After Nonfatal Overdose and Association With Repeated Overdose: A Cohort Study. Ann Intern Med. 2016;164(1):1–9. [DOI] [PubMed] [Google Scholar]
- 32.Hwang CS, Kang EM, Kornegay CJ, Staffa JA, Jones CM, McAninch JK. Trends in the Concomitant Prescribing of Opioids and Benzodiazepines, 2002–2014. Am J Prev Med 2016;51(2):151–160. [DOI] [PubMed] [Google Scholar]
- 33.U.S. Food and Drug Administration. FDA Drug Safety Communication: FDA warns about several safety issues with opioid pain medicines; requires label changes. Available at: https://www.fda.gov/Drugs/DrugSafety/ucm489676.htm. Accessed September 25, 2017.
- 34.Morton Kate J. et al. Pharmacy-based statewide naloxone distribution: A novel “top-down, bottom-up” approach. Journal of the American Pharmacists Association. 2017;57(2):S99–S106.e5 [DOI] [PubMed] [Google Scholar]
- 35.Science Legal. 2017. Available at: http://www.pdaps.org/dataset/overview/laws-regulating-administration-of-naloxone/5977b661d42e07f31dcafb6e. Accessed September 25, 2017.
- 36.Jones CM, Lurie PG, Compton WM. Increase in Naloxone Prescriptions Dispensed in US Retail Pharmacies Since 2013. American Journal of Public Health 2016;106:689–690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bailey AM, Wermeling DP. Naloxone for Opioid Overdose Prevention: Pharmacists’ Role in Community-Based Practice Settings. The Annals of pharmacotherapy. 2014;48(5):601–606. doi: 10.1177/1060028014523730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Klebacher R, Harris MI, Ariyaprakai N, Tagore A, Robbins V, Dudley LS, Bauter R, Koneru S, Hill RD, Wasserman E, Shanes A, Merlin MA. Incidence of Naloxone Redosing in the Age of the New Opioid Epidemic. Prehospital Emergency Care, DOI: 10.1080/10903127.2017.1335818 [DOI] [PubMed] [Google Scholar]
- 39.Hagemeier NE, Alamian A, Murawski MM, Pack RP. Factors associated with provision of addiction treatment information by community pharmacists. J Subst Abuse Treat. 2015;52:67–72. [DOI] [PubMed] [Google Scholar]
- 40.Volkow ND, Collins F. SThe Role of Science in Addressing the Opioid Crisis. N Engl J Med 2017; 377:391–394 July 27, 2017. DOI: 10.1056/NEJMsr1706626 [DOI] [PubMed] [Google Scholar]
- 41.Huang W, Manglik A, Venkatakrishnan AJ, et al. Structural insights into μ-opioid receptor activation. Nature 2015;524:315–321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kinsey B Vaccines against drugs of abuse: where are we now? Ther Adv Vaccines. 2014. Jul; 2(4): 106–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Green TC, Mann MR, Bowman SE, et al. How does use of a prescription monitoring program change pharmacy practice? J Am Pharm Assoc (2003) 2013;53(3):273–281 [DOI] [PubMed] [Google Scholar]
- 44.Luger L, Bathia N, Alcorn R, Power R . Involvement of community pharmacists in the care of drug misuers: pharmacy-based supervision of methadone consumption. International J of Drug Policy 2000;11(3):227–234. [DOI] [PubMed] [Google Scholar]
- 45.Tuchman E, Gregory C, Mitchell S, Drucker Ernest. Safety, efficacy, and feasibility of office-based prescribing and community pharmacy dispensing of methadone: results of a pilot study in New Mexico. Addictive Disorders & Their Treatment 2006;5(2):43–51. [Google Scholar]
- 46.Mezei L, Murinson BB. Pain Education in North American Medical Schools. The Journal of Pain 2011;12(12):1199–1208. 10.1016/j.jpain.2011.06.006. [DOI] [PubMed] [Google Scholar]
- 47.American Society of Health-System Pharmacists (ASHP) ASHP statement on the pharmacist’s role in substance abuse prevention, education, and assistance. Am J Health Syst Pharm 2014;71(3):243–246. [DOI] [PubMed] [Google Scholar]